Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Infant Iron Status Affects Iron Absorption in Peruvian Breastfed Infants at 2 and 5 Mo of Age
Caricato da
Aldo Paz MarchenaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Infant Iron Status Affects Iron Absorption in Peruvian Breastfed Infants at 2 and 5 Mo of Age
Caricato da
Aldo Paz MarchenaCopyright:
Formati disponibili
Infant iron status affects iron absorption in Peruvian breastfed infants at
2 and 5 mo of age
13
Julia L Finkelstein, Kimberly O OBrien, Steven A Abrams, and Nelly Zavaleta
ABSTRACT
Background: Effects of prenatal iron supplementation on maternal
postpartum iron status and early infant iron homeostasis remain
largely unknown.
Objective: We examined iron absorption and growth in exclusively
breastfed infants in relation to fetal iron exposure and iron status
during early infancy.
Design: Longitudinal, paired iron-absorption (
58
Fe) studies were
conducted in 59 exclusively breastfed Peruvian infants at 23 mo
of age (2M) and 56 mo of age (5M). Infants were born to women
who received $5100 or #1320 mg supplemental prenatal Fe. Iron
status was assessed in mothers and infants at 2M and 5M.
Results: Infant iron absorption from breast milk averaged 7.1%
and 13.9% at 2M and 5M. Maternal iron status (at 2M) predicted
infant iron deciency (ID) at 5M. Although no infants were iron
decient at 2M, 28.6% of infants had depleted iron stores (ferritin
concentration ,12 mg/L) by 5M. Infant serum ferritin decreased
(P , 0.0001), serum transferrin receptor (sTfR) increased (P ,
0.0001), and serum iron decreased from 2M to 5M (P , 0.01).
Higher infant sTfR (P , 0.01) and breast-milk copper (P , 0.01)
predicted increased iron absorption at 5M. Prenatal iron supplemen-
tation had no effects on infant iron status or breast-milk nutrient
concentrations at 2M or 5M. However, fetal iron exposure predicted
increased infant length at 2M (P , 0.01) and 5M (P , 0.05).
Conclusions: Fetal iron exposure affected early infant growth but
did not signicantly improve iron status or absorption. Young, ex-
clusively breastfed infants upregulated iron absorption when iron
stores were depleted at both 2M and 5M. Am J Clin Nutr
2013;98:147584.
INTRODUCTION
An estimated 1.6 billion people worldwide are anemic (1, 2)
and iron deciency (ID)
4
is the leading cause of anemia (1, 3).
Pregnant women are at increased risk of anemia and ID because
of, in part, increased nutritional requirements of pregnancy
coupled with a lack of adequate dietary iron intake and bio-
availability to meet these increased demands (3, 4). In resource-
limited settings, it has been estimated that 50% of pregnant
women had anemia (1) compared with 1225% in developed
regions (3, 5, 6). When anemia or ID occurs during pregnancy,
risk of maternal (7) and infant mortality (8) is increased, but
little is known about how this affects early infant iron homeo-
stasis or growth.
The impact of maternal iron status and iron supplementation
during pregnancy on neonatal iron status has not been fully
characterized. Several studies have shown no signicant asso-
ciation between maternal and infant iron status (9, 10), whereas
other evidence has suggested an association between maternal
iron status in pregnancy and infant iron stores postpartum (11
14); maternal iron-deciency anemia (IDA) in pregnancy has
been associated with compromised fetal iron reserves (11, 15
17). Recent data by Roberfroid et al (18) have indicated that the
physiologic anemia of pregnancy occurs even in women re-
ceiving iron supplementation.
Several studies have shown that placental iron transfer can be
upregulated when maternal or fetal iron stores are limited (19
23). We have previously reported that a signicantly larger
fraction of maternally ingested iron is transferred to the fetus in
women with depleted iron stores (23, 24). Recent animal studies
also suggested that the timing at which iron supplementation is
initiated during pregnancy may also inuence subsequent neo-
natal outcomes (25). Although acute studies of placental iron
transport have highlighted the adaptability of maternal-fetal iron
partitioning, little is known about the long-term impact of this
transfer on early iron homeostasis. In Peru, the estimated pre-
valence of anemia in infants 68 mo old is 69.3% (26); reasons
for this high prevalence in relation to early iron absorption need
to be investigated.
To address this issue, we conducted longitudinal, paired iron-
absorption studies in exclusively breastfed Peruvian infants at 2
and 5 mo of age to 1) characterize longitudinal determinants of
iron absorption from breast milk in young infants as the iron
stores of birth are depleted and 2) examine the impact of fetal
iron exposure on early infant iron homeostasis and growth.
1
Fromthe Division of Nutritional Sciences, Cornell University, Ithaca,
NY (JLF and KOO); the USDA/Agricultural Research Service Childrens
Nutrition Research Center, Baylor College of Medicine, Houston, TX
(SAA); and the Instituto de Investigacion Nutricional, Lima, Peru (NZ).
2
Supported by a grant from the Nestle Foundation.
3
Address reprint requests and correspondence and to KO OBrien, Divi-
sion of Nutritional Sciences, Cornell University, 230 Savage Hall, Ithaca,
NY 14853. E-mail: koo4@cornell.edu.
4
Abbreviations used: ID, iron deciency; IDA, iron-deciency anemia;
SF, serum ferritin; sTfR, serum transferrin receptor; 2M, 23 mo of age;
5M, 56 mo of age; 2Fe, #1320 mg supplemental prenatal Fe; +Fe, $5100
mg supplemental prenatal Fe.
ReceivedDecember 19, 2012. Accepted for publication September 11, 2013.
First published online October 2, 2013; doi: 10.3945/ajcn.112.056945.
Am J Clin Nutr 2013;98:147584. Printed in USA. 2013 American Society for Nutrition 1475
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
SUBJECTS AND METHODS
Study population
Two groups of Peruvian women and their 23-mo-old infants
were recruited from Villa El Salvador, which is a low-income
periurban area of Lima, Peru. One group of women (n = 30) had
received supplemental iron [60 mg Fe/d for $3 mo during
pregnancy for a total of $5100 mg supplemental prenatal iron
(+Fe)], whereas the other group (n = 29) had not consumed iron
supplements or consumed ,1 mo of supplemental iron during
pregnancy [dened as #1320 mg supplemental prenatal Fe (2Fe)
across pregnancy]. Maternal supplemental iron intake and ad-
herence during pregnancy was evaluated by self-report. This
study was conducted during 1998; at that time, pregnant women
receiving care at health centers frequently did not ingest iron
supplements either by low adherence to prenatal supplementation
or because supplements were not regularly available in health
centers. Recent survey data on prenatal iron supplementation (60
mg/d) in this community reported an average intake of 6360 mg
Fe (IQR: 48607980 mg Fe) over the course of pregnancy (27).
All infants recruited were receiving care at the well baby clinic
at the Cesar Lopez Silva Hospital. Infants were eligible for
participation if they were 23 mo old, healthy, full-term sin-
gletons ($37 to ,42 wk of gestation) with a birth weight
$2500 g. Data on infant weight and length at birth were ob-
tained from medical records. Infants were exclusively breastfed
(ie, none had received any infant formula, herbal infusions, or
foods), had not received any supplemental iron, and lived in
Lima (at sea level) since birth. The study protocol was explained
in detail to mothers by the eld nurse and study doctor, and
informed written consent was obtained before study enrollment.
The study protocol was approved by the Committee on Human
Research at Johns Hopkins Bloomberg School of Public Health
and by the Institutional Review Board at the Instituto de In-
vestigacion Nutricional, Lima, Peru.
Study design
Longitudinal, paired iron-absorption (
58
Fe) studies were un-
dertaken in infants at 23 mo of age (2M) and again at 56 mo of
age (5M). All study visits were conducted at the outpatient well
baby clinic in Cesar Lopez Silva Hospital, Villa El Salvador, Lima,
Peru. On the morning of the rst iron-absorption study, the infant
was examined by the study pediatrician, weight was measured by
using a digital scale (SECA) (610 g), and recumbent length was
measured to the nearest 0.1 cm by using a wooden measuring
board. Each infant then had a 3-mL venous blood sample collected
to assess baseline iron status, including hemoglobin, serum
transferrin receptor (sTfR), serum ferritin (SF), and C-reactive
protein (evacuated tubes containing EDTA; SARSDET). Breast-
milk samples were collected from each mother into containers free
from trace minerals; samples were obtained from early, middle,
and late feed for assessment of iron, zinc, and copper concentra-
tions. A maternal 3-mL venous blood sample was obtained on the
day the infant was dosed at both 2M and 5M to evaluate the same
iron-status indicators as measured in each infant.
