Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Spine Cages
Caricato da
Eric Chambers0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
13 visualizzazioni16 pagineSpine - Sciatica
Copyright
© © All Rights Reserved
Formati disponibili
DOC, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoSpine - Sciatica
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
13 visualizzazioni16 pagineSpine Cages
Caricato da
Eric ChambersSpine - Sciatica
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 16
Introduction
In recent years the excitement about the
development and use of spine cages has
escalated. However, unless you are a spine
specialist, you may find it difficult to appreciate
what all the commotion is about. Lets face it, for
most people, spine cages are not an everyday
topic of conversation. Most people do not know
what spine cages are, how they are used, and
how they benefit patients.
To begin, a brief introduction to cages is needed
to help you understand why these devices are
so important in spine surgery today ... and
tomorrow.
ages! "n #verview
" cage is a small hollow cylindrical device,
usually made of titanium, with perforated walls.
These devices are sometimes called $interbody
cages.$ The word $interbody$ refers to where
these cages are used %i.e. the disc space
between two vertebrae&. The purpose of using
cages is often to restore lost disc height
resulting from a collapsed disc and to relieve
pressure on nerve roots.
Lost disc height is restored when the cages,
packed with bone graft are inserted into the
space between the two vertebrae. 'asically
what happens is the bone graft, which has been
neatly packed into and around the cages, begins
to grow through the perforated walls of the
cages eventually forming a solid bond %or
$fusion$& holding the vertebrae together. This
process is known as $interbody fusion.$ (ou
could loosely compare cages to building blocks
and bone graft to the mortar that binds the
structure together. The end result is fusion, a
strong and stable construct.
)xample of an LT
age*
inserted between L+
and ,-
. /ray illustrating LT
age*
placement between L+
and ,-
0atients who are to undergo surgery due to
degenerative disc disease, disc herniation or
low/grade spondylolisthesis may have cages
implanted during their surgical procedure. These
conditions can cause vertebrae to grate against
each other during motion and cause nerve
impingement when a disc is damaged. " solid
cage fusion can eliminate the motion, increase
the space for the nerve roots, stabili1e the spine,
restore spine alignment, and relieve pain.
age 2evelopment! " 'rief History
3emarkably, the history of cages begins with
horses. ,everal decades ago 2r. 4eorge 'agby,
an orthopaedic surgeon from ,pokane,
5ashington invented the first cage. 6'agby$s
'asket,6 as it was called, became popular when
a horse named ,eattle ,lew7 the first unbeaten
Triple rown 5inner, was diagnosed with
65obbler$s ,yndrome,6 a degenerative condition
causing serious neck instability.
5orking with an e8uine veterinary specialist, 2r.
'agby implanted his cylindrical stainless steel
6basket6 into ,eattle ,lew$s spine.
"fter securing the basket in place, it was packed
with the horse$s own bone graft. In time the bone
graft grew into and around the basket creating a
solid fusion and saving ,eattle ,lew from certain
death. "fter the ,eattle ,lew episode, several
years passed without any notable cage
developments. Then in the late -9:;$s significant
advancement was made when 2r. ,tephen 2.
<uslich, a spine surgeon from Minneapolis,
Minnesota converted 2r. 'agby$s design into a
cage suitable for human use. 2r. <uslich$s cage,
a threaded hollow titanium cylinder with thick
perforated walls, was designed for the posterior
%back& part of the spine. His cage design 8uickly
caught the attention of his peers.
,ince then, several surgeons, including myself
became involved to develop anterior cage
systems.
"nterior 0lacement! 5hy=
"n anterior approach, meaning through the front
of the body, allows the surgeon to work through
the abdomen to reach the spine. In this way
spine muscles located in the back are not
damaged or cut7 avoiding muscle weakness and
scarring. In addition, minimally invasive surgical
techni8ues serve to dramatically accelerate
patient recovery. #ver 9;/percent of my patients
who have undergone this procedure have gone
home the morning after surgery.
