Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Transfusion en Paciente Critico
Caricato da
Felipe Murillo Arias0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
22 visualizzazioni2 pagineA single centre cohort study evaluating the relationship between anaemia, blood transfusions and mortality in patients admitted to a surgical ICU. The authors found that transfusions were associated with lower patient mortality, especially among older sicker patients. This contradicts the majority of previous cohort studies and the only large randomised trial of different transfusion triggers in critically ill patients.
Descrizione originale:
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoA single centre cohort study evaluating the relationship between anaemia, blood transfusions and mortality in patients admitted to a surgical ICU. The authors found that transfusions were associated with lower patient mortality, especially among older sicker patients. This contradicts the majority of previous cohort studies and the only large randomised trial of different transfusion triggers in critically ill patients.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
22 visualizzazioni2 pagineTransfusion en Paciente Critico
Caricato da
Felipe Murillo AriasA single centre cohort study evaluating the relationship between anaemia, blood transfusions and mortality in patients admitted to a surgical ICU. The authors found that transfusions were associated with lower patient mortality, especially among older sicker patients. This contradicts the majority of previous cohort studies and the only large randomised trial of different transfusion triggers in critically ill patients.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 2
Dr Sakr and colleagues [1] report a single centre cohort
study evaluating the relationship between anaemia, blood
transfusions and mortality in patients admitted to a
surgical ICU. Te authors report some ndings that are
not new or surprising, namely that anaemia is associated
with adverse patient outcomes. However, when they
performed multivariate analyses with adjustment for
potential confounders to the blood transfusion/patient
outcomes relationship they found that transfusions were
associated with lower patient mortality, especially among
older sicker patients. At face value this contradicts the
majority of previous cohort studies [2] and the only large
randomised trial of dierent transfusion triggers in
critically ill patients (the Canadian Critical Care Trials
Groups Transfusion requirements in critical care
(TRICC) trial) [3]. Te authors ndings raise a number
of questions, including: does this association indicate
cause and eect? Are the ndings of the TRICC trial
generalisable to intensive care patients today? And,
perhaps most importantly, should we use blood more
liberally in critically ill patients than the TRICC trial and
our current guidelines suggest?
Does this association indicate cause and efect?
Although it is possible to perform complex statistical
adjustments for potential confounders in cohort studies
to try to clarify the true relationship between a variable
or intervention of interest and an outcome, this is
notoriously problematic, especially in relation to blood
transfusions [4]. Adjustments can be made for measured
factors, but there is always the possibility of residual
confounding from unknowns, which is more likely in
complex heterogeneous populations. ICU populations
are highly heterogeneous at multiple levels, including
pre-illness co-morbidity, diagnosis requiring admission,
early illness severity, and subsequent complications, to
name a few. Dr Sakr and colleagues included adjustment
for some factors but, as they acknowledge, it is very likely
there were many unknowns that were potentially rele-
vant. Bias by indication is very likely in this sort of
analysis whereby factors aecting a clinical decision (blood
transfusion in this case) cannot be adequately captured
or adjusted for, thereby introducing an imbalance. Dr
Sakr and colleagues used propensity analysis in an
attempt to overcome this problem, which attempts to
produce matched pairs from observational data to
simulate a virtual randomised trial. Te limitations of
this approach have been previously discussed in detail in
relation to another cohort study involving some of these
authors [5,6]. Although the chance of erroneous asso-
ciations is probably reduced, the problem remains that
the patients being matched may dier in unmeasured
ways. Tis might be more likely in a single centre study,
such as the one performed by Dr Sakr and colleagues,
where transfusion decision-making was presumably
more consistent. Te mean hemoglobin transfusion
trigger was 8.2 g/dL and in 30% of cases it was >9 g/dL, so
this ICU was signicantly more liberal than the restrictive
arm of the TRICC trial [3]. Another issue is that there
was no information about the indications for transfusion,
especially bleeding, which could have created imbalance
between the matched pairs. In short, we cannot be sure
of causality between blood transfusions and better
outcomes, but the study does stimulate us to look again
at the TRICC trial and its relevance today.
Abstract
Current evidence suggests that critically ill patients
tolerate anaemia well and that blood transfusions
may increase the risk of adverse outcomes. Dr Sakr
and colleagues present a contradictory analysis of a
surgical ICU cohort, fnding an association between
blood transfusions and lower hospital mortality after
adjustment for a range of potential confounders.
Analyses of this kind are interesting and provocative,
but are limited by residual confounding and bias by
indication. The data emphasise the need for additional
high quality trials of transfusion practice in critical care.
2010 BioMed Central Ltd
Red cell transfusion triggers in critically ill patients:
time for some new TRICCs?