In the initial iron-absorption studies, women expressed breast
milk into a sterile trace mineralfree container, iron tracer (150
mg
58
Fe) was added to the expressed breast milk, and the mix-
ture was allowed to sit overnight in a cold room on a shaker. At
the clinic the next morning, infants were fed the extrinsically
labeled breast milk (the container with milk was warmed in hot
water) from a bottle ad libidum after a 2-h fast, and the quantity
of milk and tracer ingested was determined by preweighing and
postweighing the feed. However, the initial iron-absorption data
from the rst 9 infants were much lower than anticipated on the
basis of existing literature at the time the study was undertaken.
As a result, to ensure that all tracer was delivered, the study
design was modied to administer 150 mg
58
Fe (after a 2-h fast)
in a avored syrup by syringe directly into the infants mouth.
Then, mothers breastfed their infants ad libidum. Infant weight
was recorded before and after the feeding interval to assess the
total intake of breast milk. Statistical analyses were conducted
both with and without adjustment for the method of tracer ad-
ministration; there were no signicant differences in iron ab-
sorption in subjects who received tracer that had equilibrated in
breast milk overnight (n = 15; 9 +Fe and 6 2Fe), compared with
those who received tracer alone before being breastfed (n = 44;
21 +Fe and 23 2Fe). Thus, the dosing method was not adjusted
for in subsequent analyses.
Syringes were weighed before and after dosing to determine
the exact quantity of isotope administered. All mother and infant
pairs studied remained in the clinic for 1 h postdosing to ensure
that tracer was not regurgitated; no breast milk, other food, or
liquid was given for 2 h after the feed that contained the iron dose
was completed. Anthropometric, dietary, and health data were
collected. Fourteen days after dosing, mothers and infants
returned to the study hospital. A 3-mL venous blood sample was
collected to assess concentrations of stable iron isotopes and
biochemical indicators in infants. Anthropometric, dietary, and
health data were also collected. After the blood collection,
mothers and infants returned home.
Three months after the rst iron-absorption study, mother-
infant pairs returned to the study hospital, and a second iron
absorption study was conducted by using the same labeling
method as used at the rst study except that a 3-mL venous blood
sample was collected from each infant before dosing to assess
baseline
58
Fe enrichment, and the
58
Fe dose was increased to
200 mg. The baseline enrichment at 5M was used as the new
baseline value for the second absorption-study calculations.
Maternal blood samples were also collected for the same anal-
yses as those measured in the rst study. As in the rst study, the
mother and infant remained in the clinic for the following hour
postdosing to ensure that tracer was not regurgitated and the
same anthropometric, biochemical, dietary, and health data were
collected. Fourteen days after the second dosing study, mothers
and infants returned to the study hospital, and a venous blood
sample (3 mL) was obtained from each infant to assess iron
enrichment in red blood cells and concentrations of biochemical
indicators. Anthropometric data, dietary, and health data were
also collected, and mothers and infants returned home. At the
end of the second study, any mother or infant who was shown to
be anemic was treated for anemia in accordance with standard of
care guidelines for the WHO and government of Peru (3).
Biochemical indicators
Hemoglobin concentrations were assessed in whole blood
samples by using the Hemocue method. The packed cell volume
was analyzed by using the microhematocrit method. SF was
1476 FINKELSTEIN ET AL
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
measured by using an ELISA with human antiferritin and anti-
ferritin peroxidase antibodies purchased from DAKO. sTfR was
measured by using a commercially available ELISA(Quantikine;
R&D Systems). Laboratory samples were tested in batches by an
experienced biochemist at Instituto de Investigacion Nutricional,
and instruments were calibrated daily by using standardized
procedures.
Preparation of stable iron isotope
A stable iron isotope (
58
Fe at 93.13% enrichment) was pur-
chased in elemental form from Trace Sciences International.
The metal was converted into ferrous sulfate solutions (0.5 mg/
mL) according to the procedure of Kastenmayer et al (28), ex-
cept that no ascorbic acid was added during the tracer prepa-
ration to avoid its inuence on iron absorption. Isotope solutions
were checked for sterility before administration. The
58
Fe en-
richment of the nal ferrous sulfate tracer solution was de-
termined by using magnetic sector thermal ionization mass
spectrometry (Thermoquest Triton TI), and the total iron content
was measured by using atomic absorption spectrophotometry
(Perkin Elmer 3300;Perkin Elmer).
Isolation of iron from red blood cells
Approximately 1 mL whole blood was digested on a hot plate
with Ultrex nitric acid following previously published methods
(24, 29). When the digest was clear, it was evaporated to dryness,
reconstituted, and iron was extracted from this digest by using
anion-exchange chromatography as previously reported (24, 29).
After the iron was eluted from the column, the sample was dried
and reconstituted in 30 mL 0.3N ultrapure nitric acid.
Measurement of iron isotope enrichment
Extracted iron (10 mL) was loaded onto rhenium laments
and isotopic ratios (
58
Fe:
56
Fe ratios normalized for isotopic
fractionation by using the
54
Fe:
56
Fe ratio) were analyzed by
using a magnetic sector thermal ionization mass spectrometer
(Thermoquest TI). The instrumentation achieved a relative SD
of 0.16% for the
58
Fe isotope used.
Iron-absorption calculations
The amount of circulating iron in each infant was estimated
after assuming that the blood volume was 80 mL/kg by using the
following equation:
Circulating iron mg hemoglobin concentration g=L
3blood volume mL
3concentration of iron in hemoglobin
3:47 mg Fe=g hemoglobin
31 L=1000mL 1
The percentage of iron absorption was determined by measuring the
incorporation of
58
Fe tracer into red blood cells collected 14 d post-
dosing by using previously reported equations (29) and assuming that
90% of the absorbed iron was incorporated into red blood cells (28).
Statistical analyses
Linear regression was used to examine associations between
iron-status indicators and iron absorption at 2M and 5M and
assess determinants of iron absorption. Binomial regression was
used to obtain risk ratio estimates (3032) to examine the effect
of fetal iron exposure on categorical outcomes. To adjust for
multiple hypothesis testing, signicance was determined after
applying the Bonferroni correction. All P values presented are
original (unadjusted) P values for interpretation purposes, and
the threshold used to determine statistical signicance was
a On 2
where a is the level of signicance (a = 0.05), and n is the
number of multiple comparison tests conducted. If results were
signicant after the application of the Bonferroni correction, the
signicance is reported in the text.
Conventional cutoffs were used to categorize risk factors,
where available; otherwise, medians were used to classify var-
iables. Anemia was dened as hemoglobin concentrations ,12.0
g/dL in postpartum women and ,11.0 g/dL in infants in ac-
cordance with WHO criteria and clinical guidelines in Peru (3).
ID was dened as SF concentrations ,12 mg/L in both mothers
and infants (5). IDA was dened in the presence of both anemia
and depleted ferritin stores. Maternal sTfR concentrations
.5.33 mg/L were classied as ID on the basis of recent
NHANES data from nonpregnant women (33). BMI (in kg/m
2
)
was dened as the ratio of weight to height squared. Infant
ponderal index was calculated as the ratio of grams to the length
cubed (g/cm
3
3 100). Ferritin values were log-transformed to
account for the nonnormal distribution of this variable, but
values in the text are presented as nontransformed values for
interpretation purposes. In predictor analyses, variables with
univariate P values ,0.20 were included in each of the multi-
variate regression models and retained if their P values were
,0.05.
We examined potential confounders, and adjusted all gesta-
tional iron exposure and growth analyses for infant sex. The
missing indicator method was used to account for missing pre-
dictor data (34).
Potential predictors of study outcomes were also examined as
continuous variables. We explored the potential nonlinearity of
relations between covariates and outcomes nonparametrically by
using stepwise restricted cubic splines (35, 36). We used tests for
nonlinearity by using the likelihood ratio test and comparing the
model with only the linear term to the model with the linear and
the cubic spline terms. If nonlinear associations are not reported,
they were not signicant. Statistical analyses were performed
with SAS software (version 9.3; SAS Institute Inc).
