Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Malaria
Caricato da
Cassandra LaoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Malaria
Caricato da
Cassandra LaoCopyright:
Formati disponibili
MALARIA
The word malaria comes from 18th century Italian mala meaning "bad" and aria meaning
"air". The term was first used by Dr. Francisco Torti, Italy, when people thought the disease was
caused by foul air in marshy areas. It was not until 1880 that scientists discovered that malaria
was a parasitic disease which is transmitted by the anopheles mosquito. The mosquito infects the
host with a one-cell parasite called plasmodium. Not long after they found out that Malaria is
transmitted from human-to-human through the bite of the female mosquito, which needs blood
for her eggs.
Malaria is a mosquito-borne infectious disease of humans and other animals caused
by protists (a type of microorganism) of the genus Plasmodium. Infection is initiated by a bite
from an infected female Anopheles mosquito, which introduces the protists via its saliva into the
circulatory system, and ultimately to the liver where they mature and reproduce. Malaria is
widespread in tropical and subtropical regions in a broad band around the equator, including
much of Sub-Saharan Africa, Asia, and the Americas. It is prevalent in tropical regions because
the significant amounts of rainfall, consistently high temperatures and high humidity, along with
stagnant waters in which mosquito larvae readily mature, provide them with the environment
they need for continuous breeding.
History
2700 BC - 340 CE several characteristic symptoms of what would later be named malaria
were described in the Nei Ching, The Canon of Medicine (Chinese). A number of Roman
writers attributed malarial diseases to the swamps.
340 CE The antifever properties of Qinghao plant (artemisinin) were first described by Ge
Hong of the East Yin Dynasty.
1820 Quinine first purified from tree bark. For many years prior, the ground bark had been
used to treat malaria.
1880 Charles Louis Alphonse Laveran first identifies the malaria parasite. He is awarded the
1907 Nobel Prize for the discovery.
1898 Sir Ronald Ross demonstrates that mosquitoes transmit malaria. He wins the 1902
Nobel Prize for this work.
1934 Hans Andersag in Germany discovers the Anti-malarial drug Chloroquine, which is not
widely used until after World War II.
1939 Paul Hermann Muller in Switzerland tests the insecticide DDT. He wins the Nobel
Prize for this work in 1948.
1952 Malaria is eliminated in the United States.
1957 First documented case of resistance to Chloroquine is reported.
1976 William Trager and JB Jensen grow parasite in culture for the first time, opening the
way for drug discovery and vaccine research.
2008 United Nations adopt April 25 as World Malaria Day.
Epidemiology
WHO estimates that there were 216 million cases of malaria in 2010 resulting in 655,000
deaths.
3.3 billion people (half the worlds population) live in areas at risk of malaria transmission in
109 countries and territories.
35 countries (30 in sub-Saharan Africa and 5 in Asia) account for 98% of global malaria
deaths.
89% of the malaria deaths worldwide occur in Africa.
Malaria is the 5th cause of death from infectious diseases worldwide (after respiratory
infections, HIV/AIDS, diarrheal diseases, and tuberculosis).
The majority of cases occur in children under five years old.
Pregnant women are also especially vulnerable. About 125 million pregnant women are at
risk of infection each year, and in sub-Saharan Africa, maternal malaria is associated with an
estimated 200,000 infant deaths yearly.
Philippines: Out of the 79 provinces nationwide, 57 are malaria endemic.
Causative Agent
Five species of Plasmodium can infect and be transmitted by humans. The vast majority
of deaths are caused by P. falciparum while P. vivax, P. ovale, and P. malariae cause a generally
milder form of malaria that is rarely fatal. The zoonotic species P. knowlesi, prevalent in
Southeast Asia, causes malaria in macaques but can also cause severe infections in humans.
There are five types of Malaria:
Plasmodium vivax (P. vivax) - milder form of the disease, generally not fatal. However,
infected people still need treatment because their untreated progress can also cause a host of
health problems. This type has the widest geographic distribution globally. About 60% of
infections in India are due to P. vivax. This parasite has a liver stage and can remain in the
body for years without causing sickness. If the patient is not treated, the liver stage may re-
activate and cause relapses - malaria attacks - after months, or even years without symptoms.
Plasmodium malariae (P. malariae) - milder form of the disease, generally not fatal.
However, the infected human still needs treatment because no treatment can also lead to a host
of health problems. This type of parasite has been known to stay in the blood of some people
for several decades.
