Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Peptic Ulcer
Caricato da
neleh grayCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Peptic Ulcer
Caricato da
neleh grayCopyright:
Formati disponibili
PEPTIC ULCER A peptic ulcer is a defect in the lining of the stomach or the first part of the small intestine,
an area called the duodenum. A peptic ulcer in the stomach is called a gastric ulcer. An ulcer in the duodenum is called a duodenal ulcer. A peptic ulcer is an excavation formed in the mucosal wall of the stomach, pylorus, duodenum, or esophagus. It is frequently referred to as a gastric, duodenal, or esophageal ulcer, depending on its location. It is caused by the erosion of a circumscribed area of mucous membrane. Peptic ulcer has been associated with bacterial infection, such as Helicobacter pylori. The greatest frequency is noted in people between the ages of 40 and 60 years. After menopause, the incidence among women is almost equal to that in men. Predisposing factors include family history of peptic ulcer, blood type O, chronic use of nonsteroidal antiinammatory drugs (NSAIDs), alcohol ingestion, excessive smoking, and, possibly, high stress. Esophageal ulcers result from the backward ow of hydrochloric acid from the stomach into the esophagus. Clinical Manifestations
relieved by ejection of the acid gastric contents. Constipation or diarrhea may result from diet and medications. Bleeding (15% of patients with gastric ulcers) and tarry stools may occur; a small portion of patients who bleed from an acute ulcer have only very mild symptoms or none at all.
Assessment and Diagnostic Methods
Physical examination (epigastric tenderness, abdominal distention). Endoscopy (preferred, but upper gastrointestinal [GI] barium study may be done). Diagnostic tests include analysis of stool specimens for occult blood, gastric secretory studies, and biopsy and histology with culture to detect H. pylori (serologic testing, stool antigen tests, or a breath test may also detect H. pylori).
Medical Management
The goals of treatment are to eradicate H. pylori and manage gastric acidity.
Pharmacologic Therapy
Symptoms of an ulcer may last days, weeks, or months and may subside only to reappear without cause. Many patients have asymptomatic ulcers. Dull, gnawing pain and a burning sensation in the mid epigastrium or in the back are characteristic. Pain is relieved by eating or taking alkali; once the stomach has emptied or the alkali wears off, the pain returns. Sharply localized tenderness is elicited by gentle pressure on the epigastrium or slightly right of the midline. Other symptoms include pyrosis (heartburn) and a burning sensation in the esophagus and stomach, which moves up to the mouth, occasionally with sour eructation (burping). Vomiting is rare in uncomplicated duodenal ulcer; it may or may not be preceded by nausea and usually follows a bout of severe pain and bloating; it is
Antibiotics combined with proton pump inhibitors and bismuth salts to suppress H. pylori. H2receptor antagonists (in high doses in patients with ZollingerEllison syndrome) to decrease stomach acid secretion; maintenance doses of H2receptor antagonists are usually recommended for 1 year. Proton pump inhibitors may also be prescribed. Cytoprotective agents (protect mucosal cells from acid or NSAIDs). Antacids in combination with cimetidine (Tagamet) or ranitidine (Zantac) for treatment of stress ulcer and for prophylactic use.
Lifestyle Changes
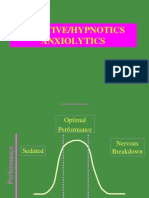
Stress reduction and rest are priority interventions. The patient needs to identify situations that are stressful or exhausting (eg, rushed lifestyle and
irregular schedules) and implement changes, such as establishing regular rest periods during the day in the acute phase of the disease. Biofeedback, hypnosis, behavior modication, massage, or acupuncture may also be useful. Smoking cessation is strongly encouraged because smoking raises duodenal acidity and signicantly inhibits ulcer repair. Support groups may be helpful. Dietary modication may be helpful. Patients should eat whatever agrees with them; small, frequent meals are not necessary if antacids or histamine blockers are part of therapy. Oversecretion and hypermotility of the GI tract can be minimized by avoiding extremes of temperature and over stimulation by meat extracts. Alcohol and caffeinated beverages such as coffee (including decaffeinated coffee, which stimulates acid secretion) should be avoided. Diets rich in milk and cream should be avoided also because they are potent acid stimulators. The patient is encouraged to eat three regular meals a day.