RESULTS
Baseline characteristics of the 59 women and infant pairs
included in the analyses are presented in Table 1. The average
age of women in the study was 24.3 y, and the average BMI was
25.2. None of the women were underweight (BMI ,18.5), and
50.9% of women were overweight (BMI $25.0) at the 2M
study. Of the 59 infants initially enrolled, 30 infants were born to
+Fe women, and 29 infants were born to 2Fe women (#1320
mg Fe supplementation across gestation).
Maternal and infant iron status at 2M and 5M are presented in
Table 2. At the 2M postpartum baseline assessment, 64.9% of
IRON ABSORPTION IN BREASTFED PERUVIAN INFANTS 1477
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
women were anemic, with a mean (6SD) hemoglobin concen-
tration of 11.4 6 1.6 g/dL. The prevalence of anemia in infants
was similarly high; 77.2% of infants had hemoglobin concen-
trations ,11.0 g/dL (ranging from 8.0 to 14.6 g/dL, with 31.6%
and 8.9% of infants with hemoglobin concentrations ,10.0 and
,9.0 g/dL, respectively). Despite the high prevalence of infant
anemia, maternal and infant ferritin concentrations averaged
20.6 620.3 and 164.46103.8 mg/L, respectively, at 2M. A total
of 49.0% of mothers were iron decient (ferritin concentration
,12 mg/L), and 36.7% of mothers had IDA at 2M compared
with 31.9% (P = 0.01) and 21.3% (P . 0.05) of mothers at 5M
postpartum. Although no infants had ID (ferritin ,12 mg/L) or
IDA at 2M, 28.6% of infants had ferritin concentrations ,12
mg/L, 59.2% of infants had ferritin concentrations ,30 mg/L,
and 24.5% of infants had IDA at 5 mo of age. Prenatal iron
supplementation had no signicant effects on indicators of
postpartum maternal or infant iron status measured, except he-
matocrit and sTfR (compared with infants born to 2Fe mothers,
infants born to +Fe mothers had higher hematocrit and sTfR at
2M; P , 0.05). After correction for multiple hypothesis testing,
prenatal iron supplementation had no signicant effects on in-
dicators of postpartum maternal or infant iron status measured
(P . 0.0025).
In analyses of correlations between maternal and infant iron
status at both 2M and 5M time points, maternal hemoglobin
concentrations were associated with infant hemoglobin at both
time points; low maternal hemoglobin concentrations were sig-
nicantly associated with low infant hemoglobin concentrations
at both 2M (R = 0.38, P = 0.007) and 5M (R = 0.31, P = 0.02),
although the magnitude of association decreased at 5M. Maternal
and infant hematocrit were signicantly correlated at 5M (R = 0.42,
P = 0.01). Infants born to iron-decient mothers (at 2M) were
signicantly more likely to be iron decient at 5M (R = 0.33, P =
0.008), irrespective of iron group.
In analyses of longitudinal changes in maternal and infant iron
status between 2M and 5M, maternal sTfR signicantly de-
creased between 2M and 5M (P = 0.02); and maternal serum iron
signicantly increased during the follow-up period (P = 0.01).
There were no signicant changes in maternal hemoglobin, SF,
or hematocrit between 2M and 5M. Although no infants had
ferritin concentrations ,12 mg/L at 2M, infant SF signicantly
decreased (P , 0.0001), infant sTfR signicantly increased
(P , 0.0001), and infant serum iron signicantly decreased
between 2M and 5M (P , 0.01). Although signicant changes
in infant iron stores were apparent, there were no signicant
changes in infant hemoglobin, hematocrit, or CRP between 2M
and 5M, nor were there any signicant differences in changes in
any of the iron status indicators previously mentioned by ges-
tational iron exposure (Table 2). As expected, infant weight
(P , 0.0001) and length (P , 0.0001) signicantly increased,
and the ponderal index (P , 0.001) signicantly decreased be-
tween 2M and 5M (Table 1). Findings from these analyses re-
mained signicant after correction for multiple hypothesis testing,
except for changes in maternal sTfR (,0.05 but .0.0125).
Breast-milk micronutrient concentrations and infant iron ab-
sorption at 2M and 5M and average changes between time points
are presented in Table 3. Breast-milk iron concentrations de-
creased between 2M and 5M, although this change was not
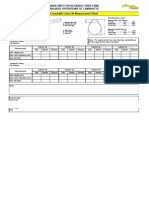
TABLE 1
Characteristics of the mothers and infants
1
Variables Total (n = 59) +Fe (n = 30) 2Fe (n = 29)
Maternal
Age (y) 24.3 6 4.8
2
24.9 6 5.6 23.7 6 3.8
Height (m) 1.5 6 0.1 1.5 6 0.1 1.5 6 0.1
Supplemental iron intake (mg) 3050.1 6 3276.3 6118.6 6 2114.3 299.1 6 358.5
Weight (2M) (kg) 56.9 6 7.1 57.6 6 6.3 56.2 6 7.8
BMI (2M) (kg/m
2
) 25.2 6 3.2 25.0 6 3.1 25.4 6 3.4
Overweight (2M) [n (%)]
3
30 (50.9) 14 (46.7) 16 (55.2)
Weight (5M) (kg) 55.7 6 8.1 55.4 6 7.1 56.0 6 9.1
BMI (5M) (kg/m
2
) 24.7 6 3.9 24.1 6 3.4 25.3 6 4.3
Overweight (5M) [n (%)]
3
26 (47.3) 13 (44.8) 13 (50.0)
Infant
Sex (F) [n (%)] 28 (47.5) 13 (43.3) 15 (51.7)
Birth weight (kg) 3.47 6 0.45 3.57 6 0.44 3.37 6 0.45
Birth length (cm) 50.6 6 1.7 50.9 6 1.9 50.2 6 1.4
Ponderal index at birth (g/cm
3
) 2.7 6 0.3 2.7 6 0.3 2.6 6 0.3
Age at 2M study (d) 69.2 6 9.1 70.3 6 9.7 68.0 6 8.6
Weight (2M) (kg) 5.89 6 0.80 6.0 6 0.7 5.76 6 0.85
Weight (5M) (kg) 7.72 6 0.97 7.9 6 0.9 7.58 6 1.01
Length (2M) (cm)** 59.1 6 2.7 59.9 6 2.3 58.1 6 2.8
Length (5M) (cm) 65.8 6 2.5 66.4 6 2.5 65.1 6 2.3
Ponderal index (2M) (g/cm
3
) 2.9 6 0.3 2.8 6 0.2 2.9 6 0.3
Ponderal index (5M) (g/cm
3
) 2.7 6 0.3 2.7 6 0.3 2.7 6 0.2
1
For statistical analyses, linear regression and binomial regression were used to examine differences in characteristics
between iron groups. **No signicant differences between the 2 groups after correction for multiple hypothesis testing,
except for infant length at 2M, P ,0.01. 2M, 23 mo of age; 5M, 56 mo of age; 2Fe, infants born to women who received
#1320 mg supplemental prenatal Fe; +Fe, infants born to women who received $5100 mg supplemental prenatal Fe.
2
Mean 6 SD (all such values).
3
Overweight was dened as BMI (in kg/m
2
) $25.
