Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Emphysema Brochure
Caricato da
api-2423943020 valutazioniIl 0% ha trovato utile questo documento (0 voti)
501 visualizzazioni2 pagineTitolo originale
emphysema brochure
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
501 visualizzazioni2 pagineEmphysema Brochure
Caricato da
api-242394302Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 2
A permanent, abnormal enlargement of gas-
exchange airways, with destruction of alveolar
walls, without fibrosis (2).
SYDONIE STOCK
RESOURCES
(1) Chronic obstructive pulmonary disease among
adults - United States, 2011. (2012). MMWR:
Morbidity & Mortality Weekly Report, 61938-943.
(2) Huether, Sue & McCance, Kathryn. (2012).
Understanding Pathophysiology (5
th
ed) p.693-4.
St. Louis, MO: Elsevier Mosby Inc.
(3) Ladwig, Gail & Ackley, Betty. (2011). Mosbys
guide to nursing diagnosis (3
rd
ed). Maryland
Heights, MO: Mosby Inc.
(4) Lynn, Pamela. (2011). Clinical nursing skills: A
nursing process approach (3
rd
ed). Philadelphia,
PA: Lippincott, Williams & Wilkins.
(5) Mitzner, W. (2011). Emphysema--a disease of
small airways or lung parenchyma? New England
Journal of Medicine, 365(17), 1637-1639.
(6)Tabloski, Patricia. (1995). NCLEX Review
Questions. Gerontological Nursing. Chapter 16.
Pearson.
All pictures were found in Google Images. Emphysema
patient.
What is Emphysema?
The accepted definition of emphysema is a
permanent, abnormal enlargement of acini with
destruction of alveolar walls without fibrosis (2).
Etiology There could be two different ways
emphysema forms. One way is the commonly
accepted explanation: inflammation of the alveoli
leads to the destruction of the alveolar walls and
the elastic fibers that connect the acini to the
terminal bronchiole, which causes airway
enlargement and narrowing of the small airway at
the bronchiole opening. The other explanation
could be that the small airway is narrowed and
obstructed by inflammation. The resulting
increased pressure in the acini would cause folding
and breaking of the alveolar walls and destruction
of the elastic fibers (5).
Incidence COPD, the category of pulmonary
disorders that emphysema falls under, became the
third leading cause of death in 2008. According to
a randomized national telephone survey, whose
participation average was 74.2%, approximately 15
million people have been diagnosed with COPD by
their physician. More than 11.6% of this population
was 65 years or older (1).
Risk Factors There are two categories of
emphysema: primary and secondary. Primary
emphysema is associated with an inherited
deficiency of the enzyme 1-antitrypsin [which]
inhibits the action of many proteolytic enzymes.
Without this enzyme, there is a greater chance the
patient will develop emphysema due to proteolysis
in the lung tissue (2). Secondary emphysema is
caused by inhalation of cigarette smoke. Other
contributing factors are air pollution, occupational
exposure, and childhood respiratory tract
infections (2).
Pathophysiology With the inhalation of tobacco
smoke or chemicals, antiproteases are inhibited
while inflammation and protease activity are
stimulated. This stimulation promotes alveolar
destruction by cellular apoptosis and senescence.
The alveolar destruction produces bullae, large air
spaces in the lung parenchyma, and blebs, air
spaces by the pleurae. The bullae and blebs do not
promote gas exchange and the result is an
alteration to the ventilation-perfusion ratio, leading
to hypoxemia. The barrel chest appearance is
caused by air trapped within the lung, resulting in
hyperexpansion of the chest. This stretches the
muscles used during respiration and more effort is
required during breathing (2).
NCLEX Questions (6)
All of the following nursing diagnoses are
important for a client with chronic pulmonary
emphysema (COPD). Which would receive
priority when planning nursing interventions?
A. Self-care deficit
B. Activity intolerance
C. Ineffective airway clearance
D. Impaired gas exchange
Answer: D
Which of the following interventions would be a
priority in the plan of care for the person with
pulmonary emphysema?
