Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Parasites Evade The
Caricato da
Mike zombieDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Parasites Evade The
Caricato da
Mike zombieCopyright:
Formati disponibili
REVIEW
www.nature.com/natureimmunology november 2002 volume 3 no 11 nature immunology 1041
Parasitic protozoa are a major cause of global
infectious disease. These eukaryotic pathogens
have evolved with the vertebrate immune system
and typically produce long-lasting chronic infec-
tions. A critical step in their host interaction is
the evasion of innate immune defenses. The abili-
ty to avoid attack by humoral effector mecha-
nisms, such as complement lysis, is of particular
importance to extracellular parasites, whereas
intracellular protozoa must resist killing by lyso-
somal enzymes and toxic metabolites. They do so
by remodeling the phagosomal compartments in
which they reside and by interfering with signal-
ing pathways that lead to cellular activation. In
addition, there is growing evidence that proto-
zoan pathogens modify the antigen-presenting
and immunoregulatory functions of dendritic
cells, a process that facilitates their evasion of
both innate and adaptive immunity.
Laboratory of Parasitic Diseases, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD 20892, USA.
Correspondence should be addressed to D. S. (dsacks@nih.gov).
Evasion of innate immunity by
parasitic protozoa
David Sacks and Alan Sher
Parasitic protozoa are unicellular eukaryotic pathogens that dwell
inside host cells and/or in extracellular fluids. These organisms typical-
ly produce long-lasting chronic infections in order to maximize their
opportunities for successful transmission by contact with their interme-
diate hosts or release into the environment. Their success as parasites
depends on a series of intricate and highly evolved host adaptations that
enable them to evade destruction by the immune system.
Protozoan infections are a major global health problem, affecting
over half a billion people world wide. Several of the diseases they
induce (such as malaria, African trypanosomiasis and visceral leishma-
niasis) represent major causes of mortality and morbidity in tropical
countries and, as such, are important impediments to economic devel-
opment. No standardized vaccines exist for preventing any of the pro-
tozoan infections of humans, a situation attributed both to the com-
plexity of the pathogens involved and their sophisticated strategies for
evading host immune responses
1
.
Protozoan parasites are highly adept at escaping the effects of adap-
tive humoral and cellular immunity. Perhaps the simplest solution for
evading antibody responses is the adoption of an intracellular life style,
as is done by Leishmania, Trypanosoma cruzi, Toxoplasma gondii and
the liver and blood stages of malaria. Another major strategyanti-
genic variationprotects extracellular protozoa such as African try-
panosomes
2
and Giardia
3
and even malaria parasites
4
, which express
their antigens on the surface of infected erythrocytes, from immune
recognition. In addition, there is abundant evidence that protozoan
infections actively regulate adaptive T cell responses, resulting in sup-
pressed effector functions
1
. A striking example of this phenomenon is
the recent demonstration that Leishmania major actively induces inter-
leukin 10 (IL-10)producing CD25
+
T regulatory cells to prevent com-
plete clearance of the parasite
5
.
Although parasitic protozoa have provided some of the best stud-
ied paradigms of evasion of antibody- and T cellmediated immunity
by pathogens, a series of equally important adaptations occur during
the initial establishment of infection, when parasitic invaders confront
the innate immune system. The innate host defenses that the major
blood and tissue protozoan pathogens of humans must penetrate,
modify or avoid vary according to their mode of entry and the prima-
ry host tissue encountered (Table 1). These innate defenses include
the epithelial barrier of the skin, the alternative complement cascade
and other lytic serum components, lysosomal hydrolases and toxic
oxygen metabolites of mononuclear phagocytes and the antigen-pre-
sentation and immunoregulatory functions of dendritic cells (DCs),
which provide a crucial link with the adaptive immune response
6
.
That protozoa have evolved specific mechanisms to evade these
defenses is dramatically shown by the rapid destruction of preinfec-
tive vector-derived life cycle stages when artificially inoculated into
mammalian hosts. These developmental adaptations, which enable
blood and tissue protozoa to run the gauntlet of the vertebrate
innate response, are the focus of our review.
Evasion of humoral innate defenses
Innate resistance to protozoa is mediated, in part, by pre-existing sol-
uble factors that can potentially recognize and destroy invading para-
sites or target them for killing by effector cells. The alternative path-
way of complement activation provides a first line of defense against
extracellular parasites that must be subverted for infection to proceed.
For example, whereas the epimastigote stage of T. cruzi found in
insect vectors is susceptible to the alternative complement pathway,
infective metacyclic and blood-stream trypomastigotes are resistant
7
.
In this case, evasion of complement appears to be due to trypo-
mastigote expression of a 160-kD glycoprotein (gp160), which is a
homolog of the host complement-regulatory protein decay-accelerat-
ing factor (DAF)
8
. Like DAF, gp160 can bind to C3b and C4b and
inhibit the uptake of subsequent members of the complement cascade,
thus preventing convertase formation and lysis of the parasite.
Importantly, whereas complement-sensitive epimastigotes fail to
express gp160, epimastigotes transfected with gp160 are resistant to
complement-mediated lysis
9
.
Another interesting strategy is deployed by Leishmania species, for
which the infective insect stage is transiently exposed to potentially
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
nature immunology volume 3 no 11 november 2002 www.nature.com/natureimmunology
REVIEW
1042
lethal serum components after inoculation by pool-feeding phle-
botomine vectors. Leishmania evade complement-mediated lysis
while using complement activation as a mechanism for targeting host
cells. When insect-stage procyclic promastigotes develop into infec-
tive metacyclic forms, their membrane is altered to prevent insertion
of the lytic C5b-C9 membrane attack complex (MAC)
10
. This corre-
lates with their expression of a modified surface lipophosphoglycan
(LPG) that is approximately twice as long as the form on procyclic
promastigotes, and which may act as a barrier for insertion of the
MAC into the parasite surface membrane
11
. A further developmental
change that occurs during generation of metacyclics is enhanced syn-
thesis of the surface proteinase gp63, which can cleave C3b to the
inactive iC3b form, thus preventing deposition of the lytic C5b-C9
complex
12
. However, iC3b also opsonizes the parasites for phagocyto-
sis through the complement receptors CR3 and CR1, thereby targeting
the parasite to the macrophage, its host cell of choice
13
. Conclusive
evidence that LPG and gp63 are virulence factors has emerged from
studies with L. major null-mutants that do not express these mole-
cules; in each case these mutants were highly sensitive to complement-
mediated lysis and showed reduced virulence in BALB/c mice
14,15
.
In addition to complement, protozoa must evade other soluble
mediators of innate immunity in order to establish a foothold in the
host. Perhaps the best studied are the primate-specific trypanosome
lysis factors (TLFs)
16
, which contribute to the resistance of humans to
infection with Trypanosoma brucei, an important pathogen of live-
stock. Biochemical analysis of the activity present in human serum
revealed that high-density lipoproteins are part of the substance that
mediates cytolysis of the parasite, and initial studies demonstrated
that this complex, TLF1, is composed of several common apolipopro-
teins as well as a haptoglobin-related protein (Hpr)
17,18
. A second
cytolytic complex, TLF2, has also been identified that shares many of
the components of TLF1 but contains a distinct immunoglobulin M
component and a lower lipid content
19
. Although the final lytic event
has not been delineated, TLF must undergo receptor-mediated uptake
and enter an intracellular acidic compartment for cytotoxicity to
occur
18
. Whereas T. brucei is sensitive to TLF-mediated killing, the
species that infect humansT. brucei gambiense and T. brucei rhode-
sienseare both refractory. This resistance is associated with a block
in TLF endocytosis and retention of the complex in a structure known
as the flagellar pocket
16
. The refractoriness of certain T. brucei rho-
densiese strains to lysis also correlates with the expression of a serum
resistanceassociated (SRA) gene that is equivalent to truncated vari-
ant surface glycoprotein
20
. Importantly, transfection of SRA from T.
brucei rhodesiense into T. brucei confers resistance to lysis by human
serum; this argues that its expression may have been a critical step in
the adaptation of an ancestral parasite for infection of primates
21
.
Interestingly, antibodies raised against a homolog of SRA localize to
the flagellar pocket, suggesting a possible role for the protein in TLF
retention
22
.
