Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Bugs & Drugs
Caricato da
veronica100%(1)Il 100% ha trovato utile questo documento (1 voto)
207 visualizzazioni33 pagineLearn
Copyright
© Attribution Non-Commercial (BY-NC)
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoLearn
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
100%(1)Il 100% ha trovato utile questo documento (1 voto)
207 visualizzazioni33 pagineBugs & Drugs
Caricato da
veronicaLearn
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 33
Bugs and Drugs: Antibacterials
RHCHP School of Pharmacy Integrated Pharmacotherapy 4 Spring 2013
FACILITATORS
READING AND REFERENCES
Required
Integrated Pharmacotherapy 4 Bugs and Drugs: Antibacterials course notes
Optional
Goodman & Gilman's The Pharmacological Basis of Therapeutics 11th edition chapters 43 - 46 (available at
AccessPharmacy)
Basic and Clinical Pharmacology 11th edition chapters 43 - 46 (available at AccessPharmacy)
Netter's Illustrated Pharmacology pages 298 - 299, 301 - 323 (page 300 is a little out of date)
Audio PowerPoint Presentation on Bugs and Drugs in order to assist your learning of this difficult topic. It is available
at: http://rhchp.regis.edu/Pharm/BugsDrugsOverviewSpring13/index.htm
RAT 7 (APRIL 17TH) LEARNING OBJECTIVES: STUDENT NOTE PACKET THROUGH AND INCLUDING PAGE 17
1. Categorize a given antibacterial agent by pharmacological class and mechanism of action (you are expected to know specifc details as
indicated in objectives 2 - 7).
2. Identify the specifc site of cell wall synthesis inhibition for -lactams, vancomycin and telavancin.
3. Explain how the instability of the -lactam ring afects the mechanism of antibacterial action.
4. When given an antibacterial mechanism of action predict whether it is bacteriostatic or bactericidal.
5. Explain the importance of bacterial target selectivity with regard to antibacterial mechanism of action.
6. Describe the antibacterial spectrum of activity for a given antibacterial or antibacterial class.
7. Identify bacteria that are covered and those which are not covered when given an antibacterial or an antibacterial class.
8. When given a patient case use spectrum of activity and allergy information to recommend the most appropriate antibacterial therapy.
9. Describe strategies to minimize the incidence of antibacterial resistance.
10. List and describe three mechanisms of genetic exchange that lead to antibacterial resistance.
11. Identify common mechanisms of antibacterial resistance for a given antibacterial or antibacterial class.
12. Identify and discuss chemical features of antibacterials that impact their clinical use and ef cacy.
13. Identify a -lactam ring structure and a sulfonamide moiety.
14. Explain how the instability of the -lactam ring afects the mechanism of antibacterial resistance and hypersensitivity.
15. Apply side-chain chemistry concepts to predict likelihood of -lactam cross-sensitivity.
16. Identify the mechanism by which specifc microorganisms become resistant to -lactamase.
17. Describe the pathology for the development of Clostridium dif cile infection.
18. Identify common and/or life-threatening adverse efects for a given antibacterial or antibacterial class.
Matt Fete, PhD
mfete@regis.edu
964-5232
Allana Sucher, PharmD, BCPS
asucher@regis.edu
625-1281
RAT 8 (APRIL 19TH) LEARNING OBJECTIVES: STUDENT NOTE PACKET, PAGE 18 - PAGE 33
1. Categorize a given antibacterial agent by pharmacological class and mechanism of action.
2. Identify the specifc site of protein synthesis inhibition for aminoglycosides, ketolides, macrolides, lincosamides, streptogramins,
chloramphenicol, oxazolidinones, tetracyclines and glycylcyclines.
3. Describe the antibacterial spectrum of activity for a given antibacterial or antibacterial class.
4. Identify the specifc steps of bacterial folic acid utilization inhibited by sulfamethoxazole and trimethoprim.
5. Describe the efect of fuoroquinolones and rifampin on bacterial nucleic acid synthesis.
6. Describe the efect of daptomycin and colistimethate on the bacterial cell membrane and function.
7. Categorize a given antibacterial as generally bacteriostatic or bactericidal.
8. Identify common mechanisms of antibacterial resistance for a given antibacterial or antibacterial class.
9. Identify and discuss chemical features of antibacterials that impact their clinical use and ef cacy.
10. Explain the importance of drug distribution for antibacterial activity.
11. Diferentiate antibacterials by renal and hepatic elimination.
12. Describe the impact of renal antibacterial elimination on dosing.
13. Describe and compare concentration-dependent and concentration-independent antibacterial activity.
14. Apply concentration-dependent and concentration-independent concepts to antibacterial dosing recommendations.
15. Describe antibacterial synergy and antagonism.
16. Describe the post-antibiotic efect.
17. Identify major drug-drug interactions for antibacterials.
18. Identify common and/or life-threatening adverse efects for a given antibacterial or antibacterial class.
19. When given a patient case use spectrum of activity and allergy information to recommend the most appropriate antibacterial therapy.
20. When given a patient case apply pharmacokinetic, pharmacodynamic, drug-drug interaction data, adverse efects, allergy data,
contraindications and clinical best practice concepts to recommend the most appropriate antibacterial therapy.
Integrated Pharmacotherapy 4 Bugs and Drugs 3
ANTIBACTERIALS: GENERAL PHARMACOLOGIC CONCEPTS
Bugs and Drugs Unit Overview
Dr. Sucher created an OPTIONAL audio PowerPoint Presentation on Bugs and Drugs in order to assist your learning of this dif cult
topic. It is available at: http://rhchp.regis.edu/Pharm/BugsDrugsOverviewSpring13/index.htm
Bugs and drugs is a phrase for the study of antimicrobials and the microorganisms that they either kill or whose growth they
inhibit. Tis IP 4 unit will focus on bacteria and systemic antibacterials. Not all antibacterials are covered in this packet. Tose that
are not covered in this unit will be discussed in future IP units. In general, the learning objectives for the RATs cover the classifcation,
chemistry and mechanisms of action of antibacterials and the bacteria that they are active against. For the RATs you should be able
to classify each antibacterial, describe its mechanism of action and relevant chemical features, and match it with bacteria that it is
active against (i.e., "covers"). General clinical concepts will also be included on the RAT. Te frst RAT will cover the beta-lactams,
vancomycin, and telavancin, while the second RAT will cover the other antimicrobial classes and agents included in this packet.
Additional learning objectives associated with mechanisms of bacterial resistance, adverse efects, and pharmacokinetic properties will
be covered on the fnal exam from this unit (see page 1 for specifc learning objectives for the RAT and fnal exam).
Antibacterial Activity: Selectivity for bacterial targets
If an antibacterial is "active against" or "covers" a bacteria, then it either kills the bacteria (a bactericidal efect) or it stops the bacteria
from growing (a bacteriostatic efect). For an antibacterial to be useful and safe it must selectively harm bacterial cells (prokaryotic
cells) while sparing human cells (eukaryotic cells). Tis means that antibacterials must target specifcities in bacterial cells that are
either not present in human cells or diferent from human cells. In some cases, antibacterials target a cellular component or an enzyme
that is not produced in human cells (e.g., the bacterial cell wall). In other cases, antibacterials are selective for the bacterial version
of a cellular component or enzyme and spare the same cellular component or enzyme in human cells (e.g., selectivity for the bacteria
version of dihydrofolate reductase).
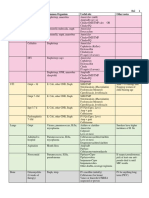
Figure 1 classifes antibacterials by the bacterial function or location that they target. Tis is a good place to begin when learning
antibacterials. Prior to the RAT and exam, you should be able to place any antibacterial by name into this fgure.
Glycopeptides
Lipoglycopeptides
Antibacterials
Penicillins
Natural
Penicillinase-Pesistant
Aminopenicillins
Antipseudomonal
Cephalosporins
Pirst-generation
Second-generation
Third-generation
Pourth-generation
Pifth-generation
-Lactam +-Lactamase
Inhibitor
Aminopenicillin + |nhibitor
Antipseudomonal + |nhibitor
Carbapenems
Monobactams
Beta-Lactams
Cell Wall Synthesis Inhibitors
Protein Synthesis Inhibitors
Aminoglycosides
Macrodides
Ketolides
Lincosamides
Streptogramins
Oxazolidinones
Chloramphenicol
Tetracyclines
Glycylcyclines
Toxic to Nucleic Acid
Synthesis or Function
Pluoroquinolones
Cyclic Lipopeptides
Antifolates
Sulfonamides
Trimethoprim
Nitroimidazoles
Nitrofurantoin
Pifampin
Toxic to Cell Membrane
Cyclic Lipopeptides
Colistimethate (Colistin)
Figure 1. Antibacterial Classifcation
Integrated Pharmacotherapy 4 Bugs and Drugs 4
Spectrum of Activity
Te set of bacteria that an antibacterial is active against is called its spectrum of activity. Tis IP 4 unit focuses on the clinically
useful spectrum of activity for antibacterials by distilling the list down to the most common and/or most important bacteria. Realize,
however, that the spectrums of activity provided in these notes are not comprehensive and that spectrums of activity can change as
bacteria evolve.
Te spectrum of activity for a given antibacterial will change over time, by geographic location, and by practice setting. For example,
an antibacterial may have high activity against a bacteria in Denver, but resistance may limit its activity against that bacteria in
Seattle. Terefore, it is imperative that you understand that it is impossible for the spectrums of activity provided in these notes to be
accurate for every possible practice setting. Rather, they refect what is usually the case in most practice settings. Tese notes are a
starting point, but always refer to your institution's antibiogram or the sensitivity trends in your geographic area when assisting
with antibacterial selection.
Resistance
One of the exciting things about infectious disease is that drug therapy best practices are always changing based on the simple
fact that bacteria become resistant to antibacterials. For example, ciprofoxacin was highly active against S. pneumoniae when
it was frst marketed in the late 1980s; now, ciprofoxacin does not have useful coverage against S. pneumoniae due to resistance
mechanisms. Mastery of resistance mechanisms will help you understand the spectrum of activity for some antibacterials (especially
the -lactams).
"Te World Health Organization (WHO) has identifed antimicrobial resistance as one of the three greatest threats to human health."
(CID 2010;50:1081-83) Antibacterial resistance may be thought of as either (1) primary drug resistance or (2) secondary drug
resistance. Primary drug resistance refers to resistance that is inherent to the organism and that was present before the antibacterial
was ever used. In other words, some organisms were just born resistant to certain antibacterials. Secondary, or acquired, drug
resistance refers to resistance that develops following exposure of an organism to an antibacterial.
Te widespread use and overuse of antibacterials has led to the emergence of drug-resistant organisms. Relative to human cells,
bacteria replicate rapidly and during replication there is always a risk for random genetic mutations. With time and chance,
a microorganism will eventually develop a mutation that renders it resistant to an antibacterial, or even to a whole class of
antibacterials. If a microorganism develops resistance against multiple classes of drugs it is referred to as multi-drug resistant or
termed a superbug.
SURVIVAL OF THE FITTEST
Te most sensitive microorganisms will be the frst
to be killed or the frst to have their growth halted
by an anti-infective agent (see Figure 2). Terefore,
constant exposure to (or pressure from) anti-infectives
selects the strongest, least sensitive microorganisms
for proliferation, while the weaker, more sensitive
microorganisms are wiped out. Tis alone may lead
to the development of antibacterial resistance. In
addition, using too low of a dose and/or an insuf cient
length of therapy usually increases the rate of
development of antibacterial resistance.
Unfortunately, the genes that code for antibacterial
resistance may be passed among microorganisms. In
fact, some forms of resistance may be passed from one
species to another species (e.g., from Staphylococcus
aureus to Staphylococcus epidermidis) or from one genus to another genus (e.g., plasmid transfer of the gene for -lactamase from
Staphylococcus aureus to Neisseria gonorrhoeae).
GENETIC DEVELOPMENT OF RESISTANCE
Drug resistance occurs when a genetic change in a microorganism results in a structural or functional change that interferes with anti-
infective activity. Tere are two general processes by which these genetic alterations occur.
Vertical Evolution
Mutation of chromosomal DNA in microbes can lead to alteration of microbes such that resistance develops. When microbes acquire
Figure 2. Selective Pressure of Antibacterials Promotes Bacterial Resistance
CMAJ 2009;180:408-415
Integrated Pharmacotherapy 4 Bugs and Drugs 5
resistance by random mutation within their own chromosome they will most likely pass this resistance to daughter cells during
replication: this process is called vertical evolution.
Horizontal Evolution
Microbes may acquire resistance from other resistant organisms. When this
happens, the process is called horizontal evolution. Resistance may be acquired
from within the same species (e.g. one strain of S. aureus passing resistance
to another strain of S. aureus) or from another species (e.g., S. aureus passing
resistance to N. gonorrhoeae).
Tere are three mechanisms by which genetic exchange occurs during
horizontal evolution. Conjugation occurs by transfer of a plasmid containing
a resistance factor (i.e. a gene) from one microbe to another (see Figure
3). Transduction occurs by a bacteriophage (a virus) transferring resistance
genes from one microbe to another. Transformation occurs by release of
genetic information containing resistance factors into the environment by
a microbe and subsequent uptake of that genetic information by another
microbe.
Te specifc mechanism of resistance varies by drug and bacteria. Te
following is a list of general mechanisms known for antibacterial resistance:
Enzymatic Inactivation: Production of an enzyme that destroys the drug.
Alteration of Target Site: All antibacterial drugs have a site of action
and their efficacy is dependent on a high affinity for that site of action. If
a genetic mutation occurs such that the target site is altered, then the
antibacterial may have a decreased affinity for the site of action such that it
is no longer effective.
Overproduction of Target Site: Excess production of antibacterial target site results in insufficient antibacterial activity.
Antibacterial Efflux: Protein efflux pumps embedded in the cell membrane actively transport antibacterials from the bacteria.
Metabolism of Antibacterials: Bacteria may use enzymes to metabolize antibacterials to inactive metabolites in a similar manner
as phase-II human drug metabolism pathways.
Alteration of Membrane Permeability: Both the inner and outer (if present) membrane of bacteria may be altered by genetic
mutation such that certain antibacterials can no longer diffuse into the cell.
Figure 4 provides a summary of antibacterial sites of action and mechanisms of resistance for your reference.
Toxicity Common to Most Antibacterials
OVERGROWTH OF NON-SENSITIVE BACTERIA
Te body maintains a balance of various bacteria in the gastrointestinal tract known as the normal fora. Antibacterials will kill
or inhibit the growth of some, but usually not all, of these bacteria. Te bacteria that are not targeted by an antibacterial have the
opportunity to increase more in growth relative to other bacteria due to increased growth resources and space. Te overgrowth of non-
sensitive bacteria may cause gastrointestinal toxicity. Usually this manifest as mild diarrhea that subsides afer a few days of therapy or
when therapy is complete or discontinued. In some cases, however, the overgrowth of some bacteria may cause serious gastrointestinal
complications. An example is the overgrowth of Clostridium dif cile, a gram-positive anaerobe that produces a toxin. Excess
production of this toxin may cause pseudomembraneous colitis.
