Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Spinal Cord Injury
Caricato da
Reylan Deo Rallo AsioCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Spinal Cord Injury
Caricato da
Reylan Deo Rallo AsioCopyright:
Formati disponibili
Spinal cord injury (SCI) is a major health disorder.
Almost
200,000 people in the United States live each day with a
disability from SCI, and an estimated 11,000 new injuries
occur each year (Hickey, 2009). SCI is primarily an injury
of young adult males and 50% of those injured are between
16 and 30 years of age. Patients over the age of 60 years account
for 10% of SCIs, and this figure has steadily risen over
the past 25 years (Dawodu, 2007).
Motor vehicle crashes account for 48% of reported cases
of SCI, with falls (23%), violence primarily from gunshot
wounds (14%), recreational sporting activities (9%), and
other events accounting for the remaining injuries. Paraplegia
(paralysis of the lower body) and tetraplegia (formerly
quadriplegiaparalysis of all four extremities) can
occur, with incomplete tetraplegia (formerly quadriplegia)
the largest category, followed by complete paraplegia, complete
tetraplegia, and paraplegia.
The predominant risk factors for SCI include young age,
male gender, and alcohol and drug use. The frequency with
which these risk factors are associated with SCI serves to
emphasize the importance of primary prevention. The same
interventions suggested earlier in this chapter for head injury
prevention serve to decrease the incidence of SCI as
well (see Chart 63-1).
Most (80%) people who live with SCIs are men. The approximate
ethnic distribution is 62% Caucasian, 22%
African American, 13% Hispanic, and 3% other racial or
ethnic groups (Dawodu, 2007). Life expectancy continues
to increase for people with SCI because of improved health
care but remains slightly lower than for those without SCI.
The major causes of death are pneumonia, pulmonary emboli
(PE), and septicemia (Dawodu, 2007; Hickey, 2009).
Pathophysiology
Damage in SCI ranges from transient concussion (from
which the patient fully recovers), to contusion, laceration,
and compression of the spinal cord substance (either alone
or in combination), to complete transection (severing) of
the spinal cord (which renders the patient paralyzed below
the level of the injury). The vertebrae most frequently involved
are the 5th, 6th, and 7th cervical vertebrae (C5 to
C7), the 12th thoracic vertebra (T12), and the 1st lumbar
vertebra (L1). These vertebrae are most susceptible because
there is a greater range of mobility in the vertebral column
in these areas (Sherwood, Crago, Spiro, et al., 2007).
SCIs can be separated into two categories: primary injuries
and secondary injuries. Primary injuries are the result
of the initial insult or trauma and are usually permanent.
Secondary injuries are usually the result of a contusion ortear injury, in which the nerve fibers begin to
swell and disintegrate.
A secondary chain of events produces ischemia,
hypoxia, edema, and hemorrhagic lesions, which in turn
result in destruction of myelin and axons. The secondary
injury is of primary concern for critical care nurses. Experts
believe secondary injury is the principal cause of spinal
cord degeneration at the level of injury and that it is reversible
during the first 4 to 6 hours after injury. Methods
of early treatment are essential to prevent partial damage
from becoming total and permanent (Sherwood, et al.,
2007).
Clinical Manifestations
Manifestations of SCI depend on the type and level of injury
(Chart 63-7). The type of injury refers to the extent of
injury to the spinal cord itself. Incomplete spinal cord lesions
(the sensory or motor fibers, or both, are preserved below
the lesion) are classified according to the area of spinal
cord damage: central, lateral, anterior, or peripheral. The
American Spinal Injury Association (ASIA) provides classification
of SCI according to the degree of sensory and motor
function present after injury (Chart 63-8). Neurologic
level refers to the lowest level at which sensory and motor
functions are normal. Below the neurologic level, there is
total sensory and motor paralysis, loss of bladder and bowel
control (usually with urinary retention and bladder distention),
loss of sweating and vasomotor tone, and marked reduction
of blood pressure from loss of peripheral vascular resistance.
A complete spinal cord lesion (total loss of
sensation and voluntary muscle control below the lesion)
can result in paraplegia or tetraplegia.