Remodeling host-cell compartments
Parasitic protozoa that are adapted to an intracellular lifestyle must
resist the antimicrobial mechanisms that can be induced in phagocytic
and even nonphagoctyic host cells. Insofar as the acidified hydrolytic
environment of host cell lysosomes represents the heart of the defensive
machinery of many nucleated cells, the ability of acid-labile protease-
sensitive parasites to avoid or modify this compartment is likely to be
one key to their survival (Fig. 1). T. gondii resides in a phagosome that
restricts its fusion with host endosomes and lysosomes. Toxoplasma
actively penetrates both phagocytic and nonphagocytic cells, propelled
by an actin-myosindependent gliding motility
23
. In the process, it
establishes a nonfusigenic compartment, called the parasitophorous
vacuole (PV), that lacks integral membrane proteins of host cell origin,
but is extensively modified by secreted parasite proteins
24,25
. This
remodeling seems to be crucial to the inhibition of PV acidification and
lysosome fusion, as these events proceed normally after uptake of dead
or opsonized parasites, which are internalized via classical receptor-
mediated phagocytosis.
T. cruzi trypomastigotes also actively invade mammalian cells but,
unlike T. gondii, their cell entry is dependent not on the propulsive
properties of the parasite, but on their ability to subvert a Ca
2+
-regulat-
ed lysosomal exocytic pathway
23
. The membrane of the para-
sitophorous vacuole is, therefore, derived from the membrane of lyso-
somes, and the vacuole itself remains acidic and potentially fusigenic
with other lysosomes. T. cruzi growth and development cannot be sus-
tained within this compartment; it depends instead on the ability of the
parasite to escape rapidly into the cytosol. Exit from the vacuole is
mediated by a parasite-secreted molecule, Tc-TOX, which has mem-
brane pore-forming activity at acidic pH and is facilitated by a trans-
sialidase present on the trypomastigote surface
26,27
. Interestingly,
T. cruzi is unable to invade cells lacking transforming growth factor-
(TGF-) receptors I or II
28
; this suggests that triggering this signaling
pathway, perhaps by some parasite TNF- homolog, might be needed
to deactivate host cells during the early stages of infection.
Leishmania parasites lack the machinery necessary for active inva-
sion and are confined instead to professional phagocytes, mainly
macrophages, with some exceptions (for example, fibroblasts, DCs and
neutrophils)
29
. The uptake of Leishmania by macrophages proceeds via
conventional receptor-mediated phagocytosis that involves a diversity
of opsonic or pattern-recognition receptors (for example, CR3, CR1
and mannose fucose receptors)
30
that are used depending on the species
and stage of parasite and the presence or absence of fresh serum.
Leishmania metacyclic promastigotes and amastigotes do not seem to
remodel the phagosome in a major way because it rapidly fuses (with-
in 30 min) with late endosomes or lysosomes
31
, generating a para-
sitophorous vacuole that maintains an acidic pH and hydrolytic activi-
ty. Using macrophage cell lines and unselected promastigotes,
researchers have shown that LPG-repeating units can transiently inhib-
it phagosome maturation and that this delay may be necessary to allow
Table 1.The major protozoan pathogens of humans
Parasite Vertebrate host habitat Mode of transmission Primary site of host invasion
Malaria Intracellular (erythrocytes + hepatocytes) Vector-born (mosquitoes) Skin, blood (sporozoites)
Leishmania Intracellular (macrophages) Vector-born (sand flies) Skin
Toxoplasma Intracellular (macrophages, other Ingestion of parasite cysts Intestinal epithelial cells
nucleated cells)
T. cruzi Intracellular (macrophages, muscle cells, Vector-born (reduviid bugs) Skin, conjunctival mucosa
other nucleated cells) and extracellular
African trypanosomes Extracellular Vector-born (tse-tse flies) Blood
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
REVIEW
www.nature.com/natureimmunology november 2002 volume 3 no 11 nature immunology 1043
sufficient time for promastigotes
to differentiate into more hydro-
lase-resistant amastigotes
32,33
.
These findings are consistent with
the attenuation of L. major pro-
mastigote survival within macro-
phages after infection with target-
ed null mutants lacking LPG
14
.
The general significance of the
transient inhibition of phago-
some-endosome fusion has been
questioned, however, for two rea-
sons. First, Leishmania mexicana
promastigote mutants deficient in
LPG or other phosphoglycan-con-
taining molecules survive equally
well as wild-type organisms with-
in macrophages
34
, and second,
there is an absence of direct data
to indicate that mature promastig-
otes are any less hydrolase-resis-
tant than amastigotes. That
amastigotes are remarkably robust
is clear: the parasite does not
escape from the vacuole, but man-
ages to withstand the low pH and
onslaught of acid hydrolases, pre-
sumably by producing an abun-
dance of cell surface and secreted
glyconjugates that protect the cell
from proteolytic damage. As the
L. mexicana phosphoglycandeficient mutants were able to survive
normally, it is likely that this species displays different or redundant
virulence determinants. It is possible, for example, that the huge para-
sitophorous vacuole that is formed after infection with parasites of the
L. mexicana complex might effectively dilute the hydrolases to which
the parasite is exposed within the vacuole and obviate the need for cer-
tain surface or secreted glycans.
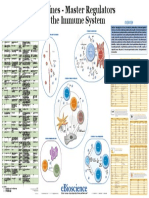
Inhibition of host cell signaling pathways
Macrophages possess primary defense mechanismsincluding activa-
tion of macrophage oxidative metabolism and synthesis and release of
arachidonic acid metabolitesthat are induced by the attachment and
engulfment of microbial agents. The major source of reactive oxygen
intermediates (ROIs) in macrophages is the NADPH oxidase, a multi-
component enzyme that catalyzes the transfer of electrons from
NADPH to molecular oxygen, resulting in the production of superox-
ide and hydrogen peroxide
35
. It is generally believed that activation of
protein kinase C (PKC) and protein tyrosine kinases (PTKs) are the two
critical events involved in regulating phagocyte functions in response to
a variety of extracellular stimuli. In vitro studies involving human cells
have shown that macrophage functions, including phagocytosis and
ROI generation, are severely impaired after uptake of an insoluble
degraded host hemoglobin, called hemozoin, generated during blood-
stage malarial infection
36
(Fig. 2). These dysfunctions were attributed
to inhibition of PKC translocation and activation in the hemozoin-
loaded cells
37
. Early studies suggested that Leishmania parasites also
avoid triggering the oxidative burst by actively inhibiting PKC activa-
tion in macrophages
38,39
. Inhibition of PKC-mediated protein phospho-
rylation was observed with purified LPG
40
, which might act either as
competitive inhibitor of the PKC
activator DAG and/or by altering
the physical properties of the
bilayer to inhibit PKC membrane
translocation. These findings are
again consistent with impaired
intracellular survival of the L.
major LPGdeficient mutant
compared to the mutant in which
LPG expression was restored,
although effects on specific sig-
naling events were not directly
compared
14
.
In addition to their innate
microbicidal responses, macro-
phages can initiate the host acti-
vation cascade by presenting anti-
gens and costimulatory molecules
and by providing regulatory
cytokines to T cells. A number of
studies suggest mechanisms by
which intracellular protozoa can
interfere with the immune-initia-
tion functions of macrophages.
One of the more consistent and
striking dysfunctions observed in
macrophages infected with proto-
zoan parasites is their inability to
produce IL-12, whichas the
main physiological inducer of
interferon- (IFN-) and T helper
type 1 (TH1) cell differentiationis an essential cytokine for the devel-
opment of acquired resistance to most intracellular pathogens. In addi-
tion, excess IL-12 production can lead to severe tissue damage and even
mortality, a consequence that may also be detrimental to the parasite in
blocking its transmission cycle. It is no wonder then that protozoa have
evolved a series of intricate and often redundant mechanisms for regu-
lating IL-12 production by antigen-presenting cells, especially
macrophages, which are the major potential source of the cytokine
stimulated during early infection.
Infectious stages of Leishmania do not merely avoid IL-12 induc-
tion, they actively and selectively inhibit it, leaving other pro-inflam-
matory cytokine or chemokine response pathways relatively intact
41
.
