Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
P6030 SysThink1 Plesk2001 Required
Caricato da
char21830 valutazioniIl 0% ha trovato utile questo documento (0 voti)
15 visualizzazioni4 paginehealth systems
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentohealth systems
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
15 visualizzazioni4 pagineP6030 SysThink1 Plesk2001 Required
Caricato da
char2183health systems
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 4
Complexity science
The challenge of complexity in health care
Paul E Plsek, Trisha Greenhalgh
Across all disciplines, at all levels, and throughout the
world, health care is becoming more complex. Just 30
years ago the typical general practitioner in the United
Kingdom practised from privately owned premises
with a minimum of support staff, subscribed to a single
journal, phoned up a specialist whenever he or she
needed advice, and did around an hours paperwork
per week. The specialist worked in a hospital, focused
explicitly on a particular system of the body, was undis-
puted leader of his or her firm, and generally left
administration to the administrators. These individuals
often worked long hours, but most of their problems
could be described in biomedical terms and tackled
using the knowledge and skills they had acquired at
medical school.
You used to go to the doctor when you felt ill, to
find out what was wrong with you and get some medi-
cine that would make you better. These days you are as
likely to be there because the doctor (or the nurse, the
care coordinator, or even the computer) has sent for
you. Your treatment will now be dictated by the
evidencebut this may well be imprecise, equivocal, or
conflicting. Your declared values and preferences may
be used, formally or informally, in a shared
management decision about your illness. The solution
to your problemis unlikely to come in a bottle and may
well involve a multidisciplinary team.
Not so long ago public health was the science of
controlling infectious diseases by identifying the
cause (an alien organism) and taking steps to remove
or contain it. Todays epidemics have fuzzier bounda-
ries (one is even known as syndrome X
1
): they are the
result of the interplay of genetic predisposition,
environmental context, and lifestyle choices.
The experience of escalating complexity on a prac-
tical and personal level can lead to frustration and dis-
illusionment. This may be because there is genuine
cause for alarm, but it may simply be that traditional
ways of getting our heads round the problem are no
longer appropriate. Newtons clockwork universe, in
which big problems can be broken down into smaller
ones, analysed, and solved by rational deduction, has
strongly influenced both the practice of medicine and
the leadership of organisations. For example, images
such as the heart as a pump frame medical thinking,
and conventional management thinking assumes that
work and organisations can be thoroughly planned,
broken down into units, and optimised.
2
But the machine metaphor lets us down badly
when no part of the equation is constant, independent,
or predictable. The new science of complex adaptive
systems may provide new metaphors that can help us
to deal with these issues better.
3
In this series of articles
we shall explore new approaches to issues in clinical
practice, organisational leadership, and education. In
this introductory article, we lay out some basic
principles for understanding complex systems.
Complex adaptive systems: some basic
concepts
Definitions and examples
A complex adaptive system is a collection of individual
agents with freedom to act in ways that are not always
totally predictable, and whose actions are intercon-
nected so that one agents actions changes the context
for other agents. Examples include the immune
system,
4
a colony of termites,
5
the financial market,
6
and just about any collection of humans (for example,
a family, a committee, or a primary healthcare team).
Fuzzy, rather than rigid, boundaries
In mechanical systems boundaries are fixed and well
defined; for example, knowing what is and is not a part
of a car is no problem. Complex systems typically have
fuzzy boundaries. Membership can change, and agents
can simultaneously be members of several systems.
This can complicate problem solving and lead to unex-
pected actions in response to change. For example, Dr
Simon (box) cannot understand why staff are so resist-
ant to a small extension of surgery opening hours. Per-
haps it is the fact that the apparently simple adjustment
to working arrangements will play havoc with their
own lunchtime inivolvlements with other social
systemsbe these meeting a child from school, attend-
ing a meeting or study class, or making contact with
others who themselves have fixed lunch hours.
