Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Bacteria and Food
Caricato da
Guranjan MatharooCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Bacteria and Food
Caricato da
Guranjan MatharooCopyright:
Formati disponibili
Bacteria and Food Poisoning
The U.S. Centers for Disease Control and Prevention (CDC) estimates that around
80 million people a year in the U.S. alone contract food poisoning or other
foodborne diseases.
Foodborne illness is caused by eating or drinking food that contains disease
causing agents. The most common causes of foodborne diseases are
bacteria, viruses, and parasites. Foods containing toxic chemicals can cause
foodborne diseases as well.
There are over two hundred types of bacteria, viruses and parasites that can
cause foodborne diseases. Reactions to these germs can range from mild gastric
discomfort to death. The easiest way to prevent foodborne illness is to properly
handle and cook foods. This includes washing your hands and utensils carefully
and cooking meat thoroughly.
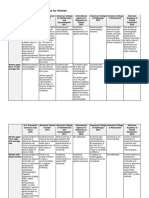
Below is a list of a few bacteria that cause foodborne diseases, along with the
foods that are associated with them, as well as symptoms that are likely to
develop from ingesting the contaminated foods.
Bacteria and Food Poisoning
Microbe - Aeromonas hydrophila
Affiliated Foods - Fish, Shellfish, Beef, Pork, Lamb, and Poultry
Diseases - Gastroenteritis, Septicemia
Symptoms - Diarrhea, Blood and Mucus in Stool
Microbe - Bacillus cereu
Affiliated Foods - Meats, Milk, Rice, Potato, and Cheese Products
Diseases - B. cereus Food Poisoning
Symptoms - Diarrhea, Abdominal Cramps, Nausea
Microbe - Campylobacter jejuni
Affiliated Foods - Raw Chicken, Unpasteurized Milk, Non-chlorinated Water
Diseases - B. cereus Campylobacteriosis
Symptoms - Diarrhea, Abdominal Cramps, Nausea and Fever, Headache and
Muscle Pain
Microbe - Clostridium botulinum
Affiliated Foods - Canned Foods Including: Vegetables, Meats, and Soups
Diseases - Foodborne Botulism
Symptoms - Weakness, Double Vision and Vertigo, Difficulty in Speaking,
Swallowing, and Breathing, Constipation
Microbe - Clostridium perfringens
Affiliated Foods - Non-refrigerated Prepared Foods: Meats and Meat Products,
Gravy
Diseases - Perfringens Food Poisoning
Symptoms - Severe Abdominal Cramps, Diarrhea
Microbe - Escherichia coli O157:H7
Affiliated Foods - Undercooked Meats, Raw Ground Beef
Diseases - Hemorrhagic colitis
Symptoms - Severe Abdominal Pain, Watery and Bloody Diarrhea, Vomiting
Microbe - Listeria monocytogenes
Affiliated Foods - Dairy Products, Raw Vegetables, Raw Meats, Smoked Fish
Diseases - Listeriosis
Symptoms - Flu-like Symptoms, Persistent Fever, Nausea and Vomiting,
Diarrhea
Microbe - Salmonella spp.
Affiliated Foods - Poultry and Eggs, Milk and Dairy Products, Raw Meats, Fish,
Shrimp, Peanut Butter
Diseases - Salmonellosis
Symptoms - Nausea, Vomiting, Abdominal Pain, Fever, Headache, Diarrhea
Microbe - Shigella spp
Affiliated Foods - Poultry, Milk and Dairy Products, Raw Vegetables, Fecally
contaminated water, Salads: Potato, Chicken, Tuna, Shrimp
Diseases - Shigellosis
Symptoms - Diarrhea, Abdominal Pain, Fever, Vomiting, Blood or Mucus in
Stool
Microbe - Staphylococcus aureus
Affiliated Foods - Poultry and Egg Products, Meat Products, Dairy Products
Diseases - Staphyloenterotoxicosis, Staphyloenterotoxemia
Symptoms - Abdominal Cramping, Nausea and Vomiting, Prostration
Microbe - Vibrio cholerae
Affiliated Foods - Contaminated Water, Shellfish
Diseases - Cholera
Symptoms - Watery Diarrhea, Abdominal Pain, Dehydration, Vomiting, Shock
Types of Food poisoning
Nonbacterial
It is caused by chemicals such as arsenic, certain plant and sea
foods, etc. In recent years, there has been a growing concern
about contamination of food by chemicals, eg. fertilizers,
pesticides, cadmium and mercury.
