Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Blunt The Haemodynamic Respon From Laryngoscopy and Endotracheal Intubation
Caricato da
yehezkiel_yesiTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Blunt The Haemodynamic Respon From Laryngoscopy and Endotracheal Intubation
Caricato da
yehezkiel_yesiCopyright:
Formati disponibili
17 January 2014
No. 02
BLUNTING THE INTUBATION
RESPONSE: FACT OR FICTION
Pur!"a#$
Moderator: C Evans
%&#!&'(&n$ o) Ana$#*"$*&!#
CONTENTS
+ECHANIS+ OF THE INTUBATION RESPONSE................................................4
BLUNTING THE HAE+O%,NA+IC RESPONSE..................................................7
OPIOI%S.................................................................................................................-
. 2 AGONISTS.....................................................................................................10
/ BLOCERS.......................................................................................................11
+AGNESIU+ SULPHATE 0+GSO41...................................................................12
NO2EL I%EAS......................................................................................................13
SU++AR, OF E2I%ENCE..................................................................................14
BENEFITS OF ATTENUATING THE RESPONSE...............................................17
CONCLUSION......................................................................................................20
REFERENCES......................................................................................................21
Page 2 of 27
OBJECTI2ES
Discuss the mechanism of the intubation response
Explore the various pharmacological methods to attenuate the intubation the
response
Attempt to determine the benefits of blunting the intubation response
Page 3 of 27
BLUNTING THE INTUBATION RESPONSE: FACT OR FICTION
INTRO%UCTION
ar!ngoscop! and tracheal intubation are noxious stimuli associated "ith a
transient increase in autonomic response# $ing et al described this response more
than %& !ears ago#
'()
*t is most often associated "ith an increase in heart rate and blood pressure and
is thought to be of little conse+uence in the health! individual but could be
deleterious in the vulnerable patient#
'2)
,his response varies "ith depth of
anaesthesia- duration and difficulties during lar!ngoscop! and intubation- and
certain patient factors including histor! of diabetes
'3)
and cardiovascular disease
'.)
'/)
+ECHANIS+ OF THE INTUBATION RESPONSE
0asic anatom!:
F&5ur$ 1: the sensor! innervation of the air"a!s
'%)
,he phar!nx: sensor! innervation 1 2lossophar!ngeal nerve supplies the
posterior third of the tongue- the fauces and tonsillae- anterior epiglottis and all
parts of the phar!nx "ith visceral sensor! 3bers#Motor innervation4 the phar!nx
receives efferent suppl! from the vagus nerve through its phar!ngeal branch#
'%)
Page . of 27
,he lar!nx: sensor! innervation 1 the internal lar!ngeal nerve- branch of the
superior lar!ngeal nerve- provides sensor! suppl! from the posterior epiglottis to
the vocal cords# ,he recurrent lar!ngeal nerve supplies the lar!nx belo" the vocal
cords and the trachea#
Motor innervation: the recurrent lar!ngeal nerve supplies all intrinsic muscles of
the lar!nx except the cricoth!roid muscles#
'%)
F&5ur$ 2: innervation of the lar!nx
'7)
5impl! put- "ith regards to sensor! innervation- the orophar!nx- posterior third of
the tongue and anterior part of the epiglottis are supplied b! glossophar!ngeal#
,he posterior epiglottis and distal air"a! structures are supplied b! branches of
the vagus nerve#
+$!"an o) *"$ &n*u7a*&on r$#'on#$
,he precise mechanism of the intubation response '*6) is elusive but it has been
established that it has both a s!mpathetic and paras!mpathetic element# ,he
effect is transient occurring 3& seconds after intubation and lasting for less than
(& minutes thereafter#
'7)
,he s!mpathetic response is a pol!s!naptic path"a! "ith
the glossophar!ngeal and vagus nerve forming the afferent arc to the s!mpathetic
nervous s!stem via the brain stem and spinal cord# ,his ensures a diffuse
autonomic response at the efferent side including increased firing of the cardio4
accelerator fibres and release of adrenergic mediators including norepinephrine-
epinephrine and vasopressin#
Page / of 27
,he net effect of this autonomic surge is an increased 0lood pressure '0P)- heart
rate '86)- pulmonar! arter! "edge pressure and decreased e9ection fraction#
,he paras!mpathetic reflex is monos!naptic and more common in children but
can occur in some adults# ,he reflex is mediated b! increased vagal tone at the
5A node#
'2)
,he haemod!namic response to lar!ngeal and endo4 tracheal intubation 'E,*) is
transient and in most patients thought to be of little conse+uence# *n patients "ith
coronar! arter! disease 'CAD)- h!pertension- raised intra cranial or intra ocular
pressure it ma! be associated "ith m!ocardial ischaemia- infarction- arrh!thmias-
cardiac failure- pulmonar! oedema and cerebral haemorrhage#
'/)
,he process of intubation comprises of different phases and these affect the
haemod!namic response differentl!# :rotracheal intubation consists of 2 phases:
direct lar!ngoscop! and passing of endotracheal tube through the vocal cords and
trachea#
';)
<our studies loo=ed at this differential effect# 5ing
';)
- 5hin9i
'(&)
and 8assan
'(()
concur that tracheal intubation and cuff inflation produce a substantial
haemod!namic effect- significantl! greater than lar!ngoscop! alone# 5hribman
'(2)
ho"ever found that orotracheal intubation did not significantl! contribute to the
haemod!namic effect# ,hese studies give the impression that greatest increase in
86 occurs during E,* and greatest increase in 0P occurs during lar!ngoscop!#
>ith no active attempt at blunting this haemod!namic response- increases in 50P
of .(4/3 mm8g- 86 2&423 and MAP of up to (&&? above baseline have been
documented#
'()'(3)
Page % of 27
BLUNTING THE HAE+O%,NA+IC RESPONSE
,he possibilities to offset or blunt the intubation response are numerous# :ptions
include pharmacological- peripheral bloc=s and variations in techni+ues including
various blades and conduits for intubations#
,his boo=let "ill onl! focus on pharmacological techni+ues#
Pharmacological options:
ocal anaesthetics
:pioids
@
2
agonists
A
2
bloc=ers
Mg5:
.
2abapentin- pregabalin
LIGNOCAINE:
,he effectiveness of lignocaine to blunt the intubation response '*6) is
contentious# Bumerous studies dating from (;%& have loo=ed at different doses-
timing and routes of administering ignocaine# <rom the discussion above on the
nerve suppl! of the lar!nx and the effect that tracheal intubation has on the *6 it is
apparent "h! lar!ngeal tracheal routes "ill not entirel! blunt the response#
'(.)'(/)
8amill et al and aurito et al both loo=ed at the *C route of ignocaine to blunt the
response to E,*#
8amill
'(.)
used a dose of (#/mgD=g- ivi (minute prior to E,* and compared this to
.ml of a .? solution spra!ed lar!ngealtracheall!# ,he group that received topical
lignocaine sustained significant increase in 86 and 0P after E,* that lasted for
more than 2 minutes# ,he authors note that the *C route did not completel!
attenuate the response as there "as still significant increase in 0P and 86
although onl! sustained for ( minute or less# aurito et al
'(%)
compared *C
ignocaine '2mgD=g) ( minute pre E,* to nebuliEed lignocaine .mgD=g (/
minutes prior to E,*# >ithin each group all haemod!namic variables increased
significantl!# >ith mean arterial pressures of (.&mm8g recorded#
Miller et al
'(7)
also failed to demonstrate that ignocaine attenuates the
haemod!namic response to E,*# ,he! studied ignocaine (#/mg ivi given (-2
and 3 minutes prior to E,*# 5=lar et al
'(7)
found that aerosol application of
lignocaine (2&mg "as effective in attenuating the both the 0P and 86 response
in adults# ,his "as applied for / minutes duration and 7#/ min prior to induction#
Carious other studies support the use of ignocaine (-/mgD=g ivi given bet"een 24
. minutes to attenuate the response# ,am et al
'(;)
and 5plinter et al
'2&)
could onl!