Gene coding for
resistance factor
Plasmid enters sensitive bacteria
Sensitive bacteria uses
gene to make resistance factor
Resistant bacteria
Figure 3. Mechanism of Plasmid-Mediated Resistance
Integrated Pharmacotherapy 4 Bugs and Drugs 6
Figure 4. Site of Antibacterial Action and Mechanisms of Resistance
CMAJ FEBRUARY 17, 2009 180(4) 410
Mechanisms of resistance
Permeability barriers
Efflux pump
Antibiotic target
modification:
Altered penicillin-
binding proteins
Altered DNA gyrase
Antibiotic
Inactivating enzymes:
-lactamase
Aminoglycoside-
modifying enzymes
Agents that bind to ribosomes
and inhibit protein synthesis:
Aminoglycosides
Tetracyclines
Macrolides
Clindamycin
Chloramphenicol
Linezolid
Agents that inhibit
cell wall synthesis:
Penicillins
Cephalosporins
Carbapenems
Glycopeptides
(vancomycin)
Agents that inhibit
DNA synthesis:
Fluoroquinolones
Agents that inhibit
RNA polymerase:
Rifampin
Bacterial
cell wall
Bacterium
DNA
DNA
gyrase
RNA
polymerase
Ribosomes
mRNA
Sites of action
Antibiotics
??
??
? ?
Figure 1: Sites of action and potential mechanisms of bacterial resistance to antimicrobial agents. Modified with permission from the
American Association for the Advancement of Science (Science 1992;257:106473).
3
L
i
a
n
n
e
F
r
i
e
s
e
n
a
n
d
N
i
c
h
o
l
a
s
W
o
o
l
r
i
d
g
e
Integrated Pharmacotherapy 4 Bugs and Drugs 7
ANTIBACTERIALS: THERAPEUTIC CONSIDERATIONS
Strategies to Minimize the Spread of Antimicrobial Resistance
Te Centers for Disease Control and Prevention (CDC) has several
activities which target inappropriate antimicrobial use with an ultimate
goal of decreasing the spread of antimicrobial resistance. Tese strategies
target educating clinicians on appropriate practice guidelines while
simultaneously educating patients on realistic expectations and possibly
inappropriate demands for antibiotics. See Figure 5 for the key points of
this important campaign targeted toward the lay public and Table 1 and
Figure 6 for information targeted at clinicians. In addition, as previously
discussed in the Introduction to Infectious Diseases packet, antimicrobial
stewardship is important. Antimicrobial stewardship has 3 main goals:
Ensure patient receives the most appropriate antimicrobial with the
correct dose and duration
Follow the "4 D's": right Drug, right Dose, De-escalation to
pathogen-directed therapy, and right Duration of therapy
Prevent antimicrobial overuse, misuse, and abuse
Minimize the development of resistance
Patients exposed to antibiotics are at higher risk of becoming
colonized or infected by resistant organisms
Other Considerations
Te use of any antibiotic may result in fungal or bacterial superinfection, including C. dif cile-associated diarrhea (CDAD), also known
as C. dif cile infection, antibiotic-associated diarrhea, or pseudomembranous colitis. How does this happen? Antibiotic use may disrupt
intestinal fora, resulting in an overgrowth of C. dif cile, an organism that normally colonizes the intestine. C. dif cile produces 2 main
toxins, toxin A and toxin B, which cause infammation, pseudomembrane formation, and watery diarrhea, as further described in
Figure 7 on page 8.
You have just filled
a prescription for an
antibiotic
READ THIS IMPORTANT INFORMATION
Take it exactly as your medical expert tells you
Do not skip doses
Do not share it with others
Finish the prescription even if you feel better
Do not save it for later
Why is this checklist so important?
Using an antibiotic the wrong way can make infections
stronger and harder to treat. You can prevent this
problem by getting smart about antibiotics.
Take antibiotics the right way.
For more information call
1-800-CDC-INFO or visit
www.cdc.gov/getsmart
Figure 5. CDC GET SMART Campaign
Table 1. Role of Clinicians to Minimize the Spread of Resistance
Use point-of-care tests to determine if an infection has a viral or bacterial
etiology
Educate patients on the prevalence of infections caused by viruses
Routinely question patients on history of recent antibiotic exposure and if
possible, use an alternate antibiotic class
Be aware of local geographic susceptibility data
Figure 6. CDC GET SMART Campaign
http://www.cdc.gov/getsmart/campaign-materials/week/downloads/
GetSmart-wdates.pdf
For more information visit www.cdc.gov/getsmart or
call 1-800-CDC-INFO
1 2 3
Counsel Patients on
Antibiotic Resistance
and
Recommend
Symptomatic Therapy
for
Viral Illnesses
CS203953-A
Counsel Patients
on Appropriate
Antibiotic Use
P
H
A
R
M
A
C
I
S
T
S
C
A
N
M
A
K
E
T
H
E
D
I
F
F
E
R
E
N
C
E
more rr informati a on visit www. ww cdc.go g v/ge g / tsmart o t r
call 1-800-CDC-INFO
2 3
Counsel Patients on Counsel P Counsel P
Antibiotic Resistance
and
Recommend Recom Reco
Symptomatic Therapy
for
Viral Illnesses
CS203953 A CS203953-A
el Patients e
ppropriate
biotic Use
P
H
A
R
M
A
C
I
S
T
S
C
A
N
M
N
A
K
E
T
H
E
D
I
F
F
E
R
E
N
C
E
P
R
O
M
O
T
E
A
P
P
ROP
R
I
A
T
E
A
N
T
I
B
I
O
T
I
C
U
S
E
Adverse Effects
6et $mzrt Ab60t Aatibi6titt Neek
November 14-20, 2011
Integrated Pharmacotherapy 4 Bugs and Drugs 8
CLEVELAND CLI NI C J OURNAL OF MEDI CI NE VOLUME 73 NUMBER 2 FEBRUARY 2006 191
Pathogenesis of C difficile-associated disease
Clostridium difficile is
spread via the fecal-oral
route. The organism is
ingested either as the
vegetative form or as
hardy spores, which can
survive for long periods
in the environment and
can traverse the acidic
stomach.
In the large intestine,
C difficile-associated
disease can arise if the
normal flora has been
disrupted by antibiotic
therapy.
Toxin A attracts neutrophils and
monocytes, and toxin B degrades
the colonic epithelial cells, both
leading to colitis, pseudomembrane
formation, and watery diarrhea.
C difficile reproduces in the
intestinal crypts, releasing
toxins A and B, causing
severe inflammation.
Mucous and cellular debris
are expelled, leading to the
formation of
pseudomembranes.
C difficile
Toxins
Monocyte
Neutrophil
Pseudomembrane
In the small intestine,
spores germinate into
the vegetative form.
FIGURE 3
CCF
2006 Medical Illustrator: David Schumick
Figure 7. Clostridium dif cile
Integrated Pharmacotherapy 4 Bugs and Drugs 9
ANTIBACTERIAL MECHANISMS OF ACTION, MECHANISMS OF RESISTANCE, SPECTRUM OF ACTIVITY, AND TOXIC-
ITY
-Lactams
The -lactams are a large family of antibacterials that are divided into four classes: penicillins, cephalosporins, carbapenems and
monobactams. Penicillins and cephalosporins are further broken down into subclasses. All -lactam antibacterials contain a -lactam
ring in their chemical structure (see Figure 8). With the exception of
monobactams, all -lactams have a second ring system attached to the
-lactam ring. All -lactams also have an acyl side chain attached to
the -lactam ring, and variations in this side chain afect the -lactam
properties (see Figure 8).
CHEMISTRY
Te -lactam ring is an unstable functional group, subject to
nucleophilic attack and subsequent ring opening. Te susceptibility
of the -lactam to nucleophilic degradation varies depending on the
ring system and acyl side chain attached to the -lactam ring. In
one respect, nucleophilic attack and breakdown of -lactams is
advantageous because this is how they produce their antibacterial
efect (discussed below); however, this susceptibility makes -lactams
vulnerable to antibacterial resistance mechanisms and is a cause of
allergic hypersensitivity reactions (also discussed below).
MECHANISM OF ACTION
All -lactams have the same general mechanism of action:
inhibition of bacterial cell wall synthesis. Specifcally, -lactams
interfere in the fnal steps of peptidoglycan synthesis. Peptidoglycan,
which is not found in eukaryotic cells, is analogous to a non-
stretchable bag that encloses the entire bacterium. Gram-negative
bacteria have a thin peptidoglycan layer while gram-positive bacteria
have a thick peptidoglycan layer. Each layer must be attached to
adjacent layers to maintain rigidity, and therefore preserve the
intracellular integrity of the bacterium. Te layer to layer attachment
process is called cross-linking, and -lactams block cross-linking
during peptidoglycan synthesis (see Figure 9 on page 10).
-lactams block peptidoglycan cross-linking by inhibiting enzymes
called transpeptidases that catalyze cross-linking. Specifcally,
transpeptidases attack the -lactam ring, forming a covalent bond that
permanently disables the enzyme. For this reason, transpeptidases are
more commonly known as penicillin-binding proteins, or PBPs for
short. Tis name is a little misleading, however, because all -lactams
(not just the penicillins) bind to PBPs to exert their antibacterial
action.
Inhibition of peptidoglycan cross-linking in bacteria has the overall
efect of inhibiting bacterial cell wall synthesis. A functional cell wall is essential to life for most bacteria, and inhibition of cell wall
synthesis by -lactams has a bactericidal efect due to rapid lysis of the bacterium.
MECHANISMS OF RESISTANCE
Figure 10 on page 11 summarizes the cellular sites of the three forms of resistance described in this section. One common mechanism
of resistance to -lactams is degradation by bacterial enzymes. Some bacteria produce enzymes that attack the -lactam bond in the
same manner as PBPs. Tese enzymes are called -lactamases (also called penicillinases). Covalent binding of a -lactamase to a
-lactam destroys the ring system and renders the -lactam inactive. -lactamases live in the space formed between the cell wall and
cell membrane of bacteria, called the periplasmic space. In this manner, they are located in the perfect spot to destroy -lactams just
before the -lactam can block cell wall synthesis.
Just as with PBPs, there are a number of diferent -lactamases that bacteria may produce, and a whole nomenclature system for
N
H
HN R
O
O
Diferent ring for each
class of -lactams
(monobactams have no ring) N
O
-lactam ring
Variation in acyl side chain
afects spectrum of activity
and cross-sensitivity risk.
N
H
HN R
O
O
HN
H
HN R
O
HO
Nucleophile
Nucleophilic
Attack
Nucleophile
Nucleophilic attack on -lactam ring explains:
1. Mechanism of action (PBP binding)
2. Mehanism of resistance (-lactamase)
3. A cause of hypersensitivity (hapten formation)
Figure 8. -Lactam Chemistry
Integrated Pharmacotherapy 4 Bugs and Drugs 10
-lactamases has been created to keep track of the enzymes. Te nomenclature of -lactamases will not be covered here.
All -lactams are not equally susceptible to -lactamase degradation. As a general rule, penicillins are most susceptible, followed by
cephalosporins. Carbapenems and monobactams have a relatively high level of resistance to -lactamase degradation.
Te other common mechanism of bacterial resistance to -lactams is an alteration in PBP structure, such that the -lactam has
less af nity for the active site of the PBP. Tese alterations reduced antibacterial binding and render the bacteria less sensitive to
-lactams. Tis is an example of a common general mechanism of antibacterial resistance called alteration of target site. -lactams
put selective pressure on bacterial to favor growth of strains that produce mutated, but still functional, PBPs. In some cases, this form
of resistance may be overcome by increasing the dose of the -lactam such that
the concentration of -lactam is higher at the site of infection (i.e., overcoming the
decrease in PBP af nity by increasing the drug concentration).
A third mechanism of -lactam resistance is alteration of porin structure in gram-
negative bacteria. Many gram-negative bacteria have an additional outer membrane
that surrounds the cell wall. Protein channels called porins are embedded in this
outer membrane and allow substances, such as -lactams, to difuse across the outer
membrane and reach the cell wall. Mutations in porin genes result in porins that
have an altered shape and no longer allow -lactams to difuse as well, or even at all.
PENICILLINS
All penicillins share a common chemical structure with variations from one drug to the next occurring in the acyl side chain as
depicted in Figure 11 on page 11. Penicillins are divided into subclasses based on structural attributes and their spectrum of activity.
G M G M G M
G M G M G M G M
G M G M G M
G M G M G M G M
G M
G M
D-Ala
D-Ala
D-Ala
D-Ala
The terminal D-Ala must be removed by
transpeptidase during cross-linking of
peptidoglycan layer.
Vancomyin and Telavancin bind to
D-Ala-D-Ala and prevent transpeptidase
(PBPs) from cross-linking.
Replacement of terminal D-Ala with D-lactate
causes resistance to vanocmycin because it
prevents vancomycin from binding.
Step 1: Addition of G-M to growing peptidoglycan chain
(Polymerization)
G M G M G M
G M G M G M G M
G M
Step 2: Cross-linking of peptidoglycan layer
Beta-lactams inhibit cross-linking
of growing peptidoglycan layers by
binding to and inhibiting PBPs from
catalyzing cross-linking.
Mutation of PBPs is one form of
beta-lactam resistance.
Catalyzed by transpeptidases also known as
Penicillin-Binding Proteins (PBPs)
Synthesis of peptidoglycan in bacterial cell wall.
G = N-acetylglucosamine
Telavancin blocks polymerization
of peptidoglycan chain
Figure 9. Mechanism of Action for Beta-Lactams and Vancomycin
MECHANISMS OF -LACTAM RESISTANCE
Production of -lactamase (penicilliase & cephalosporinase)
MSSA, H. influenze, M. catarrhalis, Bacteroides spp.
Alteration of -lactam target site (PBPs)
MRSA, S. pneumoniae
Alteration of porin structure in gram-negative bacteria
Enterobacteriaceae, Pseudomonas spp.
Integrated Pharmacotherapy 4 Bugs and Drugs 11
Natural Penicillins
Penicillin G and V are called "natural penicillins" because they are
produced in fungi cultures. Each penicillin can be preferentially
created in the fungi culture by "feeding" the culture specifc
chemical precursors that are incorporated into the acyl side chain
(position 6 in Figure 11).
Penicillin G is highly unstable to acid and readily breaks down in
a low pH environment; accordingly, penicillin G is administered
by parenteral injection. Penicillin V is considerably more stable to
acid, and may be successfully administered orally.
Te spectrum of activity of penicillin G and V is important
mostly for their activity against Streptococcus spp. (see Table
2) Most Streptococcus spp. (including Group A streptococci)
have remained highly sensitive due to lack of -lactamase
production. However, PBP alteration in S. pneumoniae has led
to increasing rates of penicillin-resistant strains. For some S.
pneumoniae strains this resistance may be overcome by increasing
the penicillin dose, but for other strains the resistance is too
strong. Currently, natural penicillins should
be used for S. pneumoniae only afer obtaining
appropriate sensitivity results.
Penicillinase-Resistant Penicillins
Te natural penicillins were initially active against
many bacteria, but production of -lactamase
developed rapidly in many bacteria following
widespread use of these drugs in the 1950s. To
overcome this form of resistance in Staphylococcus
spp., a large bulky acyl side chain was added to
the penicillin structure which blocks the drug
from entering the active site of -lactamase. As
a result, these drugs are resistant to -lactamase
produced by Staphylococcus spp., and retain activity
against Staphylococcus spp. that are resistant to
penicillins due to -lactamase production (see
Table 22). However, other forms of resistance in
Staphylococcus spp. (e.g., PBP alteration) will cause
resistance. Penicillinase-resistant penicillins are
importrant for their activity against methicillin-
sensitive S. aureus (MSSA). Methicillin was the
original drug in this subclass of penicillins, but
Table 2. Summary of Clinically Useful Spectrums of Activity for Penicillins
Penicillin Class MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Natural Penicillins +
Penicillinase-Resistant + +
Aminopenicillins + +
A
+
B
Antipseudomonal + +
A
+ +
-Lactamase Inhibitor
Combinations
+ + +
A
+ +
C
+
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
A: Only active against Enterococcus spp. that are sensitive to ampicillin
B: Limited GNR spectrum to some E. coli strains and other gram-negative bacteria that do not produce -lacatmase (increasingly uncommon)
C: Only -lactamase inhibitor combinations with an antipseudomonal penicillin cover P. aeruginosa (e.g., piperacillin + tazobactam)
Figure 10. Sites of Resistance to Penicillins
N
S
O
OH
H
HN
O
O
Penicillin G
Amoxicillin
Nafcillin
Piperacillin
N
S
O
OH
H
HN
O
N
S
O
OH
H
HN
O
O
O
Bulky side chain prevents
-lactamase degradation
Polar side chain greatly improves
penetration into gram-negative bacteria
Amino side chain improves penetration
into gram-negative bacteria
N
S
H
N
O
O
O
NH
2
HO
HO
N
S
O
OH
H
HN
O
O
H
N N
O
N
O
O
1
2
3
4
5
6 7
Substitutions at
6-position afect
bacterial coverage and
risk for cross-sensitivity
Figure 11. Penicillin Chemistry
Integrated Pharmacotherapy 4 Bugs and Drugs 12
is no longer marketed today. However, it is forever remembered in the name
methicillin-resistant S. aureus (MRSA). See Te MRSA Story on page 12.