Plasmodium ovale (P. ovale) - milder form of the disease, generally not fatal. However, the
infected human still needs to be treated because it may progress and cause a host of health
problems. This parasite has a liver stage and can remain in the body for years without causing
sickness. If the patient is not treated, the liver stage may re-activate and cause relapses -
malaria attacks - after months, or even years without symptoms.
Plasmodium falciparum (P. faliparum) - the most serious form of the disease. It is most
common in Africa, especially sub-Saharan Africa.
Plasmodium knowlesi (P. knowlesi) - causes malaria in macaques but can also infect humans.
Pathogenesis
The life cycle of malaria parasites: A mosquito causes infection by taking a blood meal.
First, sporozoites enter the bloodstream, and migrate to the liver. They infect liver cells, where
they multiply into merozoites, rupture the liver cells, and return to the bloodstream. Then, the
merozoites infect red blood cells, where they develop into ring forms, trophozoites and schizonts
that in turn produce further merozoites. Sexual forms are also produced, which, if taken up by a
mosquito, will infect the insect and continue the life cycle.
Transmission/Cause
A person gets malaria when bitten by a female Anopheles mosquito that is looking for a blood
meal and is infected with the malaria parasite. Such blood meals are the link between the human
and the mosquito hosts in the parasite life cycle.
A mosquito becomes infected when it takes a blood meal from an infected vertebrate. Once
blood is ingested, the parasite gametocytes taken up in the blood will further differentiate into
male or female gametes and then fuse in the mosquito's gut.
This produces an ookinete that penetrates the gut lining and produces an oocyst in the gut wall.
When the oocyst ruptures, it releases sporozoites that migrate through the mosquito's body to the
salivary glands, where they are then ready to infect a new human host. The sporozoites are
injected into the skin, alongside saliva, when the mosquito takes a subsequent blood meal. This
type of transmission is occasionally referred to as anterior station transfer.
Terms:
Merozoite: The form of the malaria parasite that invades red blood cells.
Oocyst: A stage of the malaria parasite within the mosquito which is produced when male
and female gametes combine.
Ookinete: The actively moving zygote of the malarial organism that penetrates the
mosquito stomach to form an oocyst under the outer gut lining.
Sporozoite: The infectious form of the malaria parasite, which is injected into people by
mosquitoes.
Malaria cannot be casually transmitted directly from one person to another. Instead, a mosquito
bites an infected person and then passes the infection on to the next human it bites. It is also
possible to spread malaria via organ transplants, contaminated needles or in blood transfusions.
This is why all blood donors are carefully screened with questionnaires for possible exposure to
malaria. An infected mother may also pass malaria on to her baby during delivery - this is called
'congenital malaria'.
Vector
Human malaria is transmitted only by females of the genus Anopheles. Of the approximately 430
Anopheles species, only 30-40 transmit malaria (i.e., are "vectors") in nature.
Like all mosquitoes, anophelines go through four stages in their life cycle: egg, larva, pupa, and
adult. The first three stages are aquatic and last 5-14 days, depending on the species and the
ambient temperature. The adult stage is when the female Anopheles mosquito acts as malaria
vector. The adult females can live up to a month (or more in captivity) but most probably do not
live more than 1-2 weeks in nature.
Anopheles mosquitoes can be distinguished from other mosquitoes by the palps, which are as
long as the proboscis, and by the presence of discrete blocks of black and white scales on the
wings. Adult Anopheles can also be identified by their typical resting position: males and
females rest with their abdomens sticking up in the air rather than parallel to the surface on
which they are resting.
Signs and Symptoms
The symptoms of Malaria can vary greatly, from no symptoms at all or mild to extremely serious
and may even result in death. Malaria is often divided into two different categories. The first
category is called the uncomplicated category and the other is complicated category.
1. Uncomplicated Malaria
The general (but very infrequent) attack of malaria usually continues 6-10 hours. There are three
phases to this and these usually return every 2 to 3 days depending upon the type of parasite.
A. The cold phase (shivering, feeling cold)
B. The hot phase (vomiting, fever, headache; convulsions in children)
C. The Sweating phase (sweating, normal temperature, sleepiness)
However, more often the patient usually has the following signs and symptoms:
Chills
Fever
Nausea and vomiting
Headache
General discomfort Body aches
In some patients, one may observe enlarged spleen, fever, perspiration, general weakness. If a
patient is infected with P. Falciparum, they may develop symptoms such as enlarged liver, mild
jaundice, and increase respiratory rate.
Depending upon the country and the frequency that malaria is experienced the patient will either
self-medicate; or they will seek professional help after improper medications fail to take effect.
