Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Routine Birth Canal Exam Reduces Postpartum Hemorrhage
Caricato da
Yeli AstiDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Routine Birth Canal Exam Reduces Postpartum Hemorrhage
Caricato da
Yeli AstiCopyright:
Formati disponibili
1176 Edington: Examination
of
Birth Canal
Canad. Med. Ass. J. June 22 and 29, 1968, vol. 98
Routine Examination of the Birth Canal
R. F. EDINGTON,
not
a
Following Delivery
ab
are on
M.D., F.R.C.S.[C], Sudbury, Ont. jaws, twisted gently and removed. Any normality of the uterine cavity is noted, as
uterine or adnexal tumours. An assistant presses down the posterior vaginal wall is
routine manual exploration of the reproTHE ductive tract following delivery is pro cedure that is
generally taught or practised.1, 2 The fear of thereby introducing infection and causing an increase in maternal morbidity is well ingrained, and the benefits which result from such an examination of the uterine cavity and vagina are not generally realized. Hemorrhage still ranks in the forefront as a cause of maternal deaths. It is responsible for 29.8% of these tragedies in the United States.3
In Ontario, between 1958 and 1961, 33% of all direct obstetrical deaths were due to hemor rhage; if deaths from rupture of the uterus were included, over half (52%) occurred in the post
partum period.4
undertakes to show that there is no increase in morbidity attributable to the procedure, which reduces to a minimum both early and delayed postpartum hemorrhage. In addition, the ex amination may reveal hitherto unsuspected pelvic conditions. The 1050 patients reported are those personally delivered by the author between 1959 and 1966. The technique is simple, requires no special instruments and needs no scrubbed assistant. Anesthesia is not a pre-
walls, can prevent a considerable number of postpartum hemorrhages. This paper describes the technique used for this examination, and
Routine manual exploration of the uterine in the immediate postpartum period, followed by visual and manual examination of the cervix, the fornices and the lateral vaginal
cavity
the fundus, and depressed with the examiner's left hand, while the cervix is grasped with the sponge forceps. The whole circumfer ence of the cervix is systematically examined, and any lacerations are then repaired. The assistant then dips the fingers down be hind the patient's symphysis pubis and elevates the uterine body cephalad, thus opening up and tenting the vaginal fornices. The light is adjusted and any blood in the vagina is re moved with swabs. The lateral and posterior fornices are examined, as well as the areas over the bladder and over the ischial spines. The apex of the episiotomy is located and a suture suitably placed to begin the episiorrhaphy.
patients is reported, 68% of whom were delivered under conduction or in halation anesthesia. Twenty-nine per cent of the patients were delivered using a combination of pudendal block or local inflltration of the perineum with anesthetic solution and trichlorethylene (Trilene) by Duke inhaler. Three per cent of the patients had no anesthesia for
Results A total of 1050
delivery.
requisite.
Technique
Immediately after delivery of the placenta and before repair of the episiotomy, the hands are rinsed in sterile solution in the splash basin, and the vulva, perineal and perirectal areas are swabbed with wet sponges. The drapes are not into the changed. The cupped hand is inserted other cervix. The the and hand, through vagina on the patient's abdomen, steadies the uterus and pushes it gently down towards the examin ing hand. The uterine cavity is systematically examined and the placental site identified. Any retained placental fragments are removed manually and any membranes are grasped with a straight sponge-holding forceps with serrated
to: Dr. R. F. Edington, 60 Drinkwater Reprint requests Ontario. Street, Sudbury,
of membrane. During the course of study number of other conditions were detected by this examination (Table I). The occurrence of miscellaneous conditions that were discovered by this method at the time of delivery was quite surprising, and as the physician becomes more skilled in the technique of intrauterine examination, fibroids and uterine anomalies previously unsuspected may also be detected. In the two cases of fibroids, the tumours were present in the posterior uterine wall and could not have been palpated by routine abdominal examination. In both cases the fibroids became very much smaller and after six weeks were hardly palpable. Two ovarian cysts were found, one of which disappeared by
nants
a
Abnormalities Detected by Manual Exploration At first the main reason for the routine exploration of the uterine cavity was to confirm that the uterus was empty of placenta or rem-
Canad. Med. Ass. J. June 22 and 29, 1968, vol. 98
Edington: Examination
by
of
Birth Canal 1177
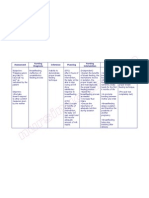
TABLE I..Abnormalities Detected Manual Exploration 1. Unsuspected cervical laceration over 2.5
cm.
