Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Imperforate Anus
Caricato da
Shafira Sepriana ShoburCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Imperforate Anus
Caricato da
Shafira Sepriana ShoburCopyright:
Formati disponibili
Imperforate Anus
Article Last Updated: Apr 19, 2007
emedicine
Background
Anorectal malformations include a wide spectrum of defects in the deelopment of the lowest portion of the intestinal and urogenital tracts!
"an# children with these malformations are said to hae an imperforate anus $ecause the# hae no opening where the anus should $e!
Although the term ma# accuratel# descri$e a child%s outward appearance, it often $elies the true comple&it# of the malformation $eneath!
'hen a malformation of the anus is present, the muscles and neres associated with the anus often hae a similar degree of malformation!
(he spine and urogenital tract ma# also $e inoled!
(he affected organs are located deep in the pelis and are not well isuali)ed through a$dominal incisions! (raditional surgical dictum did not
allow for diision of the posterior midline $ecause this diision of the muscle was $elieed to cause incontinence in the child! (herefore,
surgeons approached these malformations using a com$ined a$dominal, sacral, and perineal approach, with limited isi$ilit#! *uch approaches
hae put continence at greater risk than simpl# cutting sphincter muscles to ade+uatel# isuali)e the malformation! (his principle was
central to the deelopment of the surgical techni+ues currentl# used to repair these malformations!
,n 19-2, .e/a et al reported the results of the use of a posterior sagittal surgical repair approach! .e/a et al used the traditional approach
with a sacral incision and made the incisions progressiel# larger in an attempt to ade+uatel# isuali)e the anatom#! 0entuall#, the entire
posterior sagittal plane was opened, affording a full iew of the complete malformation! (his techni+ue, referred to as posterior sagittal
anorectoplast# 1.*A2.3 or posterior sagittal anorectoaginourethroplast# 1.*A24U.3, has led to a more complete understanding of the
anatom# of these children and of what is re+uired to repair the malformations with optimal results!
After the procedure, man# children still e&perience effects of their malformation in the form of urinar# or fecal incontinence! 5espite
optimal surgical management, no ade+uate repair for poorl# deeloped muscles or neres has $een deeloped! Bowel6management regimens
can proide an e&cellent +ualit# of life for these children when primar# continence is not achiea$le!
Pathophysiology
(he em$r#ogenesis of these malformations remains unclear! (he rectum and anus are $elieed to deelop from the dorsal potion of the
hindgut or cloacal cait# when lateral ingrowth of the mesench#me forms the urorectal septum in the midline! (his septum separates the
rectum and anal canal dorsall# from the $ladder and urethra! (he cloacal duct is a small communication $etween the 2 portions of the
hindgut! 5owngrowth of the urorectal septum is $elieed to close this duct $# 7 weeks% gestation! 5uring this time, the entral urogenital
portion ac+uires an e&ternal opening7 the dorsal anal mem$rane opens later! (he anus deelops $# a fusion of the anal tu$ercles and an
e&ternal inagination, known as the proctodeum, which deepens toward the rectum $ut is separated from it $# the anal mem$rane! (his
separating mem$rane should disintegrate at - weeks% gestation!
,nterference with anorectal structure deelopment at ar#ing stages leads to arious anomalies, ranging from anal stenosis, incomplete
rupture of the anal mem$rane, or anal agenesis to complete failure of the upper portion of the cloaca to descend and failure of the
proctodeum to inaginate! 8ontinued communication $etween the urogenital tract and rectal portions of the cloacal plate causes
rectourethral fistulas or rectoesti$ular fistulas!
(he e&ternal anal sphincter, deried from e&terior mesoderm, is usuall# present $ut has ar#ing degrees of formation, ranging from ro$ust
muscle 1perineal or esti$ular fistula3 to irtuall# no muscle 1comple& long9common6channel cloaca, prostatic or $ladder6neck fistula3!
Frequency
United States
Anorectal malformations occur in appro&imatel# 1 new$orn per :000 lie $irths!
Mortality/Morbidity
Anorectal and urogenital malformations are rarel# fatal, although some associated anomalies 1cardiac, renal3 can $e life threatening!
,ntestinal perforation or postoperatie septic complications in a new$orn with imperforate anus can result in mortalit# or seere mor$idit#!
"or$idit# generall# arises from the following 2 sources:
"alformation6related mor$idit#
o "alformation6related mor$idit# relates to associated malformations of rectal motilit#, anorectal inneration, and
sphincteric musculature! (he most common mor$idit# in this categor# is constipation! "ost children hae mild
malformations that commonl# result in constipation for reasons that remain unclear! ,f left untreated, chronic
constipation results in rectal dilation, which worsens the constipation! (his $ecomes a icious c#cle, which, if untreated,
results in fecal impaction and oerflow pseudoincontinence or encopresis!
o
o (he most seere forms of malformation6associated mor$idit# are fecal and urinar# incontinence! ;igher malformations,
such as long9common6channel cloacae and prostatic or $ladder6neck fistulas, are associated with more fre+uent spinal
malformations and poorer nere and muscle formation, all of which increase the likelihood of fecal or urinar#
incontinence! "alformations that directl# inole urinar# sphincteric mechanisms, and, specificall#, an# malformation in
which the rectum or agina <oins the urinar# tract at the $ladder neck, often results in either urinar# incontinence or
ina$ilit# to completel# oid!
*urger#6related mor$idit#
o (his can include standard complications such as line infections and pneumonia!
o
o 'ound infections or anastomotic $reakdowns can occur in an# intestinal surger#!
o
o 8hildren with imperforate anus are at greater risk for in<ur# to surrounding pelic organs $ecause these organs ma# also
$e inoled in the malformation in some unsuspected wa#!
o
o 5uring $lind e&ploration in the pelis, a dilated ureter can $e mistaken for the rectum! Urethras can $e opened or
transected, and prostates or seminal esicals can $e easil# in<ured! 5issection of these delicate structures can result in
ischemia and possi$le stricture or complete stenosis!
Race
=o known racial predilection has $een reported!
Sex
=o known se& predilection has $een reported!
Age
"ost children with an anorectal malformation are identified upon routine new$orn ph#sical e&amination! 5ela#ed presentation is often the
result of incomplete initial e&amination! =ew$orn anorectal and urogenital e&amination can $e technicall# challenging and makes man#
practitioners uncomforta$le!
*u$tle malformations, such as those in some children with perineal fistula that ma# look normal to the casual glance, ma# present
months or #ears after $irth when the child presents to a primar# care proider for constipation or urinar# tract infection and
appears to hae a small perineal $od# upon ph#sical e&amination!
