Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Deepa Metgud
Caricato da
Mutiara SazkiaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Deepa Metgud
Caricato da
Mutiara SazkiaCopyright:
Formati disponibili
1
Predicting Neurological Outcome in Very Low Birth
Weight Infants Using Movement Assessment of
Infants-A Longitudinal Study.
Thesis Submitted to
THE KLE ACADEMY OF HIGHER EDUCATION AND RESEARCH, BELGAUM
(KLE DEEMED UNIVERSITY)
[Declared as Deemed-to-be-University u/s 3 of the UGC Act, 1956 vide Govt. of India Notification No.F.9-19/2000-U.3 (A)]
(Accredited A Grade by NAAC)
For the award of the Degree of
Doctor of Philosophy
in the Faculty of
Medicine (Physiotherapy)
by
Mrs. Deepa Metgud M.P.T.
(Registration No: KLEU/Ph.D/07-08/DOUNO7044
Under the Guidance of
Prof. Dr. V. D. Patil M.D., DCH
K.L.E. University J. N. Medical College,
Belgaum 590010. Karnataka, India
April - 2011
Kvisoft PDF Merger DEMO : Purchase from www.kvisoft.com to remove the watermark
2
KLE ACADEMY OF HIGHER EDUCATION AND
RESEARCH,
(KLE DEEMED UNIVERSITY)
[Declared as Deemed-to-be-University u/s 3 of the UGC Act, 1956 vide Govt. of India Notification No.F.9-19/2000-U.3 (A)]
(Accredited A Grade by NAAC)
BELGAUM
Certificate By the Dean
This is to certify that the thesis entitled Predicting Neurological
Outcome in Very Low Birth Weight Infants Using
Movement Assessment of Infants-A Longitudinal Study is a
bonafide and genuine research carried out by Mrs. Deepa.Metgud under the
guidance of Dr. V. D. Patil, Professor, Department of Pediatrics, K.L.E.
University, J. N. Medical college, Belgaum.
Place: Belgaum
Date:
Prof. Dr. V. D. Patil M.D.,DCH
Dean Faculty of Medicine,
K.L.E. University,
J. N. Medical College,
Belgaum -590010. Karnataka
III
KLE ACADEMY OF HIGHER EDUCATION AND
RESEARCH,
(KLE DEEMED UNIVERSITY)
[Declared as Deemed-to-be-University u/s 3 of the UGC Act, 1956 vide Govt. of India Notification No.F.9-19/2000-U.3 (A)]
(Accredited A Grade by NAAC)
BELGAUM
Declaration By the Candidate
I hereby declare that the thesis entitled Predicting Neurological
Outcome in Very Low Birth Weight Infants Using Movement
Assessment of Infants-A Longitudinal Study is a bonafide and original
research carried out by me under the guidance of Dr. V. D. Patil, Professor,
Department of Pediatrics and Dean Faculty of Medicine , K.L.E.U J N
Medical college, Belgaum. The thesis or any part thereof has not formed the
basis for the award of any degree/fellowship or similar title to any candidate of
any University.
Place : Belgaum
Date :
Mrs. Deepa Metgud M.P.T.
KLEU Institute of Physiotherapy,
Belgaum
IV
KLE ACADEMY OF HIGHER EDUCATION AND
RESEARCH,
(KLE DEEMED UNIVERSITY)
[Declared as Deemed-to-be-University u/s 3 of the UGC Act, 1956 vide Govt. of India Notification No.F.9-19/2000-U.3 (A)]
(Accredited A Grade by NAAC)
BELGAUM
Certificate by the Guide
This is to certify that the thesis titled Predicting Neurological
Outcome in Very Low Birth Weight Infants Using Movement
Assessment of Infants-A Longitudinal Study is a bonafide research
work done by Mrs. Deepa.Metgud.
Place: Belgaum
Date
Dr. V .D. Patil M.D., DCH
Principal,
Professor, Department of Pediatrics
KLE University,
J. N. Medical College, Belgaum
V
KLE ACADEMY OF HIGHER EDUCATION AND
RESEARCH,
(KLE DEEMED UNIVERSITY)
[Declared as Deemed-to-be-University u/s 3 of the UGC Act, 1956 vide Govt. of India Notification No.F.9-19/2000-U.3 (A)]
(Accredited A Grade by NAAC)
BELGAUM
Endorsement by the Principal
This is to certify that the dissertation titled Predicting
Neurological Outcome in Very Low Birth Weight Infants Using
Movement Assessment of Infants-A Longitudinal Study under the
guidance of Dr. V. D. Patil
MD, D.C.H
, KLE University, J N Medical college,
Belgaum.
Date :
Place : Belgaum
Principal,
Dr. Sanjiv Kumar
KLEU Institute of Physiotherapy,Belgaum
VI
KLE ACADEMY OF HIGHER EDUCATION AND
RESEARCH,
(KLE DEEMED UNIVERSITY)
[Declared as Deemed-to-be-University u/s 3 of the UGC Act, 1956 vide Govt. of India Notification No.F.9-19/2000-U.3 (A)]
(Accredited A Grade by NAAC)
BELGAUM
Copyright Declaration
We hereby declare that KLE Academy of Higher Education and
Research, Belgaum, Karnataka, shall have the rights to preserve, use and
disseminate this thesis in print or electronic format for academic/research
purpose.
Place: Belgaum
Date
Dr. V. D. Patil
M.D., DCH
Mrs. Deepa Metgud M.P.T.
KLE ACADEMY OF HIGHER EDUCATION AND RESEARCH,
BELGAUM
VII
ACKNOWLEDGEMENT
I take this opportunity to thank all those people who have encouraged me right from
the conception of this work till its present form.
This masterpiece, the brainchild of my beloved guide and mentor Dr. V. D. Patil
MD
Dean, K.L.E.U J.N.Medical College, Belgaum, without whose support, timely guidance and
continued inspiration, the mission would not have accomplished. I feel honored in
expressing my sincere gratitude for his valuable guidance.
I express my sincere gratitude to Dr. Dhaded
MD, DM
Professor and Head of
Department of Pediatrics J.N.Medical College Belgaum, for his valuable time, critical
suggestions and consistent support for my research work. Words are inadequate to express
my indebtness and deep respect to him for his able guidance and encouragement.
With great privilege, I take the opportunity to express my heartfelt thanks to
Honorable Chancellor KLE University, Dr. Prabhakar. B. Kore, MLC, Chairman K.L.E
Society for his encouragement and providing the opportunity to reach the goal.
I am grateful to Honorable Vice-Chancellor KLE University Dr. (Prof) C. K. Kokate,
Belgaum, for his timely motivation and inspiration throughout the course.
I am extremely happy to extend my heartfelt thanks to Dr. P. F. Kotur Registrar,
KLEs University Belgaum, for his support and encouragement.
With great respect, I extend my special thanks and gratitude to Mr. Sanjeev Kumar
MPT
, Principal KLEU Institute of Physiotherapy, Belgaum for his continued support,
motivation and encouragement throughout the study.
VIII
My sincere thanks to Shri. M.D.Mallapur, Lecturer Department of Community
Medicine J.N.Medical College, Belgaum, for his valuable time, critical suggestions and
support in statistical analyses. I have no words to express my indebtness for his help and
patience for solving every single doubt about statistics in my work.
With great respect, I extend my special thanks and gratitude to Susan Harris,
Kathaleen Washington, Marcia Swanson and Jean Deitz from University of Washington
USA for their valuable guidance, encouragement and answering all my queries and
supporting me through out the study. It was my privilege to get the guidance from the
international faculty who were pioneers in research on Movement Assessment of Infants.
My sincere gratitude to Dr.Mahesh Kamate Pediatric Neurologist J.N.Medical
College Belgaum, for his valuable suggestions and guidance.
I extend my sincere and special thanks to Dr. Snehal Dharmayat, Dr. Anand
Heggannavar, Dr. Peeyusha, Dr. Arati Ramannavar, Dr. Renu Pattanshetty, Dr.
Santosh.Metgud, Dr. Vijay, Dr. Anil, Dr. Chitra and Dr Basavaraj, staff KLEU Institute of
Physiotherapy for their constant support, suggestion and motivation throughout the study.
I am greatful to my in-laws Smt and Dr.(Shri) S. S. Palled, former Registrar UAS
Dharwad, for their motivation and support throughout my research project. I am greatful to
my mother, brother and husband for their valuable support.
My gratitude to Mr.Raju, assistant at Child Development Centre, KLE Belgaum for
coordinating with me to arrange for the regular follow ups of the study participants.
IX
I am extremely grateful to my Post Graduate students Ms. Sonia, Ms. Sneha, Ms.
Suchitra, Ms. Komal, Ms. Yashoda, Ms. Pallavi, Ms. Neha, Ms Shukhra, and Ms. Namyata
for their every smiling and willing attitude to support me throughout the study.
I thank Mr. Mahesh for the technical help in accomplishing the thesis.
It would be unfair of me if I fail to give heartfelt gratitude to all the children and
parents for participating in the study and making it a success.
I certainly owe my gratitude to my family and for their never ending love, support
and encouragement. This task would not have been completed without the grace of
ALMI GHTY, the most beneficent and most merciful, the best healer.
Place : Belgaum
Date : Dr. Deepa Metgud
X
LIST OF ABBREVIATIONS
AIMS Albert Infant Motor Scale
AR Automatic Reactions
BOMT Bruininks- Oseretsky Test of Motor Performance
BSID Bayley Scale of Infant development
CLD Chronic Lung Disease
CNS Central Nervous System
CP Cerebral Palsy
CS Categorical score
DA Developmental Age
DASII Developmental Assessment Scale for Indian Infants
DDST Denver Developmental Screening Test
DQ Developmental Quotient
ELBW Extremely Low Birth Weight
GA Gestational Age
GM General Movements
HMD Hyaline membrane Disease
IMS Infant Motor Screen
IVH Intraventricular Haemorrhage
LBW Low birth Weight
MAI Movement Assessment of Infants
XI
MDI Mental Development Index
MMCL Meade Movement Check List
MT Muscle Tone
NICU Neonatal Intensive Care Unit
NPV Negative Predictive Value
PD-GMS Peabody Developmental Gross Motor Scale
PDI Psychomotor Developmental Index
PDMS Peabody Developmental Motor Scale
PPV Positive Predictive Value
PR Primitive Reflex
PVHI Periventricular Haemorraghic Infarction
ROP Retinopathy of Prematurity
RS Raw Score
SGA Small For Gestational Age
TIMP Test of Infant Motor Performance
TRS Total Risk Score
VLBW Very Low Birth Weight
VM Volitional Movements
WHO World Health Organization
XII
ABSTRACT
Background and Purpose- With the advances in neonatal intensive care, the survival of
Very low birth weight children has improved considerably in India. However, these children
are at risk for significant motor impairment with poor developmental outcomes. The
Movement Assessment of Infants is a widely used tool to assess motor dysfunction in high
risk infants with good predictive validity for its 4 and 8 months profiles but has no validity
studies for its preliminary 6-month profile. The predictive accuracy of Movement
Assessment of Infants for high risk Indian infants has not been examined at any age. Hence
the aim of this study was to evaluate the validity of the MAI to predict neuromotor outcome
in very low birth weight infants at specific corrected ages of four, six and eight months
during the first year of life.
Methodology- This hospital based prospective observational study consecutively recruited
72 babies with birth weight 1500gms; admitted to Neonatal Intensive Care Unit of which
60 babies completed the one year follow up . The infants were evaluated at 4, 6 and 8
months of corrected age using the Movement Assessment of Infants scale and risk scores
were recorded. A total score of 10 at 4 and 8 months evaluations was considered as risk for
abnormal neurodevelopmental outcome and a score of 6 was considered as risk for 6
month examination. This was followed by evaluation at 12 months using the gold standard
Bayley Scale of Infant Development-II by a clinical psychologist. The Psychomotor
Developmental Index and Mental Developmental Index scores were computed and a score
of 84 was considered as abnormal neurodevelopmental outcome.
XIII
Results- The incidence of neurodevelopmental problems in VLBW infants at one year was
28.33% with 16.66% of them having significantly delayed development. The predictive
validity of 4-month MAI relative to PDI 84 was good with a sensitivity of 82.3%,
specificity 74.4% and Negative predictive Value of 91.4%.The Positive predictive Value
was lower (56%) with higher rate of false positives at 4 months. The 6-month evaluation had
acceptable sensitivity of 70.6% and high specificity of 81.4%. The 8-month evaluation
showed the best combination of predictive values with sensitivity 82.3%, specificity 95.3%,
positive predictive value of 87.5% and negative predictive value of 93.2%.
The risk scores of Movement Assessments of Infants (Total Risk Score and
categorical scores) at four, six and eight months significantly correlated with both the
Motor and Mental scale of Bayley at one year value (p<0.001). The mean total risk score
and categorical scores were significantly higher in infants with abnormal outcome (p<0.001)
compared to normal outcome group. The mean Bayley Mental and Motor scores were
significantly lower for infants with abnormal outcome than abnormal outcome (p<0.001).
Conclusion-The Movement Assessment of Infants has very good predictive validity at all
three corrected ages, but the four and eight month profiles were more sensitive to identify
VLBW infants who would have delayed neuromotor development at one year of corrected
age than the six months profile used.
Key Words- Motor development, Very Low Birth Weight, Movement Assessment of
Infants, Predictive validity, Neurodevelopmental outcome.
XIV
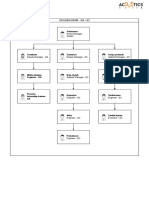
CONTENTS
Sl. No. Sections Page no.
1. INTRODUCTION 1-4
2. RESEARCH QUESTION 5
3. OBJECTIVES 6
4. OPERATIONAL DEFINITION 7 - 8
5. REVIEW OF LITERATURE 9 - 42
6. METHODOLOGY 43 50
7. RESULTS 51 58
8. DISCUSSION 59 73
9. CONCLUSION 74
10. SUMMARY 75 - 78
11. BIBLOGRAPHY 79 97
12. ANNEXURE - I TABLES 98 106
13. ANNEXURE II GRAPHS 107 111
14. ANNEXURE III PHOTOGRAPHS 112 118
15. ANNEXURE IV
ETHICAL CLEARANCE, CONSENT FORM,
PROFORMA
119 124
16. ANNEXURE V
MAI - TEST MATERIAL, DIRECTION FOR
TESTING, RECORDING & SCORING, PROFILE
SHEETS (4, 6 & 8 MONTHS)
BSID II CUE SHEET
125
17. ANNEXURE VI
PUBLICATIONS & PRESENTATIONS
18. ANNEXURE VII
MASTER CHART
XV
LIST OF TABLES
Table No Particulars Pages
01 Maternal Characteristics 98
02 Infant Characteristics 99
03 Neonatal problems during their NICU stay 99
04 Mean scores of MAI at 4, 6 and 8 months 100
05 Mean Mental and Motor scores of BSID-II at 12
months
100
06 Predictive validity of 4 month MAI for neuromotor
outcome at 12 months
101
07 Predictive validity of 6- month MAI for neuromotor
outcome at 12 months
101
08 Predictive validity of 8- month MAI for neuromotor
outcome at 12 months
101
09 Comparison of predictive validity of 4, 6 and 8 months
MAI for neuromotor outcome at 12 months
102
10 Correlation between the 4-month MAI and BSID-II at
12 months
102
11 Correlation between the 6-month MAI and BSID-II at
12 months
102
12 Correlation between the 8-month MAI and BSID-II at
12 months
103
13 Neurodevelopmental problems in VLBW at one year
based on BSID-II score
103
14 Four-months MAI scores of infants with normal and
abnormal neuromotor outcome
103
15 Six-months MAI scores of infants with normal and
abnormal neuromotor outcome
104
XVI
Table No Particulars Pages
16 Eight-months MAI scores of infants with normal and
abnormal neuromotor outcome
104
17 Mean Bayley Mental Scale scores of infants with
normal and abnormal outcome at 12 months
104
18 Mean Bayley Motor Scale scores of infants with
normal and abnormal outcome at 12 months
105
19 Association of MAI and BSID-II scores with maternal
characteristics
105
20 Correlation between the number of days in NICU with
MAI and BSID-II
105
21 Correlation between the number of neonatal problems
with MAI and BSID-II scores
106
XVII
LIST OF GRAPHS
Graph No Particulars Pages
01 Maternal characteristics 107
02 Sex distribution 107
03 Distribution of infants based on gestational age 108
04 Mean scores of MAI at 4, 6 and 8 months 108
05 Mean Mental and Motor scores of BSID-II at 12 months 109
06 Comparison of predictive validity of 4, 6 and 8 months
MAI for neuromotor outcome at 12 months
109
07 Neurodevelopmental problems in VLBW at one year based
on BSID-II score
110
08 Mean MAI scores at 4, 6 & 8 months for infants with
normal and abnormal neuromotor outcome
110
09 Mean Bayley Mental Scale scores of infants with normal
and abnormal outcome at 12 months
111
10 Mean Bayley Motor Scale scores of infants with normal
and abnormal outcome at 12 months
111
XVIII
LIST OF PHOTOGRAPHS
Photograph
No
Particulars Pages
01 MAI Manual and Test material 112
02 BSIDII Manual and Test material 112
03 Plantar grasp 113
04 Extensibility of adductor muscles 113
05 Placing of hands 113
06 Head Righting Lateral 114
07 Landau reaction 114
08 Reach out for object in supine and head centering 114
09 Rolling from supine to side lying 115
10 Prone weight bearing on palms 115
11 Head Righting flexion 115
12 Sits when placed and back straight in sitting 116
13 Equilibrium reactions in sitting 116
14 Walking with one hand support 116
15 Picks up cube 117
16 Finds toy under the cups 117
17 Places cube in cup 117
18 Retrieves toy 118
19 Places circle in the board 118
20 Turns pages of book 118
Introduction
1
INTRODUCTION
Low birth weight (LBW) is a major public health problem worldwide, and the
burden is considerably higher in the developing countries. The percentage of low birth
weight babies in developing countries (16.5percent) is double that of the developed
countries. India alone accounts for 40 per cent of low birth weight babies in the developing
world and more than half of those in Asia.
1
The category of Very Low Birth Weight
(VLBW) infants has an incidence of less than 2% of the births globally.
2
In India, VLBW
infants constitute approximately 4% 7% of all live births and contribute to as much as
30% of early neonatal deaths.
3
Although VLBW is a relatively small proportion of total
births globally, this category of infants accounts for the highest neonatal mortality and
greatest morbidity among newborns.
Low birth weight babies are at high risk of immediate problems like birth asphyxia,
hypoglycemia, convulsions, apnea, sepsis, hypothermia, and feeding problems. They are
more prone for long-term problems such as mental retardation, cerebral palsy, impairment of
lung function, visual and hearing impairment.
Minor neurological deviations like attention
deficit hyperactivity disorder,
4
clumsiness, and intention tremors are also common in them.
They show functional disabilities of 26.7% and the factors associated with functional
disability include neonatal illness, poor weight gain and rehospitalization.
5
With the advances in neonatal intensive care, the survival of VLBW infants (<1500
grams) children has improved considerably. However, these children are at risk for poor
developmental outcomes due to a variety of risk factors associated with preterm and low
birth weight.
6
The proportion of VLBW infants survivors with disabling motor impairments
Introduction
2
is around 8-15%.
7
Cerebral palsy is the most common major neurological abnormality seen
in very low birth weight children. Studies have reported a high prevalence of severe
neurological impairments and minor psychomotor deficits in VLBW infants.
8,9,10,11
They
have problems with fine motor functions ,coordination
12,13
and visual-motor integration.
14
They present with poor quality of motor function and coordination, even without evident
neurological impairment. There is increased risk of delayed attainment of walking in these
children.
15
This indicates that the presence of motor dysfunction due to very preterm and
VLBW may crucially affect the childs exploration of the world, attainment of handwriting
skills, and involvement in social activities.
16,17,18
Due to this effect on adaptive functioning,
impaired motor development is a risk factor for later poor cognitive performance,
19,20
learning disabilities, and behavior problems.
21,22,23
This clearly highlights the need for an
accurate and early prediction of motor consequences of very premature and VLBW infants.
This has led to development of extensive follow up programs worldwide to
determine which of these infants needs intervention. Early identification of motor
dysfunction in monitoring programs are essential to implement appropriate intervention as
the infants brain development and myelination are rapid in first year of life.
24
Numerous tools like Gesell Development Schedules Test,
25
Peabody Developmental
Motor Scales,
26
Denver Developmental Screening Test,
27
and Bayley Scale of Infant
Development
28
have been developed to assess motor development in children.
Physiotherapists have been increasingly involved in using these tools as they are primarily
concerned with motor behavior. An important limitation of the vast majority of the existing
tools is that they focus on the acquisition of motor milestones and lack the sensitivity in
Introduction
3
identifying infants with subtle movement disorders. The development of an infant refers to
both qualitative and quantitative changes for optimal functioning. An infant may show
clinical improvement in pattern and quality of movement, but this may not be reflected in
the acquisition of motor milestones. In order to improve the accuracy of early identification,
tests of motor development for infants should include quality of movement component.
29, 30
The neuromotor tools that assess quality of movement like Alberta Infant Motor
Scale
31
Test of Infant Motor Performance,
32
and General Movements
33
primarily focus on
gross motor development and do not include fine motor and neurological components
necessary for performance of motor function. Tools which are based on normative data are
not suitable to identify neuromotor dysfunction in preterm VLBW infants as they have
variations in motor development although that may not necessarily be abnormal.
34
For this
reason, criterion-referenced tools designed specifically for preterm infants to discriminate
between typical and atypical development are appropriate in children with variation in motor
patterns of development.
The Movement Assessment of Infants (MAI) Scale addresses most of the limitations
of the traditional diagnostic tools and the currently developed motor performance tools.
Hence it was considered as an appropriate tool and was used in the present study to identify
neuromotor dysfunction.
The MAI is a landmark tool and a sensitive measure of quality of movement in high
risk infants as early as four months of age. It is a criterion referenced scale with risk profiles
available for four, six and eight months of age that can appropriately measure movement
performance even in preterm infants with variation in motor development. It is a potentially
useful and cost-effective assessment tool .It has been shown to be sensitive and specific for
Introduction
4
detecting neurological disorders at four and eight months in both pre term and term
infants.
35,36,37
In India comprehensive assessment tools that focus on acquisition of motor milestones
are used in monitoring programs for high risk infants. There is no much published evidence
on the use of motor tools that measure quality of movement performance except the one
published on the use of Infant Motor Screen tool in early intervention program for high risk
infants.
38
Predictive validity of MAI has been established for the originally developed 4 and 8
months profiles for high risk infants like preterm, low birth weight, cocaine abuse and
infants at social risk in western countries.
39,40,41
Although literature demonstrates the clinical
utility of the MAI with good predictive validity, its applicability for Indian infants with
VLBW has not been studied at 4 or 8 months.
Babies can report at any age for developmental concerns and may require sequential
longitudinal assessments rather than single assessment. Despite the availability of the
published preliminary 6-month MAI profile based on normal term infants its predictive
validity for neurodevelopmental outcome in high risk infants has not been explored either in
Indian or western population.
42
This limits the clinical utility of the tool. Hence this study
was undertaken in an effort to evaluate the validity of MAI at 4, 6, and 8 months of
corrected ages to predict neuromotor outcome in Indian population of VLBW infants and
broaden the scope of use of MAI in clinical practice.
Research Question
5
RESEARCH QUESTION
What is the validity of the Movement Assessment of Infants tool for predicting
neuromotor outcome in very low birth weight infants at specific corrected ages of
four, six and eight months during the first year of life ?
Objectives
6
OBJECTIVES
Primary Objective:
To assess the validity of the Movement Assessment of Infants for predicting
neuromotor outcome in very low birth weight infants at specific corrected ages of
four, six and eight months during the first year of life.
Secondary Objective:
To determine the incidence of neurodevelopmental problems in very low birth
weight infants during the first year of life.
Operational Definition
7
OPERATIONAL DEFINITIONS
Age of mother: Age was recorded to the nearest completed years.
Primary education: The person who had studied from first to seventh standard.
Secondary education: The person who had studied from eighth to tenth standards.
Higher secondary: The person who had studied from 10th to 12
th
standard.
Graduate: Bachelor degree
Postgraduate: Masters degree
Socioeconomic status: Socioeconomic status was based on per capita income in
rupees per month and was classified using the modified BG Prasad classification.
Modified B. G. Prasad Classification
Socioeconomic
class
Modified Prasad's classification in the study period 2009.