demonstrate benefit "ith regards to the 0P response- ho"ever 8elfman
'2()
found a
dose of (-/ mgD=g- given 2 minutes prior to E,*- to blunt both the 0P and 86
response#
,he principal limitation "hen comparing studies is heterogeneit! of the studies#
Carious doses- timings- pre medications and induction agents are used#
Page 7 of 27
At best- intra venous ignocaine "ill occasionall! blunt the 0P response and
almost never the 86 response# *f administered it should be at a dose of (-/mgD=g-
3 minutes prior to intubation
#'2)
,opical routes are not effective in blunting the intubation response and fe" studies
have sho"n convincing benefit of the aerosol route#
'22)
OPIOI%S
,he addition of opioids deepens the level of anaesthesia and therefor decreases
the s!mpathetic outflo"#
Alfentanil: numerous studies sho" that a dose of 3&FgD=g given bet"een (#/ and
2 minutes prior to intubation provides complete attenuation of the haemod!namic
response#
'23)'2.)'2/)'2%)
o"er dosages- (/FgD=g- seem to attenuate the 0P response but not the 86
response#
'2%)
*n the elderl! (&FgD=g given 34. minutes pre induction has also been sho"n to
completel! blunt the haemod!namic response#
'27)
8igher dosages have been associated "ith brad!cardia and h!potension#
'23)
<e" studies distinguish bet"een h!pertensive and non4h!pertensive patients#
:nl! Miller
'2/)
et al used patients from A5A (43 stages but did not specif! the
reason for the staging#
A dose of Alfentanil (&FgD=g given over 3& seconds has been suggested to be
effective in blunting the cardiovascular effect in h!pertensive patients on long term
treatment# *n this stud! 3D2& patients developed h!potension re+uiring Ephedrine#
'27)
6emifentanil:
,he rapid onset and short duration of 6emifentanil ma=es it an attractive drug for
attenuating the *6#
,hompson et al
'2;)
initiall! found that a dose of (FgD=g follo"ed b! and infusion of
&#/FgD=gDmin attenuated the haemod!namic response in health! adults# ,his dose
"as associated "ith profound brad!cardia and h!potension in half the patients#
A subse+uent stud!
'3&)
indicated that &#/FgD=g follo"ed b! an infusion of
/FgD=gDmin "as as effective in blunting the response "ith no incidence of
brad!cardia or h!potension re+uiring treatment# ,he! also indicate that at the
higher doses- pre4treatment "ith gl!cop!rrolate 2&&Fg- decreases the incidence of
side effects#
Page 7 of 27
Maguire et al
'27)
demonstrated that a bolus dose of &#/FgD=g follo"ed b! infusion
at &#(FgD=gDmin effectivel! reduces the response to E,* in h!pertensive patients
on treatment# :f note is that all patients "ere pre4treated "ith gl!cop!rrolate 2&&
Fg# Bone of the patients developed a brad!cardia but 7D2& patients re+uired
rescue medication for h!potension# '50P 7&4(&& mm82)#
Most studies agree that a dose of 2FgD=g significantl! reduces the 0P and 86 and
that this dose is not recommended for the elderl! or compromised patient#
'22)
8art et al
'3()
compared 6emifentanil ' &#/FgD=g follo"ed b! an infusion of
&#(FgD=gDmin) and Alfentanil ' (&FgD=g) in elderl! patients# ,he stud! included
patients of A5A *4*** but excluded patients "ith evidence of cardiovascular
disease#
,he! concluded that both drugs similarl! attenuated the haemod!namic response
but that the incidence of h!potension in both groups 9ustifies caution in the elderl!#
<entan!l:
Bumerous studies have loo=ed at various doses and timing to administer <entan!l
and its effect on the intubation response# Gnsurprisingl!- high doses of /&47/FgD=g
completel! blunt the response but are associated "ith significant side effects#
'2)
*n normotensive A5A *D** patients various authors indicate that a dose of 2FgD=g
given bet"een 3-/4/ min pre E,* suppress the response#
'32)'33)
$autto et al
'3.)
and <eng at al
'33)
indicated that although the 0P response "as
attenuated at this dose- the 86 response "as not sufficientl! obtunded#
:thers indicate that a dose of /47FgD=g given bet"een 3-/4/ min pre E,*
completel! blunts the response#
'3.)'3/)'3%)
*n elderl! patients a dose of 3FD=g has been indicated to prevent a haemod!namic
response
#'37)
Again- most studies are heterogenic and difficult to compare# Dosages that seem
to be most effective are bet"een /4%FgD=g given 34/ minutes prior to E,*# Dose
reduction is prudent in the elderl!# >ith these doses there is a ris= for
complications including respirator! depression and dela!ed a"a=ening in short
cases#
'2)
5ufentanil:
,he use of 5ufentanil has been researched extensivel! in the paediatric
population but research in the adult population appears scant!#
$a! et al reported a dose of &-/4(FgD=g given 2 minutes pre E,* sufficientl!
bloc=ed the response in adults
#'37)
Hhang et al
'3;)
reported that in patients for heart valve replacement- a dose of
(FgD=g sufficientl! bloc=ed the 0P and 86 response# A dose of (#/FgD=g "as
associated "ith significant brad!cardia re+uiring Atropine administration in 27? of
cases#
Page ; of 27
*n t"o comparable studies in normotensive A5A *4*** patients- a bolus dose of
&#(FgD=g follo"ed b! an infusion of &#&(FgD=gDmin for / minutes prior to E,* "as
effective in blunting both the 0P and 86 response#
'.&)'.()
*n children- a dose bet"een FgD=g administered 2 min prior to E,* has
been found to significantl! attenuate the haemod!namic response to intubation#
'.2)
'.3)
Bone of the children in the higher range group experienced significant side
effects re+uiring treatment#
. 2 AGONISTS
5timulation of the pres!naptic @ receptors leads to reduced secretion of nor4
adrenaline and renin# Cagotonic effects that decrease the 86 are also present#
Most of the studies compare Clonidine as a premedication to various methods of
anaesthesia that included variable doses of <entan!l and Alfentanil#
5tudies indicate that- used in addition to a standard general anaesthetic- Clonidine
.4/FgD=g po given bet"een %&4;& minutes prior to surger! can be beneficial#
0enefits include reduced doses of opioids and induction agents- decreased
haemod!namic response to E,* and improved intraoperative haemod!namics#
,he ris= of brad!cardia is al"a!s present and "as treated "ith Atropine in some
of the studies#
'..)'./)'.%)'.7)'.7)
Dra"bac=s of Clonidine include long duration of onset- prolonged duration of
action and therefore the ris= of post4operative sedation in short procedures as "ell
as the ris= of h!potension and brad!cardia#
'2)'..)
