Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
057
Caricato da
Riot Riot Adja0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
11 visualizzazioni3 paginer
Titolo originale
19992_057
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentor
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
11 visualizzazioni3 pagine057
Caricato da
Riot Riot Adjar
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 3
57
Neurol J Southeast Asia 1999; 4 : 57 59
Address for correspondence: Prof C T Tan, Neurology Laboratory, University Hospital, 59100 Kuala Lumpur. Fax: 603-7557740, e-mail: tlip@pl.jaring.my
VIEWS AND REVIEWS VIEWS AND REVIEWS VIEWS AND REVIEWS VIEWS AND REVIEWS VIEWS AND REVIEWS
Devics disease and multiple sclerosis in Asia Devics disease and multiple sclerosis in Asia Devics disease and multiple sclerosis in Asia Devics disease and multiple sclerosis in Asia Devics disease and multiple sclerosis in Asia
Chong Tin TAN FRCP MD, Heng Thay CHONG MRCP
Division of Neurology, Department of Medicine, University of Malaya, Kuala Lumpur
Abstract
There has been a number of recent publications citing differences in clinical features, CSF, MRI and
pathology to support Devics disease as a distinct disease from multiple sclerosis. However, the
interpretation of the studies is complicated by the varied definitions. Many of the patients included
in these studies would be classified as optic-spinal recurrent form of multiple sclerosis in the Asian
literature. The evidences cited also suffer from circular nature of the argument. Data from the
Malaysian multiple sclerosis patients showed that features of severe spinal cord disease was seen
among classical Western multiple sclerosis patients as well as the optic-spinal recurrent form. It point
to a general preponderance for severe spinal cord involvement among Asians with multiple sclerosis,
rather than optic-spinal recurrent (or Devics disease) as a distinct disease from multiple sclerosis.
Key words: Devics disease, neuomyelitis optica, Asian multiple sclerosis
INTRODUCTION INTRODUCTION INTRODUCTION INTRODUCTION INTRODUCTION
There has been a number of recent publications
in Devics disease (neuromyelitis optica)
1-5
indicative of renewed interest in the disease.
The main focus of the publications was to show
that there were sufficient differences in the
pathology, MRI, CSF and clinical features of
Devics disease when compared to multiple
sclerosis for the former to be considered a distinct
disease. Devics disease has been known to be
more common among Asians.
6
With the recent
availability of disease modifying treatment in
multiple sclerosis, the discussions on Devics
disease are highly relevant to neurology practice
in Asia. The Consensus Report by the Asia
Pacific Multiple Sclerosis Consensus Group in
this issue of the Journal is thus an important
contribution.
7
Varied definitions of Devics disease Varied definitions of Devics disease Varied definitions of Devics disease Varied definitions of Devics disease Varied definitions of Devics disease
A recurring problem in the discussion of Devics
disease is the varied definitions used by different
authors.
8,9
The late Kuroiwa, a well-known
authority on multiple sclerosis in Asia defined
Devics disease as a monophasic illness with
acute bilateral optic neuritis and transverse
(severe) myelitis occurring successively within
a period of less than several weeks.
6
This is
close to the original understanding of Devics
disease.
8,9
In the recent studies by Mandler et al
1
and ORiodan et al
3
, although the requirement
of optic neuropathy and severe myelopathy was
retained, a multiphasic illness and long interval
between optic and spinal involvement were also
allowed. Another recent study by Wingerchuk
et al
4
defined Devics disease as involvement
confined to the optic nerve and spinal cord. A
multiphasic disease was allowed and myelopathy
need not be severe. Most of the recent Asian
publications on multiple sclerosis and Devics
disease adopted the definitions of Kuroiwa and
his colleagues. As such, many of the patients
from Mandler et al
1
, ORiodan et al
3
and
Wingerchuk et al
4
would be classified as optic-
spinal recurrence form of multiple sclerosis rather
than Devics disease in these Asian literature.
10,11
Interpretation and application of these recent
studies should thus be exercised with care.
Evidence supporting Devics disease as a Evidence supporting Devics disease as a Evidence supporting Devics disease as a Evidence supporting Devics disease as a Evidence supporting Devics disease as a
distinct entity distinct entity distinct entity distinct entity distinct entity
The evidence cited to support the view that
Devics disease is distinct from multiple sclerosis
were based on clinical, CSF, MRI and
pathological findings. Clinically, relapses in
Devics disease tended to be confined to the eye
and the spinal cord. The prognosis was worse
than the usual multiple sclerosis patients. The
CSF may show pleocytosis of >50 cells/mm
3
with fewer patients having oligoclonal bands.