Per capital per month income (Rs.)
I 3600 & Above
II 1800 & 3599
III 1080 & 1799
IV 540 & 1079
V <540
Operational Definition
8
Age of baby: Chronological age: Date of testing minus date of birth.
Corrected Age: Chronological age minus Days of prematurity
Days of prematurity- (40 weeks minus gestational age in weeks)X 7
Gestational age: Age or duration of the gestation, from the last menstrual period to
birth.
Birth
o Term birth: Delivery occurring between 37 and 42 weeks of gestational age.
o Preterm birth: Delivery occurring before 37 weeks of gestational age.
Birth weight
o Low-birth-weight infant: Infant with birth weight less than or equal to 2500
grams, regardless of gestational age.
o Very Low birth weight-Infant with birth weight between 1000 to 1500
grams regardless of gestational age.
Review of Li terature
9
REVIEW OF LITERATURE
MAGNITUDE OF THE PROBLEM
Low birth weight has been defined by the World Health Organization (WHO) as
weight at birth of less than 2,500 grams (5.5 pounds).
43
Low birth weight neonates are
further classified as very low birth weight (VLBW <1500 g) and extremely low birth weight
(ELBW <1000 g) infants. Newborns with a birth weight (for gestational age) of less than the
10
th
percentile are categorized as small for date (SFD). Some pediatricians use two
standard deviations below the mean weight for gestational age as a cut-off point for defining
LBW. Thus, the term LBW includes pre-term babies (those born before 37 weeks of
gestation), as well as full term babies who are small for date due to intra-uterine growth
retardation.
1
Globally, more than 20 million infants or 15.5 per cent of all births, are born with low
birth weight. More than 95 per cent of low birth weight babies are born in developing
countries.
1
Global incidence of LBW according to WHO states that Bangladesh has the
highest incidence of 30 percent and Indian ranks second with 26%.
44
The institution based
National Neonatology Forum data for the year 1995 on 37082 live births (nearly 0.1% births
in the country) from 15 participating centers reported a LBW prevalence of 32.8% .The
prevalence of babies with birth weight <2000 g was 10.2%, <1500 g was 3.3% and <1000g
was 0.7%.
45
As per WHO report each year, more than three million children die in the neonatal
period. Newborn, deaths account for 37% of all deaths among children under five. The
majority of all neonatal deaths (75%) occur during the first week of life, and of those deaths,
Review of Li terature
10
25% to 45% occur within the first 24 hours. The main causes of newborn deaths are
prematurity and LBW (30%), infections (25%), asphyxia and birth trauma (23%). These
causes account for nearly 80% of deaths in this age group. Close to 25,000 children die
every day, mostly due to pneumonia, diarrohea and newborn problems.
46
The factors influencing LBW of baby include short gestational period, socio economic
standard, nutritional status and environmental factors. Low birth weight continues as an
important social health problem. It is one of the most serious challenges in maternal and
child health in both developed and developing countries. It is the single most important
factor that determines the changes of child survival.
NEONATAL PROBLEMS AND ITS ASSOCIATED RISK IN VLBW INFANTS:
VLBW infants face immediate serious health problems as newborn and also later
long term developmental problems. Low birth weight infants could be preterm or small for
gestational age and are prone for multisystemic complications during neonatal period and
may have long-term implications.
48
The following are the most common problems in VLBW
infants which are associated with potential risk of poor developmental outcomes :
Delivery Room Care and Resuscitation
Premature infants require additional special care in delivery room such as
precautions to prevent heat loss because of thinner skin and an increased surface area to
body-weight ratio, respiratory support for apnea due to respiratory insufficiency which is
more likely at lower gestational age. Depending on the reason for premature birth, perinatal
infection is more likely in premature infants, which increases their risk of perinatal
depression. Preterm and IUGR babies are at risk of meconium aspiration and birth asphyxia
and may require to be delivered by cesarean section and may be depressed at birth.
49
Review of Li terature
11
Hypothermia
Hypothermia in newborns is commonly due to lack of awareness and knowledge
about the importance of maintenance of temperature amongst the health care personnel, than
due to lack of equipment. In the developing countries, hypothermia contributes significantly
to neonatal morbidity and mortality. The low birth weight infant is particularly at increased
risk of hypothermia because of larger surface area to weight, increased transepidermal water
loss, increased exposed area, thin and immature skin, increased cutaneous blood flow,
decreased energy stores, less brown fat, limitation of oxygen consumption because of
pulmonary problems and increased respiratory rate.
49
Hypoglycemia
Hypoglycemia is common in VLBW due to their poor ability to breast feed
immediately after delivery because of poor oromotor control and reduced respiratory effort.
They are more prone to get neonatal seizures which may cause neurological damage.
Neonatal hypoglycemia, independent of HIE, has been associated with adverse
outcome in both term and preterm infants.
50
However, no conclusive evidence on the
severity and duration of hypoglycemia causing brain damage has been reported.
51, 52
A study was done to find the adverse neurodevelopmental outcome of moderate
neonatal hypoglycemia in a multicentre trail of 661 preterm infants. The number of days on
which moderate hypoglycemia occurred was strongly related to reduced mental and motor
developmental scores at 18 months , even after adjustment for a wide range of factors
known to influence development. The mental and motor developmental scores at 18 months
(corrected age) were significantly reduced and the incidence of neurodevelopmental
impairment (cerebral palsy or developmental delay) was increased. These data suggest that,
Review of Li terature
12
contrary to general belief, moderate hypoglycemia may have serious neurodevelopmental
consequences, and reappraisal of current management is urgently required.
53
Prospective serial evaluation was done on 85 small for gestational age preterm
neonates with hypoglycemia to investigate the effects of neonatal hypoglycemia on physical
growth and neurocognitive function They found that recurrent hypoglycemic episodes were
correlated with neurodevelopmental and physical growth deficits till five years of age and
long term effects.
54
Respiratory
In preterm VLBW infants respiratory difficulties constitute the commonest cause of
morbidity and pulmonary pathology is the most frequent autopsy finding; the commonest
conditions in this group include aspiration, infections, HMD, massive pulmonary
hemorrhage, pneumothorax and congenital malformations.
A retrospective case-control study was done to describe the clinical course, neonatal
morbidity, and neurodevelopmental outcomes of VLBW children who develop pulmonary
hemorrhage. They found that pulmonary hemorrhage occurred in 5.7% of the total
population of VLBW infants. There were no significant differences in neurodevelopmental
outcomes at 20 months' corrected age. It was concluded that although mortality is high,
pulmonary hemorrhage does not significantly increase the risk of later pulmonary or
neurodevelopmental disabilities among those who survive.
55
Premature infants may adapt poorly to air breathing and present with perinatal
depression in the delivery room. Respiratory distress syndrome may occur because of
surfactant deficiency in babies <34 weeks of gestation and the incidence is inversely
proportional to the gestational age of the newborn.
56
Review of Li terature
13
Apnea may occur because of immaturity of the mechanisms controlling breathing
and ineffective ventilation.
57
Meconium aspiration syndrome is commonly the result of fetal
distress and is frequently associated with small for gestational age babies.
58
Finally oxygen
therapy for respiratory distress needs to be monitored as it has its long term side effects.
59
Low Apgar
Low birth weight and immaturity are associated with a low Apgar score.
60
More
recent studies have found a strong association between low Apgar score and cerebral palsy
in children born at term or with normal birth weight
61, 62
whereas studies in children with a
low birth weight or born preterm have shown conflicting results.
63,64
In a population based
cohort study the low Apgar score was strongly associated with cerebral palsy. This
association was high in children with normal birth weight and modest in children with low
birth weight.
65
Cardiovascular
Premature infants may present with hypotension due to hypovolemia, cardiac
dysfunction and vasodilatation due to sepsis. Patent Ductus Arteriosus is common and may
lead to congestive heart failure.
Gastrointestinal
Prematurity is single greatest risk factor for necrotizing enterocolitis.
66
Feeding
problems are common in LBW babies because of immaturity of the suck-swallow-breathing
coordination.
67,68
Renal
The preterm babies are characterized by low glomerular filtration rate, an inability to
handle water, solute and acid load because of immature kidneys. Therefore fluid and
electrolyte management can be difficult.
Review of Li terature
14
Hematological
Polycythemia is common in babies who are small for gestational age secondary to
placental insufficiency and chronic hypoxia. Anemia and hyperbilirubinemia are other
hematological problems in preterm VLBW infants. Anemia is frequently seen in preterm
babies because of decreased RBC mass and iron stores. Infants needs extra concern as iron
is actively transferred from mother to fetus during pregnancy, the maximal time of transfer
being during the third trimester. As a consequence the premature infant is born with
relatively lower iron stores depending on the gestational age. Iron deficiency causes varying
degrees of impairment in cognitive performance; reduced psychomotor skills and lower
immunity to infections.
69
Premature babies are more likely to develop hyperbilirubinemia
and can develop kernicterus at low levels of bilirubin.
70
Poor weight gain
The low birth weight babies frequently show an exaggerated weight loss and slower
rate of weight gain in the postnatal period due to inadequate calorie intake, frequent
illnesses, hypothermia and sepsis.
71
Infections
Low birth weight infants are particularly vulnerable to infections because of epidermal
barrier immaturity, poor defense mechanisms, interventions and procedures carried out for
routine monitoring and treatment.
70
Rate of infection increases with decreasing gestational
age. Moreover, postnatal infection is associated with an increased risk of neonatal
complications, prolonged hospitalization, and death.
Review of Li terature
15
In a cross sectional study to know the incidence, presenting features, risk factors and
significance of late onset septicemia in very low birth weight infants it was found that
sixteen percent of VLBW infants developed septicemia at a median age of 17 days. Factors
associated with septicemia included male gender, lower gestational age, birth weight and
decreased baseline serum IgG concentrations. Septicemia infants, compared with non
septicemia infants, had significantly increased mortality, longer hospital stay and more
serious morbidity. They concluded that late onset septicemia is common in very low birth
weight infants, and the rate is inversely proportional to gestational age and birth weight.
72
A
casecontrol study found that prematurity and neonatal infection were the dominant factors
associated with neurological morbidity in VLBW infants.
73
Neurological
The main causes of newborn deaths are prematurity and low-birth-weight (30%),
infections (25%), asphyxia and birth trauma (23%). Combinations of antenatal and perinatal
problems rather than single event, in combinations with suboptimal socioeconomic and
environmental conditions in infancy, contribute most to poor long term neurodevelopmental
outcome. LBW babies are more prone for perinatal depression, seizures and intracranial
bleeds that may have long term implications.
74
The incidence of severe perinatal asphyxia in resource-rich countries, (causing death
or severe neurological impairment) is about 1/1000 live births
75
where as in resource-poor
countries, the incidence is about 5 to 10/1000 live births.
76
It is inversely related to
gestational age and birth weight. The factors that increase the risk of perinatal asphyxia
include decreased blood flow from mother to placenta or placenta to fetus, fetal anemia,
infection severe cardiac and circulatory insufficiency. It causes increased ICP or cerebral
Review of Li terature
16
edema which often reflects extensive prior cerebral necrosis rather than the swelling of
intact cells. It carries poor prognosis. The risk of the CP in survivors of perinatal asphyxia is
5% to 10% compared to 0.2% in the general population.
Seizures occur in 20 to 50% of preterm infants and usually start between 6 and 24
hours after the insult. Neonatal seizures are the clinical manifestation of serious underlying
neurologic disease and can cause additional brain injury. About 45% have mild to severe
disabilities (25% neuromotor, 20% sensory). Recurrent seizures occur in approximately
20%. The worst prognosis is for infants with tonic seizures, seizures resulting from IVH or
hypoxic ischemic encephalopathy and seizures lasting more than three days (66%).
77
Periventricular leukomalacia is necrosis of the cerebral white matter dorsal and
lateral to external angle of the lateral ventricles. In premature infants especially the ill ones
have pressure passive cerebral circulation. The periventricular region is particularly
vulnerable to ischemia because arterial border and end zones are vulnerable to decreased
perfusion pressure and decreased cerebral blood flow.
78
Periventricular hemorrhagic infarction (PVHI) is most common in the premature
infants. It is characterized by a large region of hemorrhagic necrosis in the periventricular
white matter that is usually unilateral or bilaterally asymmetric. The overall incidence of
IVH in premature infants is approximately 30%, but it can be over 70% in ELBW infants
weighing less than 750 gm at birth.
79
A case control study was done to identify factors during the neonatal period in babies
born at term and preterm that are associated with the subsequent development of cerebral
palsy (CP). They found that seizures, congenital abnormalities of the brain and elsewhere,
Review of Li terature
17
'other lesions', abnormal muscle tone and meconium aspiration were common in term
babies. Among babies born preterm; seizures, IVH, periventricular leukomalacia, 'other
lesions' and abnormal muscle tone were seen. They concluded that the neonatal factors
which best identify neonates who will subsequently develop CP are different for term and
preterm babies.
80
Visual problems
Visual function of LBW children is poorer than that of normal birth weight babies.
The vision is a crucial determinant of early motor and cognitive development. They are at
increased risk for retinal and non retinal ophthalmic disorder that leads to visual disability.
The degree of visual impairment correlates very strongly with degree of neurodevelopmental
impairment. The VLBW infants are also at increased risk of developing severe retinopathy
of prematurity (ROP).
81
These children with the most severe ROP have disproportionately
high rates of severe multiple developmental disabilities and severe functional
limitations.
82
Severity of neonatal ROP seems to be a marker for functional disability at age
5.5 years among very low birth weight survivors. High rates of functional limitations in
multiple domains occur in children who had threshold ROP, particularly if they have
unfavorable visual acuity.
83
This evidence emphasizes the importance of ocular assessment of LBW children
with CNS damage and neurodevelopmental assessment in LBW children with visual
disabilities. Studies done on the impact of LBW on the visual pathway showed that
impairments was highest for those under 1500 grams, decreasing with increasing birth
weight for those over 3500 gms.
84, 85
Review of Li terature
18
Hearing loss is more likely in premature babies. Strong evidence indicates increased
risk of speech and language delays in LBW babies. There is 25% incidence of language
delay among premature
infants with birth weight at <1500 g. However studies have shown
that
hyperbilirubinemia, defined as peak total serum
bilirubin level or duration of elevated
bilirubin in days, is
not associated with language delay in premature infants.
86
NEURODEVELOPMENTAL PROBLEMS AND THEIR OUTCOME IN VLBW
INFANTS
Reports from developed countries world wide describing the outcome for infants of
very low birth weight, born since 1946 showed that, the mortality rates and prevalence of
major handicap in survivors were high until 1960 because of inadequate treatment and
knowledge of neonatal diseases. In the late 50's and 60's, knowledge concerning the normal
physiology of VLBW infants and derangement which cause death and damage in newborns
increased. Treatments were developed and mortality rate started declining but at the expense
of increased prevalence of handicap at a rate 6-8% of VLBW live births.
87
A study in 1977 done to find the Outcome of infants of very low birth weight treated
in neonatal intensive care unit showed that the improvement in neonatal care was associated
with a decrease in the incidence of major neurological sequele from 21.1% to 12.2%
between 1961 and 1973. There was decrease in incidence of cerebral palsy, epilepsy and
mental retardation. They suggested that improvement in perinatal care is likely to further
reduce the incidence of major handicaps.
88
In India three major longitudinal studies on outcome of LBW babies has been carried
out. The first one was a hospital-based study in Delhi.
89
The study showed retardation in
Review of Li terature
19
motor, adaptive, and personal social and language development in first 5 years, further
studies between 6-10 years for intelligence, academic achievement, behavior orientation
confirmed the previous results of disadvantage of being born LBW. Though the LBW had
test results within normal range, they scored significantly less than the controls.
Another hospital- based study where in children born during 1983-1989 were followed
up to 1995 with a mean age of 8.5 years.
90
The follow up of unimpaired survivors along with
matched normal weight children revealed that LBW children had significantly lower scores
for tests of intelligence, visuomotor co-ordination. Also neurological soft signs, behavior
problems and learning disabilities were more in LBW infants. Follow up of preterms during
first 18 months revealed that out of 150 LBW followed up, 7.0 % had developmental delay,
4 % had cerebral palsy and 10% had transitory dystonia which resolved by 18 months. Pune
study showed that the LBW children are at disadvantage for poor visuomotor co-ordination,
reading, writing and mathematical skills.
91
A cohort study at a tertiary care neonatal service in Delhi, was undertaken to
determine the neurodevelopmental outcome of neonates who required intensive care. They
observed that 85% of subjects had normal neurodevelopmental outcome, and 15% had
adverse outcome. Among the neonatal risk factors, seizures, sepsis and hypoxic ischemic
encephalopathy had a significant association with adverse outcome. Despite serious neonatal
morbidity, the early neurodevelopmental outcome of nursery children was reasonably
good.
92
The longitudinal and cross-sectional studies on the cognitive development of 83
children of VLBW, ages three
to seven years, were evaluated on the McCarthy Scales of
Review of Li terature
20
Children's
Abilities. The factors related to lower cognitive scores included
neurological
complications during hospitalization
in the NICU, the child's age, and the mother's level
of
education. In the cross-sectional study,
the VLBW children were compared with control
groups of children from middle class families (MC) and lower
class families (LC). The
VLBW group scored significantly
lower than the MC group on all the McCarthy scales, but
did not differ from the LC group.
93
A study was conducted to document the psychomotor development and general health
of former VLBW infants born between 1980 and 1986 from birth up to school age in Central
Switzerland and found that 1/5th of these infants had transient motor problems treated by
physical therapy. Twenty-three percent of the infants seen in follow-up had persistent but
mainly minor motor handicaps, and only two infants (2%) had multiple handicaps. Ninety-
six percent attended regular school, but almost half of them had significant school problems
and required professional help.
94
A recent comparison made in various European, American
and Australian Centers reveals an average of 7% of cerebral palsy and 15% of mental
retardation among VLBW infants.
47
In a study on development of healthy VLBW preterm infants they found that even if
they are healthy as a group, they suffer from a larger proportion of developmental
difficulties in comparison to the general population. Their academic, social and behavioral
achievements are lower as a group than full term infants. The source of the developmental
risk factors is both biological and environmental in origin. It is hypothesized that the source
of these risk factors is at least partially due to differences in the development of specific
brain areas such as the hippocampus.
95
Review of Li terature
21
A study was done in Chandigadh on the neurodevelopmental and behavioral
assessment of VLBW at corrected age of 2 years and they found that 17% of the children
had mean MDI score of <70 and 25.7% had a mean PDI of <70.
96
A Meta-Analysis of studies published between1998 and 2008 was carried out to find
the neurobehavioral outcomes in Very Preterm and VLBW children in terms of academic
achievement, behavioral functioning, and executive functions. The analysis showed that
very preterm and/or VLBW children scored lower on mathematics tests, reading tests, and
spelling tests than term-born peers. Among all the behavioral problems, attention problems
were most pronounced in these children compared to the controls as per the teacher and
parent ratings .There was decrease in Executive Functions (EF) as observed by decreased
score in verbal fluency, working memory, and cognitive flexibility in comparison to
controls. All the neurobehavioral outcome measures showed strong and positive correlations
with mean birth weight and mean gestational age.
97
A cohort of 78 VLBW infants were followed prospectively to determine the impact of
birth weight, age of assessment, and skill area on their developmental performance based on
the Griffiths Mental Scales of Development at 6, 12, 24, and 36 months of age. A significant
age and skill interaction was found, with the locomotor and eye-hand skills decreasing
consistently over time, and the personal-social, hearing and speech skills initially decreasing
and then rising from 12 to 36 months.
98
A study on Growth of Very Low Birth Weight Infants to age 20 years found that
VLBW females catch up in growth by 20 years of age whereas VLBW males remain
significantly shorter and lighter than controls. Since catch-up growth may be associated with
Review of Li terature
22
metabolic and cardiovascular risk later in life, these findings may have implications for the
future adult health of VLBW survivors.
99
Studies examined Quality of life in preschool-aged
children who were born at VLBW and/or preterm. Significant differences in physical
functioning between study groups and controls were found in those studies, most notably in
motor functioning,
100,101
with poorer performance by the preterm and/or VLBW children.
The Social functioning was found to be significantly lower for preterm and VLBW
preschool-aged children compared with those in the control groups.
103,104
In some studies,
there was no significant difference between the 2 groups in emotional functioning,
103,104
whereas in others, preterm children were significantly more anxious than those in the control
groups.
100,101
Studies explored Quality of Life in preterm adolescents and term peers using the
Health Utilities Index, and the Child Health Questionnaire. They found that the VLBW
teenagers did not rate themselves as significantly different from their peers on a generic
health measure.
Parents of VLBW teenagers with low IQ indicated that their children
performed significantly lower in terms of global health and behavior, general health
perception, self esteem, and family activities.
105,106
A Meta-analysis of motor development in Very Preterm and VLBW Children was
done to investigate the relationship between very
preterm birth and VLBW with motor
development. The results of the analysis were in comparison with term-born peers, very
preterm
and VLBW children obtained significantly lower scores on all
3 motor tests that is
the BSID-II,
Movement Assessment Battery for Children and BOTMP, indicating that
Review of Li terature
23
preterm or VLBW is associated with
significant motor impairment persisting throughout
childhood.
107
In a study on the developmental profile of 61 very low birth weight infants
without
major cognitive, motor, or sensory deficits compared
with that of 28 term infants at 1 year
chronologic age found that the VLBW
infant's motor performance significantly correlated
with bronchopulmonary
dysplasia, intracranial hemorrhage, and number of days spent
in the
hospital.
108
A longitudinal study on was done to evaluate the stability of motor development and
its association with birth weight , gestational age at birth, intraventricular haemorrhage ,
periventricular leucomalacia and retinopathy of prematurity till 5.5 years found that fifty-
three percent of the VLBW infants displayed a stable motor development. Only
periventricular leucomalacia and birth weight contributed significantly to the variability in
their motor performance. Forty-seven percent of the infants exhibited an unstable motor
development with no association to risk factors.
109
In a study on the characteristics of the VLBW babies suggested that they have an
increased risk for developmental delays and are apt to have difficult behavioral styles. There
was a negative relationship between infants with difficult behavioral styles and maternal
involvement and responsivity.
110
A study in Canada examined school performance at 8 years of preterm, small for
gestational age VLBW infants compared to that of VLBW children born appropriate for
gestational age. The IUGR children did not differ in school performance when compared to
Review of Li terature
24
either birth weight- or gestational-age-matched controls. All the VLBW groups had
significantly inferior outcomes when compared to a normal-birth weight control group.
111
The age of gross motor milestone attainment and how it is affected by degree of
prematurity at delivery were studied in 100 high-risk, preterm (<32 weeks) infants with
normal motor outcome and found that very preterm infants can be expected to demonstrate
sequential gross motor development at a rate expected for degree of prematurity.
Chronologic age is not a valid measurement scale to use in determining motor delay in very
preterm infants.
112
The assessment of motor development in 89 VLBW infants at 4, 8 and 12 months
chronological age was done to describe the acquisition of gross and fine motor skills in these
infants. They concluded that the developmental pathways whereby milestones are achieved,
during first 12 months appear to be different in VLBW and full term infants and so the
standardized instruments used for assessment of term infants may not be serving well for
VLBW infants.
113
A cohort study on very preterm infants with birth weight <1500g to assess the value of
term neurological examination and cranial ultrasound in the early prediction of neurological
outcome at 12 months corrected age, found that neurological examination of preterm babies
at term may be unreliable for prediction of neurological outcome at 12 months CA. This
was because most of the infants who had suboptimal total neurological scores at term went
on to have optimal neurological scores at 12 months CA. For early prediction of
neurological outcome cranial ultrasound examination was found to be more reliable.
114
A
Review of Li terature
25
review of published studies of infants born between 1960 and mid-1980s weighing less than
1500g at birth concluded that the median CP rate in all cohorts was 7.7%.
115
The epidemiological study on sensorineural impairment in very premature infants
reports that the prevalence for CP remained unchanged in extremely and very preterm
infants since 1990. The prevalence estimates of moderate and severe cognitive impairments
were 15 to 25% in very preterm children.
116
In the USA among the 80% survivors of
VLBW, 5-15% develop cerebral palsy.