Dexmedetomidine is a highl! selective @
2
agonist# A biphasic cardiovascular
response has been described# After a bolus of (FgD=g- a transient increase in 0P
and decrease in 86 is seen# ,his is thought to be due to stimulation of @
2
receptors in vascular smooth muscle# ,he vasoconstriction effect thus appears
before the central effects# ,his response can be decreased but not completel!
avoided b! giving the bolus dose as an infusion over (& minutes#
'.;)
Aho et al
'/&)
sho"ed in health! patients a bolus infusion of &#(2FgD=g over (& min
follo"ed b! an infusion of &#&&%FgD=g significantl! reduced the 86 but not the 0P
response to E,*# :f note is that .&? of the patients in the Dexmedetomidine
group re+uired Atropine to treat brad!cardia#
Iaa=ola et al
'/()
found an infusion of &#%FgD=gDmin (& minutes prior to E,*
reduced the 0P and 86 response in patients presenting for ophthalmic surger!#
0a9"a et al
'/2)
indicated that an infusion of (FgD=g over 2& minutes attenuated but
did not completel! obtund the response to E,*# Bone of the patients in this stud!
had a significant brad!cardiac or h!potensive episode ho"ever onl! health! A5A *
patients "ere included#
Page (& of 27
Menda et al investigated patients undergoing fast trac= CA02 surger!# An
infusion of (FgD=g "as given over (/ minutes# ,his "as compared to a placebo
group# ,heir conclusion "as that Dexmedetomidine can safel! be used to
attenuate the haemod!namic response# ,he incidence of h!pertension post
intubation in the placebo group "as statisticall! significant# ,he incidence of
h!potension "as not statisticall! significantl! bet"een the 2 groups#
'/3)
5ulaiman et al
'/.)
confirm these results but at much lo"er doses# %& patients for off
pump CA02 "ere randoml! allocated to a Dexmedetomidine group or placebo
group# An infusion of &#/FgD=g over (& minutes found better haemod!namic
control post E,* in the Dexmedetomidine group# Bo adverse effects needing
treatment "ere observed# 5ignificantl!- almost /&? of the patients in each group
"ere on A4bloc=ers pre4operativel!#
*n summar!- from the above studies- it appears that doses bet"een &#/4(FgD=g as
an infusion over (&42& minutes prior to E,*- in addition to lo" dose opioids-
decrease the response to E,* and improve haemod!namics#
,he ris= of h!potension and brad!cardia should al"a!s be considered# A recent
meta4anal!sis confirmed- in cardiac patients for non4cardiac surger!- peri4
operative Dexmedetomidine significantl! increased the incidence of h!potension
and brad!cardia#
'//)
/ BLOCERS
abetolol has a combination of @ and A bloc=ade# ,he @ bloc=ade is specific for @
(
and non4specific for A bloc=ade# ,he ratio of @
(
to A bloc=ing effect is (:7# *t has an
onset of (4/ minutes and a half4life of up to /#/ hours#
'72)
*nanda et al
'%()
compared abetolol '/mg and (&mg) to ignocaine '(&&mg) and a
placebo group in health! patients presenting for general surger!#
abetolol (&mg ivi 'JD4 &#(.mgD=g) 2 minutes prior to E,* bloc=ed the 86
response better than the other 2 groups but the 0P response "as the same in all
four groups#
Chung et al
'%2)
confirmed these findings "ith a larger dose of &#.mgD=g
administered / minutes prior to E,*#
eslie et al
'%3)
compared doses bet"een /mgD=g to (mgD=g# *t "as found that
abetalol effectivel! attenuated the 86 and 0P response in a dose dependant
manner# 0ut the! also state that although the higher doses bloc= the 0P
response- the! are at the expense of significant post intubation h!potension#
:ne of the main concerns of abetalol is the prolonged duration of action#
Esmolol is a cardio selective A bloc=er "ith rapid onset and offset#
'72)
*t reaches
pea= blood levels in about 2 minutes and has an approximated half4life of ;
minutes#
'2)
Page (( of 27
5everal studies have assessed the effectiveness of Esmolol in blunting the
response to E,*# As "ith man! of the other drugs mentioned- little consensus
has been reached "ith regards to optimal dose- time and ris= of side effects in the
different population groups#
A recent meta4anal!sis
'/)
attempts to determine the optimal dose of Esmolol
needed to minimiEe the response to E,* and decrease post intubation
h!potension# ,he anal!sis includes 37 studies and concludes that a loading dose
of /&&FgD=g over . minutes follo"ed b! an infusion of 2&&43&&FgD=gDmin is the
best approach# *t also states that a dose dependant ris= of h!potension is entailed
during induction and its routine use is not recommended#
A comment on this meta4anal!sis is that of the 37 studies evaluated- onl! %
studies evaluated the use of Esmolol in patients "ith h!pertension or coronar!
arter! disease# A sub anal!sis could not be done as the numbers "ere insufficient#
Bevertheless these % studies indicated that neither the effectiveness of the drug
nor the magnitude of adverse effects "ere seemingl! different from the studies in
health! patients#
:f note is that (; of the included studies included the use of different opioids as
premedication or as part of induction#
+AGNESIU+ SULPHATE 0+GSO
4
1
Mg5:. is involved in several ph!siological processes including control of
vasomotor tone- cardiac excitabilit! and release of neurotransmitters# ,hrough
various methods it causes vasodilation and decreases release of catecholamines
from the nerve terminals and adrenal gland#
'/%)
A small but elo+uent stud! b! Iames et al
'/7)
studied the effect of %&mgD=g Mg5:
.
pre4treatment on the cardiovascular response to E,* and catecholamine release#
(% health! male patients "ere randoml! allocated to a placebo group or the
Mg5:
.
group# All patients "ere pre4medicated "ith DiaEepam (&mg po ( hour pre
surger!# Bo opioids "ere used during induction# Although Mg5:
.
caused a slight
increase in 86 after in9ection- the increase post intubation "as still less "hen
compared to the placebo group#
0P readings "ere significantl! lo"er in the Mg5:
.
group post E,*# ,he stud!
also indicated that Mg5:
.
can significantl! attenuate catecholamine output at the
time of E,*#
Puri et al
'/7)
studied the use of Mg5:
.
in patients "ith coronar! arter! disease
presenting for CA02# A dose of /&mgD=g'nK(;) "as compared to ignocaine
(mgL=g 'nK(7)#
Page (2 of 27
,he! concluded that Mg5:
.
attenuated the haemod!namic response to E,*
more effectivel! than ignocaine# Bone of the patients in the Mg5:
.
had
significant 5, changes- compared "ith three patients in the ignocaine group#
Panda et al
'/%)
determined that the minimal effective dose of Mg5:
.
needed to
attenuate the intubation response in controlled h!pertensive patients "as
3&mgD=g#
8igher dosages "ere associated "ith significant h!potension#
Iames et al
'/;)
compared ignocaine '(-/mgD=g)- Alfentanil '(&FgD=g) and Mg5:
.
'.&mgD=g) in h!pertensive- proteinuric pregnant patients# 5!stolic blood pressure
exceeded baseline values the first / min after tracheal intubation in the lignocaine
group- but no mean increase in pressure occurred in the t"o other groups#
Alfentanil caused the least change in heart rate- but resulted in significant fetal
depression#
*n a subse+uent stud!
'%&)
- Mg5:
.
.&mgD=g "as compared to Mg5:
.