Whereas the glycophosphatidylinositol (GPI) anchors of many para-
sites are potent macrophage activators, Leishmania LPG and gly-
coinositol phospholipid (GIPL) inhibit IL-12p40 transcription while
failing to suppress TNF gene expression
42
. Although the receptors and
signaling pathways involved in this selective inhibition of IL-12 syn-
thesis have yet to be identified, suppression of NF-B activity does not
appear to be involved. Because many IL-12 agonists that are inhibited
in Leishmania-infected macrophagesincluding lipopolysaccharide
(LPS), CD40 ligand (CD40L) and especially IFN-signal primarily
through protein-tyrosine kinases, the observation that Janus kinasesig-
nal transducers and activators of transcription (Jak-STAT) signaling
pathways are also inhibited in Leishmania-infected cells seems espe-
cially relevant to the defective IL-12 response
43
. Defective phosphory-
lation of Jak2 is attributed to rapid activation of a cytoplasmic protein
tyrosine phosphatase (PTP), SHP-1
44
(Fig. 2). SHP-1 is necessary for
L. major survival insofar as SHP-1deficient motheaten mice do not
produce lesions and their macrophages fail to support infection in
Figure 1. Remodeling of macrophage intracellular compartments by
parasitic protozoa. T. cruzi trypomastigotes enter the macrophage by induc-
ing the recruitment of lysosomes to the plasma membrane; they only transient-
ly reside in the parasitophorous vacuole before escape into the cytoplasm via
secretion of a pore-forming molecule, termed Tc-TOX (yellow). T. gondii tachy-
zoites actively invade the cell and remodel a parasitophorous vacuole membrane
(blue) that contains secreted parasite proteins but excludes host proteins that
would normally promote phagosome maturation, thereby preventing lysosome
fusion. Leishmania metacyclic promastigotes are taken up by receptor-mediated
phagocytosis; phagosome maturation may be transiently inhibited by LPG
(green), which becomes incorporated into the phagosome membrane.The repli-
cating amastigote stage ultimately resides within a phagolysosome where they
survive via production of cell-surface and secreted glycoconjugates, including
GIPLS and proteophosphoglycan (PPG) (green).
Phagosome
T. cruzi
trypomastigote
Toxoplasma gondii
tachyzoite
Parasitophorous
vacuoles
Lysosomes
Phagolysosome
Leishmania
promastigote
Leishmania
amastigote
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
nature immunology volume 3 no 11 november 2002 www.nature.com/natureimmunology
REVIEW
1044
vitro
45
. Because specific ligation of the macrophage receptors CR1 and
CR3 also leads to selective inhibition of IL-12 productionwhich, at
least in the case of CR3, is associated with impaired tyrosine phospho-
rylation of STAT1
46
it is likely that host cell PTPs are rapidly induced
by CR3 ligation during attachment and uptake of serum-exposed C3-
opsonized parasites.
Given that Jak-STAT signaling pathways are involved in a broad
range of macrophage responses, including induction of most pro-
inflammatory cytokines, it is difficult to understand how Leishmania
infection maintains such a selective effect on IL-12. One possible
explanation lies in two observations: first, STAT1 regulates IFN con-
sensus-binding protein (ICSBP) induction andof the cytokines
assayedonly activation of the IL-12p40 promoter appears to require
ICSBP, and second, ICSBP knock-out mice (on resistant background)
are susceptible to L. major infection
47
. The involvement of redundant
STAT1-independent induction pathways for tumor necrosis factor-
(TNF-), IL-1 and inducible nitric oxide synthase (iNOS) has been
described (see below) and suggests a basis for the maintenance of these
responses in Leishmania-infected cells. A similar mechanism may
account for the down-regulation of IL-12p40 gene expression in mouse
macrophages after uptake of Plasmodium bergheiinfected erythro-
cytes
48
, which appear to be selective for IL-12 also and do not appear to
be due to impaired NF-B activation.
The NF-B family of transcription factors is an evolutionarily con-
served group of proteins that are important in the regulation of numerous
genes involved in innate and adaptive immunityincluding those encod-
ing IL-12, IFN-, TNF-, iNOS and adhesion moleculesas well as
those involved in cell proliferation and survival. Studies in T. gondii
49,50
have demonstrated the ability of intracellular protozoa to actively interfere
with the NF-Bactivation pathway in macrophages. In T. gondiiinfect-
ed cells, despite rapid IB phosphorylation and degradation, NF-B fails
to translocate to the nucleus. In contrast to Leishmania, T. gondiiinduced
response defects are more generalized and include both IL-12 and TNF-
. With the use of virulent strains of T. gondii, the inhibition of NF-B
translocation in macrophages and its effect on iNOS expression was
shown to be dependent on HS70 expression by the parasite that might
impede nuclear transport by competing for access to nuclear pore com-
plexes
51
. Disrupted nuclear transport of phosphorylated STAT has also
been reported for T. gondiiinfected macrophages and is thought to inhib-
it Jak-STATdependent MHC class II expression
51
(Fig. 2).
In addition to being directly suppressed by the parasite within infect-
ed cells, macrophage IL-12 production and effector functions can also
be held in check by the down-modulatory cytokines IL-10 and TGF-,
which can themselves be up-regulated by the parasites or their prod-
ucts. Striking evidence in support of the importance of IL-10depen-
dent down-regulation of IL-12 production for both host and parasite
comes from studies in IL-10deficient mice infected with either T.
gondii or T. cruzi. These animals display dysregulated IL-12 production
and die of cytokine-associated tissue damage while showing decreased
parasite burdens
52,53
. Similarly, low amounts of active TGF- produc-
tion by splenic mononuclear cells are associated with a lethal outcome
in rodent malaria, and antiTGF- treatment transformed a normally
resolving infection into a lethal one due to overproduction of patho-
genic pro-inflammatory cytokines
54
. With respect to Leishmania, there
is as yet no evidence that deficient production of these anti-inflamma-
tory mediators is responsible for severe clinical outcomes. In contrast,
there is ample evidence to suggest that overproduction of these
cytokines contribute to uncontrolled parasite growth and nonhealing
infections. Both IL-10 and TGF- are produced by murine
macrophages after Leishmania infection in vitro, and both promote
intramacrophage replication and are important factors for determining
in vivo susceptibility
55,56
.
Finally, parasitic protozoa have evolved strategies to down-modulate
signaling pathways leading to host cell apoptosis, thereby prolonging
the life of the host cell and their own intracellular survival
57
. Induced
apoptotic pathways in macrophages infected with either Leishmania
donovani promastigotes
58
or T. gondii tachyzoites
59
were strongly inhib-
ited, perhaps by parasite induced up-regulation of Bcl-2 homologs.
Interestingly, the pro-apoptotic effects that T. cruzi infection has on
both CD4
+
and CD8
+
T cells indirectly enhanced parasite growth, as the
binding of apoptotic lymphocytes to vitronectin receptors on
macrophages triggered TGF- production and a burst of parasite repli-
cation in infected cells
60
.
Manipulation of DC function
To the extent that pathogenic protozoa have learned to condition their
initial encounter with the innate immune system as a means of manip-
ulating the subsequent adaptive immune response, it has been impor-
tant to extend these observations to effects on professional antigen-
presenting cells. In contrast to primary targets of infection, such as
Figure 2. Inhibition of macrophage signaling
pathways. Inhibition of pathways by malaria-gener-
ated hemozoin or infection with Leishmania or T.
gondii. Hemozoin and Leishmania impair the oxidative
burst associated with phagocytosis by inhibiting the
PKC activation required for assembly of the NADPH
oxidase complex in its active form. Leishmania para-
sites also inhibit IFN- or CD40L-induced PTK-
dependent signaling involved in IL-12 production by
activation of the cellular phosphatase SHP-1 that
inhibits Jak2 and STAT1 phosphorylation (P).
Toxoplasma inhibits LPS-induced cytokine responses
by inhibiting nuclear translocation of NF-B and pos-
sibly phosphorylated STAT1.
RhoGDI
SHP1
p67-
phox
p47-
phox
p40-
phox
P
P
P
P
P
STAT
LPS
TLR
Jak Jak
Cytoplasm
Nucleus
Y Y
Y
NF-B
O
2
O
2
Degradation
of IB
Induction of inflammatory and
immune-response genes
cytb558
Cytokine
PKC
CIS
?
Y
Y
STAT
STAT
P P
Y
Y
STAT
STAT
Toxoplasma
Hemozoin
Rac
GDP
Leishmania
IB
MAP
3K
IKK1 IKK2
IRAK IRAK
TRAF6
MyD88
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
REVIEW
www.nature.com/natureimmunology november 2002 volume 3 no 11 nature immunology 1045
macrophages, DCs may be temporally removed from encounter with
parasites or their products and may respond distinctively. For example,
whereas IL-12 production is actively suppressed in macrophages
infected with L. major or T. gondii, DCs actively produce IL-12p40 in
response to the same parasites, both in vitro and in vivo
6165
. It should be
noted that in each case the parasite infection alone was not sufficient for
high IL-12p70 production in vitro and that endogenous agonists, such
as CD40L or IFN-, were necessary as costimuli. The different out-
comes of protozoan encounter on IL-12 production by macrophages
versus DCs is consistent with the delayed, albeit effective, immune
response to these infections that is ultimately achieved. Apart from the
obvious parasite advantage that delayed onset of immunity brings to
bear, suppression of IL-12 production by infected macrophages may
again represent a coadaptation that dampens their local activation while
protecting the host from cytokine shock.