117
Literature overwhelmingly supports that the risk of CP and major neurologic disability
is increased among VLBW infants compared to full-term infants. The literature is consistent
in demonstrating that risk of CP or major neurosensory and/or neurologic disability is
inversely proportional to the degree of immaturity whether measured by gestational age or
by birth weight. The incidence of CP is currently stable compared to the 1980s (710%
VLBW infants; 717% ELBW infants) or modestly decreased despite improved survival of
extremely immature infants. This suggests that recent advances in neonatal care have had
either no or modest effect on further reduction in the incidence of Cerebral palsy. Studies
have demonstrated that the risk of major neurosensory or neurologic disability might range
from 1250 percent among VLBW and ELBW infants. Despite the stable risk of Cerebral
Palsy, the risk of disability primarily to visual disabilities has increased since the 1980s.
Differences among studies regarding the incidence of Cerebral Palsy, neurologic, and
neurosensory disability may be accounted for differences in the criteria for
neurologic/neurosensory disability, the era of study, the degree of immaturity, and other
characteristics or risk factors of the patient population, neonatal care practices, as well as
length and completeness of follow-up.
118
Review of Li terature
26
A three year follow up study was done to find the neurologic sequelae in high risk
infants discharged from the Neonatal Special Care Unit (NSCU) of a referral hospital in
Pune. The Amiel-Tison Method, Bayley Scales of Infant Development and Raval's Scale for
social maturity were used to evaluate the babies and reported a low incidence of handicap in
their sample which could be due to good antenatal and perinatal care.
119
Considering the extent and severity of various neurodevelopmental problems in
VLBW infants, early identification of the problems is very essential both for healthy and
risk VLBW infants in order to start timely intervention and prevent long term disabilities.
SCALES FOR ASSESSMENT OF NEUROMOTOR DEVELOPMENT
Developmental scales are used as screening tools which promotes early intervention
for deviation from the normal growth and development in young children. It can assist in
determining the diagnosis. It facilitates early identification of deviation; provide the
anticipatory advice to parents, clinicians and caregivers for future planning. It is helpful for
early recognition and focused plan for intervention which may prevent severe disability. It
facilitates the planning of a treatment program. It provides important information about the
level of operation of the child and milestones achieved. The test results may help the parents
to understand the child limitations, what can and cannot be expected makings it possible to
establish common goals and to plan for the future. The report of testing may reveal specific
areas of deficit that require additional evaluation to discover the underlying cause of the
delay. Sequential tests reveal the rate and trend of development of a child. It can be used to
monitor the progress and determine whether and when the child has achieved the goals.
Screening tests are intended to differentiate between those persons who are normal
and healthy in a particular aspect from those who are not.
Review of Li terature
27
Milani-Comparetti motor development test
120
It is a screening test of motor development that evaluates infants on the basis of a
correlation between the functional motor achievements of the child and underlying reflex
structures. Test age for the scale is from birth to approximately two years of the age. During
the test the examiner physically manipulate the child for a particular motor response. Parents
can provide the information if the child is uncooperative. Experienced observes can do the
test in four to eight minutes.
The summaries of reports are shown by a vertical alignment of notations that is
consistent with the childs chronological age. A wider scattering of lines is an indicator of a
more severe, a possibly more specific motor dysfunction such as cerebral palsy. Test-retest
reliability results showed percentage agreement ranging from 82 to 100%. This screening
test can be done quickly and does not require any special equipment or setting. It can
provide early evidence of neuromotor delay of deficits.
Denver Development Screening Test (DDST)
27
It is used to screen for developmental delay. The Denver II screens general
development in five areas such as personal, social, fine motor adaptive, language, gross
motor and behavior. It is used to test children between birth to six years. The mean examiner
observer reliability was found to be 0.99. The test administration and scoring is done quickly
and the test is acceptable for both children and parents. This test is excellent for identifying
children who are at risk for developmental problems and for monitoring a child
longitudinally. The validity of this test in children below 30 months has been questioned.
121
Review of Li terature
28
Alberta Infant Motor Scale (AIMS)
31
It measures gross motor maturation in infants from birth (term 40 weeks post
conception) through independent walking (0 to 18 months of age). The focus of the
assessment is an evaluation of the sequential development of postural control relative to four
postural positions supine, prone, sitting and standing. The interrater reliability is 0.99 and
test - retest reliability is 0.99. The advantage of the test is it provides the ability to detect, as
early as possible, any deviation from the normal, thereby permitting early intervention to
minimize the effect of dysfunction. Although it has good concurrent validity, but its
predictive validity for major developmental disorders is only moderate.
122
The other
limitation of the tool is it only evaluates gross motor behavior.
Amiel Tison test
123
It was developed by Amiel Tison and Gosselin and is applicable for high risk infants.
The target population includes one month to six years. It is based on traditional
neuropediatric concepts (French School).It includes assessment of active and passive muscle
tone, reflexes, spontaneous motor behavior and qualitative abnormal behavior.
123
It is a pure
neuromotor test and does not take into consideration the mental development of the child at
all.
122
Infant Motor screen (IMS)
124
IMS consists of 25 test items which assess muscle tone, primitive reflexes, automatic
reactions and asymmetry of motor skills. It is designed to be administered initially at 4
months and is useful till the development of independent walking. This test aids in
identifying early motor development and risk of abnormal development. There are three
Review of Li terature
29
levels of scoring: the test score, the item score and the test rating. The test rating is 0-9
points as normal, 10-14 points as questionable and 15 and above points as abnormal
development. A study has been done in Indian high risk infants using IMS and DDST at 4
and 8 months and the neurodevelopmental outcome was tested against BSID. They
concluded that both IMS and DDST have high accuracy in identifying neurodevelopmental
abnormalities.
38
Test of Infant Motor Performance (TIMP)
32
TIMP is a functional motor scale for newborns and infants less than four months of
age. It has 59 items with observed scale items of 28, dichotomously scored and elicited scale
of 31 items scored on five, six or seven point scale. The observed scale examines infants
spontaneous movements such as head centering and individual finger, ankle and wrist
movements. The elicited scale tests the infants movement responses to placement in various
positions and to interesting sights and sounds. The maximum possible raw score is 170, and
the test can be used in infants from 32 weeks post-conceptional age through four months
post term. The purpose of TIMP is identification of children with developmental motor
delay and has test-retest reliability of 0.89.It has good construct and concurrent
validity.
125,126
Limitation of the test is its applicability beyond four months of age , addresses
only gross motor behavior and requires training for administration.
General Movements (GMs) Assessment
33
It is more recently developed tool by Prechtls in 2004 for preterm infants to be used
from birth to four months of age. It is a criterion referenced tool used to discriminate and
predict neuromotor abnormalities. The test components include spontaneous movement and
neurological integrity. The infants spontaneous movements are videotaped and then scored.
Review of Li terature
30
It is good predictive tool but needs compulsory training to use from the general movements
trust which limits its clinical and research utility.
122
There are others scales like, Posture and Fine Motor Assessment (PFMAI),
127
Toddler
and Infant Motor Examination (TIME)
128
and Neuro Sensory Motor Development
Assessment (NSMDA)
29
which are used to assess motor performance in risk babies.
Peabody Development Motor Scale
26
It provides a comprehensive sequence of gross and fine motor skills. Children from
birth through 83 months of age are included. Test retest reliability is 0.99 for fine motor and
gross motor scales. The disadvantage of this tool, is it does not provide all of the items
necessary for administration of the fine and gross motor scales.
Gesell Development Schedules Test
25
It assesses behavior in the areas of adaptive, gross motor, fine motor, language and
personal social development. The test is appropriate for children ages of one month to 36
months. The test retest reliability is reported to be 0.82. The disadvantage of the test is that it
requires extensive practice and use in order to ensure valid results.
Developmental Assessment Scales for Indian Infants (DASII)
130
It is an Indian adaptation of Bayley Scale of Infant Development. It is standardized for
children of Baroda and is culturally relevant. It measures motor and mental development
from birth to 30 months. It provides overall motor and mental scores and in addition
indicates the specific clusters of delay in areas of motor and mental development. A study
was done in Chandighar on the neurodevelopmental and behavioral assessment of very low
birth weight babies (VLBW) using DASII at 18 months. They found that 17% had mental
Review of Li terature
31
developmental quotient and 25.7% had motor developmental quotient score <70 in VLBW
babies based on DASII evaluation.
91
The study done on 30 neonates to compare changes in
apparent diffusion coefficient in neonatal meningitis using serial diffusion-weighted imaging
had their neurodevelopment assessment performed at 3 months using Indian adaptation of
Bayley scales of Infant Development kit and found significant reduction in scores of patients
compared to the controls.
131
DASII evaluation was done to evaluate the effect of play based
stimulation program for children with cerebral palsy or mental retardation and found that
66% children showed increase in motor score and 100% showed increase in mental score.
132
Bayley Scale of Infant Development-II (BSID-II)
28
Bayley scale of Infant Development second edition like its predecessor, the BSID-I is
an individually administered examination that evaluates the current developmental
functioning of the infants and children. It was developed by Nancy Bayley in 1969 and has
been revised in 1993.
It consists of three scales: the mental scale, motor scale and the behavior rating scale.
The mental scale has items that assess memory, habituation, problem solving, early number
concepts, generalization, classification, vocalization, language and social skills. The motor
scale assesses gross and fine motor control. It includes gross motor items like rolling,
crawling, running, jumping and fine motor items like prehension, adaptive use of writing
implements and imitation of hand movements. The Behavior rating scale assess qualitative
aspects of the childs test taking behavior. It evaluates attention, arousal, orientation,
engagement to task, emotional regulations and quality of movement. Complete assessment
requires 45 minutes to an hour to administer and require an advanced level of training and
expertise in administration. This scale is a comprehensive diagnostic tool applicable to
Review of Li terature
32
infants from 1month to 42 months of age. The BSID-II has good construct, content,
predictive, and discriminative validity.
Inter observer reliability rates for the mental scale and the motor scale were 89.4%
and 93.4% respectively. Test and retest reliability was 76.4 and 75.3% for the mental and
motor scale respectively. The tests represent the best standardized techniques for the
behavioral assessment available for infants. The major disadvantage is one must has to
undergo training sessions and validated as an examiner. It does not predict the long term
outcome. It can be widely utilize as formal indicator of need for timely intervention
services.
133
Many studies of BSID have been carried out to discriminate between children
with risk of developmental delay and who are developing normally. Studies have reported
correlation of birth weight with BSID scores in preterm infants.
134,135
There was
significantly lower MDI and PDI scores in premature infants compared to full term infants
at 1,4,8 and 12 months of corrected age.
136
A study was done to describe the neurobehavioral and developmental profile of very
low birth weight preterm infants in early infancy at 3 and 6 months using the Bayley motor,
mental and behavior rating scales with control group. VLBW infants performed lower on the
Bayley Motor, Mental and Behavioral Rating Scale and concluded that most of the VLBW
infants showed non-optimal motor quality behavior at 6 months and encountered far more
problems with self-regulation compared with term infants.
137
BSID II mental scores are sensitive to patterns of development changed in the first 2
years of life that are specific to infants with Downs syndrome and medically fragile infants.
But the authors cautioned that the results from the BSID II assessment of high risk infants in
the first year of life should not be used for predictive purposes.
138
Review of Li terature
33
Concurrent validity study of the BSID-II with the Peabody developmental motor
scale in children with developmental delay at 12 months reported that the concurrent validity
of the tool is good for certain subscales age equivalent scores, particularly the BSID motor
scale with the PDMS-2 locomotor scale.
139
BSID-II is a gold standard diagnostic tool with good content, concurrent and
criterion validity for developmental assessment and hence was used in the present study to
measure developmental outcome in VLBW infants.
Movement Assessment of Infants Scale (MAI)
140
MAI was developed by Lynette Chandler in 1975 at the Clinical Training Unit of the
Child Development and mental Retardation Center of the University of Washington .It was
created out of need for a uniform approach to the evaluation of high risk infants. MAI
provides a detailed and systematic appraisal of motor behaviors that occur during the first
year of life. It is a criterion-referenced scale which assesses motor dysfunction in high risk
infants from birth to 12 months of age. It has 65 items and evaluates four components;
Muscle tone (10 items), Primitive reflexes (14 items), Automatic reactions (16 items)
Volitional movements (25 items). It has established risk profiles for 4, 6 and 8 months based
on normative data. The indications of MAI are as follows:
1) To identify motor dysfunction in infants upto the age of 12 months.
2) To establish the basis for an early intervention program.
3) To monitor the effects of physical therapy on infants and on children whose motor
behavior is at or below 1 year.
4) To aid in research on motor development by using a standard system of assessment.
5) To teach skillful observation of movement and motor development through
evaluation of normal and handicapped children.
Review of Li terature
34
The assessment of infant movement patterns is an important evaluation component in
the early identification and management of high risk and handicapped infants. Difference in
infant movement patterns may provide early clues to diagnosis of cerebral palsy and other
developmental disabilities. Although the use of norm-referenced developmental assessment
tools is an important component of infant evaluation, a need exists for standardized
qualitative assessment tools as well. The MAI represents an important first step towards the
clinical measurement of qualitative aspects of infant movement.
141
A review of the MAI by Campbell stated, "The MAI appears well-suited to the stated
purposes and is more comprehensive in its assessment of total motor performance than any
other published test. If the appropriateness of the MAI is to be demonstrated, both normal
and abnormal children must be studied, so advised for normative data collection on both
full-term and premature infants.
142
This led to the study in 1988 in which they compared the test results of 50 healthy
normal 4-month-old infants on the Movement Assessment of Infants with the published
Movement Assessment of Infants a priori profile. Thirty percent of the infants tested had
total-risk scores greater than 7, which differed significantly from the 15% in the original
Movement Assessment of Infants data. On 18 of the 65 Movement Assessment of Infants
items, more than 15% of the study sample had risk scores that differed from Movement
Assessment of Infants profile normative scores. Suggestions for revising the Movement
Assessment of Infants were made that could improve the reliability and validity of the test
(especially the TRS>10).
143
Review of Li terature
35
Although the MAI test was not yet normed in 1980s, some reliability and validity
studies have been reported for the a priori profile. The MAI authors originally stated that the
interrater reliability for the MAI was 0.90 or above.
140
A reliability study conducted with 53 infants found an interrater reliability of 0.72 and
a test-retest reliability of 0.76. An analysis of item reliability using the same 53 infants
showed that 40% of the MAI items had poor inter-observer reliability, and 48% of the items
had poor intra -observer reliability. Further data are needed to clarify which MAI items may
warrant elimination or modification.
144
But a subsequent study reported a higher reliability. It was done to compare the
standard and a revised version of the four-month Movement Assessment of Infants (MAI),
on a group of 60 high-risk infants to find the inter-rater and test-retest reliabilities. Based on
the results, the tests inter-rater and test-retest reliabilities were considered excellent on both
the standard (0.91 and 0.79, respectively) and revised (0.93 and 0.83, respectively) MAI.
The results of this study suggest that there is a high reliability for the MAI.
145
In a review of instruments that measure quality of movement in cerebral palsy they
focused on the Volitional Movement section of the MAI, because this section describes both
functional and qualitative components of gross motor behavior. They commented that the
MAI is a landmark test, as it was the first to apply the assessment of movement performance
to children with disordered movement.
146
Another review on reliability and validity of the Movement Assessment of Infants
reported that the Volitional Movement section was the best predictor of outcome. This
finding indicates the importance of items that assess function and performance in the
prediction of a diagnosis of cerebral palsy.
147
Review of Li terature
36
The predictive validity of MAI was evaluated on 246 high risk infants admitted in
NICU. These babies were evaluated at 4 months and follow up examinations using BSID
were scheduled at 12 and 24 months. The results of the study showed a highly significant
correlation between the MAI risk score and the Bayley Motor and Mental scale at one and
two year indicating the clinical relevance of MAI in identifying neuromotor dysfunction as
early as four months of corrected age.
36
A retrospective study was done to examine the sensitivity and specificity of the Bayley
motor scale and the MAI for early identification of cerebral palsy at 4-months of corrected
age with outcome tested at 3years and 8 years .The results demonstrated that the MAI was
more than twice as sensitive as Bayley motor scale (73.5% Vs 35.3%) in correctly identifying
children with later diagnosis of cerebral palsy as either suspect or abnormal at 4-months of
age. However the specificity of MAI was lower than Bayley motor scale (62.7%Vs 94.9).
37
MAI was tested on 86 preterm infants of 32 wks and between 32 to 36 weeks to
establish two preterm four month risk profiles based on gestational age and the results
suggested that the current MAI risk profile may be applicable to infants of 32-36 weeks
gestation but not to infants < 32 weeks gestation.
148
A prospective study was done on 160 risk babies to identify neurodevelopmental
abnormalities at 4 and 8 months by MAI with neurodevelopment outcome tested at 18
months using BSID scale. They evaluated high risk infants with preterm low birth weight
<1750g.They found a high sensitivity and specificity of MAI at 4 month and at 8 months
They also reported strong correlation between MAI TRS and categorical score with MDI
and PDI of BSID scores at 18 months. The study concluded that MAI has high predictive
validity at both 4 and 8 months in identifying neurodevelopmental abnormality at 18
months.
35
Review of Li terature
37
A study was done to present early developmental data on a group of low-birth weight
infants with normal developmental outcomes. Subjects were 118 infants initially assessed at
4 months corrected age on the Bayley Scales of Infant Development and the Movement
Assessment of Infants (MAI) with outcome evaluation at 12 months on the Bayley and
compared to that of a group of 36 infants later diagnosed as having cerebral palsy (CP).
Results for the infants with normal outcomes showed that the CP group had significantly
lower Bayley scores and significantly higher MAI total risk scores than the non handicapped
group.
149
A prospective study to evaluate one year neurodevelopmental outcome using Bayley
Motor Scale for at risk infants assessed on MAI at 4 months reported a sensitivity of 67%,
specificity of 35% and PPV of 65% at a cut-off score of 8 and with a cut-off score of 13,
sensitivity dropped and specificity raised. They also reported that the volitional movement
and primitive reflexes section risk score on MAI were significantly negatively correlated
with Griffiths mental score and PDI at 12 months. They concluded that certain MAI risk
scores at 4 months enable prediction of one year outcome.
150
The purpose of a retrospective study was to analyze which neuromotor behaviors in a
sample of four-month-old low-birth weight infants were most predictive of later cerebral
palsy. The infants (n=229) were evaluated at four months corrected age on the Movement
Assessment of Infants (MAI) and were followed to between three and eight years of age. For
the CP group as a whole, 17 neuromotor items from the MA1 were highly significant
predictors of cerebral palsy. A further 15 items also were significant, but less significant
than the other 17 items. Seven items were predictive of later spastic diplegia, seven for
spastic hemiplegia, and 35 items differentiated quadriplegic infants. The authors
Review of Li terature
38
recommended a shorter version of the MA1 should be developed to increase its over-all
reliability and validity in the early detection of cerebral palsy.
151
A recent study in 2006 was done to study the item validity analysis of MAI to detect
cerebral palsy in 76 preterm infants assessed at 4 and 8 months. The results indicated
general suitability of the test to the expectations of the Rasch model to detect cerebral palsy.
Further analysis showed that a statistically significant number of items do not fit the model,
which compromises the construct validity of the test. They suggested that the erroneous
items should be revised or even eliminated, because there was no consistent information
about the motor development at the corrected ages of four and eight months. Even with the
restrictions MAI has positive aspects and suggestions were in this study to improve the
validity of the tool.
152
A study examined the performance of Asian American infants on the Movement
Assessment of Infants (MAI). The sample consisted of 30 full-term 6-month-old Asian
American infants. These infants tended to have slightly slower integration of some primitive
reflexes and to acquire automatic reactions and volitional motor skills at a slightly different
rate than the predominantly Caucasian group of infants in a previous study. When the
Washington and Deitz 6-Month Profile was used with the Asian American infants, 40% of
them were identified as having risk scores higher than any of the infants in the Washington
and Deitz study. This finding suggests that clinicians should be cautious when using the
MAI 6-Month Profile to assess Asian American infants.
153
A prospective study has evaluated the predictive validity of the MAI in extremely low
birth weight infants (<1000 grams) and found it to be highly specific (91%) and acceptably
Review of Li terature
39
sensitive (64%) to detect cerebral palsy. The outcome was evaluated based on the BSID
scores at 2 years. They also evaluated the predictability of MAI for identifying minor
neurological disorders (MND) using a cuff-off score of five and found that MAI had
sensitivity of 44%,specificity of 71% and PPV and NPV of 50% and 67% respectively.
39
A retrospective study was to examine the relationship between early neuromotor
findings, as assessed by the Movement Assessment of Infants (MAI), and later gross and
fine motor outcomes, as measured by the Peabody Developmental Gross Motor Scale and
the Frostig Eye-Motor Coordination Subtest. The sample consisted of 77 children who had
been identified in infancy as biologically at risk and who had 4-month MAI scores and 4.5-
year motor evaluation scores. Spearman's rank correlation between the MAI scores and the
two motor outcome measures yielded no clinically significant relationships. These findings
suggest that therapists should use the MAI as a reflection of an infant's performance at the
time of testing rather than as an indicator of future potential.
154
A study examining the ability of the MAI "to detect subtle changes in motor
development of infants with Down's syndrome" over a six-week period in responsiveness to
the Peabody Gross Motor Scale and reported that the MAI was sensitive to developmental
changes in the subjects tested from initial test to follow-up, thus further suggesting the
predictive value of this tool in assessing a group of infants with known handicaps.
155
In a prospective study the performance of 57 healthy full term 6-month old infants in
order to provide a standard against which to compare the motor performance of 6 month old
infants at risk for developmental abnormalities. The results included identification of those
motor behaviors which are both typical and infrequent for 6 month old infants with normal
Review of Li terature
40
motor outcome. A total risk score for the sample ranged from 0 to 5 and a score 6 was
considered as risk for abnormal development in 6-month old infants. There are no other
studies on performance of 6-month old infants on MAI .This study was used as the base to
study the predictive validity of MAI in 6 months old Very low birth weight infants.
42
The predictive validity of the Movement Assessment of Infants (MAI) for the
detection of cerebral palsy was analyzed in 89 Brazilian infants, born with gestational age <
32 weeks and weight < 1500g. The infants were assessed with the MAI at 4 and 8 months,
corrected ages, and were submitted to a neurological evaluation between the ages 2 and 7
years old. Their results showed a high sensitivity of 4 and 8 month MAI for prediction of
Cerebral palsy with cut off score of >10. The best predictive values were obtained at 8
months, with a cut off > 13 risk points. A less restrictive criteria (> 10 points) might be
useful for the prediction of motor coordination problems at school age.
156
A study was conducted to compare the predictive abilities of the AIMS with those of
the Movement Assessment of Infants (MAI) and the Peabody Developmental Gross Motor
Scale (PDGMS). One hundred and sixty-four infants were assessed at 4 and 8 months
adjusted ages on the three measures. A pediatrician assessed each infant's gross motor
development at 18 months as normal, suspicious, or abnormal. The MAI provided the best
specificity rates at 4 months while the AIMS were superior in specificity at 8 months.
Sensitivity rates were comparable between the two tests.
157
A prospective longitudinal study to evaluate whether the four-month Movement
Assessment of Infants (MAI), predicted two-year cognitive and motor developmental status.
The subjects were 134 infants born at term who were considered at developmental risk due
Review of Li terature
41
to biological and social risk factors. Infants average MAI total risk scores at four months
were negatively correlated with their BSID MDI scores but not PDI scores at two years.
Infants classified as high risk on the MAI were approximately three times more likely than
infants with a lower risk MAI classification to have a high-risk MDI scores. They concluded
that the MAI appears to be valid for use with infants born at term who are at risk of
developmental delay and may be a useful tool to help clinicians make decisions about
intervention services.
41
The longitudinal motor development of a group of infants exposed to cocaine in utero
and was compared to an unexposed control group, and were evaluated at 1 month with the
AIMS, at 4 and 7 months with the AIMS and MAI, and at 15 months with the Peabody
Developmental Motor Scales (PDMS) and they concluded that in utero cocaine exposure has
a significant, although relatively small, effect on infant motor performance late in infancy.
However, regardless of exposure status, these infants had poor performance that may be
accounted for by a heavy accumulation of risk factors associated with poverty.
40
Study in group of infants exposed in utero to multiple drugs was done to compare the
predictive power of the Alberta Infant Motor scale (AIMS) and the Movement Assessment
of Infants (MAI) administered at four and seven months for detection of gross motor delays
at 15 months based on the Peabody developmental motor scales (PDMS).The study reported
that the for both tests, the best combination of sensitivity and specificity values was at seven
months. The MAI over identifies infants with motor problems in comparison to the AIMS,
but neither test adequately identifies infants who go on to have poor motor scores on the
PDMS-GM.