46 2. Retained membrane. (4.4%) 3. Vaginal lacerations (including episiotomy 42 (4.0%) extension). 4. Retained placental tissue. 16 (1.5%) 5. Bicornuate uterus. 5 (0.5%) 2 6. Fibroids. (0.2%) 2 7. Ovarian cyst. (0.2%) 8. Vaginal cyst. 1 (0.1%)
69(6.6%)
lead to increased postpartum morbidity, and this conclusion is also evident in other series of cases.1618
Discussion The routine exploration of the uterus is not taught in many medical schools or residency training programs. The main objection to this
the second month post partum; the other per sisted and at operation proved to be a 5-cm.
serous
cystadenoma. Repair of all cervical lacerations, including those not bleeding actively, leads to healthier cervices and to fewer delayed cervical complica tions of delivery. Of the cervical lacerations de tected in the series, 64% were associated with spontaneous or outlet forceps delivery. Therefore it is not necessarily the difficult deliveries that are associated with cervical trauma. In a series of cases quoted by Danforth,15 large tears occurred in non-traumatic deliveries and the incidence of lacerations over 3 cm. in length was 11.2% in primiparas and 4.1% in multiparas. Bleeding does not always occur from cervical lacerations, and some surprisingly deep tears, measuring up to 4 cm. in extent, may be present without due blood loss, especially when located posteriorly.
These asymptomatic cervical lacerations are overlooked unless routine examination of the cervix is practised. The whole of the cervix should be examined, bringing it into view by traction with sponge forceps. Only by doing this will these asymptomatic cervical lacerations be seen. Vaginal lacerations including episiotomy extensions were found in 42 patients and were these lacerations were not repaired. Some of and if the vagina had not bleeding actively, been examined they would have been missed.
Morbidity
procedure has been the high morbidity rate quoted in cases of manual removal of the placenta.57 In these reports, maternal mortality rates of 2.7% and maternal morbidity rates of 43.1% were not uncommon. However, the cases quoted are those in which manual removal of the placenta and invasion of the uterus was per formed after considerable blood loss and procrastination. Thus, the intrauterine manipulation was a last resort in an already traumatized patient. The distinction between manual re moval of the placenta, performed of necessity for postpartum hemorrhage, and the routine postpartum exploration of the uterine cavity in a stabilized patient who is not bleeding is certainly an important one, and mortality and morbidity rates cannot be compared. Recent series of cases of manual removal of the placenta reported by Hoffman,8 Thomas9 and Sauer10 show no maternal mortality and a morbidity rate equal to that of the respective service as a whole. At the beginning of the study considerable difficulty was encountered in differentiating the normal from the abnormal. The collapsed post partum uterine cavity is longitudinally rugose with a rough placental area that may lead the
unwary to think that there are retained secundines. The lower uterine segment is
Morbidity was defined as a temperature eleva F., occurring on any two of the first 10 days post partum exclusive of the first 24 hours. By this definition, 24 patients were
tion of 100.4
2.3%. Of these 24 patients, there
uncorrected incidence of were 14 with for the causes morbidity, 6 due to genital and 8 due to endometritis. infection episiotomy There were extragenital causes in 10 patients: 3 had upper respiratory infection, 5 had genitourinary infection and 2 developed thrombophlebitis. Thus, genital causes for the morbidity occurred in only 1.4% of all the pa tients examined. This low figure would seem to demonstrate that manual exploration did not
considered morbid,
an
flaccid and easily traumatized, and the junction of this with the upper segment is quite abrupt, leading the examiner to believe that there is a definite contraction ring. Intrauterine blood clots give the sensation of placental cotyledons until they are removed and examined. It is con sidered, therefore, that planned exploration of the birth canal done electively and in the nonemergent cases gives the examiner confidence in the detection of those abnormalities that are potentially dangerous in the emergency case. In the series of cases here reported 24 pa tients were morbid, a gross rate of 2.3%. How ever, some of these patients had extragenital causes for their morbidity, such as upper respira tory or genitourinary infection. Comparison of this series with those of other authors (Table II) shows that in non-traumatized stabilized pa tients the morbidity rate is certainly not high, and if the corrected figure is taken, the genital
1178 EDINGTON: EXAMINATION
OF
BmRTH CANAL
Med. Ass. J. Canad. June 22 and 29. 1968, vol. 98
TABLE II.-COMPARISON OF MORBIDITY
Author
Year 1966 1965
Number of patients 1050 1000 921 3022
Gross
2.5
-
Corrected
1.5 1.6 1.2 0.26
Jones et al. 17 ............... Thomasg ..................