1478 FINKELSTEIN ET AL
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
TABLE 2
Maternal and infant iron status by prenatal iron supplementation
1
Variables Time point Total (n = 59) +Fe (n = 30) 2Fe (n = 29)
Maternal
Hemoglobin (g/dL) 2M 11.4 6 1.6
2
11.2 6 1.8 11.8 6 1.2
5M 11.7 6 1.3 11.6 6 1.3 11.8 6 1.3
D2M to 5M 0.2 6 2.0 0.4 6 2.3 0.0 6 1.6
Anemic [n (%)]
3
2M 37 (64.9) 20 (66.7) 17 (63.0)
5M 26 (47.3) 13 (46.4) 13 (48.2)
Serum ferritin (mg/L) 2M 20.6 6 20.3 21.3 6 22.3 20.0 6 18.4
5M 22.8 6 18.5 24.6 6 21.4 18.8 6 14.7
D2M to 5M 0.6 6 16.6 3.0 6 18.9 21.8 6 13.8
Serum ferritin concentration ,12 mg/L [n (%)] 2M 24 (49.0) 11 (44.0) 13 (54.2)
5M 15 (31.9) 7 (29.2) 8 (34.8)
IDA [n (%)]
3
2M 18 (36.7) 10 (40.0) 8 (33.3)
5M 10 (21.3) 4 (16.7) 6 (26.1)
Hematocrit 2M 34.5 6 3.8 33.4 6 4.3 35.8 6 2.7
5M 35.5 6 3.6 35.3 6 3.9 35.8 6 3.3
D2M to 5M 0.8 6 5.1 1.5 6 6.2 0.0 6 3.6
Total iron binding capacity (mg/dL) 2M 391.8 6 62.4 382.8 6 59.3 400.9 6 66.3
5M 370.2 6 70.4 347.2 6 52.4 393.3 6 80.3
D2M to 5M 221.6 6 87.0 235.6 6 60.4 27.5 6 108.1
sTfR (mg/L) 2M 6.9 6 3.1 6.5 6 2.8 7.3 6 3.4
5M 6.3 6 3.0 6.1 6 2.2 6.4 6 3.7
D2M to 5M 20.7 6 1.7 20.4 6 1.6 20.9 6 1.8
sTfR concentration .5.33 mg/L (%) 2M 67.6 6 25 50.0 6 9 84.2 6 16
5M 56.8 6 21 44.4 6 8 68.4 6 13
Serum iron (mg/dL) 2M 57.6 6 20.8 63.9 6 19.6 49.6 6 21.0
5M 74.3 6 29.7 85.6 6 29.3 59.9 6 25.1
D2M to 5M 16.7 6 23.8 21.7 6 25.5 10.3 6 21.5
Infant
Hemoglobin (g/dL) 2M 10.4 6 1.2 10.5 6 1.0 10.4 6 1.5
5M 10.4 6 1.0 10.2 6 1.0 10.7 6 0.9
D2M to 5M 20.0 6 1.4 20.3 6 1.0 0.3 6 1.8
Anemic [n (%)]
3
2M 44 (77.2) 24 (80.0) 20 (74.1)
5M 41 (78.9) 24 (88.9) 17 (68.0)
Serum ferritin (mg/L) 2M 164.4 6 103.8 151.1 6 79.5 178.3 6 124.5
5M 34.5 6 31.4 31.5 6 26.7 37.7 6 35.9
D2M to 5M 2129.9 6 91.3 2119.6 6 61.9 2140.6 6 114.8
Serum ferritin concentration ,12 mg/L [n (%)] 2M 0.0 6 0 0.0 6 0 0.0 6 0
5M 28.6 6 14 32.0 6 8 25.0 6 6
IDA [n (%)]
4
2M 0.0 6 0 0.0 6 0 0.0 6 0
5M 24.5 6 12 32.0 6 8 16.7 6 4
sTfR (mg/L) 2M 2.3 6 1.9 2.6 6 1.8** 2.1 6 1.9**
5M 4.7 6 2.0 4.7 6 1.9 4.7 6 2.0
D2M to 5M 2.4 6 2.3 2.2 6 2.4 2.7 6 2.2
Hematocrit 2M 30.2 6 5.3 31.0 6 2.0** 29.4 6 7.2**
5M 31.3 6 3.1 31.1 6 2.9 31.6 6 3.4
D2M to 5M 1.2 6 5.0 20.2 6 2.7 2.4 6 6.3
Serum iron (mg/dL) 2M 70.9 6 25.1 72.2 6 31.0 69.4 6 17.0
5M 60.5 6 26.3 62.8 6 23.8 57.9 6 23.5
D2M to 5M 220.7 6 28.0 218.8 6 31.2 223.9 6 23.5
CRP (mg/L) 2M 4.5 6 6.7 3.6 6 3.1 5.5 6 9.1
5M 4.1 6 3.3 4.3 6 4.4 3.9 6 1.8
D2M to 5M 20.5 6 6.9 0.7 6 5.9 21.6 6 7.7
CRP concentration .5 mg/L (%) 2M 15.4 6 4 7.7 6 1 23.1 6 3
5M 15.4 6 4 23.1 6 3 7.7 6 1
1
For statistical analyses, linear and binomial regression analyses were conducted to examine associations between iron supplementation and iron-status
indicators. **No signicant differences between the 2 groups after correction for multiple hypothesis testing, P .0.0025. CRP, C-reactive protein; IDA, iron-
deciency anemia; sTfR, serum transferrin receptor; 2M, 23 mo of age; 5M, 56 mo of age; 2Fe, infants born to women who received #1320 mg
supplemental prenatal Fe; +Fe, infants born to women who received $5100 mg supplemental prenatal Fe.
2
Mean 6 SD (all such values).
3
Anemia if hemoglobin concentrations ,12.0 g/dL for women and ,11.0 g/dL for infants.
4
IDA if hemoglobin concentrations ,12.0 g/dL and serum ferritin concentrations ,12 mg/L for women and hemoglobin concentrations ,11.0 g/dL and
serum ferritin concentrations ,12 mg/L for infants.
IRON ABSORPTION IN BREASTFED PERUVIAN INFANTS 1479
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
statistically signicant (P . 0.05). In contrast, breast-milk
copper (P = 0.001) and zinc (P , 0.001) concentrations both
signicantly decreased across the study period after adjustment
for multiple hypothesis testing.
Iron absorption from breast milk averaged 7.1 6 6.6% and
13.9 6 12.1% at 2M and 5M, respectively (Table 3). Iron ab-
sorption tended to increase between 2M and 5M (P = 0.09),
which was consistent with the response to the depletion of iron
stores. Although the percentage iron absorption tended to in-
crease, because of the low iron content of breast milk, this in-
crease would not lead to a marked increase in net iron
absorption. There were no signicant associations of fetal iron
exposure and subsequent iron absorption at 2M and 5M or on
changes between time points. There were no signicant differ-
ences in iron absorption in subjects who received tracer that had
equilibrated in breast milk overnight (n = 15) compared with in
subjects who received the tracer alone before being breastfed
(n = 44) [median (IQR): 4.0% (2.15.8%) equilibrated compared
with 5.1% (3.49.5%) nonequilibrated at 2M; 7.7% (3.98.8%)
equilibrated compared with 10.4% (6.519.4%) nonequilibrated
at 5M]. In analyses of the method of dose administration
(equilibrated compared with nonequilibrated with breast milk)
and iron absorption, there were no signicant differences be-
tween iron absorption at 2M and 5M or paired changes between
time points after adjustment for multiple hypothesis testing.
The value of a 90% red blood cell incorporation rate (28) was
used to be consistent with other data reported in healthy infants
(3739) and, in particular, to be consistent with values used in
healthy infants from the same Peruvian community (37). Other
published literature has used lower red blood cell incorporation
values that ranged from 23% to 80% (40, 41). If the middle
range of these estimates were used (60%), the average iron-
absorption value obtained would have been 10.6 6 9.9% and
20.9 6 18.1% at 2M and 5M, respectively (90%: 7.1 6 6.6%
at 2M and 13.9 6 12.1% at 5M; 80%: 8.0 6 7.4% at 2M and
15.7 613.6% at 5M). Fomon et al (41) reported that erythrocyte
incorporation of an orally administered
58
Fe tracer was 52% in
older infants (168 d old) compared with 23% in younger infants
(56 d old); the use of Fomon et al (41) values of 23% and/or
52% would have increased our absolute absorption results fur-
ther (23%: 27.8 6 25.8% at 2M; 52%: 24.1 6 20.9% at 5M; or
23%: 54.5 6 47.2% at 5M) but would not have changed the
relative associations we reported for other observations.