Timothy S Walsh*
See related research by Sakr et al., http://ccforum.com/content/14/3/R92
COMMENTARY
*Correspondence: twalsh@stafmail.ed.ac.uk
Anaesthetics, Critical Care and Pain Medicine, Royal Infrmary of Edinburgh, Little
France Crescent, Edinburgh EH16 2SA, UK
Walsh Critical Care 2010, 14:170
http://ccforum.com/content/14/3/170
2010 BioMed Central Ltd
Are the fndings of the TRICC trial generalisable to
intensive care patients today?
Te TRICC trial found that mortality was higher in
younger patients (aged <55 years) and those with
APACHE II scores <20 when blood was used liberally [3].
Treatment eects were similar for older patients and
those with APACHE II scores 20, and in subgroup
analyses no strong signals favouring either group were
found in relation to duration of mechanical ventilation
[7], or trauma diagnosis [8]. Patients with ischemic heart
disease as a baseline comorbidity had a trend towards
better outcome with more liberal blood use [9] and a
later analysis highlighted the potential interaction
between ischemic heart disease and the hemoglobin level
maintained in intensive care, which could have been
underestimated in the original trial report [10]. All of
these subgroup analyses were underpowered, and even
the full trial was much smaller than intended (the
intended sample size was 1,620; achieved was 838).
Another relevant factor was that clinicians declined to
enrol 29% of eligible patients. Tese issues raise the
possibility that dierent treatment eects might exist for
patients with ischemic heart disease, and among older
and/or sicker patients, especially those with evidence of
inadequate oxygen delivery or delayed weaning from
mechanical ventilation. Tese uncertainties are acknow-
ledged in recent guidelines and systematic reviews
[11,12], and it is perhaps not surprising that surveys
indicate continued variation in clinical practice [11,13].
Te other key uncertainty relates to the impact of pre-
storage leucodepletion, which was not used during the
TRICC trial, but is now undertaken routinely in most
developed countries. Tis additional processing step was
associated with small (1% absolute risk reduction) but
signicant ICU mortality reduction in Canada, and may
be particularly important with prolonged red cell storage
[14,15].
Should we use blood more liberally in critically
ill patients than the TRICC trial and our current
guidelines suggest?
Te answer to this question for younger, less severely
unwell patients is surely NO. For other patients we need
to continue to use clinical judgement, but the evidence is
still most consistent with a target haemoglobin concen-
tration of <9 g/dL, especially given the potential risks of
blood transfusions and uncertain eectiveness of stored
red cells [11,15]. Given our recent experiences of thera-
peutic strategies with early promise, but for which later
trials showed conicting safety data either overall (for
example, tight glycaemic control) or in patient subgroups
(for example, activated protein C), it is surely time for a
new TRICC. Only well designed randomised trials will
improve our condence in making transfusion decisions.
Unfortunately, studies such as the one performed by Dr
Sakr and colleagues simply add to our uncertainty.
Abbreviations
TRICC = Transfusion requirements in critical care.
Competing interests
The author declares that he has no competing interests.
Published: 23 June 2010
References
1. Sakr Y, Lobo S, Knuepfer S, Esser E, Bauer M, Settmacher U, Barz D, Reinhart K:
Anemia and blood transfusion in a surgical intensive care unit. Crit Care
2010, 14:R92.
2. Marik PE, Corwin HL: Ef cacy of red blood cell transfusion in the critically ill:
a systematic review of the literature. Crit Care Med 2008, 36:2667-2674.
3. Hbert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G,
Tweeddale M, Schweitzer I, Yetisir E: A multicenter, randomized, controlled
clinical trial of transfusion requirements in critical care. N Engl J Med 1999,
340:409-417.
4. Carson JL, Reynolds RC, Klein HG: Bad bad blood? Crit Care Med 2008,
36:2707-2708.
5. Vincent JL, Sakr Y, Sprung C, Harboe S, Damas P: Are blood transfusions
associated with greater mortality rates? Results of the Sepsis Occurrence
in Acutely Ill Patients study. Anesthesiology 2008, 108:31-39.
6. Nuttall GA, Houle TT: Liars, damn liars, and propensity scores. Anesthesiology
2008, 108:3-4.
7. Hbert PC, Blajchman MA, Cook DJ, Yetisir E, Wells G, Marshall J, Schweitzer I;
Transfusion Requirements in Critical Care Investigators for the Canadian
Critical Care Trials Group: Do blood transfusions improve outcomes related
to mechanical ventilation? Chest 2001, 119:1850-1857.