2. Complicated Malaria
This usually occurs where there is either low or no immunity to this disease, including locations
where Malaria disease is rare or immunity is low because of other health risks. Complicated
malaria results in blood and organ disorders, including fluid on the lung, and loss of kidney
function.
In all areas of the world complicated Malaria disease is an emergency and should be treated as
quickly and as intensely as possible because without treatment other major medical problems
appear and eventually death does occur. As with other conditions pregnancy may be complicated
resulting in pre-term labor or low birth-weight babies. In some extreme cases, there is a
possibility of early termination of the pregnancy.
Severe Malarial Bouts
When a patients develops a serious P. falciparum infection, it results in multiple organ failure. It
may even lead to abnormalities in the normal metabolism of the patient and blood. These
complications include:
Severe anemia due to destruction of normal red blood cells
Presence of hemoglobin urine (hemoglobinuria)
Pulmonary edema and acute respiratory distress syndrome (ARDS)
Decrease in blood platelets that leads to blood coagulation and thrombocytopenia
Cardiovascular shock
Low blood sugar levels (hypoglycemia), especially in pregnant women
Incubation period
The amount of time between the mosquito bite and the appearance of symptoms varies,
depending on the strain of parasite involved. Symptoms from some strains of P. vivax may not
appear until 8-10 months after the mosquito bite occurred.
Incubation depends on the type of parasite:
P. falciparum - 8 to 12 days
P. vivax - 12 to 18 days
P. ovale - 12 to 18 days
P. malariae - 18 to 40 days
Incubation periods can vary from as little as 7 days, to several months for P. vivax and P. ovale.
If you are taking medication to prevent infection (chemoprophylaxis) the incubation period is
usually longer.
Diagnosis
WHO recommends that all cases of suspected malaria be confirmed using parasite-based
diagnostic testing (either microscopy or rapid diagnostic test) before administering treatment.
Results of parasitological confirmation can be available in 15 minutes or less.
Malaria is diagnosed by examining blood under a microscope. The parasite can be seen in
the blood smears on a slide. These blood smears may need to be repeated over a 72-hour period
in order to make a diagnosis. Antibody tests are not usually helpful because many people
developed antibodies from past infections, and the tests may not be readily available.
Two new techniques to speed the laboratory diagnosis of malaria show promise as of late 2002.
1. Acridine orange (AO), a staining agent that works much faster (3-10 min) than the traditional
Giemsa stain (45-60 min) in making the malaria parasites visible under a microscope.
2. A bioassay technique that measures the amount of a substance called histadine-rich protein II
(HRP2) in the patient's blood. It allows for a very accurate estimation of parasite development. A
dip strip that tests for the presence of HRP2 in blood samples appears to be more accurate in
diagnosing malaria than standard microscopic analysis.
Anyone who becomes ill with chills and fever after being in an area where malaria exists
must see a doctor and mention their recent travel to endemic areas. The doctor may believe the
symptoms are just the common flu virus. Malaria is often misdiagnosed by North American
doctors who are not used to seeing the disease. Delaying treatment of falciparum malaria can be
fatal.
Treatment
How to treat a patient with malaria depends on:
The type (species) of the infecting parasite
The area where the infection was acquired and its drug-resistance status
The clinical status of the patient
Any accompanying illness or condition
Pregnancy
Drug allergies, or other medications taken by the patient
Most drugs used in treatment are active against the parasite forms in the blood (the form
that causes disease) and include:
chloroquine
atovaquone-proguanil (Malarone)
artemether-lumefantrine (Coartem)
mefloquine (Lariam)
quinine
doxycycline (used in combination
with quinine)
clindamycin (used in combination
with quinine)
artesunat
In addition, primaquine is active against the dormant parasite liver forms (hypnozoites) and
prevents relapses. Primaquine should not be taken by pregnant women or by people who are
deficient in G6PD (glucose-6-phosphate dehydrogenase). Patients should not take primaquine
until a screening test has excluded G6PD deficiency
Prevention
Awareness of risk.
Bite avoidance.
Chemoprophylaxis (taking preventive medicines if you are travelling to or living in a
malaria region).
Diagnosis made promptly with early treatment of an infected case.
No vaccine has been approved to prevent malaria.
Stay inside when it is dark outside, preferably in a screened or air-conditioned room.
Wear protective clothing (long pants and long-sleeved shirts).
Use insect repellent with DEET (N,N diethylmetatoluamide).
Use bed nets (mosquito netting) sprayed with or soaked in an insecticide such as
permethrin or deltamethrin.
Use flying-insect spray indoors around sleeping areas.