Associations of breast-milk nutrient concentrations and infant
iron absorption are presented in Table 4. Breast-milk nutrient
concentrations at 2M were not signicantly associated with in-
fant iron absorption at 2M (P . 0.05). Breast-milk iron con-
centrations at 5M (P = 0.07) and changes in iron concentrations
between 2M and 5M (P = 0.04) were associated with increased
infant iron absorption at 5M. Higher breast-milk copper
concentrations (5M) (P = 0.03) were associated with signi-
cantly increased infant iron absorption at 5M. After adjust-
ment for multiple hypothesis testing, these associations were
no longer signicant (P , 0.05 but .0.0167). There were no
signicant differences in associations between breast-milk
TABLE 3
Breast-milk nutrient concentrations and infant iron absorption by iron supplementation
1
Variable Total (n = 59) +Fe (n = 30) 2Fe (n = 29)
Iron absorption (%)
2M 7.1 6 6.6 8.0 6 8.9 6.3 6 3.6
5M 13.9 6 12.1 13.0 6 13.3 14.8 6 11.1
D2M to 5M 5.2 6 13.3 2.8 6 15.9 7.1 6 11.1
Breast-milk nutrient concentrations
Iron (mmol/L)
2M 8.0 6 3.3 8.1 6 4.0 7.9 6 2.3
5M 7.4 6 2.9 7.2 6 3.0 7.6 6 2.9
D2M to 5M 20.6 6 3.7 20.9 6 4.2 20.2 6 3.0
Copper (mmol/L)
2M 5.1 6 1.5 4.9 6 1.4 5.3 6 1.6
5M 4.3 6 1.3 4.1 6 1.5 4.4 6 1.2
D2M to 5M 20.8 6 1.5*** 20.7 6 1.4 20.8 6 1.7
Zinc (mmol/L)
2M 27.1 6 11.2 26.1 6 10.3 28.3 6 12.1
5M 17.7 6 7.9 16.1 6 6.2 19.3 6 9.4
D2M to 5M 29.5 6 8.3*** 210.0 6 9.1 28.9 6 7.5
1
All values are means 6 SDs. For statistical analyses, linear regression was used to examine differences in iron
absorption and breast-milk nutrient concentrations by iron supplementation. ***Remained signicant after correction for
multiple hypothesis testing (P , 0.01). 2M, 23 mo of age; 5M, 56 mo of age; 2Fe, infants born to women who received
#1320 mg supplemental prenatal Fe; +Fe, infants born to women who received $5100 mg supplemental prenatal Fe.
TABLE 4
Breast-milk nutrient concentrations and infant iron absorption
1
Iron absorption (5M) Time point Value P
Breast-milk iron (mmol/L) 2M 20.40 6 0.61 0.52
5M 1.36 6 0.72 0.07
D2M to 5M 1.12 6 0.53 0.04*
Breast-milk copper (mmol/L) 2M 2.89 6 1.46 0.06
5M 3.71 6 1.67 0.03*
D2M to 5M 20.14 6 1.49 0.93
Breast-milk zinc (mmol/L) 2M 0.12 6 0.18 0.51
5M 20.02 6 0.25 0.92
D2M to 5M 20.26 6 0.25 0.30
1
All values are means 6 SDs. For statistical analyses, linear regression
was used to examine associations between breast-milk nutrient concentra-
tions and iron absorption. *NS after correction for multiple hypothesis test-
ing (P , 0.05 but .0.0167). 2M, 23 mo of age; 5M, 56 mo of age.
1480 FINKELSTEIN ET AL
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
nutrient concentrations and iron absorption by gestational
iron exposure.
Results from analyses of predictors of infant iron absorption at
2M and 5M are presented in Table 5. Maternal anemia (2M) (P =
0.02) and higher infant sTfR concentrations (2M) (P = 0.02)
were associated with increased infant iron absorption at 2M. In
analyses of predictors of iron absorption at 5M, breast-milk
copper concentrations (5M) (P , 0.01) and infant sTfR con-
centrations (5M) (P , 0.01) were associated with increased
infant iron absorption (5M).
Associations of fetal iron exposure and infant length, weight,
and ponderal index are presented in Table 6. Fetal iron exposure
was not associated with differences in birth length but was as-
sociated with signicantly greater infant length at 2M (P ,
0.01) and 5M (P , 0.05), indicative of a change in the early
tempo of growth between these 2 groups. There were no sig-
nicant effects of fetal iron exposure on infant weight at any
time point (birth, 2M, or 5M). Fetal iron exposure was associ-
ated with a signicantly reduced ponderal index at 2M (P ,
0.05). Results in analyses of fetal iron exposure on infant growth
remained similar (and more signicant) after adjustment for
infant sex (Table 6), and the effects of iron exposure on infant
length at 2M and 5M remained signicant (P , 0.01) after
adjustment for multiple hypothesis testing.
DISCUSSION
In this study, anemia and ID were common in lactating women
at 2 and 5 mo postpartum and in their exclusively breastfed
infants. Although there are limited data on the iron status of
postpartum women and young infants, the prevalence of anemia
and ID in this study were similar to previous data from resource-
limited settings (1, 2) and higher than in studies in pregnant
women (4245) and older infants (37, 46, 47). In an analysis of
data from 6 studies in exclusively breastfed infants at 6 mo of
age, the prevalence of ID (SF ,12 mg/L) was 6% in Sweden,
17% in Mexico, 1325% in Honduras, and 1237% in Ghana
(46). In a previous study in 612-mo-old Peruvian infants, 67%
of infants were anemic and 60% were iron decient (SF con-
centration ,20 mg/L) (47). National surveys in Peru have re-
ported an anemia prevalence of 69% (68 mo of age) to 72%
(911 mo of age) in older infants (26, 37). However, little data
are available from infants ,6 mo of age, and most data relied on
cross-sectional assessments.
The lack of normative iron status data in young, healthy infants
may have been attributable to challenges in obtaining venous
samples and the belief that, in most instances, the iron endow-
ment of birth should be sufcient to maintain early iron status
over the rst 6 mo of life. In this study, iron stores of birth were
signicantly depleted between 2 and 5 mo of age; nearly one-
third of infants had depleted iron stores (SF concentration ,12
mg/L), and 78.9% of infants were anemic by 5M. These results
suggested that these full-term, exclusively breastfed Peruvian
infants were not endowed with sufcient body iron at birth to
meet requirements for growth and development over the rst 46
mo of life (48, 49). It is known that delayed cord clamping has
a considerable impact on infant iron status (50, 51) and can
increase neonatal blood volume by 60% (52) and red blood cells
by .30% (53). Although we did not have data on cord-clamping
times in these infants, delayed cord clamping is routinely un-
dertaken in the Villa El Salvador community. Young, exclusively
breastfed infants may be vulnerable to ID and IDA unless in-
testinal iron absorption can be upregulated in response to iron
demands.
Infant iron absorption from breast milk in this study (2M: 7.1
66.6%; 5M: 13.9 612.1%) was similar to data from a previous
Swedish study in which iron absorption from tracer given with
a breast-milk feed averaged 16.4 611.4% in 56-mo-old infants
and 25.7 6 17.2% in 59-mo-old infants (54). However, these
data were lower than the 36.8 6 9.3% (anemic) and 41.8 6
7.9% (nonanemic) iron absorption reported in 56-mo-old
nonexclusively breastfed Peruvian infants when tracer was ad-
ministered along with breast milk (37).
TABLE 5
Predictors of infant iron absorption
1
Variable
Univariate
(P , 0.20)
Multivariate
(P , 0.05)
Value P Value P
Iron absorption (2M)
Maternal anemia (2M)
2
4.05 6 2.32 0.09 5.44 6 2.24 0.02
Infant sTfR (2M) (mg/L) 1.13 6 0.63 0.08 1.47 6 0.59 0.02
Iron absorption (5M)
Breast-milk copper (5M)
(mmol/L)
3.71 6 1.67 0.03 4.06 6 1.46 ,0.01
Infant sTfR (5M) (mg/L) 2.78 6 1.00 ,0.01 2.96 6 0.92 ,0.01
1
All values are parameters 6 SEs. For statistical analyses, linear re-
gression was used to assess determinants of iron absorption. sTfR, serum
transferrin receptor; 2M, 23 mo of age; 5M, 56 mo of age.
2
Anemia was dened as hemoglobin concentrations ,12.0 g/dL for
women.
TABLE 6
Maternal prenatal iron supplementation and infant length, weight, and
ponderal index
1
Variable 2Fe (n = 29)
+Fe (n = 30)
P P
2
Difference
Length (cm)
Birth 50.2 6 0.3 0.7 6 0.4 0.12 0.16
2M 58.1 6 0.5 1.9 6 0.7 ,0.01** ,0.01**
5M 65.1 6 0.5 1.3 6 0.7 ,0.05 0.01**
Weight (kg)
Birth 3.4 6 0.1 0.2 6 0.1 0.10 0.13
2M 5.8 6 0.2 0.2 6 0.2 0.24 0.33
5M 7.6 6 0.2 0.3 6 0.3 0.29 0.29
Ponderal index (g/cm
3
)
Birth 2.7 6 0.1 0.1 6 0.1 0.51 0.48
2M 2.9 6 0.1 20.2 6 0.1 ,0.05 0.04
5M 2.7 6 0.1 20.1 6 0.1 0.46 0.49
1
All values are parameters 6 SEs. Infant length, weight, and ponderal
index are presented for the iron-unsupplemented group; the difference
(6SE) is the average difference of infant length, weight, and ponderal index
between iron-supplemented and -unsupplemented groups. For statistical
analyses, binomial regression was used to obtain risk-ratio estimates to
examine the effect of fetal iron exposure on categorical outcomes. **Re-
mained signicant after correcting for multiple hypothesis testing, P ,
0.0167. 2M, 23 mo of age; 5M, 56 mo of age; 2Fe, infants born to women
who received #1320 mg supplemental prenatal Fe; +Fe, infants born to
women who received $5100 mg supplemental prenatal Fe.