(NSAIDs), and level of tension or nervousness. Ask how patient expresses anger (especially at work and with family), and determine whether patient is experiencing occupational stress or family problems. Obtain a family history of ulcer disease. Assess vital signs for indicators of anemia (tachycardia, hypotension). Assess for blood in the stools with an occult blood test. Palpate abdomen for localized tenderness.
Diagnosis Nursing Diagnoses
Surgical Management
Acute pain related to the effect of gastric acid secretion on damaged tissue Anxiety related to coping with an acute disease Imbalanced nutrition related to changes in diet Decient knowledge about preventing symptoms and managing the condition
With the advent of H2receptor antagonists, surgical intervention is less common. If recommended, surgery is usually for intractable ulcers (particularly with ZollingerEllison syndrome), lifethreatening hemorrhage, perforation, or obstruction. Surgical procedures include vagotomy, vagotomy with pyloroplasty, or Billroth I or II.
Collaborative Problems/Potential Complications
Hemorrhage: upper GI Perforation Penetration Pyloric obstruction (gastric outlet obstruction)
Planning and Goals
Nursing Process Assessment
Assess pain and methods used to relieve it; take a thorough history, including a 72hour food intake history. If patient has vomited, determine whether emesis is bright red or coffee ground in appearance. This helps identify source of the blood. Ask patient about usual food habits, alcohol, smoking, medication use
The major goals of the patient may include relief of pain, reduced anxiety, maintenance of nutritional requirements, knowledge about the management and prevention of ulcer recurrence, and absence of complications.
Nursing Interventions Relieving Pain and Improving Nutrition
prevent hypotension, or place the patient on the left side to prevent aspiration from vomiting. Treat hypovolemic shock as indicated.
Administer prescribed medications. Avoid aspirin, which is an anticoagulant, and foods and beverages that contain acidenhancing caffeine (colas, tea, coffee, chocolate), along with decaffeinated coffee. Encourage patient to eat regularly spaced meals in a relaxed atmosphere; obtain regular weights and encourage dietary modications. Encourage relaxation techniques.
If perforation and penetration are concerns
Reducing Anxiety
Assess what patient wants to know about the disease, and evaluate level of anxiety; encourage patient to express fears openly and without criticism. Explain diagnostic tests and administering medications on schedule. Interact in a relaxing manner, help in identifying stressors, and explain effective coping techniques and relaxation methods. Encourage family to participate in care, and give emotional support.
Note and report symptoms of penetration (back and epigastric pain not relieved by medications that were effective in the past). Note and report symptoms of perforation (sudden abdominal pain, referred pain to shoulders, vomiting and collapse, extremely tender and rigid abdomen, hypotension and tachycardia, or other signs of shock).
Promoting Home and Community Based Care TEACHING PATIENTS SELF CARE
Monitoring and Managing Complications
If hemorrhage is a concern
Assess for faintness or dizziness and nausea, before or with bleeding; test stool for occult or gross blood; monitor vital signs frequently (tachycardia, hypotension, and tachypnea). Insert an indwelling urinary catheter and monitor intake and output; insert and maintain an IV line for infusing uid and blood. Monitor laboratory values (hemoglobin and hematocrit). Insert and maintain a nasogastric tube and monitor drainage; provide lavage as ordered. Monitor oxygen saturation and administering oxygen therapy. Place the patient in the recumbent position with the legs elevated to
Assist the patient in understanding the condition and factors that help or aggravate it. Teach patient about prescribed medications, including name, dosage, frequency, and possible side effects. Also identify medications such as aspirin that patient should avoid. Instruct patient about particular foods that will upset the gastric mucosa, such as coffee, tea, colas, and alcohol, which have acidproducing potential. Encourage patient to eat regular meals in a relaxed setting and to avoid overeating. Explain that smoking may interfere with ulcer healing; refer patient to programs to assist with smoking cessation. Alert patient to signs and symptoms of complications to be reported. These complications include hemorrhage (cool skin, confusion, increased heart rate, labored breathing, and blood in the stool), penetration and perforation (severe abdominal pain, rigid and tender abdomen, vomiting, elevated temperature, and increased heart
rate), and pyloric obstruction (nausea, vomiting, distended abdomen, and abdominal pain). To identify obstruction, insert and monitor nasogastric tube; more than 400 mL residual suggests obstruction. CONTINUING CARE
Teach patient that followup supervision is necessary for about 1 year. Tell patient that the ulcer could recur; advise patient to seek medical assistance if symptoms recur. Inform patient and family that surgery is no guarantee of cure. Discuss possible postoperative sequelae, such as intolerance to dairy products and sweet foods.