If conscious, the patient usually complains of acute pain
in the back or neck, which may radiate along the involved
nerve. However, absence of pain does not rule out spinal injury,
and a careful assessment of the spine should be conducted
if there has been a significant force and mechanism
of injury (ie, concomitant head injury). Often the patient
speaks of fear that the neck or back is broken.
Respiratory dysfunction is related to the level of injury.
The muscles contributing to respiration are the abdominals
and intercostals (T1 to T11) and the diaphragm (C4). In
high cervical cord injury, acute respiratory failure is the
leading cause of death. Functional abilities by level of injury
are described in Table 63-3.
Assessment and Diagnostic Findings
A detailed neurologic examination is performed. Diagnostic
x-rays (lateral cervical spine x-rays) and CT scanning
are usually performed initially. An MRI scan may be
ordered as a further workup if a ligamentous injury is suspected,
because significant spinal cord damage may exist
even in the absence of bony injury (Hickey, 2009). If an
MRI scan is contraindicated, a myelogram may be used
to visualize the spinal axis. An assessment is made for
other injuries, because spinal trauma often is accompanied
by concomitant injuries, commonly to the head and
chest. Continuous electrocardiographic monitoring may
be indicated if a spinal cord injury is suspected, because
bradycardia (slow heart rate) and asystole (cardiac
standstill) are common in patients with acute spinal cord
injuries.
Emergency Management
The immediate management at the scene of the injury is
critical, because improper handling of the patient can cause
further damage and loss of neurologic function. Any patient
who is involved in a motor vehicle crash, a diving or contact
sports injury, a fall, or any direct trauma to the head
and neck must be considered to have SCI until such an injury
is ruled out. Initial care must include a rapid assessment,
immobilization, extrication, and stabilization or control
of life-threatening injuries, and transportation to the
most appropriate medical facility. Immediate transportation
to a trauma center with the capacity to manage major neurologic
trauma is then necessary (Hickey, 2009).
At the scene of the injury, the patient must be immobilized
on a spinal (back) board, with the head and neck maintained
in a neutral position, to prevent an incomplete injury from becoming
complete. One member of the team must assume control
of the patients head to prevent flexion, rotation, or extension;
this is done by placing the hands on both sides of the
patients head at about ear level to limit movement and maintain
alignment while a spinal board or cervical immobilizing
device is applied. If possible, at least four people should slide
the patient carefully onto a board for transfer to the hospital.
Any twisting movement may irreversibly damage the spinal
cord by causing a bony fragment of the vertebra to cut into,
crush, or sever the cord completely.
The standard of care is that the patient is referred to a
regional spinal injury or trauma center because of the multidisciplinary
personnel and support services required to
counteract the destructive changes that occur in the first
24 hours after injury. However, no randomized controlled
trials have been conducted to confirm that referral results in
better outcomes for the patient with SCI (Jones & Bagnall,
2008). During treatment in the emergency and x-ray departments,
the patient is kept on the transfer board. The patient
must always be maintained in an extended position. No part
of the body should be twisted or turned, and the patient is
not allowed to sit up. Once the extent of the injury has been
determined, the patient may be placed on a rotating specialty
bed (Fig. 63-6) or in a cervical collar (Fig. 63-7). Later,
if SCI and bone instability have been ruled out, the patient
may be moved to a conventional bed or the collar may be
removed without harm. If a specialty bed is needed but not
available, the patient should be placed in a cervical collar
and on a firm mattress.
Medical Management (Acute Phase)
The goals of management are to prevent secondary injury,
to observe for symptoms of progressive neurologic deficits,
and to prevent complications. The patient is resuscitated as
necessary, and oxygenation and cardiovascular stability are
maintained. SCI is a devastating event; new treatment
methods and medications are continually being investigated
for the acute and chronic phases of care (Fehlings &
Baptiste, 2005).
Pharmacologic Therapy
Administration of high-dose IV corticosteroids or methylprednisolone
sodium succinate in the first 24 or 48 hours iscontroversial. Despite the ongoing controversy surrounding
the practice, the use of IV high-dose methylprednisolone is
accepted as standard therapy for SCI in many countries and
remains an established clinical practice in most trauma centers
in the United States (Hickey, 2009).