Anorectal malformations in females with a normal6appearing anus who hae a$sent agina or persistent urogenital sinus ma# go
undiagnosed for #ears $ecause of e&aminer reluctance to separate the la$ia during ph#sical e&amination! (hese malformations can
$e discoered upon ealuation for urinar# tract infection or primar# amenorrhea!
istory
.renatal ultrasonograph# e&amination findings are often normal, although the pol#h#dramnios or intraa$dominal c#sts ma# suggest
imperforate anus with associated h#drocolpos or h#dronephrosis!
=ew$orns with imperforate anus are usuall# identified upon the first ph#sical e&amination! "alformations in new$orns that are missed upon
initial e&amination are often discoered within 2> hours when the new$orn is o$sered to hae distention and has failed to pass meconium
and a more thorough e&amination is performed!
Physical
5uring a thorough ph#sical e&amination, attention should $e focused on the a$domen, genitals, rectum, and lower spine!
(he um$ilicus should $e e&amined for the a$sence of an um$ilical arter# 126essel cord3, which ma# suggest an a$sent kidne#! (he
a$domen should $e palpated for masses, which ma# include a dilated kidne#, $ladder, h#drocolpos, ectopic kidne#, duplication, or
other c#stic structure!
,n males, the testicles must $e palpated in the scrotum! (he perineum is then e&amined! .erineal fistulas are diagnosed upon
discoer# of openings on the perineum, meconium or mucus in a small strip running up into the scrotal median raphe, a perineal
grooe, or a $ucket6handle malformation in the anal dimple skin! ,f no opening is present, urine is o$tained for stud#, and the child
is o$sered for 2> hours!
,n females, a perineal fistula can $e directl# identified as a small opening on the perineum! ,f none is present, the la$ia are
separated to search for a esti$ular fistula!
o A fourchette fistula is a t#pe of esti$ular fistula that straddles the spectrum of malformation $etween perineal and
esti$ular7 it is characteri)ed $# wet mucosa of the esti$ule anteriorl# and a dr# anoderm posteriorl# at the <unction of
the esti$ule and perineum 1see ,mage ?3!
o
o ,f no fistula is isi$le and onl# one opening $etween shortened la$ia is o$sered, the child has a cloaca!
o
o ,f the child has a normal urethra and no esti$ular fistula, she ma# hae imperforate anus without fistula!
o
o ,f she appears to hae trisom# 21, the likelihood increases that she does not hae a fistula!
o
o @irls with normal urethra and no isi$le fistula are o$sered for 2> hours to allow a perineal fistula to present $efore
operation is re+uired! (his waiting period is $eneficial in differentiating $etween children with perineal fistula who ma#
$e effectiel# treated using onl# a minimal anoplast# from those who re+uire colostom# with further ealuation using
distal colostograph#!
(he remainder of ph#sical e&amination is focused associated malformations!
o 8ardioascular malformations occur in 12622A of patients!
(he most common lesions are tetralog# of Ballot and entricular septal defects!
(ransposition of the great arteries and h#poplastic left heart s#ndrome hae $een reported $ut are rare!
o
o "an# @, malformations hae $een descri$ed in association with imperforate anus!
Up to 10A of patients hae tracheoesophageal a$normalities!
5uodenal o$struction due to annular pancreas or duodenal atresia occurs in a small percentage of patients!
"alrotation with Ladd $ands that causes o$struction has also $een descri$ed!
;irschsprung disease has $een well descri$ed in association with imperforate anus, although the incidence of
this com$ined condition is unknown!
8onstipation is common!
o
o (he association of imperforate anus and erte$ral anomalies has $een recogni)ed for man# #ears! .atients with high
lesions hae an increased risk of this association!
Lum$osacral anomalies predominate and occur in appro&imatel# one third of patients with imperforate anus!
(he fre+uenc# of spinal d#sraphism 1ealuated with ultrasonograph# or "2,3 increases with the seerit# of the
lesion 1ie, 17A in patients with low lesions, as high as >?A in patients with cloacal anomalies3! (he most common
t#pe of d#sraphism is tethered spinal cord, which is present in as man# as 2:A of patients! (he normal spinal
cord terminates $etween the first and second lum$ar erte$ral $odies! ,n patients with a tethered spinal cord,
the cord ends lower in the lum$ar spine! 8ord lipomas and s#ringoh#drom#elia are also common! All lum$osacral
spinal malformations negatiel# affect the child%s prognosis with respect to urinar# and fecal incontinence!
8urrarino descri$ed a triad of sacral defect, presacral mass, and imperforate anus! All patients with an
anorectal malformation must $e screened for these erte$ral a$normalities in the new$orn period using sacral
radiograph# and lum$osacral spinal ultrasonograph#!
o
o Up to one half of patients with anorectal malformations hae urologic a$normalities! Urinar# anomalies are more common
in patients with more comple& lesions!
,mproed imaging studies hae proided the a$ilit# to document an increased range of a$normalities! "ild
h#dronephrosis is the most common a$normal ultrasonograph# finding! 4esicoureteric reflu& is also a fre+uent
finding, followed $# renal agenesis and d#splasia!
8r#ptorchidism reportedl# occurs in C619A of males!
4aginal and uterine a$normalities are common! Bicornate uterus and uterus didelph#s occur in C:A of female
patients with imperforate anus! A aginal septum is the most common aginal a$normalit# and is seen in as man#
as one half of girls $orn with a cloacal malformation! 4aginal duplication and agenesis hae also $een reported!
4aginal agenesis ma# $e associated with ipsilateral a$sent oar# and kidne#!
!auses
Although the precise em$r#ologic defect that causes the spectrum of malformations descri$ed as imperforate anus has not $een
determined, cloacal mem$rane formation and su$se+uent $reakdown into urogenital and anal openings should occur $# - weeks% gestation!
5efects in the formation or shape of the posterior urorectal septum account for man# of the descri$ed a$normalities of imperforate anus!
"Dllerian ducts appear after this critical period7 how the# are incorporated into this deelopment is unclear!
=o clear risk factors predispose a person to hae a child with imperforate anus! ;oweer, a genetic linkage is sometimes present! "ost cases
of imperforate anus are sporadic without a famil# histor# of the condition, $ut some families hae seeral children with malformations!
@enetic studies are ongoing!
"ab Studies
8B8 count, $lood t#ping and screening, and serum electrol#te leels should $e measured in all children who re+uire operation!