158
Review of Li terature
42
A study was conducted to evaluate whether Chronic Lung Disease (CLD) without
concomitant brain lesions constitutes a risk factor for adverse developmental outcome. Forty
three very low birth weight infants with CLD and without CLD were evaluated at 5 and 10
months of corrected age using the MAI scale. The Griffiths developmental test was carried
out at 10 months of age. The results indicated that CLD has a deleterious effect on the
control of hand and eye coordination and on perception and intelligence.
159
A study conducted to validate a 2-step infant developmental screening protocol
administered by nonphysician health professionals in community clinics administered the
Bayley Scales of Infant Development II and Movement Assessment of Infants at 6 months
to compare the infants scores on The Parent Concerns Survey and the Meade Movement
Checklist (MMCL) at 4 months .The correlation between infant MMCL scores at 4months
and Movement Assessment of Infants was significant with Bayley Scales of Infant
Development II scores at 6 months. This 2-step screening by non physician health
professionals provides a valid, new perspective for screening young infants.
160
Methodology
43
METHODOLOGY
Study Type: Observational Study
Study Design: - Prospective Longitudinal Study
Study Place: - The study was conducted in Department of Pediatrics Physiotherapy, KLES
Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum
Study Duration: - January 2008 to December 2010.The babies were enrolled from January
2008 to June 2009 and followed up to one year of corrected age till December 2010.
Source of Data Collection: - Neonatal Intensive Care Unit (NICU) of KLEs Dr Prabhakar
Kore Hospital and Medical Research Centre, Belgaum -590 010, Karnataka State, India
Sample Size: - 60
Calculation of sample size: The sample size was calculated with the aim of obtaining at
least 80% sensitivity for the MAI tool to predict neurodevelopmental outcome at 12 months.
Sample size calculation for predictive validity studies to find the sensitivity of the test is
4Z
2
pq
d
2
Where p=sensitivity of the tool
q = (100-p) %
d = error allowed
Z = Standard normal constant for (1-) %
For a Sensitivity (p)=80% based on previous studies, allowing 20% error(d) with 95%
confidence the required sample size is
4 x (1.96)
2
x 80 x 20
= 61.46
20
2
Methodology
44
Sampling Design: - Non- probability sampling
Sampling method: - Consecutive sampling
Study Participants All male and female babies with birth weight of 1500gms admitted
to NICU
Instruments: -
1) Movement Assessment of Infants Manual- It is a criterion-referenced scale which
assesses motor dysfunction in high risk infants from birth to 12 months of age. It
assesses the quality of movement performance in children with disordered
movement. It has established risk profiles for 4 and 8 months based on degree of risk
approach .It also has a preliminary 6-month profile based on normative approach .It
is a comprehensive assessment and requires 30 to 45 minutes for administration and
scoring. It has 65 items and evaluates four components; Muscle tone (10 items),
Primitive reflexes (14items), Automatic reactions (16items) and Volitional
movements (25items). Maximum numbers of items that can be administered at 4
months of age are 48 and at 8 months of age are 61.
140
2) Bayley Scale of Infant Development (BSID-II) Second Edition Manual-It is a
comprehensive diagnostic tool that evaluates children between birth and 42 months.
It is based on normative data and consists of a Mental Scale, a Motor Scale, and a
Behavior Rating Scale. According to the manual, the Motor Scale assesses degree of
control of the body, coordination of the large muscles, finer manipulatory skills of
the hands and fingers, dynamic movement, dynamic praxis, postural limitation and
stereognosis. The Mental scale assesses environmental responsiveness, sensorial and
perceptual abilities.
28
Methodology
45
Materials used: - Structured proforma, Consent form, MAI profile score sheet of 4, 6 and 8
months, Bayley Motor and Mental Cue sheets for 12 months and the MAI and BSID-II test
materials.(Annexure No. IV & V)
INCLUSION CRITERIA: -
1. Infants with birth weight 1500 grams admitted to NICU of KLEs Dr Prabhakar
Kore hospital and MRC Belgaum.
2. Mothers who consented for their infants participation in the study.
EXCLUSION CRITERIA: -
Newborns with-
1. Dysmorphic features
2. Neuromuscular disorders
3. Congenital anomalies influencing developmental or neurological outcome
4. History of Meningitis, hydrocephalus and encephalitis in neonatal period or later.
5. Metabolic disorders
PROCEDURE
Infants with birth weight 1500gms admitted to NICU of KLEs Dr Prabhakar
Kore hospital and medical research center, Belgaum during the one and half year period
from January 2008 to June 2009 formed the cohort of the study. A total of 107 VLBW were
admitted to NICU during the study period. From those admitted 35 babies couldnt be
recruited as 21 got discharged against medical advice, 10 expired and 4 didnt meet the
study criteria. The remaining 72 infants were consecutively recruited for the study based on
the inclusion and exclusion criteria, of which one infant died after 2 month due to sepsis and
diaphragmatic hernia, one developed hydrocephalus and 09 babies were lost to follow up. Of
Methodology
46
the 72 infants recruited only 60 infants who completed all the evaluations till one year were
included in the final data analysis.
Babies were managed for their clinical problems by using standard protocol by the
neonatologist during their stay in NICU. Once the neonates were clinically stable (no
respiratory distress, no hypotension, not on medications causing hypotonia and altered
sensorium, no seizers) and discharged from the NICU, they were recruited for the study after
obtaining consent from the mother. The ethical clearance for the study was obtained from
KLE Universitys ethics committee. A routine standard neurological evaluation was
performed by the investigator and the mothers and infants details with their neonatal
problems were recorded from the discharge card in a structured proforma. The mothers were
given appointment for follow up evaluation at 4 months of corrected age after calculating
the degree of prematurity as mentioned in the MAI manual.
Before data were collected on VLBW infants inter-rater reliability for MAI was
established on normal term babies at 0.80 for 4- and 6- months and above 0.90 for 8 month
between the investigator and another experienced physiotherapist .It was re-obtained for
VLBW infants during the course of study and was established at 0.80 for 4 months and
above 0.90 for 6 and 8 months. The MAI evaluation was repeated by the investigator within
24- 48 hours after the first evaluation and intra rater reliability of above 0.90 was obtained.
Both the therapists had received initial training on the MAI from the training DVD of MAI
received from the developers of the MAI from University of Washington USA. The
investigator also received 2 weeks training at the Child Development Center Trivendrum in
use of various neuromotor tools in high risk infants. The investigator and the clinical
psychologist received 4 days training in using BSID-II at the Department of Medical
Education, J. N. Medical College by the international faculty from the University of
Alabama USA.
Methodology
47
Once inter-rater reliability was established, all the scheduled follow up evaluations
of MAI were done by the investigator at the physiotherapy department of the hospital where
the test material and testing environment was set as described in the manual. The mothers
were reminded of follow up dates regularly by telephone and according to there convenience
and suitability appointments were fixed for MAI examination. All the evaluations on the
infants were done in presences of primary caregiver and enough time was spent in
establishing rapport with the child before the testing so as to elicit the childs best
performance.
The four months corrected age MAI examination was performed between 3 months
15 days and 4 months 15 days. The 65 items of MAI with its components of muscle tone,
primitive reflexes, automatic reactions and volitional movements were divided into groups
of preferred positions of testing and were administered by direct handling and observation of
the infants in different positions. A symmetrical position in relation to the child was
maintained throughout the testing .There was no set order for administrations of the test
items but grouping of items by test position was done to avoid tiring the child. Items that
required the most concentration, such as manipulating the pellet, were presented when the
child was in the most favorable mood; items that were most likely to distress or irritate the
child, such as Moro and Asymmetric Tonic Neck Reflex, were deferred to end of testing.
The order of testing was modified, if child showed restlessness, irritability, and loss of
attention or fatigue; however changes were not made in the specific method of presenting
each test item.
After completing the administration of MAI, the test items were scored numerically
according to specific criteria described in the manual on the 4 month profile score sheet
Methodology
48
which was developed based on degree of risk approach. The score received by the child, if
considered to be questionable, one high risk point was given and was recorded by circling
the corresponding number in the profile. The high risk points were added and recorded for
each section and then the total high risk points was established by adding the high risk
scores of all four sections. At the four-month examination the potential score ranges from 0
to 48 with higher score indicating greater deviance. Following the 4-month examination
appointments were given for the second and third follow up evaluation of MAI at 6 and 8
months of corrected age and reminded telephonically.
The 6 months corrected age MAI evaluation was performed between 5 months 15
days to 6 months 15 days and scoring was done on the preliminary 6- month profile score
sheet which was developed based on normative approach and the total high risk points were
calculated similar to the 4-month examination. The third follow up MAI evaluation at 8
months corrected age was performed between 7 months 15 days to 8 months 15 days and
scoring was done on the 8 month profile score sheet and the total high risk points were
calculated. The potential score ranges from 0 to 61 at the eight month examination.
A cut-off score of 10 was considered as risk for abnormal neuromotor outcome for
the 4-month and 8- month MAI which is one standard deviation above the mean for normal
low birth weight infants. This score was selected based on previous studies
35
and as
recommended by other studies
144
which reported that the cut-off >/= 8, mentioned in the
manual was insufficient to identify normal neuromotor development. A score of 6 was
considered as risk for 6- month MAI based on the 6-month MAI preliminary study on
normal term infants.
42
Methodology
49
The neurodevelopmental outcome at 12 months was evaluated using the gold
standard; BSID-II. It was administered by an experience and trained clinical psychologist
who was masked to infants history and prior MAI scores. Both the mental and motor scales
were administered as per instructions in the manual and credit score was given for each item
the child successfully performed. The total number of credit points was added for motor and
mental component separately to compute the raw score and developmental age. The raw
scores were then converted into Psychomotor Developmental Index (PDI) and Mental
Developmental Index (MDI) scores based on the normative index score ranges available in
the BSID-II manual. Based on the index scores the interpretation of test; 85-115 was
considered as normal development, 70 to 84 as mild delay and 69 as significant delay.
Methodology
50
Statistical Analysis
The data was entered into excel spread sheet, tabulated and subjected to statistical
analyses using SPSS software version 12.The infant data was analyzed in terms of mean and
standard deviation. The MAI scores at 4, 6 and 8 months and Bayley Mental and Motor
scores at 12 months were also analyzed in terms of mean and standard deviation.
The predictive validity of MAI was computed to determine its accuracy in detecting
neurodevelopmental abnormality at 12 months by using statistical measure of validity like:
Sensitivity-True Positive
Specificity-True Negative
Positive Predictive Value (PPV)-False Positive
Negative Predictive Value (NPV)-False Negative
Spearman's rank correlation was used to determine the inter-rater and intra-rater
reliability between pair of examiners.
Pearson product moment correlation was used to examine the relationship between the
MAI risk scores (4, 6 and 8 months) and BSID-II mental and motor scores at 12 months. It
was also used to find relationship between the neonatal variables (number of neonatal
problems, number of day in NICU) with the MAI and BSID-II scores.
Students t test was used to compare the MAI performance at 4, 6 and 8 months as
measured by the TRS and categorical score between the normal and abnormal outcome
group.
Chi square test with Yates correction was used to find association between maternal
variables and the MAI and BSID score.
Results
51
RESULTS
A total of 107 babies were admitted to NICU with birth weight <1500 grams during
the study recruitment period, out of which 72 babies were enrolled into the study, based on
the eligibility criteria. From the 72 enrolled only 60 babies completed the follow up. The
results of the study were based on the data analyzed for 60 VLBW infants who completed
all the MAI evaluations at 4, 6 and 8 months and the outcome evaluation on BSID-II at 12
month. The level of significance was set at p<0.05
Maternal Characteristics- Table No.1 shows age distribution, educational and
socioeconomic status of mothers.
Age distribution of the mothers- The majority of mothers were in the age range of 21 to 25
years followed by 26 to 30 years. Mother less than 20yrs and greater than 31 years were
comparatively less and were in the range of 11% to 15%.
Educational status of mothers About 70% of the mothers had education below
graduation with majority of the mothers having secondary (33.33%) and higher secondary
education (26.66%). Less than 10% had higher education till post graduation and none of
them were illiterate.
Socioeconomic Status of mothers Majority of the children in the study belonged to class
I (40%) and Class II (31.66%) socioeconomic status families compared to Class IV and V
economic status families. (Annexure I, Table No. 1)
Results
52
Infant Characteristics - Table No. 2- describes the characteristics of the VLBW infants.
The mean gestational age was 32.9 2.53 with the mean birth weight of 1365.5 135.50.
The mean number of days in NICU was 20.212.53. Out of the total 60 babies participated
in the study, 33(55%) were males and 27 (45%) were females. 53(88%) were preterm
VLBW and 7(12%) were term VLBW babies having intrauterine growth retardation.
Majority of the VLBW (58.33%) had <3 neonatal problems during their stay in NICU and
none of them had more than 6 neonatal problems. (Annexure I, Table No. 2)
Neonatal problems in VLBW infants during their NICU stay Table No. 3 - shows the
common neonatal problems among the study sample of VLBW infants during their NICU
stay. Maximum number of infants had hyperbilirubinemia (78.33%) followed by sepsis 55%
followed by hypoglycemia 45%.The other neonatal problems ranged between 6.66% to
18.3%.(Annexure I - Table No. 3)
Mean MAI scores- Table No. 4 - shows the mean scores of MAI at 4, 6 and 8 months.
4-month score -The 4-month MAI mean TRS score was 9.95 7.10, muscle tone section
mean score was 4.96 2.69, primitive reflex and automatic reaction section scores were 1.5
each and the volitional movement section score was 22.51.The mean scores were higher
for the TRS followed by muscle tone and volitional movements.
6-month score- The 6-month MAI mean TRS score was 68.33.The mean categorical score
for muscle tone, primitive reflex and automatic reaction ranged from 1.06 to 1.31 with SD
varying from 1.83 to 2.10.The mean volitional movement score was 2.333.31.The mean
risk scores for muscle tone, primitive reflex and automatic reaction were almost similar in
range but lower than the volitional movement section scores.
Results
53
8-month score- The 8-month MAI mean TRS score was 8.06 10.04.The mean scores for
muscle tone, primitive reflex score and automatic reaction ranged from 1.31 to 1.65 with
SD varying from 1.83 to 2.64 .The mean volitional movement score was 2.733.99. The
mean risk scores were lower for muscle tone, primitive reflex and automatic reaction than
the volitional movement section scores. (Annexure I, Table No. 4)
Mean Mental and Motor scores of BSID-II at 12 months Table No. 5 - shows that the
12 month Bayley Mental Scale has a mean raw score of 85.518.95, MDI score of 102.8
16.76 and mean developmental age of 10.11 2.45. The Bayley Motor Scale had a mean raw
score of 60.959.77, mean PDI score of 90.8 21.48 and mean developmental age was
9.53 2.34. The mean motor scores at 12 months were less compared to the mean mental
scores. The mean motor developmental age was also less than the mental age.(Annexure I -
Table No. 5)
Predictive validity of 4 month MAI for neuromotor outcome at 12 months
Table No.6 - shows the number of infants having MAI, TRS 10 and <10 with normal (>85)
and abnormal (84) outcome at 12 months based on BSID scores.
This table describes that out of 17 infants with abnormal motor outcome at 12 months based
on PDI(84) score, 14 had TRS10 which gives a sensitivity of 82.3%.Out of 43 infants
with normal outcome, 32 had TRS <10 which gives a specificity of 74.4%.From the 25
infants with TRS 10 only 14 had abnormal outcome giving a positive predictive value of
56% and out of 35 with TRS <10 about 32 turned out to have normal outcome giving a NPV
of 91.4%.(Annexure I - Table No. 6)
Results
54
Predictive validity of 6- month MAI for neuromotor outcome at 12 months
Table No. 7 - shows that out of 17 infants with abnormal outcome at 12 months based on
Bayley Motor score, 12 had TRS 6 which gives a sensitivity of 70.6%.Out of 43 infants with
normal outcome 35 had TRS < 6 which gives a specificity of 81.4%.From the 20 infants with
TRS 6 only 12 had abnormal outcome giving a positive predictive value of 60% and out of
40 with TRS < 6 about 35 turned out to have normal outcome giving a NPV of 87.5%.
(Annexure I- Table No. 7)
Predictive validity of 8- month MAI for neuromotor outcome at 12 months
Table No. 8 - shows that out of 17 infants with abnormal outcome at 12 months based on
PDI ( 84) score, 14 had TRS 10 which gives sensitivity of 82.3%.Out of 43 infants with
normal outcome 41 had TRS < 10 which gives specificity of 95.3%.From the 16 infants with
TRS 10 about 14 had abnormal outcome giving a positive predictive value of 87.5% and
out of 44 with TRS < 10 about 41 turned out to have normal outcome giving a NPV of
93.2%. All the measures of validity were above 80 %.( Annexure I - Table No. 8)
Comparison of predictive validity of 4, 6 and 8 months MAI for neuromotor outcome
at 12 months -
Table No. 9 describes the predictive validity of MAI at all three ages. MAI has higher
sensitive of 82.3% at 4 and 8 months MAI than 6-month MAI (70%). The specificity has
progressively increased from 4 to 6 to 8 months ranging from 74.4% to 95.3% .Similarly
PPV has increased from 4 to 6 to 8month ranging from 56% to 87.5%. The negative
predictive value is good at all three ages and is above 90% for 4 and 8 months of MAI. All
the measures of predictive validity were above 80% for 8 months MAI. (Annexure I - Table
No. 9)
Results
55
Correlation between the 4-month MAI and BSID-II at 12 month Pearson Product
Moment correlation showed statistically significant inverse correlation between 4-month
MAI total risk score and 12 month PDI with r = - 0.710 and p<0.001.Similar correlation
with MDI scores was seen with r = - 0.501 and p<0.001.All the categorical scores for
muscle tone, primitive reflexes, automatic reactions and volitional movement of the 4-month
MAI also showed significant negative correlation with both MDI and PDI scores at 12
month with p<0.005.The automatic reactions and volitional movements section showed
stronger correlation with PDI at 12 months whereas the PR and VM showed better
correlation with MDI scores. (Annexure I - Table No. 10)
Correlation between the 6-month MAI and BSID-II at 12 month-The Pearson product
moment correlation showed statistically significant inverse correlation between 6-month
MAI total risk score and 12 month MDI scores with r = -0.683 and p<0.001.Similar
correlation with PDI was seen with r = - 0.639 and p<0.001.All the categorical scores for
muscle tone, primitive reflexes, automatic reactions and volitional movement of the 6-month
MAI also showed significant correlation with both MDI and PDI scores at 12 month with
p<0.001 . The TRS, automatic reactions and volitional movements section showed stronger
correlation with PDI and MDI at 12 months. (Annexure I - Table No. 11)
Correlation between the 8-month MAI and BSID-II at12 month - Pearson product
moment correlation showed statistically significant inverse correlation between 8-month
MAI total risk score and 12 month MDI with r = -0.735 and p<0.001.Similar correlation
with PDI was seen with r = - 0.724 and p<0.001.All the categorical scores for muscle tone,
primitive reflexes, automatic reactions and volitional movement of the 8-month MAI also
showed significant negative correlation with both MDI and PDI scores at 12 month with
Results
56
p<0.001. The TRS, muscle tone and volitional movements section showed stronger
correlation with PDI at 12 months whereas the MDI strongly correlated with the TRS and
VM section score. (Annexure I , Table No. 12)
Neurodevelopmental problems in VLBW at one year based on BSID-II score Table
No-13 shows that out of 60 babies, total of 17 babies had neurodevelopmental problems at
12 months based on BSID-II scores which constitute 28.33% of neurodevelopmental
abnormality. Of the 10 babies with only motor delay, 3 had mild delay and 7 had significant
delay. Out of 7 babies with both motor and mental delay 4 had mild delay and 3 had
significant delay. None of the babies had isolated mental delay while majority of the babies
had motor delay. Mild delay was in 11.66% and significant delay in 16.66% of the children.
(Annexure I, Table No. 13)
Four-months MAI scores of infants with normal and abnormal neuromotor outcome at
12 months Based on the BSID-II scores at 12 months the children were retrosepectively
divided into normal and abnormal outcome groups.Table No. 14 - shows the mean differences
in the TRS and categorical scores of MAI at 4-month between the children in normal outcome
and abnormal outcome group based on the BSID scores at 12 months. The students t test
showed statistically significant difference in TRS and categorical risk score between the groups
at p < 0.001 except the AR which was significant at p<0.05.The muscle tone had higher mean
score in the normal outcome group and in the abnormal outcome group VM and MT had
higher risk scores . (Annexure I, Table No. 14)
Results
57
Six-months MAI scores of infants with normal and abnormal neuromotor outcome at 12
months- Table No. 15 shows the mean differences in the TRS and categorical scores of MAI at
6-month between the children in normal outcome and abnormal outcome group based on the
BSID scores at 12 months. The studentst test showed statistically significant difference in
TRS and categorical risk scores between the groups at p < 0.005. There was significant
difference in the TRS scores compared to the muscle tone and primitive reflexes between the
two groups. (Annexure I, Table No. 15)
Eight-months MAI scores of infants with normal and abnormal neuromotor outcome
at 12 months Table No. 16 - shows the mean differences in the TRS and categorical scores
of MAI at 8-month between the children in normal outcome group and abnormal outcome
group based on the BSID scores at 12 months. The students t test showed statistically
significant difference in TRS and categorical risk score between the groups at
p<0.005.There was significant difference in the TRS, VM and MT section of MAI between
the two groups with p<0.001. (Annexure I, Table No. 16)
Mean Bayley Mental Scale scores of infants with normal and abnormal Cognitive
outcome at 12 months-Table No. 17 showed that there was statistically significant
(p<0.001) difference in the mean Bayley Mental Scales raw score, MDI score and
developmental age between the normal outcome and abnormal mental outcome group at 12
months with t value ranging from 8.66 to 12.20. The developmental age in the abnormal
outcome children was 5 months lower than the normal outcome children. (Annexure I, Table
No. 17)
Results
58
Mean Bayley Motor Scale scores of infants with normal and abnormal motor outcome
at 12 months- Table No. 18 showed that there was statistically significant p<0.001
difference in the mean raw score ,PDI and developmental age between the normal outcome
and abnormal outcome group at 12 months with t value ranging from 7.21 to 10.26.
(Annexure I, Table No. 18)
Association of MAI and BSID-II scores with maternal characteristics Table No. 19-
shows that there is statistically significant association between maternal literacy and TRS at
4,6 and 8 months of MAI and 12 month PDI at p<0.05.There is marginally significant
associate between literacy and MDI score with p=0.06.The other maternal characteristics
like age of mother, gestational age and socioeconomic status were not associated with TRS
or the PDI and MDI scores.(Annexure I, Table No. 19)
Correlation between the number of days in NICU with MAI and BSID-II scores-There
was a positive correlation between the number of days in NICU and the MAI total risk
scores at all three age and was statistically significant with p value ranging from 0.05 to
0.002.There was negative correlation between the number of days in NICU and the Bayley
motor and mental scores with p value of 0.037 and 0.002 respectively. The correlations were
statistically significant. (Annexure I, Table No. 20)
Correlation between the number of neonatal problems with MAI and BSID-II scores-
There was a positive correlation between the number of neonatal problems and the TRS
scores of MAI at all three ages but was statistically not significant. There was negative
correlation between the MDI and PDI scores of BSID-II and the number of neonatal
problems but was statistically significant only for PDI scores with p=0.003. (Annexure I,
Table No. 21)
Discussion
59
DISCUSSION
This prospective longitudinal study is the first in India, to evaluate the predictive
accuracy of the Movement Assessment of Infants scale, which measures infant neuromotor
development in the first year of life.
The results of this study demonstrate that the MAI is an accurate and effective tool
for identification of neurodevelopment abnormalities in VLBW Indian infants at 4-month, 6-
month and 8- months corrected ages. Our study offers the first evaluation of the predictive
validity of the preliminary 6-month MAI profile in a high-risk population of VLBW infants.
This is new and important information for the clinical utility of MAI which was not explored
to date. This study has broadened the scope of use of MAI at various ages.
The data of the infant characteristics showed a mean gestational age of 322.53
weeks and birth weight of 1365.5 135.50 grams. It also showed that most of the VLBW
infants were preterm (88%) with only 12% term infants which indicates that the study
sample had more preterm VLBW infants who are vulnerable for developmental risk with
complications of long term minor and major disabilities. The mean gestational age of the
infants in our study was comparable to the mean gestational age of another study in which
the sample included both preterm and term infants with known high risk of delayed
development.
36
The mean number of days babies stayed in NICU was 20.4 12.20 which could be
the reason for higher rates of abnormal neuromotor outcome as studies have reported
association between NICU stay and outcome.