For those parasitic infections associated with T cell control mecha-
nisms that are not simply delayed, but are persistently compromised,
impaired maturation and function of appropriate DC subsets might be
more expected (Table 2). A particularly interesting example is the inhi-
bition of DC maturation by the malaria parasite Plasmodium falci-
parum
66
. Malaria-infected erythrocytes bind to the surface of myeloid
DCs in vitro and markedly suppress the normal up-regulation of major
histocompatibility complex (MHC) class II molecules, adhesion mole-
cules (for example, ICAM-1) and costimulatory molecules (CD83 and
CD86) on the cells after stimulation with LPS. The resulting DCs were
severely impaired in their capacity to induce allogenic as well as anti-
gen-specific primary and secondary T cell responses
67
. The receptors on
the surface of DCs mediating this inhibitory effect are CD36 and CD51,
and their artificial ligation mimicked the suppression induced by infect-
ed erythrocytes
68
. Interestingly, the same receptors are also involved in
the recognition of apoptotic cells and, when incubated with DCs, such
cells trigger reduced secretion of IL-12 and increased production of IL-
10 by these antigen-presenting cells. The major parasite ligand for
CD36 binding in infected erythrocytes is thought to be a conserved
domain of P. falciparum erythrocyte membrane protein 1 (PfEMP1), a
molecule that undergoes antigenic variation. Thus, a nonadherent para-
site line, which does not express PfEMP1 antigens on the red cell sur-
face, failed to inhibit DC maturation.
The relevance of these observations to acute disease is indicated by
the finding that the percentage of HLA-DR
+
DCs was significantly
lower in children with severe or mild malaria compared to healthy con-
trols
68
. At present there is no direct evidence that impaired DC matura-
tion in children with acute malaria is CD36-mediated or that this event
is at all necessary for successful malaria infection. Nevertheless, it is
intriguing that infected erythrocytes with high CD36 binding affinity
are more frequently observed in isolates from patients with mild as
opposed to severe disease
69,70
. It suggests that adhesion of infected ery-
throcytes to CD36 may suppress the pro-inflammatory response to the
parasite, an outcome that would favor both host and parasite.
Infection of monocyte-
derived human DCs with T.
cruzi trypomastigotes also
inhibits LPS-induced secre-
tion of pro-inflammatory
cytokinesincluding IL-12
and TNF-as well as HLA-
DR and CD40 up-regulation
71
.
Similar effects were observed
when human DCs were
exposed to T. cruziderived
GIPL or to only the ceramide portion of the compound
72
, although
nonphysiological high concentrations of both molecules were used in
this in vitro study.
With respect to Leishmania, the spontaneous migration of murine
splenic DCs or Langerhans cells (LCs) was inhibited by L. major pro-
mastigoteconditioned media or L. major LPGs, respectively; this sug-
gested that their ability to transport antigen to or within lymphoid tis-
sue might be impaired during infection
73,74
. These effects need to be
interpreted, however, in the context of other studies (referred to above).
These studies involved infection of murine DCs with viable L. major
promastigotes or amastigotes; the infected cells up-regulated MHC
class II and costimulatory molecules, produced IL-12p40 and down
regulated E-cadherin, which indicated that they were competent for
antigen transport and presentation
61,75
. Uptake of Leishmania amazo-
nensis amastigotes or metacyclic promastigotes by mouse bone mar-
rowderived DCs (BMDCs) also induced up-regulated expression of
MHC class II, CD40, CD80 and CD86 but, in contrast to L. major, the
infected DCs produced IL-4 and no IL-12
76
. This suggested that the
DCs were conditioned by the parasite to prime the pathogenic TH2 cells
that dominate the response in vivo.
Studies involving yet other Leishmania species suggest a more pas-
sive strategy for immune evasion, in which their interactions with anti-
gen-presenting cells appear to proceed in a relatively silent fashion.
Uptake of L. mexicana by mouse BMDCs was not sufficient to activate
them in vitro, although their maturation response to other stimuli was
not impaired
77
. A similar species restriction in Leishmania-induced DC
activation was observed after uptake of metacyclic promastigotes by
human myeloid DCs, which were efficiently primed for CD40L-
induced ILp70 secretion by L. major, but not by L. tropica or L. dono-
vani
78
. These observations may be significant because whereas L. major
produces self-limiting infections that are controlled in the skin, the
other species mentioned are capable of disseminating to the viscera or
to other cutaneous sites. Given the well described polymorphisms in the
surface and secreted glycan structures that are expressed by different
Leishmania species
79
, it will be interesting to determine whether they
accountat least in partfor the differences in innate response pat-
terns and the spectrum of clinical disease.
From the above discussion it would appear that parasites carefully
regulate the induction of IL-12 from DCs during early infection as a
means of determining the character of the adaptive immune response
that eventually decides their fate in the host. In addition, there is emerg-
ing evidence for the existence of distinct parasite-triggered pathways
for regulating DC IL-12 production once it has been initiated. One such
mechanism has been identified by studies of IL-12 synthesis by murine
splenic DCs after injection of a soluble extract of T. gondii tachyzoites
(STAg). The response was short-lived and could not be recalled by a
second injection of STAg for a period of 1 week after initial priming
80
.
This paralysis of the DC IL-12 response induced by STAg does not
require IL-10 but instead appears to depend on the induction of lipoxin
Table 2. Impairment of DC function by parasitic protozoa
Parasite Inhibitory signal Immunologic effects
Leishmania Live infection (L. amazonensis) Inhibition of DC IL-12 production with turn on of IL-4
76
Parasite culture media or LPG Inhibition of DC or LC migration
73,74
T. cruzi Live infection GIPL (or ceramide portion) Suppression of LPS-induced IL-12, TNF-, HLA-DR and
CD40 expression in human DCs
71,72
T. gondii Parasite induction of host LXA4 in vivo Inhibition of CCR5-dependent IL-12 production by DCs
80,81
P. falciparum Ligation of CD36 (or CD51) by parasitized Suppression of DC maturation and function
67,68
erythrocytes
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
nature immunology volume 3 no 11 november 2002 www.nature.com/natureimmunology
REVIEW
1046
A4 (LXA4), a product of arachadonic metabolism
81
. This eicosonoid
appears to function by suppressing CCR5 expression, a chemokine
receptor involved in IL-12 stimulation by STAg. The same mechanism
of IL-12 suppression is likely to operate during natural infection
because T. gondiiinfected mice with a defect in an enzyme (5-LO)
required for LXA4 show excess IL-12 production and, in common with
infected IL-10deficient mice
53
, succumb to cytokine shock and show
decreased parasite burdens (J. Aliberti et al., unpublished data). Taken
together, these findings suggest that once IL-12 production by DCs has
been induced and TH1 responses initiated, synthesis of the cytokine is
actively down-regulated, probably to the joint benefit of both host and
parasite. Whether analogous mechanisms suppress the IL-12 responses
of DCs to other protozoa remains to be determined.
Concluding comments
In learning to evade innate host defenses, protozoan parasites appear to
have mastered the intricacies of both cell biology and cellular
immunology. As such, they can teach us important lessons about both
fields of biology as well as their points of intersection. In particular, the
strategies used by these pathogens for remodeling cellular compart-
ments offer insights into the dynamics of host membranes and intracel-
lular trafficking. At the same time there is much to be learned about
host-signaling pathways and immune-response initiation and polariza-
tion by studying the mechanisms used by protozoa to suppress or divert
immune responses. Because innate defenses (for example, lysis by
complement or TLF) have the potential to block infection, the mecha-
nisms used to evade them are potential Achilles heels, and offer
newly identified and largely unexploited targets for vaccine and/or
pharmacologic intervention.
1. Pearce, E. J., Scott, P. A. & Sher, A. in Fundamental immunology (ed. Paul, W.) 12711294 (Lippincott-
Raven, Philadelphia, 1999).
2. Borst, P. et al. Antigenic variation in trypanosomes. Arch. Med. Res. 27, 379388 (1996).
3. Nash, T. E. Surface antigenic variation in Giardia lamblia. Mol. Microbiol. 45, 585590 (2002).
4. Kyes, S., Horrocks, P. & Newbold, C. Antigenic variation at the infected red cell surface in malaria.
Annu. Rev. Microbiol. 55, 673707 (2001).
5. Belkaid,Y. et al. The role of interleukin (IL)-10 in the persistence of Leishmania major in the skin after
healing and the therapeutic potential of anti-IL-10 receptor antibody for sterile cure. J. Exp. Med.
194, 1497506 (2001).
6. Hunter, C. & Sher, A. in Immunology of Infectious Diseases (eds. Kaufman, S., Sher, A. & Ahmed, R.)
111126 (ASM Press, Washington DC, 2001).