Agents actions are based on internalised rules
In a complex adaptive system, agents respond to their
environment by using internalised rule sets that drive
action. In a biochemical system, the rules are a series
of chemical reactions. At a human level, the rules can
be expressed as instincts, constructs, and mental mod-
Summary points
The science of complex adaptive systems provides
important concepts and tools for responding to
the challenges of health care in the 21st century
Clinical practice, organisation, information
management, research, education, and
professional development are interdependent and
built around multiple self adjusting and
interacting systems
In complex systems, unpredictability and paradox
are ever present, and some things will remain
unknowable
New conceptual frameworks that incorporate a
dynamic, emergent, creative, and intuitive view of
the world must replace traditional reduce and
resolve approaches to clinical care and service
organisation
Education and debate
This is the first
in a series of
four articles
Paul E Plsek &
Associates Inc, 1005
Allenbrook Lane,
Roswell, GA 30075,
USA
Paul Plsek
director
University College
London, London
N19 3UA
Trisha Greenhalgh
professor of primary
health care
Correspondence to:
P E Plsek
paulplsek@
directedcreativity.com
Series editors:
Trisha Greenhalgh
and Paul Plsek
BMJ 2001;323:6258
625 BMJ VOLUME 323 15 SEPTEMBER 2001 bmj.com
els. Explore the patients ideas, concerns, and expecta-
tions is an example of an internalised rule that might
drive a doctors actions.
These internal rules need not be shared, explicit, or
even logical when viewed by another agent.
7
For exam-
ple, another doctor might act according to the
internalised rule Patients come to the doctor for a sci-
entific diagnosis. In the example in the box Dr Simons
partners and staff probably do not share her implicit
behaviour ruleTry to accommodate patients desire
to be seen outside standard surgery hours.
The mental models and rules within which
independent agents operate are not fixed. The fourth
article in this serieson complexity and education
will explore this point in more detail.
8
The agents and the system are adaptive
Because the agents within it can change, a complex sys-
temcan adapt its behaviour over time.
9
At a biochemical
level, adaptive micro-organisms frequently develop anti-
biotic resistance. At the level of human behaviour, Mr
Henderson (see box) seems to have learnt that the
surgery is somewhere he can come for a friendly chat. As
this example illustrates, adaptation within the systemcan
be for better or for worse, depending on whose point of
view is being considered.
Systems are embedded within other systems and
co-evolve
The evolution of one system influences and is
influenced by that of other systems.
10
Dr Simon and Mr
Henderson have together evolved a system of
behaviour; they have both contributed to the pattern of
frequent visits we now observe. The health centre is
also embedded within a locality and the wider society,
and these also play a part in Mr Hendersons
behaviour. A subsequent article in this series will
explore how medical care for people with diabetes is
embedded in wider social and other systems.
11
Our
efforts to improve the formal system of medical care
can be aided or thwarted by these other more informal
shadow systems.
12
Since each agent and each system
is nested within other systems, all evolving together
and interacting, we cannot fully understand any of the
agents or systems without reference to the others.
Tension and paradox are natural phenomena, not
necessarily to be resolved
The fact that complex systems interact with other com-
plex systems leads to tension and paradox that can
never be fully resolved. In complex social systems, the
seemingly opposing forces of competition and
cooperation often work together in positive ways
fierce competition within an industry can improve the
collective performance of all participants.
13
Many will sympathise with Dr Simons uneasiness
about evidence based medicine. There is an insoluble
paradox between the need for consistent and evidence
based standards of care and the unique predicament,
context, priorities, and choices of the individual
patient. Whereas conventional reductionist scientific
thinking assumes that we shall eventually figure it all
out and resolve all the unresolved issues, complexity
theory is comfortable with and even values such inher-
ent tension between different parts of the system.
Interaction leads to continually emerging, novel
behaviour
The behaviour of a complex system emerges from the
interaction among the agents. The observable out-
comes are more than merely the sum of the partsthe
properties of hydrogen and oxygen atoms cannot be
simply combined to account for the noise or shimmer
of a babbling brook.
14
The next article in this series
considers the application of complexity thinking in
healthcare organisations; it will describe how the
productive interaction of individuals can lead to novel
approaches to issues.
15
The inability to account for sur-
prise, creativity, and emergent phenomena is the major
shortcoming of reductionist thinking.
Inherent non-linearity
The behaviour of a complex system is often non-linear.
For example, in weather forecasting the fundamental
laws governing gases contain non-linear terms that
lead to what complexity scientists have called sensitive
dependence on initial conditions, such that a small
difference in the initial variables leads to huge
differences in outcomes.