The >ext 4eneration of ages Today
In recent years cages have undergone
numerous modifications to improve their
effectiveness. ,ome of these cages include the
'"<* , 3ay T?* , the ontact ?usion
age* , and I>T)3 ?I.* .
LT age*
"lthough, as a patient, you don$t need to
understand all the technical details about cages,
we thought we would highlight some basic
details about a specific cage. #ne of the newest
and most technically advanced is the LT age*
. ,urgeons are reporting very good results using
this cage as a result of its uni8ue design
elements. ?or example!
The LT age* is tapered %similar to a door
wedge&. This cage$s tapered shape helps to
restore the spine$s correct alignment or
curves7 an essential goal of spine surgery.
#ften surgeons use two cages next to each
other in surgery. The problem in the past
has been the curved sides of cages make it
difficult to get the cages close together. The
LT age* has flat sides, meaning that
cages can be placed very close together.
This might sound like a small change, but it
is an important development to help cages
succeed in creating strong constructs.
The perforations or holes in the cage walls
are larger thus helping create fusion by
allowing for increased bony growth in and
around the cage.
The LT age * is titanium, which makes it
very strong and durable. There are no
reported cases of an LT age* failing
structurally. In addition, its titanium
construction allows the cage to be seen by
T or M3I scanning.
If you are interested in more technical
information about the LT age* , click here.
5ill a age be @sed in (our ,urgery=
Hundreds of thousands of people suffer from
degenerative disc disease, disc herniation or
low/grade spondylolisthesis. Thankfully, surgery
is not necessary for the vast maAority of patients
as non/surgical treatments most often provide
relief from symptoms. However, for those
patients who do re8uire surgery, we hope this
article will help you better understand what the
surgeon means when he discusses your surgical
options and refers to using cages. If you want to
learn more about cages, see the links following
this article.
"nd remember, if you are scheduled for surgery,
patients who are motivated to maintain a healthy
lifestyle and take responsibility for their care,
make great patientsB Their commitment to health
puts them in the fast lane for a more rapid
recovery from surgery.
ages have been used since -99C to help fuse
lumbar vertebra. The lumbar vertebrae are the
bones of the spinal column. These bones are
separated from each other by the lumbar disc,
which acts as a shock absorber. The spinal cord
and spinal nerves run behind the vertebral
bodies and disc and are covered by surrounding
bone and Aoints that are on the back, or
posterior, portion of the spine. Traditionally,
spinal fusions were performed by laying bone
graft on the back, or posterior, aspects of the
spine in hopes that they would fuse, or heal,
together. However, this necessitated incisions in
the back and division of the back musculature.
The fusion rate with laying bone on the spine
only, was less than optimal and therefore, the
systems to make the spine more rigid, such as
screws and rods, were developed. However,
these screw and rod systems also necessitated
muscle dissection from the back of the spine.
?usion cages were developed to allow the spine
to heal between the vertebral bodies rather than
along the back of the spine. 'y completely
removing the disc, which is between vertebral
bodies, and replacing it with cages and bone
graft, a more stable fusion can be obtained. In
years past, fusions of this type were attempted
by replacing the disc with bone graft alone.
However, this led to collapse of the graft and a
poor rate of healing. 'y utili1ing metallic or
carbon fiber fusion cages, structural support is
obtained from the cage while healing goes on
both through the cage and around the cage with
bone graft or bone substitutes.
The most common indication for an anterior
fusion with cages is disc degeneration. In this
case, a patient will have chronic low back pain
because his disc has degenerated, or collapsed.
This is often a conse8uence of a previous disc
herniation, an inAury where the disc is torn, or
from accelerated degeneration from repetitive
trauma, smoking or obesity. 0atients often
complain of chronic back pain that may radiate
into the buttocks. >on/surgical treatments for
degenerative disc disease include aggressive
and active physical therapy for strengthening the
trunk musculature, the short/term use of a brace
or corset, anti/inflammatory medications. Most
patients can learn to live with their back pain
from disc degeneration through non/operative
means. However, for those patients in whom
pain is severe or unremitting, surgical fusion is
an option.