Evaluation Expected Patient Outcomes
Remains free of pain between meals Experiences less anxiety Complies with therapeutic regimen Maintains weight Experiences no complications
Potrebbero piacerti anche
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- Glossary of Immune System TermsDocumento5 pagineGlossary of Immune System Termsneleh grayNessuna valutazione finora
- BurnsDocumento7 pagineBurnsneleh grayNessuna valutazione finora
- ncm105 /mental HealthDocumento8 paginencm105 /mental Healthneleh grayNessuna valutazione finora
- Peptic UlcerDocumento4 paginePeptic Ulcerneleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- Physical Assessment Guide of Head-To-ToeDocumento9 paginePhysical Assessment Guide of Head-To-Toeneleh gray100% (2)
- Immunology Notes 104Documento29 pagineImmunology Notes 104neleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- Sedative Hypnotics Anxiolytics Benzodiazepines BarbituratesDocumento60 pagineSedative Hypnotics Anxiolytics Benzodiazepines Barbituratesneleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- Terms and AbbreviationsDocumento67 pagineTerms and Abbreviationsneleh grayNessuna valutazione finora
- Key Areas of ResponsibilityDocumento2 pagineKey Areas of Responsibilityneleh grayNessuna valutazione finora
- Vital Signs TableDocumento5 pagineVital Signs Tableneleh grayNessuna valutazione finora
- CASE STUDY of AGE With Moderate DehydrationDocumento13 pagineCASE STUDY of AGE With Moderate Dehydrationneleh grayNessuna valutazione finora
- Fundamentals of Nursing NotesDocumento11 pagineFundamentals of Nursing Notesneleh grayNessuna valutazione finora
- CBVDDocumento55 pagineCBVDneleh grayNessuna valutazione finora
- Blood Supply of The BrainDocumento11 pagineBlood Supply of The Brainneleh grayNessuna valutazione finora
- An Xy Olitics HypnoticsDocumento59 pagineAn Xy Olitics Hypnoticsneleh grayNessuna valutazione finora
- Small Bowel ObstructionDocumento3 pagineSmall Bowel Obstructionneleh grayNessuna valutazione finora
- Small Bowel ObstructionDocumento3 pagineSmall Bowel Obstructionneleh grayNessuna valutazione finora
- Terms and AbbreviationsDocumento89 pagineTerms and Abbreviationsneleh grayNessuna valutazione finora
- Cerebral Anatomy and Physiology Part Iids08Documento25 pagineCerebral Anatomy and Physiology Part Iids08rocketwapNessuna valutazione finora
- Neurological DisorderDocumento262 pagineNeurological Disorderneleh grayNessuna valutazione finora
- Family PlanningDocumento9 pagineFamily Planningneleh grayNessuna valutazione finora
- Small Bowel ObstructionDocumento3 pagineSmall Bowel Obstructionneleh grayNessuna valutazione finora
- Fundamentals of NursingDocumento3 pagineFundamentals of Nursingneleh grayNessuna valutazione finora
- Feeding Via Gastric GavageDocumento3 pagineFeeding Via Gastric Gavageneleh gray0% (1)
- Feeding Via Gastric GavageDocumento3 pagineFeeding Via Gastric Gavageneleh gray0% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Motor GraderDocumento24 pagineMotor GraderRafael OtuboguatiaNessuna valutazione finora
- VT6050 VT6010 QuickGuide ENDocumento19 pagineVT6050 VT6010 QuickGuide ENPriyank KumarNessuna valutazione finora