Aminopenicillins
Te name aminopenicillin refers to penicillins containing an amino functional
group on the acyl side chain (see Figure 11 on page 11). Te amino group is
believed to increase the penetration of aminopenicillins into the periplasmic
space of gram-negative bacteria. Amoxicillin has improved oral bioavailability
relative to ampicillin, and is preferred for oral use over ampicillin.
Te spectrum of activity for aminopenicillins is extended to some gram-
negative bacteria relative to natural penicillins (see Table 2 on page 11). However,
production of -lactamase is common among many gram-negative bacteria
and the reliability of aminopenicillins for gram-negative coverage has
waned. Examples of gram-negative bacteria covered by aminopenicillins
include the non--lactamase producing strains of E. coli and H. infuenzae.
Aminopenicillins are important for their activity against the Gram-positive
organisms Enterococcus and Listeria monocytogenes (cause of meningitis).
Amoxicillin is also used to treat some upper respiratory tract infections
(otitis media) caused by Streptococcus pneumoniae, when given at high doses.
Antipseudomonal Penicillins (Carboxypenicillins and Ureidopenicillins)
Piperacillin is an ampicillin derivative in which the acyl side chain has
been replaced with a urea derivative. Tis type of penicillin is called a
ureidopenicillin (see Figure 11 on page 11). Ticarcillin (not shown in Figure
11) contains a carboxyl acyl side chain and is called
a carboxypenicillin. Tese acyl side chains greatly
increase the activity for these penicillins against gram-
negative bacteria. Tese penicillins were originally
developed to target P. aeruginosa, and are accordingly
called antipseudomonal penicillins. You may also see
them referred to as "extended-spectrum" or "broad-
spectrum" penicillins.
As shown in Table 2 on page 11, antipseudomonal
penicillins have the broadest gram-negative spectrum
of all penicillins because they cover P. aeruginosa. Of
the two, piperacillin is more commonly used, most frequently in combination
with tazobactam as the product Zosyn.
-lactamase inhibitor combinations
Resistance to penicillins due to -lactamase production may be overcome by
combining a penicillin with a -lactamase inhibitor. Clavulanic acid, sulbactam
and tazobactam are the three -lactamase inhibitors currently used in the U.S.
-lactamase inhibitors have high af nity for binding to the active site of
-lactamase, where they form a covalent bond with the enzyme in a similar
manner as penicillins (see Figure 1212). Since they have a higher af nity
for -lactamase than the penicillin that they are combined with, -lactamase
inhibitors protect penicillins from degradation.
-lactamase inhibitors increase the spectrum of activity to include bacteria
that produce -lactamase. Tese organisms include: MSSA, Bacteroides spp.,
and some gram-negative bacteria (H. infuenzae and M. catarrhalis).
Adverse Efects
Penicillins are generally very well tolerated, allowing for large doses to be
administered if necessary. Of the diferent classes of antibacterials, penicillins
seem especially prone to causing hypersensitivity due to immune reactions. One
PENICILLINS
Natural Penicillins
Aqueous Penicillin G (benzylpenicillin) (IM, IV)
Benzathine Penicillin G (Bicillin) (IM depot)
Penicillin G Procaine (Wycillin) (IM depot)
Penicillin V Potassium (Pen-VK, Veetids) (PO)
Penicillinase-Resistant Penicillins
Dicloxacillin (PO)
Nafcillin (IM, IV)
Oxacillin (IM, IV, PO)
Aminopenicillins
Ampicillin (Principen) (IM, IV, PO)
Amoxicillin (Amoxil) (PO)
Antipseudomonal Penicillins
Piperacillin (Pipracil) (IV)
Ticarcillin (Ticar) (IV)
-Lactamase Inhibitor Combinations
Amoxicillin + Clavulanic acid (Augmentin)
(PO)
Ampicillin + Sulbactam (Unasyn) (IV)
Piperacillin + Tazobactam (Zosyn) (IV)
Ticarcillin + Clavulanic acid (Timentin) (IV)
THE MRSA STORY
MRSA is Methicillin-resistant Staphylococcus aureus and is a multi-
drug resistant strain of S. aureus associated with significant
morbidity and mortality.
When penicillin was originally discovered S. aureus was highly
sensitive. Resistance to penicillin in S. aureus first developed
due to production of -lactamase (or penicillinase). To fight
this resistance, methicillin was developed and became the
first member of a new class of penicillins called penicillin-
ase-resistant penicillins. As time passed, nearly all strains of
S. aureus acquired beta-lactamase.
Eventually S. aureus developed a second form of resistance
to all penicillins, including methicillin, due to mutations at
the target site of penicillins (PBPs). This resulted in a form
of S. aureus that was resistant to all penicillins as well as all
other beta-lactams due to acquisition of two mechanisms
of resistance. Due to its resistance to methicillin, the name
given to this strain of S. aureus was MRSA.
Many other antibacterials have been used against MRSA,
and as a result MRSA has acquired even more forms of
antibacterial resistance. Currently, there are relatively few
choices for effective treatment of MRSA that is acquired in
the hospital. Community-acquired infections of MRSA are
currently on the rise, but fortunately the strains of MRSA
causing these infections are often sensitive to several ad-
ditional antibacterials.
N
S
O
O
O
H
N
N
N
O OH
N
S
O
O
H
N
N
N
O OH
Beta-Lactamase
C
O
HO
Beta Lactamase
Tazobactam Tazobactam covalently bound to beta-lactamase,
preventing the enzyme from degrading pencillins
Figure 12. Mechanism of Action of -Lactamase Inhibitors
Integrated Pharmacotherapy 4 Bugs and Drugs 13
possible cause for hypersensitivity is binding of the -lactam ring to endogenous
proteins, forming a hapten which is recognized by the body's immune system
as foreign. Subsequent to this, the body will mount an IgE-related immune
response. Te most dangerous form of hypersensitivity is anaphylaxis, which
is life-threatening. Patients that are allergic to penicillins may also be allergic
to other -lactams. Te risk appears to be related to similarities in side chain
functionality (position 6 for penicillins and positions 3 and 7 for cephalosporins)
(the greater the similarity between two drugs the higher the risk of cross-
sensitivity). Te likelihood of cross-sensitivity has been reported at 10% for
cephalosporins (but is likely lower), up to 50% for carbapenems (but likely
lower), and unlikely with monobactams. Cefazidime (a third-generation
cephalosporin) has the same acyl side chain as aztreonam (a monobactam); thus
there is a risk for cross-sensitivity between these 2 agents. Penicillin allergy may
be confrmed using a skin test. If a penicillin must be used in a patient with a
documented penicillin allergy, then desensitization protocols exist in which a very
low dose is initiated followed by frequent doses that gradually increase in amount.
CEPHALOSPORINS
All cephalosporins share a common -lactam ring system as highlighted in
Figure 13. Cephalosporins are similar to penicillins, but their chemical structure
provides high stability to -lactamase degradation. Side-chain substitutions afect bacterial coverage, pharmacokinetics, and allergy
cross-sensitivity with penicillins (see adverse efect section). However, cephalosporinases (-lactamases that cephalosporins are
susceptible to) do exist (e.g., anaerobic bacteria). More concerning are extended-spectrum -lactamases (ESBLs) that are inducible by
third-generation cephalosporins. ESBLs confer resistance to all -lactams except cefepime, cephamycins (see second-generation
agents) and carbapenems.
Cephalosporins are divided into fve generations, largely based on their spectrum of bacterial coverage. However, the generations
also parallel the time course of cephalosporin discovery, as older cephalosporins are the frst- and second-generation agents
and newer cephalosporins are third-, fourth-, and ffh generation agents. As a very general rule, gram-negative coverage
increases with increasing cephalosporin generations. Other general spectrum of activity points are 1) no cephalosporin covers
Enterococcus spp. and 2) the only cephalosporins active against anaerobes are the second-generation cephamycins (cefoxitin and
Cephalexin
Ceftriaxone Cefepime
Cefotetan
N
S
HO O
O
H
HN
O
NH
2
N
S
O
O OH
S
H
N
H
O
O
S
S
O OH
H
2
N
O
N N
N
N
N
S
HO O
O
H
HN
O
N
O
S
N
H
2
N
S
N
NH
N
O
O
O
N
O
H
N S
N
O
-
O O
N
+
S
H
2
N
N
H
S
N N
N
N
Methylthiotetrazole ring
Methoxy group
N
S
HO O
O
H
HN
N
S
O
O OH
H
N
H
N
S
HO O
O
H
HN N S
N
O
-
O O
H
O
1
2
3 5 6
7
8
4
Substitutions at 3-position
afect pharmacokinetics and
allergy cross-sensitivity
Substitutions at 7-position
afect spectrum of activity
and allergy cross-sensitivity
Figure 13. Cephalosporin Chemistry
PENICILLIN ADVERSE EFFECTS
Allergic Reaction (Hypersensitivity)
May lead to life-threatening anaphylaxis
Other -lactams may be cross-sensitive and also cause an allergic
reaction in PCN-allergic patients
Rash
More common with aminopenicillins, may or may not be due to
a true drug allergy
Excessive Sodium
IV products contain large amounts of sodium
May cause fluid overload, particularly dangerous in CHF patients
Seizures and CNS Excitability
Dose-dependent
Risk is greater in patients with renal insufficiency
Neutropenia & Thrombocytopenia
Dose-dependent
More likely with piperacillin/tazobactam
Antibiotic-Related Diarrhea
Particularly common with ampicillin
Integrated Pharmacotherapy 4 Bugs and Drugs 14
cefotetan). Mastering the spectrum of activity for cephalosporins is particularly tedious... please note that Table 3 on page 14 includes
acronyms to help you.
First-Generation Cephalosporins
While others are still marketed, cefazolin (IM, IV) and cephalexin (PO) are the
only two commonly used frst-generation cephalosporins. Tey are primarily
useful for their gram-positive spectrum of activity, but are also active against a
few gram-negative bacteria (see Table 3 on page 14).
Second-Generation Cephalosporins
Most second-generation cephalosporins have better activity towards S.
pneumoniae and less activity towards Staphylococcus spp. than the frst-generation
agents. Gram-negative coverage includes organisms covered by frst-generation
agents and extends to several additional gram-negative organisms (see Table 33).
In addition, the second-generation includes the only two cephalosporins with
clinically useful activity against anaerobic bacteria: cefoxitin and cefotetan (also
classifed as cephamycins). Te addition of a methoxy group to the -lactam ring
(as depicted in Figure 13 on page 13 for cefotetan) of these two drugs decreases
susceptibility to -lactamases (cephalosporinases) produced by anaerobic bacteria
which degrade other cephalosporins.
Third-Generation Cephalosporins
Relative to frst- and second-generation cephalosporins, the third-generation
cephalosporins penetrate better into gram-negative bacteria and have
extended gram-negative coverage (see Table 33). However, gram-positive
coverage is less reliable for the third-generation agents as a general rule. Only
cefotaxime, cefriaxone, cefpodoxime, cefdinir and cefditoren have reliable
MSSA coverage. Cefriaxone, cefotaxime and cefpodoxime are useful for S.
pneumoniae. Cefazidime is only efective against gram-negative bacteria, and is
the only third-generation agent with reliable activity against P. aeruginosa. As will
be discussed in a future TBL unit, cefxime and cefriaxone are also used to treat
Neisseria gonorrhoeae.
Fourth-Generation Cephalosporins
Cefepime is a fourth-generation cephalosporin with good gram-positive activity that retains reliable gram-negative activity (including
P. aeruginosa).
Fifth-Generation Cephalosporins
Te most recently approved cephalosporin is cefaroline (Tefaro). Tis agent is considered to be a ffh generation cephalosporin
because it is unique in its antimicrobial coverage as compared to other agents in the class. Cefaroline covers Staphylococcus aureus
(including MRSA and strains that are vancomycin-intermediate and resistant), Streptococcus pneumoniae, and some Gram-negatives
(but NOT Pseudomonas). Cefaroline is the only beta-lactam that has coverage against MRSA.
Table 3. Summary of Clinically Useful Spectrums of Activity for Cephalosporins
Generation MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
First-generation + + PEcK
Second-generation + + HiMPEcK
+only for
cefoxitin and
cefotetan
Third-generation
+ (NOT
ceftazidime)
+ (NOT
ceftazidime)
HiMPEcK
SPACE
A
+ only for
ceftazidime
Fourth-generation + +
HiMPEcK, SPACE,
and ESBL-producers
+
Fifth-generation + +
F
+ HiMPEcK
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
PEcK = Proteus mirabilis, E. coli, Klebsiella spp. HiMPEcK = Haemophilus infuenzae, Moraxella catarrhalis, Proteus mirabilis, E. coli, Klebsiella spp.
SPACE = Serratia spp., Proteus spp. (mirabilis + vulgaris), Acinetobacter spp., Citrobacter spp., Enterobacter spp.
A: Third-generation agents can stimulate SPACE, E. coli and Klebsiella spp. to hyperproduce ESBLs (extended-spectrum -lactamases)
CEPHALOSPORINS
First-Generation
Cefadroxil (Duricef) (PO)
Cefazolin (Ancef) (IV, IM)
Cephalexin (Keflex) (PO)
Second-Generation
Cefaclor (Ceclor) (PO)
Cefotetan (Cefotan) (IV, IM)
Cefoxitin (Mefoxin) (IV, IM)
Cefprozil (Cefzil) (PO)
Cefuroxime (Zinacef) (IV, IM)
Cefuroxime axetil (Ceftin) (PO)
Third-Generation
Cefdinir (Omnicef) (PO)
Cefditoren (Spectracef) (PO)
Cefixime (Suprax) (PO)
Cefpodoxime (Vantin) (PO)
Ceftazidime (Fortaz) (IV, IM)
Ceftibuten (Cedax) (PO)
Ceftizoxime (Cefizox) (IV, IM)
Ceftriaxone (Rocephin) (IV, IM)
Cefotaxime (Claforan) (IV, IM)
Fourth-Generation
Cefepime (Maxipime) (IV, IM)
Fifth-Generation
Ceftaroline (Teflaro) (IV)
Bolded names: Know generation classification for exams
Integrated Pharmacotherapy 4 Bugs and Drugs 15
Adverse Efects
Like penicillins, cephalosporins are remarkably well-tolerated given how frequently they are used and their relatively high
doses. Hypersensitivity is a risk, but not as frequent as penicillins (cross-sensitivity information covered in the penicillin section).