16
This property of non-linearity appears in all
complex systems. Dr Simon, for example, was
surprised by the uproar over her suggestion of a seem-
ingly small changeto remain open an additional 30
minutes during the lunch hour.
Inherent unpredictability
Because the elements are changeable, the relationships
non-linear, and the behaviour emergent and sensitive
to small changes, the detailed behaviour of any
Complexity in the life of an ordinary GP
Dr Fiona Simon is a part time partner in a large health
centre and the clinical governance lead for her
primary care trust. After a busy morning surgery she
goes on to chair a multidisciplinary educational
meeting on a local initiative to establish local asthma
guidelines at which an academic expert gives a talk on
evidence. She emerges from the meeting somewhat
irritated that the world presented by the academic is so
black and white. She was surprised to hear herself
described by a colleague as an opinion leader and
advocate of evidence based medicine. In fact, she
reflects, she found herself agreeing with a group of
nurses in the audience, who protested that patients
very rarely fit the textbook case or the evidence based
medicine guidelines.
Later, during an overbooked afternoon surgery, she
sees Mr Henderson, a 71 year old widower who has
diabetes and little in the way of social support. He has
no new physical problems and Dr Simon notes that
the patient was told last time to see her in six months
timebut once again he has returned after less than
two weeks. She gives him five minutes and writes Gen.
chat in his record.
In the evening, there is a practice staff meeting to
discuss a proposal that the surgery should stay open an
additional 30 minutes over lunch to accommodate
patients who can only leave work in their lunch breaks.
Dr Simon has sent round a memo suggesting that a
different duty team of doctor, nurse, and receptionist
could run the service each day. The meeting was
scheduled to last 20 minutes but goes on for over an
hour, and the issue is not resolved; two of the five
partners are vehemently opposed and did not even stay
for the meeting. Opening over lunch worked fine in my
brothers practice, thinks Dr Simon on her way home.
Why the furore among the staff and my partners?
Education and debate
626 BMJ VOLUME 323 15 SEPTEMBER 2001 bmj.com
complex system is fundamentally unpredictable over
time.
16
Ultimately, the only way to know exactly what a
complex system will do is to observe it: it is not a ques-
tion of better understanding of the agents, of better
models, or of more analysis.
Inherent pattern
Despite the lack of detailed predictability, it is often
possible to make generally true and practically useful
statements about the behaviour of a complex system.
There is often an overall pattern.
17
For example, Mr
Henderson will turn up periodically in Dr Simons sur-
gery until something is done to alter his behaviour. We
cannot predict the exact timing of his appointments or
his chief complaintnor is this detailed information
necessary to deal with the problem.
Attractor behaviour
Complexity science notes a specific type of pattern
called an attractor. Attractor patterns provide com-
paratively simple understanding of what at first seems
to be extremely complex behaviour. For example, in
psychotherapy, clients are more likely to accept a
counsellors advice when it is framed in ways that
enhance their core sense of autonomy, integrity, and
ideals.
18
These are underlying attractors within the
complex and ever changing system of a persons
detailed behaviour. Relatively simple attractor patterns
have been shown in share prices in a financial market,
6
biological systems (such as beat to beat variation in
heart rate
19
), human behaviour (such as Mr Hender-
sons frequent consulting), and social systems (such as
nurses staffing patterns on a hospital ward
20
).
Doctors behaviour is notoriously difficult to
influence, but, as we shall illustrate in the article on
organisational applications in this series,
21
attractor
metaphors can be used to identify potentially fruitful
areas for work.
Inherent self organisation through simple locally
applied rules
Order, innovation, and progress can emerge naturally
from the interactions within a complex system; they do
not need to be imposed centrally or from outside. For
example, termite colonies construct the highest
structures on the planet relative to the size of the build-
ers.
5
Yet there is no chief executive termite, no architect
termite, and no blueprint. Each individual termite acts
locally, seemingly following only a few simple shared
rules of behaviour, within a context of other termites
also acting locally. The termite mound emerges from a
process of self organisation.