Urinal#sis should $e performed to determine the presence of a rectourinar# fistula in all cases in which the diagnosis cannot $e
made $ased solel# on the ph#sical e&amination findings! ,f a child has a perineal fistula, esti$ular fistula, or a single perineal
orifice, urinal#sis is unnecessar#! Urinal#sis is re+uired in all other affected children!
Imaging Studies
*acral radiograph#: (wo iews of the sacrum, posteroanterior and lateral, should $e o$tained to measure sacral ratios and to look
for sacral defects, hemierte$rae, and presacral masses! (his should $e performed $efore surger#!
A$dominal ultrasonograph#: (his stud# is specificall# used to e&amine the genitourinar# tract and to look for an# other masses!
;#dronephrosis, h#drocolpos, presacral mass, a$dominal mass, or an# similar finding can profoundl# affect management! (his stud#
should $e performed $efore surger# and must $e repeated after 72 hours $ecause earl# ultrasonograph# findings ma# $e
insufficient to rule out h#dronephrosis due to esicoureteral reflu&!
*pinal ultrasonograph# or "2,: "an# children with anorectal malformations ma# hae a tethered spinal cord, which ma# affect
prognosis! (his lesion can $e diagnosed using ultrasonograph# prior to the ossification of the spine! Ultrasonograph# should $e
performed as earl# as possi$le $ut is not essential prior to a new$orn surgical procedure! B# age ? months, "2, is usuall#
necessar# $ecause the spine is no longer cartilaginous!
Lateral pelic radiograph# at 2> hours: 8hildren who could not $e diagnosed $ased solel# on ph#sical e&amination findings,
traditionall# underwent inertograph#, which consisted of holding the $a$# upside down and using lateral radiograph# to o$sere
the leel of gas in the distal rectum! A similar, $ut more humane, approach is to wait 2> hours after $irth to o$sere for possi$le
ma&imal pelic pouch distension and then to use cross6ta$le lateral pelic radiograph# with a radio6opa+ue marker on the anal
dimple with the child in the prone position and the hips slightl# raised! ,f the pouch is o$sered within 1 cm of the marker, some
surgeons offer primar# repair without colostom#! Bor pouches farther than 1 cm, colostom# is performed! (his 16cm guideline has
$een alidated onl# using radiographic measurements and is not directl# translata$le for measurements made using
ultrasonograph#! 8urrentl#, perineal ultrasonograph# has no role in diagnosis!
Augmented6pressure distal colostograph#: (his is the single most important diagnostic test used to clarif# the anatom# in all
children with malformations who re+uire colostom#! ,t is personall# performed $# the colorectal surgeon in man# centers! ,n a
fluoroscop# suite, a $alloon catheter is placed into the distal stoma, and the $alloon is inflated! (he catheter is pulled $ack, and
water6solu$le contrast is in<ected $# hand! (his pressure is re+uired to oercome the pressure of the leator muscles and to allow
the contrast to flow into the lowest part of the colon and reeal an# fistula! ,n patients with a fistula to the urinar# tract, the
$ladder often fills, and the stud# is continued to o$tain as much information as is proided with oiding c#stourethrograph#! ,f no
fistula is present, the distal pouch has a rounded appearance, and no urinar# e&traasation is isi$le!
4oiding c#stourethrograph# or micturating c#stourethrograph#: (hese studies are not necessar# if comprehensie distal
colostograph# is performed! (he# are not recommended for primar# ealuation of children with anorectal malformations $ecause
of poor sensitiit# compared with that of distal colostograph#!
"2,: All children with sacral defects should undergo spine ultrasonograph# to rule out associated malformations, such as
meningocele or meningom#elocele, teratoma, or mi&ed lesions! ,f ultrasonograph# finding are suggestie or nondiagnostic, "2,
should $e performed!
8( scanning: 8( scanning presentl# pla#s no role in the routine ealuation of children with anorectal malformations!
#ther $ests
Anorectal manometr#: Although this stud# has no role in the new$orn period, it ma# $e used in older children who suffer from
ar#ing degrees of incontinence! ;oweer, the findings are primaril# of academic interest!
Staging
,mperforate anus was historicall# classified $ased on the position of the distal6most aspect of the colon in relation to the leator ani
muscles! "alformations at or a$oe the leator muscle comple& were defined as high anomalies! ,nfraleator lesions were termed low and
were considered simpler and were associated with $etter prognosis! (his s#stem was $ased on the now o$solete 'ingspread classification!
,nformation o$tained from the posterior sagittal approach has led to an anatomic classification that lists malformations $ased on their
specific anatom#! (he following is a list of the most common malformations:
.erineal fistula
o (his malformation is associated with good prognosis, occurs in either se&, and inoles a closed anus with a small
connection opening on the perineal $od#!
o
o *ome $a$ies with this malformation hae a small loop of skin at the anal opening that resem$les a $ucket6handle! (his is
pathognomonic for perineal fistula!
o
o *ome $o#s ma# hae no isi$le perineal opening $ut ma# accumulate mucous or meconium in the fistula, which can e&tend
up the median raphe of the scrotum and resem$les a $lack cord 1meconium3 or a string of pearls 1mucous3!
o
o (his malformation is amena$le to primar# neonatal pull6through!
o
o ;ealth# girls who hae normal6si)ed anal openings and small6appearing perineal $odies do not hae perineal fistula! (his is
easil# determined $# measuring the si)e of the anus using ;egar dilators! (he anus of an aerage6term new$orn should $e
appro&imatel# 12 mm $ut aries with the si)e of the child! (he EcorrectE si)e of the perineum is largel# a matter of
e&perience!
4esti$ular fistula
o (his malformation is associated with good prognosis and is easil# diagnosed upon ph#sical e&amination $ased on the
appearance of a small opening at the posterior aspect of the esti$ule! (he opening is e&ternal to the h#men and is,
therefore, not aginal!
o
o (he term aginal fistula was commonl# and incorrectl# used to descri$e esti$ular fistula! (rue solitar# congenital
rectoaginal fistula is e&ceedingl# rare!
o
o 4esti$ular fistula is safel# treated with dierting colostom#, although some pediatric colorectal surgeons repair this
malformation primaril# in the new$orn period without using colostom#!
8loaca
o .ersistent cloaca is a malformation in females that encompasses a spectrum of defects, including the presence of a
common channel that incorporates the urethra, agina, and rectum!
o
o (he length of the common channel correlates with comple&it# and prognosis! *horter channels 1FC cm3 hae fewer
associated malformations and carr# a $etter prognosis! Longer channels hae more comple& malformations and poorer
prognosis!
o
o Gne half of all girls with this malformation hae 2 hemiaginas and man# hae h#drocolpos!
o
o (his malformation is easil# diagnosed upon ph#sical e&amination $ased on the presence of a solitar# perineal orifice!