Avoid areas where malaria and mosquitoes are present if you are at higher risk (for
example, if you are pregnant, very young, or very old).
Government Programs
Malaria Control Program
Based on the 2011-2016 Malaria Program Medium Term Plan, it aims to:
1. Ensure universal access to reliable diagnosis, highly effective, and appropriate
treatment and preventive measures;
2. Capacitate local government units (LGUs) to own, manage, and sustain the Malaria
Program in their respective localities;
3. Sustain financing of anti-malaria efforts at all levels of operation; and
4. Ensure a functioning quality assurance system for malaria operations.
Program Strategies:
The DOH, in coordination with its key partners and the LGUs, implements the following
interventions:
1. Early diagnosis and prompt treatment
Diagnostic Centers were established and strengthened to achieve this strategy. The
utilization of these diagnostic centers is promoted to sustain its functionality.
2. Vector control
The use of insecticide-treated mosquito nets, complemented with indoor residual
spraying, prevents malaria transmission.
3. Enhancement of local capacity
LGUs are capacitated to manage and implement community-based malaria control
through social mobilization.
Program Accomplishments:
For the development of health policies, the Malaria Medium Term Plan (2011-2016) is already in
its final draft while the Malaria Monitoring and Evaluation Framework and Plan is being drafted.
The Malaria Program is being monitored in six provinces as the Philippine Malaria Information
System is being reviewed and enhanced.
In strengthening the capabilities of the LGUs, trainings are conducted. These include: series of
Basic and Advance Malaria Microscopy Training; Malaria Program Management Orientation
and Training for the rural health unit (RHU) staff; and Data Utilization Training. Also, there are
the Clinical Management for Uncomplicated and Severe Malaria and the Malaria Epidemic
Management.
Lastly, health services are leveraged through the provision of anti-malaria commodities.
Questions:
1. What is the most common type of malaria in the Philippines? P. falciparum
2. What is the most common type of malaria globally? P. vivax
3. Why is it that only female mosquitoes transmit malaria? Female mosquitoes need to take
blood meals for the development of their eggs.
4. How do you differentiate one type of malaria from the others?
P. falciparum blood smears are characterized by the presence of young trophozoites (ie, rings) in
the absence of mature trophozoites and schizonts. The ring stages of P. falciparum tend to be
slightly smaller than the other species and are generally more numerous. Multiply infected
erythrocytes and appliqu forms are seen more often in P. falciparum than in the other species.
The crescent-shaped gametocytes of P. falciparum are very distinctive, but tend to only appear
late in the infection.
The most distinctive features of P. vivax are the enlarged infected erythrocytes and the
appearance of granules, called 'Schffner's dots', over the erythrocyte cytoplasm. These granules
are manifestation of caveola-vesicle complexes that form on the erythrocyte membrane. The
growing trophozoite of P. vivax often has an ameboid apearance and the schizonts can have more
than 20 merozoites.
P. ovale also exhibits Schffner's dots and an enlarged erythrocyte, making it difficult to
distinguish from P. vivax. In general, P. ovale is a more compact parasite than P. vivax. This
compactness is most evident in the growing trophozite stage and fewer merozoites are found per
schizont. P. ovale also has more of a tendency to form elongated host erythrocytes.