Respiratory Therapy
Oxygen is administered to maintain a high partial pressure
of oxygen (PaO2), because hypoxemia can create or worsen
a neurologic deficit of the spinal cord. If endotracheal intubation
is necessary, extreme care is taken to avoid flexing or
extending the patients neck, which can result in extension
of a cervical injury.
In high cervical spine injuries, spinal cord innervation to
the phrenic nerve, which stimulates the diaphragm, is lost.
Diaphragmatic pacing (electrical stimulation of the phrenic
nerve) attempts to stimulate the diaphragm to help the patient
breathe (Sole, Klein & Moseley, 2009). Intramuscular
diaphragmatic pacing is currently in the clinical trial phase
for the patient with a high cervical injury. This is implanted
via laparoscopic surgery, usually after the acute phase.
Skeletal Fracture Reduction and Traction
Management of SCI requires immobilization and reduction
of dislocations (restoration of normal position) and stabilization
of the vertebral column.
Cervical fractures are reduced, and the cervical spine is
aligned with some form of skeletal traction, such as skeletal
tongs or calipers, or with use of the halo device (Sole, et al.,
2009). A variety of skeletal tongs are available, all of which
involve fixation in the skull in some manner. The Gardner-
Wells tongs require no predrilled holes in the skull. Crutchfield
and Vinke tongs are inserted through holes made in
the skull with a special drill under local anesthesia.
Traction is applied to the skeletal traction device by
weights, the amount depending on the size of the patient
and the degree of fracture displacement. The traction force
is exerted along the longitudinal axis of the vertebral bodies,
with the patients neck in a neutral position. The traction
is then gradually increased by adding more weights. As
the amount of traction is increased, the spaces between the
intervertebral disks widen and the vertebrae are given a
chance to slip back into position. Reduction usually occurs
after correct alignment has been restored. Once reduction isachieved, as verified by cervical spine x-rays
and neurologic
examination, the weights are gradually removed until the
amount of weight needed to maintain the alignment is
identified. The weights should hang freely so as not to interfere
with the traction. Traction is sometimes supplemented
with manual manipulation of the neck by a surgeon
to help achieve realignment of the vertebral bodies.
A halo device may be used initially with traction, or may
be applied after removal of the tongs. It consists of a stainless
steel halo ring that is fixed to the skull by four pins. The
ring is attached to a removable halo vest, a device thatsuspends the weight of the unit circumferentially
around
the chest. A metal frame connects the ring to the chest.
Halo devices provide immobilization of the cervical spine
while allowing early ambulation (Fig. 63-8).
Thoracic and lumbar injuries are usually treated with
surgical intervention followed by immobilization with a fitted
brace. Traction is not indicated either before or after
surgery, due to the relative stability of the spine in these
regions. Surgical Management
Surgery is indicated in any of the following situations:
Compression of the cord is evident.
The injury results in a fragmented or unstable vertebral
body.
The injury involves a wound that penetrates the cord.
Bony fragments are in the spinal canal.
The patients neurologic status is deteriorating.
Research indicates that early surgical stabilization improves
the clinical outcome of patients compared to surgeryperformed later during the clinical course. The goals
of surgical
treatment are to preserve neurologic function by removing
pressure from the spinal cord and to provide stability
(Sherwood, et al., 2007).
Management of Acute Complications of
Spinal Cord Injury
Spinal and Neurogenic Shock
The spinal shock associated with SCI reflects a sudden depression
of reflex activity in the spinal cord (areflexia) below
the level of injury. The muscles innervated by the part
of the spinal cord segment below the level of the lesion are
without sensation, paralyzed, and flaccid, and the reflexes
are absent. In particular, the reflexes that initiate bladder
and bowel function are affected. Bowel distention and paralytic
ileus can be caused by depression of the reflexes and
are treated with intestinal decompression by insertion of a
nasogastric tube (Dawodu, 2007).
Neurogenic shock develops as a result of the loss of autonomic
nervous system function below the level of the lesion
(Dawodu, 2007). The vital organs are affected, causing decreases
in blood pressure, heart rate, and cardiac output, as
well as venous pooling in the extremities and peripheral vasodilation.
In addition, the patient does not perspire in the
paralyzed portions of the body, because sympathetic activity
is blocked; therefore, close observation is required for early
detection of an abrupt onset of fever. Further discussion of
neurogenic shock can be found in Chapter 15.