Edington......
Mozley'2
1960
1957
2.4
-
..................
membranes were removed successfully without recourse to inhalation anesthesia. That this procedure is possible with minimal analgesia is also borne out by Doolittle's report16 of 1000 cases delivered using pudendal block
anesthesia, supplemented with predelivery meperidine and scopolamine. In some of these cases even manual removal of the placenta was accomplished without added anesthesia.
A personal series is presented of 1050 Summary patients who had routine intrauterine
metritis
1955 Hawkins" ................. DuCkman and Dennen'9..... 1955 Hoffman8 .................. 1954 1954 Briscoe18 .................. 1269 83 977 500 2.5 2.7 2.25
1.9
-
(Endoonly)
0.4
1.12
1.0
infection rate is low. The lack of morbidity in both this small series of patients and in larger series't' 12 would seem to overrule the main objection to incorporating this technique in the method of delivery. Examination of the uterine cavity with removal of retained placental remnants and membranes which otherwise would have been left behind reduces postpartum hemorrhage and postpartum morbidity with fever, uterine tenderness and foul lochia. The secondary anemia and dangers of multiple blood transfusions that can be a consequence of postpartum hemorrhage are thus avoided. In Ontario in 1963, 20 out of 39 direct obstetrical deaths were due to hemorrhage. Included in these 20 maternal mortality reports were five cases due to uterine rupture, and not one of these cases was recognized even though the patient was bleeding briskly. A study of maternal mortality reports'3' 14 in The Canadian Medical Association Journal brings to notice a disquieting number of cases due to postpartum hemorrhage. These include cases of undiagnosed vaginal lacerations, rupture of the uterus and extensive cervical tears. The majority of these cases either were not examined adequately or were examined after serious blood loss had rendered the patient a poor risk for any type of surgical intervention. Whether this failure to carry out a proper examination of the whole birth canal was due to ignorance of the procedure or to fear of producing infection it is impossible to say. However, if the reluctance to perform this type of examination can be dispelled, perhaps maternal deaths due to undiagnosed uterine rupture and vaginal lacerations will gradually cease. The fact that general or regional anesthesia is not necessary for this procedure is borne out by the fact that 32% of the patients received either trichloroethylene inhalation analgesia by Duke inhaler or no analgesia at all. In this group, routine manual exploration of the genital tract was carried out without incident, and on several occasions small placental remnants and
and vaginal canal examination performed immediately post partum. Adoption of this technique as a part of delivery room procedure is suggested. From this series of cases it would appear that when performed carefully this examination carries no undue danger to the patient. The general morbidity rate is not increased, and valuable information about the patient's uterus, cervix and vagina can be gained. Causes of postpartum hemorrhage can be diagnosed rapidly and simply, so that prompt treatment can be lifesaving, while future gynecological complications may be prevented.
L'auteur passe en revue 1050 accouchements qu'il a pratiques lui-meme. Chacune des parturientes a ete soumise a un examen approfondi de la filiere pelvienne immediatement apres la delivrance. Cet examen n'a entraine aucune augmentation de la morbidite au cours du postpartum mais a eu l'avantage de pouvoir deceler des lacerations cervicales et vaginales chez plus de 10% des femmes. La retention de debris placentaires a ete egalement notee chez 9.9% des accouchees. D'autres anomalies ont ete egalement constatees. L'auteur est grand partisan d'un examen approfondi de la filiere pelvienne apres l'accouchement et considere qu'il doit etre partie integrante de tout accouchement.
Re'sume
R m
1955. 12. MOZLEY, P. D.: Ibid., 75: 1126, 1958. 13. Canadian Medical Association, Committee on Maternal Welfare: Canad. Med. Ass. J., 94: 1314, 1966. 14. Idem: Ibid., 95: 219, 1966. 15. DANFORTH, W. C.: Amer. J. Obstet. Gynec., 32: 710, 1936. 16. DOOLITTLE, H. H.: Obstet. Gynec., 9: 422, 1957. 17. JONES, R. F.. WARREN, B. L., JR. AND THORNTON, W. N., JR.: Ibid., 27: 699, 1966. 18. BRISCOE, C. C.: Ibid., 4: 375, 1954. 19. DUCKMAN, S. AND DENNEN, P.: Ibid., 5: 628, 1955.