Most cephalosporins are eliminated unchanged by the kidneys. Cefriaxone is an exception to this rule, and undergoes extensive
hepatobiliary (liver + bile excretion) elimination. While this is advantageous in terms of cefriaxone having a relatively long half-
life allowing for once-daily dosing, it also causes precipitation of bile (biliary sludging/gallbladder disease) in some patients. Elderly
patients receiving lengthy therapy may be at higher risk. Cefriaxone should be avoided in neonates with hyperbilirubinemia due to
the need for biliary function to clear excess bile; use of cefriaxone in these patients may cause encephalopathy due to exacerbation of
hyperbilirubinemia. Cefriaxone has also been associated with fatal lung and kidney precipitate reactions when given concomitantly
with IV calcium-containing products, and this combination should be avoided in neonates (age 28 days).
Cephalosporins with a methylthiotetrazole ring system (as depicted for cefotetan in Figure 13) may be associated with a risk for
increased bleeding due to decreased coagulation function.
CARBAPENEMS
Carbapenems are -lactams contain a carbon instead of a sulfur in their ring system (as compared with penicillins and cephalosporins),
and are therefore called carbapenems (see Figure 14). Tey all share a common ring system but vary in terms of side chain
chemistry. Imipenem is susceptible to breakdown by renal dehydropeptidase-1 (an enzyme produced by humans to break down
peptides). Cilastatin, an inhibitor of this enzyme, is combined with imipenem to prolong its half-life such that it is efective. Te
carbapenem ring system confers a high level of resistance to -lactamase degradation.
Te spectrum of activity for carbapenems can be simplifed by considering ertapenem separate from other carbapenems. In part due
to their resistance to -lactamase degradation, carbapenems have extensive gram-negative activity including P. aeruginosa; however,
ertapenem does not cover for P. aeruginosa. Te gram-positive spectrum of coverage extends to Enterococcus spp. (except ertapenem),
but only if the Enterococcus strain is sensitive to ampicillin.
Te carbapenems are broad-spectrum antibacterials that should be reserved for directed therapy when more narrow spectrum
antibacterials will not suf ce. Some healthcare institutions have restricted carbapenem use unless approved by an ID specialist.
N
O
OH
H H
O
OH
S
HN
NH
Imipenem Cilastatin
Primaxin = Imipenem + Cilastatin
O
HO
NH
2
S
NH O
OH
O
Carbon instead of sulfur
Carbon instead of sulfur
N
S
N
H
HO
O
O
OH
H
H
H
N
O
OH
O
Ertapenem Aztreonam
N
H
N
O
S
N
H
2
N
O
O
OH
N
S
OH
O
O
O
N
O
H H
O
OH
S
N
S
HO
O
O
H
H
H
N
N
O
Monobactam ring
Figure 14. Carbapenem and Monobactam Chemistry
Integrated Pharmacotherapy 4 Bugs and Drugs 16
Hypersensitivity is a risk with carbapenems, but less so than when compared to penicillins. While most cross-sensitivity data indicates
a low risk for allergy in penicillin-allergic patients, a few reports have claimed as high of a rate as 50%. Most clinicians believe the
actual number to be much lower.
Carbapenems may cause seizures in a dose-dependent manner (higher dose =
greater risk). Tis is believed to be due to blocking GABA receptors in the CNS
(GABA is an inhibitory neurotransmitter that suppresses seizure activity). Tis
risk is less common with ertapenem, and is increased in patients with renal
insuf ciency (due to decreased drug elimination), elderly patients, patients with
a seizure disorder history, or when given with other medications that increase the
risk for seizures.
MONOBACTAMS
Aztreonam is the only monobactam currently marketed in the U.S. Te name
monobactam is the result of aztreonam containing only a -lactam ring in its structure (Figure 14), as opposed to having a second ring
fused to the -lactam ring as the case for each of the previously mentioned b-lactam antibiotics.
Te spectrum of activity for aztreonam is relatively simple: gram-negative aerobic rods (including P. aeruginosa) and nothing else.
Te risk for cross-sensitivity for aztreonam with penicillin-allergic patients is essentially zero. Aztreonam is recommended for the
treatment of aerobic gram-negative infections in patients allergic to -lactams.
Table 4. Summary of Clinically Useful Spectrums of Activity for Carbapenems and Aztreonam
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Cabapenems
(except ertapenem)
+ +
+ only for E. faecalis
sensitive to ampicillin
+ + +
Ertapenem + + + +
Aztreonam + +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
CARBAPENEMS AND MONOBACTAMS
Carbapenems
Doripenem (Doribax) (IV, IM)
Ertapenem (Invanz) (IV, IM)
Imipenem + Cilastatin (Primaxin) (IM, IV)
Meropenem (Merrem) (IV, IM)
Monobactams
Aztreonam (Azactam) (IV, IM)
Integrated Pharmacotherapy 4 Bugs and Drugs 17
Glycopeptides and Lipoglycopeptides
CHEMISTRY
Vancomycin is a natural product consisting of a complex glycolated peptide
structure that is classifed as a glycopeptide. Telavancin, a new antibacterial,
contains glycopeptide chemistry but has additional saturated carbon chain
(lipophilic) chemistry, and it is classifed as a lipoglycopeptide.
Both drugs are too polar and large to be systemically absorbed by oral
administration. Vancomycin is available in an oral formulation only for the
purpose of treating colitis due to C. dif cile overgrowth.
MECHANISM OF ACTION
Like the -lactams, vancomycin and telavancin have a bactericidal efect due
to inhibition of bacterial cell wall synthesis by interfering with peptidoglycan
synthesis. However, their sites of action are diferent than -lactams. Figure 9 on
page 10 shows the steps of bacterial cell wall synthesis inhibited by vancomycin and
telavancin.
Both drugs bind with the D-ALA-D-ALA (D-alanine-D-alanine) dipeptide
that is attached to peptidoglycan precursors (i.e., building blocks for
peptidoglycan). During the transpeptidation (cross-linking catalyzed by
transpeptidases) step of peptidoglycan synthesis, the terminal D-ALA must be
removed. By binding with D-ALA-D-ALA, vancomycin and telavancin block this
step and prevent cross-linking. Telavancin has the addition efect of blocking
peptidoglycan polymerization (the growth of individual peptidoglycan chains).
SPECTRUM OF ACTIVITY
Although vancomycin and telavancin cover many gram-positive organisms,
they do not cover gram-negative bacteria (see Table 5). Tink extensive
gram-positive activity when you hear vancomycin or telavancin. Importantly,
they cover MRSA, penicillin-resistant S. pneumoniae, and Enterococcus
spp. Telavancin also has activity against vancomycin-resistant gram-positive
bacteria.
MECHANISM OF RESISTANCE
Bacteria become resistant to vancomycin by altering the gene that codes for the D-ALA-D-ALA amino acid sequence to code for a
diferent sequence (e.g., D-ALA-D-Lactate) which vancomycin cannot bind with. Tis is a particularly important form of resistance
with Enterococcus spp., resulting in vancomycin-resistant E. faecalis (VRE) and vancomycin-resistant E. faecium (VREF). In recent
years, resistance to vancomcyin in MRSA has emerged by a similar mechanism, and is classifed as either vancomycin-intermediate S.
aureus (VISA) or vancomycin-resistant S. aureus (VRSA).
Telavancin overcomes most forms of vancomycin resistance, although its clinical
utility for VISA and VRSA have yet to be proven in large studies.
Table 5. Summary of Clinically Useful Spectrums of Activity for Vancomycin and Telavancin
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Vancomycin + + + +
Telavancin + + + +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
O
O O
O
O
O
OH
NH
3
+
OH
HO
NH
O
H2
+
N
N
H
H
N
OH HO
H
N
OH
N
H
O
O
HN
O
OH
HO
-
O
O
O
NH
2
O O
Cl
Cl
HO
Telavancin
Vancomycin
Figure 15. Glycopeptide and Lipoglycopeptide Chemistry
GLYCOPEPTIDES AND LIPOGLYCOPEPTIDES
Glycopeptides
Vancomycin (IV)
Vancomycin (Vancocin) (PO)
Lipoglycopeptides
Telavancin (Vibativ) (IV)
Integrated Pharmacotherapy 4 Bugs and Drugs 18
ADVERSE EFFECTS
Vancomycin may cause nephrotoxicity and ototoxicity, both of which are more common when used in combination with
other nephrotoxic and ototoxic drugs (e.g., aminoglycosides). Te use of vancomycin by itself does not usually cuase signifcant
nephrotoxicity or ototoxicity. Renal dosing and blood levels of vancomycin are ofen monitored by pharmacists to prevents these
adverse efects. You will learn about vancomycin pharmacokinetics in a future IP unit. Vancomycin is also associated with infusion-
related adverse efects that may be mistaken for an allergic reaction. Symptoms include pruritis and a red rash on the face and neck
secondary to histamine release. Tis reaction is called "red man" syndrome. To prevent this, up to 500 mg should be administered
over 1 hour and higher doses should be administered as separate 1000 mg infusions over at least 1 hour each.
Telavancin may also cause nephrotoxicity, but pharmacokinetic blood level monitoring is unnecessary with this drug. Telavancin
may prolong the QTc interval (an EKG measurement), which may put patients at risk for cardiac arrhythmias (rare in patients who
do not receive other QTc-prolonging drugs or have preexisting cardiac conduction
abnormalities).
Aminoglycosides
CHEMISTRY
Te aminoglycosides contain linked sugars (glyosides) with amino groups attached
(see Figure 16). Tey are polar and are not absorbed orally. Like vancomycin,
when they are administered orally it is for an antibacterial efect localized in the GI
tract. Oral aminoglycosides are used most commonly for GI decontamination prior
to GI surgery.
MECHANISM OF ACTION
Aminoglycosides are the frst of a series of antibacterial classes presented in these
notes that inhibit bacterial protein synthesis. See Bacterial Protein Synthesis
Inhibition by Antibacterials on page 21 for a review of critical steps in bacterial protein synthesis.
Tere are several proposed mechanisms by which aminoglycosides inhibit bacterial protein synthesis. Aminoglycosides bind to the
30S ribosomal subunit and promote mistranslation of the mRNA template by causing the wrong amino-acyl tRNA to bind in the A site
(i.e., the wrong amino acid will be added to the growing protein chain). Tey also
bind the 50S ribosomal subunit and inhibit the formation of the protein synthesis
initiation complex. Te mistranslation of mRNA results in proteins that are not
functional and toxic to the cell. For example, aminoglycosides cause membrane
proteins to be made that do not maintain cell membrane function, resulting in cell
toxicity. While most bacterial protein synthesis inhibitors are bacteriostatic, the
toxicity induced by the aminoglycosides results in a bactericidal efect.
SPECTRUM OF ACTIVITY
Aminoglycosides must be actively transported into cells, a process that requires
oxygen and a neutral pH. As a result, anaerobic bacteria are inherently resistant
to aminoglycosides due to their low oxygen environment. Terefore, the spectrum of activity is limited to aerobic bacteria. Alone,
aminoglycoside activity is essentially useful only for aerobic gram-negative bacteria, including P. aeruginosa. When combined
with a -lactam or vancomycin, they have synergistic activity against aerobic gram-positive bacteria.
Table 6. Summary of Clinically Useful Spectrums of Activity for Aminoglycosides
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Aminoglycoside alone + +
Aminoglycoside + Cell wall
synthesis inhibitor
+ +
A
+ + + +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
A: Active against MRSA if cell wall synthesis inhibitor is active against MRSA (e.g., vancomycin)
O
O
NH
H
2
N
O
HO
NH
2
NH
2
HO OH
HN
O
Gentamicin
Bacterial enzymes may
acetylate here
Bacterial enzymes may
phosphorylate here
Figure 16. Aminoglycoside Chemistry
AMINOGLYCOSIDES
Amikacin (Amikin)
IM, IV
Gentamicin (Garamycin)
IM, IV
Neomycin (Mycifradin, Neo-fradin)
PO (for GI decontamination prior to surgery)
Tobramycin (Nebcin)
IM, IV
Integrated Pharmacotherapy 4 Bugs and Drugs 19
MECHANISM OF RESISTANCE
Te most common form of bacterial resistance is production of enzymes that acetylate, phosphorylate or adenylate aminoglycosides
(see Figure 16), which inactivates the aminoglycoside (similar to human phase II drug metabolism, except these enzymes are made
by the bacteria). Amikacin is an aminoglycoside that contains an additional side chain which prevents most bacterial enzymes from
binding to it and metabolizing it. Other forms of resistance include alteration of ribosomal binding sites and production of ef ux
pumps that transport aminoglycosides out of the bacteria.
ADVERSE EFFECTS
Aminoglycosides have a black box warning of nephrotoxicity and ototoxicity. Nephrotoxicity from aminoglycosides is dependent
on the amount of time that a patient is exposed to high trough blood levels and ototoxicity is dependent on the peak (Cmax)
concentration (one way to remember is by realizing that your ears are higher than you kidneys). Aminoglycoside kinetics will be
discussed in a future IP unit.
Aminoglycosides may also cause neuromuscular blockade, resulting in
skeletal muscle paralysis. However this is uncommon unless a risk factor is
present (myasthenia gravis, hypomagnesemia, hypocalcemia, concomitant
neuromuscular blockers (an anesthetic)).
Macrolides and Ketolides
CHEMISTRY
Te name macrolide is derived from the large lactone
ring (a cyclic ester) found in these compounds (see
Figure 17). Erythromycin is susceptible to acid-
catalyzed degradation, but clarithromcyin contains
a methyl substitution that prevents acid-catalyzed
degradation and is both better tolerated and absorbed
orally. Azithromycin contains an added methylated
nitrogen in the lactone ring leading to high accumulation
in tissues and a corresponding long half-life (about 3
days) allowing for once-daily dosing.
Ketolides are macrolide analogs in which a cladinose
sugar group is replaced by a ketone. Telithromycin,
the only ketolide currently available, also has a long side
chain substitution. Together these changes result in
increased activity against macrolide-resistant bacteria.
MECHANISM OF ACTION
Macrolides and ketolides bind to the same spot on the
50S bacterial ribosome and inhibit protein synthesis,
halting growth of bacteria and producing a bacteriostatic
efect. Specifcally, they block the translocation step of
protein synthesis (see Figure 20 on page 21).
Table 7. Summary of Clinically Useful Spectrums of Activity for Macrolides and Ketolides
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Erythromycin
Clarithromycin
+ See below +
Azithromycin + See below +
Telithromycin + See below +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
Gram-negative activity: Inactive against most gram-negative rods; active against the respiratory gram-negatives M. catarrhalis and H. infuenzae (erythromycin does
NOT have reliable activity against H. infuenzae)
O
O
O O
OH
O
O
HO N
OR
OH
O
O
OH
Erythromycin R = H
Clarithromycin R = CH
3
(Decreased breakdown by acid)
OR
O
N
O
O
O
O
N
O
HO
OH
OH
OH
O
HO
Azithromycin
Telithromycin
O
O O
HO
N
O
O
O
N
O
H
O
N
N
N
O N
O
H
O
N
N
N
O
Decreases susceptibility
to efux-related and
methylation-related forms
of macrolide resistance
Decreases susceptibility
to efux-related and
methylation-related forms
of macrolide resistance
Figure 17. Macrolide and Ketolide Chemistry
MACROLIDES AND KETOLIDES
Macrolides
Azithromycin (Zithromax) (IV, PO)
Clarithromycin (Biaxin) (PO)
Erythromycin (multiple PO formulations, IV)
Ketolides
Telithromycin (Ketek) (PO)
Integrated Pharmacotherapy 4 Bugs and Drugs 20
SPECTRUM OF ACTIVITY
Te spectrum of activity is similar at frst glance (Table 7 on page 19) among macrolides and ketolides, but ketolides may have activity
against gram-postive bacteria that are resistant to macrolides. Note that macrolides cover streptococci and the atypical organisms,
but their gram-negative activity is limited to only a few organisms and excludes the Enterobacteriaceae. When comparing the
spectrum of activity of macrolides, erythromycin does NOT have reliable activity against H. infuenzae.