A. Intravenous ampicillin therapy
B. Maintaining hydration status
C. Low-flow oxygen via face mask
D. Intravenous aminophylline
Answer: C
EMPHYSEMA
Lifespan and Cultural Considerations
Emphysema typically affects the older generation. In
the survey mentioned previously, 3.2% of those
diagnosed with COPD were between the ages of 18
and 44 while more than 11.6% were 65 years or
more. The subjects could have been diagnosed with
COPD, emphysema, or chronic bronchitis (1). If the
younger generation was in fact diagnosed with
emphysema, it was most likely primary emphysema
(2).
Culturally, those diagnosed with emphysema would
have a history of inhaled tobacco use, additionally
they could have had exposure to inhaled chemicals
either in their place of employment or simply have
lived in a highly polluted area (2).
CLINICAL MANIFESTATIONS
The classic sign of emphysema is the barrel
chest and a prolonged expiration is always
present. The common manifestations are
dyspnea and wheezing. Most likely, the patient
has a history of smoking. Late in the course of
the disease, the patient may present with chronic
hypoventilation, polycythemia, or cor pulmonale.
If there is an infection with the emphysema, the
patient could have a productive cough as well (2).
PINK PUFFER
BULLAE
WHAT IS EMPHYSEMA?
DIFFERENCES SHOWN
CAUSE & EFFECT
Impaired gas exchange related to ventilation-
perfusion inequality (3).
The client will verbalize understanding of
oxygen supplementation and other
therapeutic interventions by day two (3).
Noncompliance related to reluctance to accept
responsibility for changing detrimental health
practices (3).
The client will review emphysema literature
and verbally admit responsibility for the
current health state by day five.
Imbalanced nutrition: less than body
requirements related to decreased intake
because of dyspnea (3).
The client will consume adequate
nourishment during at least five meals in one
week (3).
COMPLICATIONS
Complications that could be associated with
emphysema are related to the increased effort it
takes to breathe and to chronic inflammation of
the airways. Because there is greater resistance
against the respiratory muscles, respiratory
fatigue could develop after a while. This fatigue
may lead to hypoventilation and hypercapnia.
Inflammation could result in bronchi
hyperreactivity and bronchioconstriction, making
breathing even more difficult. Chronic
inflammation could also have systemic affects.
Weight loss, muscle weakness, and increased
susceptibility to comorbidities, such as infection
could all be caused by chronic inflammation of
the airways (2).
NURSING DIAGNOSES
SIGNIFICANCE TO NURSING
Emphysema has a significant impact on nursing
and respiratory therapists. When treating an
emphysema patient, the nurse needs to
remember the fragile state the patients lungs are
in. With any COPD patient, the nurse has to take
care not to force too much oxygen into the lungs
because this could rupture the already damaged
alveoli. The highest level should be no greater
than 3 L/min (4). Also, with the advancing age of
the baby boomer generation, there could be an
increase in patients diagnosed with emphysema.
I know a 79 year old male who was diagnosed
with emphysema within the last year.
Potrebbero piacerti anche
- Sam CD Asthma ReciveredDocumento36 pagineSam CD Asthma ReciveredDr. Muha. Hasan Mahbub-Ur-RahmanNessuna valutazione finora
- SL NO Content NODocumento12 pagineSL NO Content NOPdianghunNessuna valutazione finora
- Acute Lung InjuryDocumento18 pagineAcute Lung InjuryM Rizal IsburhanNessuna valutazione finora
- Practice Mod 6 Case StudyDocumento6 paginePractice Mod 6 Case Studyvanessa100% (1)