Bemales with this malformation often hae er# small6appearing la$ia!
o
o All children with cloacae should undergo colostom# shortl# after $irth!
Bul$ar urethral fistula
o (his malformation o$sered in $o#s is relatiel# common!
o
o =o fistula is o$sered upon ph#sical e&amination, and urinal#sis often shows meconium!
o
o 8olostom# is essential to reliee o$struction, preent urinar# soiling, and to allow for distal colostograph#, which clarifies
the malformation for definitie surgical repair!
.rostatic urethral fistula
o (his malformation o$sered in $o#s is rarer than $ul$ar fistula and carries a poorer prognosis!
o
o (he diagnosis and treatment algorithm are identical to those of $ul$ar fistula, although the surgical procedures used
differ!
Bladder6neck fistula
o (his rare malformation o$sered in males 110A of all malformations in males3 carries a er# poor prognosis!
o
o "ost patients with $ladder6neck fistula re+uire $owel6management regimens!
o
o (he diagnosis and treatment algorithm are identical to those of $ul$ar and prostatic fistulas, although the surgical
procedures used differ!
o
o (his fistula is $est approached a$dominall#!
A$sent fistula
o (his malformation can occur in either se&, is somewhat rare, and is associated with a good prognosis! ,t is commonl#
associated with trisom# 21!
o
o 5iagnosis is primaril# $# e&clusion!
o
o Lateral pelic radiograph# is performed in $a$ies who hae no e&ternal eidence of fistula, who pass no meconium after
2> hours, and who hae no meconium in the urine!
o
o ,f the pelic rectal pouch is within 1 cm of the anal dimple, a primar# pull6through ma# $e performed! ,n these instances,
a fistula is unlikel# $ut should $e definitel# e&cluded using the proper surgical techni+ue!
o
o ,f the surgeon opts for colostom#, the a$sence of a fistula is confirmed using distal colostograph#!
8loacal e&stroph#
o (his e&tremel# rare malformation can occur in either se& $ut is most common in $o#s! ,t encompasses a spectrum that
includes ariant forms of coered e&stroph#! (he classic form is deastatingl# comple&!
o
o Affected children hae an omphalocele and a large e&trophied cloacal plate on their lower a$dominal wall! (he# hae 2
hemi$ladders separated $# an intestinal plate, often with prolapsed terminal ileum that proceeds distall# to include an
e&trophied urethral plate flanked $# 2 hemiphallic or hemiclitoral structures!
o
o All children with cloacal e&stroph# hae some degree of pu$ic s#mph#sis diastasis and ma# hae a spinal malformation,
most commonl# m#eloc#stocele!
o
o (hankfull#, this comple& malformation is rare $ut it has deastating implications on +ualit# of life!
Medical !are
=ew$orns with imperforate anus should not $e fed and should receie intraenous h#dration! Life6threatening comor$idities take
precedence and must $e treated first!
,f a urinar# fistula is suspected, $road6spectrum anti$iotics can $e administered, although anaero$ic coerage is unnecessar# within the
first >- hours of life! An# cardiac murmurs identified upon ph#sical e&amination should $e ealuated using echocardiograph# prior to surgical
interention! (he remainder of treatment includes diagnostics and surgical ealuation and management!
Surgical !are
(he decision6making process aims to determine which children should undergo primar# repair in the neonatal period and which children
re+uire colostom# and definitie repair in a staged fashion! 8hildren with anorectal malformations ma# undergo one or seeral of the
following surgical procedures $ased on the child%s presentation, ph#sical e&amination findings, and imaging stud# findings!
=eonatal colostom#
o A colostom# is performed in children who are not amena$le to primar# pull6through either $ecause of malformation
comple&it# 1an# urinar# fistula in $o#s, esti$ular fistula and cloaca in girls, no fistula in either se& H1 cm from perineal
skin3 or associated comor$idit#!
o
o (he colostom# is usuall# fashioned through a left lower +uadrant incision! (he colon is diided at the point where the
descending colon meets the sigmoid colon, and $oth ends are $rought to the a$dominal wall! B# fashioning the
colostom# at this location, the entire sigmoid colon is kept in place7 thus, when the pull6through is eentuall# performed, a
large portion of the colon is aaila$le for the surgeon to $ring down to the perineal skin!
o
o (he mucous fistula 1the downstream segment3 should $e er# small, flush with the skin, and far enough from the pro&imal
end to $e outside the colostom# appliance 1or under the flange3 to aoid continued urinar# soiling with feces!
o
o 5uring this operation, the distal segment of the colon must $e e&haustiel# irrigated to clean out the impacted meconium,
which is alwa#s significant! (his preents postdiersion urinar# sepsis and allows for effectie distal colostograph#!
.rimar# neonatal pull6through without colostom#
o "an# pediatric surgeons opt for primar# pull6through in children with perineal fistulas 1or no fistulas3 and close 1F1 cm3
rectal pouches on 2>6hour lateral pelic radiograph#! *ome pediatric surgeons who speciali)e in colorectal pro$lems often
offer the same procedure for girls with esti$ular fistulas!
o
o 8#stoscop# is usuall# performed to rule out associated malformation! (his is performed immediatel# prior to the pull6
through operation! A Bole# catheter is inserted following the c#stoscop#!
o
o (he preferred surgical approach is the posterior sagittal approach deeloped $# .e/a et al!
o
(he child is placed in the prone position with generous padding under the face and chest and a large $olster
under the hips to eleate the area of interest!
A muscle stimulator is used to show the precise position of the rectal muscle comple& to ena$le e&act diision
at the midline! (he midline for this operation is defined $# the line that precisel# diides the muscle comple& in
half!
5issection proceeds until the rectal pouch is identified! (he pouch is then mo$ili)ed until ade+uate length is
o$tained and the rectum is full# separated from its attachment to the genitourinar# tract! 0en if the
structures do not communicate, the# remain intimatel# associated until full# mo$ili)ed! (his step ensures that
the surgeon does not miss a fistula that was missed on urinal#sis findings!
Gnce the rectum has $een mo$ili)ed, the muscle stimulator is used to mark the anterior and posterior limits of
the muscle comple&! (he perineal $od# is then reconstructed, and the rectum is tacked down in the middle of
the muscle comple&! (he posterior wound is closed and anoplast# is performed!