2
After adjustment for infant sex.
IRON ABSORPTION IN BREASTFED PERUVIAN INFANTS 1481
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
In adults, absorption of nonheme iron is regulated in response
to iron stores (55), but the degree to which this occurs over early
infancy is uncertain. Data from Honduras and Sweden suggested
there is a developmental delay in the regulation of iron ab-
sorption, and healthy neonates do not develop the ability to
regulate iron absorption in response to iron stores until 69 mo of
age (54, 56). However, a previous study from Peru showed that
infants with low iron stores (SF concentration ,12 mg/L) up-
regulated iron absorption from breast milk at 56 and 910 mo
of age (37). The current study provides evidence that this effect
may occur even earlier, as early as 25 mo of age.
The effects of maternal iron supplementation on iron status
have been equivocal to date. In the current study, supplemental
gestational iron intake had no signicant effects on maternal or
infant iron status, breast-milk iron concentrations, or infant iron
absorption in early infancy, although iron intake and dietary
variability were low in this population (57). Despite a lack of
an impact on iron status, in utero iron exposure signicantly
inuenced early growth potential, as evidenced by increased
infant length at 2M and 5M. Findings from studies of the effects
of prenatal iron supplementation on early infant growth have
been inconsistent. In a randomized placebo-controlled trial of
iron supplementation in Niger in pregnant women, prenatal iron
supplementation was associated with signicantly increased
infant length at birth (10). Iron was also associated with increased
infant length at 3 and 6 mo of age compared with a placebo,
although this difference was not statistically signicant (10). In
a randomized placebo-controlled trial of iron supplementation in
pregnant women in Cleveland, OH, birth length was slightly
higher in the Fe-supplemented group, although this result was not
statistically signicant (58). However, in a meta-analysis, iron-
only interventions (n = 27) had no effect on linear growth,
whereas multiple micronutrients (n = 20) signicantly improved
linear growth (59). A recent randomized trial in Burkina Faso
noted a signicant cumulative effect of both multiple micro-
nutrients and iron folate on fetal growth (60). This result was
consistent with the growing appreciation of the impact of in
utero iron status on developmental programming (6163).
In the current study, we examined breast-milk iron, zinc, and copper
concentrations and their associations with infant iron absorption and
status prospectively. Iron and copper concentrations at 5M and
changes in iron concentrations between 2Mand 5Mwere associated
with signicantly increased iron absorption at 5M. Breast-milk iron,
zinc, and copper molar concentrations were similar to a previous
study in Lima, Peru, in breastfeeding mothers at delivery to 6 mo
postpartum (64). Breast-milk iron, zinc, and copper concentrations
declined between 2M and 5M (P , 0.001).
To date, there has been a limited assessment of iron absorption
in exclusively breastfed, young infants. Few studies have
assessed the impact of fetal iron exposure on early infant iron
homeostasis (65), particularly in ID populations. Our analysis
was distinct from previous studies because of the young age of
infants studied, assessment of both maternal and infant iron
status, longitudinal paired iron-absorption measures, selection of
infants on the basis of gestational iron exposure, and role of
breast-milk micronutrient ratios in iron absorption. To our
knowledge, this was the rst such longitudinal iron absorption
study of 25-mo-old infants.
One limitation of this analysis was the lack of data on ma-
ternal iron status during pregnancy, delivery practices (eg, cord
clamping), and neonatal iron status at birth. These factors
would have provided additional information on determinants of
early iron homeostasis. Similarly, maternal supplemental iron
intake was based on self-report. Because this study was not
a randomized trial of iron supplementation, the study design did
not rule out the possible inuence of other potential con-
founders, which may have explained the observed associations
between iron intake and infant growth. Additional biomarkers,
such as hepcidin, or additional measures of inammation (eg,
alpha-1-acid glycoprotein) would have strengthened this
analysis.
In conclusion, fetal iron exposure did not signicantly affect
iron status or absorption in young, exclusively breastfed infants at
25 mo of age. However, fetal iron exposure across gestation
was associated with signicantly improved infant growth, which
was a nding that warrants additional investigation. Full-term,
exclusively breastfed infants from this community may not be
endowed with sufcient body iron to meet the iron requirements
needed for the rst 6 mo of life. Young infants are able to up-
regulate iron absorption when iron stores are depleted, as early
as 25 mo of age, but this may not be adequate to meet iron
demands. Thus, young exclusively breastfed infants may be
vulnerable to ID and IDA and represent an important risk group.
Additional attention needs to be focused on optimizing the iron
endowment at birth and characterizing sources of variability in
iron absorption and determinants of ID across early infancy.
Screening and targeted preventive interventions are needed for
ID and anemia in young infants, particularly in settings with
high ID burden.
We are grateful to the mothers, children, and eld teams, including phy-
sicians, nurses, eld staff, laboratory staff, and the administrative staff, who
made this study possible and the Cesar Lopez Silva Hospital Micro Red Villa
El Salvador-Lurin Pachacamac Pucusana and Direccion de Salud Integral
Lima Sur for institutional support.
The authors responsibilities were as followsKOO, SAA, and NZ: de-
signed and conducted the study; JLF: performed statistical analyses and
wrote the initial draft of the manuscript; and all authors: assisted in the
interpretation of data and writing of the manuscript. The funders of the study
had no role in the study design, implementation of data collection, data
analysis, data interpretation, or writing of the manuscript. None of the au-
thors had a conict of interest.
REFERENCES
1. WHO/CDC. Worldwide prevalence of anaemia 1993-2005. WHO
Global Database on Anaemia. Geneva, Switzerland: WHO, 2008.
2. McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide
prevalence of anaemia, WHO Vitamin and Mineral Nutrition In-
formation System, 1993-2005. Public Health Nutr 2009;12:44454.
3. WHO. Iron deciency anemia: assessment, prevention and control:
a guide for programme managers. Geneva, Switzerland: WHO, 2001.
4. Bowman BA, Russell RM. Present knowledge in nutrition. 9th ed.
Washington, DC: ILSI Press, 2006.
5. Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Preva-
lence of iron deciency in the United States. JAMA 1997;277:9736.
6. Hallberg L. Results of surveys to assess iron status in Europe. Nutr Rev
1995;53:31422.
7. WHO. Global health risks. Mortality and burden of disease attributable
to selected major risk factors. Geneva, Switzerland: WHO, 2009.
8. Brabin BJ, Premji Z, Verhoeff F. An analysis of anemia and child
mortality. J Nutr 2001;131(2S-2):636S45S; discussion 646S8S.
9. Ervasti M, Sankilampi U, Heinonen S, Punnonen K. Early signs of
maternal iron deciency do not inuence the iron status of the new-
born, but are associated with higher infant birthweight. Acta Obstet
Gynecol Scand 2009;88:8390.
1482 FINKELSTEIN ET AL
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
10. Preziosi P, Prual A, Galan P, Daouda H, Boureima H, Hercberg S.
Effect of iron supplementation on the iron status of pregnant
women: consequences for newborns. Am J Clin Nutr 1997;66:1178
82.
11. Allen LH. Pregnancy and iron deciency: unresolved issues. Nutr Rev
1997;55:91101.
12. El-Farrash RA, Ismail EA, Nada AS. Cord blood iron prole and breast
milk micronutrients in maternal iron deciency anemia. Pediatr Blood
Cancer 2012;58:2338.
13. Colomer J, Colomer C, Gutierrez D, Jubert A, Nolasco A, Donat J,
Fernandez-Delgado R, Donat F, Alvarez-Dardet C. Anaemia during
pregnancy as a risk factor for infant iron deciency: report from the
Valencia Infant Anaemia Cohort (VIAC) study. Paediatr Perinat Epi-
demiol 1990;4:196204.
14. Singla PN, Tyagi M, Shankar R, Dash D, Kumar A. Fetal iron status in
maternal anemia. Acta Paediatr 1996;85:132730.