With injuries to the cervical and upper thoracic spinal cord,
innervation to the major accessory muscles of respiration is lost
and respiratory problems develop. These include decreased
vital capacity, retention of secretions, increased partial pressure
of arterial carbon dioxide (PaCO2) levels and decreased
oxygen levels, respiratory failure, and pulmonary edema.
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a potential complication of
immobility and is common in patients with SCI. Patients who
develop DVT are at risk for PE, a life-threatening complication.
Manifestations of PE include pleuritic chest pain, anxiety,
shortness of breath, and abnormal blood gas values (increased
PaCO2 and decreased PaO2). Low-dose anticoagulation therapy
usually is initiated to prevent DVT and PE, along with the
use of anti-embolism stockings or pneumatic compression devices.
In some cases, permanent indwelling filters (see Chapter
23) may be placed prophylactically in the vena cava to prevent
emboli (dislodged clots) from migrating to the lungs and causing
a PE (Hickey, 2009).
Other Complications
In addition to respiratory complications (respiratory failure,
pneumonia) and autonomic dysreflexia (characterized by
pounding headache, profuse sweating, nasal congestion, piloerection [goose bumps], bradycardia, and
hypertension),
other complications that may occur include pressure
ulcers and infection (urinary, respiratory, and local infection
at the skeletal traction pin sites) (Vacca, 2007a).
THE PATIENT WITH ACUTE SPINAL
CORD INJURY
Assessment
The patients breathing pattern and the strength of the
cough are assessed, and the lungs are auscultated, because
paralysis of abdominal and respiratory muscles diminishes
coughing and makes clearing of bronchial and
pharyngeal secretions difficult. Reduced excursion of the
chest also results.
The patient is monitored closely for any changes in motor
or sensory function and for symptoms of progressive neurologic
damage. In the early stages of SCI, determining
whether the cord has been severed may not be possible, because
signs and symptoms of cord edema are indistinguishable
from those of cord transection. Edema of the spinal
cord may occur with any severe cord injury and may further
compromise spinal cord function.
Motor and sensory functions are assessed through careful
neurologic examination. These findings are recorded on a flow
sheet so that changes in the baseline neurologic status can be
monitored closely and accurately. The ASIA classification is
commonly used to describe level of function for patients with
SCI (see Chart 63-8). Chart 63-7 gives examples of the effects
of altered spinal cord function. At the minimum:
Motor ability is tested by asking the patient to spread
the fingers, squeeze the examiners hand, and move
the toes or turn the feet.
Sensation is evaluated by gently pinching the skin or
touching it lightly with an object such as a tongue
blade, starting at shoulder level and working down
both sides of the extremities. The patient should have
both eyes closed so that the examination reveals true
findings, not what the patient hopes to feel. The patient
is asked where the sensation is felt.
Any decrease in neurologic function is reported immediately.
The patient is also assessed for spinal shock, a complete
loss of all reflex, motor, sensory, and autonomic activity below
the level of the lesion that causes bladder paralysis and
distention. The lower abdomen is palpated for signs of urinary
retention and overdistention of the bladder. Further
assessment is made for gastric dilation and paralytic ileus
caused by an atonic bowel, a result of autonomic disruption.
Temperature is monitored, because the patient may have
periods of hyperthermia as a result of alteration in temperature
control due to autonomic disruption.
Diagnosis
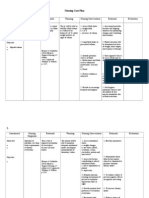
Nursing Diagnoses
Based on the assessment data, the patients major nursing
diagnoses may include the following:
Potrebbero piacerti anche
- Estimated Fluid and Blood LossDocumento1 paginaEstimated Fluid and Blood LossReylan Deo Rallo AsioNessuna valutazione finora
- Spinal Cord InjuryDocumento7 pagineSpinal Cord InjuryReylan Deo Rallo AsioNessuna valutazione finora
- Nursing Care Plan CKDDocumento6 pagineNursing Care Plan CKDReylan Deo Rallo Asio100% (5)
- A Psalm of LifeDocumento1 paginaA Psalm of LifeReylan Deo Rallo Asio100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)