3&mgD=g "ith
Alfentanil 7#/FgD=g# ,he conclusion "as that both methods controlled the
haemod!namic response satisfactoril! but that the combination "as superior in
controlling both the 0P and 86 response# ,here "as no difference in fetal
outcome bet"een the t"o groups#
NO2EL I%EAS
2abapentin inhibits membrane voltage gated calcium channels# *t is being used
more fre+uentl! as an ad9unct for treatment of acute post4operative pain in the
setting of chronic pain#
'%()'72)
<assoula=i et al
'%()
studied the impact of their standard analgesic regime of
2abapentin- on the haemod!namic changes during E,*# .% A5A *4** patients
scheduled for elective h!sterectom! "ere randoml! allocated to receive
2abapentin .&&mg or placebo % hourl!- starting at noon the da! prior to theatre
'total dose (%&&mg)# Bo other premedication "as given and a standard induction
"as done "ith Propofol and Cisatracuruim# Bo opioids "ere given prior to
intubation# ,he! found that this regime attenuated the 0P response but not the 86
response#
$umari et al
'%2)
studied the effect of a single dose of ;&&mg given 2 hours pre4
operativel!# ,he onl! statisticall! significant effect "as noted at the (& minute post
E,* interval# Although this stud! came to the conclusion that a single dose is
effective in reducing the response to E,*- it is +uestionable since most authors
agree that the response to E,* lasts a maximum of (& minutes "ith the pea=
effect in the first fe" minutes# Bo mention is made of an anxiol!tic or opioid given
pre induction "ith Propofol 2#/mgD=g#
*n a similar stud! 0afna et al
'%3)
found that a single dose of (g- (hour pre op had a
statisticall! significant effect in controlling the 0P and 86# :nce again this stud!
"as conducted in health! patients for elective surger!#
Page (3 of 27
,he significant difference is that the patients "ere pre4medicated "ith MidaEolam
and <entan!l and induced "ith ,hiopentone /mgD=g# ,he most convincing stud!
of a single dose of 2abapentin is Memis et al
'%.)
# ;& health! patients "ere
randomised to either a placebo- 2abapentin .&&mg or 7&&mg group administered
( hour before surger!# Bo other pre medications "ere given and no opioids "ere
used during induction# Patients "ere induced "ith Propofol 2mgD=g# ,he! sho"ed
a statisticall! significant decrease in 86 and 0P- in the 7&&mg group- at all
intervals recorded "hen compared to the other groups#
Pregabalin is structurall! but not functionall! related to gamma4aminobut!ric acid
'2A0A)# *t acts b! inhibiting the s!nthesis of the neurotransmitter glutamate#
'72)
*n
a prospective stud! 0ha"na et al
'%/)
randoml! allocated ;& health! patients to
either a placebo 'group *)- Pregabalin 7/mg 'group **) or Pregabalin (/&mg 'group
***) group administered ( hour pre induction# 5tatisticall! significant increases in
0P post E,* "ere seen in group * and ** "hile a significant decrease "as seen in
group ***# ,here "as no significant decrease in 86 in an! group# ,hese results
are confirmed b! another stud!# 5under et al
'73)
found that a single dose of
Pregabalin (/&mg attenuated the response to E,* in patients presenting for
cardiac surger!# *n contrast to 0ha"na et al this stud! sho"ed a statisticall!
significant reduction in 86 response to E,*# Possible reasons for this include that
the 5under trial "as done in cardiac patients and a therefor a significant
proportion of patients "ere on rate modulating medication# Another contributing
factor is that the 5under stud! used opioids a part of the induction#
Page (. of 27
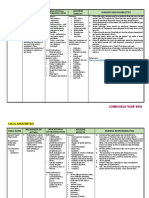
SU++AR, OF E2I%ENCE
%ru5
%o#$ Rou*
$
B(un*$
8 BP
B(un*$
8 HR
No
$))$!
*
R$)$r$n!$
L&5no!a&n$ .ml of .?
solution
,opi4
cal
M (.
(#/mgD=g ivi moder
ate
modera
te
(.
.mgD=g Bebu4
lised
M (%
2mgD=g ivi M (%
(#/mgD=g ivi M (7
(2&mg Aero4
sol
M M (7
(#/mgD=g ivi M (;-2&
(#/mgD=g ivi M M 2(
A()$n*an&( 3&FgD=g ivi M M 2342%
(/FD=g
elderl!
ivi M M 27
Page (/ of 27
1095:;5
Lon5#*an8&n
5
Tr$a*$8 HT
&<& = = 2-
F$n*any( 2FgD=g
34/ min pre
E,*
ivi moderate moderate 32
2FgD=g ivi M none 33-3.
/47FgD=g ivi M M 3.43%
R$6&)$n*an&( &#/FgD=g
bolus then
/FgD=gDmin
ivi M M 3&
&#/FgD=g then
&#(FD=gDmin in
8,D elderl!
ivi M M 27-3(
Su)$n*an&( (FgD=g 2min
prior to E,*
ivi M M 3743;
&#(FgD=g then
&#&(FgD=gDmin
for / min
ivi M M .&-.(
C(on&8&n$ /FgD=g
%&4;& pre
E,*
po moderate moderate ./4.7
%$>6$8$*o
6&8&n$
&#(2FgD=g
over (&min
then
&#&&%FgD=gD
min
ivi M /&
&#%FgD=gDmin
over (& min
ivi M M /(
(FgD=g over
2& min
ivi moderate moderate /2
&#/FgD=g over
(& minutes- in
cardiac pt
ivi moderate moderate /.
La7$*o(o( (&mg ivi M %(
&#.mgD=g ivi M %2
E#6o(o( /&&FgD=g
over .min
then 2&&4
3&&FgD=gDmin
ivi moderate M /
Pr$5a7a(&n 7/mg-( hour
pre E,*
po x %/
Page (% of 27
(/&mg-( hour
pre op
po M %/-73
Ga7a'$n*&n .&&mgD%
hourl!
po M %(
;&&mg-2hour
s pre E,*
po M %2
(g- ( hour pre
E,*
po M M %3
.&&mg ( hour
pre E,*
po M
7&&mg-( hour
pre op
po moderate moderate %.
+a5n$#&u6 %&mgD=g ivi M moderate /7
3&mgD=g ivi M moderate /%
.&mgL=g ivi M moderate /;4%&
/&mgL=g ivi M moderate /7
MK effect on parameter
BENEFITS OF ATTENUATING THE RESPONSE
Central to the +uestion regarding the benefit of blunting the *6 is the differentiation
bet"een final outcomes 'death- peri4operative M*) and process outcome
'ischemia-h!potension-tach!cardia-arrh!thmias)
#'2)
As seen- numerous studies have been done to modif! the response to E,*# ,he!
invariabl! report on variables such as 86- 0P- rate4 pressure ratio and 5,
changes#
Most studies record this for approximatel! (& minutes post E,*# Cer! fe" report
on the influence these have on final outcomes# '%%)
,herefore- benefits of the techni+ues described are presumptive and "e assume
that b! altering the haemod!namic response to E,*- "e "ill improve or alter
outcome#
0oth 86 and 0P are determinants of deliver! and demand of ox!gen# An increase
in heart rate deleteriousl! affects both suppl! and demand of ox!gen# 0P is
related to cardiac output 'C:) and s!stemic vascular resistance '5C6)# A change
in either C: or 5C6 "ill result in a compensator! change in the other#
8!pertension can therefore affect both suppl! and demand
'%%)
# All other organs but
most important to this discussion- the brain- heart and =idne!s depend on
s!stemic pressure to maintain perfusion pressure#
,herefore it is inferred that certain patients cannot tolerate the conse+uences of
the haemod!namic response to E,*#
Page (7 of 27
,hese "ould unarguabl! include eclamptic patients due to the ris= of cerebral
haemorrhage and pulmonar! oedema# :ther such populations "ould include
patients "ith raised intra cranial pressure- patients presenting for cardiac surger!
or patients "ith acute h!pertensive urgenciesDemergencies#
,he gre! area appears "hen researching the benefit in patients "ith ris= factors
for cardiovascular disease but "ith no target organ damage presenting for non4
cardiac surger!#
6eich et al
'%7)
performed a retrospective sub anal!sis 'nK7;7)# ,he aim "as to see
if intra4operative deviations of 86 and 0P "ere associated "ith peri4operative
mortalit! and morbidit!# All patients "ere undergoing complex non cardiac surger!