7. Joiner, K. A. Complement evasion by bacteria and parasites. Annu. Rev. Microbiol. 42, 201230 (1988).
8. Norris, K. A., Bradt, B., Cooper, N. R. & So, M. Characterization of a Trypanosoma cruzi C3 binding
protein with functional and genetic similarities to the human complement regulatory protein, decay-
accelerating factor. J. Immunol. 147, 22402247 (1991).
9. Norris, K. A. Stable transfection of Trypanosoma cruzi epimastigotes with the trypomastigote-specif-
ic complement regulatory protein cDNA confers complement resistance. Infect. Immun. 66,
24602465 (1998).
10. Puentes, S. M., Da Silva, R. P., Sacks, D. L., Hammer, C. H. & Joiner, K. A. Serum resistance of meta-
cyclic stage Leishmania major promastigotes is due to release of C5b-9. J. Immunol. 145,
43114316 (1990).
11. McConville, M. J., Turco, S. J., Ferguson, M. A. & Sacks, D. L. Developmental modification of lipophos-
phoglycan during the differentiation of Leishmania major promastigotes to an infectious stage. EMBO
J. 11, 35933600 (1992).
12. Brittingham, A. et al. Role of the Leishmania surface protease gp63 in complement fixation, cell adhe-
sion, and resistance to complement-mediated lysis. J. Immunol. 155, 31023111 (1995).
13. Mosser, D. M. & Edelson, P. J. The mouse macrophage receptor for C3bi (CR3) is a major mechanism
in the phagocytosis of Leishmania promastigotes. J. Immunol. 135, 27852789 (1985).
14. Spath, G. F. et al. Lipophosphoglycan is a virulence factor distinct from related glycoconjugates in the
protozoan parasite Leishmania major. Proc. Natl. Acad. Sci. USA 97, 92589263 (2000).
15. Joshi, P. B., Kelly, B. L., Kamhawi, S., Sacks, D. L. & McMaster, W. R. Targeted gene deletion in Leishmania
major identifies leishmanolysin (GP63) as a virulence factor. Mol. Biochem. Parasitol. 120, 3340 (2002).
16. Raper, J., Portela, M. P., Lugli, E., Frevert, U. & Tomlinson, S. Trypanosome lytic factors: novel mediators
of human innate immunity. Curr. Opin. Microbiol. 4, 402408 (2001).
17. Hajduk, S. L. et al. Lysis of Trypanosoma brucei by a toxic subspecies of human high density lipopro-
tein. J. Biol. Chem. 264, 52105217 (1989).
18. Smith, A. B., Esko, J. D. & Hajduk, S. L. Killing of trypanosomes by the human haptoglobin-related pro-
tein. Science 268, 284286 (1995).
19. Raper, J., Fung, R., Ghiso, J., Nussenzweig,V. & Tomlinson, S. Characterization of a novel trypanosome
lytic factor from human serum. Infect. Immun. 67, 19101916 (1999).
20. De Greef, C. & Hamers, R. The serum resistance-associated (SRA) gene of Trypanosoma brucei rhode-
siense encodes a variant surface glycoprotein-like protein. Mol. Biochem. Parasitol. 68, 277284 (1994).
21. Xong, H.V. et al. A VSG expression site-associated gene confers resistance to human serum in
Trypanosoma rhodesiense. Cell 95, 839846 (1998).
22. Milner, J. D. & Hajduk, S. L. Expression and localization of serum resistance associated protein in
Trypanosoma brucei rhodesiense. Mol. Biochem. Parasitol. 104, 271283 (1999).
23. Sibley, L. D. & Andrews, N. W. Cell invasion by un-palatable parasites. Traffic 1, 100106 (2000).
24. Mordue, D. G., Desai, N., Dustin, M. & Sibley, L. D. Invasion by Toxoplasma gondii establishes a moving
junction that selectively excludes host cell plasma membrane proteins on the basis of their mem-
brane anchoring. J. Exp. Med. 190, 17831792 (1999).
25. Lingelbach, K. & Joiner, K. A. The parasitophorous vacuole membrane surrounding Plasmodium and
Toxoplasma: an unusual compartment in infected cells. J. Cell Sci. 111, 14671475 (1998).
26. Andrews, N. W., Abrams, C. K., Slatin, S. L. & Griffiths, G. A T. cruzi-secreted protein immunologically
related to the complement component C9: evidence for membrane poreforming activity at low
pH. Cell 61, 12771287 (1990).
27. Hall, B. F., Webster, P., Ma, A. K., Joiner, K. A. & Andrews, N. W. Desialylation of lysosomal membrane
glycoproteins by Trypanosoma cruzi: a role for the surface neuraminidase in facilitating parasite entry
into the host cell cytoplasm. J. Exp. Med. 176, 313325 (1992).
28. Ming, M., Ewen, M. E. & Pereira, M. E. Trypanosome invasion of mammalian cells requires activation of
the TGF- signaling pathway. Cell 82, 287296 (1995).
29. Rittig, M. G. & Bogdan, C. Leishmania-host-cell interaction: complexities and alternative views.
Parasitol.Today 16, 292297 (2000).
30. Alexander, J. & Russell, D. G. The interaction of Leishmania species with macrophages. Adv. Parasitol.
31, 175254 (1992).
31. Courret, N. et al. Biogenesis of Leishmania-harbouring parasitophorous vacuoles following phagocy-
tosis of the metacyclic promastigote or amastigote stages of the parasites. J. Cell Sci. 115,
23032316 (2002).
32. Desjardins, M. & Descoteaux, A. Inhibition of phagolysosomal biogenesis by the Leishmania lipophos-
phoglycan. J. Exp. Med. 185, 20612068 (1997).
33. Dermine, J. F., Scianimanico, S., Prive, C., Descoteaux, A. & Desjardins, M. Leishmania promastigotes
require lipophosphoglycan to actively modulate the fusion properties of phagosomes at an early
step of phagocytosis. Cell Microbiol. 2, 115126 (2000).
34. Ilg, T., Demar, M. & Harbecke, D. Phosphoglycan repeat-deficient Leishmania mexicana parasites
remain infectious to macrophages and mice. J. Biol. Chem. 276, 49884997 (2001).
35. Nathan, C. & Shiloh, M. U. Reactive oxygen and nitrogen intermediates in the relationship between
mammalian hosts and microbial pathogens. Proc. Natl. Acad. Sci. USA 97, 88418848 (2000).
36. Schwarzer, E. et al. Impairment of macrophage functions after ingestion of Plasmodium falciparum-
infected erythrocytes or isolated malarial pigment. J. Exp. Med. 176, 10331041 (1992).
37. Schwarzer, E., Turrini, F., Giribaldi, G., Cappadoro, M. & Arese, P. Phagocytosis of P. falciparum malarial
pigment hemozoin by human monocytes inactivates monocyte protein kinase C. Biochim. Biophys.
Acta 1181, 5154 (1993).
38. Moore, K. J., Labrecque, S. & Matlashewski, G. Alteration of Leishmania donovani infection levels by
selective impairment of macrophage signal transduction. J. Immunol. 150, 44574465 (1993).
39. Olivier, M., Brownsey, R. W. & Reiner, N. E. Defective stimulus-response coupling in human mono-
cytes infected with Leishmania donovani is associated with altered activation and translocation of
protein kinase C. Proc. Natl. Acad. Sci. USA 89, 74817485 (1992).
40. Descoteaux, A., Matlashewski, G. & Turco, S. J. Inhibition of macrophage protein kinase C-mediated pro-
tein phosphorylation by Leishmania donovani lipophosphoglycan. J. Immunol. 149, 30083015 (1992).
41. McDowell, M. A. & Sacks, D. L. Inhibition of host cell signal transduction by Leishmania: observations
relevant to the selective impairment of IL-12 responses. Curr. Opin. Microbiol. 2, 438443 (1999).
42. Piedrafita, D. et al. Regulation of macrophage IL-12 synthesis by Leishmania phosphoglycans. Eur. J.
Immunol. 29, 235244 (1999).
43. Nandan, D. & Reiner, N. E. Attenuation of interferon-induced tyrosine phosphorylation in mononu-
clear phagocytes infected with Leishmania donovani: selective inhibition of signaling through Janus
kinases and Stat1. Infect. Immun. 63, 44954500 (1995).
44. Blanchette, J., Racette, N., Faure, R., Siminovitch, K. A. & Olivier, M. Leishmania-induced increases in
activation of macrophage SHP-1 tyrosine phosphatase are associated with impaired IFN--triggered
Jak2 activation. Eur J. Immunol. 29, 37373744 (1999).
45. Forget, G. et al. Role of host phosphotyrosine phosphatase SHP-1 in the development of murine
Leishmaniasis. Eur. J. Immunol. 31, 31853196 (2001).
46. Marth, T. & Kelsall, B. L. Regulation of interleukin-12 by complement receptor 3 signaling. J. Exp. Med.
185, 19871995 (1997).