MECHANISMS OF RESISTANCE
Tere are two important mechanisms of macrolide resistance. First, methylation of the binding site by methylase enzymes at the 50S
ribosome subunit (specifcally, the 23S portion of the 50S subunit) prevents macrolides from binding to their active site. Te second
important mechanism is production of ef ux proteins that actively transport macrolides out of bacteria. Te chemical changes in
telithromycin make it a poor substrate for these ef ux proteins.
ADVERSE EFFECTS
Gastrointestinal irritation is a common adverse efect of macrolides. Agents should be used with caution in patients with pre-existing
liver disease because worsening liver disease/liver failure may occur. Macrolides may also increase the chance of cardiac arrhythmias
due to prolongation of the QTc interval. Patients at risk for arrhythmia include those with existing QTc interval prolongation,
concomitant use of meds that cause prolongation, uncorrected hypokalemia or hypomagnesemia, or bradycardia (heart rate < 50 bpm).
Telithromycin is associated with several life-threatening adverse efects (acute hepatic failure / severe liver injury and respiratory failure
in patients with myasthenia gravis) that have limited its use and resulted in a required medication guide to be dispensed with each
telithromycin prescription.
Lincosamides
CHEMISTRY AND MECHANISM OF ACTION
Lincomycin is an antibacterial produced in nature that was originally discovered near Lincoln,
NE. It is no longer marketed. Clindamycin (IV, PO) is a chlorinated derivative (see Figure 18)
with greatly improved oral absorption relative to lincomycin.
Clindamycin binds to the same portion of the 50S ribosome as macrolides (the same mechanism
of action) and is bacteriostatic. Because the macrolides bind the same active site, clindamycin
may antagonize the macrolides and the two classes should not be used concomitantly.
SPECTRUM OF ACTIVITY
See Table 8 on page 22. Clindamycin is useful for its activity against MSSA and streptococci. It may have activity against some strains
of community-acquired MRSA (CA-MRSA). It is also active against some weak gram-positive anaerobes (e.g., Peptostreptococcus
spp.), but does not have reliable coverage of the main anaerobe, Bacteroides fragilis.
ADVERSE EFFECTS
Diarrhea is the most common adverse efect, and clindamycin may be associated with a higher rate
of colitis as compared to other antibiotics due to overgrowth of Clostridium dif cile (due to activity
against other gram-positive anaerobes in the gastrointestinal tract).
Streptogramins
CHEMISTRY AND MECHANISM OF ACTION
Quinupristin and dalfopristin are semi-synthetic derviatives of streptogramins produced by
Streptomyces spp. (fungi). Tey are administered in a single combination product (Synercid, IV only)
as a 30:70 (quinupristin:dalfopristin) ratio of molecules because they have synergistic activity. Te use
of this agent has fallen out of favor due to its side efect profle. Quinupristin binds to the same site
on the 50S ribosomal subunit as macrolides, ketolides and clindamycin. Dalfopristin binds allosteric
to the 50S ribosome and changes its conformation such that quinupristin binds with higher af nity
(the source of the synergy). Dalfopristin also inhibits the transpeptidation step of bacterial protein
synthesis (see Bacterial Protein Synthesis Inhibition by Antibacterials on page 21).
SPECTRUM OF ACTIVITY
See Table 8 on page 22. Quinupristin/dalfopristin is active against most clinically important gram-positive aerobes,
including MRSA and penicillin-resistant S. pneumoniae. Teir activity against Enterococcus spp. is divided: they are
active against vancomycin-resistant E. faecium (VREF) but are not active against E. faecalis (regardless of vancomycin
sensitivity). Quinupristin/dalfopristin does not cover any gram-negative bacteria. Quinupristin/dalfopristin is bactericidal for
most sensitive gram-positive bacteria, but it has a bacteriostatic efect on VREF.
O
H
N
N
O
S
OH
HO
HO
Cl
H
Clindamycin
Figure 18. Lincosamide Chemistry
N S
N
O
N
O
N
O
H
N
O
O
NH
O
O
NH
O
N
OH
O
N
Quinupristin
Dalfopristin
O
N
H
OH
O
O
O
N
S
O
O
N
N
O
O
Synercid = Quinupristin + Dalfopristin
Figure 19. Streptogramin Chemistry
Integrated Pharmacotherapy 4 Bugs and Drugs 21
Codons on mRNA template
30S subunit
50S subunit
E P A
E P A
E P A
E P A
E = Exit site P = Peptidyl site A = Aminoacyl site
Growing peptide chain
attached to peptidyl tRNA
Aminoacyl tRNA carries
a new amino acid into
ribosome complex
Aminoacyl tRNA binds in A site
by complimentary base-pairing
Growing peptide chain is
transferred from peptidyl
tRNA to aminoacyl tRNA
tRNA with growing peptide chain
is translocated from A to P site when
ribosome shifts down one codon
Transpeptidation Step
Translocation Step
Former peptidyl tRNA is translocated
from P to E site, where is will be ejected
Aminoglycosides bind with 30S
and cause incorrect tRNA to bind
Tetracyclines bind with 30S
and prevent tRNA from binding
Chloramphenicol binds with 50S
and prevents transpeptidation step
Linezolid and Aminoglycosides
bind 50S and prevent protein
synthesis from beginning (initiating)
Macrolides, Ketolides and Clindamycin
bind to 50S and inhibit translocation step
Quinupristin binds to 50S and inhibit
translocation step (below)
Dalfopristin binds to 50S and enhances
binding of quinupristin and blocks
transpeptidation
Figure 20. Bacterial Protein Synthesis Inhibition by Antibacterials
Integrated Pharmacotherapy 4 Bugs and Drugs 22
MECHANISM OF RESISTANCE
Quinupristin resistance may develop by the same methylation mechanism that
produces macrolide and clindamycin resistance. Dalfopristin resistance occurs by
bacterial enzymatic drug-modifcation and by ef ux pumps.
Oxazolidinones
CHEMISTRY AND MECHANISM OF ACTION
Linezolid (IV, PO) is a synthetic antibacterial and the only member of the
oxazolidinone class currently marketed (see Figure 21). Linezolid binds to the
50S ribosome (see Bacterial Protein Synthesis Inhibition by Antibacterials on page
21) and prevents the initiation of bacterial protein synthesis (bacteriostatic against
Staphylococcus spp., bactericidal against Streptococcus spp.). Linezolid does not
interfere with other antibacterials that bind to the 50S ribosome because it binds to
a unique area within the 50S ribosome (the 23s portion).
SPECTRUM OF ACTIVITY
See Table 8 on page 22. Linezolid is notable for its coverage of resistant gram-
positive organisms, including MRSA, VRE and VREF. It has no coverage of
gram-negative bacteria.
MECHANISM OF RESISTANCE
Resistance to linezolid occurs by alteration of its target site on the 50S ribosome
subunit.
Chloramphenicol
CHEMISTRY AND MECHANISM OF ACTION
Chloramphenicol (IV, PO) is an older naturally-occurring antibacterial that fell
out of favor many years ago due to its adverse efect profle. It binds near the
macrolide, clindamycin and dalfopristin binding site of the 50S ribosome and
prevents the transpeptidation step of bacterial protein synthesis (bacteriostatic).
SPECTRUM OF ACTIVITY
See Table 8 on page 22.
ADVERSE EFFECTS
Chloramphenicol causes reversible dose-dependent suppression of red blood cell
production which may be managed by monitoring blood levels. However, it is also
associated with irreversible aplastic anemia (uncommon, but ofen fatal). It is eliminated by
glucuronidation, a metabolism pathway that is undeveloped early in life. Accordingly, chloramphenicol should be avoided or used at
much lower doses in infants to avoid a fatal accumulation (called gray baby syndrome).
Table 8. Summary of Clinically Useful Spectrums of Activity for Miscellaneous Protein Synthesis Inhibitors
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Clindamycin +
some CA-
MRSA
+
Streptogramins + + + only E. faecium
Linezolid + + +
E. faecalis and E.
faecium
Chloramphenicol + +
E. faecalis and E.
faecium
+ + +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus CA-MRSA = community-acquired methicillin-resistant
Staphylococcus aureus GNR = Gram-negative rod (bacilli)
Clindamycin: Active against some weak gram-positive anaerobes (e.g., Peptostreptococcus spp.)
STREPTOGRAMIN ADVERSE EFFECTS
Arthralgia and Myalgia
Phlebitis
Must be infused via a central intravenous line
Hyperbilirubinemia
LINEZOLID ADVERSE EFFECTS
Myelosuppression
Anemia, thrombocytopenia, leukopenia, pancytopenia
Especially with duration of therapy > 2 weeks
Monitor complete blood count (CBC) weekly
Lactic acidosis
Peripheral and Optic Neuropathy
Especially with duration of therapy > 28 days
Serotonin-syndrome
Due to inhibition of monoamine oxidase (MAO)
Avoid use with SSRIs and MAOIs
Hypertension
Unless can closely monitor blood pressure, avoid use in patients
with uncontrolled hypertension, uncontrolled hyperthyroidism,
concomitant use with vasopressors or dopaminergic agents
N O
N
O
O F
HN
O
Figure 21. Linezolid
N
+
OH
H
N
OH
O
Cl
Cl
O
-
O
Figure 22. Chloramphenicol
Integrated Pharmacotherapy 4 Bugs and Drugs 23
Tetracyclines and Glycylcyclines
CHEMISTRY AND MECHANISM OF ACTION
As their name suggests, tetracyclines are composed of four rings fused
together (see Figure 23). As a class, they are susceptible to acid-
catalyzed degradation, but this is less common with doxycycline and
minocycline resulting in greater oral bioavailability.
Tetracyclines inhibit bacterial protein synthesis and are bacteriostatic.
Specifcally, tetracyclines bind to the 30S ribosomal subunit in the A site
and block the aminoacyl tRNA from carrying in an amino acid to add to
the growing peptide chain.
Glycylcyclines are glycylamido tetracycline derivatives that work by the
same mechanism of action as tetracyclines.
SPECTRUM OF ACTIVITY
See Table 9. Tetracyclines once had a relatively broad spectrum of
activity, but overuse in humans and animals has led to widespread
resistance. Tey are currently most important for their atypical,
MSSA and streptococci coverage. Tetracyclines also cover some
strains of CA-MRSA.
Tigecycline has an extended spectrum of activity relative to
tetracyclines. Of note, it covers Bacteroides spp., MRSA and some
Enterococcus spp. in addition to many gram-positive and gram-
negative bacteria (except for two "P" gram-negative bacteria: Proteus
spp. Pseudomonas spp.).
MECHANISM OF RESISTANCE
Many mechanisms of tetracycline resistance have developed over the years, and
many are inducible by tetracyclines. Examples include alteration of the 30S
binding site, ef ux proteins, and bacteria enzymes that degrade tetracyclines.
Tigecycline is much less susceptible to tetracycline resistance.
ADVERSE EFFECTS
Tetracyclines chelate cations such as magnesium, calcium, aluminum and iron (see Tetracycline Chelation on page 31). In children
chelation of tetracyclines with calcium may lead to permanent discoloration of teeth and bone malformation. For this reason they are
contraindicated in children 8 years old and also in pregnant patients.
Other adverse efects of tetracyclines include light sensitivity (phototoxicity), vertigo and ataxia (mostly with minocycline).
In addition to having adverse efects of the tetracyclines, tigecycline has been associated with hepatic dysfunction and acute
pancreatitis. Also, in phase 3 and 4 clinical trials, an increase in all-cause mortality was observed in patients treated with tigecycline as
compared to other antibiotics. Te manufacturer's website states that "this increase in all-cause mortality should be considered when
selecting among treatment options."
Table 9. Summary of Clinically Useful Spectrums of Activity for Tetracyclines and Glycylcyclines
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Tetracyclines +
only some strains
of CA-MRSA
+ +
A
+
Tigecycline + + +
only
vancomycin-
sensitive E.
faecalis
+ (but NOT
Proteus spp.)
+ +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
A: Activity against some GNR but limited due to increasing resistance rates
Doxycycline
Tigecycline
N
O O
OH
O OH
OH
OH
NH
2
OH
H H
OH O OH O O
NH
2
OH
N
H
N
O
N
H
H H
N
OH
O O
OH
OH OH
OH O OH O
OH
Figure 23. Tetracycline and Glycylcycline Chemistry
TETRACYCLINES & GLYCYLCYCLINES
Tetracyclines
Doxycycline (Vibramycin, Doryx, Monodox) (IV, PO)
Minocycline (Minocin) (PO)
Tetracycline (PO)
Glycylcyclines
Tigecycline (Tygacil) (IV)
Integrated Pharmacotherapy 4 Bugs and Drugs 24
Fluoroquinolones
CHEMISTRY AND MECHANISM OF ACTION
Te fuoroquinolones are a class of synthetic antibacterials characterized by a fuorinated quinolone ring
system (see Figure 24). Teir small molecular size and relatively lipophilic chemistry allows generally
high oral bioavailability and uncomplicated IV formulation and administration. Levofoxacin, a third-
generation agent, is the active S-enantiomer of ofoxacin, a second-generation agent.
Fluoroquinolones inhibit DNA synthesis. During DNA replication the bacterial enzyme DNA gyrase
plays a critical role in the coiling and uncoiling of bacterial DNA. It is analogous to topoisomerase
enzymes in human cells. Proper coiling and uncoiling of DNA is critical to cell replication and
function. Fluoroquinolones inhibit this enzyme and are bactericidal to susceptible bacteria.
FIRST-GENERATION QUINOLONES
Te frst-generation agents were simply quinolones, as they did not contain a fuorine. Tey were only
used for urinary tract infections (UTIs) and are no longer marketed.
SPECTRUM OF ACTIVITY
All Fluoroquinolones
All fuoroquinolones have activity against atypical bacteria and many gram-negative
rods. Tey are distinguished one from another by activity against gram-positive bacteria, P.
aeruginosa, and Bacteroides spp.
Second-Generation Fluoroquinolones
Ciprofoxacin is the most commonly used second-generation fuoroquinolone. While it once had
reliable gram-positive activity, resistance now limits its clinically useful activity to gram-negative
bacteria (see Table 10). Of note, ciprofoxacin has coverage against P. aeruginosa. Perhaps the
one gram-positive organism you may see ciprofoxacin used for is Bacillus anthracis. In terms of
the spectrum of activity you are responsible for, ciprofoxacin predominantly has gram-negative activity, including coverage of P.
aeruginosa.
Third-Generation Fluoroquinolones
Levofoxacin is the most commonly used third-generation fuoroquinolone. It has a
similar gram-negative spectrum of coverage as ciprofoxacin (including P. aeruginosa),
but also has reliable activity against S. pneumoniae and other streptococci. S.
pneumoniae is a common cause of bacterial respiratory infections, and therefore
levofoxacin is also referred to as a "respiratory fuoroquinolone."
Advanced-Generation Fluoroquinolones
Moxifoxacin is the only fuoroquinolone with Bacteroides spp. activity. Like
levofoxacin, advanced-generation fuoroquinolones are also called "respiratory
fuoroquinolones" due to their activity against S. pneumoniae. However, these agents
do not have activity against P. aeruginosa.
MECHANISM OF RESISTANCE
Te common mechanisms of bacteria resistance to fuoroquinolones are: altered structure
of DNA gyrase (decreasing drug binding affinity), production of active efflux transport
pumps, and alteration in porin structure such that fluoroquinolones cannot enter bacteria.