In everyday life many complex behaviours emerge
from relatively simple rules in such things as driving in
traffic or interacting in meetings. While no one directs
our detailed actions in such situations, we all know how
to behave adaptively and end up getting to where we
want to go. We shall explore this concept further in the
forthcoming article on management and leadership in
healthcare organisations.
21
The zone of complexity
Langton has termed the set of circumstances that call
for adaptive behaviours the edge of chaos.
22
This
zone (the middle area in the figure) has insufficient
agreement and certainty to make the choice of the next
step obvious (as it is in simple linear systems), but not
so much disagreement and uncertainty that the system
is thrown into chaos (figure).
23
The development and
application of clinical guidelines, the care of a patient
with multiple clinical and social needs, and the coordi-
nation of educational and development initiatives
throughout a practice or department are all issues that
lie in the zone of complexity.
Our learnt instinct with such issues, based on
reductionist thinking, is to troubleshoot and fix
thingsin essence to break down the ambiguity,
resolve any paradox, achieve more certainty and
agreement, and move into the simple system zone. But
complexity science suggests that it is often better to try
multiple approaches and let direction arise by
gradually shifting time and attention towards those
things that seem to be working best.
24
Schns reflective
practitioner,
25
Kolbs experiential learning model,
26
and
the plan-do-study-act cycle of quality improvement
27
are examples of activities that explore new possibilities
through experimentation, autonomy, and working at
the edge of knowledge and experience.
Not all problems lie in the zone of complexity.
Where there is a high level of certainty about what is
required and agreement among agents (for example,
the actions of a surgical theatre team in a routine
operation) it is appropriate for individuals to think in
somewhat mechanistic terms and to fall into their pre-
agreed role. In such situations the individuals I
I
A
N
E
P
A
Y
N
E
Degree of certainty
D
e
g
r
e
e
o
f
a
g
r
e
e
m
e
n
t
High Low
High
Low
C
o
m
p
le
x
Simple
Chaotic
The certainty-agreement diagram (based on Stacey
23
)
Education and debate
627 BMJ VOLUME 323 15 SEPTEMBER 2001 bmj.com
relinquish some autonomy in order to accomplish a
common and undisputed goal; the system displays less
emergent behaviour but the job gets done efficiently.
Few situations in modern health care, however, have
such a high degree of certainty and agreement, and
rigid protocols are often rightly abandoned.
Conclusion
This introductory article has acknowledged the
complex nature of health care in the 21st century, and
emphasised the limitations of reductionist thinking
and the clockwork universe metaphor for solving
clinical and organisational problems. To cope with
escalating complexity in health care we must abandon
linear models, accept unpredictability, respect (and uti-
lise) autonomy and creativity, and respond flexibly to
emerging patterns and opportunities.
Competing interests: None declared.
1 Hansen BC. The metabolic syndrome X. Ann N Y Acad Sci 1999;892:1-24.
2 Morgan G. Images of organization. 2nd ed. Thousand Oaks, CA: Sage,
1997.
3 Waldrop MW. Complexity: the emerging science at the edge of order and chaos.
New York: Simon and Schuster, 1992.
4 Varela F, Coutinho A. Second generation immune networks. Immunol
Today 1991;12(5):159-66.
5 Wilson EO. The insect societies. Cambridge, MA: Harvard University Press,
1971.
6 Mandelbrot B. A fractal walk on Wall Street. Sci Am 1999;280(2)70-3.
7 Stich SP. Rationality. In: Osherson DN, Smith EE, eds. An invitation to cog-
nitive science: thinking. Vol 3. Cambridge, MA: MIT Press, 1990.
8 Fraser S, Greenhalgh T. Coping with complexity: educating for capability.
BMJ (in press).
9 Holland JH. Hidden order: how adaptation builds complexity. Reading, MA:
Addison-Wesley, 1995.
10 Hurst D, Zimmerman BJ. From life cycle to ecocycle: a new perspective
on the growth, maturity, destruction, and renewal of complex systems. J
Manage Inquiry 1994:3;339-54.
11 Wilson T, Holt T, Greenhalgh T. Complexity and clinical care. BMJ (in
press).
12 Stacey RD. Strategic management and organizational dynamics. London:
Pitman Publishing, 1996.
13 Axelrod RM. The complexity of cooperation. Princeton: Princeton University
Press, 1997.