REFERENCES 1. LULL, C. B. AND KIMBROUGH, R. A., editors: Clinical obstetrics, J. B. Lippincott Co., Philadelphia, 1953, p. 472. 2. DELEE, J. B. AND GREENHILL, J. P.: Principles and practice of obstetrics. 9th ed., W. B. Saunders Company, Philadelphia, 1947, p. 278. 3. EASTMAN, N. J. AND HELLMAN, L. M.: Williams obstetrics, 12th ed., Appleton-Century-Crofts Inc., New York, 1961. 4. ALLEMANG, W. H.: Clin. Obstet. Gynec., 6: 825, 1963. 5. SCHWARTZ, H. A. AND RIcHARDS, W. R.: Amer. J. Obstet. Gynec., 45: 235, 1943. 6. PECKHAM, C. H.: Bull. Hopkins Hosp., 56: 224, 1935. 7. ODEL, L. D. AND HoVIs, W. F.: Surg. Gynec. Obstet., 77: 553, 1943. 8. HOFFMAN, R. L.: Amer. J. Obstet. Gynec., 68: 645, 1954. 9. THOMAS, W. O., JR.: Ibid., 86: 600, 1963. 10. SAUER, H. H. A.: Obstet. Gynec., 12: 221, 1958. 11. HAWKINS, R. J.: Amer. J. Obstet. Gynec., 69: 1094,
Potrebbero piacerti anche
- A Case Study About AbortionDocumento10 pagineA Case Study About AbortionPatricia JerusalemNessuna valutazione finora
- Sex ManualDocumento14 pagineSex ManualCally LiueNessuna valutazione finora
- Benign Gynecologic Lesions: Urethral Caruncle, Cyst, Nevus, Hemangioma, Fibroma, Lipoma, Endometriosis, Urethral DiverticulumDocumento158 pagineBenign Gynecologic Lesions: Urethral Caruncle, Cyst, Nevus, Hemangioma, Fibroma, Lipoma, Endometriosis, Urethral DiverticulumArianne Joy C. TamarayNessuna valutazione finora
- Ectopic PregnancyDocumento14 pagineEctopic PregnancytaufiqNessuna valutazione finora
- Premature Rupture of MembranesDocumento4 paginePremature Rupture of MembranesNikko Pabico67% (3)
- Maternity Nursing ReviewDocumento8 pagineMaternity Nursing ReviewJulienne Sanchez-Salazar100% (2)
- Nursing Care Plan Breast Feeding IneffectiveDocumento1 paginaNursing Care Plan Breast Feeding Ineffectivederic88% (8)
- Period Power by Maisie HillDocumento11 paginePeriod Power by Maisie HillsimasNessuna valutazione finora
- Grade 10 Science Quarter 3 WEEK 4 I.: Menstrual-CycleDocumento3 pagineGrade 10 Science Quarter 3 WEEK 4 I.: Menstrual-CycleAnn ClarisseNessuna valutazione finora
- HEICSDocumento36 pagineHEICSYeli Asti100% (1)
- Managing Placenta Accreta: Medical vs Surgical OptionsDocumento9 pagineManaging Placenta Accreta: Medical vs Surgical OptionsAslesa Wangpathi PagehgiriNessuna valutazione finora
- Obstetrics Mcqs PDFDocumento2 pagineObstetrics Mcqs PDFJennifer47% (17)
- Uterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewDocumento6 pagineUterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewBOHR International Journal on GynaecologyNessuna valutazione finora
- The Back Alley Revisited: Sepsis After Attempted Self-Induced AbortionDocumento3 pagineThe Back Alley Revisited: Sepsis After Attempted Self-Induced Abortionmila nurmalaNessuna valutazione finora
- Case Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaeDocumento4 pagineCase Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaemelisaberlianNessuna valutazione finora
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Documento3 paginePlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolNessuna valutazione finora
- Ultrasound Study of Ovarian Cysts in Pregnancy Prevalence and SignificanceDocumento4 pagineUltrasound Study of Ovarian Cysts in Pregnancy Prevalence and SignificanceDavid Eka PrasetyaNessuna valutazione finora
- Medicine: Intrauterine Device Found in An Ovarian TumorDocumento5 pagineMedicine: Intrauterine Device Found in An Ovarian TumorRezky amalia basirNessuna valutazione finora
- Acute Non-Puerperal Uterine Inversion Case ReportDocumento4 pagineAcute Non-Puerperal Uterine Inversion Case ReportALfuNessuna valutazione finora