108
Our study showed a statistically significant
Discussion
60
(p<0.05) negative correlation between the number of days in NICU and BSID-II scores. This
confirms that more the number of days baby stays in NICU, less is the score on PDI and
MDI with greater risk of developmental delay. There was positive correlation between the
number of days in NICU and Total Risk Score of MAI at all three ages indicating that more
the duration of stay in NICU, greater is the MAI risk score and in turn greater the chance of
developmental risk. None of the MAI studies has done the correlation between the number
of days the VLBW infant stayed in NICU and MAI total risk score.
The educational level of the mothers was low in our study with only 21.66% of them
completing graduation. A study on normal term healthy infants found no association
between maternal education and infant motor development.
161
However in our study there
was significant association. The MAI study done on term born infants has reported the
average level of education of 11.4 years, attesting to the high social risk status of the
majority of the families in their sample.
41
In our study apart for VLBW, the educational level
of the mother could be a potential social risk for poor neurodevelopmental outcome. This is
supported by the significant association that has been found in our study between the
literacy and the psychomotor index scores at 12 months with p=0.003. There was marginally
significant association between maternal education and the cognitive outcome p=0.06 also.
Our study also reported a strong association between the MAI total risk scores at 4 ,6 and 8
months with the literacy of the mother with p<0.05.This indicates the impact of maternal
education on the risk status of the infant. This could be because low education of mother is
related with low birth weight child and this in turn is associated with risk status of the baby
during infancy and in turns results in poor developmental outcome.
Discussion
61
Majority of the infants belonged to class I (40%) and class II (31.66%) economic
status based on their family monthly income
162
indicating that most of them belonged to
families with good socioeconomic status. A study has reported that poverty experienced
during early childhood is found to be more detrimental to future development than poverty
during later life.
41
However in our study there was no significant association between socio
economic status and the risk scores of MAI or the BSID-II scores at one year as majority of
the children belonged to families with better economic status.
The mean score in Muscle Tone section at 4-months was higher compared to other
sections, rightly presenting the tonal variation in preterm VLBW infants around that age.
Some preterm infants have low muscle tone, particularly in their torso. Other preterm
infants have increased muscle tone, with more distinct muscle mass, particularly in their
lower extremities. Some degree of physiological hypertonia is normally present making it
difficult to differentiate between hypertonia and normal tone. The Mean TRS of MAI at 4
months in our study was comparable to the mean TRS in a study on term infants at social
risk,
41
indicating that both VLBW and term infants with social risk score nearly to cut-off
score of 10 which is a potential developmental risk.
At 6 and 8 months, the mean Total Risk score and the Volitional Movement section
scores were higher compared to other sections signifying the importance of volitional
movements in identifying risk of abnormal development.
142
This is supported by our finding
of statistically significant (p<0.001) difference in the mean TRS and volitional movement
section scores between the children with normal and abnormal motor outcome based on
PDI<84. It is future supported by strong correlation observed in our study between the
volitional movement section scores of MAI and PDI scores at 12 months.
Discussion
62
Although the mean MDI (102.8) and PDI (90.8) scores in this study were within
normal limits, the average PDI was 12 points lower than MDI. These less optimal scores
provide support for the presence of immature gross motor development. This could be due to
the variations in motor patterns in preterm infants who may be labeled as abnormal in
essentially normal outcome VLBW infants.
34
The difference between the PDI score of
normal and abnormal outcome VLBW children is statistically significant supporting the
presence of motor dysfunction which is reported in several studies on VLBW infants.
96,107
The sensitivity (82.3%) and specificity (74.4%) obtained in our study at 4 months
were higher than those reported in a previous study of VLBW infants of 73.5% and 62.7%
respectively.
36
The sensitivity was also higher relative to another study of VLBW infants
(<1500 grams) which reported, sensitivity of 72.7% and specificity of 93%.
157
Our study
differs from the earlier studies in characteristics of study population, outcome measures, and
time of outcome evaluation. The higher sensitivity values of the present study could be
partly due to shorter duration of follow-up with outcome measured at 12 months of age
compared to 3-8 years
36
and 18 months of age.
157
One of the earlier studies used a cut-off score of >/= 8
36
whereas Darrah
157
used a
cut-off of > 9 which is comparable to the cut-off score of >/= 10 used in the present study.
Both the studies reported higher specificity which could be due to cut off >/=10 which better
identifies infants with normal development as compared to cut off >/= 8.
In a recent study in Brazil, the MAI was administered to 89 VLBW infants using a
cut-off score of >/= 10 on the MAI to determine risk.
156
Abnormal neurodevelopmental
outcomes were defined as a diagnosis of cerebral palsy at follow-up between 2 and 7 years
Discussion
63
of age. The authors 4-month MAI sensitivity of 92% and specificity of 83%, which are
generally higher than most of 4 month MAI studies, including our study. The stronger
results may be due to a different measure of abnormal outcome (diagnosis of cerebral palsy)
and later age of follow-up (2-7 years of age).
The sensitivity and specificity of 4 months MAI in our study are comparable to the
sensitivity of 83.3% and specificity of 78.2% reported in a previous study of LBW infants
(</= 1750 grams) in which a similar cut off score of >/= 10 was used and the primary
measure of developmental outcome was the Bayley Scales of Infant Development.
35
Although the PPVs were comparable (56% and 59% respectively), the NPV was higher in
our study (91% compared to 85%. The primary differences between the two studies were
age at follow-up and outcome measures. Their outcome was at 18 months and included a
neurological examination as well as the BSID. The lower NPV in their study may be due to
subtle clinical neurological sign which manifest later with increasing age.
A one year prospective study on risk infants with MAI evaluation at 4 month using a
cut-off score of >/=8 reported that MAI is not a good predictor of one year neurological
status with a low sensitivity of 67% and specificity of 35% (n=27 preterm infants) .However
they found that it was a better predictor of developmental and motor outcome based on the
strong correlation between the primitive reflex and muscle tone component of MAI with the
PDI scores at one years. They also observed a strong correlation of primitive reflex and
volitional movements components with the Griffiths developmental and locomotion
component.
150
Discussion
64
Our study had lower specificity (i.e. higher false positive rate) at 4 months which is
in agreement with other studies.
35, 150
The relatively high rate of false positives at 4 months
of age as reported by us could be a reflection of the clinical phenomenon of transient
dystonia in which abnormalities of muscle tone and posture are observed in the first months
of life among low birth weight infants but subsequently resolve. The clinical signs of
transient dystonia include extension posturing increased muscle tone particularly in lower
extremities, low muscle tone in torso or trunk, persistent reflexes, poor righting reaction, and
other clinical signs suggestive of developing cerebral palsy contribute to high risk scores on
MAI.
163,164
It is found that abnormal trunkal tone is a marker of delayed development in
LBW infants as infants with hypertonia in trunk and lower extremities showed low scores on
BSID and infants with hypotonia in trunk were associated with worst developmental
outcomes.
165
Other possible reasons for false positives could be severe respiratory disease
(bronchopulmonary dysplasia or chronic lung disease)
159,166,167
that are common in VLBW
who typically present with hypotonia and poor motor control that may persist till their
pulmonary status is resolved This results in high risk score for these infants in the section of
muscle tone and volitional movements. Once the respiratory conditions resolves their
growth and development proceeds along a normal pace and typically are functioning in the
normal range for their adjusted age around 1 to 2 years of age.
168,169
VLBW infants are
known to be at increased risk for deficits in school performance, language abnormalities,
impairments in visual-motor perception, learning disabilities, behavioral and executive
functions.
12,13,14
These problems typically are not apparent until early childhood or rent in
school age so may be identified as normal at 12 and 18 months. Children with transient
neuromotor abnormalities during first year are at greater risk for minor neurological
Discussion
65
disorders that are apparent at later ages.
163
This indicates that the false positives relative to
neurodevelopmental outcome at 12 months, may in fact be true positive indicators of later
minor neurological dysfunction which may not be evident in the first three to four years of
life.
The number of false positives can be reduced by increasing the cut-off score to >/=
13 but infants who will have true abnormal development at 12 months may be missed (i.e.
decreased sensitivity) in order to improve the specificity. The primary goal of a predictive
infant assessment is to identify infants with increased risk of abnormal developmental
outcome rather to identify infants who are likely to have normal outcome. The MAI is
designed to identify abnormal infants who require follow up and appropriate intervention, so
a less restrictive cut-off point is appropriate. Another possible way to reduce false positives
before subjecting these infants to unnecessary intervention is to re-evaluate in subsequent
follow up at 6 months of age. The PPV of 70% at 6 months obtained by our results
minimizes the likelihood of over identification and early intervention can be provided only
to those infants who continue to show risk at 6 months.
Only three studies have evaluated the predictive validity of MAI at 8 months.
35, 156,157
The first study to report predictive validity of the MAI at 8 months reported sensitivity of
96%, specificity of 64.5%, PPV of 51.9% and NPV of 90.8%.
35
While a higher sensitivity
was reported in the earlier study, the specificity, PPV and PPN were lower relative to the
present study. The lower sensitivity in our study, and the fact that the number of
abnormal infants was consistent at 4 and 8 months, suggests that 3 infants were
consistently developing more slowly. Given the limitation of outcome measure at one year,
we do not know if these children truly had abnormal neurodevelopmental outcome, or just
had slower motor development. If they did have abnormal development, it was likely mild.
Discussion
66
The coupling of high sensitivity with low specificity can indicate false positive
results for a group. So ideally tools that best discriminate between normal abnormal children
are preferred in clinical practice. Our results of validity at 8 months show considerably good
balance between sensitivity and specificity and indicated best combination of predictive
validity.
Our study demonstrates that normally developing infants can be better identified
with increasing age as observed in the comparison of our 4-month specificity results with 8-
month specificity results. The positive predictive value depends on the prevalence of the
neurodevelopmental problems and the study sample. The higher PPV obtained in our study
could be due to the higher prevalence of abnormal outcome in our study (28%) compared to
the Swanson study (17%).
35
Also, in the Swanson study, infants with suspicious
development at 18 months (PDI 70 to 84) were not included as normal or abnormal
outcomes. The number of false positive was less as compared to 4 months. This could be the
transient neurological sign present in the first few months start normalizing by 9 months and
disappear by 12 months.
170
This avoids the anxiety in parents and unnecessary burden of
intervention to a child who is going to have a normal developmental outcome in future.
Darrah and colleagues
157
evaluated 4-month and 8-month MAI scores of VLBW
infants relative to infant motor outcomes at 18 months. They reported 8-month sensitivity of
95.5% and specificity of 80.3%. This study provides support to our study in specificity at 8
months although we observed higher specificity and lower sensitivity. The two studies vary
in, duration of follow-up and measure of outcome. Their study used the pediatrician
classification for categorizing the infants as normal, suspicious and abnormal whereas
we used the Bayley Scale of Infants Development. The BSID-II has good psychometric
Discussion
67
properties as a diagnostic tool and provides a more standardized and quantitative measure of
infant development.
28
The study by Cordoza
156
et al reported high 8-month sensitivity (92%) and
acceptable specificity (79%) relative to outcome of diagnosis of cerebral palsy among
Brazilian infants. The predictive validity of MAI depends to some extent on the criteria used
to define outcome. The purpose of our study was to identify children with
neurodevelopmental abnormality and not cerebral palsy, which may be a reason for
relatively lower sensitivity in the present study. In their study, specificity decreased from
83% at 4 months to 79% at 8 months. A similar trend was observed in the study by Swanson
et al. where sensitivity increased from 4 months (83.3%) to 8 months (96%) but specificity
dropped from 78.2% to 64.5%
35
, another study by Darrah and colleagues again observed
increased sensitivity from 4 months (72.7%) to 95.5% at 8 months and a decrease in
specificity from 93% to 80.3%.
157
This trend noticed in other studies was contrary to the
results in our study which observed an improved specificity from 74.4% at 4 months to
95.3% at 8 months. The improved specificity from 4 to 8 months indicates that normally
developing infants can be better identified with increasing age. It could be because their
transient neurological sign and respiratory problems have diminished by this age and the
babies tend to improve in growth and development with better weight gain. The high
specificity helps to provide reliable reassurance to stressed parents that their children will
have a normal developmental outcome.
Using the preliminary MAI 6-month profile, the sensitivity of MAI at 6 months was
acceptable (70%) ,but less then the sensitivity at 4 and 8 months evaluation. We used a cut-
off score of 6 as recommended by the authors who proposed a preliminary 6-month profile
Discussion
68
based on MAI performance of 57, Six-month-old full term infants on MAI.
42
They
proposed 6-month profile which was based on normative approach as compared to the
degree of risk approach of development of 4- and 8- month MAI profiles. Consequently, a
score of >6 indicates infants deviation from normal development and not the infants
potential degree of risk for abnormal development. We used the only published 6-month-
profile available to us at the time of our study in order to evaluate its predictive validity in
high risk population which was not explored to date. The results indicate that the sensitivity
of-the preliminary 6-month MAI profile is inconsistent with the 4- and 8- month profiles and
suggests problem with the profile used. So our study contributes to the understanding of
accuracy of the preliminary 6-month profile in identifying risk of abnormal development.
We suggest that the preliminary profile should be revised based on degree of risk approach
and future studies of predictive validity can be carried out with the revised profile. Although
with limitations, the 6-month MAI profile has exhibited acceptable sensitivity and identified
70% of children with deviant or immature development at one year.
In comparing the sensitivity and specificity of 4-month, 6-month and 8- month MAI
scores relative to the 12-month PDI scores, the MAI at all ages has very good predictive
validity. The 4-month and 8-month MAI profiles showed better sensitivity in identification
of infants at increased risk for abnormal motor outcome at 12 months compared to the 6-
month profile. This supports the approach that was used to develop the 4-month and 8-
month profiles that is based on degree of risk and suggests that the normative approach used
to develop the preliminary 6-month profile is less effective in identification of infants with
developmental risk.
Discussion
69
The Pearsons Product Moment Correlation between the MAI Total Risk Scores and
categorical risk scores at 4, 6 and 8 months were highly significant for both MDI and PDI
scores of BSID-II at one year.
These results are similar to the findings of other reports on
correlation of MAI at 4 and 8 month with the BSID.
35, 36
Our study has additionally,
demonstrated strong correlation of 6 month MAI with 12 months BSID scores which was
not studied in the past
MAI is a test of infant neuromotor function and appropriately correlated with the
PDI of the Motor Scale at one year. The correlations between TRS and the PDI are similar
to correlations demonstrated by 4-month and 8-month MAI in low birth weight infants with
18months developmental outcome.
35
Similar correlations were reported of 4-month MAI
with neurodevelopmental outcome at 12 and 24 months.
36
The trends indicated by earlier
studies at 4 and 8 months and this study at 6- months are similar, indicating that the same
basic relationship of predictive validity exists, and encourages the clinical utility of the tool
at 6-months of age in very low birth weight infants.
At 4 months and 8 months, the TRS was the strongest correlation with motor
outcome at 12 months. This signifies the usefulness of the MAI in identifying the motor
problems. Among the categorical section scores, the strongest correlation with PDI at one
year was the Volitional Movement score of MAI at all three ages at p<0.001. Items in the
volitional movement section of the MAI include gross motor activities like prone weight
bearing, sitting, crawling, standing and walking. The Bayley motor scale at one year also has
gross motor items like pull to stand from floor, throwing ball, standing alone for 2sec and
walking.
28
Discussion
70
The finding that the TRS was the strongest predictor, with volitional movements also
very strong confirms earlier reports that combination of abnormal physical findings and
failure to pass at least one developmental milestone was a strong predictor of later cerebral
palsy than presence of neurological pathology alone.
171
The automatic reactions and muscle
tone section of 4 and 8 month MAI strongly correlated with the motor outcome that are
supported by the findings of Ross et al who reported relation between the individual items in
muscle tone and balance responses at 9 months and outcome with gross and fine motor
functions.
172
At 6 month strong correlation were obtained for automatic reaction and volitional
movements. The inability to bring hands to midline and maintain head in midline by 6
months indicates neurological problems.
35
The neuromaturational theory believes that
primitive reflexes have a time course of inhibition, which affects the emergence of
automatic responses and volitional movements.
173
But in the current study primitive reflexes
compared to other categorical scores of MAI was found to be less predictive of later motor
dysfunction at all three ages which is consistent with finding of other studies
35,36
although it
showed statistically significant correlations with motor outcome.
It is interesting that the MAI, an assessment of infants neuromotor function, was
significantly correlated with Bayley Mental Scale at one year. This could partly be due to
the test activities of the Mental Scale, which include many fine motor items like scribbling,
removing pellets from small container, putting beads in small box etc which compromise
the performance of children with neuromotor dysfunction, even if they have normal
intelligence. The test administered to assess cognition before 24 months requires a child to
perform the task physically to demonstrate that he has understood the task as they have very
Discussion
71
limited language skill. This places great demand on the childs motor skills and a child with
impaired motor function tends to perform less well on the mental items. This might be the
reason for the strong correlation obtained between the MAI and Bayley Mental Scale. This
is possibly true because in our study none of the children had isolated mental problems;
seven children had mental abnormality but along with motor abnormality .So the problems
indicated by the Bayley Mental Scale could be due to the associated motor dysfunction in
these children.
The other possible reason could be due to inter-relation between the motor and
mental functions via the neocerebellum and dorsolateral prefrontal cortex.
20
The functional
neuroimaging studies have shown activity in both structures during cognitive tasks involving
language or memory tasks. Activity in prefrontal cortex apart from cerebellum has been
observed in novel motor tasks and motor tasks involving timing.
Another potential strength of our study is that the BSID-II was used whereas most of
previous MAI studies have used BSID-I.
35, 36,150
According to the BSID-II manual, scores on
the newer version would be an average of 12 points lower on the MDI and 6 points lower on
PDI than if the older BSID version had been used. BSID-II new items added to address the
gaps in the content coverage of the scale. It is based on new normative data, so the
evaluation of VLBW based on the second edition provide better information on the
developmental status compared to old version.
28
The incidence of abnormal neurodevelopmental outcome as indicated by PDI 84 at
one year in VLBW was 28.33% which is higher than that reported in other studies of MAI in
VLBW infants
. 35,156
This could be due to the inclusion of suspect children (PDI of 70 to 84)
Discussion
72
as abnormal along with the children having significant delay/ cerebral palsy (PDI<70)
whereas other studies have included only those children with significant delay. The rate of
gross motor delay was 11.66% which is comparable to Indian hospital based study on
preterm infants with 12 month follow up period.
90
This study emphasis the need for strict monitoring programs for VLBW infants in
India with early intervention facilities as 28.33% of the sample in this study showed
neuromotor abnormality on MAI relative to PDI<84 which is definitely a serious concern in
terms of long term disability. The MAI demonstrated good predictive validity with Indian
infants, although the MAI has never previously been used with Indian infants. This confirms
that the MAI is based on the neuromotor fundamentals of normal and abnormal infant
development that are universal regardless of culture and location. Although with the
limitation of shorter duration of outcome; MAI gives the therapist an objective frame work
for assessment of Indian population of high risk VLBW babies.
LIMITATIONS OF THE STUDY:
The study has the limitation of shorter duration of follow up of one year, because the
diagnosis of cerebral palsy at one year and even at two years of age is unreliable particularly
in high risk infants who are more prone to demonstrate transient neurological signs.
Although our study did not focus on identification of significant delay or cerebral palsy
only, it included infants with PDI84 that is, infants with mild delay or suspicious
development which is another limitation. The score of PDI84 may only indicate immaturity
and not necessarily abnormal development. We choose to include PDI84 as this provided
larger number of abnormal children, and also encompasses suspicious children who
may ultimately have some impairment. This limits the predictive validity of MAI for
Discussion
73
neurodevelopmental abnormality relative to PDI84 only and does not actually represent its
validity for cerebral palsy or significant delay.
FUTURE SCOPE OF RESEARCH:
In view of limitation of shorter duration of follow up, studies with longer follow up
of at least 18 months or up to 3 years are recommended .Outcome evaluations using
diagnostic tools that have norms for Indian children would be better. Predictive validity
studies of MAI for Indian children who are born at term and exposed to perinatal and social
risk should be considered. Studies to revise the preliminary 6-month profile based on degree
of risk approach should be considered to enhance the predictive validities studies of MAI at
6-months.
Concl usion
74
CONCLUSION
1. MAI has high sensitive (82.3%) and specificity (74.4%) at 4-months and is clinically
useful tool in identifying neuromotor problems in VLBW infants as early as 4
months of age.
2. MAI at 6 months has high specificity (81.4%) with acceptable sensitivity (70%) and
identifies infants with normal neuromotor outcome at one year better.
3. The best combination of predictive values (sensitivity 82.3%, specificity 95.3%) for
MAI was obtained at 8 months age to identify VLBW infants with both normal and
abnormal neuromotor outcome at one year.
The Movement Assessment of Infants has very good predictive validity at all three
corrected ages, but the four and eight month profiles were more sensitive to identify
VLBW infants who would have delayed neuromotor development at one year of
corrected age than the six months profile used.
Summary
75
SUMMARY
Very Low Birth weight infants have higher prevalence of motor impairments with
poor developmental outcomes. They present in the form of subtle movement
disorders that are not identified by the traditional diagnostic tools as they focus on
the acquisition of motor milestones. Neuromotor tools that assess the quality of
movement are needed for early identification of these subtle motor dysfunctions, one
of them being Movement Assessment of Infant Scale. Since MAI assesses motor
dysfunction in high risk infants as early as four months of age, it was used in this
study which was undertaken:
To assess the validity of MAI for predicting neuromotor outcome in very low birth
weight infants at specific corrected ages of four, six and eight months during the first
year of life.
Out of 107 babies with birth weight 1500 grams admitted to NICU, 72 babies were
enrolled into the study based on eligibility; of which 12 babies dropped out and 60
babies completed all the required follow up assessments.
After routine examination of the babies at discharge from NICU, appointments for
MAI evaluations were given following which inter-rater and intra-rater reliability
was established between pair of examiners.
Summary
76
The babies were then subsequently evaluated on MAI scale at 4,6 and 8 months of
corrected ages following which neurodevelopmental outcome examination at one
year was done by clinical psychologist using Motor and Mental Scale of BSID-II
Data were analyzed in terms of sensitivity, specificity, Positive Predictive Value and
Negative Predictive Value and also by examining the relationship between MAI
scores and BSID-II scores using Pearsons Product Moment correlation. Students t
test was used to compare the TRS and BSID scores between the normal and
abnormal outcome groups. Association between the maternal and infant
characteristics with TRS and BSID was done
The results showed that 88% of the VLBW were preterm (mean GA=32.92.53)
with mean birth weight of 1365.5135.50. Majority of the mothers were in the age
range of 21 to 25 years.70% of them had education less then graduation and 71.66%
belonged to class I and Class II socioeconomic status families.
The incidence of neurodevelopmental problem was higher (28.33%) with significant
delay in 16.66% of the children .About 11.66% had both motor and cognitive delay
at one year.
The predictive validity of 4- month MAI for neuromotor outcome relative to PDI<84
was with a sensitivity of 82.3%, specificity 74.4%, PPV 56%, NPV 91.4%. The
sensitivity and specificity at 4 was higher indicating its ability to identify motor
dysfunction as early as four months of age. However the false positive rate was
higher at 4 months.
Summary
77
For 6-month MAI the sensitivity was 70.6%, specificity 81.4%, PPV 70%, and NPV
87.5% .It shows an acceptable sensitivity with high specificity. However, the
sensitivity of 6-month MAI was inconsistent with that of 4 and 8 months, indicating
the need for revision of the 6-month profile.
Similarly for 8-month MAI the sensitivity was 82.3%, specificity was 95.3%, PPV
87.5%, NPV 93.2% indicating the best combination of predictive validity. The PPV
was higher which could be due to higher prevalence (28.33%) of neuromotor
problem at 8 month. The higher specificity at 8 months discriminates infants with
normal outcome better.
On comparing the predictive validity at all three ages, the 4 and 8 months MAI
profiles were more sensitive to identify infants with delayed development compared
to 6 month profile used.
The correlation between the MAI Total Risk Scores and categorical risk scores at 4,
6 and 8 months were highly significant with p < 0 .001 for both MDI and PDI scores
of BSID-II at one year. This indicated that MAI at all three ages can significantly
predict cognitive outcome at 12 months apart from motor outcome.