.osterior sagittal pull6through with colostom#
o (his approach is used in $o#s with rectourinar# fistula 1$ul$ar, prostatic, or $ladder6neck fistula3, in girls with cloaca or
esti$ular fistula, and in patients of either se& who do not hae a fistula when the rectal pouch is further than 1 cm on
2>6hour lateral prone a$dominal radiograph#!
o
o (he approach is also used in children who ma# hae malformations that were amena$le to primar# neonatal pull6through
$ut were una$le to undergo such a procedure $ecause of e&treme prematurit# or other comor$idit#!
o
o 8olostom# is performed after 2> hours 1or immediatel# if one of the a$oe diagnoses is made $ased on either ph#sical
e&amination findings or meconium in the urine3!
o
o *eeral weeks following colostom#, distal colostograph# is performed, and the specifics of the malformation are
clarified!
o
o 8#stoscop# is usuall# performed to clarif# anatom# and to rule out associated malformation! (his is performed
immediatel# prior to the pull6through operation! A Bole# catheter is inserted following the c#stoscop#, e&cept in girls
with cloaca!
o
o (he reconstructie procedure aries $ased on the malformation, $ut the essential concepts include identif#ing and
separating the rectum from other structures, diiding and ligating an# fistulas, and full# reconstructing the pelic
anatom# with placement of the rectum within the confines of the muscle comple&! .rocedures for specific malformations
are as follows:
o
4esti$ular fistulas are directl# isi$le $ut hae the longest common wall $etween the rectum and agina and
re+uire significant delicate mo$ili)ation to aoid holes in either structure!
(he posterior sagittal approach is used in $o#s with $ul$ar or prostatic urethral fistulas! (he rectum is isolated
and opened, and the fistula is identified through progressie distal opening! Gnce the fistula is identified, the
rectum pro&imal to it ma# $e mo$ili)ed, and the fistula is then ligated! 2econstruction then proceeds with
primar# pull6through, as descri$ed a$oe!
A$dominal 1open or laparoscopic3 and posterior sagittal approaches are $est in $o#s with $ladder6neck fistulas
$ecause the fistula is $est identified in the a$domen!
8loaca procedures are comple&! A short9common6channel cloaca can $e repaired using total urogenital
mo$ili)ation! (he posterior sagittal wound is opened into the cloaca, which is then further pro&imall# opened
until the urethral orifice is identified and catheteri)ed! (he rectum is then sought! ,n girls with 2 hemiaginas
1:0A3, the rectum opens in the aginal septum, although significant as#metr# ma# $e present! After
identification, the rectum is separated from the urogenital tract and completel# mo$ili)ed! (he urogenital tract
is then mo$ili)ed as a solitar# structure until the urethral orifice reaches the perineum! (his is then
reconstructed, and the muscle is marked to ena$le creation of an ade+uate aginal opening and perineal $od#
without impinging on rectal space!
A long9common6channel cloaca repair often necessitates formal separation of the $ladder and agina, which
re+uires laparotom# and ureteral catheteri)ation! 4aginal replacement is sometimes necessar# if the aginal
length is insufficient for reconstruction!
8olostom# closure: Gnce the wound has completel# healed and postoperatie dilations hae achieed their goal 1ie, the neoanus is at
the desired si)e3, the colostom# ma# $e closed in traditional surgical fashion!
!onsultations
.ediatric surgeon: 0arl# consultation with a pediatric surgeon e&perienced with these anomalies is essential! ,ll6conceied
procedures during the new$orn period ma# hae lifelong conse+uences for the patient!
=eurosurgeon: 8onsultation with a neurosurgeon is warranted if a tethered spinal cord is present 12:A of all cases3!
Urologist: (he need for consultation with a urologist depends on the malformation and the indiidual pediatric surgeon!
%iet
After the o$struction is relieed using colostom#, primar# pull6through, or dilation, children do not re+uire special diet!
(he most common complication of imperforate anus repair is constipation or anal incontinence7 therefore, diet can $e a crucial part
of management! "an# patients ma# re+uire la&aties, enemas, or other medications or irrigations in addition to dietar#
manipulations! 8hildren should aoid constipating foods, such as those included in the $ananas, rice, applesauce, and toast 1B2A(3
diet! ;igh6fi$er and la&atie foods 1whole6grain foods and $reads, dair#, fruits, egeta$les, greas# foods, spic# foods3 should $e
encouraged! Unfortunatel#, dietar# manipulation is often of limited effectieness $ecause of the fuss# nature of most children
regarding diets! Bi$er supplements and la&aties can $e criticall# important in aoiding constipation, which can significantl# affect
prognosis!
Acti&ity
8hildren with anorectal malformations are often otherwise health#! Actiit# limitations are usuall# related onl# to the period around their
surgical procedures!
"an# children with anorectal malformations re+uire medications for arious reasons! Be#ond perioperatie medications, maintenance
medications often include urinar# anti$iotic proph#la&is or treatment andIor la&aties!
Urinar# proph#la&is is used to mitigate the risk of urinar# infection and urosepsis in children with risk factors for urinar# infection such as
urinar# fistula, esicoureteral reflu&, or continent diersion! 8ommon agents include oral amo&icillin, oral trimethoprimIsulfametho&a)ole,
and gentamicin $ladder irrigations! 8omprehensie information on all these medications and others is aaila$le in the e"edicine pediatric
topic Urinar# (ract ,nfection!
8ommon la&aties include senna products, milk of magnesia, and prop#lene gl#col solutions 1eg, "iraLa&, @l#coLa&3!
Further Inpatient !are
After initial colostom#, the child is a$le to eat and grow, and an# other associated malformations ma# $e addressed! "ost patients
are discharged once their ostom# has started to function and the# tolerate a regular diet!
Bollowing definitie repair, inpatient course is dictated $# the presence or a$sence of a colostom#!
o ,f a child has $een dierted with a colostom# prior to definitie repair and the repair is effectiel# completed using a
posterior sagittal incision without laparotom#, the postoperatie course is usuall# $rief! (he child ma# eat after the
anesthesia wears off and re+uires a short hospitali)ation with perioperatie anti$iotic administration!
o
o 8omplicated repairs that re+uire laparotom# also re+uire more length# postoperatie courses! (hese children usuall#
re+uire seeral da#s $efore intestinal function returns and a diet ma# $e resumed!
o
o 2epairs made without a colostom# ma# $e treated with a Emedical colostom#,E meaning the child is not fed 1ie, strict
nothing6$#6mouth J=.GK status3 and a central line is placed for total parenteral nutrition! After an ar$itrar# period
1commonl# :, 7, or 10 d, determined at the discretion of the surgeon in consideration of a host of factors3, a diet is
resumed and the total parenteral nutrition is stopped! (he central line is remoed, and the child ma# then $e discharged!
o
Bollowing ostom# closure, the child usuall# remains in the hospital for 26C da#s until intestinal function returns! 5iet is then
resumed, and the child ma# $e discharged!