- Cases Journal: Torsion of Ovarian Cyst During Pregnancy: A Case ReportDocumento3 pagineCases Journal: Torsion of Ovarian Cyst During Pregnancy: A Case ReportAde Gustina SiahaanNessuna valutazione finora
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDocumento6 pagineUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioNessuna valutazione finora
- Cesarean Scar Ectopic Pregnancy Case ReportDocumento6 pagineCesarean Scar Ectopic Pregnancy Case ReportMominah MayamNessuna valutazione finora
- 2 5 21 861 PDFDocumento3 pagine2 5 21 861 PDFAhmed ZidanNessuna valutazione finora
- Pregnancy in a Didelphic Uterus- A case ReportDocumento7 paginePregnancy in a Didelphic Uterus- A case ReportAmin BashyrNessuna valutazione finora
- Nir Hus Absite Review Q12Documento11 pagineNir Hus Absite Review Q12nir4846Nessuna valutazione finora
- Laparoscopic Management of Cervical-Isthmic Pregnancy: A Proposal MethodDocumento4 pagineLaparoscopic Management of Cervical-Isthmic Pregnancy: A Proposal MethodDinorah MarcelaNessuna valutazione finora
- 9.radha Et Al.Documento3 pagine9.radha Et Al.International Journal of Clinical and Biomedical Research (IJCBR)Nessuna valutazione finora
- Blighted Ovum: A Case ReportDocumento2 pagineBlighted Ovum: A Case Reportakhmad ikhwanNessuna valutazione finora
- Rectovaginal Fistulae: Bidhan Das, MD Michael Snyder, MDDocumento7 pagineRectovaginal Fistulae: Bidhan Das, MD Michael Snyder, MDNovaNessuna valutazione finora
- Ectopic PregnancyDocumento7 pagineEctopic PregnancyDeepshikha MahapatraNessuna valutazione finora
- Abnormal PlacentationDocumento9 pagineAbnormal PlacentationJack BladeNessuna valutazione finora
- Uterine Rupture at 21 Weeks in Twin Pregnancy WithDocumento5 pagineUterine Rupture at 21 Weeks in Twin Pregnancy WithGatoso OsoNessuna valutazione finora
- Laparoscopic Management of Rudimentary Uterine Horn Pregnancy: Case Report and Literature ReviewDocumento4 pagineLaparoscopic Management of Rudimentary Uterine Horn Pregnancy: Case Report and Literature ReviewCamacho OmarNessuna valutazione finora
- Ovarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014Documento4 pagineOvarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014alif bagusNessuna valutazione finora
- Ruptured Ectopic Pregnancy in The Presence of An Intrauterine DeviceDocumento5 pagineRuptured Ectopic Pregnancy in The Presence of An Intrauterine DevicePatrick NunsioNessuna valutazione finora
- Uterine Adherence To Anterior Abdominal Wall After Caesarean SectionDocumento3 pagineUterine Adherence To Anterior Abdominal Wall After Caesarean SectionGladstone AsadNessuna valutazione finora
- Primary Umbilical Endometriosis. Case Report and Discussion On Management OptionsDocumento7 paginePrimary Umbilical Endometriosis. Case Report and Discussion On Management Optionsari naNessuna valutazione finora
- MainDocumento4 pagineMainselvia oktavianiNessuna valutazione finora
- Abrasio PlacentaDocumento3 pagineAbrasio Placentamuhammad azamNessuna valutazione finora
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDocumento3 pagineGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelNessuna valutazione finora
- Hematometra in Uterus Didelphys With Right Hemivagina and Right Renal AgenesisDocumento3 pagineHematometra in Uterus Didelphys With Right Hemivagina and Right Renal AgenesisDexter BluesNessuna valutazione finora
- Bilateral Tubo-Ovarian Abscess After Cesarean Delivery: A Case Report and Literature ReviewDocumento4 pagineBilateral Tubo-Ovarian Abscess After Cesarean Delivery: A Case Report and Literature ReviewIntan PermataNessuna valutazione finora
- 03 JCR 004 Rajendra EndometrialDocumento4 pagine03 JCR 004 Rajendra EndometrialReza HidayatNessuna valutazione finora