Among the categorical section scores, the strongest correlation with PDI at one year
was the Volitional Movement score of MAI at all three ages at p < 0.001
On comparing the MAI scores of infants in normal and abnormal outcome groups
relative to PDI<84 ,the infants with abnormal outcome had significantly higher risk
scores then normal outcome group at all three ages p<0.001.
Summary
78
The abnormal outcome group had significantly less MDI and PDI scores then the
infants in normal outcome(p<0.001) indicating poor cognitive and motor
performance of VLBW infants with higher MAI risk scores.
There was significant association between the educational status of the mother and
TRS of MAI at 4, 6 and 8 months and PDI scores at 12 months p<0.05 but no
association was found with other maternal variables
There was significant positive correlation between the duration of stay in NICU with
TRS scores and significant negative correlation between the duration of stay and
BSID scores indicating poor developmental outcome with longer NICU stay
There was no correlation between the number of neonatal problems and the TRS or
MDI scores except for significant relation with PDI at p<0.003.
Bibliography
79
BIBLIOGRAPHY
1. UNICEF. Low birth weight: Country, regional, global estimates. New York: The
United Nations Childrens Fund and World Health Organization, 2004.
2. Stewart AL, Roth SC. Neurodevelopmental Outcome part 1.In: Janet MR, Roberton
NRC. Textbook of Neonatology.3
rd
Ed.Edinburgh.Churchill Livingstone publishers;
1999 ; p 79-100.
3. Koops BL, Morgan LJ, Battaglia FC. Neonatal mortality risk in relation to birth
weight and gestational age: update. J Pediatr 1982; 101 : 969-77.
4. Botting N, Powls A, Cooke RW, Maelow N: Attention deficit hyperactivity disorders
and other psychiatric outcomes in very low birth weight children at 12 years: J Child
Psychol Psychiatry 1997 ; 38: 931-41.
5. Were FN, Bwibo N O: Two year neurological outcome of very low birth weight
infant. East African American Journal 2006; 83 : 243- 249.
6. Vohr BR, Wright LL, Dusick AM, et al. Neurodevelopmental and functional
outcomes of extremely low birth weight infants in the National Institute of Child
Health and Human Development Neonatal Research Network, 1993-1994.Pediatrics
2000;105:1216-1226.
7. Stewart A, Pezzani- Goldsmit M, Amiel-Tison C, Stewart A. The newborn infant:
one brain for life. Les Editions INSERM, Paris.1994, pg 151-166.
8. Piecuch RE. Outcome of extremely low birth weight infants (500 to 999 grams) over
a 12- year period. Pediatrics 1997; 100:633-9.
Bibliography
80
9. Jongmans M,Mercuri E,de Vries L,Dubowitz L,Henderson SE.Minor neurological
signs and perceptual-motor difficulties in prematurely born children.Arch Dis child
1997;76:9-14.
10. Msall ME, Tremont MR .Measuring Functional outcome after prematurity:
Developmental impact of Very low birth weight and extremely low birth weight
status on childhood disability. Ment Retard Dev Disabil Res Rev 2002; 8; 258-72.
11. F oulder-Hughes LA,Cooke RW.Motor,cognitive, and behavioural disorders in
children born very preterm.Dev Med Child Neurol 2003;45:97-103.
12. Elliman AM, Brayan EM, Elliman AD, Walker J, Harvey DR. Coordination in low
birth weight seven- year old. Acta Paediatrica 1991;80:316-322.
13. Hellgren L, Gillberg C, Gillberg IC, Enerskog I. Children with deficits in attention,
motor control and perception (DAMP) almost grown up:general health at 16
years.Dev Med and Chil Neurol 1993;35:881-892.
14. Dammann O, walther H, Allers B et al. Development of a regional cohort of very
low birth weight children at six years:cognitive abilities are associated with
neurological disability and social background. Dev Med and Chil Neurol
1996;38:97-108.
15. Jeng SF, Yau KI, Liao HF, Chen LC, Chen PS: Prognostic factors for walking
attainment in very low-birth weight pre term infants; Early Hum Dev 2000; 59: 159-
73.
16. Tessier R, Nadeau L, Boivin M, Tremblay RE. The social behaviour of 11- to 12-
year-old children born as low birthweight and/or premature infants. Int J Behav Dev
1997 ; 21 : 795-811.
Bibliography
81
17. Powls A, Botting N, Cooke RW, Marlow N. Motor impairment in children 12 to 13
years old with a birthweight of less than 1250 g. Arch Dis Child Fetal Neonatal Ed.
1995;73 : p 62-66.
18. Feder KP, Majnemer A, Bourbonnais D, Platt R, Blayney M, Synnes A. Handwriting
performance in preterm children compared with term peers at age 6 to7 years. Dev
Med Child Neurol 2005;47:163-170.
19. Piek JP, Dawson L, Smith LM, Gasson N. The role of early fine and gross motor
development on later motor and cognitive ability. Hum Mov Sci 2008;27:668-681.
20. Diamond A. Close interrelation of motor development and cognitive development
and of the cerebellum and prefrontal cortex. Child Dev 2000 ; 71 : 44-56.
21. Losch H, Dammann O. Impact of motor skills on cognitive test results in very-low-
birthweight children. J Child Neurol 2004;19:318-322.
22. Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and
behavioral outcomes of school-aged children who were born preterm: a meta-
analysis. JAMA 2002 ; 288 : 728-737.
23. Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-
analysis of neurobehavioral outcomes in very preterm and/or very low birth weight
children. Pediatrics 2009 ; 124.
24. Vaccarino FM, Ment LR. Injury and repair in the developing brain. Arch Dis Child
Fetal Neonatal Ed 2004 ; 89 : 19092.
25. Knobloch H, Pasamanick B. Gessel and Armatrudas Development of Normal and
Abnormal Neurophysiologic Development in Infancy and early Childhood.
Hagerstown, MD: Harper and Row; 1974.
Bibliography
82
26. Folio MR, Fewell PR. Peabody Developmental Motor Sclaes and Activity Cards
Manual. Allen, TX: DLM Teaching Resources; 1983.
27. Frankenburg WK, Dodds J, Archer P. Denver II Training Manual. Denver, CO:
Denver Developmental Materials Inc; 1992.
28. Bayley N.Bayleys scale Of Infant Development.2nd ed.New York: The
Psychological Corporation, 1993
29. Jeng S, Tsou Yau K, Chen L, Hsiao S. Alberta Infant Motor Scale: Reliability and
validity when used on preterm infants in Taiwan. Phys Ther 2000 ; 80 : 168-78.
30. Easley A. Dynamic assessment for infants and toddlers: the relationship between
assessment and the environment. Pediatr Phys Ther 1996 ; 8 : 62-9.
31. Piper MC, Darrah J. Alberta Infant Motor Scale. Philadelphia; WB Saunders: 1995.
32. Campbell SK.The Test of Infant Motor Performance : Test Users Manual Version
1.4. Chicago, 1II : Infant Motor Performance Scales ; 2001.
33. Einspieler C,Prechtl HF, Bos AF, Ferrari F, Gioni G.Prechtls Method on the
Qualitative Assessment of General Movements in Preterm,Trem and young Infants.
Clinics in Developmental Medicine No.167.London: Mac Keith Press,2004.
34. Rosenbaum P. Variation and abnormality: recognizing the differences. J Pediatr
2006; 149: 59394.
35. Swanson MW, Bennett FC, Shy KK, et al. Identification of neurodevelopmental
abnormality at four and eight months by the movement assessment of infants. Dev
Med Child Neurol 1992; 34: 321-337.
Bibliography
83
36. Harris SR, Swanson MW, Andrews MS, et al. Predictive validity of the Movement
Assessment of Infants. J Dev Behav Pediatr 1984; 5: 336-342.
37. Harris SR. Early detection of cerebral palsy: sensitivity and specificity of two motor
assessment tools. J Perinatol 1987; 7: 11-15.
38. Nair MKC,Babu George,Suja mathews, Susan, Lekshmi and Elsie Philip. Early
Intervention Program for high risk babies-Use of Infant Motor Screen. Ind Jr of
Pediatr 1992;59 : 687-690.
39. Salokorpi T, Rajantie I, Kivikko I, Haajanen R ,Rajantie J. Predicting neurological
disorders in infants with extremely low birth weight using Movement Assessment of
infants. Pediatr Phys Ther 2001 ; 13 : 106-109.
40. Fetters L, Tornick E. Neuromotor Development of Cocaine-exposed and Control
Infants from Birth through 15 Months: Poor and Poorer Performance. Pediatrics
1996 ; 98 : 938-943.
41. Ruth Rose-Jacob,Howard Cabral, Marjorie Beeghly et al. The Movement
Assessment of Infants (MAI) as a Predictor of Two-Year Neurodevelopmental
Outcome for Infants Born at Term Who Are at Social Risk. Ped Phys Ther 2004 ; 16
: 212221.
42. Washington K, Deitz JC. Performance of full term 6 month old infants on the
Movement Assessment of Infants. Ped Phys Therapy 1995 ; 7 : 65-74.
43. World Health Organization. International Statistical classification of diseases and
related health problems, Tenth revision. World Health Organization, Geneva, 1992
44. Park K. Text book of preventive and social medicine 18
th
ed. Jabalpur: Babaridas
Bhanot publishers; 2008.
Bibliography
84
45. Neonatal morbidity and mortality: Report of the National Neonatal Perinatal
Database. Indian Pediatr 1997 ; 34 : 1089-1092.
46. World Health Organization. The global burden of disease: 2004 update. Geneva,
World Health Organization; 2008.
47. Ferrari F. Neuropsychic follow-up of the premature infant: mortality, severe
sequelae, early diagnosis and prognosis. Pediatr Med Chir 1982; 4:621-33.
48. Wang CJ, McGlynn EA, Brook RH, Leonard CH, Piecuch RE, Hsueh SI, et al.
Quality-of-care indicators for the neuro-developmental follow up of very low birth
weight children: results of an expert panel process. Pediatrics 2006; 117: 2080
2092.
49. Singh M. Care of the Newborn. 6
th
Edn. New Delhi: Sagar Publications; 2004.
50. Caraballo RH, Sakr D, Mozzi M, et al. Symptomatic occipital lobe epilepsy
following neonatal hypoglycemiaPediatr Neurol 2004, 31:249.
51. Hawdon JM: Hypoglycaemia and the neonatal brain. Eur J Pediatr 1999;158:S9-S12.
52. Rozance PJ, Hay WW. Hypoglycemia in newborn infants: Features associated with
adverse outcomes.Biol Neonate 2006;90:74-86.
53. Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate
neonatal hypoglycemia. BMJ 1988; 19 : 1304 - 8.
54. Duvanel CB, Fawer CL, Cotting J, Hohlfeld P, Matthieu JM. Long-term effects of
neonatal hypoglycemia on brain growth and psychomotor development in small-for-
gestational-age preterm infants. J Pediatr 1999 ; 134 : 389-91.
55. Tomaszewska M, Eileen S, Minich, NM, Friedman H. Pulmonary Hemorrhage:
Clinical Course and Outcomes Among Very Low-Birth-Weight Infants. Arch Pediatr
& Adolesc Med 1999; 153:715-721.
Bibliography
85
56. Taeusch WH, Ballard RA, Gleason CA. Avery's Diseases of the Newborn. 8
th
Ed,
Philadelphia: Elsevier Saunders; 2004.
57. Martin R, Abu-Shaweesh, Baird T. Pathophysiologic mechanisms underlying apnea
of prematurity. Neo Rev 2002; 3: p59-65.
58. Janssen D, Carnielli V, Cogo P, Bohlin K, Hamvas A, Luijendijk I et al. Surfactant
phosphatidylcholine metabolism in neonates with meconium aspiration syndrome.
Journal Pediatr 2006; 149: 634-9.
59. Cloherty JP, Eichenwald EC, Stark AR. Manual of neonatal care. 5
th
Ed.
Philadelphia: Lippincott Williams and Wilkins; 2004.
60. Hegyi T, Carbone T, Anwar M, Ostfeld B, Hiatt M, Koons A, et al. The Apgar score
and its components in the preterm infant. Pediatrics 1998; 101: p 77-81.
61. Moster D, Lie RT, Irgens LM, Bjerkedal T, Markestad T. The association of Apgar
score with subsequent death and cerebral palsy: a population-based study in term
infants. J Pediatr 2001 ; 138 : 798-803.
62. Thorngren-Jerneck K, Herbst A. Perinatal factors associated with cerebral palsy in
children born in Sweden. Obstet Gynecol 2006 ; 108 : 1499-505.
63. OShea TM, Klinepeter KL, Dillard RG. Prenatal events and the risk of cerebral
palsy in very low birth weight infants. Am J Epidemiol 1998 ; 147 : 362-9.
64. Grether JK, Nelson KB, Emery ES III, Cummins SK. Prenatal and perinatal factors
and cerebral palsy in very low birth weight infants. J Pediatr 1996 ; 128 : 407-14.
65. Kari Kveim Lie, Else-Karin G, Anne Eskild. Association of cerebral palsy with
Apgar score in low and normal birthweight infants: population based cohort study.
BMJ. 2010 ; 341: c4990.
Bibliography
86
66. Dimmit R, Moss RL. Clinical management of necrotizing enterocolitis. NeoReviews
2001 ; 2 : 100-117.
67. Dewey KG, Heinig MJ, Nommsen-Rivers LA. Differences in morbidity between
breast-fed and formula-fed infants. J Pediatr 1995 ; 126 : 696-702.
68. Kovar MG, Serdula MK, Marks JS, Fraser DW. Review of the epidemiologic
evidence for an association between infant feeding and infant health. Pediatr 1984;
74: 615-38.
69. Jyoti Batra and Archana Sood. Iron Deficiency Anaemia : Effect On Congnitive
Development In Children : A Review. Indian Journal of clinical Biochemistry 2005;
20: 119-125.
70. Cloherty JP, Eichenwald EC, Stark AR. Manual of Neonatal Care. 5
th
Ed.
Philadelphia: Lippincott Williams and Wilkins; 2004.
71. Steward DK, Pridham KF. Growth patterns of extremely low-birth-weight
hospitalized preterm infants. J Obstet Gynecol Neonatal Nurs 2002 ; 31: 57-65.
72. Fanaroff, Avroy A., Korones, Sheldon B, Wright, Linda L, Verter, Joel et al.
Incidence, presenting features, risk factors and significance of late onset septicemia in
very low birth weight infants: Pediatric Infectious Disease Journal 1998;17:593-598
73. Holcroft, Cynthia J, Blakemore, Karin J, Allen, Marilee, Graham, Ernest M:
Association of Prematurity and Neonatal Infection with Neurologic Morbidity in
Very Low Birth Weight Infants. Obstetrics & Gynecology 2003; 101:1249-12531.
74. Singh M. Care of the Newborn. 6
th
Edn. New Delhi: Sagar Publications; 2004.
75. Thornberg E, Thiringer K, Odeback A, Milson I. Birth asphyxia: Incidence, clinical
course and outcome in a Swedish population. Acta Paediatr 1995; 84: 927-32.
Bibliography
87
76. Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, Bellagio. Child Survival
Study Group. How many child deaths can we prevent this year? Lancet 2003; 362:
65-71.
77. Ek U, Fernell E, Jacobson L. Relation between blindness due to retinopathy of
prematurity and autistic spectrum disorders: a population- based study. Dev Med
child Neurol 1998 ; 40 : 297301.
78. Versaw-Barnes D, Wood A. The Infant at High Risk for Developmental Delay. In:
Tecklin JS. Pediatric Physical Therapy.4
th
ed. Baltimore, MD. Lipincott Williams
and Wilkins ; 2008. p 101-175.
79. Volpe JJ. Neurology of the Newborn. 4th ed. Philadelphia: WB Saunders Co; 2000.
80. Walstab, Janet E, Bell, Robin J, Reddihough, Dinah S et al. Factors identified during
the neonatal period associated with risk of cerebral palsy: Australian & New Zealand
Journal of Obstetrics & Gynaecology 2004 ; 44 : 342-346
81. Flynn JT. Retinopathy of prematurity: perspective for the nineties. Acta Opthalmol
Scand 1995 ; 73 : 1214.
82. Ek U, Fernell E, Jacobson L, et al. Relation between blindness due to retinopathy of
prematurity and autistic spectrum disorders: a population- based study. Dev Med
child Neurol 1998 ; 40 : 297301.
83. Michael EM, Dale LP, Kathleen MD, Velma Dobson, Betty Tung, Richard EM,
Graham EQ, James DR et al. Severity of Neonatal Retinopathy of Prematurity Is
Predictive of Neurodevelopmental Functional Outcome at Age 5.5 Years. Pediatrics
2000 ; 106 : 998 1005.
Bibliography
88
84. Fielder AR. The impact of birth weight on the visual pathway. Br J Ophthalmol 1998
; 82: 1-2.
85. Mohammadzadeh A, Derakhshan A, Ahmadshah F, Amiri R, Esmaeli H. Prevalence
of visual impairment in low birth weight and normal birth weight school age
children. Iran J Pediatr 2009 ; 19 : 271-6.
86. Sanjiv BA, Diane Prinzing, Gary Myers. Hyperbilirubinemia and Language Delay in
Premature Infants. Pediatrics 2009 ; 123: pp. 327-331.
87. Stewart AL, Reynolds EO, Lipscomb AP. Outcome for infants of very low birth
weight: survey of world literature. Lancet 1981 ; 9 : 1038 - 40.
88. Calame A, Prod'hom LS, Van Melle G. Outcome of infants of very low birth weight
treated in neonatal intensive care unit. Rev Epidemiol Sante Publique 1977 ; 25:21-32.
89. Bhargava S K, Kumari S, Pandit et al. Outcome of low birth weight children. LAMS
1975; 11: 77-99.
90. Tandon A, Kumari S, Ramji S, Malik A, Singh S, Nigam V R. Intellectual psycho
educational and functional status of low birth weight survivors beyond 5 years of
age. Ind J Pediatr 2000; 67: 791-796.
91. Choudhari S, Otiv M, Chitale A, Pandit A, Hoge M .Pune low birth weight study-
cognitive abilities and educational performance at 12 years. Indian Pediatr2004; 41:
114-128.
92. V. K. Paul, S. Radhika, A. K. Deorari and Meharban Singh. Neurodevelopmental
outcome of at risk nursery graduates. Indian Journal of Pediatrics 1998; 65: p 857-
862.
Bibliography
89
93. Miriam Rieck Ilan Arad Dvorah Netzer .Developmental Evaluation of Very-low-
birth weight Infants: Longitudinal and Cross-sectional Studies; International Journal
of Behavioral Development 1996; 19: 549-562.
94. Schubiger G, Lanz FZ, Caflisch U, Lanz C. Development of formerly preterm
infants with a birth weight of below 1500 grams: concept and results of a follow-up
program in up to school-aged children in central Switzerland. Schweiz Med
Wochenschr 1999 ; 129 : 1025-32.
95. Berger I. The development of very low birth weight preterm infants. Harefuah. 2004;
143 : 811- 838.
96. Mukhopadhyay K, Malhi P, Mahajan R, Narang A. Neurodevelopmental and
behavioral outcome of very low birth weight babies at corrected age of 2 years.
Indian Journal of Pediatrics 2010 ; 77 : 963-7.
97. Cornelieke Sandrine, Hanan Aarnoudse-Moens, Nynke Weisglas-Kuperus,Johannes
Bernard van Goudoever, and Jaap Oosterlaan.Meta-Analysis of Neurobehavioral
Outcomes in Very Preterm and/or Very Low Birth Weight Children. Pediatrics 2009;
124:717728.
98. Mazer B, Piper M, Ramsay M.Developmental outcome in very low birth weight
infants 6 to 36 months old. J Dev Behav Pediatr1988;9:293-7.
99. Maureen Hack, Mark Schluchter, Lydia Cartar, Mahboob Rahman, Leona Cuttler,
and Elaine Borawski. A study on Growth of Very Low Birth Weight Infants to Age
20 Years pediatrics 2003 ; 112 : p30 38.
100. Theunissen NC, Veen S, Fekkes M. Quality of life in preschool children born
preterm. Dev Med Child Neurol 2001;43:460465.
Bibliography
90
101. Fekkes M, Theunissen NC, Brugman E. Development and psychometric evaluation
of the TAPQOL: a health-related quality of life instrument for 1-5 years old
children. Qual life Res 2000 ; 9 : 961972.
102. Chien LY, Chou YH, Ko YL, Lee CF. Health-related quality of life among 3-4
year-old children born with very low birth weight. J Adv Nurs 2006; 56:916.
103. Eiser C, Eiser JR, Mayhew AG, Gibson AT. Parenting the premature infant:
balancing vulnerability and quality of life. J Child Psychol Psychiatry 2005;
46:11691177.
104. Klassen AF, Lee SK, Raina P, Chan HW, Matthew D, Brabyn D. Health status and
health-related quality of life in a population based sample of neonatal intensive care
unit graduates. Pediatrics 2004; 113:594600.
105. Indredavik MS, Vik T, Heyerdahl S, Romundstad P, Brubakk AM. Low-
birthweight adolescents: quality of life and parent child relations. Acta Pediatr
2005; 94:12951302.
106. Johnson A, Bowler U, Yudkin P, et al. Health and school performance of teenagers
born before 29 weeks gestation. Arch Dis Child Fetal Neonatal Ed 2003; 88
:p190198.
107. Jorrit F. de Kieviet, Jan P. Piek, Cornelieke S. Aarnoudse-Moens, Jaap Oosterlaan:
Motor Development in Very Preterm and Very Low-Birth-Weight Children-A
Meta analysis. JAMA 2009; 302:2235-2242.
108. Williamson WD, Wilson GS, Lifschitz MH and Thurber SA. Non handicapped
Very Low Birth Weight Infants at One Year of Age: developmental Profile. Pediatr
1990; 85: p. 405-410.
Bibliography
91
109. Erikson C, Allert C, Carlberg EB, Katz-Salamon M. Stability of longitudinal motor
development in very low birth weight infants from 5 months to 5.5 years. Acta
Paediatrica 2003; 92: p 197 203.
110. Medoff-Cooper, Barbara MS, Schraeder, Barbara DM. Developmental Trends and
Behavioral Styles in Very Low Birth Weight Infants. Nursine Research 1982; 31:
68-72.
111. Robertson CMT, Etches PC & Kyle JM: Eight-year school performance and growth
of preterm, small for gestational age infants: A comparative study with subjects
matched for birth weight or for gestational age. J Pediatrics1990; 116: 19-26.
112. Allen M, Alexander G. Gross motor milestones in preterm infants: Correction for
degree of prematurity. The Journal of Pediatrics 1990 :116: p 955-959.
113. Simons CJ, Mandich MB ,Ritchie SK,Martha .Assessment of Motor Development
in Very Low Birth Weight Infants. Jr of perinatology 2000 ; 3 : 172-175.
114. Amess P, McFerran C, Khan Y, Rabe H. Early prediction of neurological outcome
by term neurological examination and cranial ultrasound in very preterm infants.
Acta Paediatr 2009 ; 98 : p 448-453.
115. Escobar GJ, Littenberg B, Petitti D. Outcome among surviving very low birth weight
infants: a meta-analysis. Archives of disease in childhood 1991 ; 66:204-211.
116. Ancel PY. Severe sensorineural impairment in very premature infants:
epidemiological aspects. J Gynecol Obstet Biol Reprod 2004; 33:461-74
117. Protection of the Developing Brain of Very Low Birth Weight Infants,
2/1995 UCP: Research & Educational Foundation, February 1995. Available
from;URL:http://www.ucpresearch.org/fact-sheets/protection-developing-brain.php
Accessed on 2.5.2010.
Bibliography
92
118. Criteria for Determining Disability in infants and children: Low Birth Weight
(Evidence Report / Technology Assessment, Number 70) Available from; URL:
http://www.ahrq.gov/clinic/epcsums /lbwdissum. pdf Accessed on 21.08.2010.
119. Chaudhari S, Kulkarni S, Barve S, Pandit AN, Sonak U, Sarpotdar N. Neurologic
sequelae in high risk infants-a three year follow up. Indian Pediatr 1996;33:645-53.
120. Stuberg WA. The Milani Comparetti Motor Development Screening Test. 3
rd
ed.
rev., Omaha, NE: University of Nebraska Medical Centre; 1992.
121. Sudha C. Developmental assessment tests: Scope and limitations. Indian Pediatrics
1996; 33:541-5.
122. Kirsten RH,Mijna HA.Evaluation of Neuromotor function in Infancy-A systematic
Review of Available Methods. J Dev Behav Pediatr 2008 ; 29: 323-323.