- Quaternary Protoberberine Alkaloids (Must Read)Documento26 pagineQuaternary Protoberberine Alkaloids (Must Read)Akshay AgnihotriNessuna valutazione finora
- CG Module 1 NotesDocumento64 pagineCG Module 1 Notesmanjot singhNessuna valutazione finora
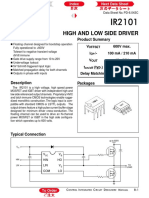
- Datasheet PDFDocumento6 pagineDatasheet PDFAhmed ElShoraNessuna valutazione finora
- Thermal BurnsDocumento50 pagineThermal BurnsPooya WindyNessuna valutazione finora
- Drugs Pharmacy BooksList2011 UBPStDocumento10 pagineDrugs Pharmacy BooksList2011 UBPStdepardieu1973Nessuna valutazione finora
- Abdomen - FRCEM SuccessDocumento275 pagineAbdomen - FRCEM SuccessAbin ThomasNessuna valutazione finora
- Monster of The Week Tome of Mysteries PlaybooksDocumento10 pagineMonster of The Week Tome of Mysteries PlaybooksHyperLanceite XNessuna valutazione finora
- Transport of OxygenDocumento13 pagineTransport of OxygenSiti Nurkhaulah JamaluddinNessuna valutazione finora
- What Is DSP BuilderDocumento3 pagineWhat Is DSP BuilderĐỗ ToànNessuna valutazione finora
- Metal Framing SystemDocumento56 pagineMetal Framing SystemNal MénNessuna valutazione finora
- PC3 The Sea PeopleDocumento100 paginePC3 The Sea PeoplePJ100% (4)
- FST Handbook 2014-Final Copy 1 PDFDocumento382 pagineFST Handbook 2014-Final Copy 1 PDFDelvon DownerNessuna valutazione finora
- Lec9-Rock Cutting ToolsDocumento35 pagineLec9-Rock Cutting ToolsAmraha NoorNessuna valutazione finora
- SRS Design Guidelines PDFDocumento46 pagineSRS Design Guidelines PDFLia FernandaNessuna valutazione finora
- Lightwave Maya 3D TutorialsDocumento8 pagineLightwave Maya 3D TutorialsrandfranNessuna valutazione finora
- Lyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticDocumento13 pagineLyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticJayr Mercado0% (1)
- Caterpillar Ep15krtDocumento37 pagineCaterpillar Ep15krtIvan MajikNessuna valutazione finora
- 9600 DocumentDocumento174 pagine9600 Documentthom38% (13)
- 2 Scour VentDocumento8 pagine2 Scour VentPrachi TaoriNessuna valutazione finora
- Chapter 16 - Energy Transfers: I) Answer The FollowingDocumento3 pagineChapter 16 - Energy Transfers: I) Answer The FollowingPauline Kezia P Gr 6 B1Nessuna valutazione finora
- Who will buy electric vehicles Segmenting the young Indian buyers using cluster analysisDocumento12 pagineWho will buy electric vehicles Segmenting the young Indian buyers using cluster analysisbhasker sharmaNessuna valutazione finora
- Diia Specification: Dali Part 252 - Energy ReportingDocumento15 pagineDiia Specification: Dali Part 252 - Energy Reportingtufta tuftaNessuna valutazione finora
- Brochure Personal CareDocumento38 pagineBrochure Personal CarechayanunNessuna valutazione finora
- Apollo TyresDocumento78 pagineApollo TyresADITYA33% (3)
- KAC-8102D/8152D KAC-9102D/9152D: Service ManualDocumento18 pagineKAC-8102D/8152D KAC-9102D/9152D: Service ManualGamerAnddsNessuna valutazione finora
- Ancient MesopotamiaDocumento69 pagineAncient MesopotamiaAlma CayapNessuna valutazione finora
- TILE QUOTEDocumento3 pagineTILE QUOTEHarsh SathvaraNessuna valutazione finora
- (Razavi) Design of Analog Cmos Integrated CircuitsDocumento21 pagine(Razavi) Design of Analog Cmos Integrated CircuitsNiveditha Nivi100% (1)