- Suspected Illegal Abortion and Unsafe Abortion Leading To Uterine RuptureDocumento4 pagineSuspected Illegal Abortion and Unsafe Abortion Leading To Uterine Ruptureoke boskuNessuna valutazione finora
- Vaginal Extrusion of A Ventriculoperitoneal Shunt A Case Report and Review ofDocumento10 pagineVaginal Extrusion of A Ventriculoperitoneal Shunt A Case Report and Review ofDian AdiNessuna valutazione finora
- Primary Ovarian Abscess in Pregnancy: Case ReportDocumento3 paginePrimary Ovarian Abscess in Pregnancy: Case ReportVinnyRevinaAdrianiNessuna valutazione finora
- Ectopic Pregnancy22Documento43 pagineEctopic Pregnancy22Sunil YadavNessuna valutazione finora
- Cesarean SectionDocumento139 pagineCesarean SectionMisganaw WorkuNessuna valutazione finora
- Ectopic PregenancyDocumento69 pagineEctopic PregenancyMahmoud AbbasNessuna valutazione finora
- Spontaneous Rupture of An Unscarred GravidDocumento4 pagineSpontaneous Rupture of An Unscarred GraviddelaNessuna valutazione finora
- Khing Journal...Documento5 pagineKhing Journal...Khing AbatNessuna valutazione finora
- A. Tunica Albuguinea: NCM 102: Assessment ExamDocumento9 pagineA. Tunica Albuguinea: NCM 102: Assessment ExamdubhieNessuna valutazione finora
- Primary Carcinoma of Fallopian Tube: Case Series Case ReportDocumento4 paginePrimary Carcinoma of Fallopian Tube: Case Series Case ReportChi NgôNessuna valutazione finora
- acute polihidramnios wong1986Documento4 pagineacute polihidramnios wong1986Francisco MirettiNessuna valutazione finora
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDocumento4 pagineAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiNessuna valutazione finora
- Case Report: Retained Intrauterine Device (IUD) : Triple Case Report and Review of The LiteratureDocumento9 pagineCase Report: Retained Intrauterine Device (IUD) : Triple Case Report and Review of The LiteratureYosie Yulanda PutraNessuna valutazione finora
- Term Live Primary Ovarian Pregnancy A Case ReportDocumento4 pagineTerm Live Primary Ovarian Pregnancy A Case ReportNico PlantadoNessuna valutazione finora
- Clinical Medicine Insights: Case ReportsDocumento4 pagineClinical Medicine Insights: Case ReportsJer KelNessuna valutazione finora
- MainDocumento3 pagineMaindivyanshu kumarNessuna valutazione finora
- Kista OvariumDocumento4 pagineKista OvariumAde Gustina SiahaanNessuna valutazione finora
- مرجع 2Documento4 pagineمرجع 2Ahmed AnwarNessuna valutazione finora
- A Case Report: Twisted Ovarian Cyst in PregnancyDocumento3 pagineA Case Report: Twisted Ovarian Cyst in PregnancyPHitphitt Jeleck SangaattNessuna valutazione finora
- Criog2014 108973Documento4 pagineCriog2014 108973Denia Haritsa AprilianiNessuna valutazione finora
- Article IJGCP 118Documento3 pagineArticle IJGCP 118Jessica MarianoNessuna valutazione finora
- Rare Uterine Leiomyoma in Adolescent FemaleDocumento3 pagineRare Uterine Leiomyoma in Adolescent Femaledr.putra888Nessuna valutazione finora
- Case Study-Endometrial PyometraDocumento7 pagineCase Study-Endometrial Pyometrasimbarashe tangwadzanaNessuna valutazione finora
- Spontaneous Perforated Pyometra With An Intrauterine Device in Menopause: A Case ReportDocumento2 pagineSpontaneous Perforated Pyometra With An Intrauterine Device in Menopause: A Case ReportTomy SaputraNessuna valutazione finora
- Uterine Myoma, Myomectomy and Minimally Invasive TreatmentsDa EverandUterine Myoma, Myomectomy and Minimally Invasive TreatmentsNessuna valutazione finora
- Damage Control in Trauma Care: An Evolving Comprehensive Team ApproachDa EverandDamage Control in Trauma Care: An Evolving Comprehensive Team ApproachJuan DuchesneNessuna valutazione finora