Table 10. Summary of Clinically Useful Spectrums of Activity for Fluoroquinolones
Fluoroquinolone MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Second-generation + + +
Third-generation + + + +
Advanced-generation + +
+ only for
moxifoxacin
+
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
FLUOROQUINOLONES
Second-Generation
Ciprofloxacin (Cipro) (IV, PO)
Ciprofloxacin XR (Proquin) (PO)
Norfloxacin (Noroxin) (PO)
Ofloxacin (Floxin) (IV, PO)
Third-Generation
Levofloxacin (Levaquin, Leva-Pak) (IV, PO)
Advanced-Generation
Gemifloxacin (Factive) (PO)
Moxifloxacin (Avelox) (PO, IV)
Ciprofoxacin
Levofoxacin
N
OH
O
N
HN
O
F
N
O
N
N
O O
F
OH
H
N
O
F
N
O
F
Figure 24. Fluoroquinolone Chemistry
FLUOROQUINOLONES ADVERSE EFFECTS
Try to avoid systemic use in patients < 18 years
Increased risk of musculoskeletal disorders
CNS
Headache, dizziness, CNS abnormalities, seizures
Tendon inflammation and/or rupture
Increased risk in age > 60 yrs, use of corticosteroids, organ
transplant
QTc interval prolongation may place patient at
risk for cardiac arrhythmias
Avoid in patients with myasthenia gravis
Phototoxicity
Hepatotoxicity
Alterations in blood glucose (hypo- or hyperglycemia)
Chelation with multivalent cations (e.g., calcium,
magnesium)
Integrated Pharmacotherapy 4 Bugs and Drugs 25
Antifolates (Sulfamethoxazole and trimethoprim)
CHEMISTRY AND MECHANISM OF ACTION
Sulfamethoxazole (SMX) is a synthetic sulfonamide antibacterial that is only administered
as a combination product (Bactrim, Septra, IV, PO) with trimethoprim (TMP) (other
sulfonamides are available for monotherapy, but will not be discussed here). Te rationale for
this combination is due to the synergistic mechanism of action of these two drugs.
Folate (folic acid) is a required cofactor in the synthesis of thymidine, which is a required
precursor for DNA synthesis. While human cells can utilize dietary folic acid, bacteria
must synthesis their own folate from para-amino benzoic acid (PABA). Sulfamethoxazole
inhibits an key enzyme in the conversion of para-amino benzoic acid to folate (see Figure
25). Sulfamethoxazole (and all other sulfamide antibacterials) mimics PABA (red highlight
in Figure 26), and competes for binding at the enzymes active sites. Trimethoprim inhibits
bacterial dihydrofolate reductase (DHFR), preventing necessary reduction of folate (see Figure
25). Note that this is the same enzyme targeted by the anticancer drug methotrexate, but
trimethoprim is selective for the bacterial version of DHFR. Trimethoprim contains structural
portions of folate, allowing it to compete against folate for binding at DHFR (blue highlight in
Figure 26).
TMP and SMX alone are bacteriostatic drugs, but the combination of TMP/SMX has synergistic
activity on inhibition of bacteria DNA synthesis and usually results in bactericidal activity.
SPECTRUM OF ACTIVITY
See Table 11 on page 26. SMX-TMP is particularly useful for activity against E. coli in the management of UTIs. Recently it has
emerged as a useful option for management of CA-MRSA.
MECHANISM OF RESISTANCE
Resistance to TMP-SMX develops by:
decreased permeability of the bacterial cell membrane to TMP
and SMX.
or
by overproduction of the enzyme targets of TMP and SMX, such
that the drugs cannot inhibit enough activity to inhibit DNA
synthesis.
ADVERSE EFFECTS
Similar to penicillins, allergic reactions (hypersensitivity) to
sulfonamides are common. While this is usually referred to as a
"sulfa" allergy in practice, it is actually due to a sulfonamide chemical
group, not simply a sulphur atom or a sulfa group (green highlight
in Figure 26). A rash is most common, but the efect can progress
to life-threatening skin reactions such as Stevens-Johnson syndrome
(rare).
Sulfonamides may precipitate in acidic environments (ofen times in
urine). Dilution of urine minimizes this risk and patients should be
counseled to drink plenty of water (at least a full glass with each oral
dose).
Bone marrow suppression (uncommon) is due to TMP inhibition
of human DHFR at higher doses in some patients (loss of bacterial
DHFR selectivity).
PABA
Folate
Tetrahydrofolate
Synthesis of Thymidine
DNA Synthesis
Dihydropteroate
Synthetase
Dihydrofolate
Reductase
SMX
-
TMP
-
Figure 25. TMP/SMX Mechanism of Action
Folic Acid
Sulfamethoxazole
Trimethoprim
OH
N
N
N
N
H
2
N
HN
HN
O
OH
O
HO
N
O
NH S
O
O
H
2
N
N
N H
2
N
NH
2
O
O
O
N
N H
2
N
N
N
H
2
N
HN
H
2
N NH S
O
O
Sulfonamide
Group
Figure 26. Antifolate Chemistry
Integrated Pharmacotherapy 4 Bugs and Drugs 26
Nitroimidazoles
CHEMISTRY AND MECHANISM OF ACTION
Nitroimidazoles are small synthetic antibacterials that contain a nitro group attached to a substituted imidazole ring (red highlight in
Figure 27). Metronidazole (Flagyl, IV, PO) is the most commonly used nitroimidazole and is the only agent that will be covered here.
Metronidazole is a prodrug and must be activated by nitroreductase enzymes found in anaerobic bacteria. Tese enzymes allow
anaerobic bacteria to utilized nitrogen sources instead of oxygen to sustain life. Once reduced by nitroreductase, metronidazole
induces DNA damage (e.g., strand breaks) through an unknown mechanism and is
bactericidal. Bacteria that do not rely upon nitroreductases to sustain life are not susceptible to
metronidazole.
SPECTRUM OF ACTIVITY
See Table 11 on page 26. Metronidazole is active against nearly all anaerobic bacteria, including
Clostridium dif cile, as well as anaerobic parasites. When you hear metronidazole, think
anaerobic coverage.
MECHANISM OF RESISTANCE
Resistance to metronidazole is uncommon. When it occurs, it is most ofen due to a defciency in
nitroreductase activation of metronidazole.
ADVERSE EFFECTS
Metronidazole may cause several CNS-related adverse efects, including headache, peripheral
neuropathy and seizures (more likely with pre-existing seizure risk or hepatic dysfunction due to
hepatic elimination). Metronidazole also has three interesting adverse efects that patients need to be warned about prior to therapy:
a metallic taste, discoloration of urine to a dark color, and has a similar reaction with ethanol as is known for disulfiram (Antabuse)
(including the small amount of ethanol found in cough syrups) (see Antibacterials:
Common Drug-Drug Interactions on page 31).
Rifampin
CHEMISTRY AND MECHANISM OF ACTION
Rifampin is a rifamycin, a family of naturally occurring (from a Streptomyces spp.)
antibacterials with large ring systems (see Figure 28).
Te rifamycins target DNA-dependent RNA polymerase. DNA-dependent RNA
polymerase is an enzyme that uses DNA as a code to synthesize RNA, which is
subsequently used as a code (mRNA) for the synthesis of proteins. Both eukaryotic
(e.g., humans) cells and prokaryotic (bacteria) cells have this enzyme. However, the
prokaryotic form of this polymerase is diferent enough from the eukaryotic form
that drugs are selective for the bacterial enzyme. Inhibition of bacterial DNA-dependent RNA polymerase, prevents the synthesis
of RNA, which in turn prevents the expression of genes and gene products (proteins), arresting cell growth in susceptible bacteria (a
bacteriostatic or bactericidal efect, depending on the drug concentration).
Table 11. Summary of Clinically Useful Spectrums of Activity for Other Antibacterials Toxic to Nucleic Acids
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Metronidazole +
TMP-SMX + +
A
+
B
+
Rifampin +
C
+
C
+
C
Nitrofurantoin +
D
+
D
+
D
+
D
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
A: Activity against community-acquired MRSA (CA-MRSA) B: Does NOT include S. pyogenes
C: Clinically useful activity against gram-positive bacteria when used in synergy with other antibacterials with gram-positive activity (especially Staphylococcus spp.)
(also active against Mycobacterium tuberculosis)
D: Due to rapid elimination into urine, only useful against urinary tract pathogens such as E. coli, Staphylococcus saprophyticus, Enterococcus spp.
Metronidazole
Active form of metronidazole
N
N
OH
N
+
-
O
O
N
N
N
+
-
O
O
Nitroreductase
Figure 27. Metronidazole Activation
NH
OH
HO
O
O
O
O
OH OH
O
OH
O
O
N
N
N
Figure 28. Rifampin
Integrated Pharmacotherapy 4 Bugs and Drugs 27
SPECTRUM OF ACTIVITY
Rifampin is not used alone for treatment of bacterial infections due to rapid
development of resistance. Instead, it may be combined with other antibacterials
active against gram-positive bacteria for a synergistic efect. It also has activity
against Neisseria spp. and may be used by itself for meningitis prophylaxis during
an epidemic known to be caused by N. meningitidis.
Te rifamycins are also useful for treatment of mycobacterial infections (e.g.,
tuberculosis), though this topic will be addressed in a separate TBL packet and facilitated later in the
curriculum.
MECHANISM OF RESISTANCE
Resistance is due to mutations in the bacterial DNA-dependent RNA polymerase, resulting in a
decrease or total loss of rifampin binding af nity.
Nitrofurantoin
CHEMISTRY AND MECHANISM OF ACTION
Nitrofurantoin (Macrobid, PO) is a synthetic nitrofuran drug (a drug with a nitro
group attached to a furan ring (red highlight in Figure 299). Nitrofurantoin is reduced
inside of bacteria by enzymes called nitrofuran reductases (do not confuse this enzyme
with nitroreductases that reduce metronidazole) to metabolites that are toxic to DNA
(bactericidal).
SPECTRUM OF ACTIVITY
Te spectrum of activity for nitrofurantoin is only relevant in the context of urinary tract bacterial pathogens. Tis is because
nitrofurnatoin has a very short elimination half-life (20 - 30 minutes in most patients) once it is absorbed, and does not accumulate
in other body tissues enough to fght infection. Nitrofurantoin should only be used in patients with a CrCl > 60 mL/min to allow for
a signifcant concentration of drug at site of action. In the urinary tract, nitrofurantoin is active against several urinary pathogens,
including E. coli, S. saprophyticus and Enterococcus spp.
MECHANISM OF RESISTANCE : Nitrofurantoin resistance is uncommon, and is due to a lack in production of the enzymes that activate
(reduce) the drug.
Cyclic Lipopeptide
CHEMISTRY AND MECHANISM OF ACTION
Daptomycin (Cubicin, IV) is a cyclic lipopeptide drug, meaning that it consists of a large cyclic peptide structure with lipophilic side
chains. Daptomycin binds to the cell membrane of bacteria and causes excessive depolarization, which interrupts DNA, RNA and
protein synthesis (bactericidal).
SPECTRUM OF ACTIVITY
See Table 12. Like vancomycin and telavancin, daptomycin is active against
many gram-positive bacteria, but it is not active against gram-negative
bacteria. Of note, its spectrum of activity includes coverage of MRSA. Tis
agent should never be used for the treatment of pneumonia caused by any
microorganism as it is inactivated by pulmonary surfactant.
ADVERSE EFFECTS
Daptomycin is associated with increased creatinine phosphokinase (CPK),
which may be indicative of muscle injury that could lead to myopathy. Te
risk for myopathy is higher when taken concomitant with statins (please review statin side efects from IP 3 Dyslipidemia if you do
understand why). To monitor, the CPK level should be measured weekly in daptomycin patients.
Daptomycin may also cause symptoms of peripheral neuropathy or eosinophilic pneumonia (rare).
N
N
O
NH
O
O
N
+
O
-
O
O
N
+
O
-
O
Figure 29. Nitrofurantoin
NITROFURANTOIN ADVERSE EFFECTS
Brown or orange discoloration of urine
Hemolytic anemia in patients with glucose-6-
phosphate dehydrogenase (G6PD) deficiency
Rare but serious side effects:
Pulmonary toxicity
Hepatotoxicity
Peripheral neuropathy
RIFAMPIN ADVERSE EFFECTS
Red or orange discoloration of body excretions (tears, urine,
saliva, sweat) which may permanently discolor clothing and
contacts
Hepatotoxicity
Potent CYP inducer, causing many drug interactions
Table 12. Summary of Clinically Useful Spectrums of Activity for Daptomycin and Colistin
Antibacterial MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Daptomycin + + + +
Colistin + +
MSSA = Methicillin-sensitive Staphylococcus aureus MRSA = Methicillin-resistant Staphylococcus aureus GNR = Gram-negative rod (bacilli)
Figure 30. Daptomycin
Integrated Pharmacotherapy 4 Bugs and Drugs 28
Colistimethate (Colistin)
CHEMISTRY AND MECHANISM OF ACTION
Colistimethate (Coly-Mycin M, IV, IM) (Figure 31) is a naturally produced polymyxin antibacterial, and is also known as polymyxin
E (polymyxin B is a common ingredient in OTC topical antibacterial preparations). Polymyxins act as cationic detergents in the cell
membrane of bacteria, where binding of cell membrane bound phosphates damages portions of the membrane and results in a leaky
cell membrane (bactericidal).
SPECTRUM OF ACTIVITY
See Table 12 on page 27. Colistimethate is active only against gram-
negative aerobes. Due to its toxicity, it is reserved for resistant
Pseudomonas spp. or resistant Acinetobacter spp. infections.
ADVERSE EFFECTS
Te major toxicity that limits colistimethate use is nephrotoxicity.
Figure 31. Colistimethate
Integrated Pharmacotherapy 4 Bugs and Drugs 29
ANTIBACTERIALS: PHARMACOKINETIC CONSIDERATIONS
When selecting appropriate antibacterial therapy, the spectrum of activity is only one of several considerations. An antibacterial may
have a great spectrum of activity against the bacteria causing an infection, but if the antibacterial does not reach the site of infection
then it is useless. Pharmacokinetics describe the movement of a drug into and out of the body. Since infections are usually not spread
throughout the body, but are localized to specifc areas, pharmacokinetics is an important consideration when choosing and evaluating
antibacterial therapy.
Drug Delivery and Absorption
Some antibacterials simply do not have a high enough oral bioavailability to be useful when taken orally. Tis is usually a result of
high drug polarity and/or large molecular size that limits absorption rather than a high frst-pass efect. In this case, to achieve a
systemic efect the antibacterial must be given through another route (most ofen parenteral injection). If the site of action is only the
gastrointestinal tract, then poorly absorbed drugs may be given orally.
Drug Distribution
Following administration, will an antibacterial distribute to the infection site and achieve high enough concentration at the site to be
efective? Tis is an important consideration for antibacterial therapy.
Drug Elimination
ANTIBACTERIAL CLASSES ELIMINATED PRIMARILY UNCHANGED BY THE KIDNEYS
Drugs that are eliminated mostly unchanged by the kidneys usually aren't
eliminated as well from the body in patients with renal insuf ciency. Tis is a
result of the body not being able to eliminate these drugs by an alternate pathway
if the kidneys aren't functioning well. Tis may result in the need to decrease
the dose to account for decreased renal elimination. What would you expect
to happen to the following PK parameters during renal insuf ciency for a drug
cleared mostly unchanged by the kidneys?
elimination half-life
concentration of drug in the blood and other body tissues
AUC
Te adjustment of a drug dose based on decreased renal function is frequently
called "renal dosing". Te dose is most ofen adjusted based on the estimated creatinine clearance. Antibacterials that are likely to
require renal dosing adjustments are listed in the box to the right.