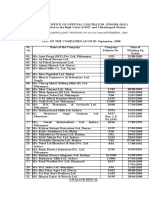
2isc 2egeneration
0ost/operative ./3ays showing cage
placement %LT cages&
"nterior fusion means the surgeon will approach
the spine from the front. The surgeon can
access the spine anteriorly using a vertical
transperitoneal incision %vertical incision through
the abdominal cavity&, a hori1ontal
retroperitoneal incision %hori1ontal incision
behind the abdominal cavity&, or
laparoscopically.
#pen Incision
In all three of these techni8ues, the internal
abdominal organs are moved away from the
spine and allow the surgeon to completely
remove the disc from the front. This gives the
surgeon a better view of the disc and allows a
more complete disc removal. In surgery, the disc
height can be restored by distracting within the
disc space. This not only restores the normal
height and alignment of the vertebral column but
also provides stability by placing the ligaments
at that level in tension. This new distracted
height is then maintained by threading the fusion
cages in place. These cages are first filled with
bone graft, which can then heal between the end
plates of the vertebral bodies. ?inally, the space
between the cages and in front of the cages is
filled with bone graft as well.
Typically, patients remain in the hospital from
one to three days after a fusion with cages. They
are allowed to walk and perform non/impact
aerobic exercise as tolerated within the first few
weeks. More aggressive weight lifting and trunk
exercises can usually be begun within six to
eight weeks. In my experience, by performing an
anterior interbody fusion with cages and
avoiding any posterior incision, patients recover
more 8uickly and more completely after this type
of fusion.
age fusions have good results for one or two
level degenerative disc disease. ?or fusions that
entail more than two levels of fusion, the results
of cage fusions have been less than optimal.
age fusions are not indicated for high/grade
spondylolisthesis or patients with marked
instability of the spine.
Most patients, once their fusion is solid, can
return to normal activities. I typically do not
restrict my patients from aggressive athletic
activities or manual labor following a successful
fusion. #bviously, the individual indications for
this procedure must be discussed with your
spinal surgeon.
)2IT#3I"L '#"32 #MM)>T
DThe use of cage devices has increased in
popularity since the early -99;s. Their
development highlighted the need to develop a
better method of achieving a solid fusion at the
disc space. "ccess to the disc space using
these devices may be accomplished from the
front or from the back. The surgical approach
rate is divided approximately e8ually in this
country. The advantages of accessing the disc
space from the front are discussed above in 2r.
EdeblickFs article. #ther authors have
experienced e8ually good results with insertion
of the cages from the back7 however, recovery
time may be prolonged due to stripping of the
muscles necessary to access the disc from the
back.
urrently neural generation of cages has been
developed, not only to promote fusion but also to
obtain and maintain more anatomic angles
between the disc spaces of the lumbar spine.
urrently, titanium and donor bone are the most
popular materials used in making fusion cages.
#ther biologic materials are also being
considered. Their use is currently limited.