Bacterial
It is caused by the ingestion of foods contaminated by living
bacteria or their toxins. The conventional classification of bacterial
food poisoning into toxic and infective types is becoming
increasingly blurred with the knowledge that in some types, both
multiplication and toxin production are involved.
Botulism
Botulism is a rare but serious illness caused by a bacterium which occurs in soil. It
produces a toxin that affects your nerves. Foodborne botulism comes from eating
foods contaminated with the toxin.
Sources Infants: Honey, home-canned vegetables and fruits, corn
syrup
Children and adults: Home-canned foods with a low acid
content, improperly canned commercial foods, home-canned
or fermented fish, herb-infused oils, baked potatoes in
aluminum foil, cheese sauce, bottled garlic, foods held warm
for extended periods of time
Incubation
Period
Infants: 3-30 days
Children and adults: 12-72 hours
Symptoms Infants: Lethargy, weakness, poor feeding, constipation, poor
head control, poor gag and sucking reflex
Children and adults: Double vision, blurred vision, drooping
eyelids, slurred speech, difficulty swallowing, dry mouth and
muscle weakness
Duration of
Illness
Variable
What Do I
Do?
Botulism is a medical emergency. If you have symptoms of botulism,
contact your doctor immediately.
How Do I
Prevent It?
Be very careful when canning foods at home
Do not let babies eat honey
Get prompt medical care for infected wounds
Bacteria Found in Bottled Mineral Water
Bottled Water May Not Be Safer Than Tap Water in Reducing Risk of Infection
Nov. 4, 2004 -- Choosing bottled mineral water over tap may not offer more
protection against potentially hazardous bacteria, according to new research.
Dutch researchers sampled bottled mineral water from 16 countries, not
including the U.S., and found about 40% of the samples showed evidence of
contamination with either bacteria or fungi. In laboratory cultures, bacteria grew
from 21 of the 68 samples.
Researchers say the high levels of bacterial contamination in commercially bottled
mineral water may pose a health threat to certain people, such as children, the
elderly, and those with weakened immune systems such as people
with cancer,kidney failure requiring dialysis, diabetes, or AIDS.
The findings were presented this week at the Interscience Conference on
Antimicrobial Agents and Chemotherapy in Washington, D.C.
Bottled Mineral Water May Not Be Safer to Drink
Researchers say people with weakened immune systems who are hospitalized are
often given bottled mineral water under the assumption that it is not
contaminated and therefore safer to drink than tap water.
But the results show that there is still a risk of infection from common illness-
causing bacteria, such as legionella, from bottled mineral water. Infection with
legionella bacteria can lead to a serious, pneumonia-like condition
calledLegionnaires' disease.
In their study, researcher Rocus Klont, of the University Medical Center Nijmegen
in the Netherlands, and colleagues analyzed bottled water from nine European
countries and seven others, including Canada, Australia, and Mexico.
They found all of the bottles appeared to have been properly sealed, which
eliminated the possibility of contamination after bottling.
Laboratory tests showed 37% of the samples had evidence for contamination with
bacteria, including legionella, and 4% had evidence of fungal contamination.
Accidental Poisoning
Accidental poisoning in children is one of the commonest emergency
encountered in pediatric practice. The reported incidence of childhood poisoning
in various studies varies from 0.3 to 7.6%(1,2) which constitutes a significant
number of admissions to the pediatric wards. So far, different regional
studies are not available to exhibit the incidence and patterns of different
poisoning. The present retrospective study aims to find out the incidence,
morbidity and mortality of different poisonings in children.
Material and Methods
This retrospective study was carried out in J.L.N. Medical College and Hospital,
Ajmer. Records of all poisoning cases admitted in children ward during period
June, 1987 to May, 1993 were analyzed. Children with idiosyncratic reactions to
prescribed drugs were not included.
Results
Of 20,011 patients admitted from June 1987 to May 1993, 223 (1.1%) were of
accidental poisoning. The commonest age group was 0-5 years constituting 81.2%
of total patients of poisonings, followed by 5-10 years (16.1%). There was an
overall male predominance, with male to female ratio of 1.6: 1. In the 0-5 years
age group, the mode of poisoning was oral in 94.1% patients and parenteral in
5.5% patients. In 5-10 years age group, oral route constituted 66.7% cases. In
children above 10 years, both routes were almost equal. The incidence of
poisoning was 41.7% in summer, 33.6% in rainy and 24.7% in winter season.