There were fewer lesions in the MRI of the
brain. The lesions in the spinal MRI may extend
Neurol J Southeast Asia December 1999
58
over more than two vertebral segments. The
pathology in spinal cord showed more necrosis
and cavitation, with less involvement of other
parts of central nervous system.
1-5,9
A major drawback in using the above
evidences is the circular nature of its argument.
As patients with disease confined to the eye and
spinal cord were the initial inclusion criteria, it
is not surprising to find the patients to have
relapses confined to the eye and spinal cord and
less MRI brain lesions. Severe spinal cord
involvement as included in the selection criteria
would also by itself cause longer MRI spinal
lesions, more pleocytosis in CSF, worse
prognosis and more severe pathology.
Furthermore, none of the features mentioned
above is specific for Devics disease. They can
all be found in classical multiple sclerosis.
Multiple sclerosis in Malaysia Multiple sclerosis in Malaysia Multiple sclerosis in Malaysia Multiple sclerosis in Malaysia Multiple sclerosis in Malaysia
As mentioned above, many of the patients
labelled as Devics disease in the recent
publications with relapsing optic nerve and spinal
cord involvement would be classified as optic-
spinal recurrence form of multiple sclerosis in
many of the Asian studies. The optic-spinal
recurrence form of multiple sclerosis is more
commonly seen among Asians, accounting for
up to 63% of the clinically definite multiple
sclerosis patients.
11
In Asia where Devics disease
or optic-spinal form of multiple sclerosis is
commonly seen, does it occur as a distinct entity?
We have analysed our earlier series of multiple
sclerosis to answer this question.
12
The clinical
definite multiple sclerosis may be divided into
two groups, 20 patients with optic-spinal
recurrent form of multiple sclerosis (Devics
disease), and another 15 patients with
involvement beyond the optic nerve and spinal
cord (Western multiple sclerosis). As shown
in Table 1, there was no difference in the age of
onset, sex ratio, relapse rate, disease severity,
mortality, occurrence of acute transverse myelitis
and paroxysmal tonic spasm in the two groups.
Acute transverse myelitis and paroxysmal tonic
spasm are features said to be particularly common
among Asians with multiple sclerosis.
10,13
We
have earlier reported 10 other patients with
clinically probable multiple sclerosis manifesting
as relapsing myelopathy. The age of onset of
these 10 patients were 32 years. The annual
relapse rate was 0.45 with a F:M sex ratio of
2.3:1. Three of these 10 patients had paroxysmal
tonic spasm. All these features are similar to the
clinically definite multiple sclerosis thus
indicating that they are same disease.
13
Thus, our data do not support the concept of
two distinct diseases, Devics disease (or optic-
spinal recurrent multiple sclerosis) and classical
Western multiple sclerosis. Rather it is multiple
sclerosis among Asians as a single disease
characterised by frequent and severe spinal cord
involvement. Among the Asians with multiple
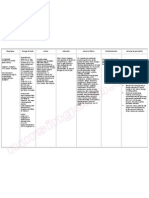
TABLE 1: TABLE 1: TABLE 1: TABLE 1: TABLE 1: Comparison between optic-spinal recurrent form of multiple sclerosis (Devics Comparison between optic-spinal recurrent form of multiple sclerosis (Devics Comparison between optic-spinal recurrent form of multiple sclerosis (Devics Comparison between optic-spinal recurrent form of multiple sclerosis (Devics Comparison between optic-spinal recurrent form of multiple sclerosis (Devics
disease) and Western multiple sclerosis in Malaysia disease) and Western multiple sclerosis in Malaysia disease) and Western multiple sclerosis in Malaysia disease) and Western multiple sclerosis in Malaysia disease) and Western multiple sclerosis in Malaysia
Devics disease Devics disease Devics disease Devics disease Devics disease Western multiple sclerosis Western multiple sclerosis Western multiple sclerosis Western multiple sclerosis Western multiple sclerosis P values P values P values P values P values
(n=20) (n=20) (n=20) (n=20) (n=20) (n=15) (n=15) (n=15) (n=15) (n=15)
Age at onset (years) 31.4 + 13.2 30.6 + 11.5 0.86
Race (Chinese) 85% 87% 0.83
Sex (female) 95% 80% 0.29
Relapse rate (per year) 0.97 1.2 0.36
Blindness (per eye) 33% 23% 0.57
Bedridden 30% 13% 0.42
Mortality 40% 20% 0.28
Acute transverse myelitis 50% 40% 0.81
Paroxysmal tonic spasm 35% 27% 1.0
Footnote on statistical analyses nonparametric variables were analysed using Mann-Whitney U statistics, Chi
square or Fisher exact tests. Parametric variables were analysed using ANOVA.