To date, experienced surgeons have reported
successful outcomes when using these cage
devices. Their superiority in promoting fusion at
the disc level when compared to more traditional
methods should help the patient recover.G
Hean Hac8ues "bitbol, M2, ?3, / )ditorial
'oard, ,pine@niverse.com
Potrebbero piacerti anche
- Body Mind MasteryDocumento13 pagineBody Mind MasteryEric ChambersNessuna valutazione finora
- Adithi StatmentDocumento2 pagineAdithi StatmentEric ChambersNessuna valutazione finora
- Elastane Blends1Documento37 pagineElastane Blends1Foued Ben Salem100% (1)
- Inefficient MarketDocumento4 pagineInefficient MarketEric ChambersNessuna valutazione finora
- The Law of Attraction: Tune in, babyDocumento14 pagineThe Law of Attraction: Tune in, babyEric Chambers71% (7)
- The Law of Attraction: Tune in, babyDocumento14 pagineThe Law of Attraction: Tune in, babyEric Chambers71% (7)
- A Big Mind, A Big HeartDocumento14 pagineA Big Mind, A Big HeartEric ChambersNessuna valutazione finora
- A New EarthDocumento13 pagineA New EarthEric Chambers100% (1)
- The Route To PerformanceDocumento3 pagineThe Route To PerformanceEric ChambersNessuna valutazione finora
- Where'd All This Rain Come FromDocumento10 pagineWhere'd All This Rain Come FromEric ChambersNessuna valutazione finora
- RiskDocumento6 pagineRiskEric ChambersNessuna valutazione finora
- Microeconomics 101Documento3 pagineMicroeconomics 101Eric ChambersNessuna valutazione finora
- Random ThoughtsDocumento4 pagineRandom ThoughtsEric Chambers100% (1)
- Fight For Your MoneyDocumento11 pagineFight For Your MoneyEric ChambersNessuna valutazione finora
- 0 - Hathaway Production ProcessesDocumento7 pagine0 - Hathaway Production ProcessesEric ChambersNessuna valutazione finora
- Costco Non-Foods QA Manual Provides Apparel Testing GuidelinesDocumento45 pagineCostco Non-Foods QA Manual Provides Apparel Testing GuidelinesEric Chambers0% (1)
- Sunny LowerDocumento1 paginaSunny LowerEric ChambersNessuna valutazione finora
- The Magic TriangleDocumento1 paginaThe Magic TriangleEric ChambersNessuna valutazione finora
- Walmart Yellow Asses Ment LetterDocumento2 pagineWalmart Yellow Asses Ment LetterEric Chambers100% (1)
- Tesco 1Documento8 pagineTesco 1Eric ChambersNessuna valutazione finora
- HTC Touch ManualDocumento208 pagineHTC Touch Manualminkx100% (38)
- TescoDocumento19 pagineTescoEric ChambersNessuna valutazione finora
- Pantaloon Crew 24.1.06Documento1 paginaPantaloon Crew 24.1.06Eric ChambersNessuna valutazione finora
- Costco Combined Regions - Adult Knit Protocol 1102 - 0 - May 10 2006Documento35 pagineCostco Combined Regions - Adult Knit Protocol 1102 - 0 - May 10 2006Eric ChambersNessuna valutazione finora
- Compliance TNADocumento7 pagineCompliance TNAEric ChambersNessuna valutazione finora
- Flat KnitsDocumento1 paginaFlat KnitsEric ChambersNessuna valutazione finora
- Amaraja Batteries - Annual Report - 06 - 07Documento64 pagineAmaraja Batteries - Annual Report - 06 - 07Eric ChambersNessuna valutazione finora
- E-Book - Kung Fu MovementsDocumento17 pagineE-Book - Kung Fu MovementsEric Chambers100% (2)
- DT-18-18 1 06Documento1 paginaDT-18-18 1 06Eric ChambersNessuna valutazione finora
- TnaDocumento1 paginaTnaEric ChambersNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- USA V BRACKLEY Jan6th Criminal ComplaintDocumento11 pagineUSA V BRACKLEY Jan6th Criminal ComplaintFile 411Nessuna valutazione finora
- Positioning for competitive advantageDocumento9 paginePositioning for competitive advantageOnos Bunny BenjaminNessuna valutazione finora
- Lecture 4Documento25 pagineLecture 4ptnyagortey91Nessuna valutazione finora