- Age Related Changes in Respiratory System I. Structural Changes 1. Lung Elasticity: II. Functional ChangesDocumento4 pagineAge Related Changes in Respiratory System I. Structural Changes 1. Lung Elasticity: II. Functional ChangesElienai de LeonNessuna valutazione finora
- Chronic Obstructive Pulmonary Disease: Respiratory Infection DepressionDocumento6 pagineChronic Obstructive Pulmonary Disease: Respiratory Infection Depressionjenn212Nessuna valutazione finora
- Acute Severe AsthmaDocumento5 pagineAcute Severe AsthmaRizsa Aulia DanestyNessuna valutazione finora
- Description: Chronic Bronchitis EmphysemaDocumento16 pagineDescription: Chronic Bronchitis EmphysemaJay-ar Zars0% (1)
- Nur 111 Session 1 Sas 1Documento8 pagineNur 111 Session 1 Sas 1Zzimply Tri Sha UmaliNessuna valutazione finora
- HSNS264 Assessment 1Documento6 pagineHSNS264 Assessment 1Sophie AndersonNessuna valutazione finora
- Nursing Respiratory System "COPD (Chronic Obstructive Pulmonary Disease) "Documento15 pagineNursing Respiratory System "COPD (Chronic Obstructive Pulmonary Disease) "ilhamNessuna valutazione finora
- Chronic Obstructive Pulmonary DiseaseDocumento37 pagineChronic Obstructive Pulmonary Diseasematchees-gone rogueNessuna valutazione finora
- CopdDocumento14 pagineCopdMohd Farid Bin RosliNessuna valutazione finora
- Chronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDocumento12 pagineChronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDiana Jalaynie S. SambolawanNessuna valutazione finora
- Chronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDocumento12 pagineChronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDiana Jalaynie S. SambolawanNessuna valutazione finora
- Inflammation OverviewDocumento44 pagineInflammation OverviewMegan MorenoNessuna valutazione finora
- CopdDocumento60 pagineCopdRizqy Shofianingrum100% (1)
- Chronic Obstructive Pulamonary DiseaseDocumento12 pagineChronic Obstructive Pulamonary Diseaseanamika sharmaNessuna valutazione finora
- Practice EamDocumento35 paginePractice EamMYKRISTIE JHO MENDEZNessuna valutazione finora
- Natalia - 130110110190 - E3/Respi: Chronic Obstructive Pulmonary Disease (COPD) - DeaDocumento5 pagineNatalia - 130110110190 - E3/Respi: Chronic Obstructive Pulmonary Disease (COPD) - DeaMarshel BudiarsaNessuna valutazione finora
- Case Vignette Analysis (Pediatric Case) I. QuestionsDocumento2 pagineCase Vignette Analysis (Pediatric Case) I. QuestionsMadelaine EvangelioNessuna valutazione finora
- Comprehensive Case Study On A Client With Chronic Obstructive PulmonaryDocumento19 pagineComprehensive Case Study On A Client With Chronic Obstructive PulmonaryDayannara AliNessuna valutazione finora
- Chronic Obstructive Pulmonary DiseaseDocumento8 pagineChronic Obstructive Pulmonary DiseaseYessamin Paith RoderosNessuna valutazione finora
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDocumento17 pagineAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengNessuna valutazione finora
- Chronic Obstructive Pulmonary Disease: BY: Hermio, Ruvy Ruthe SDocumento49 pagineChronic Obstructive Pulmonary Disease: BY: Hermio, Ruvy Ruthe SKareem WaheedNessuna valutazione finora
- The EssayDocumento33 pagineThe EssayAnonymous bLaVaKSbdBNessuna valutazione finora
- Chronic Obstructive Pulmonary Disease: Laily Hidayati, S.Kep., NS., M.KepDocumento55 pagineChronic Obstructive Pulmonary Disease: Laily Hidayati, S.Kep., NS., M.KepGlory Stefanny NorotumilenaNessuna valutazione finora
- Hide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyDocumento29 pagineHide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyAngie Mandeoya100% (1)
- Acute Respiratory Distress SyndromeDocumento21 pagineAcute Respiratory Distress Syndromemisseve252100% (1)