and controlled for the influence or pre4operative medical conditions#
Deviations "ere defined as 86N ./ DO((&- MAPN//DO(&&mm8g and
50PN7&DO(%&mm8g or an! duration of time#
,he primar! end4point "as negative surgical outcome 'B5:) including post4
operative hospital sta! O (&da!s "ith a morbid condition or death during the same
hospitaliEation#
,here "as no strong association bet"een B5: and variations in haemod!namics
in surgeries lasting less than 22& min#
<or surgeries lasting more than 22&min there "as a strong association "ith lo"
MAP and increased 86# *ncreased 86 "as the stronger predictor#
*ncreased 86 and increased 50P "ere both strong- independent predictors of
adverse outcomes in surgeries lasting more than 22& minutes#
0i9=er et al
'%7)
studied the association bet"een ( !ear mortalit! and intra operative
h!potension '*:8)# ,his retrospective revie" 'nK(7&/) included patients
undergoing general and vascular surger!# Among others- the stud! examines the
effect of h!potension- defined in .7 different "a!s- on mortalit!#
After ad9usting for confounding variables- the regression anal!sis failed to sho"
an! association bet"een *:8 and ( !ear mortalit!#
,he onl! positive associations "ere bet"een advanced age- histor! of
h!pertension- prolonged surger! and *:8# ,his stud! failed to indicate "hat
degree and "hat duration of *:8 can be tolerated during surger!#
Mon= et al
'%;)
studied the association bet"een anaesthetic management and one
!ear mortalit! after non cardiac surger!# ,his stud! included 77& patients#
Multivariate anal!sis indicated 3 significant predictors of ( !ear mortalit!# :ne of
these predictors included *:8# 5!stolic h!potension increased mortalit! ris= b!
(#&3%'66) per minute belo" N7&mm8g# ';/ ? C* (#&&%4(#&%%)
Page (7 of 27
>alsh et al
'7&)
anal!sed prospectivel! gathered data from over 33 &&& patients
undergoing non cardiac surger!# ,he! found that a MAP N//mm8g "as
independentl! associated "ith the development of acute =idne! in9ur!- m!ocardial
in9ur! and cardiac complications# ,his ris= escalates "ith time spent under
MAPN//mm8g but there does not appear to be an! safe amount of time to spend
under a MAPN//mm8g#
A Cochrane revie" from 2&(3
'7()
had the primar! ob9ective to determine the
effectiveness of pharmacological agents in preventing the morbidit! and mortalit!
resulting from the haemod!namic changes during E,*# 5econdar! ob9ectives
included the effect on arrh!thmias and on EC2 changes associated "ith
ischemia# ,he revie" included 72 randomised controls trials that studied the effect
of 32 different drugs belonging to different pharmacological classes#
:nl! 2 trials mentioned the primar! outcome of morbidit! and mortalit! and both
these trials reported no ma9or morbidit! or mortalit!# <rom this revie" there is no
observed evidence that pharmacological agents influence morbidit! or mortalit!#
,his revie" also suggests that the pre4treatment "ith pharmacological
interventions is associated "ith a decreased ris= of arrh!thmias# Bone of the
studies commented on the percentage of patients re+uiring treatment for the
observed arrh!thmias or an! further conse+uences related to the rh!thm
disturbances#
3( studies included m!ocardial ischaemia# Bone of the studies examined the final
outcome of intra operative evidence of ischaemia in the post4operative period#
:ver all- pharmacological intervention reduced the ris= of m!ocardial ischaemia#
0ut all the evidence came from ; trials and therefor it should be treated "ith
caution# <urther- ocal anaesthetic "as the onl! contributor in this sub group but
the anal!sis "as dominated b! a single stud!# A bloc=ers "ere the largest
contributor in this sub group anal!sis and sho"ed no advantage# :nce again this
should be treated "ith caution as the studies "ere mostl! underpo"ered to loo=
for this complication#
*n the sub group anal!sis comparing high ris= '(7 studies) to lo" ris= patients-
treatment "as effective in lo" ris= patients but not in high ris= patients# ,his could
be due to underpo"ering of the studies or due to other medications not accounted
for in the high ris= group# :verall all the studies "ere underpo"ered to detect a
reduction in the ris= of EC2 abnormalities#
*n summar!- in lo" ris= patients- pre4induction use of pharmacological agents
reduces the ris= of arrh!thmias from (3? to .? and appears effective in reducing
the ris= of m!ocardial ischaemia#
*n high ris= patients pharmacological agents resulted in a reduction in the ris= of
arrh!thmias but not in EC2 evidence of ischaemia#
,he above summar! must be vie"ed "ith the limitations discussed previousl!#
Page (; of 27
CONCLUSION
Evidence of the hemod!namic effect to E,* has been available for more than %&
!ears# ,he precise mechanism is still being debated but the immediate
ph!siological conse+uences are "ell documented#
Bumerous methods are available to attenuate this response and literarll!
thousands of trials have been done to this regard# ,he long4term conse+uences
and effect on morbidit! and mortalit! of the intubation response in different
surgical population groups are not "ell established# ,herefore the benefit of
attenuating this response in all patients is not clear cut#
,he interventions applied to blunt the response are not "ithout complications-
some of "hich have their o"n effect on morbidit! and mortalit!#
*n certain high ris= groups the benefit is inferred as it "ould be unethical to stud!
the conse+uence of not blunting the response#
Modification of the haemod!namic response to E,* is an admirable ob9ective and
clearl! "arranted in a select group of patients in "hom a transient h!per4d!namic
episode can lead to catastrophe# 8o"ever- extending the principle of vigilant
haemod!namic control to the entire peri4operative period holds more logic than
tunnel vision surrounding the 2 minutes around intubation#
Page 2& of 27
REFERENCES
(# $*B2 0D- 8A66*5 C-# 6eflex circulator! responses to direct lar!ngoscop!
and tracheal intubation performed during general anesthesia# Anesthesiolog!#
(;/( 5ep-(2'/)://%1%%#
2# $ovac # Controlling the hemod!namic response to lar!ngoscop! and
endotracheal intubation# I# Clin# Anesth# Anesth# (;;% <ebP7'():%317;#
3# Cohra A- $umar 5- Charlton AI-#Effect of diabetes mellitus on the
cardiovascular responses to induction of anaesthesia and tracheal intubation#
0r# I# Anaesth (;;3 Aug Q7('2):2/71%(#
.# o" IM- 8arve! I,- Pr!s46oberts C- 5tudies of anaesthesia in relation to
h!pertension# C**: Adrenergic responses to lar!ngoscop!# 0r# I# Anaesth#
Q*nternetR# (;7% Ma!P/7'/):.7(17#
/# <*2GE6ED: E and 2A6C*A4<GEB,E5 E# M# Assessment of the efficac! of
esmolol on the haemod!namic changes induced b! lar!ngoscop! and tracheal
intubation : A meta4anal!sis# Acta Anaesthesiol 5cand# 2&&(P('(():(&((122#
%# 5immons 5- 5chleich a# Air"a! regional anesthesia for a"a=e fiberoptic
intubation# 6eg# Anesth# 2&&2 MarP27'2):(7&1;2#
7# BS5:6A 4 ,he Be" Sor= 5chool of 6egional Anesthesia 4 6egional T ,opical
Anesthesia for Endotracheal *ntubation
http:DD"""#n!sora#comDtechni+uesDnerve4stimulator4and4surface4based4ra4
techni+uesDhead4and4nec=4bloc=aD3&224regional4topical4anesthesia4for4
endotracheal4intubation#html
7# 2upta A- >a=hloo 6- 2upta C- Mehta A- $apoor 00# Comparison of Esmolol
and ignocaine for Atttenuation of Cardiovascular 5tress response to
ar!ngoscop! and Endotracheal *ntubation# 2&&;P(('2):&13#
;# 5ingh 5# Cardiovascular changes after the three stages of nasotracheal
intubation# 0r# I# Anaesth 2&&3 Bov (-;('/):%%717(#
(hin9i ,- MiEutani ,- Masa!u=i M# 8emod!namic responses to tracheal
intubation "ith lar!ngoscope versus light"and intubating device ',rachlight) in
adults "ith normal air"a!# Anesth# Analg# 2&&2 p# .7&1.7.#
((#8assan 82- el45har=a"! ,S- 6enc= 8- Mansour 2- <ouda A# 8emod!namic
and catecholamine responses to lar!ngoscop! "ith vs# "ithout endotracheal
intubation# Acta Anaesthesiol# 5cand# (;;( p# ..217#
(2#5hribman AI- 5mith 2- Achola $I# Cardiovascular and catecholamine
responses to lar!ngoscop! "ith and "ithout tracheal intubation# 0r# I# Anaesth#
(;77 p# 2;/1;#
(3# Per=ins H0- 2unning M- Crill! I- oc=e! D- :U0rien 0# ,he haemod!namic
response to pre4hospital 65* in in9ured patients# *n9ur!- Elsevier tdP 2&(3 Ma!