Further #utpatient !are
8hildren with an anorectal malformation re+uire close follow6up for life! 8ontinuit# of care is essential in the growing #ears and
into adulthood, as the children deal with issues relating to continence and constipation!
Bollowing the initial colostom#, further inestigations in preparation for definitie operation, such as distal colostograph# or repeat
renal ultrasonograph#, are performed in an outpatient setting!
Bollowing definitie operation in either the neonatal period or after colostom#, follow6up is necessar# 2 weeks after surger#!
.arents are often instructed as to how to o$tain a set of ;egar dilators, which the# are to $ring to the first postoperatie isit!
At that isit, the surgeon measures the si)e of the anus and instructs the parents how to perform the dail# dilations! (hese
dilations continue until the anus has reached its goal si)e! At this time, the colostom# ma# $e closed if one was performed!
.atients with cloacal anomalies need speciali)ed follow6up care after pu$ert# to assess se&ual function and to correct
genitourinar# pro$lems!
o *ome girls who hae undergone surgical correction for cloaca hae incompletel# canali)ed fallopian tu$es and can deelop
painful c#stic collections of menstrual $lood following menarche! (his condition sometimes re+uires surgical interention!
A pediatric g#necologist can $e e&tremel# helpful for these girls and can suppress menstrual $lood production through
e&ogenous hormone administration until a clear treatment strateg# is esta$lished!
o
o Gnl# within the past 206C0 #ears hae significant num$ers of girls with cloaca undergone definitie repair! A few hae
$ecome pregnant! 'hile this is miraculous, the delier# process should include close inolement of the pediatric surgeon
who performed the original repair, if possi$le! ,f this is not possi$le, a surgeon e&perienced in cloaca repair should $e
consulted! 8aesarean delier# is the onl# safe wa# to aoid damage to tissues that originall# re+uired comple&
reconstruction!
o
*ome children present with prolapse during the toilet6training #ears! 0liminating constipation as a cause helps identif# children who
need surgical trimming of prolapsed mucosa!
4isits for constipation are fre+uent, and it is $est treated with a regular preentatie regimen that includes diet, fi$er, and
la&aties for as long as the# are needed! 5ietar# water does not influence stool +ualit# in a health# child!
In/#ut Patient Meds
2outine pain medications for surgical procedures are warranted! Acetaminophen 11: mgIkg eer# > h3 or morphine sulfate 10!0:60!1
mgIkg intraenousl# eer# 26> h3 usuall# suffices!
(he usual perioperatie anti$iotics include ampicillin 1:0 mgIkg eer# ? h3, gentamicin 12 mgIkg eer# -612 h3, and clindam#cin 110
mgIkg eer# - h3!
"an# la&aties hae $een used to control constipation in these patients! *enna comes in arious forms and can $e highl# effectie,
although dosage must $e indiiduali)ed! (he clinician must $e personall# engaged and must esta$lish an effectie dose response for
each patient on a case6$#6case $asis!
Balanced electrol#te solutions hae $een used for #ears as a $owel preparation for surgical procedures! (hese solutions hae onl#
recentl# $een made aaila$le in powdered form for mi&ing at home and for use as a la&atie 1under the name "iraLa& or @l#coLa&3!
(hese nonstimulant la&aties are er# palata$le to children $ecause the# dissole in an# $eerage with minimal impact on taste!
,n children who re+uire urinar# proph#la&is, standard medications include amo&icillin 1first6line medication in new$orns3,
nitrofurantoin, and trimethoprimIsulfametho&a)ole 1not used in $a$ies aged F2 mo3! (o ascertain a proph#la&is dose for one of
these anti$iotics, calculate a treatment dose $ased on the normal administration interal 12, C, or > times per da#3 and then
administer that same dose once per da#! Bor e&le, if the amo&icillin treatment dose is 206:0 mgIkgId diided eer# - hours
and a patient weighs 10 kg, the normal dose ma# $e C0 mgIkgId 1which falls within the recommended range3! Because the patient
weighs 10 kg, the dose is 100 mg eer# - hours! (he proph#la&is dose would then $e a once6dail# dose of 100 mg!
$ransfer
.roper consultation and surgical management are important! (ransferring these patients to a facilit# that proides pediatric
surgical care aids in proper classification, diagnosis, and management! Gptimal resources for the care of these children includes a
pediatric surgeon with e&perience in anorectal malformations, a pediatric urologist, a pediatric anesthesiologist, a critical care
specialist, and a neonatologist!
!omplications
.itfalls a$ound in the diagnosis and treatment of children with anorectal malformations! A logical approach and an e&perienced e#e
are essential for starting the child down the right path from the outset! 8omplications, while sometimes unaoida$le, can hae
deastating ramifications with respect to a child%s chances for urinar# and fecal continence!
(he following are a few of the most common issues encountered at pediatric colorectal centers:
o .rimar# repair without colostom#: 'hile certain malformations can $e primaril# repaired $# an e&perienced pediatric
surgeon in the neonatal period without the protection of colostom#, more comple& malformations should $# treated with
colostom# at the initial operation! .rimar# neonatal operations do not afford the surgeon the $enefit of distal
colostograph# to help clarif# anatom#! (his has resulted in deastating in<uries that could hae $een aoided with a
staged approach 1colostom#, followed $# definitie operation, followed $# colostom# closure3 with appropriate diagnostic
studies!
o
o 8olostom# t#pe and position: (he ideal colostom# position in children with an anorectal malformation is at the <unction of
the descending and sigmoid colon! (he colostom# should $e completel# diided, with the ends spaced far enough apart to
ensure that the mucous fistula is not located within the ostom# appliance! (his preents continued soiling of the urinar#
tract $# feces, which can result in urinar# infection! Loop colostomies are neer completel# dierting and put a child at
risk for urinar# sepsis! (ranserse colostomies seem to $e associated with a significant degree of mucous accumulation in
the long defunctionali)ed segment, resulting in chronic distension and d#smotilit# similar to that seen in children with
atresias! 5esire to perform laparoscopic pull6through should not $e a primar# factor in the decision to perform
colostom#!
o
o ,ntestinal perforation
(his complication can arise during an# phase of management!