47. Giese, N. A. et al. Interferon (IFN) consensus sequence-binding protein, a transcription factor of the
IFN regulatory factor family, regulates immune responses in vivo through control of interleukin 12
expression. J. Exp. Med. 186, 15351546 (1997).
48. Xu, X. et al. Down-regulation of IL-12 p40 gene in Plasmodium berghei-infected mice. J. Immunol. 167,
235241 (2001).
49. Butcher, B. A., Kim, L., Johnson, P. F. & Denkers, E.Y. Toxoplasma gondii tachyzoites inhibit proinflam-
matory cytokine induction in infected macrophages by preventing nuclear translocation of the tran-
scription factor NF-B. J. Immunol. 167, 21932201 (2001).
50. Shapira, S., Speirs, K., Gerstein, A., Caamano, J. & Hunter, C. A. Suppression of NF-B activation by
infection with Toxoplasma gondii. J. Infect. Dis. 185 (Suppl.) 6672 (2002).
51. Dobbin, A., Smith, N. C. & Jonson, A. M. Heat shock protein 70 is a potential virulence factor in
murine Toxoplasma infection via immunomodulation of host NF-B and nitric oxide. J. Immunol. 169,
958965 (2002).
52. Neyer, L. E. et al. Role of interleukin-10 in regulation of T-cell-dependent and T-cell- independent
mechanisms of resistance to Toxoplasma gondii. Infect. Immun. 65, 16751682 (1997).
53. Gazzinelli, R. T. et al. In the absence of endogenous IL-10, mice acutely infected with Toxoplasma
gondii succumb to a lethal immune response dependent on CD4
+
T cells and accompanied by over-
production of IL-12, IFN- and TNF-. J. Immunol. 157, 798805 (1996).
54. Omer, F. M., Kurtzhals, J. A. & Riley, E. M. Maintaining the immunological balance in parasitic infections:
a role for TGF-? Parasitol.Today 16, 1823 (2000).
55. Kane, M. M. & Mosser, D. M. The role of IL-10 in promoting disease progression in Leishmaniasis.
J. Immunol. 166, 11411147 (2001).
56. Barral, A. et al. Transforming growth factor as a virulence mechanism for Leishmania braziliensis.
Proc. Natl. Acad. Sci. USA 90, 34423446 (1993).
57. Luder, C. G., Gross, U. & Lopes, M. F. Intracellular protozoan parasites and apoptosis: diverse strate-
gies to modulate parasite-host interactions. Trends Parasitol. 17, 480486 (2001).
58. Moore, K. J., Turco, S. J. & Matlashewski, G. Leishmania donovani infection enhances macrophage viabili-
ty in the absence of exogenous growth factor. J. Leukoc. Biol. 55, 9198 (1994).
59. Nash, P. B. et al. Toxoplasma gondii-infected cells are resistant to multiple inducers of apoptosis.
J. Immunol. 160, 18241830 (1998).
60. Freire-de-Lima, C. G. et al. Uptake of apoptotic cells drives the growth of a pathogenic trypanosome
in macrophages. Nature 403, 199203 (2000).
61. von Stebut, E., Belkaid,Y., Jakob, T., Sacks, D. L. & Udey, M. C. Uptake of Leishmania major amastigotes
results in activation and interleukin 12 release from murine skin-derived dendritic cells: implications
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
REVIEW
www.nature.com/natureimmunology november 2002 volume 3 no 11 nature immunology 1047
for the initiation of anti-Leishmania immunity. J. Exp. Med. 188, 15471552 (1998).
62. Marovich, M. A., McDowell, M. A., Thomas, E. K. & Nutman, T. B. IL-12p70 production by Leishmania
major-harboring human dendritic cells is a CD40/CD40 ligand-dependent process. J. Immunol. 164,
58585865 (2000).
63. Gorak, P. M., Engwerda, C. R. & Kaye, P. M. Dendritic cells, but not macrophages, produce IL-12
immediately following Leishmania donovani infection. Eur. J. Immunol. 28, 687695 (1998).
64. Subauste, C. S. & Wessendarp, M. Human dendritic cells discriminate between viable and killed
Toxoplasma gondii tachyzoites: dendritic cell activation after infection with viable parasites results in
CD28 and CD40 ligand signaling that controls IL-12-dependent and -independent T cell production
of IFN-. J. Immunol. 165, 1498505 (2000).
65. Scanga, C. A. et al. Cutting edge: MyD88 is required for resistance to Toxoplasma gondii infection and
regulates parasite-induced IL-12 production by dendritic cells. J. Immunol. 168, 59976001 (2002).
66. Urban, B. C. & Roberts, D. J. Malaria, monocytes, macrophages and myeloid dendritic cells: sticking of
infected erythrocytes switches off host cells. Curr. Opin. Immunol. 14, 458465 (2002).
67. Urban, B. C. et al. Plasmodium falciparum-infected erythrocytes modulate the maturation of dendritic
cells. Nature 400, 7377 (1999).
68. Urban, B. C., Willcox, N. & Roberts, D. J. A role for CD36 in the regulation of dendritic cell function.
Proc. Natl. Acad. Sci. USA 98, 87508755 (2001).
69. Newbold, C. et al. Receptor-specific adhesion and clinical disease in Plasmodium falciparum. Am. J.Trop.
Med. Hyg. 57, 389398 (1997).
70. Rogerson, S. J. et al. Cytoadherence characteristics of Plasmodium falciparum-infected erythro-
cytes from Malawian children with severe and uncomplicated malaria. Am. J. Trop. Med. Hyg. 61,
467472 (1999).
71. Van Overtvelt, L. et al. Trypanosoma cruzi infects human dendritic cells and prevents their maturation:
inhibition of cytokines, HLA-DR, and costimulatory molecules. Infect. Immun. 67, 40334040 (1999).
72. Brodskyn, C. et al. Glycoinositolphospholipids from Trypanosoma cruzi interfere with macrophages
and dendritic cell responses. Infect. Immun. 70, 37363743 (2002).
73. Jebbari, H., Stagg, A. J., Davidson, R. N. & Knight, S. C. Leishmania major promastigotes inhibit dendritic
cell motility in vitro. Infect. Immun. 70, 10231026 (2002).
74. Ponte-Sucre, A., Heise, D. & Moll, H. Leishmania major lipophosphoglycan modulates the phenotype
and inhibits migration of murine Langerhans cells. Immunology 104, 462467 (2001).
75. Konecny, P. et al. Murine dendritic cells internalize Leishmania major promastigotes, produce IL-12
p40 and stimulate primary T cell proliferation in vitro. Eur. J. Immunol. 29, 18031811 (1999).
76. Qi, H., Popov,V. & Soong, L. Leishmania amazonensis-dendritic cell interactions in vitro and the priming
of parasite-specific CD4
+
T cells in vivo. J. Immunol. 167, 45344542 (2001).
77. Bennett, C. L., Misslitz, A., Colledge, L., Aebischer, T. & Blackburn, C. C. Silent infection of bone mar-
row-derived dendritic cells by Leishmania mexicana amastigotes. Eur. J. Immunol. 31, 876883 (2001).
78. McDowell, M. A., Marovich, M., Lira, R., Braun, M. & Sacks, D. Leishmania priming of human dendritic
cells for CD40 ligand-induced interleukin-12p70 secretion is strain and species dependent. Infect.
Immun. 70, 39944001 (2002).
79. Turco, S. J., Spath, G. F. & Beverley, S. M. Is lipophosphoglycan a virulence factor? A surprising diversity
between Leishmania species. Trends Parasitol. 17, 223226 (2001).
80. Reis e Sousa, C. et al. Paralysis of dendritic cell IL-12 production by microbial products prevents
infection-induced immunopathology. Immunity 11, 637647 (1999).
81. Aliberti, J., Hieny, S., Reis e Sousa, C., Serhan, C. N. & Sher, A. Lipoxin-mediated inhibition of IL-12 pro-
duction by DCs: a mechanism for regulation of microbial immunity. Nature Immunol. 3, 7682 (2002).