..'/):%(7123#
Page 2( of 27
(.# 8amill I<- 0edford 6<- >eaver DC- Colohan A6# idocaine before
endotracheal intubation: intravenous or lar!ngotrachealV Anesthesiolog! -
(;7(//'/):/7717(# Available from:
(/# aurito CE- 0aughman C- 0ec=er 2-Effects of aerosoliEed andDor
intravenous lidocaine on hemod!namic responses to lar!ngoscop! and
intubation in outpatients# Anesth# Analg# (;77 p# 37;1;2#
(%# aurito CE- 0aughman C- 0ec=er 2- Effects of aerosoliEed andDor
intravenous lidocaine on hemod!namic responses to lar!ngoscop! and
intubation in outpatients# Anesth# Analg(;77 Apr-%7'.):37;1;2#
(7# Miller CD- >arren 5I# *C lignocaine fails to attenuate the cardiovascular
response to lar!ngoscop! and tracheal intubation# 0r# I# Anaesth# (;;& Aug
%/'2):2(%1;#
(7# 5=lar 0H- urie 5- EEri ,- idocaine inhalation attenuates the circulator!
response to lar!ngoscop! and endotracheal intubation# I# Clin# Anesth#
.'/):3721/#
(;# ,am 5- Chung <- Campbell M# *ntravenous lidocaine: optimal time of in9ection
before tracheal intubation# Anesth# Analg- (;77 :ctP%%'(&):(&3%17#
2&# 5plinter >M- Cerven=o <# 8aemod!namic responses to lar!ngoscop! and
tracheal intubation in geriatric patients: effects of fentan!l- lidocaine and
thiopentone# Can# I# Anaesth# (;7; IulP3%'.):37&1%#
2(# 8elfman 5M- 2old M*- Deisser EA- 8errington CA# >hich drug prevents
tach!cardia and h!pertension associated "ith tracheal intubation: lidocaine-
fentan!l- or esmololV Anesth# Analg# (;;( Apr -72'.):.721%#
22# >oods a >- Allam 5# ,racheal intubation "ithout the use of neuromuscular
bloc=ing agents# 0r# I# Anaesth# 2&&/ <ebP;.'2):(/&17#
23# Cra"ford DC- <ell D- Achola $I-Effects of alfentanil on the pressor and
catecholamine responses to tracheal intubation# 0r# I# Anaesth# (;77 p# 7&71
(2#
2.# Martineau 6I- ,ousignant CP- Miller D6- Alfentanil controls the
haemod!namic response during rapid4se+uence induction of anaesthesia#
Can# I# Anaesth# (;;& p# 7//1%(#
2/# Miller D6- Martineau 6I- :U0rien 8- 8ull $A-#Effects of alfentanil on the
hemod!namic and catecholamine response to tracheal intubation# Anesth#
Analg# (;;3 p# (&.&1%#
2%# $orpinen 6- 5aarnivaara - 5iren $- 5arna 5# Modification of the
haemod!namic responses to induction of anaesthesia and tracheal intubation
"ith alfentanil- esmolol and their combination# Can# I# Anaesth# (;;/
AprP.2'.):2;713&.#
Page 22 of 27
27# $irb! *I- Borth"ood D- Dodson ME# Modification b! alfentanil of the
haemod!namic response to tracheal intubation in elderl! patients# A dose4
response stud!# 0r# I# Anaesth# (;77 p# 37.17#
27# Maguire a M- $umar B- Par=er I- 6o"botham DI- ,hompson IP#
Comparison of effects of remifentanil and alfentanil on cardiovascular
response to tracheal intubation in h!pertensive patients# 0r# I# Anaesth# 2&&(
IanP7%'():;&13#
2;# ,hompson IP- 8all AP- 6ussell I- Effect of remifentanil on the haemod!namic
response to orotracheal intubation# 0r# I# Anaesth# (;;7 p# .%71;#
3&# 8all AP- ,hompson IP- eslie B a Comparison of different doses of
remifentanil on the cardiovascular response to lar!ngoscop! and tracheal
intubation# 0r# I# Anaesth# 2&&& IanP7.'():(&&12#
3(# 8abib A5- Par=er I- Maguire AM- 6o"botham DI- 58:6,
C:MMGB*CA,*:B Effects of remifentanil and alfentanil on the cardiovascular
responses to induction of anaesthesia and tracheal intubation in the elderl!#
0r# I# Anaesth# 2&&2P77'3):.3&13#
32# Channaiah C0- Char! $- Cl= I- o"4dose fentan!l : hemod!namic response
to endotracheal intubation in normotensive patients# Arch Med 5ci#
2&&7P3'september):2;31;#
33# 5ong 8# 5mall4Dose <entan!l: :ptimal ,ime of *n9ection for 0lunting the
Circulator! 6esponses to ,racheal *ntubation# Anesth# Analg# (;;7P7%:%/71%(#
3.# $autto GM# Attenuation of the circulator! response to lar!ngoscop! and
intubation b! fentan!l# Acta Anaesthesiol# 5cand# (;72 IunP2%'3):2(712(#
3/# <eng C$- Chan $8- iu $B- :r C8- ee ,S# A comparison of lidocaine-
fentan!l- and esmolol for attenuation of cardiovascular response to
lar!ngoscop! and tracheal intubation# Acta Anaesthesiol##(;;% Iun 3.'2):%(17#
3%# Martin DE- 6osenberg 8- Au=burg 5I-o"4dose fentan!l blunts circulator!
responses to tracheal intubation# Anesth# Analg (;72 Aug%('7):%7&1.#
37# Chung <- Evans D# o"4dose fentan!l : haemod!namic re4 sponse during
induc4 tion and intubation in geriatric patients# Can# I# Anaesth#
(;7/P32'%):%2217#
37# $a! 0- Bolan D- Ma!all 6- 8eal! ,E# ,he effect of sufentanil on the
cardiovascular responses to tracheal intubation# Anaesthesia (;77 Apr
2&(3P.2'.):3721%#
3;# Hhang 8- 2uo W# QEffect of different doses of sufentanil on stress responses to
tracheal intubation in patients undergoing heart valve replacement surger!R#
Hhong Ban Da Mue Mue 0ao# Si Mue 0an 2&&7 Iun
Page 23 of 27
.&# *ABBGHH* E- *ABBGHH* M- C*6*: C- C*:A 2- PA6*5* 6- CE6G* A- et
al# Peri4intubation cardiovascular response during lo" dose remifentanil or
sufentanil administration in association "ith propofol ,C*: A double blind
comparison# Minerva Anestesiol# Minerva medicaP 2&&. 7&'3):(&;1(/#
.(# Casati A- <anelli 2# sfenta adult#pdf# Eur# I# Anaesthesiol# 2&&(P(7:(&71(2#
.2# Mue <5- Mu SC- iu S- Sang WS- iao M- iu 8P- et al# Different small4dose
sufentanil blunting cardiovascular responses to lar!ngoscop! and intubation in
children: a randomiEed- double4blind comparison# 0r# I# Anaesth# 2&&7 Ma!