8. McIntyre L, Hebert PC, Wells G, Fergusson D, Marshall J, Yetisir E, Blajchman
MJ; Canadian Critical Care Trials Group: Is a restrictive transfusion strategy
safe for resuscitated and critically ill trauma patients? J Trauma 2004,
57:563-568.
9. Hbert PC, Yetisir E, Martin C, Blajchman MA, Wells G, Marshall J, Tweeddale
M, Pagliarello G, Schweitzer I; Transfusion Requirements in Critical Care
Investigators for the Canadian Critical Care Trials Group: Is a low transfusion
threshold safe in critically ill patients with cardiovascular diseases? Crit
Care Med 2001, 29:227-234.
10. Deans KJ, Minneci PC, Sufredini AF, Danner RL, Hofman WD, Ciu X, Klein HG,
Schechter AN, Banks SM, Eichacker PQ, Natanson C: Randomisation in
clinical trials of titrated therapies: unintended consequences of using
fxed treatment protocols. Crit Care Med 2007, 35:1509-1516.
11. Napolitano LM, Kurek S, Luchette FA, Corwin HL, Barie PS, Tisherman SA,
Hebert PC, Anderson GL, Bard MR, Bromberg W, Chiu WC, Cipolle MD, Clancy
KD, Diebel L, Hof WS, Hughes KM, Munshi I, Nayduch D, Sandhu R, Yelon JA;
American College of Critical Care Medicine of the Society of Critical Care
Medicine; Eastern Association for the Surgery of Trauma Practice
Management Workgroup: Clinical practice guideline: red blood cell
transfusion in adult trauma and critical care. Crit Care Med 2009,
37:3124-3157.
12. Hill SR, Carless PA, Henry DA, Carson JL,Hebert PC, Henderson KM:
Transfusion thresholds and other strategies for guiding allogeneic red
blood cell transfusion. Cochrane Database Syst Rev 2002:CD002042.
13. Walsh TS, Maciver CR: A clinical scenario-based survey of transfusion
decisions for intensive care patients with delayed weaning from
mechanical ventilation. Transfusion 2009, 49:2661-2667.
14. Hbert PC, Fergusson D, Blajchman MA, Wells GA, Kmetic A, Coyle D, Heddle
N, Germain M, Goldman M, Toye B, Schweitzer I, vanWalraven C, Devine D,
Sher GD; Leukoreduction Study Investigators: Clinical outcomes following
institution of the Canadian universal leukoreduction program for red
blood cell transfusions. JAMA 2003, 289:1941-1949.
15. Zimrin AB, Hess JR: Current issues relating to the transfusion of stored red
blood cells. Vox Sanguinis 2009, 96:93-103.
doi:10.1186/cc9043
Cite this article as: Walsh TS: Red cell transfusion triggers in critically ill
patients: time for some new TRICCs? Critical Care 2010, 14:170.
Walsh Critical Care 2010, 14:170
http://ccforum.com/content/14/3/170
Page 2 of 2
Potrebbero piacerti anche
- Future E-Waste ScenariosDocumento19 pagineFuture E-Waste Scenariosmariiusssica2008Nessuna valutazione finora
- TBCDocumento3 pagineTBCwenyinriantoNessuna valutazione finora
- Future E-Waste ScenariosDocumento19 pagineFuture E-Waste Scenariosmariiusssica2008Nessuna valutazione finora
- Opti 755 TechspecsDocumento45 pagineOpti 755 TechspecsPlacidus DsilvaNessuna valutazione finora
- Colombia Highlights Spanish Web PDFDocumento16 pagineColombia Highlights Spanish Web PDFFelipe Murillo AriasNessuna valutazione finora
- Logo 2Documento1 paginaLogo 2Felipe Murillo AriasNessuna valutazione finora
- Enflis ClapDocumento1 paginaEnflis ClapFelipe Murillo AriasNessuna valutazione finora
- 1 s2.0 S2319417016000093 MainDocumento7 pagine1 s2.0 S2319417016000093 MainFelipe Murillo AriasNessuna valutazione finora
- Actualizacion en Hipertension Pulmonar 2013 JaccDocumento13 pagineActualizacion en Hipertension Pulmonar 2013 JaccFelipe Murillo AriasNessuna valutazione finora
- Lo Mejor ArcgisDocumento190 pagineLo Mejor ArcgisFelipe Murillo AriasNessuna valutazione finora
- Acv Hemorragico Lancet 2009Documento25 pagineAcv Hemorragico Lancet 2009Felipe Murillo AriasNessuna valutazione finora
- Clase 3-Distribucion FasesDocumento41 pagineClase 3-Distribucion FasesFelipe Murillo AriasNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Jurnal 2Documento8 pagineJurnal 2AnggunbokingsNessuna valutazione finora