- Ni Hms 288677Documento15 pagineNi Hms 288677Yeli AstiNessuna valutazione finora
- Risk Factors Associated With Facial FracturesDocumento7 pagineRisk Factors Associated With Facial FracturesYeli AstiNessuna valutazione finora
- Canmedaj01175 0030Documento3 pagineCanmedaj01175 0030Yeli AstiNessuna valutazione finora
- Reliabel Sikap 1Documento3 pagineReliabel Sikap 1Yeli AstiNessuna valutazione finora
- Obsgyn BooksDocumento4 pagineObsgyn BooksYulian NuswantoroNessuna valutazione finora
- Pustaka CannabisDocumento2 paginePustaka CannabisYeli AstiNessuna valutazione finora
- Molluscum Contagiosum Treatment OptionsDocumento12 pagineMolluscum Contagiosum Treatment OptionsShivani JainNessuna valutazione finora
- Obsgyn BooksDocumento4 pagineObsgyn BooksYulian NuswantoroNessuna valutazione finora
- PDF HM5 Adolescents HealthDocumento68 paginePDF HM5 Adolescents HealthYeli AstiNessuna valutazione finora
- Obsgyn BooksDocumento4 pagineObsgyn BooksYulian NuswantoroNessuna valutazione finora
- NIH Public Access: Author ManuscriptDocumento13 pagineNIH Public Access: Author ManuscriptYeli AstiNessuna valutazione finora
- Tetanus BagusDocumento11 pagineTetanus BagusArief Yudho PrabowoNessuna valutazione finora
- Risk Factors For and Prevention of Human Papillomaviruses (HPV), Genital Warts and Cervical CancerDocumento9 pagineRisk Factors For and Prevention of Human Papillomaviruses (HPV), Genital Warts and Cervical CancerYeli AstiNessuna valutazione finora
- Validitas Sikap 1Documento4 pagineValiditas Sikap 1Yeli AstiNessuna valutazione finora
- Book 2Documento7 pagineBook 2Yeli AstiNessuna valutazione finora
- Dietary Consumption of Antioxidant Nutrients and Risk of Incident Cervical Intraepithelial NeoplasiaDocumento9 pagineDietary Consumption of Antioxidant Nutrients and Risk of Incident Cervical Intraepithelial NeoplasiaYeli AstiNessuna valutazione finora
- Dietary Consumption of Antioxidant Nutrients and Risk of Incident Cervical Intraepithelial NeoplasiaDocumento9 pagineDietary Consumption of Antioxidant Nutrients and Risk of Incident Cervical Intraepithelial NeoplasiaYeli AstiNessuna valutazione finora
- Tetanus BagusDocumento11 pagineTetanus BagusArief Yudho PrabowoNessuna valutazione finora
- Kanker ServiksDocumento16 pagineKanker ServiksYeli AstiNessuna valutazione finora
- Viaviliappendix1.Php FIGODocumento3 pagineViaviliappendix1.Php FIGOYeli AstiNessuna valutazione finora
- Hospital Preparedness For Emergency ResponseDocumento15 pagineHospital Preparedness For Emergency ResponseYeli AstiNessuna valutazione finora
- Hvi 8 355Documento8 pagineHvi 8 355Yeli AstiNessuna valutazione finora
- BMC Neurology: Autonomic Nervous System Dysfunction Predicts Poor Prognosis in Patients With Mild To Moderate TetanusDocumento4 pagineBMC Neurology: Autonomic Nervous System Dysfunction Predicts Poor Prognosis in Patients With Mild To Moderate TetanusYeli AstiNessuna valutazione finora
- Antioxidants in Cervical Cancer Chemopreventive and Chemotherapeutic Effects of PolyphenolsDocumento11 pagineAntioxidants in Cervical Cancer Chemopreventive and Chemotherapeutic Effects of PolyphenolsYeli AstiNessuna valutazione finora
- Tetanus BagusDocumento11 pagineTetanus BagusArief Yudho PrabowoNessuna valutazione finora
- Reproductive Morbidity Among Iranian Women Issues Often Inappropriately Addressed in Health Seeking BehaviorsDocumento8 pagineReproductive Morbidity Among Iranian Women Issues Often Inappropriately Addressed in Health Seeking BehaviorsYeli AstiNessuna valutazione finora