(&&'/):7(7123#
.3# Mue <5- iu $P- iu S- Mu SC- Assessment of small4dose fentan!l and
sufentanil blunting the cardiovascular responses to lar!ngoscop! and
intubation in children# Paediatr# Anaesth# Q*nternetR# 2&&7 Iun Qcited 2&(3 Bov
2%RP(7'%):/%717.# Available from:
..# 2hignone M- Boe C- Calvillo :- Wuintin # Anesthesia for ophthalmic surger!
in the elderl!: the effects of clonidine on intraocular pressure- perioperative
hemod!namics- and anesthetic re+uirement# Anesthesiolog!# (;77 p# 7&71(%#
./# 2hignone M- Wuintin - Du=e PC- Effects of clonidine on narcotic re+uirements
and hemod!namic response during induction of fentan!l anesthesia and
endotracheal intubation# Anesthesiolog!# (;7% p# 3%1.2#
.%# Ma9umdar 5# Comparative evaluation of oral clonidine and midaEolam as
premedication on preoperative sedation and lar!ngoscopic stress response
attenuation for the patients undergoing general anaesthesia# *nt# I# Med# public
8eal# 2&(3P3'3):2&&17#
.7# 2upta $- 5harma D- 2upta P$# :ral premedication "ith pregabalin or
clonidine for hemod!namic stabilit! during lar!ngoscop! and laparoscopic
cholec!stectom!: A comparative evaluation# 5audi I# Anaesth# Q*nternetR# 2&((
Apr Qcited 2&(3 Bov 2%RP/'2):(7;17.# Available from:
http:DD"""#pubmedcentral#nih#govDarticlerender#fcgiV
artidK3(3;3(2TtoolKpmcentreETrendert!peKabstract
.7# aisalmi M- $oivusalo a M- Calta P- ,i==anen *- indgren # Clonidine provides
opioid4sparing effect- stable hemod!namics- and renal integrit! during
laparoscopic cholec!stectom!# 5urg# Endosc# 2&&( Bov (/'(():(33(1/#
.;# 0loor 0C- >ard D5- 0elleville IP- MaEe M# Effects of intravenous
dexmedetomidine in humans# **# 8emod!namic changes# Anesthesiolog! (;;2
Dec77'%):((3.1.2#
/&# Aho M- Er=ola :- $allio A- 5cheinin 8- $orttila $# Dexmedetomidine infusion
for maintenance of anesthesia in patients undergoing abdominal h!sterectom!#
Anesth# Analg# (;;2 DecP7/'%):;.&1%#
Page 2. of 27
/(# Iaa=ola M- Ali4Mel==ilX ,- $anto I-# Dexmedetomidine reduces intraocular
pressure- intubation responses and anaesthetic re+uirements in patients
undergoing ophthalmic surger!# 0r# I# Anaesth#(;;2 Iun %7'%):/7&1/#
/2# 0a9"a 5I5- $aur I- 5ingh A- Parmar 5- Attenuation of pressor response and
dose sparing of opioids and anaesthetics "ith pre4operative dexmedetomidine#
*ndian I# Anaesth 2&(2 Mar /%'2):(2317#
/3# Menda <- $Yner :- 5a!in M- ,Zre 8# Dexmedetomidine as an ad9unct to
anesthetic induction to attenuate hemod!namic response to endotracheal
intubation in patients undergoing fast4trac= CA02# Ann# Card# anaesthesias
Card# Anaest-2&(&-(3'():(%12(#
/.# 5ulaiman 5- $arthe=e!an 60- Ca=amudi M- ,he effects of dexmedetomidine
on attenuation of stress response to endotracheal intubation in patients
undergoing elective off4pump coronar! arter! b!pass grafting# Ann# Card#
Anaesth- 2&(2 -(/'():3;1.3#
//#0iccard 0M- 2oga 5- de 0eurs I# Dexmedetomidine and cardiac protection for
non4cardiac surger!: a meta4anal!sis of randomised controlled trials#
Anaesthesia-2&&7 IanRP%3'():.1(.#
/%# Panda B0- 0harti B- Prasad 5# Minimal effective dose of magnesium sulfate
for attenuation of intubation response in h!pertensive patients# I# Clin# Anesth#
Q*nternetR# ElsevierP 2&(3 MarP2/'2):;217#
/7# Iames M<- 0eer 6E- Esser ID# *ntravenous magnesium sulfate inhibits
catecholamine release associated "ith tracheal intubation# Anesth# Analg#
(;7; IunP%7'%):7721%#
/7# Puri 2D- Marudhachalam $5- Chari P- 5uri 6$# ,he Effect of Magnesium
5ulphate on 8emod!namics and *ts Efficac! in Attenuating the 6esponse to
Endotracheal *ntubation in Patients "ith Coronar! Arter! Disease# Anesth#
Analg# (;;7P77'.):7&71((#
/;# Allen 6>- Iames M<- G!s PC# Attenuation of the pressor response to tracheal
intubation in h!pertensive proteinuric pregnant patients b! lignocaine-
alfentanil and magnesium sulphate# 0r# I# Anaesth- (;;( <eb-%%'2):2(%123#
%&# Ashton >0- Iames M<- Ianic=i P- G!s PC# Attenuation of the pressor
response to tracheal intubation b! magnesium sulphate "ith and "ithout
alfentanil in h!pertensive proteinuric patients undergoing caesarean section#
0r# I# Anaesth (;;( Dec %7'%):7.(17#
%(# <assoula=i a- Melemeni a- Paras=eva a- Petropoulos 2# 2abapentin
attenuates the pressor response to direct lar!ngoscop! and tracheal
intubation# 0r# I# Anaesth- 2&&% Iun-;%'%):7%;173
Page 2/ of 27
%2# $umari *- Pathania C5# A Prospective 6andomised Double40lind Placebo
Controlled ,rial of :ral 2abapentin in Attenuation of 8aemod!namic
6esponses During ar!ngoscop! and ,racheal *ntubation# I# Anaesthesiol#
Clin# Pharmacol# 2&&;P2/'.):.3;1.3#
%3# 0afna G- 2o!al C$- 2arg A# A comparison of different doses of gabapentin to
attenuate the haemod!namic response to lar!ngoscop! and tracheal
intubation in normotensive patients# I# Anaesthesiol# Clin# Pharmacol# 2&((
Ian RP27'():.31%#
%.# Memis D- ,uran A- $aramanlioglu 0- ,iire M# :riginal Article 2abapetitin
reduces cardiovascular responses to lar!ngoscop! and tracheal intubation#
Eur# I# Anaesthesiol# 2&&%P23'7):%7%1;&#
%/# 6astogi 0- 2upta $- 2upta P$- Agar"al 5- Iain M- Chauhan 8# :ral
pregabalin premedication for attenuation of haemod!namic pressor response
of air"a! instrumentation during general anaesthesia: A dose response stud!#
*ndian I# Anaesth- 2&(2 IanP/%'():.;1/.#
%%#,homson *# Editorial ,he haemod!namic response to intubation : a perspective
a rrponse h%mo4 d!nami+ue a l U intu4 bation : un perspective# Can# I#
Anaesth# (;7;P3%'.):3%71;#
%7# 6eich D- 0ennett4guerrero E- 0odian CA- 8ossain 5- >infree >- $rol M#
*ntraoperative ,ach!cardia and 8!pertension Are *ndependentl! Associated