2
0
0
2
N
a
t
u
r
e
P
u
b
l
i
s
h
i
n
g
G
r
o
u
p
h
t
t
p
:
/
/
w
w
w
.
n
a
t
u
r
e
.
c
o
m
/
n
a
t
u
r
e
i
m
m
u
n
o
l
o
g
y
Potrebbero piacerti anche
- Cellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsDa EverandCellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsCharles G. CochraneNessuna valutazione finora
- Immunologyoffungal Infections: Oscar A. Fernández-García,, Jennifer M. Cuellar-RodríguezDocumento16 pagineImmunologyoffungal Infections: Oscar A. Fernández-García,, Jennifer M. Cuellar-RodríguezsilviaNessuna valutazione finora
- Immunity To ParasitesDocumento6 pagineImmunity To ParasitesDarren WilliamNessuna valutazione finora
- Complement System Part II: Role in ImmunityDocumento26 pagineComplement System Part II: Role in ImmunityAnca LunguNessuna valutazione finora
- Malaria Immunology 71Documento7 pagineMalaria Immunology 71Firda DamiruNessuna valutazione finora
- Immunity To Parasitic Infections 3Documento33 pagineImmunity To Parasitic Infections 3Fikadu AberaNessuna valutazione finora
- Jir2018 6529681Documento6 pagineJir2018 6529681Herry JapariNessuna valutazione finora
- Entamoeba Histolytica: Review ArticleDocumento11 pagineEntamoeba Histolytica: Review ArticleDian IslamiatiNessuna valutazione finora
- Immunity To Fungi: Tobias M Hohl, Amariliz Rivera and Eric G PamerDocumento8 pagineImmunity To Fungi: Tobias M Hohl, Amariliz Rivera and Eric G PamerPieralessandro LasalviaNessuna valutazione finora
- Chronic Bacterial Infections: Living With Unwanted Guests: Douglas Young, Tracy Hussell and Gordon DouganDocumento7 pagineChronic Bacterial Infections: Living With Unwanted Guests: Douglas Young, Tracy Hussell and Gordon DouganMarcus ViníciusNessuna valutazione finora
- Human Genetic Resistance To MalariaDocumento15 pagineHuman Genetic Resistance To MalariaLink BuiNessuna valutazione finora
- Role of Phagocytic Cells in Periodontal HealthDocumento49 pagineRole of Phagocytic Cells in Periodontal HealthDrKrishna DasNessuna valutazione finora
- How Can Immunology Contribute To The Control of Tuberculosis?Documento11 pagineHow Can Immunology Contribute To The Control of Tuberculosis?Parijat BanerjeeNessuna valutazione finora
- Evasion InmuneDocumento8 pagineEvasion Inmunenydiacastillom2268Nessuna valutazione finora
- Cytokine Profiling of Macrophages Exposed To Porphyromonas Gingivalis, Its Lipopolysaccharide, or Its Fima ProteinDocumento10 pagineCytokine Profiling of Macrophages Exposed To Porphyromonas Gingivalis, Its Lipopolysaccharide, or Its Fima Proteinapi-26071302Nessuna valutazione finora
- Cimid 2015 AjayDocumento7 pagineCimid 2015 AjayprashantcdriNessuna valutazione finora
- 8 - Imunologi InfeksiDocumento30 pagine8 - Imunologi InfeksiNurfitri Rahmani AwaliyahNessuna valutazione finora
- Antimicrobial ActionDocumento26 pagineAntimicrobial ActionAnne CabreraNessuna valutazione finora
- Ijeb 47 (6) 412-423Documento12 pagineIjeb 47 (6) 412-423Daniela MartinezNessuna valutazione finora
- Pyroptosis: A Caspase-1-Dependent Programmed Cell Death and A Barrier To InfectionDocumento21 paginePyroptosis: A Caspase-1-Dependent Programmed Cell Death and A Barrier To Infectionrovia achmad .Nessuna valutazione finora
- Microbioma y OtorrinoDocumento19 pagineMicrobioma y Otorrinodayenu barraNessuna valutazione finora
- Immune Responses To Human Papillomavirus: Margaret StanleyDocumento7 pagineImmune Responses To Human Papillomavirus: Margaret StanleyDina A. ŠabićNessuna valutazione finora
- Toll-Like Receptors As Key Mediators in Innate Antifungal ImmunityDocumento14 pagineToll-Like Receptors As Key Mediators in Innate Antifungal ImmunityKlaus Ramirez SuarezNessuna valutazione finora
- Gmbar ImunDocumento10 pagineGmbar ImunVera FitrianaNessuna valutazione finora
- Zii2043 PDFDocumento10 pagineZii2043 PDFPablo VelazquezNessuna valutazione finora
- Chronic Granulomatous Disease A Review of Infectious and Inflamatory Complications PDFDocumento14 pagineChronic Granulomatous Disease A Review of Infectious and Inflamatory Complications PDFYesenia Huerta100% (1)
- Interactions of Fungal Pathogens With Phagocytes: Lars P. Erwig and Neil A. R. GowDocumento14 pagineInteractions of Fungal Pathogens With Phagocytes: Lars P. Erwig and Neil A. R. GowPatrícia KellenNessuna valutazione finora
- Molecular Mechanisms Used by Salmonella To Evade The Immune SystemDocumento35 pagineMolecular Mechanisms Used by Salmonella To Evade The Immune SystemANDREA FERNANDA MUÑOZ NARVAEZNessuna valutazione finora
- 120 Paper DRAFTDocumento8 pagine120 Paper DRAFTSher LiquidoNessuna valutazione finora
- Panniculitis: Adipose Tissue and ImmunityDocumento7 paginePanniculitis: Adipose Tissue and ImmunityAnnisa Chaerani BurhanuddinNessuna valutazione finora
- Host Immune Response To Chlamydia InfectionDocumento17 pagineHost Immune Response To Chlamydia Infectionapi-266835840Nessuna valutazione finora
- Aspergillus Fumigatus Triggers Inflammatory Response in Stage Specific Beta Glucan DisplayDocumento9 pagineAspergillus Fumigatus Triggers Inflammatory Response in Stage Specific Beta Glucan Displaymumu_sukiNessuna valutazione finora
- MICR3001 Past Exams (2015 Discussion)Documento30 pagineMICR3001 Past Exams (2015 Discussion)ekampreetNessuna valutazione finora
- Helminth Infections - Recognition and Modulation of The Immune Response by Innate Immune CellsDocumento12 pagineHelminth Infections - Recognition and Modulation of The Immune Response by Innate Immune CellsponbohacopNessuna valutazione finora
- Paper Fiebre ReumDocumento10 paginePaper Fiebre ReumSara OchoaNessuna valutazione finora
- Review Article: Host Cell Signalling and Mechanisms of EvasionDocumento15 pagineReview Article: Host Cell Signalling and Mechanisms of EvasionParijat BanerjeeNessuna valutazione finora
- How Insects Combat InfectionsDocumento12 pagineHow Insects Combat InfectionsJonathan MoralesNessuna valutazione finora
- CMSA Medical PG Entrance Coaching Institute: CM SADocumento13 pagineCMSA Medical PG Entrance Coaching Institute: CM SAAmarjeet KaurNessuna valutazione finora
- Aspectos InmunologicosDocumento11 pagineAspectos InmunologicosjafralizNessuna valutazione finora
- Host Defence Mechanisms Against TumorsDocumento7 pagineHost Defence Mechanisms Against TumorsHamam AmastrdamNessuna valutazione finora
- Chapter 2 and 3 ImmunologyDocumento16 pagineChapter 2 and 3 ImmunologyRevathyNessuna valutazione finora
- Excerpts From Kuby ImmunologyDocumento2 pagineExcerpts From Kuby ImmunologyDavid Saguil100% (1)
- Macrophage Subsets Exhibit Distinct E. coli-LPS Tolerisable Cytokines Associated With The Negative Regulators, IRAK-M and TollipDocumento19 pagineMacrophage Subsets Exhibit Distinct E. coli-LPS Tolerisable Cytokines Associated With The Negative Regulators, IRAK-M and TollipFaeGiNNessuna valutazione finora
- Breaking Down BiofilmsDocumento3 pagineBreaking Down Biofilmsleila.hiloutNessuna valutazione finora
- 1 s2.0 S0021925820870148 MainDocumento11 pagine1 s2.0 S0021925820870148 MainAina SarahNessuna valutazione finora
- Level of Cytokines in Patients With Pulmonary Drug Susceptible and Resistant TuberculosisDocumento6 pagineLevel of Cytokines in Patients With Pulmonary Drug Susceptible and Resistant TuberculosispetrescumarinNessuna valutazione finora
- Basophils As Antigen Presenting Cells: Mohan S. Maddur, Srini V. Kaveri and Jagadeesh BayryDocumento4 pagineBasophils As Antigen Presenting Cells: Mohan S. Maddur, Srini V. Kaveri and Jagadeesh BayryJuan RodriguezNessuna valutazione finora