- Practical Research 2: Self-Learning PackageDocumento3 paginePractical Research 2: Self-Learning PackagePrinces BaccayNessuna valutazione finora
- Ramdump Memshare GPS 2019-04-01 09-39-17 PropsDocumento11 pagineRamdump Memshare GPS 2019-04-01 09-39-17 PropsArdillaNessuna valutazione finora
- VL2019201000534 DaDocumento2 pagineVL2019201000534 DaEnjoy LifeNessuna valutazione finora
- Electrosteel Castings Limited (ECL) - Technology That CaresDocumento4 pagineElectrosteel Castings Limited (ECL) - Technology That CaresUjjawal PrakashNessuna valutazione finora
- Vidura College Marketing AnalysisDocumento24 pagineVidura College Marketing Analysiskingcoconut kingcoconutNessuna valutazione finora
- Expressive Matter Vendor FaqDocumento14 pagineExpressive Matter Vendor FaqRobert LedermanNessuna valutazione finora
- The Singular Mind of Terry Tao - The New York TimesDocumento13 pagineThe Singular Mind of Terry Tao - The New York TimesX FlaneurNessuna valutazione finora
- PW CDocumento4 paginePW CAnonymous DduElf20ONessuna valutazione finora
- Honors Biology Unit 2 - Energy Study GuideDocumento2 pagineHonors Biology Unit 2 - Energy Study GuideMark RandolphNessuna valutazione finora
- Transformer Oil Testing MethodsDocumento10 pagineTransformer Oil Testing MethodsDEE TOTLVJANessuna valutazione finora
- Individual Sports Prelim ExamDocumento13 pagineIndividual Sports Prelim ExamTommy MarcelinoNessuna valutazione finora
- The Teacher and The Community School Culture and Organizational LeadershipDocumento10 pagineThe Teacher and The Community School Culture and Organizational LeadershipChefandrew FranciaNessuna valutazione finora
- Impolitic Art Sparks Debate Over Societal ValuesDocumento10 pagineImpolitic Art Sparks Debate Over Societal ValuesCarine KmrNessuna valutazione finora
- B. Ing Kls 6Documento5 pagineB. Ing Kls 6siskaNessuna valutazione finora
- Miami Police File The O'Nell Case - Clemen Gina D. BDocumento30 pagineMiami Police File The O'Nell Case - Clemen Gina D. Barda15biceNessuna valutazione finora
- Reinvestment Allowance (RA) : SCH 7ADocumento39 pagineReinvestment Allowance (RA) : SCH 7AchukanchukanchukanNessuna valutazione finora
- MSDS FluorouracilDocumento3 pagineMSDS FluorouracilRita NascimentoNessuna valutazione finora
- Suband Coding in MatlabDocumento5 pagineSuband Coding in MatlabZoro Roronoa0% (1)
- Doe v. Myspace, Inc. Et Al - Document No. 37Documento2 pagineDoe v. Myspace, Inc. Et Al - Document No. 37Justia.comNessuna valutazione finora
- Tender Notice and Invitation To TenderDocumento1 paginaTender Notice and Invitation To TenderWina George MuyundaNessuna valutazione finora
- Design and Analysis of Crankshaft ComponentsDocumento21 pagineDesign and Analysis of Crankshaft Componentssushant470% (1)
- Microsoft Word 2000 IntroductionDocumento72 pagineMicrosoft Word 2000 IntroductionYsmech SalazarNessuna valutazione finora
- Ana White - PLANS - A Murphy Bed YOU Can Build, and Afford To Build - 2011-03-03Documento20 pagineAna White - PLANS - A Murphy Bed YOU Can Build, and Afford To Build - 2011-03-03Ahmad KamilNessuna valutazione finora
- Machine Spindle Noses: 6 Bison - Bial S. ADocumento2 pagineMachine Spindle Noses: 6 Bison - Bial S. AshanehatfieldNessuna valutazione finora
- Statement of Compulsory Winding Up As On 30 SEPTEMBER, 2008Documento4 pagineStatement of Compulsory Winding Up As On 30 SEPTEMBER, 2008abchavhan20Nessuna valutazione finora
- Condy LatorDocumento11 pagineCondy LatorrekabiNessuna valutazione finora
- Bluetooth Home Automation Using ArduinoDocumento25 pagineBluetooth Home Automation Using ArduinoRabiNessuna valutazione finora