14 Gell-Mann M. The quark and the jaguar: adventures in the simple and complex.
New York: Freeman, 1995.
15 Plsek PE, Wilson T. Complexity, leadership, and management in
healthcare organisations. BMJ (in press).
16 Lorenz E. The essence of chaos. Seattle: University of Washington Press,
1993.
17 Briggs J. Fractals: the patterns of chaos. New York: Simon & Schuster, 1992.
18 Schafer R. A new language for psychoanalysis. New Haven, CT: Yale Univer-
sity Press, 1976.
19 Goldberger AL. Nonlinear dynamics for clinicians: chaos theory, fractals,
and complexity at the bedside. Lancet 1996;347:1312-4.
20 Sharp LF, Piesmeyer HR. Chaos theory: a primer for health care. Quality
management in healthcare 1995;3(4):71-86.
21 Plsek P, Wilson T. Complexity, leadership, and management in healthcare
organisations. BMJ (in press).
22 Langton CG. Artificial life. Proceedings of the Santa Fe Institute. Studies in the
sciences of complexity. Vol 6. Redwood City, CA: Addison-Wesley, 1989.
23 Stacey RD. Strategic management and organizational dynamics. London: Pit-
mann Publishing, 1996.
24 Zimmerman BJ, Lindberg C, Plsek PE. Edgeware: complexity resources for
healthcare leaders. Irving, TX: VHA Publishing, 1998.
25 Schon, DA. The reflective practitioner. New York: Basic Books, 1983.
26 Kolb DA. Experiential learning. Experience as the source of learning and devel-
opment. Englewood Cliffs, NJ: Prentice Hall, 1984.
27 Berwick DM. Developing and testing changes in delivery of care. Ann
Intern Med 1998;128:651-6.
A patient who changed my practice
Fifteen years before looking at job
When we recently looked at a survey on chronic
uraemia that included patients for whom there was no
occupational history, we felt that not enough attention
was paid to this factor. We went back to the story of a
38 year old man who was admitted to our hospital in
September 1976 complaining of severe abdominal
pain. His clinical history was unremarkable up to 1961,
when he first experienced abdominal pain and was
admitted to another hospital. As laboratory tests
showed no abnormalities and his clinical picture
spontaneously improved, he was discharged, but he
relapsed with colic-like severe abdominal pain and
hypertension, and he was admitted to the same
hospital once a year for the next 15 years. Diagnostic
hypotheses were pancreatitis, liver disease, diverticulitis,
and pancreatic cancer, without any confirmation.
On his admission to our hospital, a suspicion of
plumbism was formed. Body lead burden on EDTA
mobilisation tests was 1650 g (normal value 150 g,
toxic levels >1000 g). He had been working since
1952 in a ceramic industry, making hand prepared
enamel. When somebody asked him why he never
talked about his job, he said: I did, but the physicians
told me I have not black tooth, so I could not be lead
intoxicated, and I was most probably suffering from
psychosomatic symptoms or was even a drug addict. A
renal biopsy showed ischaemic glomeruli and
arteriolosclerosis compatible with lead-nephropathy.
Chelation therapy was done for 20 years (body lead
burden was still >600 g in 1992) and halted only in
1998, as normal lead excretion was obtained. There
was no relapse of abdominal pain, and he is now
enjoying good general health, with normal renal
function and good blood pressure control .
This case illustrates two important points: (a) only if
doctors ask their patients about exposure may a causal
association be established; and (b) only if doctors know
the potential risk implications of an occupation on
health may a correlation between symptoms and
exposure be recognised.
Although some doctors think occupational diseases
are a thing of the past, occupational risks do still exist,
as do environmental and lifestyle exposure risks (from
pollution, hobbies, habits) such as lead toxicity in
children and elderly people. Occupational diseases
lack glamour for potential clinical investigators, but
they are important because they can be prevented.
They also serve as models (few workers exposed to
high concentrations of toxins over short periods) that
help in the understanding of environmental diseases
(large populations exposed to low concentrations over
long periods).
So, please ask patients about job experience and
other possible occupational or environmental
exposure, as we have done routinely since looking after
this patient.