123. Amiel-Tison C. Update of the Amiel-Tison neurologic assessment for the term
neonate or at 40 weeks corrected age. Pediatr Neurol 2002; 27: 196-212.
124. Nickel RE, Renken CA, Gallenstein JS.The Infant Motor screen. Dev Med Child
Neurol 1989; 31:35-42.
125. Campbell SK, Kolobe TH, Osten ET, Lenke M, Girolami GL.Construct Validity of
test of infant motor performance.Phys Ther 1995;75:585-96.
126. Campbell SK, Kolobe THA. Concurrent Validity of the Test of Infant Motor
Performance with Alberta Infant Motor Scale. Pediatr Phys Ther 2000;12:2-9.
127. Case-Smith J, Bigsby R. Posture and Fine Motor Assessment of Infants. San
Antonio, TX : Therapy Skill Builders, 2000.
Bibliography
93
128. Miller LJ, Roid GH.The TIME Toddler and Infant Motor Evaluation: A
Standardized Assessment. Tucson, AZ : Therapy Skill Builders, 1994
129. Burns YR, Ensbey RM, Norrie MA. The Neuro-Sensory Motor Development
Assessment part 1: development and administration of the test. Aust J
Physiother1989; 35:14157.
130. Misra N,Pathak.P. Developmental Assessment Scales for Indian Infants (DASII):
Manual, Baroda,M.S. University of Baroda,1996.
131. Malik GK, Yadav A, Trivedi R, Srivastava A, Prasad KN, Gupta RK. Temporal
alterations in brain water diffusivity in neonatal meningitis. Acta Paediatr 2009 ; 98
: 1426-32.
132. Gupta. S, Bhargava. S. Play based stimulation program for infants with cerebral
palsy and mental retardation. Asia Pacific Disability Rehabilitation journal 2008 ;
19:p 114-121.
133. Carol HL, Robert EP, Bruce AC. Use of the Bayley Infant neurodevelopmental
screener with Low birth weight infants. J Pediatr Psychol 2001; 26: 33-40.
134. Barrera ME, Cunningham CE, Rosenbaum PL. Low birth weight and home
intervention strategies: Preterm Infants. Developmental and Behavioral Pediatrics
1986; 7:361-366.
135. Barrera ME, Rosenbaum PL, Cunningham CE. Corrected and Uncorrected Bayley
Scores : Longitudinal developmental patterns in low and high birth weight preterm
infants. Infant Behavior and Development 1987 ; 10:337-346.
136. Watt J. Interaction and development in first year: I. The effects of prematurity.
Early Human Development 1986;13:195-210.
Bibliography
94
137. Wolf Mj, Koldewijn K, Beelen A, Smit B, Hedlund R, De Groot Jm.
Neurobehavioral and developmental profile of very low birth weight preterm
infants in early infancy. Acta paediatrica 2002; 91: 930-938.
138. Nichols A and Latchman A. Stability of the Bayley mental scale of the infant
development with high risk infants. The British Jr of Dev Disabilities.2002;48:3-13.
139. Provost B, Heimerl S, Meclain C, Kim N, Brain RL and Kodituwakku P.
Concurrent validity of the Bayley Scale of Infant Development-II Motor scale with
the Peabody developmental motor scale-2 in children with developmental delay at
12 months. Pediatr Phys Ther 2004;16:149-156.
140. Chandler LS, Swanson MW, Andrews MS. Movement Assessment of Infants: A
Manual. Rolling Bay, Washington: 1980.
141. Susan R. Harris and Carolyn B Heriza. Measuring Infant Movement Clinical and
technological assessment techniques. Phys Ther1987; 67:1877-1880.
142. Campbell SK: Movement Assessment of Infants: An evaluation. Physical and
Occupational Therapy in Pediatrics1981; 1:53-57.
143. Harris SR, Haley SM, Tada WL, et al: Reliability of observational measures of the
Movement Assessment of Infants. Phys Ther.1984; 64:471-475.
144. Jane W. Schneider, Wynne Lee,Ira J Chasnoff. Field testing of the Movement
Assessment of Infants. Phys Ther1988; 68: 321-327.
145. Brander, Rosemary; Kramer, John et al: Inter-Rater and Test-Retest Reliabilities of
the Movement Assessment of Infants. Pediatric Physical Therapy1993; 5:16-21.
146. Boyce WF, Gowland C, Rosenbaum PL et al. Measuring quality of movement in
cerebral palsy:a review of instruments. Phys Ther 1991 ; 7 : 813-819.
Bibliography
95
147. Palisano RJ. Review of research on reliability and validity of the Movement
Assessment of Infants. Pediatrics in Physical Therapy1989 ; 1 : 167-172.
148. Darrah J, Piper MC, Byrne PJ, Waren S. Utilization of the Movement Assessment
of Infants risk profiles with preterm infants. Phys and Occup Ther in Pediatrics
1991; 11:1-12.
149. Washington, Kathleen A, Harris, Susan R. Mental and Motor Performance of Low-
Birth weight Infants with Normal Developmental Outcomes. Pediat Phys Ther
1989; 1: p 159-165.
150. Paban, M., Piper, M.C. Early predictors of one year neurodevelopmental outcome
for at risk infants. Phys and Occup Ther in Pediatr1987; 7:17-34.
151. Susan R Harris. Early Neuromotor Predictors of Cerebral Palsy in Low-Birth
weight Infants. Dev Med and child Neurol 1987;29:508-519.
152. Lacerda, Tatiana Teixeira Barrel, Magalhaes,Livin de Castro. Item validity analysis
of Movement Assessment of Infants - MAI - to preterm infants. Rev. Bras. Saude
Mater Infant 2006; 6: 297-308.
153. Colleen CT, Deitz J, Joyce M, and Wendel ES. Performance of 6-Month-Old
Asian American Infants on the Movement Assessment of Infants: A Descriptive
Study .Phy & Occ Therapy in Pediatrics 2000: 19; 5-23.
154. .Jean.C.Deitz, Terry K. Crowe, Susan R. Harris: Relationship between Infant
Neuromotor Assessment and Preschool Motor Measures. Physical
Therapy1987:67:14-17.
155. Lydic JS, Short MA, Nelson DL: Comparison of two scales for assessing motor
development in infants with Down's syndrome. The Occupational Therapy Journal
of Research1 983 ; 3 : 213-221.
Bibliography
96
156. Cardoso
AA, Magalhaes
LC, Amorim
RH, Paixao ML, Mancini
MC, Rossi LD.
Predictive Validity of the Movement Assessment of Infants for Brazilian Preterm
Children. Archives of Neuropediatrics 2004 ; 62 : 1052-7.
157. Darrah J, Piper M, Watt MJ .Assessment of gross motor skills of at-risk infants:
predictive validity of the Alberta Infant Motor Scale. Dev Med Child Neurol 1998;
40 : 485-91.
158. Fetters L, Tornick E. Discriminate Power of the Albert Infant Motor Scale and the
Movement Assessment of Infants for the prediction of Peabody Gross Motor scale
scores of infants exposed in utero to Cocaine. Pediatr Phys Ther 2000; 12:16-23.
159. Salamon MK, Gerner EM, Jonsson B, Lagercrantz H. Early motor and mental
development in very preterm infants with chronic lung disease. Arch Dis Child
Fetal Neonatal Ed 2000; 83:p16.
160. Vickie AM, Jane KS, Lynette SC and Barbara JW. Identifying 4-Month-Old
Infants at Risk in Community Screening. Pediatr Phys Ther 2009; 21:150157.
161. Ravenscroft, Eleanor F, Harris, Susan R. Is Maternal Education Related to Infant
Motor Development? Pediatric Physical Therapy 2007; 19: 56-61
162. Kulkarni AP, Baride JP. Textbook of Community Medicine 1
st
Ed. Mumbai; Vora
Medical Publications: 1998.
163. Drillien. CM:Abnormal neurologic signs in the first year of life in low birth weight
infants: possible prognostic significance. Dev Med Child Neurol, 14,575-584, 1972.
164. Saint-Anne DS. Normality and normalization as seen in long term neurological
follow up of 286 truly premature infants. Neuropediatrics 1979; 10:226-244
Bibliography
97
165. Georgieff MK, Bernbaum JC.Abnormal shoulder girdle muscle tone in premature
infants during their first 18 months of life. Pediatrics1986; 77:664-9.
166. Anderson PJ, Doyle LW.Neurodevelopmental outcome of bronchopulmonary
dysplasia. Semin Perinatol 2006 Aug ; 30:227-32.
167. Skidmore MD, Rivers, Hack M. Increased risk of cerebral palsy among very low
birth weight infants with chronic lung disease. Dev Med and Chil Neurol 1990;
32:325-332.
168. Markestad T, Fitzhardinge PM. Growth and development in children recovering
from bronchopulmonary. Jr of Pediatr 1981 ; 98 : 597-602.
169. Bennett FC, Robinson NM, Sells CJ.Hyaline membrane disease, birth weight, and
gestational age.American J of Diseases of children 1982 ; 136 : 888- 891.
170. Chaudhari S, Bhalerao M, Chitale A, Patil B, Pandit A and Hoge M. Transient
Tone Abnormalities in High Risk infants and cognitive outcome at five years.
Indian Pediatrics 2010; 47:p 931-5.
171. Elleberg J. H, Nelson K.B. Early recognition of infants at risk for cerebral palsy :
examination at age four months. Developmental and child neurology1981;23,705-
716.
172. Ross.G, Schechner.S, Frayer.W.W, Auld P.A. Perinatal and neurodevelopmental
predictors of one year outcome in infants 1500 grams. Seminars in perinatology
1982 ; 6 : 317-326.
173. Case- smith J. Analysis of current motor development theory and recently
published infant motor assessments. Inf Young Children1996; 9:29-41.
Annexure I Tables
98
TABLES
Table No. 1 : Maternal Characteristics
Variable No Percentage
Age
20 09 15%
21-25 26 43.33%
26-30 18 30%
>31 07 11.66%
Educational status
Primary education 06 10%
Secondary education 20 33.33%
Higher secondary education 16 26.66%
Graduation 13 21.66
Post graduation 05 8.33%
Socioeconomic Status
Class I 24 40%
Class II 19 31.66%
Class III 17 28.33%
Class IV 0 0
Class V 0 0
Annexure I Tables
99
Table No. 2 : Infant Characteristics
Variable Mean (SD)* or % (N)
Birth weight(gms)* 1365.5135.50
Gestational age (wks)* 32.92.53
No of days in NICU* 20.212.53
Males
Females
55% (33)
45% (27)
Preterm VLBW
Term VLBW
88% (53)
12% (07)
No of neonatal problems
<3
3-6
>6
58.33% (35)
41.33% (25)
0% (0)
*Mean (SD) Percentage (N)
Table No. 3 : Neonatal problems in the VLBW infants during their NICU stay
Neonatal problems No of Infants %
Sepsis 33 55
Hyperbilirubinemia 47 78.33
Hypoglycemia 27 45
Hypotension 7 11.66
Birth asphyxia 8 13.33
Apnea 11 18.3
Convulsion 4 6.66
RDS 8 13.33
Mechanical ventilator 6 10
Annexure I Tables
100
Table No. 4 : Mean scores of MAI at 4, 6 and 8 month
MAI score 4-month scores 6-month scores 8-month score
Mean SD Mean SD Mean SD
Total Risk Score 9.95 7.10 6 8.33 8.06 10.04
Muscle Tone 4.96 2.69 1.31 1.89 1.31 1.89
Primitive Reflex 1.5 1.74 1.3 1.83 1.3 1.83
Automatic
reaction
1.5 1.84 1.06 2.10 1.65 2.64
Volitional
Movement
2 2.51 2.33 3.31 2.73 3.99
Table No.5 : Mean Mental and Motor scores of BSID-II at 12 months
BSID scores Mean SD
Mental score
Raw score 85.5 18.95
Mental Developmental Index 102.8 16.76
Developmental Age 10.11 2.45
Motor Score
Raw score 60.95 9.77
Psychomotor Developmental Index 90.8 21.48
Developmental Age 9.53 2.34
Annexure I Tables
101
Table No. 6: Predictive validity of 4 month MAI for neuromotor outcome at 12 months
4 Month MAI
12- months motor outcome
Total
PDI84 PDI >85
TRS 10 14 11 25
TRS<10 03 32 35
Total 17 43 60
Sensitivity-82.3%, Specificity-74.4%.PPV-56%.NPV-91.4%
Table No. 7: Predictive validity of 6- month MAI for neuromotor outcome at 12 months
6 Month MAI
12- months motor outcome
Total
PDI84 PDI >85
6 12 08 20
<6 05 35 40
Total 17 43 60
Sensitivity-70.6%, Specificity-81.4%.PPV-60%.NPV-87.5%
Table No. 8 - Predictive validity of 8- month MAI for neuromotor outcome at 12 months
8 Month MAI
12- months motor outcome
Total
PDI84 PDI >85
TRS10 14 02 16
TRS<10 03 41 44
Total 17 43 60
Sensitivity- 82.3%, Specificity- 95.3%.PPV- 87.5%.NPV-93.2%
Annexure I Tables
102
Table No. 9 : Comparison of predictive validity of 4, 6 and 8 months MAI for
neuromotor outcome at 12 months
MAI Sensitivity Specificity
Positive
Predictive
value
Negative
Predictive
value
4-month 82.3% 74.4% 56% 91.4%
6-month 70.6% 81.4% 70% 87.5%
8-month 82.3% 95.3% 87.5%. 93.2%
Table No. 10 : Correlation between the 4-month MAI and BSID-II at 12 months
4 month MAI 12 month MDI P value 12 month PDI P value
Total Risk Score -0.501 .000* -0.710 .000*
Muscle Tone -0.358 .005* -0.567 .000*
Primitive Reflex -0.401 .002* -0.434 .001*
Automatic
reaction
-0.383 .002* -0.614 .000*
Volitional
Movement
-0.470 .000* -0.669 .000*
* Significant
Table No. 11 : Correlation between the 6-month MAI and BSID-II at 12 month
6 month MAI 12 month MDI P value 12 month PDI P value
Total Risk Score -0.683 .000* -0.639 .000*
Muscle Tone -0.596 .000* -0.510 .000*
Primitive Reflex -0.544 .000* -0.477 .000*
Automatic
reaction
-0.614 .000* -0.641 .000*
Volitional
Movement
-0.684 .000* -0.644 .000*
* Significant
Annexure I Tables
103
Table No. 12 : Correlation between the 8-month MAI and BSID-II at 12 month
8 month MAI 12 month MDI P value 12 month PDI P value
Total Risk Score -0.735 .000* -0.724 .000*
Muscle Tone -0.632 .000* -0.709 .000*
Primitive Reflex -0.606 .000* -0.500 .000*
Automatic reaction -0.663 .000* -0.638 .000*
Volitional Movement -0.742 .000* -0.725 .000*
* Significant
Table No. 13 : Neurodevelopmental problems in VLBW at one year based on BSID-II score
BSID-II
score
Only
motor
problem
Only
mental
problem
Both
motor &
mental
Total
neuromotor
problem
Percentage of
Neurodevelopmental
problem
Mild delay
(70-84)
03 0 04 07 11.66%
Significant
delay (<69)
07 0 03 10 16.66%
Total 10 0 07 17 28.33%
Table No. 14 : Four months MAI scores of infants with normal and abnormal
neuromotor outcome
4-month
MAI
MAI score for
PDI>85
MAI score for
PDI <84
p value
Total Risk Score 7.4 5.17 16.4 7.33 0.000*
Muscle Tone 4.2 2.64 6.7 1.88 0.001*
Primitive Reflex 1.2 1.53 2.2 2.04 0.001*
Automatic reaction 0.9 1.25 3.1 2.14 0.039*
Volitional Movement 1.0 1.41 4.4 3.08 0.000*
* Significant
Annexure I Tables
104
Table No. 15 : Six-months MAI scores of infants with normal and abnormal
neuromotor outcome
6-month
MAI
MAI score for
PDI>85
MAI score for
PDI < 84
p value
Total Risk Score 3.1 3.64 13.5 1.29 0.000*
Muscle Tone 0.9 1.40 2.4 2.52 0.004*
Primitive Reflex 0.8 1.11 2.5 2.67 0.001*
Automatic reaction 0.3 0.76 3.1 2.98 0.000*
Volitional Movement 1.1 1.50 5.5 4.41 0.000*
* Significant
Table No. 16 : Eight-months MAI scores of infants with normal and abnormal
neuromotor outcome
8-month
MAI
MAI score for
PDI>85
MAI score for
PDI < 84
p value
TRS 4.2 5.50 17.8 12.94 0.000*
MT 1.8 1.90 5.3 2.51 0.000*
PR 0.5 1.22 2 2.29 0.002*
AR 0.8 1.71 3.9 3.27 0.000*
VM 1.2 1.61 6.7 5.34 0.000*
* Significant
Table No. 17 : Mean Bayley Mental Scale scores of infants with normal and abnormal
Cognitive outcome at 12 months
Bayley Mental
Scale
MDI >85 MDI 84 t df p
Raw score 90.6 3.61 46.737.82 8.661 58 0.000*
MDI 107.9 8.30 64 13.30 12.202 58 0.000*
DA 10.7 1.11 5 3.74 8.995 58 0.000*
Annexure I Tables
105
Table No. 18 : Mean Bayley Motor Scale scores of infants with normal and abnormal
motor outcome at 12 months
Bayley
Motor scale
PDI>85 PDI 84 t df p
Raw score 65.1 3.49 50.312.39 7.211 58 0.000*
PDI 101.513.98 63.6 9.54 10.265 58 0.000*
DA 10.6 1.43 6.8 2.01 8.186 58 0.000*
* Significant
Table No. 19 : Association of MAI and BSID-II scores with maternal characteristics
Maternal
variables
TRS 4M
p value
TRS 6M
p value
TRS 8M
p value
PDI at 12 m MDI at 12m
Age 0.53 0.64 0.60 0.59 0.25
GA 0.82 0.96 0.67 0.29 0.94
Literacy 0.01* 0.03* 0.002* 0.003* 0.06
SES 0.22 0.88 0.78 0.85 0.19
* Significant based on chi square test
Table No. 20 : Correlation between the number of days in NICU with MAI and BSID-
II scores
MAI and BSID scores
Number of days in NICU
Pearsons correlation(r) p value
TRS at 4 month 0.254 0.054 *
TRS at 6 month 0.299 0.020*
TRS at 8 month 0.393 0.002*
MDI at 12 months - 0.398 0.002*
PDI at 12 months - 0.270 0.037*
* Significant
Annexure I Tables
106
Table No. 21 : Correlation between the number of neonatal problems with MAI and
BSID-II scores
MAI and BSID scores Number of neonatal problems
Pearsons correlation (r ) p value
TRS at 4 month 0.169 0.256
TRS at 6 month 0.116 0.436
TRS at 8 month 0.226 0.127
MDI at 12 months -0.189 0.203
PDI at 12 months - 0.427 0.003*
* Significant
Annexure II : Graphs
107
Graph 2 : Sex Distribution
55%
45%
Male Female
Graph 1 : Maternal Characteristics
15
43.33
30
11.66
10
33.33
26.66
21.66
8.33
40
31.66
28.33
0 0
0
5
10
15
20
25
30
35
40
45
50
2
0
2
1
-
2
5
2
6
-
3
0
>
3
1
P
r
i
m
a
r
y
e
d
u
c
a
t
i
o
n
S
e
c
o
n
d
a
r
y
e
d
u
c
a
t
i
o
n
H
i
g
h
e
r
s
e
c
o
n
d
a
r
y
G
r
a
d
u
a
t
i
o
n
P
o
s
t
g
r
a
d
u
a
t
i
o
n
C
l
a
s
s
I
C
l
a
s
s
I
I
C
l
a
s
s
I
I
I
C
l
a
s
s
I
V
C
l
a
s
s
V
Age Educational status Socioeconomic Status
P
e
r
c
e
n
t
a
g
e
Annexure II : Graphs
108
Graph 3 : Distribution of infants based on Gestational Age
88%
12%
Preterm Term
0
1
2
3
4
5
6
7
8
9
10
M
e
a
n
T
o
t
a
l
R
i
s
k
S
c
o
r
e
M
u
s
c
l
e
T
o
n
e
P
r
i
m
i
t
i
v
e
R
e
f
l
e
x
A
u
t
o
m
a
t
i
c
r
e
a
c
t
i
o
n
V
o
l
i
t
i
o
n
a
l
M
o
v
e
m
e
n
t
Graph 4 : Mean Distribution of TRS and categarical scores of MAI
4 Months 6 Months 8 Months
Annexure II : Graphs
109
0
20
40
60
80
100
120
M
e
a
n
Raw Score Index Score Developmental Age
Graph 5 : Mean Mental and Motor scores of BSID-II at 12 months
Mental score Motor Score
0
10
20
30
40
50
60
70
80
90
100
%
S
c
o
r
e
Sensitivity Specificity PPV NPV
Graph 6 : Comparison of predictive validity of 4, 6 and 8 months MAI
for neuromotor outcome at 12 months
4-month 6-month 8-month
Annexure II : Graphs
110
0
1
2
3
4
5
6
7
8
9
10
N
o
.
o
f
P
a
t
i
e
n
t
s
Mild delay (70-84) Significant delay (<69)
Graph 7 : Neurodevelopmental Outcome at 1 year based on BSID - II
Scores
0
2
4
6
8
10
12
14
16
18
T
R
S
M
T
P
R
A
R
V
M
T
R
S
M
T
P
R
A
R
V
M
T
R
S
M
T
P
R
A
R
V
M
4 6 8
Graph 8 : Mean MAI scores at 4, 6 & 8 months for infants with
normal and abnormal neuromotor outcome
Normal Abnormal
Annexure II : Graphs
111
0
20
40
60
80
100
120
M
e
a
n
Raw score MDI Developmental Age
Graph 9 : Mean Bayley Mental Scale scores of infants with normal and
abnormal outcome at 12 months
Normal outcome >85 Abnormal outcome </= 84
0
20
40
60
80
100
120
M
e
a
n
Raw score MDI DA
Graph 10 : Mean Bayley Motor Scale scores of infants with normal and
abnormal outcome at 12 months
Normal outcome >85 Abnormal outcome </= 84
Annexure - III : Photographs
112
Photograph 2 : BSID-II test material
Photograph 1 : MAI test material
Annexure - III : Photographs
113
Photograph 3 : Plantar Grasp
Photograph 4 : Extensibility of adductor muscles
Photograph 5 : Placing of Hands
Annexure - III : Photographs
114
Photograph 6 : Head Righting Lateral
Photograph 7 : Landau reaction
Photograph 8 : Reach out for object in supine and head centering
Annexure - III : Photographs
115
Photograph 9 : Rolling from supine to side lying
Photograph 10 : Prone weight bearing on palms
Photograph 11 : Head Righting flexion
Annexure - III : Photographs
116
Photograph 12 : Sits when placed and back straight in sitting
Photograph 13 : Equilibrium reactions in sitting
Photograph 14 : Walking with one hand support
Annexure - III : Photographs
117
Photograph 15 : Picks up cube
Photograph 16 : Finds toy under the cups
Photograph 17 : Places cube in cup
Annexure - III : Photographs
118
Photograph 19 : Places circle in the board
Photograph 20 : Turns pages of book
Photograph 18 : Retrieves toy
Annexure IV : Ethical Cl erance
119
Annexure IV : Consent Form
120
INFORMED CONSENT FORM
PREDICTING NEUROLOGICAL OUTCOME IN VERY LOW BIRTH WEIGHT
INFANTS USING MOVEMENT ASSESSMENT OF INFANTS A LONGITUDINAL
STUDY.
Investigators: Dr.Deepa.Metgud, Dr. V.D.Patil
Introduction:
You are being invited to participate in this study to find the neurological outcome in
very low birth weight infants using Movement Assessment of Infants A Longitudinal
Study. The study will be carried out in Neonatal Intensive Care Unit of KLES Dr Prabhakar
Kore Hospital, Belgaum.
Explanation of Procedure:
In this study your baby will be subjected to standard neurological evaluation and
evaluation using the test instrument MAI, which contains items on muscle tone, primitive
reflexes, automatic reactions, and volitional movements. The babys height, weight and head
circumference will be recorded. You are required to provide information regarding antenatal
care, labour and delivery, education, income and family background. You are also required
to provide information about the baby. The entire procedure may take 30 to 45 minutes.
Four follow up visits will be carried out to collect the information.