,n children diagnosed with imperforate anus at $irth, 2> hours is allowed to pass prior to surgical treatment if
perineal fistula 1or other isi$le malformation, eg, esti$ular fistula or cloaca3 is not eident and urinal#sis
findings do not show meconium! (his allows the distal colon to distend a $it, and meconium occasionall# leaks out
on the perineum from a tin# perineal fistula! (his waiting period is adocated $# the most e&perienced surgeons
and should not increase the risk of perforation prior to repair or colostom#! Although e&ceedingl# rare, some
children hae perforated during this period!
.erforation has also occurred during anal dilations! 5ilations should alwa#s $e performed first $# the surgical
staff! 5ilation 1performed instead of anoplast#3 should $e performed onl# $# the surgical staff in e&tremel#
low $irthweight premature $a$ies! .arents ma# $e taught how to dilate larger $a$ies $ut must $e closel#
superised!
.erforation is minimi)ed $# appropriatel# positioning the colostom# while aoiding a transerse colostom#!
o
o Gperatie complications: 8orrection of malformations, een those that some surgeons ma# descri$e as minor, re+uires
significant e&perience, a keen e#e, and a sensitie hand! 5eastating complications 1eg, complete dehiscence,
postoperatie fistula, missed fistula, urologic in<ur#, ischemia3 can render a child who ma# hae $een continent after a
successful operation completel# incontinent! (hus, these children should $e directed to a su$specialist with a special
interest in this area at the earliest possi$le opportunit#!
o
o *tenosis: (his is a narrowing of the new anus! A tight ring of scar tissue forms instead of a soft and stretcha$le anus!
(his is a deastating complication and usuall# re+uires complete surgical repair! A regular schedule of slow progressie
dilation of the neoanus preents stenosis! 'eekl# dilations increase risk of stenosis! ,f the dilations are spaced too far
apart, the anus can narrow $etween the dilations! Large dilations prooke tears! (ears heal with scar tissue, which causes
stenosis!
o
o Undrained h#drocolpos
"an# $a$# girls $orn with cloaca hae a er# large mucous6filled agina! (his ma# appear as a giant c#stic
structure on prenatal ultrasonograph#! Ultrasonograph# should $e performed at $irth to look for such a c#stic
mass! ,f present, it must $e drained either from $elow 1through the cloaca3 or at the time of colostom# using a
aginostom# tu$e! ,f it is left undrained, complications ensue!
;#drocolpos can large enough to o$struct the ureters! *ome children with undrained h#drocolpos hae
undergone esicostom# and ureterostom#, when simple drainage of the h#drocolpos would hae sufficed!
;#drocolpos can also $ecome infected! ,f the agina perforates, it usuall# scars and $ecomes unusa$le, often
necessitating aginal replacement!
o
o 8onstipation
"an# children who hae undergone anorectal malformation repair deelop constipation! (his must $e preented
$# strong parental counseling and diligence to ensure the child clears the rectum dail#! 8onstipation on its own
is not a complication! (he complication is not preenting the constipation through close follow6up and parental
counseling!
Gnce constipation deelops, the distal colon can $ecome dilated, which e&acer$ates the constipation $ecause
the dilated $owel has poor motilit#! (he end result is termed encopresis! Becal impaction forms, and li+uid stool
leaks around it constantl#, leaing the child incontinent! (his can $e treated $ut is $est preented!
,ncontinence: "an# children who hae malformations associated with poor prognosis deelop fecal or urinar#
incontinence, een after a flawless operation without complication! 'hile Ethe plum$ingE ma# seem to $e a
relatiel# simple matter of rearranging some tu$es, continence is a comple& state that re+uires a delicate
$alance of neres, anorectal and colonic motilit#, and sphincter muscles! .arents should $e gien realistic
e&pectations and should $e made aware of all options, including $owel management or continent diersion and
intermittent catheteri)ation, should incontinence occur!
Prognosis
All patients who hae an anorectal malformation with no significant life6threatening comor$idit# should surie! (herefore,
prognosis is $est determined $ased on the pro$a$ilit# of primar# fecal continence!
8ontinence, defined as oluntar# $owel moements with minimal soiling, aries $ased on primar# and associated malformations! A
tethered spinal cord or another spinal malformation, such as hemierte$rae or spinal d#sraphism, ma# significantl# increase the
risk of incontinence!
*urgical complications worsen the chances for primar# continence, although this effect is difficult to +uantif#! 2eoperation
significantl# decreases the opportunit# for primaril# continence!
All children with a perineal fistula should $e continent! *pinal malformations are e&ceedingl# rare in this group!
Appro&imatel# 90A of girls with a esti$ular fistula hae oluntar# $owel moements 1.e/a, 199:3!
Appro&imatel# -0A of $o#s with a $ul$ar urethral fistula hae oluntar# $owel moements, whereas ??A of $o#s with prostatic
urethral fistula hae oluntar# $owel moements! Gnl# 1:A of $o#s with $ladder6neck fistulas hae oluntar# $owel moements
1.e/a, 199:3!
8hildren with imperforate anus without fistula hae a 7?A chance of haing oluntar# $owel moements 1.e/a, 199:3!
(he chance of fecal and urinar# continence in girls with cloaca aries $ased on the length of the common channel! @irls with a short
common channel and no associated urological or spinal malformations can hae e&cellent results, with as man# as 7:A of girls
deeloping oluntar# $owel moements! Urinar# or fecal continence is er# unlikel# in girls with long9common6channel cloacae, sacral
malformations, and a tethered spinal cord 1.e/a, 199:3!
(he $est determination for future continence is o$seration of function! A child who constantl# leaks stool or urine constantl# will
pro$a$l# not improe $# school age and ma# $enefit from earl# $owel management or intermittent catheteri)ation! ,f a child is
a$le to hold urine, stool, or $oth, the $est course is to o$sere his or her function!
2egardless of what the child will $e capa$le of in the future, cleanliness of urine and stool must $e esta$lished $efore a child
enters a school peer group! =o child should $e allowed to suffer the stigma of $eing the Esmell#E child simpl# $ecause their
ph#sician or parents were una$le to accept the child%s incontinence or $ecause the# were not #et read# to proceed! 0en in the
worst cases, hope remains! ;oweer, the decisions made must $e practical and must allow the child to seamlessl# fit in with their
peer groups!
Medical/"egal Pitfalls
.itfalls a$ound in the diagnosis and treatment of children with anorectal malformations! A logical approach and an e&perienced e#e
are essential for starting the child down the right path from the outset! 8omplications, while sometimes unaoida$le, can hae
deastating ramifications with respect to a child%s opportunit# for urinar# and fecal continence!