59
sclerosis, there is a group of patients whose
relapses is confined to the optic nerve and spinal
cord. There is another group with a more
disseminated involvement simulating classical
Western multiple sclerosis. However, even
within these patients, there is more severe spinal
cord involvement. There is a third group of
patients whose manifestation is confined to spinal
cord only. This is in addition to other
characteristics of Asian patients with multiple
sclerosis; lower prevalence, rare occurrence of
similar family history, higher female to male
sex ratio and lower occurrence of oligoclonal
band.
10,13
This is consistent with a large
comparative pathological studies on American
and Japanese multiple sclerosis patients, where
there were more Japanese patients with
simultaneous optic and spinal involvement, often
with necrotic and destructive lesions. However,
similar necrotic and destructive cases were also
seen among the patients from North America.
14
Kira et al
15
reported that the Western-type
multiple sclerosis among Japanese was
associated with HLA DRB1*1501 allele and
DRB 5*0101allele but not the Asian-type
multiple sclerosis. Yamasaki et al
16
found that
Japanese patients with optico-spinal multiple
sclerosis were more likely to have HLA
DPB1*0501. The difference in genetic make-up
such as HLA typing, may determine the target
organs in multiple sclerosis and the severity of
the inflammation.
REFERENCES REFERENCES REFERENCES REFERENCES REFERENCES
1. Mandler RN, Davis LE, Jeffrey DR and Kornfeld
M. Devics neuromyelitis optica: A clinicopatho-
logical study of 8 patients. Ann Neurol 1993;34:162-
8.
2. Fazekas F, Offenbacher H, Schmidt R. MRI of
neuromyelitis optica: evidence for a distinct entity.
J Neurol Neurosurg Psychiatry 1994;59:1140-2
3. ORiordan JI, Gallagher HL, Thompson AJ, Howard
RS, Kingsley DPE, Thompson EJ, McDonald WI.
and Miller DH. Clinical, CSF and MRI findings in
Devics neuromyelitis optica. J Neurol Neurosurg
Psychiatry 1996; 60:3827.
4. Wingerchuk DM, Hogancamp WF, OBrien PC
and Weinshenker BG. The clinical course of
neuromyelitis Optica (Devics Syndrome).
Neurology 1999;53:1107-14.
5. Filippi M., Rocca MA., Moiola L., Martinelli V.,
Ghezzi A., Capra R., Salvi F. and Comi G. MRI and
Magnetization transfer imaging changes in the brain
and cervical cord of patients with Devics
neuromyelitis optica. Neurology 1999:53:170510.
6. Kuroiwa Y. Neuromyelitis optica (Devics disease,
Devics syndrome). In: Koetsier JC (ed): Handbook
of Clinical Neurology Vol 3 (47): Demyelinating
diseases. Elsevier Science Publishers B.V. 1985:
397-408
7. Li PCK, Ong B, Lee KH, Prayoorwiwat N, Tan CT,
Tsai CP. Asia Pacific multiple sclerosis consensus.
Neurol J Southeast Asia 1999;4:89-90
8. Cloys DE, Netsky MG. Neuromyelitis optica. In:
Vinken PJ, Bruyn GW (eds) Handbook of Clinical
Neurology Vol 9: Multiple sclerosis and other
demyelinating diseases. North-Holland Publishing
Co. 1970:426-36
9. Pambakian A, Akdal G, Kennard C. Neuromyelitis
optica (Devics disease) and its relationship to MS.
The International MS Journal 2000; 6:91-5
10. Kuroiwa Y, Shibashaki H, Tabira T, Itoyama Y.
Clinical pictures of multiple sclerosis in Asia. In:
Kuroiwa Y, Kurland LT (eds): Multiple Sclerosis
East and West. Fukuoka, Japan, Kyushu University
Press. 1982:43-7.
11. Tan CT. Multiple sclerosis in Malaysia. Arch Neurol
1988;45:624-7.
12. Tan CT. Multiple sclerosis and other related diseases
in Malaysia: Their clinical manifestations and
laboratory findings. University of Malaya, 1990,
MD dissertation.
13. Tan CT. Multiple sclerosis in Malaysia. Neurol J
Southeast Asia 1997; 2:1-5
14. Ikuta F, Koga M, Takeda S, Ohama E, Takeshita I,
Ogawa H and Wang MY. Comparison of multiple
sclerosis pathology between 70 American and 75
Japanese autopsy Cases. In: Kuroiwa Y, Kurland
LT (eds): Multiple Sclerosis East and West.