Possible Benefits:
Investigators do not promise or guarantee that you or your baby will receive any
direct benefits for being in the study. There are no known physical risks involved to the
Annexure IV : Consent Form
121
participants in this study. The procedures will be done with care, taking aseptic precaution
using standard equipments.
Confidentiality:
Your identity will be kept confidential, so that no one else will know your identity.
Publication Rights:
The results of the study will be used for teaching and medical publications; however
the participants identity will be kept confidential.
Withdrawal:
Participation in this study is voluntary. If you dont wish to participate in this study,
you will not loose benefits to which your child is entitled. You are free to withdraw your
consent and to discontinue participation from this study at any time.
Cost of Participation:
The cost will be borne by the researcher. There will be no additional cost to you for
participating in this study.
Payment for participation:
There will be no payment to you for participating in this study. As a result of your
participation, if your baby experiences injury from know or unknown risk of the research
procedures as described, immediate care and treatment, including hospitalization if
necessary will be available within the facilities available in the free section of the hospital.
However there will be no monetary compensation in the event of injury resulting from the
research.
Annexure IV : Consent Form
122
Questions:
If you have any questions about this study, questions about the research related
injury, or experience any problems during the study, you should contact Dr Deepa Metgud
(9845861236) or Dr V. D. Patil (9448190231).
Consent Statement
I am making a voluntary decision for my baby to participate in this study. My
signature below indicates that I have decided to participate, and I have read (or been read)
the information provided above, and I was given the opportunity to ask questions and that
they have been answered to my satisfaction, and that I have received a copy of this signed
consent form.
_______________________ __________
Signature of the Participant
(Left Hand Thumb Impression) Date
__________________________ ____________
Signature of principal Investigator Date
__________________ ______________
Signature of Witness Date
Annexure IV : Proforma
123
PROFORMA
Sl. No: I.P. No / OPD No:
Maternal Data:
Name:
Mothers Age:
Education:
Primary
Secondary
Higher Secondary
Graduation
Post graduation
Socioeconomic Status based on family income :
Class I
Class II
Class III
Class IV
Class V
Annexure IV : Proforma
124
Gestational age: __________Weeks
Address:
Phone:
Neonatal Data:
Date of Birth:
Inborn/Out born :
DOA to NICU:
DOD from NICU:
Number of days in NICU:
Sex: Male Female
Birth Weight: grams
Preterm
Term
Neonatal Problems:
No. of neonatal problems
< 3 3 to 6 > 6
KEY TO MASTER CHART
Maternal Education
Primary---------------1
Secondary------------2
Higher Secondary---3
Graduates------------4
Post graduates-------5
Socio-economic status
Class I----------------1
Class II---------------2
Class III--------------3
Class IV -------------4
Class V --------------5
Neonatal Problems
Present---------------1
Absent ---------------2
Inborn----------------1
Out born--------------2
Sex
Male -----------------1
Female---------------2
Interpretation - PDI and MDI
Accelerated performance--------------1
Within normal limits-------------------2
Mild delayed performance------------3
Significantly delayed performance--4
Neonatal data
Sl.
No
Age
(Yrs)
Edu
Eco
status
GA
(Wks)
Sex
I/O
Born
Days
NICU
B.Wt
(Gms)
Preterm
/ Term
IUGR Anemia Hyperbilir RDS HMD Hypoglyce Apnoea NEC Hypotens IVH
Birth
asphy
Ventilator
Convulsi
on
Sepsis
No of
Problems
1 33 4 1 32 1 1 10 1160 1 2 2 2 2 2 2 2 2 2 2 2 2 2 1 2
2 24 5 1 33 1 1 13 1450 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
3 18 1 3 30 1 2 32 1300 1 2 2 2 2 2 2 2 2 1 1 2 2 2 1 3
4 28 4 1 31 2 1 30 1160 1 2 1 1 1 2 2 2 2 1 2 2 2 2 1 3
5 26 2 1 28 1 1 60 1160 1 2 2 1 2 2 2 1 2 1 2 2 2 2 1 3
6 21 3 1 34 2 1 11 1460 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
7 23 4 2 35 1 1 7 1500 2 1 2 1 2 2 2 2 2 2 2 2 2 2 2 1
8 19 2 3 32 1 1 17 1450 1 2 2 2 2 2 2 2 2 1 2 2 2 2 1 1
9 35 4 1 32 2 1 35 1270 1 2 2 1 2 2 2 2 2 1 2 1 2 2 1 2
10 30 3 2 32 1 1 30 1360 1 2 1 1 2 2 2 1 1 1 2 1 2 2 1 3
11 20 2 2 32 1 1 17 1500 1 2 2 1 2 2 2 1 2 1 2 2 2 2 2 3
12 30 4 1 31 1 1 40 1500 1 2 2 1 2 2 2 2 2 1 2 2 2 2 2 1
13 30 4 1 31 1 1 40 1150 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
14 25 2 2 31 1 1 15 1340 1 2 2 1 2 2 2 1 2 1 2 2 2 2 1 3
15 25 2 2 31 1 1 15 1500 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
16 25 2 2 31 1 1 15 1420 1 2 2 1 2 2 2 2 2 1 2 2 2 2 2 1
17 22 3 2 32 2 1 25 1500 1 2 2 2 2 2 2 2 2 2 2 2 2 2 1 2
18 33 5 3 30 2 1 37 1200 1 2 2 1 2 1 2 2 2 1 2 2 1 2 1 3
19 32 4 3 32 1 1 25 1130 1 2 1 1 2 2 1 2 1 2 2 2 2 2 1 3
20 19 3 3 34 1 2 17 1250 1 2 2 1 2 2 2 2 2 2 2 1 2 2 2 1
21 29 4 3 32 2 1 15 1200 1 2 1 1 2 2 2 1 2 2 2 2 2 2 1 3
22 27 3 2 32 1 1 18 1480 1 2 2 1 2 2 2 2 2 1 2 2 2 2 2 2
23 20 1 3 32 1 1 11 1450 1 2 2 1 2 2 2 2 2 2 2 1 2 2 1 3
24 26 3 1 31 1 1 27 1300 1 2 2 1 1 2 2 2 2 2 2 2 2 2 1 2
25 20 2 3 37 2 1 14 1500 2 1 2 1 2 2 2 2 2 2 2 2 2 2 2 1
26 28 3 1 35 1 1 43 1500 2 2 1 1 2 2 1 2 2 2 2 2 1 1 2 3
27 26 2 1 32 1 2 27 1500 1 2 2 2 2 2 2 1 2 1 2 2 1 1 1 2
28 24 4 3 35 2 1 8 1500 1 2 2 2 2 2 2 2 2 1 2 2 2 2 1 1
29 20 2 2 32 1 1 6 1500 1 2 2 1 2 2 2 2 2 2 2 1 2 2 2 1
30 25 1 2 40 2 2 15 1500 2 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2
31 25 1 3 35 2 1 31 1400 1 2 1 2 2 2 2 2 2 2 2 2 2 2 1 2
32 27 2 3 31 2 1 26 1100 1 2 2 1 2 2 2 1 2 2 2 2 2 2 1 3
33 27 4 1 29 1 1 21 1250 1 2 1 1 1 2 2 2 2 1 2 2 2 2 1 3
34 25 2 2 33 2 1 10 1000 1 2 2 1 2 2 2 2 2 2 2 2 2 2 1 3
35 24 3 2 34 2 1 5 1500 1 2 2 2 2 2 2 2 2 2 2 2 2 2 2 1
36 26 5 1 33 1 1 32 1500 1 2 1 1 2 2 2 2 2 1 2 2 2 2 2 3
37 37 2 3 33 2 1 27 1500 1 2 1 1 2 2 2 1 1 2 2 2 2 2 1 3
38 35 2 2 30 2 1 8 1200 1 2 2 1 2 2 2 2 2 2 2 2 2 2 1 2
39 22 3 1 32 2 1 13 1400 1 2 2 1 2 2 1 2 2 1 2 2 2 2 1 3
40 23 4 1 31 1 1 20 1500 1 2 2 1 1 2 2 1 2 1 2 2 1 2 1 3
41 21 3 2 34 1 1 16 1400 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
42 22 2 2 35 2 2 16 1500 1 2 2 1 2 2 2 2 2 1 2 2 2 2 2 3
43 21 3 1 33 1 1 41 1200 1 2 2 1 1 2 2 1 2 1 2 2 1 2 1 3
44 25 2 1 38 2 1 17 1500 2 1 2 1 2 2 2 2 2 1 2 2 2 2 1 2
45 21 2 2 40 2 1 10 1500 2 1 2 2 2 2 1 2 2 2 2 2 2 2 1 1
46 20 2 3 31 2 1 40 1300 1 2 2 1 2 1 1 2 2 1 2 2 2 2 2 3
47 27 5 1 33 1 1 51 1450 1 2 2 2 1 2 2 2 2 1 2 2 1 2 1 3
48 22 1 3 36 2 1 12 1500 2 1 2 1 2 2 2 2 2 2 2 2 2 2 2 1
49 23 3 3 32 1 1 15 1450 1 2 2 1 2 2 2 2 2 2 2 1 2 2 1 2
50 24 3 1 33 2 1 12 1350 1 2 2 2 2 2 2 2 2 2 2 1 2 2 2 1
51 28 3 2 32 1 1 15 1400 1 2 2 1 2 2 2 2 2 1 2 2 2 1 1 3
52 38 5 1 32 1 1 24 1220 1 2 2 1 2 2 1 2 2 1 2 2 2 2 2 2
53 23 4 1 34 2 1 5 1300 1 2 2 1 2 2 2 1 2 2 2 2 2 2 1 2
54 23 4 1 34 2 1 5 1500 1 2 2 1 2 2 2 2 2 2 2 2 2 2 1 2
55 22 3 1 32 2 1 15 1300 1 2 2 1 1 2 2 2 2 2 2 2 2 2 1 2
56 30 2 1 39 1 1 11 1250 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
57 30 2 3 39 1 1 11 1250 1 2 2 1 2 2 2 2 2 2 2 2 2 2 2 1
58 20 1 2 35 1 1 12 1500 2 1 1 2 2 2 1 2 2 1 2 1 2 1 2 3
59 22 2 3 32 2 1 8 1320 1 2 2 1 2 2 2 2 2 1 2 2 2 2 2 1
60 21 3 2 32 2 1 20 1200 1 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2
Neonatal problems Maternal data
Sl.
No
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
TRS MT PR AR VM TRS MT PR AR VM TRS MT PR AR VM RS MDI DA Interpretation RS PDI DA Interpretation
8 7 0 0 1 7 1 1 0 5 3 0 0 0 3 92 111 11 2 68 113 12 2
7 4 2 0 1 2 0 1 0 1 1 1 0 0 0 90 107 13 2 64 97 10 2
10 7 1 0 2 8 1 2 0 5 15 7 0 3 6 78 77 8 3 56 65 7 4
8 5 1 2 0 0 0 0 0 0 4 1 0 0 3 84 90 9 2 61 85 9 2
18 8 1 4 5 41 9 8 9 15 41 9 8 9 15 8 50 1 4 23 50 3 4
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 96 120 12 1 69 117 12 1
5 3 2 0 0 2 1 0 0 1 0 0 0 0 0 90 107 13 2 68 113 12 2
7 5 1 1 0 0 0 0 0 0 4 2 1 0 1 86 96 9 2 62 89 9 2
17 7 5 1 4 2 2 0 0 0 3 1 0 1 0 94 115 11 1 65 101 12 2
19 8 5 4 2 12 3 4 3 2 21 4 6 7 4 85 93 9 2 61 85 9 2
4 3 1 0 0 1 0 0 0 1 1 1 0 0 0 91 109 11 2 69 117 12 1
2 2 0 0 0 1 0 0 0 1 2 2 0 0 0 95 117 11 1 70 121 12 1
2 1 0 0 1 0 0 0 0 0 0 0 0 0 0 94 115 11 1 71 125 13 1
9 8 1 0 0 8 5 2 0 1 3 3 0 0 0 89 105 10 2 63 93 10 2
3 3 0 0 0 2 0 2 0 0 1 1 0 0 0 91 109 11 2 70 121 12 1
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 93 113 12 2 69 117 12 1
9 3 2 2 2 1 1 0 0 0 1 0 0 0 1 92 111 11 2 59 77 9 3
13 5 2 3 3 3 0 0 0 3 2 2 0 0 0 94 115 11 1 67 109 12 2
20 9 5 2 4 9 4 2 2 1 23 6 4 6 7 92 111 11 2 64 97 10 2
25 9 3 6 9 17 2 4 5 6 20 7 2 3 8 89 105 10 2 54 57 7 4
16 7 5 1 3 9 3 4 0 2 4 1 0 0 3 92 111 11 2 62 89 9 2
2 2 0 0 0 0 0 0 0 0 0 0 0 0 0 95 117 11 1 70 121 12 1
22 8 3 5 6 15 1 2 4 8 18 6 3 4 5 86 96 9 2 55 61 7 4
5 3 0 1 1 0 0 0 0 0 3 2 0 1 0 89 105 10 2 69 117 12 1
10 8 0 1 1 2 0 1 0 1 2 0 1 0 1 90 107 13 2 66 105 11 2
8 5 1 2 0 3 1 0 2 0 6 2 2 1 1 78 77 8 3 58 73 9 3
32 8 6 6 12 31 8 5 5 13 41 10 3 9 19 3 50 1 4 33 50 4 4
8 5 1 0 2 6 1 1 1 3 6 3 2 1 0 95 117 11 1 68 113 12 2
6 3 2 0 1 2 0 0 0 2 0 0 0 0 0 95 117 11 1 62 89 9 2
18 8 1 4 5 14 2 2 3 7 20 4 3 5 8 75 70 8 3 40 50 5 4
17 8 2 2 5 5 0 0 2 3 13 4 2 2 5 90 107 11 1 57 69 7 4
13 8 0 1 4 3 1 1 0 1 20 7 3 5 5 91 109 11 2 54 57 7 4
10 7 3 0 0 4 4 0 0 0 7 5 0 1 1 87 99 12 2 63 93 10 2
5 5 0 0 0 2 1 1 0 0 1 1 0 0 0 94 115 11 1 67 109 12 2
4 3 0 0 1 1 0 1 0 0 1 1 0 0 0 94 115 11 1 62 89 9 2
6 1 1 3 1 0 0 0 0 0 5 0 0 4 1 96 120 12 1 64 97 10 2
3 0 1 1 1 0 0 0 0 0 8 5 0 1 2 84 90 9 2 61 85 9 2
2 0 0 0 2 0 0 0 0 0 5 3 0 0 2 92 111 11 2 62 89 9 2
6 5 0 1 0 1 0 0 0 1 5 3 0 0 2 89 105 10 2 62 89 9 2
5 4 0 1 0 0 0 0 0 0 2 1 0 1 0 95 117 11 1 70 121 12 1
16 7 2 5 2 15 3 2 3 7 21 8 3 5 5 83 88 9 2 63 93 10 2
17 8 0 4 5 6 1 0 3 2 10 6 0 1 3 92 111 11 2 57 69 7 4
20 7 2 6 5 20 3 5 4 8 22 5 2 5 10 83 111 9 2 57 69 7 4
9 7 0 1 1 4 1 3 0 0 7 3 2 0 2 95 117 11 1 70 121 12 1
3 0 1 1 1 1 0 1 0 0 1 0 0 0 1 91 109 11 2 68 113 12 2
7 5 0 2 0 2 2 0 0 0 8 1 0 4 3 93 113 12 2 61 85 9 2
12 7 2 1 2 8 2 1 0 5 10 4 0 2 3 77 74 8 3 58 73 9 3
10 5 3 1 1 2 0 1 0 1 3 2 0 0 1 86 96 9 2 61 85 9 2
18 8 0 4 6 11 4 1 2 4 9 4 1 1 3 91 109 11 2 61 85 9 2
10 4 2 2 2 6 2 0 0 4 10 5 0 1 4 86 96 9 2 58 73 9 3
8 7 0 0 1 0 0 0 0 0 1 1 0 0 0 90 107 13 2 61 85 9 2
22 6 7 2 7 28 4 7 8 9 38 6 6 11 15 8 50 1 4 23 50 3 4
4 3 1 0 0 4 0 3 0 1 0 0 0 0 0 92 111 11 2 68 113 12 2
2 1 1 0 0 4 1 2 0 1 1 1 0 0 0 94 115 11 1 67 109 12 2
11 5 1 1 4 4 0 1 1 2 9 5 1 0 3 88 102 12 2 62 89 9 2
9 7 2 0 0 4 1 1 0 2 2 1 0 0 1 91 109 11 2 61 85 9 2
7 3 3 1 0 4 1 1 0 2 2 1 0 0 1 91 109 11 2 61 85 9 2
23 8 5 6 4 23 3 5 7 8 17 6 0 5 6 89 105 10 2 56 65 7 4
2 2 0 0 0 1 0 0 0 1 0 0 0 0 0 94 115 11 1 68 113 12 2
3 3 0 0 0 0 0 0 0 0 4 2 0 0 2 84 90 9 2 58 73 9 3
MAI at 4-month MAI at 6-month MAI at 8M Bayleys at 12M
Mental Motor
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- SMOOSAJEEDocumento319 pagineSMOOSAJEEMutiara SazkiaNessuna valutazione finora
- Care of The Newborn in Developing Countries Book 2 Chapter 7 The Normal NewbornDocumento10 pagineCare of The Newborn in Developing Countries Book 2 Chapter 7 The Normal NewbornMutiara SazkiaNessuna valutazione finora
- Programme BookDocumento151 pagineProgramme BookMutiara SazkiaNessuna valutazione finora
- Ophthalmology Emergencies HandoutDocumento9 pagineOphthalmology Emergencies HandoutMutiara SazkiaNessuna valutazione finora
- File1 146 1714383Documento366 pagineFile1 146 1714383Mutiara SazkiaNessuna valutazione finora
- Ch15-Central Vision PathwaysDocumento10 pagineCh15-Central Vision PathwaysMutiara SazkiaNessuna valutazione finora
- MK Giz Slide Pediatric Nutrition Care As A Strategy To Prevent Hospital MalnutritionDocumento44 pagineMK Giz Slide Pediatric Nutrition Care As A Strategy To Prevent Hospital MalnutritionMutiara SazkiaNessuna valutazione finora
- Myopia in Singapore: Taking A Public Health ApproachDocumento6 pagineMyopia in Singapore: Taking A Public Health ApproachMutiara SazkiaNessuna valutazione finora
- The Disaster Cycle LeDuc 01-20-06Documento6 pagineThe Disaster Cycle LeDuc 01-20-06Mutiara SazkiaNessuna valutazione finora
- General Anesthesia 1 PDFDocumento49 pagineGeneral Anesthesia 1 PDFYokita JanarthananNessuna valutazione finora
- Basic Anesthetic Monitoring 2011Documento3 pagineBasic Anesthetic Monitoring 2011egomezgrasNessuna valutazione finora
- Flood Information BrochureDocumento2 pagineFlood Information BrochureMutiara SazkiaNessuna valutazione finora
- Time and Expense Management Applications 133333Documento3 pagineTime and Expense Management Applications 133333Mutiara SazkiaNessuna valutazione finora
- ES GuideDocumento37 pagineES GuideRaghavendra Pundaleek ChittaNessuna valutazione finora
- Sunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJDocumento37 pagineSunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJMutiara SazkiaNessuna valutazione finora
- Sunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJDocumento37 pagineSunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJMutiara SazkiaNessuna valutazione finora
- Public Health Consequences of Earthquakes: Eric K. NojiDocumento32 paginePublic Health Consequences of Earthquakes: Eric K. NojiMutiara SazkiaNessuna valutazione finora
- 292Documento6 pagine292Mutiara SazkiaNessuna valutazione finora
- DafpusDocumento2 pagineDafpusMutiara SazkiaNessuna valutazione finora
- Emerging Trends in Disaster ImpactDocumento4 pagineEmerging Trends in Disaster ImpactMutiara SazkiaNessuna valutazione finora
- Final Exh. 10 TBIDocumento95 pagineFinal Exh. 10 TBIMutiara SazkiaNessuna valutazione finora
- A4 Boys 0-4YRS (4th Jan 2013)Documento2 pagineA4 Boys 0-4YRS (4th Jan 2013)Mutiara SazkiaNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- SanMilan Inigo Cycling Physiology and Physiological TestingDocumento67 pagineSanMilan Inigo Cycling Physiology and Physiological Testingjesus.clemente.90Nessuna valutazione finora
- Employee Final SettlementDocumento1 paginaEmployee Final SettlementZeeshan Mirza0% (1)
- Psychoanalysis AND History: Freud: Dreaming, Creativity and TherapyDocumento2 paginePsychoanalysis AND History: Freud: Dreaming, Creativity and TherapyJuan David Millán MendozaNessuna valutazione finora
- FEM 3004 - Lab 10 Part 2editedDocumento26 pagineFEM 3004 - Lab 10 Part 2editedAINA NADHIRAH BINTI A ROZEY / UPMNessuna valutazione finora
- Eric Koech CV - Docx..bakDocumento7 pagineEric Koech CV - Docx..bakPeter Osundwa KitekiNessuna valutazione finora
- The Effects of Violent Video Games Research Paper English Comp2Documento11 pagineThe Effects of Violent Video Games Research Paper English Comp2api-451442670Nessuna valutazione finora
- Current Concepts of Enzyme Histochemistry in Modern PathologyDocumento11 pagineCurrent Concepts of Enzyme Histochemistry in Modern PathologyRosa AquinoNessuna valutazione finora
- Birding The Gulf Stream: Inside This IssueDocumento5 pagineBirding The Gulf Stream: Inside This IssueChoctawhatchee Audubon SocietyNessuna valutazione finora
- Reaction Paper-RprDocumento6 pagineReaction Paper-Rprapi-543457981Nessuna valutazione finora
- Carboset CA-600 - CST600 - CO - enDocumento3 pagineCarboset CA-600 - CST600 - CO - enNilsNessuna valutazione finora
- Science 9 Q4 SML17 V2Documento15 pagineScience 9 Q4 SML17 V2HotdogNessuna valutazione finora
- Sanctuary Policy PomonaDocumento3 pagineSanctuary Policy PomonaGabriel EliasNessuna valutazione finora
- J130KDocumento6 pagineJ130KBelkisa ŠaćiriNessuna valutazione finora
- Unit-3.1.2-Sleeve and Cotter JointDocumento18 pagineUnit-3.1.2-Sleeve and Cotter JointAsvath Guru100% (2)
- High Speed DoorsDocumento64 pagineHigh Speed DoorsVadimMedooffNessuna valutazione finora
- Art of Facing InterviewsDocumento15 pagineArt of Facing Interviewskrish_cvr2937100% (2)
- 41 Assignment Worksheets For SchoolDocumento26 pagine41 Assignment Worksheets For Schoolsoinarana456Nessuna valutazione finora
- Characteristics of Testable HypothesesDocumento30 pagineCharacteristics of Testable HypothesesMarivic Diano67% (3)
- Organogram - Qa / QC: Srinivasan SrinivasanDocumento4 pagineOrganogram - Qa / QC: Srinivasan SrinivasanGowtham VenkatNessuna valutazione finora
- Adsorbents and Adsorption Processes For Pollution ControlDocumento30 pagineAdsorbents and Adsorption Processes For Pollution ControlJoao MinhoNessuna valutazione finora
- Cadorna, Chesca L. - NCPDocumento2 pagineCadorna, Chesca L. - NCPCadorna Chesca LoboNessuna valutazione finora
- Report in Per Dev CorrectedDocumento34 pagineReport in Per Dev CorrectedJosh lyan RiveraNessuna valutazione finora
- Demages Goods RecordDocumento22 pagineDemages Goods Recordtariq malikNessuna valutazione finora
- Entitlement Cure SampleDocumento34 pagineEntitlement Cure SampleZondervan100% (1)
- Bio411 C1Documento1 paginaBio411 C1Aqiena BalqisNessuna valutazione finora
- VPD RashchrtDocumento2 pagineVPD RashchrtMarco Ramos JacobNessuna valutazione finora
- Penilaian Akhir TahunDocumento4 paginePenilaian Akhir TahunRestu Suci UtamiNessuna valutazione finora
- A Critical Appreciation of Ode To NightingaleDocumento3 pagineA Critical Appreciation of Ode To NightingaleBaloch Karawan100% (2)
- Care of Clients With Problems in OxygenationDocumento5 pagineCare of Clients With Problems in OxygenationSkyla FiestaNessuna valutazione finora
- Those With MoonDocumento1 paginaThose With MoonRosee AldamaNessuna valutazione finora