Piero Stratta clinician
Caterina Canavese clinician, Nephrology, Dialysis, and
Transplantation, University of Torino, Italy
We welcome articles up to 600 words on topics such as
A memorable patient, A paper that changed my practice, My
most unfortunate mistake, or any other piece conveying
instruction, pathos, or humour. If possible the article
should be supplied on a disk. Permission is needed
from the patient or a relative if an identifiable patient is
referred to.
Education and debate
628 BMJ VOLUME 323 15 SEPTEMBER 2001 bmj.com
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Basics of Spiritual Life-1Documento33 pagineBasics of Spiritual Life-1rommel duran67% (3)
- Rainbow Bridge 0Documento26 pagineRainbow Bridge 0rezalene velez50% (4)
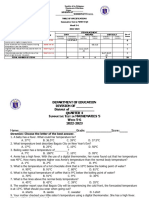
- Table of Specification - K-12Documento15 pagineTable of Specification - K-12caroline dullete77% (31)
- 6-Cross Training As A Motivational and ProblemDocumento3 pagine6-Cross Training As A Motivational and Problemakositabon100% (1)
- P6030 Qual2 Shelley2007Documento6 pagineP6030 Qual2 Shelley2007char2183Nessuna valutazione finora
- USHealth11 MarmorDocumento6 pagineUSHealth11 Marmorchar2183Nessuna valutazione finora
- Health Payment Brief 2011Documento8 pagineHealth Payment Brief 2011char2183Nessuna valutazione finora
- True Worship Part 3Documento12 pagineTrue Worship Part 3char2183Nessuna valutazione finora
- Evolution of The U.S. Long-Term Care SystemDocumento6 pagineEvolution of The U.S. Long-Term Care Systemchar2183Nessuna valutazione finora
- 2003 Parables of JesusDocumento56 pagine2003 Parables of Jesuschar2183Nessuna valutazione finora
- Entry Point: Requiem For The Class ActDocumento4 pagineEntry Point: Requiem For The Class Actchar2183Nessuna valutazione finora
- Riverstone Internship ProjectDocumento2 pagineRiverstone Internship Projectchar2183Nessuna valutazione finora
- The Transformed Life Part 3Documento19 pagineThe Transformed Life Part 3char2183Nessuna valutazione finora
- Bible Study - Drifting 1Documento2 pagineBible Study - Drifting 1char2183Nessuna valutazione finora
- P6050 LC2 Franco2007Documento7 pagineP6050 LC2 Franco2007char2183Nessuna valutazione finora
- Bible Study On Hermeneutics - Handout 5 Grace Bible Chapel: Pastor/Teacher Jim BryantDocumento3 pagineBible Study On Hermeneutics - Handout 5 Grace Bible Chapel: Pastor/Teacher Jim Bryantchar2183Nessuna valutazione finora
- How To Be A Servant - A Personal Bible StudyDocumento3 pagineHow To Be A Servant - A Personal Bible Studychar2183Nessuna valutazione finora
- ChristologyDocumento16 pagineChristologychar2183Nessuna valutazione finora
- The Judgment of BelieversDocumento9 pagineThe Judgment of Believerschar2183Nessuna valutazione finora
- Sin and AdamDocumento26 pagineSin and Adamchar2183Nessuna valutazione finora
- Academic Policy Advisor: Health Policy and ManagementDocumento7 pagineAcademic Policy Advisor: Health Policy and Managementchar2183Nessuna valutazione finora
- Hebrews Study GuideDocumento14 pagineHebrews Study Guidechar2183Nessuna valutazione finora
- ParablesDocumento28 pagineParableschar2183Nessuna valutazione finora
- Holiness 8Documento2 pagineHoliness 8char2183Nessuna valutazione finora
- Lesson 9 - Holiness and Our Wills (Chapter 13) : "Be Holy, Because I Am Holy"Documento2 pagineLesson 9 - Holiness and Our Wills (Chapter 13) : "Be Holy, Because I Am Holy"char2183Nessuna valutazione finora
- Lesson PlananuDocumento5 pagineLesson PlananuanushadaNessuna valutazione finora