ANTIBACTERIAL CLASSES ELIMINATED PRIMARILY BY HEPATIC METABOLISM
Antibacterials that are eliminated mostly by hepatic metabolism most likely
will not need renal dose adjustments. However, caution with high doses is
encouraged in patients with hepatic dysfunction. Additionally, antibacterials
that undergo extensive hepatic metabolism may be more prone to be involved
with drug metabolism-related drug-drug interactions. Antibacterials that are
eliminated primarily by the liver are listed to the right.
ANTIBACTERIAL THAT REQUIRE RENAL DOSING
aminoglycosides
colistimethate
daptomycin
fluoroquinolones (except moxifloxacin)
most -lactams (exceptions include ceftriaxone and
penicillinase-resistant penicillins)
tmp/smx
telavancin
vancomycin
ANTIBACTERIALS ELIMINATED BY THE LIVER
clindamycin
glycylcyclines and tetracyclines
ketolides and macrolides
linezolid
metronidazole
moxifloxacin
rifampin (potent CYP3A4 inducer!)
streptogramins
Integrated Pharmacotherapy 4 Bugs and Drugs 30
ANTIBACTERIALS: PHARMACODYNAMIC CONSIDERATIONS
Concentration-Dependent versus Concentration-Independent Activity
Te type of activity that an antibacterial agent displays can be classifed as concentration-dependent versus concentration-independent
(also known as time-dependent) activity. Diferences are discussed in Table 13 and graphically depicted in (Figure 32).
Post-Antibiotic Efect
Te post-antibiotic efect (PAE)
is the persistent suppression of
bacterial growth afer exposure to
the antibiotic has ceased. Te exact
mechanism is unknown. Tink of
the PAE as being similar to part of
the arcade game Pac-Man at one
point in the game, the ghosts are
not killed, but they shake a little
bit as they are made incapacitated.
Tis is the PAE the organism is
not killed, but it cant grow for a
period of time. Aminoglycosides
have been shown to have a PAE of
2 to 6 hours against Gram-negative
organisms.
Synergy and Antagonism
Pharmacodynamic interactions include the concepts
of synergy and antagonism. Synergy means that the
combined efect of 2 agents is greater than the sum of
their individual efects when measured separately, i.e. 2 +
2 = 5. An antibacterial example of this is that individually,
trimethoprim is bacteriostatic and sulfamethoxazole
is bacteriostatic; however, the combination drug
trimethoprim/sulfamethoxazole (Bactrim, Septra) is
bactericidal. Another example is that the combination
of a cell-wall active agent with an aminoglycoside is
bactericidal against Enterococcus spp. Antagonism
means that the activity of the combination of 2 agents
results in an efect that is less than their individual efects,
i.e. 2 + 2 = 3. Tis may occur if the clinician uses 2 antibacterial agents with the same target site of action (for example, using 2 agents
that target the 50S ribosomal subunit at the same time.) Te concepts of synergy and antagonism will be discussed in further detail in
future IP units.
Dosing Concepts
ONCE-DAILY DOSING VERSUS MULTIPLE DOSING
Antibacterials that are efective with only once-daily dosing ofer several advantages:
increased patient adherence to therapy (once-daily is easier to remember than multiple daily doses)
decreased administration costs for IV drug delivery (nursing + administration material costs are higher with multiple daily dosing)
Cefriaxone, a third-generation IV cephalosporin with a relatively long half-life, is most ofen administered once-daily. Tis partly
explains why cefriaxone is such a popular antibacterial. Azithromycin has an elimination half-life of about 3 days, and 5 days of once-
daily oral therapy results in about 10 days of antibacterial therapy due to drug accumulation. Tis is an attractive alternative to other
macrolides that require multiple daily dosing.
Table 13. Concentration-dependent versus concentration-independent activity
Concentration-dependent activity
Concentration-independent (time-
dependent) activity
Type of activity
Rate and extent of bacterial killing is
dependent upon the extent that the
peak drug concentration is > the MIC, or
the peak:MIC ratio
Extent of activity / killing depends upon
the length of time that the active drug
concentration is > the MIC; time > MIC should
be 40% to 60% of the dosing interval
Considerations for
dosing
Supports infrequent, high dosing
Supports frequent doses or a prolonged /
continuous infusion#
Example agents
Aminoglycosides, daptomycin,
telavancin, fuoroquinolones*
Vancomycin, penicillins, cephalosporins,
carbapenems, clindamycin, macrolides,
linezolid, tetracyclines
*For the fuoroquinolone class of antibiotics, the AUC to MIC ratio (which is the AUIC) has been shown to predict clinical
response. It is recommended to target an AUIC 125 for Gram-negative organisms and an AUIC 30 for Gram-positives.
This is mostly used in clinical trials and research, as routine, multiple blood levels of drug are not routinely drawn in
clinical practice to calculate a patients AUC.
#continuous infusions being used more commonly in clinical practice for select beta-lactams
Figure 32. Peak, AUC, and MIC Measurement
Integrated Pharmacotherapy 4 Bugs and Drugs 31
ANTIBACTERIALS: COMMON DRUG-DRUG INTERACTIONS
Antibacterials and Warfarin
Any antibacterial agent given in combination with warfarin (an oral anticoagulant), will result in
increased activity of warfarin. Tis is because bacteria found in the GI tract normally produce small
amounts of vitamin K (which has clotting activity- the opposite efect of warfarin.) Antibacterials
eliminate some of these gut bacteria, resulting in decreased production of vitamin K, and enhanced
activity of warfarin.
INTERRUPTION OF ORAL CONTRACEPTIVE ENTEROHEPATIC RECYCLING
Tere are also bacteria in the gut that cause enterohepatic recycling of oral contraceptives, particularly
products containing ethinyl estradiol. Tere is a subset of women in whom this enterohepatic recycling
plays an important role in maintaining adequate drug levels of contraceptive. It is currently not feasible
to identify this subset of women, so all women should be counseled to use barrier contraception or
avoid intercourse while taking antibiotics and for 7 days afer completion of a course of therapy.
T w o T et r ac y c l i n e M o l ec u l es ( A c t i v e)
O H O O H
O H
O
C O N H
2
O H
N ( C H
3
)
2
H H O C H
3
Met al C at i on
C a
+2
, A l
+2
, M g
+2
F e
+2
, F e
+3
O H O O
H O
O
C O N H
2
H O
N ( C H
3
)
2
H O H H
3
C
O H O O
O H
O
C O N H
2
O H
N ( C H
3
)
2
H H O C H
3
M
C h el at ed T et r ac y c l i n es
( I n ac t i v e, P o o r l y A b s o r b ed )
(M)
Figure 33. Tetracycline Chelation
Table 14. Select Major Drug-Drug Interactions with Antibacterials
Antibacterial Class Other Drug(s) Notes
Penicillins Probenecid
A
Blocks renal excretion of antibiotic causing
increased levels
A
Vancomycin Nephrotoxins
Ototoxins
Additive adverse efects
Aminoglycosides Neuromuscular blockers
Nephrotoxins
Ototoxins
Additive adverse efects
Macrolides Class Ia and Class III antiarrhythmics Try to avoid may cause arrhythmia
Linezolid Any serotonergic drugs (e.g., many
antidepressants)
Vasopressors, dopaminergic agents
Possible serotonin-syndrome
Hypertension
Tetracyclines Chelation with multivalent cations (antacids,
iron, zinc, dairy) (see Figure 333)
Must separate to achieve active
antibacterial levels
Fluoroquinolones Chelation with multivalent cations (antacids,
iron, zinc, dairy)
Class Ia and Class III antiarrhythmics
Corticosteroids
Must separate to achieve active
antibacterial levels
Try to avoid may cause arrhythmia
Try to avoid may cause tendon rupture
TMP/SMX Warfarin Antibiotic displaces warfarin from protein
causing increased warfarin levels
Metronidazole Ethanol and drugs-containing ethanol
Warfarin
Disulfram-like reaction
Antibiotic displaces warfarin from protein
causing increased warfarin levels
A: Penicillin used to be prescribed with probenecid to decrease amount of penicillin needed to treat infections
Integrated Pharmacotherapy 4 Bugs and Drugs 32
REFERENCES
1. Alvarez-Elcoro S, Enzler M. The Macrolides: erythromycin, clarithromycin, and azithromycin. Mayo Clin Proc. 1999;74:613-34.
2. Basic and Clinical Pharmacology 11th edition
3. Centers for Disease Control and Prevention. Antibiotic / Antimicrobial Resistance. Available at: http://www.cdc.gov/drugresistance/index.html. Accessed 5
April 2013.
4. DePestel D, Benninger M, Danziger L, et al. Cephalosporin use in treatment of patients with penicillin allergies. J Am Pharm Assoc. 2008;48:530-40.
5. Doron S, Davidson L. Antimicrobial stewardship. Mayo Clin Proc. 2011;86:1113-23.
6. Edson R, Terrell C. The Aminoglycosides. Mayo Clin Proc. 1999;74:519-28.
7. Foye's Principles of Medicinal Chemistry 6th edition
8. Gruchalla R, Pirmohamed M. Antibiotic allergy. New Engl J Med. 2006;354:601-9.
9. Hellinger W, Brewer N. Carbapenems and monobactams: imipenem, meropenem, and aztreonam. Mayo Clin Proc. 1999;74:420-34.
10. Gilbert D, Moellering R, Eliopoulos G, Sande M, eds. The Sanford Guide to Antimicrobial Therapy, 40th Ed. Sperryville, VA: Antimicrobial Therapy, Inc.; 2010.
11. Goodman and Gilman's The Pharmacological Basis of Therapeutics 11th edition
12. Kanj S, Kanafani Z. Current concepts in antimicrobial therapy against resistant Gram-negative organisms: extended-spectrum -lactamase-producing
Enterobacteriaceae, carbapenem-resistant enterobacteriaceae, and multidrug-resistant Pseudomonas aeruginosa. Mayo Clin Proc. 2011;86:250-9.
13. Kasten M. Clindamycin, metronidazole, and chloramphenicol. Mayo Clin Proc. 1999;74:825-33.
14. Kelkar P, Li J. Cephalosporin allergy. New Engl J Med. 2001;345:804-9.
15. Lexi-Comp, Inc. (Lexi-Drugs). Lexi-Comp, Inc.; April 5, 2013.
16. Marshall W, Blair J. The Cephalosporins. Mayo Clin Proc. 1999;74:187-95.
17. Mehlhorn (Sucher) A, Chahine E, Butcher A. Antimicrobial resistance among community pathogens. Drug Topics. 2008;152:64-73.
18. Mulvey M, Simor A. Antimicrobial resistance in hospital's: How concerned should we be? CMAJ. 2009;180:408-15.
19. Nicolau D, Freeman C, Belliveau P, et al. Experience with once-daily aminoglycoside program administered to 2184 adult patients. Antimicrob Agents
Chemother. 1995;39:650-55.
20. ODonnell J, Gelone S. Fluoroquinolones. ID Clin of No Amer. 2000;14:489-513.
21. Prescott W, DePestel D, Ellis J, et al. Incidence of carbapenem-associated allergic-type reactions among patients with versus patients without a reported
penicillin allergy. Clin Infect Dis. 2004;38:1102-7.
22. Rang & Dales Pharmacology 6th edition
23. Rice L, Mechanisms of resistance and clinical relevance of resistance to -lactams, glycopeptides, and fuoroquinolones. Mayo Clin Proc. 2012;87:198-208.
24. Rivera A, Boucher H. Current concepts in antimicrobial therapy against select Gram-positive organisms: methicillin-resistant Staphylococcus aureus, penicillin-
resistant pneumococci, and vancomycin-resistant enterococci. Mayo Clin Proc. 2011;86:1230-42.
25. Smilack J. The Tetracyclines. Mayo Clin Proc. 1999;74:727-29.
26. Smilack J. Trimethoprim-sulfamethoxazole. Mayo Clin Proc. 1999;74:730-34.
27. Sucher A, Sucher B, Randall C. Update on upper respiratory tract infections. Drug Topics. 2010;154:28-37.
28. Sunenshine R, McDonald L. Clostridium dif cile-associated disease: New challenges from an established pathogen. Cleve Clin J Med. 2006;73:187-9.
29. Walker R. The Fluoroquinolones. Mayo Clin Proc. 1999;74:1030-37.
30. Weisberg E. Interactions between oral contraceptives and antifungals/antibacterials: is contraceptive failure the result? Clin Pharmacokinet 1999;36:309-13.
31. Wilhelm M, Estes L. Vancomycin. Mayo Clin Proc. 1999;74:928-35.
32. Wilson and Gisvold's Textbook of Organic Medicinal and Pharmaceutical Chemistry 11th edition
33. Wright A. The Penicillins. Mayo Clin Proc. 1999;74:290-307.
Integrated Pharmacotherapy 4 Bugs and Drugs 33
SPECTRUM OF ACTIVITY PRACTICE TABLE
Tis table is provided to you as a study resource. Prior to the RAT test yourself on your spectrum of activity skill.
Impress your family, friends, and pets with your superior ID knowledge!