- Reproductive Morbidity Among Iranian Women Issues Often Inappropriately Addressed in Health Seeking BehaviorsDocumento8 pagineReproductive Morbidity Among Iranian Women Issues Often Inappropriately Addressed in Health Seeking BehaviorsYeli AstiNessuna valutazione finora
- BMC Neurology: Autonomic Nervous System Dysfunction Predicts Poor Prognosis in Patients With Mild To Moderate TetanusDocumento4 pagineBMC Neurology: Autonomic Nervous System Dysfunction Predicts Poor Prognosis in Patients With Mild To Moderate TetanusYeli AstiNessuna valutazione finora
- Sen, Gita y Östlin. Gender Inequity in Health, Why It Exists and How We Can Change It. 2008Documento14 pagineSen, Gita y Östlin. Gender Inequity in Health, Why It Exists and How We Can Change It. 2008Diana Paola Valencia CamachoNessuna valutazione finora
- Assessment Nursing Diagnosis Rationale Expected Outcome Nursing Interventions Rationale EvaluationDocumento1 paginaAssessment Nursing Diagnosis Rationale Expected Outcome Nursing Interventions Rationale EvaluationMark FernandezNessuna valutazione finora
- OBSTETRICS Enhancement - FINAL COPY 1Documento17 pagineOBSTETRICS Enhancement - FINAL COPY 1Jan Joseph BanzuelaNessuna valutazione finora
- Chlamydia TrachomatisDocumento7 pagineChlamydia TrachomatisDewi SetiawatiNessuna valutazione finora
- Case Study For Uterine-CancerDocumento9 pagineCase Study For Uterine-CancerGabbii CincoNessuna valutazione finora
- Malpresentations: Liji Raichel Kurian Dept of OBGDocumento41 pagineMalpresentations: Liji Raichel Kurian Dept of OBGliji raichel kurian100% (1)
- Opd SheetDocumento1 paginaOpd SheetTwingkol Just TwingkolNessuna valutazione finora
- Presentation-WPS OfficeDocumento47 paginePresentation-WPS OfficeJeffrey JasarenoNessuna valutazione finora
- Episiotomy Case and Postpartum HemorrhageDocumento2 pagineEpisiotomy Case and Postpartum HemorrhageRoni NurdiantoNessuna valutazione finora
- INCOMPETENT CER-WPS OfficeDocumento5 pagineINCOMPETENT CER-WPS OfficeRickNessuna valutazione finora
- The Role of Parity in The Mode of DeliveryDocumento11 pagineThe Role of Parity in The Mode of DeliveryKanuyasa GekzNessuna valutazione finora
- The Female Reproductive System: Paul F. Terranova, PH.DDocumento17 pagineThe Female Reproductive System: Paul F. Terranova, PH.DMekuriya BeregaNessuna valutazione finora
- Female Reproductive SystemDocumento2 pagineFemale Reproductive SystemVishesh KumarNessuna valutazione finora
- Womens Knowledge Regarding Symptoms of Menopause in Al Najaf CityDocumento9 pagineWomens Knowledge Regarding Symptoms of Menopause in Al Najaf CityakankshaNessuna valutazione finora
- The Use of Acupuncture With in Vitro Fertilization: Is There A Point?Documento10 pagineThe Use of Acupuncture With in Vitro Fertilization: Is There A Point?lu salviaNessuna valutazione finora
- Jurnal HPP TinaDocumento8 pagineJurnal HPP TinaShafa AnitasyahNessuna valutazione finora
- Prior Cesarean Delivery: 100 Years of ControversyDocumento17 paginePrior Cesarean Delivery: 100 Years of ControversyNoahYudhaNessuna valutazione finora
- 2.1 Assessment of Normal Pregnant MotherDocumento41 pagine2.1 Assessment of Normal Pregnant Mother11 - JEMELYN LOTERTENessuna valutazione finora
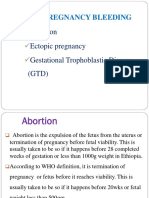
- 2.early Pregnancy and BleedingDocumento79 pagine2.early Pregnancy and BleedingjosephNessuna valutazione finora
- Superior Hypogastric Plexus Anatomy QuizDocumento4 pagineSuperior Hypogastric Plexus Anatomy QuizMaryneth EvangelistaNessuna valutazione finora
- HORMON REPRODUKSI DAN SIKLUS HAID Prof. Dr. Dr. Nusratuddin Abdullah, SP - OG (K) MARSDocumento21 pagineHORMON REPRODUKSI DAN SIKLUS HAID Prof. Dr. Dr. Nusratuddin Abdullah, SP - OG (K) MARStenri olaNessuna valutazione finora