Fukuoka, Japan, Kyushu University Press.
1982:297-305.
15. Kira J, Kanai T, Nishimura Y, Yamasaki K,
Matsushita S, Kawano Y, Hasuo K, Tobimatsu S
and Kobayashi T. Western versus Asian types of
multiple sclerosis: Immunogenetically and clinically
distinct disorders. Ann Neurol 1996;40:569-74.
16. Yamasaki K, Horiuchi I, Minohara M et al. HLA-
DPB *0501-associated opticospinal multiple
sclerosis: Clinical, neuroimaging and
immunogenetic studies. Brain 1999;122:1689-96
Potrebbero piacerti anche
- Print 1Documento38 paginePrint 1Riot Riot AdjaNessuna valutazione finora
- Sek UnderDocumento1 paginaSek UnderRiot Riot AdjaNessuna valutazione finora
- Print 4Documento331 paginePrint 4Riot Riot AdjaNessuna valutazione finora
- Print 2Documento29 paginePrint 2Riot Riot AdjaNessuna valutazione finora
- Print 3Documento27 paginePrint 3Riot Riot AdjaNessuna valutazione finora
- Artikel B InggrisDocumento1 paginaArtikel B InggrisRiot Riot AdjaNessuna valutazione finora
- Hemorrhagic Disease of The NewbornDocumento1 paginaHemorrhagic Disease of The NewbornRiot Riot AdjaNessuna valutazione finora
- 34Documento19 pagine34Riot Riot AdjaNessuna valutazione finora
- In CompletDocumento1 paginaIn CompletRiot Riot AdjaNessuna valutazione finora
- Jurnal Reading SarafDocumento7 pagineJurnal Reading SarafRiot Riot AdjaNessuna valutazione finora
- Comparing Radiological Features of Pulmonary Tuberculosis With and Without Hiv Infection 2155 6113.1000188Documento3 pagineComparing Radiological Features of Pulmonary Tuberculosis With and Without Hiv Infection 2155 6113.1000188Riot Riot AdjaNessuna valutazione finora
- A Long-Term Followup of 30 Neuropsychiatric-Tuberculosis Patients With The "Open-Negative" Syndrome of Indefinitely Prolonged ChemotherapyDocumento7 pagineA Long-Term Followup of 30 Neuropsychiatric-Tuberculosis Patients With The "Open-Negative" Syndrome of Indefinitely Prolonged ChemotherapyRiot Riot AdjaNessuna valutazione finora
- Imaging of Genitourinary TraumaDocumento8 pagineImaging of Genitourinary TraumaRiot Riot AdjaNessuna valutazione finora
- Update:: The Radiographic Features of Pulmonary TuberculosisDocumento10 pagineUpdate:: The Radiographic Features of Pulmonary TuberculosisRiot Riot AdjaNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- I R C U (Ircu) : V F U P W P S C R S ?Documento15 pagineI R C U (Ircu) : V F U P W P S C R S ?Riot Riot AdjaNessuna valutazione finora
- Radiologic Findings of PulmonaryDocumento6 pagineRadiologic Findings of PulmonaryRiot Riot AdjaNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Comparing Radiological Features of Pulmonary Tuberculosis With and Without Hiv Infection 2155 6113.1000188Documento3 pagineComparing Radiological Features of Pulmonary Tuberculosis With and Without Hiv Infection 2155 6113.1000188Riot Riot AdjaNessuna valutazione finora
- Dika Factor DiscreteDocumento2 pagineDika Factor DiscreteRiot Riot AdjaNessuna valutazione finora
- Was SalamDocumento1 paginaWas SalamRiot Riot AdjaNessuna valutazione finora
- Luka AaaaaDocumento1 paginaLuka AaaaaRiot Riot AdjaNessuna valutazione finora
- Soft TissueDocumento1 paginaSoft TissueRiot Riot AdjaNessuna valutazione finora
- Pro LapsDocumento1 paginaPro LapsRiot Riot AdjaNessuna valutazione finora
- Rafe RatDocumento1 paginaRafe RatRiot Riot AdjaNessuna valutazione finora
- Luka BkarDocumento1 paginaLuka BkarRiot Riot AdjaNessuna valutazione finora
- RESEARCH ARTICLE Open AccessDocumento14 pagineRESEARCH ARTICLE Open AccessRiot Riot AdjaNessuna valutazione finora
- Cover Laporan KimiaDocumento2 pagineCover Laporan KimiaRiot Riot AdjaNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Answer: 1Documento4 pagineAnswer: 1Jeffrey ViernesNessuna valutazione finora