P. malariae is characterized by a compact parasite (all stages) and does not alter the host
erythrocyte or cause enlargment. Elongated trophozoites stretching across the erythrocyte, called
band forms, are sometimes observed. Schizonts will typically have 8-10 merozoites that are often
arranged in a rosette pattern with a clump of pigment in the center.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Dosage Form Design Pharmaceutical and Formulation ConsiderationsDocumento103 pagineDosage Form Design Pharmaceutical and Formulation Considerationsprinceamit67% (3)
- Med2 Patient Write-Up Template-Aug 2015 by DR - Villespin-Lanzona For UST Med StudentsDocumento6 pagineMed2 Patient Write-Up Template-Aug 2015 by DR - Villespin-Lanzona For UST Med StudentsGeraldCalimbasNessuna valutazione finora
- Muscular HandoutDocumento5 pagineMuscular HandoutFredrick Rivera AlteaNessuna valutazione finora
- HistoryDocumento11 pagineHistoryJerrica Mae TanNessuna valutazione finora
- Genesis Learnings and PassagesDocumento6 pagineGenesis Learnings and PassagesCassandra LaoNessuna valutazione finora
- GR2 Plasmodium-Spp PDFDocumento29 pagineGR2 Plasmodium-Spp PDFEran Mark RojasNessuna valutazione finora
- Vishamajwaram Kc029gdg 121226100307 Phpapp02Documento238 pagineVishamajwaram Kc029gdg 121226100307 Phpapp02Samhitha Ayurvedic Chennai100% (2)
- Malaria NotesDocumento3 pagineMalaria NotesAbynarh PinaNessuna valutazione finora
- Sporozoa 4Documento27 pagineSporozoa 4ebenezermanzanormtNessuna valutazione finora
- Plasmodium VivaxDocumento4 paginePlasmodium VivaxSUTHAN100% (1)
- Malaria: Transmission SymptomsDocumento5 pagineMalaria: Transmission SymptomsDinartaNessuna valutazione finora
- Malaria - WikipediaDocumento75 pagineMalaria - Wikipediaadandiba06Nessuna valutazione finora
- Plasmodium Falciparum Malaria: A Multicentre, Open-Label,: ArticlesDocumento16 paginePlasmodium Falciparum Malaria: A Multicentre, Open-Label,: ArticlesmdNessuna valutazione finora
- Blood and Tissue ProtozoaDocumento60 pagineBlood and Tissue ProtozoaOvidiuNessuna valutazione finora
- Malaria EssayDocumento5 pagineMalaria EssayJuanma AsensioNessuna valutazione finora
- Ntegeka Community Development AssistantsDocumento2 pagineNtegeka Community Development Assistantsapi-322948949Nessuna valutazione finora
- Malaria Plasmodium SPP WPDocumento5 pagineMalaria Plasmodium SPP WPPerlie CNessuna valutazione finora
- Shreyas N B Bio Investigatory ProjectDocumento16 pagineShreyas N B Bio Investigatory ProjectShreyas GamerNessuna valutazione finora
- MALARIA DR - PAULDocumento67 pagineMALARIA DR - PAULNodi Rahma DiniNessuna valutazione finora
- Anti-Malerials MaterialsDocumento13 pagineAnti-Malerials Materialsraj royelNessuna valutazione finora
- Topic:: Operasi Semburan Dalam Kawalan MalariaDocumento33 pagineTopic:: Operasi Semburan Dalam Kawalan MalariarayNessuna valutazione finora
- Antimalarial Drugs: Presenter Basil Mupita Rgn/BscneDocumento35 pagineAntimalarial Drugs: Presenter Basil Mupita Rgn/BscneTapiwaNessuna valutazione finora
- MalariaDocumento28 pagineMalariaArthur Samuel ShavaniNessuna valutazione finora
- MalariaDocumento6 pagineMalariaShadab Ahmad KhanNessuna valutazione finora
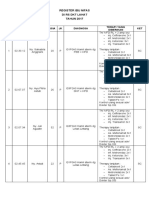
- Register Ibu Nifas 2017Documento6 pagineRegister Ibu Nifas 2017jkn rsiampNessuna valutazione finora
- Malaria 1Documento14 pagineMalaria 1sonya nataliaNessuna valutazione finora
- Malaria Schematic DiagramDocumento5 pagineMalaria Schematic DiagramCrazy about JunglesNessuna valutazione finora
- Malaria Best Investigatory ProjectDocumento37 pagineMalaria Best Investigatory ProjectDivyansh PandeyNessuna valutazione finora
- Cause & Pathophysiology of MalariaDocumento8 pagineCause & Pathophysiology of MalariaMariam Mohamed RagehNessuna valutazione finora
- ON Plasmodium Vivax (Malarial Parasite)Documento10 pagineON Plasmodium Vivax (Malarial Parasite)Raja Marudut SimatupangNessuna valutazione finora
- Assingment of ParasateDocumento36 pagineAssingment of ParasateHibaaq AxmedNessuna valutazione finora
- Salinan Dari Malaria Disease by SlidegoDocumento9 pagineSalinan Dari Malaria Disease by SlidegoShinta WahyoeNessuna valutazione finora
- Malaria Summary: TermsDocumento5 pagineMalaria Summary: TermsDianne GalangNessuna valutazione finora
- Daftar Dosis Obat MalariaDocumento1 paginaDaftar Dosis Obat MalariaIriani ImbabNessuna valutazione finora
- Medicinal Plants Used in The Treatment of Malaria, A Key Emphasis To Artemisia, Cinchona, Cryptolepis, and Tabebuia GeneraDocumento14 pagineMedicinal Plants Used in The Treatment of Malaria, A Key Emphasis To Artemisia, Cinchona, Cryptolepis, and Tabebuia GeneraJ Elver SilvaNessuna valutazione finora