- Camp Signalling in Trypanosomatids: Role in Pathogenesis and As A Drug TargetDocumento7 pagineCamp Signalling in Trypanosomatids: Role in Pathogenesis and As A Drug TargetCamilo Ernesto Araujo BarabasNessuna valutazione finora
- Streptococcus Pyogenes and Streptococcal Disease (Page 1) : © Kenneth Todar, PHDDocumento16 pagineStreptococcus Pyogenes and Streptococcal Disease (Page 1) : © Kenneth Todar, PHDRiska PashaNessuna valutazione finora
- Jun Zou, Nathan ShankarDocumento11 pagineJun Zou, Nathan ShankarHQ HQNessuna valutazione finora
- Zii 3122Documento10 pagineZii 3122Muhammad Ricky RamadhianNessuna valutazione finora
- Mannheimia Haemolytica A N D Pasteurella Multocida in BovinerespiratorydiseaseDocumento16 pagineMannheimia Haemolytica A N D Pasteurella Multocida in BovinerespiratorydiseaseFREDY GUTIERREZNessuna valutazione finora
- Immune Activation in Sepsis 2018 Critical Care ClinicsDocumento14 pagineImmune Activation in Sepsis 2018 Critical Care ClinicsgiseladlrNessuna valutazione finora
- Immune System and Immunology: German VersionDocumento68 pagineImmune System and Immunology: German VersionKhushbuNessuna valutazione finora
- Entamoeba Histolytica Under Oxidative Stress: What Countermeasure Mechanisms Are in Place?Documento14 pagineEntamoeba Histolytica Under Oxidative Stress: What Countermeasure Mechanisms Are in Place?aulia hanin fakhiraNessuna valutazione finora
- Streptococcus Group A InfectionsDocumento13 pagineStreptococcus Group A InfectionsLidia GotoYourhappyplaceNessuna valutazione finora
- Describe The Transmission Routes For Bacteria.: 1. A. B. C. D. 2. A. B. C. D. eDocumento2 pagineDescribe The Transmission Routes For Bacteria.: 1. A. B. C. D. 2. A. B. C. D. ekep1313Nessuna valutazione finora
- Basic ImmunologyDocumento9 pagineBasic Immunologyarsyiadlina100% (1)
- Finlay & Mcfadden 2006 Anti-ImmunologyDocumento16 pagineFinlay & Mcfadden 2006 Anti-ImmunologyMaria Sofia del BosqueNessuna valutazione finora
- Chikungunya Viral Infections An Emerging ProblemDocumento6 pagineChikungunya Viral Infections An Emerging ProblemMike zombieNessuna valutazione finora
- Mechanisms Ofcancerdrug ResistanceDocumento15 pagineMechanisms Ofcancerdrug ResistanceMike zombieNessuna valutazione finora
- Juno Is The Egg Izumo Receptor and IsDocumento16 pagineJuno Is The Egg Izumo Receptor and IsMike zombieNessuna valutazione finora
- Antibody Drug ConjugatesDocumento6 pagineAntibody Drug ConjugatesMike zombieNessuna valutazione finora
- Antibodies: Immunoglobulins - A Family of ProteinsDocumento21 pagineAntibodies: Immunoglobulins - A Family of ProteinsMike zombieNessuna valutazione finora
- Antibodies: Immunoglobulins - A Family of ProteinsDocumento21 pagineAntibodies: Immunoglobulins - A Family of ProteinsMike zombieNessuna valutazione finora
- Enterobius GregoriiDocumento4 pagineEnterobius GregoriiMike zombieNessuna valutazione finora
- Microbiology Question Bank-1Documento40 pagineMicrobiology Question Bank-1Abd El-Rahman SalahNessuna valutazione finora
- 151 - Effects of Exercise On Immuine Function - Gleeson 2015Documento6 pagine151 - Effects of Exercise On Immuine Function - Gleeson 2015Rahil PatelNessuna valutazione finora
- First French-Argentine Immunology Congress, 2010 Abstracts Held On Buenos Aires, Argentina, 2nd-5th November, 2010Documento105 pagineFirst French-Argentine Immunology Congress, 2010 Abstracts Held On Buenos Aires, Argentina, 2nd-5th November, 2010International Medical PublisherNessuna valutazione finora
- The Use of Phyllanthus Niruri L As An ImmunomodulaDocumento10 pagineThe Use of Phyllanthus Niruri L As An ImmunomodulaMuhammad Arif MahfudinNessuna valutazione finora
- Chapter 28 PROMDocumento24 pagineChapter 28 PROMTansya PurnaningrumNessuna valutazione finora
- Role of Immune Cells in Obesity Induced Low Grade Inflammation and Insulin ResistanceDocumento9 pagineRole of Immune Cells in Obesity Induced Low Grade Inflammation and Insulin ResistanceThamyres CristhinaNessuna valutazione finora
- Etiology and Pathogenesis of Preeclampsia: Current Concepts: Ajog ReviewsDocumento17 pagineEtiology and Pathogenesis of Preeclampsia: Current Concepts: Ajog ReviewstapayanaNessuna valutazione finora
- Pathology Book - Chapter 2 - Inflammation - HKDocumento12 paginePathology Book - Chapter 2 - Inflammation - HKagar agarNessuna valutazione finora
- Journal Pmed 1001125 s005Documento71 pagineJournal Pmed 1001125 s005Arhi WidhiaNessuna valutazione finora
- The Role of Diet in Multiple Sclerosis - A ReviewDocumento16 pagineThe Role of Diet in Multiple Sclerosis - A ReviewHabib G. Moutran BarrosoNessuna valutazione finora
- Clinical Applications and Pharmacological Resea - 2021 - Journal of TraditionalDocumento9 pagineClinical Applications and Pharmacological Resea - 2021 - Journal of Traditionalayarin heNessuna valutazione finora
- Non-Analgesic Effects of OpioidsDocumento9 pagineNon-Analgesic Effects of OpioidsFrancisco MirettiNessuna valutazione finora
- InterleukinDocumento10 pagineInterleukinKhristy AbrielleNessuna valutazione finora
- The Inmuen Response To Surgery and TraumaDocumento8 pagineThe Inmuen Response To Surgery and TraumaCorin Boice TelloNessuna valutazione finora
- Immune Recap 2Documento8 pagineImmune Recap 2ibrahimNessuna valutazione finora
- Caselli Et Al. - 2013 - Actual Concept of Probiotics Is It More Functional To Science or Business PDFDocumento14 pagineCaselli Et Al. - 2013 - Actual Concept of Probiotics Is It More Functional To Science or Business PDFДжулиан Родригес РуисNessuna valutazione finora
- Cytokines BluesDocumento15 pagineCytokines BluesantonioNessuna valutazione finora
- 1 Il-10 ElisaDocumento15 pagine1 Il-10 ElisaYousra ZeidanNessuna valutazione finora
- Inflammatory Mechanisms in Hidradenitis SuppurativaDocumento8 pagineInflammatory Mechanisms in Hidradenitis SuppurativaIsmailNessuna valutazione finora
- Cannabinoid-Based Drugs As Anti-Inflammatory TherapeuticsDocumento12 pagineCannabinoid-Based Drugs As Anti-Inflammatory TherapeuticsAldo BustamanteNessuna valutazione finora
- Insight and Control of Infectious Disease in Global Scenario - P. Roy (Intech, 2012) WWDocumento454 pagineInsight and Control of Infectious Disease in Global Scenario - P. Roy (Intech, 2012) WWgoutham sivasailamNessuna valutazione finora
- Immune Responses in NeonatesDocumento26 pagineImmune Responses in NeonatesCony GSNessuna valutazione finora
- Immunologic Pathomechanism of Hodgkin's Lymphoma: ReviewDocumento10 pagineImmunologic Pathomechanism of Hodgkin's Lymphoma: ReviewPaola Alexandra Chavez FNessuna valutazione finora
- Presepsin 6Documento189 paginePresepsin 6donkeyendutNessuna valutazione finora
- The Hyperferritinemic Syndrome: Macrophage Activation Syndrome, Still 'S Disease, Septic Shock and Catastrophic Antiphospholipid SyndromeDocumento11 pagineThe Hyperferritinemic Syndrome: Macrophage Activation Syndrome, Still 'S Disease, Septic Shock and Catastrophic Antiphospholipid SyndromeLUCIENE CRISTALDO ALBUQUERQUENessuna valutazione finora
- Alteration of Host Cell Behavior by PathogensDocumento7 pagineAlteration of Host Cell Behavior by PathogensAbhijit SatpatiNessuna valutazione finora
- Overview of The Pathogenesis of SLEDocumento8 pagineOverview of The Pathogenesis of SLEferifhransNessuna valutazione finora
- Cytokines 1 PDFDocumento1 paginaCytokines 1 PDFzalmezeydNessuna valutazione finora
- MacrófagoDocumento10 pagineMacrófagoFabro BianNessuna valutazione finora
- Male Qbank PDFDocumento126 pagineMale Qbank PDFgabby_54everNessuna valutazione finora