- PsychopharmacologyDocumento30 paginePsychopharmacologyHilma Nadhifa100% (1)
- Auriculotherapy For Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocumento12 pagineAuriculotherapy For Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsSol Instituto TerapêuticoNessuna valutazione finora
- May3031 June 1-2-2017 Guidelines in The Practical Phase of The DentDocumento3 pagineMay3031 June 1-2-2017 Guidelines in The Practical Phase of The DentKarla MerxNessuna valutazione finora
- The Auburn Plainsman 12-3-1998Documento32 pagineThe Auburn Plainsman 12-3-1998The Auburn PlainsmanNessuna valutazione finora
- EcgDocumento18 pagineEcgDelyn Gamutan MillanNessuna valutazione finora
- 柳奇學姐提供的Mode of Mechanical VentilatorDocumento79 pagine柳奇學姐提供的Mode of Mechanical Ventilatorapi-25944730100% (10)
- HSV Keratitis Treatment Guideline HarvardDocumento69 pagineHSV Keratitis Treatment Guideline HarvardabciximabNessuna valutazione finora
- Medical Surgical Nursing 2nd Edition Osborn Test BankDocumento17 pagineMedical Surgical Nursing 2nd Edition Osborn Test BankdimyjebaNessuna valutazione finora
- Kugel PDFDocumento260 pagineKugel PDFUsman SanaNessuna valutazione finora
- Clonidine HydrochlorideDocumento1 paginaClonidine HydrochlorideLovelyn Joy Abubo CortezNessuna valutazione finora
- Strickland PresentationDocumento1 paginaStrickland Presentationmariopi2495Nessuna valutazione finora
- Hearing LossDocumento9 pagineHearing Lossvicky singhNessuna valutazione finora
- Excess Fluid Volume PPT (Case Press)Documento10 pagineExcess Fluid Volume PPT (Case Press)Perrilyn PereyNessuna valutazione finora
- Acute Respiratory Distress Syndrome (ARDS)Documento3 pagineAcute Respiratory Distress Syndrome (ARDS)akish4uNessuna valutazione finora
- SE 300 OperatorsDocumento95 pagineSE 300 OperatorsCukup StsajaNessuna valutazione finora
- Gluten-Casein Peptides TestDocumento2 pagineGluten-Casein Peptides TestjmkcbeNessuna valutazione finora
- Raquiestenosis. Scielo PDFDocumento8 pagineRaquiestenosis. Scielo PDFKaren Torres PantojaNessuna valutazione finora
- Oral Manifestations of Connective Tissue Disease (CTDDocumento34 pagineOral Manifestations of Connective Tissue Disease (CTDFatin Nabihah Jamil67% (3)
- Case Study of A Boy With HaemophiliaDocumento18 pagineCase Study of A Boy With HaemophiliaImanuel Far-FarNessuna valutazione finora
- KCC Emergency High Angle DrillDocumento18 pagineKCC Emergency High Angle DrillSandy M. MaddaganNessuna valutazione finora
- Medical Vocabulary - HOSPITALDocumento4 pagineMedical Vocabulary - HOSPITALBianca AndreeaNessuna valutazione finora
- Nonoperative Proximal Humeus FractureDocumento20 pagineNonoperative Proximal Humeus FractureLuka DamjanovicNessuna valutazione finora
- Essentials of Physiotherapy After Thoracic Surgery - What Physiotherapists Need To Know. A Narrative ReviewDocumento15 pagineEssentials of Physiotherapy After Thoracic Surgery - What Physiotherapists Need To Know. A Narrative ReviewMariana MadridNessuna valutazione finora
- Biology 2 JournalDocumento5 pagineBiology 2 JournalKadymars JaboneroNessuna valutazione finora
- Listening Sample Test 2 Audio ScriptDocumento12 pagineListening Sample Test 2 Audio ScriptCCCAXANessuna valutazione finora
- Issues Around Vaginal Vault Closure: ReviewDocumento6 pagineIssues Around Vaginal Vault Closure: ReviewKeeranmayeeishraNessuna valutazione finora
- Glucosamine SulfateDocumento9 pagineGlucosamine Sulfateriga_ayuNessuna valutazione finora
- Bedside ClinicDocumento6 pagineBedside Clinicyer tagalajNessuna valutazione finora
- Cellular AberrationDocumento2 pagineCellular AberrationFrances Gaviola100% (1)