"edicolegal legal issues could logicall# stem from the following situations:
o *urgeons seem willing to perform the operations $ut appear less interested in dedicated long6term follow6up! 8hildren
with anorectal malformations and their parents re+uire significant close support from $oth a pediatrician and the
operatie surgeon!
o
o Gnl# e&perienced surgeons should perform these procedures! (hese malformations are rare, and the comple&
malformations are een rarer! ,f a surgeon with special e&pertise in this area is unaaila$le, patients are usuall# $est
sered $# receiing a dierting colostom# and transferring to a different center!
o
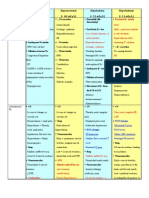
"edia file 1: %istal colostogram' posteroanterior &ie() $he initial phase of augmented*pressure distal colostography aims to
determine (here the colostomy (as placed in the colon and ho( much colon is a&ailable for pull*through' (ithout ta+ing do(n the
colostomy)
"edia file 2: %istal colostogram' lateral &ie() $his image sho(s the second phase of distal colostography' in (hich the patient is
placed in the lateral position) A radio*opaque mar+er is clearly &isible in the lo(er right side of the image' mar+ing the muscle
complex on the s+in) $his image sho(s that the rectal pouch ,oins the urinary tract at the le&el of the bulbar urethra' a relati&ely
common malformation in boys)
"edia file C: -uc+et*handle malformation) $he appearance of a band of s+in o&erlying the sphincteric muscle complex is a common
sign in a child born (ith imperforate anus and perineal fistula)
"edia file >: String*of*pearls malformation) $his image sho(s (hite mucoid material (ithin a perineal fistula) $he fistula frequently
extends anteriorly up the scrotum.s median raphe)
"edia file :: !loaca) $his is the classic appearance of a girl (ith a cloacal malformation (ith a single perineal orifice) $he genitals
appear quite short' (hich is a finding consistent (ith cloaca)
"edia file ?: Fourchette fistula) $his malformation is some(here half(ay bet(een perineal fistula and &estibular fistula) $he fistula
has a (et &estibular mucosal lining on its anterior half' but the posterior half is dry perineal s+in)
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Imaging of AdrenalsDocumento140 pagineImaging of AdrenalsSahana RNessuna valutazione finora
- Applied Equine Nutrition and TrainingDocumento232 pagineApplied Equine Nutrition and TrainingAndrea Villanueva50% (2)
- NCM 103 Fluids and Electrolytes 2019Documento257 pagineNCM 103 Fluids and Electrolytes 2019Jeth PadillaNessuna valutazione finora
- MCQ MicrobDocumento9 pagineMCQ Microbstationsectiontiga80% (5)
- AG Dairy Farm Project PlanDocumento11 pagineAG Dairy Farm Project Planvinay kumar0% (1)
- Meat Inspection GuidelineDocumento43 pagineMeat Inspection GuidelineABOHEMEED ALY0% (1)
- Acls MegacodeDocumento8 pagineAcls MegacodeRachel PerandoNessuna valutazione finora
- AEMV 2009 Conference Full ProceedingsDocumento66 pagineAEMV 2009 Conference Full Proceedingscristina_gomhNessuna valutazione finora
- Sesi 3-Promoting B'feeding During PregnancyDocumento64 pagineSesi 3-Promoting B'feeding During PregnancyMazlina MaidinNessuna valutazione finora
- Embryology - Notes To PGDocumento13 pagineEmbryology - Notes To PGskycall28Nessuna valutazione finora
- Crude Fat, Hexanes Extraction, in Feed, Cereal Grain, and Forage (Randall/Soxtec/Submersion Method) : Collaborative StudyDocumento10 pagineCrude Fat, Hexanes Extraction, in Feed, Cereal Grain, and Forage (Randall/Soxtec/Submersion Method) : Collaborative StudyIshtiaque IshtiNessuna valutazione finora
- Electrolyte ImbalancesDocumento4 pagineElectrolyte Imbalancessccctutor100% (2)
- Riddle of DeathDocumento2 pagineRiddle of DeathReka182Nessuna valutazione finora
- Biology Test Prep End of Course StudentDocumento11 pagineBiology Test Prep End of Course StudentdanielleamyaNessuna valutazione finora
- Soni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyDocumento1 paginaSoni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyVishalNessuna valutazione finora
- Handout Orthopedic Nursing Assisstive DevicesDocumento14 pagineHandout Orthopedic Nursing Assisstive DevicesPaul Christian P. Santos, RN100% (2)
- AP Module4 Trans DiazDocumento18 pagineAP Module4 Trans DiazJohn Rafael DiazNessuna valutazione finora
- Pediatric PneumoniaDocumento58 paginePediatric PneumoniaJohn Christopher LucesNessuna valutazione finora
- Treatment of Nutritional AnemiasDocumento12 pagineTreatment of Nutritional AnemiasPosan Samser LimbuNessuna valutazione finora
- Year 9 Term 2 Science Formative AssessmentDocumento2 pagineYear 9 Term 2 Science Formative AssessmentAditya N WardhanaNessuna valutazione finora
- Natural Selection Lab-Phet SimulationDocumento7 pagineNatural Selection Lab-Phet Simulationapi-319540611Nessuna valutazione finora
- Parts of Speech KIPS Academy (Free Download)Documento43 pagineParts of Speech KIPS Academy (Free Download)AyshahNessuna valutazione finora
- Test Bank For The Sociology of Health Illness and Health Care A Critical Approach 7th EditionDocumento35 pagineTest Bank For The Sociology of Health Illness and Health Care A Critical Approach 7th Editionpledgerzea.rus7as100% (34)
- The Chapeter That Is TissueDocumento36 pagineThe Chapeter That Is TissuereemNessuna valutazione finora
- Hydrocephalus KuliahDocumento19 pagineHydrocephalus KuliahamiraNessuna valutazione finora
- 02.1 Cell Theory WorksheetDocumento9 pagine02.1 Cell Theory WorksheetJoelle PoweNessuna valutazione finora
- Primary Carcinoid Tumor of The Urinary BladderDocumento5 paginePrimary Carcinoid Tumor of The Urinary BladdermikalraNessuna valutazione finora
- Form SPK Dan RKK Dokter Umum-1Documento4 pagineForm SPK Dan RKK Dokter Umum-1Vivin Mai diatyNessuna valutazione finora
- Introduction CASE STUDYDocumento3 pagineIntroduction CASE STUDYDavid CalaloNessuna valutazione finora