- Eating Attitudes Test (EAT-40) J-swinbourne-ThesisDocumento442 pagineEating Attitudes Test (EAT-40) J-swinbourne-ThesisMilosNessuna valutazione finora
- Emergence of OBDocumento4 pagineEmergence of OBBhavya VermaNessuna valutazione finora
- Robert HavighurstDocumento3 pagineRobert HavighurstRafael Delloma100% (2)
- Columbia University Map LocationsDocumento2 pagineColumbia University Map LocationsElizabeth BNessuna valutazione finora
- Knowledge Is WealthDocumento100 pagineKnowledge Is WealthmustaqNessuna valutazione finora
- The Implications of The Dodo Bird Verdict For Training in Psychotherapy Prioritizing Process ObservationDocumento4 pagineThe Implications of The Dodo Bird Verdict For Training in Psychotherapy Prioritizing Process ObservationSebastian PorcelNessuna valutazione finora
- The Anatomical and Functional Relation Between Gluteus Maximus and Fascia LataDocumento6 pagineThe Anatomical and Functional Relation Between Gluteus Maximus and Fascia LataRodrigo Ruiz CarrascoNessuna valutazione finora
- Final English 7 1ST QuarterDocumento4 pagineFinal English 7 1ST QuarterRosel GumabatNessuna valutazione finora
- Incorporating Music Videos in Theory CoursesDocumento5 pagineIncorporating Music Videos in Theory Coursesapi-246372446Nessuna valutazione finora
- 32.kushtia (Life Old)Documento6 pagine32.kushtia (Life Old)Habib AliNessuna valutazione finora
- Operator's Manual V3.0: FGRDEI01.fm Page - 1 Tuesday, November 12, 2002 2:04 PMDocumento14 pagineOperator's Manual V3.0: FGRDEI01.fm Page - 1 Tuesday, November 12, 2002 2:04 PMDumitru CristianNessuna valutazione finora
- HOSTEL FEE PAYMENT PROCEDURE FOR SY To FINAL YEARDocumento2 pagineHOSTEL FEE PAYMENT PROCEDURE FOR SY To FINAL YEARAbhishek PawarNessuna valutazione finora
- Journal 1Documento3 pagineJournal 1Nagaraj ManogaranNessuna valutazione finora
- Hidden CurriculumDocumento11 pagineHidden CurriculumRamakant Patil100% (4)
- Literacy Unit Plan Lesson 4Documento2 pagineLiteracy Unit Plan Lesson 4api-212727998Nessuna valutazione finora
- Academic TextDocumento2 pagineAcademic TextCatherine ProndosoNessuna valutazione finora
- Note MakingDocumento5 pagineNote MakingAnushka MishraNessuna valutazione finora
- Patient A (Click On The Link To "Complete Patient A's Karyotype")Documento2 paginePatient A (Click On The Link To "Complete Patient A's Karyotype")ZzaiRraNessuna valutazione finora
- TOR EMBeD Summer 2020 InternshipDocumento2 pagineTOR EMBeD Summer 2020 InternshipvishakhaNessuna valutazione finora
- Module 1 Teaching PE Health in Elem. Updated 1Documento10 pagineModule 1 Teaching PE Health in Elem. Updated 1ja ninNessuna valutazione finora
- Principles of Information Technology Syllabus 2015Documento4 paginePrinciples of Information Technology Syllabus 2015api-234035809Nessuna valutazione finora
- The Stage Approach: Developed by W. Huitt (1999)Documento39 pagineThe Stage Approach: Developed by W. Huitt (1999)Ruchika AgarwalNessuna valutazione finora
- NBB 302 (PSYC 353) : Behavioral NeuroscienceDocumento46 pagineNBB 302 (PSYC 353) : Behavioral NeuroscienceThomas CarswellNessuna valutazione finora
- Imslp652595-Pmlp17533-Chaminade Concertino For Flute and Orchestra - Full Score No PartsDocumento32 pagineImslp652595-Pmlp17533-Chaminade Concertino For Flute and Orchestra - Full Score No PartsDulce SánchezNessuna valutazione finora
- ST3 - Math 5 - Q4Documento3 pagineST3 - Math 5 - Q4Maria Angeline Delos SantosNessuna valutazione finora
- LCZ 400 Unit 3 4 RevisionDocumento12 pagineLCZ 400 Unit 3 4 RevisionLebohang ZwaneNessuna valutazione finora