15. Harthoorn-Lasthuizen EJ, Lindemans J, Langenhuijsen MM. Does
iron-decient erythropoiesis in pregnancy inuence fetal iron supply?
Acta Obstet Gynecol Scand 2001;80:3926.
16. Georgieff MK, MIlls MM, Gordon K, Wobken JD. Reduced neonatal
liver iron concentrations after uteroplacental insufciency. J Pediatr
1995;127:30811.
17. Choi JW, Kim CS, Pai SH. Erythropoietic activity and soluble trans-
ferrin receptor level in neonates and maternal blood. Acta Paediatr
2000;89:6759.
18. Roberfroid D, Huybregts L, Habicht JP, Lanou H, Henry MC, Meda N,
dAlessandro U, Kolsteren P. Randomized controlled trial of 2 prenatal
iron supplements: is there a dose-response relation with maternal he-
moglobin? Am J Clin Nutr 2011;93:10128.
19. Gambling L, Danzeisen R, Gair S, Lea RG, Charania Z, Solanky N,
Joory KD, Srai SK, McArdle HJ. Effect of iron deciency on placental
transfer of iron and expression of iron transport proteins in vivo and in
vitro. Biochem J 2001;356:8839.
20. McArdle HJ, Lang C, Hayes H, Gambling L. Role of the placenta in
regulation of fetal iron status. Nutr Rev 2011;69(suppl 1):S1722.
21. Balesaria S, Hanif R, Salama M, Raja K, Bayele HK, McArdle H, Srai
SK. Fetal iron levels are regulated by maternal and fetal Hfe genotype
and dietary iron. Haematologica 201297:6619.
22. Li YQ, Yan H, Bai B. Change in iron transporter expression in human
term placenta with different maternal iron status. Eur J Obstet Gynecol
Reprod Biol 2008;140:4854.
23. Young MF, Pressman E, Foehr ML, McNanley T, Cooper E, Guillet R,
Orlando M, McIntyre AW, Lafond J, OBrien KO. Impact of maternal
and neonatal iron status on placental transferrin receptor expression in
pregnant adolescents. Placenta 2010;31:10104.
24. OBrien KO, Zavaleta N, Abrams SA, Cauleld LE. Maternal iron
status inuences iron transfer to the fetus during the third trimester of
pregnancy. Am J Clin Nutr 2003;77:92430.
25. Mihaila C, Schramm J, Strathmann FG, Lee DL, Gelein RM, Luebke
AE, Mayer-Proschel M. Identifying a window of vulnerability during
fetal development in a maternal iron restriction model. PLoS ONE
2011;6:e17483.
26. National Institute of Statistics and Informatics (INEI) and ICF Macro.
Demographic and Health Survey - nal report continuous, 2010. May
2011:2548 (in Spanish). Available from: http://www.measuredhs.com/
pubs/pdf/FR250/FR250.pdf.
27. Zavaleta N, Cauleld LE, Figueroa A, Chen P. Patterns of compliance
with prenatal iron supplementation among Peruvian women. Matern
Child Nutr (Epub ahead of print 16 May 2012).
28. Kastenmayer P, Davidsson L, Galan P, Cherouvrier F, Hercberg S,
Hurrell RF. A double stable isotope technique for measuring iron ab-
sorption in infants. Br J Nutr 1994;71:41124.
29. Abrams SA, OBrien KO, Wen J, Liang LK, Stuff JE. Absorption by 1-
year-old children of an iron supplement given with cows milk or juice.
Pediatr Res 1996;39:1715.
30. Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prev-
alence ratios and differences. Am J Epidemiol 2005;162:199200.
31. Wacholder S. Binomial regression in GLIM: estimating risk ratios and
risk differences. Am J Epidemiol 1986;123:17484.
32. Zou G. A modied poisson regression approach to prospective studies
with binary data. Am J Epidemiol 2004;159:7026.
33. Mei Z, Pfeiffer CM, Looker AC, Flores-Ayala RC, Lacher DA, Mirel
LB, Grummer-Strawn LM. Serum soluble transferrin receptor con-
centrations in US preschool children and non-pregnant women of
childbearing age from the National Health and Nutrition Examination
Survey 2003-2010. Clin Chim Acta 2012;413:147984.
34. Miettinen O. Theoretical epidemiology. New York, NY: John Wiley &
Sons, 1985.
35. Durrleman S, Simon R. Flexible regression models with cubic splines.
Stat Med 1989;8:55161.
36. Govindarajulu US, Spiegelman D, Thurston SW, Ganguli B, Eisen EA.
Comparing smoothing techniques in Cox models for exposure-
response relationships. Stat Med 2007;26:373552.
37. Hicks PD, Zavaleta N, Chen Z, Abrams SA, Lonnerdal B. Iron de-
ciency, but not anemia, upregulates iron absorption in breast-fed
Peruvian infants. J Nutr 2006;136:24358.
38. Davidsson L, Kastenmayer P, Yuen M, Lonnerdal B, Hurrell RF. In-
uence of lactoferrin on iron absorption from human milk in infants.
Pediatr Res 1994;35:11724.
39. Abrams SA, Wen J, Stuff JE. Absorption of calcium, zinc, and iron
from breast milk by ve- to seven-month-old infants. Pediatr Res 1997;
41:38490.
40. Fomon SJ, Ziegler EE, Serfass RE, Nelson SE, Rogers RR, Frantz JA.
Less than 80% of absorbed iron is promptly incorporated into eryth-
rocytes of infants. J Nutr 2000;130:4552.
41. Fomon SJ, Serfass RE, Nelson SE, Rogers RR, Frantz JA. Time course
of and effect of dietary iron level on iron incorporation into erythro-
cytes by infants. J Nutr 2000;130:5415.
42. Zavaleta N, Cauleld LE, Garcia T. Changes in iron status during
pregnancy in peruvian women receiving prenatal iron and folic
acid supplements with or without zinc. Am J Clin Nutr 2000;71:95661.
43. Larocque R, Casapia M, Gotuzzo E, Gyorkos TW. Relationship be-
tween intensity of soil-transmitted helminth infections and anemia
during pregnancy. Am J Trop Med Hyg 2005;73:7839.
44. OBrien KO, Zavaleta N, Cauleld LE, Yang DX, Abrams SA. In-
uence of prenatal iron and zinc supplements on supplemental iron
absorption, red blood cell iron incorporation, and iron status in preg-
nant Peruvian women. Am J Clin Nutr 1999;69:50915.
45. Becerra C, Gonzales GF, Villena A, de la Cruz D, Florian A. [Preva-
lence of anemia in pregnancy, Pucallpa Regional Hospital, Peru.] Rev
Panam Salud Publica 1998;3:28592 (in Spanish).
46. Yang Z, Lonnerdal B, Adu-Afarwuah S, Brown KH, Chaparro CM,
Cohen RJ, Domellof M, Hernell O, Lartey A, Dewey KG. Prevalence
and predictors of iron deciency in fully breastfed infants at 6 mo of age:
comparison of data from 6 studies. Am J Clin Nutr 2009;89:143340.
47. Lopez de Romana G, Cusirramos S, Lopez de Romana D, Gross R.
Efcacy of multiple micronutrient supplementation for improving
anemia, micronutrient status, growth, and morbidity of Peruvian in-
fants. J Nutr 2005;135:646S52S.
48. Domellof M. Iron requirements in infancy. Ann Nutr Metab 2011;59:
5963.
49. Baker RD, Greer FR. Diagnosis and prevention of iron deciency and
iron-deciency anemia in infants and young children (0-3 years of
age). Pediatrics 2010;126:104050.
50. Chaparro CM, Neufeld LM, Tena Alavez G, Eguia-Liz Cedillo R,
Dewey KG. Effect of timing of umbilical cord clamping on iron status
in Mexican infants: a randomised controlled trial. Lancet 2006;367:
19972004.
51. McDonald SJ, Middleton P. Effect of timing of umbilical cord clamping
of term infants on maternal and neonatal outcomes. Cochrane Database
Syst Rev 2008;2:CD004074.
52. Garofalo M, Abenhaim HA. Early versus delayed cord clamping in term
and preterm births: a review. J Obstet Gynaecol Can2012;34:52531.