Kerosene poisoning occurred throughout the year, peaking in summer while
maximum cases of snake bite were seen in rainy season with no case recorded
during winter. Accidental ingestion of kerosene was the commonest poisoning
(48.8%), followed by accidental ingestion of drugs (11.7%), and snake bite
(11.2%). Other causes included dhatura poisoning (8.1%), food poisoning (7.2%)
and ingestion of Paris Green (3.1%). Of all the cases, 3 patients, two of snake bite
and one from severe dhatura poisoning, died.
Kerosene Poisoning
Accidental ingestion of kerosene oil was the commonest poisoning in this study.
The amount ingested could not be calculated properly. However, it was never
more than 10-15 ml. Of 109 cases (48.8%), 29 (13.3%) were asymptomatic. The
common symptoms included cough (75.8%) and fever (66.9%). Other symptoms
were restlessness, vomiting and drowsiness. X-ray chest showed features of
pneumonitis in 44 cases (40.3%) only. All cases recovered.
Snake Bite
Snake bite was commonest among parenteral poisoning. Out of total 20 cases, 15
(75%) were due to nonpoisonous snakes. Out of 5 poisonous, 3 cases presented
with hemorrhagic manifestations and one each with paralytic features and local
cellulitis. Drugs: Of 26 cases of drug ingestion, phenothiazine was ingested in 11
(42.3%),codeine group of drugs in 5(19.2%) and iron tablets in 3 (11.5%) patients.
Discussion
The reported prevalence of accidental poisoning in children varies from 0.3% to
7.6%. The prevalence in our study was 1.1%, which is similar to those reported by
various authors (1-7) (Table 1).The commonest accidental poisoning in children
was ingestion of kerosene oil accounting for 48.9% cases. This is in agreement
with the already reported childhood poisonings (Table I).Accidental poisoning in
children is preventable. The incidence of oral poisoning has declined. This may be
due to increased literacy, urbanization and better child care. On the other hand,
there is increased incidence of poisoning due to various medicaments. This
increased incidence may be attributed to easy availability of drugs from medical
shops without physician's prescription, repeated administration of drugs by
parents without the advice of treating physician, less knowledge of drug dosage
and interactions to most of the private practitioners. The patterns of poisoning
are also changing This may be due to less availability of some previously used
offending agents, as seen with poisonings due to barbiturates and opium. Newer
drugs and chemicals are replacing the older ones. Paris green, which is used in
malaria control programme, accounted for 3.6% of all poisoning cases in our
study. Poisoning with this substance has not been reported in earlier studies. As
all these cases are preventable, there is need to strengthen the preventive
measures. All poisonous substances, drugs and chemicals should be kept out of
the reach of children. As the kitchen is the commonest place of poisoning, use of
standing type of kitchen should be encouraged. Other measures include adoption
of safe packings, child proof bottle caps, training of paramedical workers and rural
health personnel about basic principles of identification and safe storage of
potentially dangerous substances. Mass media such as TV, radio, newspapers can
be used for spreading the simple rules of prevention of poisoning. Legal
enforcement of over the country sale of drugs should be done. Treatment should
be instituted promptly and flow charts for emergency management and specific
antidotes should be available at all health centres.
Preventive measures:
Environmental standards that remove lead from petrol/gasoline, paint and
plumbing.
If lead pipes cannot be removed, water (cold should be flushed through in the
morning before drinking).
Enforcement of occupational health standards.
Surveillance of potentially exposed population groups, especially the vulnerable
ones (small children, pregnant women, workers).
Water treatment.
Removing lead solder from food cans.
Use of lead-free paint in homes.
Screening of children for blood levels over acceptable limit and referral for
medical care as necessary.