"ith Adverse :utcome in Boncardiac 5urger! of ong Duration# Anesth#
Analg# 2&&2P;/'2):27317#
%7# 0i9=er I0- van $lei >A- Cergou"e S- Eleveld DI- van >olfs"in=el - Moons
$2M- et al# *ntraoperative h!potension and (4!ear mortalit! after noncardiac
surger!# Anesthesiolog! 2&&; DecP((('%):(2(712%#
%;# Mon= ,2- 5aini C- >eldon 0C- 5igl IC# Anesthetic management and one4!ear
mortalit! after noncardiac surger!# Anesth# Analg# 2&&/ Ian(&&'():.1(&#
7&# >alsh M- Devereaux P- 6odseth 6B- 6elationship bet"een *ntraoperative
Mean Arterial Pressure and Clinical :utcomes after Boncardiac 5urger!#
Anesthesiolog!# 2&(3P((;'3):/&71(/#
7(# $han <- Gllah 8# Pharmacological agents for preventing morbidit! associated
"ith the haemod!namic response to tracheal intubation ' 6evie" ) 5GMMA6S
:< <*BD*B25 <:6 ,8E MA*B C:MPA6*5:B# Cochrane Database 5!st#
6ev# 2&(3P'7)#
72# Pharmacolog! for Anaesthesia and *ntensive care- 3
rd
edition-,#E Pec=-5#A 8ill
73# 5undar- A-5- $odali- 6- 5ulaiman- 5# ,he effects of preemptive pregabalin on
attenuation of stress response to endotracheal intubation and opioid4sparing
Page 2% of 27
effect in patients undergoing off4pump coronar! arter! b!pass grafting# Annals
of cardiac anaesthesia 2&(2-(/ '() (742/
Page 27 of 27
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Urget LP MSD Cpu Dhs Special Urgent 001 2020 Closing On 15 04 2020Documento89 pagineUrget LP MSD Cpu Dhs Special Urgent 001 2020 Closing On 15 04 2020Sanjeev JayaratnaNessuna valutazione finora
- Xylocaine Dentaland AdrenalineDocumento3 pagineXylocaine Dentaland AdrenalinePir Majid ShahNessuna valutazione finora
- LidocaineDocumento2 pagineLidocaineLeigh Marie LastimosaNessuna valutazione finora
- ParaphrasingDocumento4 pagineParaphrasingDamla Özkapıcı100% (1)
- Local AnestheticsDocumento35 pagineLocal AnestheticsLuluul MaghfirohNessuna valutazione finora
- Drug Study RLE PDFDocumento15 pagineDrug Study RLE PDFCzarina Isabela Tuazon100% (1)
- PharmacologyDocumento218 paginePharmacologydaisyNessuna valutazione finora
- Use During Pregnancy and LactationDocumento2 pagineUse During Pregnancy and LactationYdha FpNessuna valutazione finora
- MBR 2019 - Anes ENT Ophtha HandoutsDocumento17 pagineMBR 2019 - Anes ENT Ophtha HandoutsNica Lopez FernandezNessuna valutazione finora
- Adverse Effects Following Dental Local ADocumento19 pagineAdverse Effects Following Dental Local AMaura HokamaNessuna valutazione finora
- 4) General Anesthesia in Neonates and Children Agents and Techniques - UpToDateDocumento57 pagine4) General Anesthesia in Neonates and Children Agents and Techniques - UpToDatePablo MartinezNessuna valutazione finora
- Acute Rehabilitation Program After Laparoscopic Colectomy Using Intravenous LidocaineDocumento6 pagineAcute Rehabilitation Program After Laparoscopic Colectomy Using Intravenous LidocaineKu Badlisyah Ku AzizNessuna valutazione finora
- Consensus Recommendations For The Use Of.2Documento9 pagineConsensus Recommendations For The Use Of.2fregianiNessuna valutazione finora
- Nursing Management During Stages of Labor and Delivery UpdatedDocumento40 pagineNursing Management During Stages of Labor and Delivery UpdatedCharlmagne LinnamNessuna valutazione finora
- Math Practice For Paramedic StudentsDocumento8 pagineMath Practice For Paramedic StudentsGreg Zeitlin50% (2)
- LOCAL ANAESTHETIC DRUGS: PROPERTIES AND TOXICITYDocumento35 pagineLOCAL ANAESTHETIC DRUGS: PROPERTIES AND TOXICITYmealiella omarNessuna valutazione finora
- Modern dental pain control techniquesDocumento7 pagineModern dental pain control techniquesProgynanika BarmanNessuna valutazione finora
- Local and Regional Anaesthesia in Dogs Cats Part 1 Overview of Concepts Drugs Grubb Lobprise 2020Documento9 pagineLocal and Regional Anaesthesia in Dogs Cats Part 1 Overview of Concepts Drugs Grubb Lobprise 2020Carolina Duque RodriguezNessuna valutazione finora
- Local Anesthesia in Pediatric Dentistry Lecture Students 2009 MDocumento88 pagineLocal Anesthesia in Pediatric Dentistry Lecture Students 2009 MIoana DănilăNessuna valutazione finora
- Effect of 2% Hyaluronic Acid On The Rate of Healing of Corneal Epithelial Defect After Pterygium SurgeryDocumento9 pagineEffect of 2% Hyaluronic Acid On The Rate of Healing of Corneal Epithelial Defect After Pterygium Surgerykoas mr14Nessuna valutazione finora
- Molecules: Transdermal and Topical Drug Administration in The Treatment of PainDocumento16 pagineMolecules: Transdermal and Topical Drug Administration in The Treatment of PainAbraham GomezNessuna valutazione finora
- Efficient Clinical ProceduresDocumento57 pagineEfficient Clinical ProceduresEmad AlryashiNessuna valutazione finora
- Local Anaesthesia TechniquesDocumento21 pagineLocal Anaesthesia TechniquesZaki MubaraqNessuna valutazione finora
- Perioperative CareDocumento18 paginePerioperative CareCo Pablico EricNessuna valutazione finora
- Indian Medicine ListsDocumento294 pagineIndian Medicine ListsAmjad ShareefNessuna valutazione finora
- OB Drug Study - MethylergonovineDocumento2 pagineOB Drug Study - MethylergonovineJustin Ancog0% (1)
- Drug Allergy BookDocumento332 pagineDrug Allergy Bookmegah_asia13Nessuna valutazione finora
- Pharmacology - MCQsDocumento17 paginePharmacology - MCQsMahmoud HassanNessuna valutazione finora
- Pharm (Nursing) Dosage Practice Problems - Reconstitution With Answers 1Documento5 paginePharm (Nursing) Dosage Practice Problems - Reconstitution With Answers 1Linsey Bowen73% (11)
- Articaine Dental Update 2015Documento5 pagineArticaine Dental Update 2015Ashley WrightNessuna valutazione finora