53. Strauss RG, Mock DM, Johnson KJ, Cress GA, Burmeister LF, Zim-
merman MB, Bell EF, Rijhsinghani A. A randomized clinical trial
comparing immediate versus delayed clamping of the umbilical cord in
preterm infants: short-term clinical and laboratory endpoints. Trans-
fusion 2008;48:65865
54. Domellof M, Lonnerdal B, Abrams SA, Hernell O. Iron absorption in
breast-fed infants: effects of age, iron status, iron supplements, and
complementary foods. Am J Clin Nutr 2002;76:198204.
55. Finch C. Regulators of iron balance in humans. Blood 1994;84:1697702.
56. Domellof M, Cohen RJ, Dewey KG, Hernell O, Rivera LL, Lonnerdal
B. Iron supplementation of breast-fed Honduran and Swedish infants
from 4 to 9 months of age. J Pediatr 2001;138:67987.
57. Sacco LM, Cauleld LE, Zavaleta N, Retamozo L. Dietary pattern and
usual nutrient intakes of Peruvian women during pregnancy. Eur J Clin
Nutr 2003;57:14927.
IRON ABSORPTION IN BREASTFED PERUVIAN INFANTS 1483
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
58. Cogswell ME, Parvanta I, Ickes L, Yip R, Brittenham GM. Iron sup-
plementation during pregnancy, anemia, and birth weight: a random-
ized controlled trial. Am J Clin Nutr 2003;78:77381.
59. Ramakrishnan U, Nguyen P, Martorell R. Effects of micronutrients
on growth of children under 5 y of age: meta-analyses of single
and multiple nutrient interventions. Am J Clin Nutr 2009;89:191
203.
60. Roberfroid D, Huybregts L, Lanou H, Habicht JP, Henry MC, Meda N,
Kolsteren P. Prenatal micronutrient supplements cumulatively increase
fetal growth. J Nutr 2012;142:54854.
61. Gambling L, Kennedy C, McArdle HJ. Iron and copper in fetal de-
velopment. Semin Cell Dev Biol 2011;22:63744.
62. Tamura T, Goldenberg RL, Hou J, Johnston KE, Cliver SP, Ramey SL,
Nelson KG. Cord serum ferritin concentrations and mental and psy-
chomotor development of children at ve years of age. J Pediatr 2002;
140:16570.
63. Ashworth CJ, Antipatis C. Micronutrient programming of development
throughout gestation. Reproduction 2001;122:52735.
64. Zavaleta N, Lanata C, Butron B, Peerson JM, Brown KH, Lonnerdal B.
Effect of acute maternal infection on quantity and composition of
breast milk. Am J Clin Nutr 1995;62:55963.
65. Grantham-McGregor S, Ani C. A review of studies on the effect of iron
deciency on cognitive development in children. J Nutr 2001;131(2S-
2):649S66S; discussion 66S8S.
1484 FINKELSTEIN ET AL
a
t
E
B
S
C
O
h
o
s
t
o
n
N
o
v
e
m
b
e
r
2
1
,
2
0
1
3
a
j
c
n
.
n
u
t
r
i
t
i
o
n
.
o
r
g
D
o
w
n
l
o
a
d
e
d
f
r
o
m
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Guidelines Skin Infections Guia Infeccion Piel 1373.fullDocumento34 pagineGuidelines Skin Infections Guia Infeccion Piel 1373.fullAldo Paz MarchenaNessuna valutazione finora
- Infecciones Oportunistas 2009Documento216 pagineInfecciones Oportunistas 2009Gilberto Gonzalez AquinoNessuna valutazione finora
- Profilaxis Tetanos Heridas TetwdmgmtcDocumento1 paginaProfilaxis Tetanos Heridas TetwdmgmtcAldo Paz MarchenaNessuna valutazione finora
- Acute Myocardial Infarction EkgDocumento4 pagineAcute Myocardial Infarction EkgAldo Paz MarchenaNessuna valutazione finora
- Acute Myocardial Infarction EkgDocumento4 pagineAcute Myocardial Infarction EkgAldo Paz MarchenaNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Ferrites and AccessoriesDocumento11 pagineFerrites and AccessoriesMaulik ShahNessuna valutazione finora
- Notifier Battery Calculations-ReadmeDocumento11 pagineNotifier Battery Calculations-ReadmeJeanCarlosRiveroNessuna valutazione finora
- Introduction To Curve FittingDocumento10 pagineIntroduction To Curve FittingscjofyWFawlroa2r06YFVabfbajNessuna valutazione finora
- Technical Data: Pump NameDocumento6 pagineTechnical Data: Pump Nameسمير البسيونىNessuna valutazione finora
- Rochor Station Pile Design CalculationsDocumento15 pagineRochor Station Pile Design CalculationsDifa LiuNessuna valutazione finora
- Craig Vaughan CHPTR 07Documento44 pagineCraig Vaughan CHPTR 07Jorge CananeaNessuna valutazione finora
- Operational Guidelines For VlsfoDocumento2 pagineOperational Guidelines For VlsfoИгорьNessuna valutazione finora
- Steps For Charm ConfigurationDocumento7 pagineSteps For Charm ConfigurationpoornasapNessuna valutazione finora
- Reference Mil-Aero Guide ConnectorDocumento80 pagineReference Mil-Aero Guide ConnectorjamesclhNessuna valutazione finora
- 2017 Yr 9 Linear Relations Test A SolutionsDocumento13 pagine2017 Yr 9 Linear Relations Test A SolutionsSam JeffreyNessuna valutazione finora
- Camshaft Test SheetDocumento4 pagineCamshaft Test SheetsughieantoNessuna valutazione finora
- F 2786538d6cdc0bb1Documento245 pagineF 2786538d6cdc0bb1Daniel HarutyunyanNessuna valutazione finora
- FMDS0129Documento49 pagineFMDS0129hhNessuna valutazione finora
- PDF Solution Manual For Gas Turbine Theory 6th Edition Saravanamuttoo Rogers CompressDocumento7 paginePDF Solution Manual For Gas Turbine Theory 6th Edition Saravanamuttoo Rogers CompressErickson Brayner MarBerNessuna valutazione finora
- 2010 MaxxForce DT-9-10 DiagnosticDocumento1.329 pagine2010 MaxxForce DT-9-10 Diagnosticbullfly100% (8)
- Probability Statistics and Random Processes Third Edition T Veerarajan PDFDocumento3 pagineProbability Statistics and Random Processes Third Edition T Veerarajan PDFbhavyamNessuna valutazione finora
- Leroy Somer 3434c - GB-NyDocumento28 pagineLeroy Somer 3434c - GB-NyCris_eu09100% (1)
- Create an access point for non-RouterOS laptop clientsDocumento8 pagineCreate an access point for non-RouterOS laptop clientsGorgeus WaffleNessuna valutazione finora
- Lecture 1: Encoding Language: LING 1330/2330: Introduction To Computational Linguistics Na-Rae HanDocumento18 pagineLecture 1: Encoding Language: LING 1330/2330: Introduction To Computational Linguistics Na-Rae HanLaura AmwayiNessuna valutazione finora
- Instrumentation Design UTHMDocumento5 pagineInstrumentation Design UTHMAnis AzwaNessuna valutazione finora
- Geophysical Report Megnatic SurveyDocumento29 pagineGeophysical Report Megnatic SurveyShahzad KhanNessuna valutazione finora
- Network Layer: Computer Networking: A Top Down ApproachDocumento83 pagineNetwork Layer: Computer Networking: A Top Down ApproachMuhammad Bin ShehzadNessuna valutazione finora
- Module 1 Introduction To Highway and Railroad EngineeringDocumento43 pagineModule 1 Introduction To Highway and Railroad EngineeringKenneth FajardoNessuna valutazione finora
- How To Publish A Package in RDocumento14 pagineHow To Publish A Package in Rtoton1181Nessuna valutazione finora
- Bab 8Documento29 pagineBab 8Nurul AmirahNessuna valutazione finora
- Data Structures and AlgorithmsDocumento45 pagineData Structures and AlgorithmsKeith Tanaka MagakaNessuna valutazione finora
- SRM Institute of Science and Technology Department of Mathematics Probability and Queueing Theory Tutorial Sheet I2Documento1 paginaSRM Institute of Science and Technology Department of Mathematics Probability and Queueing Theory Tutorial Sheet I2Cooldude 69Nessuna valutazione finora
- Logic CHPT71Documento27 pagineLogic CHPT71Eronjosh FontanozaNessuna valutazione finora
- NewsDocumento26 pagineNewsMaria Jose Soliz OportoNessuna valutazione finora