- GMMMC Sukkur MbbsDocumento6 pagineGMMMC Sukkur MbbsSherazAhmedNessuna valutazione finora
- Helping Psychiatry Residents Cope With Patient SuicideDocumento5 pagineHelping Psychiatry Residents Cope With Patient SuicidedrguillermomedinaNessuna valutazione finora
- Hospitalization and Its Effect For Patient - UNTAD 2011 PDFDocumento26 pagineHospitalization and Its Effect For Patient - UNTAD 2011 PDFRiris SutrisnoNessuna valutazione finora
- Special Round Seats For MD - MS - Diploma & DNB SeatsDocumento23 pagineSpecial Round Seats For MD - MS - Diploma & DNB SeatsManoj KashyapNessuna valutazione finora
- Revision Notes On FRCRDocumento385 pagineRevision Notes On FRCRObaidy Albushaher100% (2)
- Acetaminophen (Paracetamol, Tylenol, Tempra, Panadol)Documento3 pagineAcetaminophen (Paracetamol, Tylenol, Tempra, Panadol)Jocelyn Rivera0% (1)
- Case Report: Hepatitis BDocumento34 pagineCase Report: Hepatitis Bdewi sartikaNessuna valutazione finora
- Law Exam NotesDocumento11 pagineLaw Exam NotesEric Cheng100% (1)
- Notes On MRI - FinalDocumento16 pagineNotes On MRI - FinalAnju GuptaNessuna valutazione finora
- Dietary Supplements and Functional Foods 2 Sides of A Coin PDFDocumento7 pagineDietary Supplements and Functional Foods 2 Sides of A Coin PDFNoor FadhilaNessuna valutazione finora
- JednjakDocumento15 pagineJednjakbojana1994Nessuna valutazione finora
- 1st Floor No 105 Above Raymonds Opp Medical College Koti: SHARMA Bpo SupportDocumento4 pagine1st Floor No 105 Above Raymonds Opp Medical College Koti: SHARMA Bpo SupportMK Musthafa GudalurNessuna valutazione finora
- Cardiac MarkersDocumento23 pagineCardiac Markerssulastri triNessuna valutazione finora
- BeraDocumento20 pagineBeraMuhamad SyaifulNessuna valutazione finora
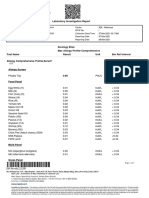
- Laboratory Investigation ReportDocumento7 pagineLaboratory Investigation ReportAmarjeetNessuna valutazione finora
- Head Nurse Experience (Staffing)Documento3 pagineHead Nurse Experience (Staffing)Abigail BrillantesNessuna valutazione finora
- Vascular DementiaDocumento8 pagineVascular Dementiaddelindaaa100% (1)
- Tetanus and Tetanus ToxoidDocumento24 pagineTetanus and Tetanus ToxoidFikar MajidNessuna valutazione finora
- Optic Nerve Glioma: Case Series With Review of Clinical, Radiologic, Molecular, and Histopathologic CharacteristicsDocumento5 pagineOptic Nerve Glioma: Case Series With Review of Clinical, Radiologic, Molecular, and Histopathologic CharacteristicsUtama Hadiputra SurbaktiNessuna valutazione finora
- How To Prepare For ExamDocumento4 pagineHow To Prepare For ExamJaspreet KaurNessuna valutazione finora
- Test Bank For Phlebotomy 4th Edition by Warekois DownloadDocumento9 pagineTest Bank For Phlebotomy 4th Edition by Warekois Downloadryanparker18011988fno100% (23)
- Rich Picture Blood BankDocumento3 pagineRich Picture Blood Bankviannyzerlinda50% (2)
- Management of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesDocumento7 pagineManagement of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesdaypranitaNessuna valutazione finora
- Muir's Textbook of Pathology 15e KulitDocumento35 pagineMuir's Textbook of Pathology 15e Kulitputri theresiaNessuna valutazione finora
- Daftar PustakaDocumento2 pagineDaftar PustakaErick PrasetyaNessuna valutazione finora
- The Cracked Mirror, Karen KernbergDocumento10 pagineThe Cracked Mirror, Karen Kernbergjuaromer100% (1)
- Female Sexual DysfunctionDocumento18 pagineFemale Sexual DysfunctionRisky SetiawanNessuna valutazione finora
- AAPM-TG53 (Quality Assurance For Clinical RTP)Documento57 pagineAAPM-TG53 (Quality Assurance For Clinical RTP)ΜΡ_Nessuna valutazione finora
- 5 - Formal ReportDocumento16 pagine5 - Formal ReportJacob MarczakNessuna valutazione finora