- Chronic Obstructive Pulmunary DiseaseDocumento39 pagineChronic Obstructive Pulmunary DiseaseshaitabliganNessuna valutazione finora
- Acute Respiratory Distress SyndromeDocumento9 pagineAcute Respiratory Distress SyndromeMatthew Ryan100% (2)
- Topic 2 COPD and AsthmaDocumento18 pagineTopic 2 COPD and AsthmaCaitlynNessuna valutazione finora
- Systems Plus College Foundation Macarthur Highway, Balibago, Angeles CityDocumento13 pagineSystems Plus College Foundation Macarthur Highway, Balibago, Angeles CityLeanne Princess GamboaNessuna valutazione finora
- Case Study Copd P. CongestionDocumento80 pagineCase Study Copd P. CongestionBryant Riego IIINessuna valutazione finora
- UMTC PCAP - C Case StudyDocumento17 pagineUMTC PCAP - C Case StudyMary Ann Credo Manlangit100% (2)
- Mostafa 33 2Documento12 pagineMostafa 33 2Ahmed AshrafNessuna valutazione finora
- DR Ambreen Shams NephrologistDocumento58 pagineDR Ambreen Shams NephrologistAamer NaeemNessuna valutazione finora
- Chapter 10 Interstitial Lung DiseaseDocumento10 pagineChapter 10 Interstitial Lung DiseaseAleksandar Tasic100% (1)
- A Care Study On BronchopneumoniaDocumento35 pagineA Care Study On Bronchopneumoniaedna100% (1)
- Asthma and COPD: More InformationDocumento10 pagineAsthma and COPD: More InformationNur SolichahNessuna valutazione finora
- Copd 2Documento26 pagineCopd 2Abid SunhanNessuna valutazione finora
- Pathophysiology of COPD - The BasicsDocumento11 paginePathophysiology of COPD - The BasicstiaranindyNessuna valutazione finora
- Emphysema Is A LongDocumento54 pagineEmphysema Is A LongryemoralesNessuna valutazione finora
- CR Patho SummaryDocumento22 pagineCR Patho SummaryDNAANessuna valutazione finora
- 2019 - Chronic Obstructive Pulmonary Disease andDocumento6 pagine2019 - Chronic Obstructive Pulmonary Disease andAndreea MoalesNessuna valutazione finora
- The Pharmacotherapy of Chronic Obstructive Pulmonary Disease in The ElderlyDocumento14 pagineThe Pharmacotherapy of Chronic Obstructive Pulmonary Disease in The Elderlydanny17phNessuna valutazione finora
- Case Study For EmphysemaDocumento5 pagineCase Study For EmphysemaGabbii CincoNessuna valutazione finora
- FPI Progn TratDocumento13 pagineFPI Progn TratTurcu AndreeaNessuna valutazione finora
- PCRJ 201325Documento13 paginePCRJ 201325ashlyn granthamNessuna valutazione finora
- BSN-3 M6bcdDocumento26 pagineBSN-3 M6bcdZel Natulla MoranoNessuna valutazione finora
- 2copd FinalDocumento2 pagine2copd FinaluikapuNessuna valutazione finora
- COPD Case PresentationDocumento15 pagineCOPD Case PresentationBola Kwentua29% (7)
- COPD Pathology WindowDocumento1 paginaCOPD Pathology WindowKurstie Franks100% (1)
- CopdDocumento3 pagineCopdFawad HameediNessuna valutazione finora
- 1 s2.0 S0929664615003460 MainDocumento7 pagine1 s2.0 S0929664615003460 MainEva GarciaNessuna valutazione finora
- Pathophysiology of Asthma - StatPearls - NCBI BookshelfDocumento7 paginePathophysiology of Asthma - StatPearls - NCBI BookshelfJEAN CERNA SOLISNessuna valutazione finora
- Asthma Thesis TopicsDocumento5 pagineAsthma Thesis Topicsgjfcp5jb100% (1)
- Copd: Defining and Magnitude of ProblemDocumento37 pagineCopd: Defining and Magnitude of ProblemSiti AmandaNessuna valutazione finora
- Sydonie Stock ResumeDocumento2 pagineSydonie Stock Resumeapi-242394302Nessuna valutazione finora
- Family Assessment PaperDocumento11 pagineFamily Assessment Paperapi-24239430233% (3)
- Drug HistoryDocumento4 pagineDrug Historyapi-242394302Nessuna valutazione finora
- Nurse BurnoutDocumento6 pagineNurse Burnoutapi-242394302Nessuna valutazione finora
- Reflection On Recognizing and Treating IV InfiltrationDocumento8 pagineReflection On Recognizing and Treating IV Infiltrationapi-242394302Nessuna valutazione finora