Penicillin Class MSSA MRSA Streptococci Enterococci GNR P. aeruginosa Bacteroides Atypicals
Natural Penicillins
Penicillinase-Resistant
Aminopenicillins
Antipseudomonal
-Lactamase Inhibitor
Combinations
1st-Gen Cephalosporins
2nd-Gen Cephalosporins
3rd-Gen Cephalosporins
4th-Gen Cephalosporins
5th-Gen Cephalosporin
Carbapenems (not ertapenem)
Ertapenem
Aztreonam
Vancomycin
Telavancin
Aminoglycosides
Macrolides
Ketolides
Clindamycin
Streptogramins
Linezolid
Chloramphenicol
Streptogramines
Tetracyclines
Glycylcyclines
Fluoroquinolones
TMP/TMX
Metronidazole
Rifampin
Nitrofurantoin
Daptomycin
Colistimethate
Potrebbero piacerti anche
- Top 300 Drugs PDFDocumento31 pagineTop 300 Drugs PDFVin Bitz100% (1)
- Clinical Performance Evaluation → Asthma ACR-DIDDocumento1 paginaClinical Performance Evaluation → Asthma ACR-DIDveronica100% (1)
- Top 300 Drugs Pocket Reference Guide (2021 Edition)Da EverandTop 300 Drugs Pocket Reference Guide (2021 Edition)Valutazione: 5 su 5 stelle5/5 (1)
- Rxexam'S Biostatistics Questions & Answers: 2019-2020 EditionDocumento15 pagineRxexam'S Biostatistics Questions & Answers: 2019-2020 EditionPrakash100% (2)
- NAPLEX Prep 2018 Ch01 CardioDocumento56 pagineNAPLEX Prep 2018 Ch01 CardioFaith50% (2)
- 2019 NAPLEX and MPJE Review MaterialsPDFDocumento7 pagine2019 NAPLEX and MPJE Review MaterialsPDFsara0% (2)
- Infectious Diseases IDocumento7 pagineInfectious Diseases ITiff VoNessuna valutazione finora
- Antiplatelet and anticoagulant drug comparison chartDocumento10 pagineAntiplatelet and anticoagulant drug comparison chartDrashtibahen PatelNessuna valutazione finora
- MULTISTATE PHARMACY JURISPRUDENCE EXAMINATION (MPJE): Passbooks Study GuideDa EverandMULTISTATE PHARMACY JURISPRUDENCE EXAMINATION (MPJE): Passbooks Study GuideNessuna valutazione finora
- North American Pharmacist Licensure Examination (NAPLEX) Study GuideDocumento20 pagineNorth American Pharmacist Licensure Examination (NAPLEX) Study GuideMcRee Learning CenterNessuna valutazione finora
- Science of Happiness Paper 1Documento5 pagineScience of Happiness Paper 1Palak PatelNessuna valutazione finora
- Chapter 32 - Pulmonary Arterial HypertensionDocumento3 pagineChapter 32 - Pulmonary Arterial HypertensionDrashtibahen PatelNessuna valutazione finora
- Top 200 Drug ExamDocumento1 paginaTop 200 Drug ExamUyen V. NguyenNessuna valutazione finora
- Top-200-Drug ETSYDocumento31 pagineTop-200-Drug ETSYBetsy Brown ByersmithNessuna valutazione finora
- Brand Generic Class Other: NAPLEX ReviewDocumento72 pagineBrand Generic Class Other: NAPLEX Reviewbapimirab654Nessuna valutazione finora
- Chemotherapy NDocumento28 pagineChemotherapy NFaisal MehboobNessuna valutazione finora
- Quizlet PracticeDocumento23 pagineQuizlet Practicetohomas100% (1)
- Pharmacy Law & Ethics Regulations StandardsDocumento62 paginePharmacy Law & Ethics Regulations Standardsaberhaneth1163Nessuna valutazione finora
- Chapter 35 AsthmaDocumento4 pagineChapter 35 AsthmaDrashtibahen PatelNessuna valutazione finora
- Drug of Choice and First Line of TreatmentDocumento2 pagineDrug of Choice and First Line of Treatmentprinz1mendezNessuna valutazione finora
- (DownSub - Com) Pharmacology - PHARMACOKINETICS (MADE EASY)Documento8 pagine(DownSub - Com) Pharmacology - PHARMACOKINETICS (MADE EASY)Stephen VuelbanNessuna valutazione finora
- Chapter 18 Common Drugs PDFDocumento221 pagineChapter 18 Common Drugs PDFlalallalaNessuna valutazione finora
- Penicinillase - Sensible: Inhibit Clasification AntibioticsDocumento1 paginaPenicinillase - Sensible: Inhibit Clasification AntibioticsАндрій ДанильцівNessuna valutazione finora
- Pharmacist's Letter: Prescriber's LetterDocumento6 paginePharmacist's Letter: Prescriber's LetterJaved AkhtarNessuna valutazione finora
- PERIOPERATIVE ANTIBIOTICS AND MENINGITIS GUIDELINESDocumento10 paginePERIOPERATIVE ANTIBIOTICS AND MENINGITIS GUIDELINESDrashtibahen PatelNessuna valutazione finora
- M. Pharm Review NAPLEX36Documento1 paginaM. Pharm Review NAPLEX36JUSASBNessuna valutazione finora
- Northern Ireland Management of Infection Guidelines For Primary and Community Care 2016Documento48 pagineNorthern Ireland Management of Infection Guidelines For Primary and Community Care 2016dreneavalentinstefanNessuna valutazione finora
- 9535103899ClinicalApplicationsPharmacogenetics PDFDocumento304 pagine9535103899ClinicalApplicationsPharmacogenetics PDFAnonymous nFeOeX4Nessuna valutazione finora
- Class Medication MOA Side Effects: Intranasal SteroidsDocumento2 pagineClass Medication MOA Side Effects: Intranasal SteroidsChron MedNessuna valutazione finora
- OTC Exam 2 Study GuideDocumento32 pagineOTC Exam 2 Study GuideDave WinNessuna valutazione finora
- Pharmacy Law Final Study GuideDocumento21 paginePharmacy Law Final Study Guidetohomas100% (1)
- Brad Hinton CVDocumento6 pagineBrad Hinton CVapi-486072801Nessuna valutazione finora
- 2006 Info For MpjeDocumento28 pagine2006 Info For Mpjemina75% (4)
- Licensing and Compliance Requirements for Pharmacy OperationsDocumento5 pagineLicensing and Compliance Requirements for Pharmacy OperationsHitomi Shiroshita100% (1)
- Pharmaceutical Calculation Volume 2Documento4 paginePharmaceutical Calculation Volume 2Tony AnsahNessuna valutazione finora
- M. Pharm Review NAPLEX32Documento1 paginaM. Pharm Review NAPLEX32JUSASBNessuna valutazione finora
- Naplex 1Documento7 pagineNaplex 1baniyoNessuna valutazione finora
- Federal LawDocumento13 pagineFederal Lawmihir1188Nessuna valutazione finora
- PK Equations To Know For NaplexDocumento1 paginaPK Equations To Know For NaplexNasru DiinNessuna valutazione finora
- Naplex NotesDocumento226 pagineNaplex NotesløzanNessuna valutazione finora
- M. Pharm Review NAPLEX28Documento1 paginaM. Pharm Review NAPLEX28JUSASBNessuna valutazione finora
- Apha Naplex PDFDocumento408 pagineApha Naplex PDFsweetNessuna valutazione finora
- IV PO Conversion CAPDocumento3 pagineIV PO Conversion CAPdamondouglasNessuna valutazione finora
- AntibioticsDocumento4 pagineAntibioticsTan Geok Eng100% (1)
- Classification of major antibiotic classes and examplesDocumento1 paginaClassification of major antibiotic classes and examplesSY WongNessuna valutazione finora
- APHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDocumento13 pagineAPHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDrSamia El WakilNessuna valutazione finora
- TPN CalculationDocumento3 pagineTPN CalculationSARANYANessuna valutazione finora
- Naplex MpjeDocumento35 pagineNaplex MpjeAtlantis ManNessuna valutazione finora
- Vancomycin Pharmacology Indications, Mechanism, and Side Effects! PDFDocumento1 paginaVancomycin Pharmacology Indications, Mechanism, and Side Effects! PDFFrancis PasayNessuna valutazione finora
- Total Pharmacy Notes TPN For EEDocumento1.601 pagineTotal Pharmacy Notes TPN For EEClaire Cura100% (1)
- Neuro Psych - Antiepileptic Drug ChartDocumento5 pagineNeuro Psych - Antiepileptic Drug ChartMonica J Ortiz Pereira100% (1)
- Top 200 Drug Study Reference RLPDocumento31 pagineTop 200 Drug Study Reference RLPYathrika YathrikaNessuna valutazione finora
- General Pharmacology - Sources of Drugs and Routes of AdministrationDocumento48 pagineGeneral Pharmacology - Sources of Drugs and Routes of AdministrationDhriti Brahma78% (9)
- Antibiotic Summary - DraftDocumento10 pagineAntibiotic Summary - DraftStrept Pneumonia100% (1)
- M. Pharm Review NAPLEX38Documento1 paginaM. Pharm Review NAPLEX38JUSASBNessuna valutazione finora
- Common infections and recommended antibioticsDocumento3 pagineCommon infections and recommended antibioticsNicole BerryNessuna valutazione finora
- Warfarin Sodium: INR Levels 4.0 or Less Ok To Carry Out Procedure Test Atleast 72 Hrs Prior To ProcedureDocumento6 pagineWarfarin Sodium: INR Levels 4.0 or Less Ok To Carry Out Procedure Test Atleast 72 Hrs Prior To ProcedureVimi GeorgeNessuna valutazione finora
- Drug InteractionsDocumento3 pagineDrug InteractionsgirlwithbrowneyesNessuna valutazione finora
- Electrolytes and Minerals/Acid Base Common Serum Enzymes: Table 8-1Documento1 paginaElectrolytes and Minerals/Acid Base Common Serum Enzymes: Table 8-1JUSASBNessuna valutazione finora
- State Board of PharmacyDocumento66 pagineState Board of PharmacyAnonymous hF5zAdvwCC100% (1)
- Drug ListsDocumento10 pagineDrug ListsAmber Merritt100% (1)
- A Quick Understanding on What Doctors Are Prescribing: Pharmacology for Everyday People & Finding Alternative MedicationsDa EverandA Quick Understanding on What Doctors Are Prescribing: Pharmacology for Everyday People & Finding Alternative MedicationsValutazione: 3.5 su 5 stelle3.5/5 (3)
- HMS III OsteomyelitisDocumento36 pagineHMS III OsteomyelitisveronicaNessuna valutazione finora
- CV 2 PredictsDocumento4 pagineCV 2 PredictsveronicaNessuna valutazione finora
- ABX SummaryDocumento4 pagineABX SummaryveronicaNessuna valutazione finora
- Cervogenic HA Small GRP QsDocumento2 pagineCervogenic HA Small GRP QsveronicaNessuna valutazione finora
- ENDO Exam II PreDocumento5 pagineENDO Exam II PreveronicaNessuna valutazione finora
- BL Final PredictionsDocumento6 pagineBL Final PredictionsveronicaNessuna valutazione finora
- Exam 3 PrintedDocumento3 pagineExam 3 PrintedveronicaNessuna valutazione finora
- BL Final PredictionsDocumento6 pagineBL Final PredictionsveronicaNessuna valutazione finora
- Predict 3Documento7 paginePredict 3veronicaNessuna valutazione finora
- Study Guide - EDDocumento2 pagineStudy Guide - EDveronicaNessuna valutazione finora
- Respiratory SDocumento124 pagineRespiratory SveronicaNessuna valutazione finora
- RespiratoDocumento76 pagineRespiratoveronicaNessuna valutazione finora
- 00 Geriatric Online Mfdsodule 1Documento4 pagine00 Geriatric Online Mfdsodule 1veronicaNessuna valutazione finora
- Vs Predictions Neuro 3Documento1 paginaVs Predictions Neuro 3veronicaNessuna valutazione finora
- Repro ILS Case PrimerDocumento4 pagineRepro ILS Case PrimerveronicaNessuna valutazione finora
- Geriatrics SummaryDocumento13 pagineGeriatrics SummaryveronicaNessuna valutazione finora
- Ils Repro QsDocumento2 pagineIls Repro QsveronicaNessuna valutazione finora
- Geri FDocumento4 pagineGeri FveronicaNessuna valutazione finora
- ILS HeaDocumento4 pagineILS HeaveronicaNessuna valutazione finora
- Respiratory QDocumento6 pagineRespiratory QveronicaNessuna valutazione finora
- Sddmalll Group Cases 1 2015 (v1)Documento3 pagineSddmalll Group Cases 1 2015 (v1)veronicaNessuna valutazione finora
- GI System Pain Evaluation and OMT PlanDocumento6 pagineGI System Pain Evaluation and OMT PlanveronicaNessuna valutazione finora
- Final 2014 Fall S18 19 LE Art and ME New BBDocumento35 pagineFinal 2014 Fall S18 19 LE Art and ME New BBveronicaNessuna valutazione finora
- Repro ILS Case PrimerDocumento4 pagineRepro ILS Case PrimerveronicaNessuna valutazione finora
- Vs High Yield Neuro 2Documento2 pagineVs High Yield Neuro 2veronicaNessuna valutazione finora
- COdddMLEX - Student Login Info - 2011Documento6 pagineCOdddMLEX - Student Login Info - 2011veronicaNessuna valutazione finora
- Thru S-S Pivot - Jugular ProcessesDocumento5 pagineThru S-S Pivot - Jugular ProcessesveronicaNessuna valutazione finora
- Psych Exam PredictionsDocumento4 paginePsych Exam PredictionsveronicaNessuna valutazione finora
- MSK Review Sheet by ProfDocumento4 pagineMSK Review Sheet by ProfveronicaNessuna valutazione finora
- Chapter 10 HandoutDocumento18 pagineChapter 10 HandoutChad FerninNessuna valutazione finora
- Onsemi ATX PSU DesignDocumento37 pagineOnsemi ATX PSU Designusuariojuan100% (1)
- The Other Side of Love AutosavedDocumento17 pagineThe Other Side of Love AutosavedPatrick EdrosoloNessuna valutazione finora
- Why Narcissists Need You To Feel Bad About Yourself - Psychology TodayDocumento51 pagineWhy Narcissists Need You To Feel Bad About Yourself - Psychology Todaytigerlo75Nessuna valutazione finora
- Lecture 15 (91 Slides)Documento91 pagineLecture 15 (91 Slides)Hasnain GoharNessuna valutazione finora
- Philhis Handouts Week 1Documento5 paginePhilhis Handouts Week 1Jeen JeenNessuna valutazione finora
- Goan Bread Tradition Questions AnsweredDocumento2 pagineGoan Bread Tradition Questions AnsweredPreeti SharmaNessuna valutazione finora
- Why Research Is Important in The BusinessDocumento2 pagineWhy Research Is Important in The BusinessBricx BalerosNessuna valutazione finora
- Circumstances Which Aggravate Criminal Liability People vs. Barcela GR No. 208760 April 23, 2014 FactsDocumento8 pagineCircumstances Which Aggravate Criminal Liability People vs. Barcela GR No. 208760 April 23, 2014 FactsJerome ArañezNessuna valutazione finora
- Marwar Steel Tubes Pipes StudyDocumento39 pagineMarwar Steel Tubes Pipes Studydeepak kumarNessuna valutazione finora
- Cash Flow StatementDocumento57 pagineCash Flow StatementSurabhi GuptaNessuna valutazione finora
- Ash ContentDocumento2 pagineAsh Contentvikasbnsl1Nessuna valutazione finora
- 6 Strategies For Effective Financial Management Trends in K12 SchoolsDocumento16 pagine6 Strategies For Effective Financial Management Trends in K12 SchoolsRainiel Victor M. CrisologoNessuna valutazione finora
- P7 Summary of ISADocumento76 pagineP7 Summary of ISAAlina Tariq100% (1)
- Henderson - Historical Documents of The Middle AgesDocumento536 pagineHenderson - Historical Documents of The Middle AgesVlad VieriuNessuna valutazione finora
- Bruno Latour: What Is Iconoclash?Documento3 pagineBruno Latour: What Is Iconoclash?Clara HabibNessuna valutazione finora
- Chapter One - Understanding The Digital WorldDocumento8 pagineChapter One - Understanding The Digital Worldlaith alakelNessuna valutazione finora
- Elementary Hebrew Gram 00 GreeDocumento216 pagineElementary Hebrew Gram 00 GreeRobert CampoNessuna valutazione finora
- Web Search - One People's Public Trust 1776 UCCDocumento28 pagineWeb Search - One People's Public Trust 1776 UCCVincent J. CataldiNessuna valutazione finora
- Ch.24.2 Animal Evolution and DiversityDocumento34 pagineCh.24.2 Animal Evolution and DiversityweldeenytNessuna valutazione finora
- Viennas Cafe Louvre in The 1920s and 1930Documento18 pagineViennas Cafe Louvre in The 1920s and 1930Friso HoeneveldNessuna valutazione finora
- Mr. Honey's Large Business DictionaryEnglish-German by Honig, WinfriedDocumento538 pagineMr. Honey's Large Business DictionaryEnglish-German by Honig, WinfriedGutenberg.orgNessuna valutazione finora
- Contemporary Philippine Arts From The RegionsDocumento29 pagineContemporary Philippine Arts From The RegionsDina Ilagan50% (2)
- Sexual Self PDFDocumento23 pagineSexual Self PDFEden Faith Aggalao100% (1)
- Discrete Mathematics - Logical EquivalenceDocumento9 pagineDiscrete Mathematics - Logical EquivalenceEisha IslamNessuna valutazione finora
- Psychology - A Separate PeaceDocumento2 paginePsychology - A Separate PeacevasudhaaaaaNessuna valutazione finora
- Japanese Tea Cups LessonDocumento3 pagineJapanese Tea Cups Lessonapi-525048974Nessuna valutazione finora
- Epithelial and connective tissue types in the human bodyDocumento4 pagineEpithelial and connective tissue types in the human bodyrenee belle isturisNessuna valutazione finora
- 59-33 ATO Implementation Journal KSA 100Documento18 pagine59-33 ATO Implementation Journal KSA 100nicolas valentinNessuna valutazione finora