The health based guideline for lead in drinking water is 0.1 milligrams per litre
(WHO, 1993). If high levels are detected in a supply, alternative supplies or bottled
water maybe necessary to protect young children.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Important Causes of Sudden Cardiac DeathDocumento2 pagineImportant Causes of Sudden Cardiac DeathTausif AbbasNessuna valutazione finora
- The Three Basic Components of A Pulse: Shape, Jump, and LevelDocumento3 pagineThe Three Basic Components of A Pulse: Shape, Jump, and LevelShahul Hameed100% (1)
- VTR 214 PDFDocumento2 pagineVTR 214 PDFKimberly AndrzejewskiNessuna valutazione finora
- Brosur ZONCARE Full Digital Color Doppler Ultrasound Diagnostic System (Portable) V3Documento2 pagineBrosur ZONCARE Full Digital Color Doppler Ultrasound Diagnostic System (Portable) V3Gorengan 27Nessuna valutazione finora
- CT ScanDocumento37 pagineCT ScanBayu Ihkshan Yamada TriatmojoNessuna valutazione finora
- Type 2 Diabetes MellitusDocumento7 pagineType 2 Diabetes MellitusCadiz Etrama Di RaizelNessuna valutazione finora
- MestastaseDocumento10 pagineMestastaseCahyono YudiantoNessuna valutazione finora
- Sitecore - Media Library - Files.3d Imaging - Shared.7701 3dbrochure UsDocumento28 pagineSitecore - Media Library - Files.3d Imaging - Shared.7701 3dbrochure UsandiNessuna valutazione finora
- Determinants of HealthDocumento29 pagineDeterminants of HealthMayom Mabuong92% (12)
- Pcap - PathophysiologyDocumento4 paginePcap - PathophysiologyAyla Mar100% (1)
- Rajasekhar2021 Article TheUsefulnessOfGenelynEmbalminDocumento4 pagineRajasekhar2021 Article TheUsefulnessOfGenelynEmbalminyordin deontaNessuna valutazione finora
- Breast Cancer Screening GuidelinesDocumento4 pagineBreast Cancer Screening GuidelinesvaluatNessuna valutazione finora
- Vasopressors For ShockDocumento21 pagineVasopressors For ShocknugrahaNessuna valutazione finora
- Drug Study - LevetiracetamDocumento3 pagineDrug Study - LevetiracetamCath Bril100% (4)
- Rundown ISMI Hotti 2016Documento5 pagineRundown ISMI Hotti 2016Wahyu PurnomoNessuna valutazione finora
- PartografDocumento31 paginePartografrovi wilmanNessuna valutazione finora
- Onco-Critical Care An Evidence-Based ApproachDocumento539 pagineOnco-Critical Care An Evidence-Based ApproachZuriNessuna valutazione finora
- Ginjal Polikistik PDFDocumento15 pagineGinjal Polikistik PDFAgunkRestuMaulanaNessuna valutazione finora
- Perioperative Hemodynamic MonitoringDocumento9 paginePerioperative Hemodynamic MonitoringjayezmenonNessuna valutazione finora
- DFGHJKDocumento3 pagineDFGHJKcliffwinskyNessuna valutazione finora
- English GuideDocumento85 pagineEnglish GuideanandkishoreNessuna valutazione finora
- Checklist of Quality Indicators For NABH Accreditation PreparationDocumento11 pagineChecklist of Quality Indicators For NABH Accreditation PreparationQUALITY SIDARTH HOSPITALSNessuna valutazione finora
- مختارات د.ومضة-1-1Documento5 pagineمختارات د.ومضة-1-1Djdjjd SiisusNessuna valutazione finora
- Pes Planus Concept MapDocumento2 paginePes Planus Concept MapVeronica Jean U. TubaonNessuna valutazione finora
- 3f - 1 (Division of Task)Documento33 pagine3f - 1 (Division of Task)Trisha ArtosNessuna valutazione finora
- Structural and Dynamic Bases of Hand Surgery by Eduardo Zancolli 1969Documento1 paginaStructural and Dynamic Bases of Hand Surgery by Eduardo Zancolli 1969khox0% (1)
- EXERCISE Stress Testing FOR HEARTDocumento52 pagineEXERCISE Stress Testing FOR HEARTBenjamin GonzalezNessuna valutazione finora
- Amee Guide No 81 Part 1Documento10 pagineAmee Guide No 81 Part 1CatharinaWidiartiniNessuna valutazione finora
- Infection and Tumorigenesis of Biomaterials by Smit Prajapati-200280103028 and Yukta Dodia - 200280103052Documento18 pagineInfection and Tumorigenesis of Biomaterials by Smit Prajapati-200280103028 and Yukta Dodia - 200280103052Yukta DodiaNessuna valutazione finora
- Sensitivity and SpecificityDocumento12 pagineSensitivity and Specificitymia farrowNessuna valutazione finora