- CBSE Class 7 Science MCQs-Respiration in OrganismsDocumento2 pagineCBSE Class 7 Science MCQs-Respiration in Organismssiba padhy100% (3)
- Respiratory SystemDocumento25 pagineRespiratory Systemlobna HijliNessuna valutazione finora
- Astm ErsDocumento9 pagineAstm ErsAdrian RomanNessuna valutazione finora
- Nursing Care Plan Impaired Gas ExchangeDocumento1 paginaNursing Care Plan Impaired Gas Exchangecuicuita100% (3)
- H2A019109 - Annisa R.A Putri - Last StepDocumento8 pagineH2A019109 - Annisa R.A Putri - Last Step109 -Annisa RANessuna valutazione finora
- Oxygenation ProblemsDocumento4 pagineOxygenation ProblemsAlec Xavier MirandaNessuna valutazione finora
- Apnea of Prematurity: UnderstandingDocumento2 pagineApnea of Prematurity: UnderstandingEmil JaniakNessuna valutazione finora
- An Detailed Lesson Plan For Circulatory and Respiratory SystemDocumento9 pagineAn Detailed Lesson Plan For Circulatory and Respiratory SystemclarisseNessuna valutazione finora
- Woc ArdsDocumento2 pagineWoc Ardssyarifah salmaNessuna valutazione finora
- Respirator LangmanDocumento10 pagineRespirator LangmanSavu MalinaNessuna valutazione finora
- Grade 9 ScienceDocumento19 pagineGrade 9 ScienceChristine Grace GiradoNessuna valutazione finora
- COPDDocumento25 pagineCOPDCharles S. Williams RRT, AE-C100% (3)
- Respiratory - Gas ExchangeDocumento3 pagineRespiratory - Gas ExchangeChris P. BeaconNessuna valutazione finora
- Fathur Rahman PDFDocumento1 paginaFathur Rahman PDFRSCERIA KANDANGANNessuna valutazione finora
- Measure Oxygen Uptake by RespirometerDocumento17 pagineMeasure Oxygen Uptake by RespirometerTootsie100% (12)
- Myrna CruzDocumento3 pagineMyrna CruzChris Opal NamocatcatNessuna valutazione finora
- The Respiratory SystemDocumento61 pagineThe Respiratory SystemLuna JadeNessuna valutazione finora
- Auto PEEPDocumento16 pagineAuto PEEPVishwajith Murthy100% (1)
- The Respiratory System: SubtitleDocumento89 pagineThe Respiratory System: SubtitleAaaNessuna valutazione finora
- Mechanics of RespirationDocumento78 pagineMechanics of Respirationnirilib100% (4)
- Pathophysiology of Respiratory System Feghiu I., Tacu L. Lutan VDocumento55 paginePathophysiology of Respiratory System Feghiu I., Tacu L. Lutan VLunguVictoriaNessuna valutazione finora
- Hypoxemic Respiratory FailureDocumento70 pagineHypoxemic Respiratory FailureMohamed Rikarz Ahamed RikarzNessuna valutazione finora
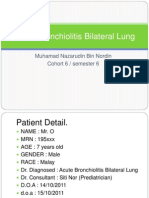
- Acute Bronchiolitis Bilateral Lung Case Study PresentationDocumento36 pagineAcute Bronchiolitis Bilateral Lung Case Study PresentationPyka Izzaty100% (1)
- BiPAP Full FlowchartDocumento1 paginaBiPAP Full FlowchartArjun KumarNessuna valutazione finora
- Respironics V200 DatasheetDocumento4 pagineRespironics V200 DatasheetkrsrinivasarajuNessuna valutazione finora
- Respiratory System: Done By: Daniella DhanesarDocumento25 pagineRespiratory System: Done By: Daniella DhanesarDaniellaNessuna valutazione finora
- Fisioterapi Dada Dan Batuk Efektif Sebagai Penatalaksanaan Ketidakefektifan Bersihan Jalan NafasDocumento7 pagineFisioterapi Dada Dan Batuk Efektif Sebagai Penatalaksanaan Ketidakefektifan Bersihan Jalan NafasFirdaus Martha FriansahNessuna valutazione finora
- Chapter 40. Nursing Care of A Child With Respiratory Disorder TermsDocumento3 pagineChapter 40. Nursing Care of A Child With Respiratory Disorder TermsJœnríčk AzueloNessuna valutazione finora
- 11.1 Gas Exchange in Humans Igcse Cie Biology Ext Theory QP Unlock9bDocumento11 pagine11.1 Gas Exchange in Humans Igcse Cie Biology Ext Theory QP Unlock9bAnnmary AbrahamNessuna valutazione finora
- Breathe Light To Breathe Right - PDF RoomDocumento58 pagineBreathe Light To Breathe Right - PDF Roomfabricio100% (2)