Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cervical Pain
Caricato da
steffiecruz06Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cervical Pain
Caricato da
steffiecruz06Copyright:
Formati disponibili
CERVICAL PAIN Definition It is the pain occurring in all or part of a corridor extending from the inferior occiput inferiorly
to the superior interscapular region, localizing to the midline or just paramidline. The patient perceives it as stemming from the neck. Anatomy
The cervical spine is a discrete segment of the axial skeleton and functions to support and stabilize the head, allow the head to move in all planes of motion and protect the spinal cord, nerve roots, spinal nerves and vertebral arteries. There 7 cervical vertebrae, 5 intervertebral disc and 8 cervical nerve roots. The atlantooccipital articulation permits 10 of cervical flexion and 25 cervical extension while the atlantoaxial articulation is responsible for the 45 rotation in either direction. The intervertebral discs are located between C2 to C7 which comprises an outer annulus fibrosus and an inner nucleus pulposus. These intervertebral discs articulate anteriorly while the zygapophyseal joints articulates posteriorly. The intervertebral discs are thicker anteriorly than posteriorly which contributes to the natural cervical lordotic curvature.
Etiology Classification of Neck Pain
Neck pain without stiffness (most common) Enhanced by swallowing Salivary gland (mumps or suppurative parotiditis) Thyroid gland (acute suppurative thyroiditis, subacute thyroiditis with pain radiating to the ear, hemorrhage, or thyroid cystadenoma) Tongue (ulcers or neoplasm) Tonsils (tonsillitis) Enhanced by chewing Mandible (fracture, osteomyelitis, or periodontitis) Temporomandibular joint (associated with myofascial pain syndrome in neck) Enhanced by head movement Cervical spine (whiplash, acute or subacute fracture, dislocation, herniated intervertebral disk, facet joint syndrome or occipital neuralgia with C1 to C2 arthrosis syndrome. Trapezius muscles (MPS) Sternocleidomastoid (torticollis or myofascial pain syndrome) Enhanced by shoulder movement Cervical rib Costoclavicular syndrome Scalenus anticus syndrome Pectoralis minor syndrome Not enhanced by movement Lymph node, acute or chronic (Hodgkins disease) Nervous system (cervical herpes zoster, spinal cord neoplasm, epidural abscess or hematoma or poliomyelitis) Skin and subcutaneous tissue (furuncle, carbuncle) Soft tissue calcium deposit at first and second cervical vertebrae Subclavian artery (aneurysm) Referred pain to the neck Angina Bronchus (bronchial tumor) Pain from 6th cervical dermatomal band Pancoast tumor Stiff Neck: Neck Pain and Limitation of Motion Acquired (spasmodic torticollis) Acute infections Fibrositis (transient stiff neck) Reflex spasm (meningitis)
Torticollis Acute trauma Cervical spine strain Dislocations Fractures Herniated disk Subluxation Chronic infection Infectious arthritis TB spondylitis Congenital (congenital torticollis) Degenerative ( cervical spondylosis with fibrositis)
Epidemiology At any given time, 10% to 15% of people are experiencing neck pain, and two thirds of people have neck pain sometime during their lives. Neck pain is one of the most common complaints primary care providers encounter. Even with a full biomedical course of treatment, neck pain often recurs. Pathophysiology Pain begins with tissue irritation, which may be caused by infection, joint deterioration, sustained use (or sustained immobility), psychological stress, or trauma. Irritation activates nociception. Muscle spasms often occur as the neck is voluntarily or involuntarily repositioned to avoid pain. Inflammation follows, and a vicious positive-feedback circle arises as inflammation leads to even more pain. As edema, structural changes, and harmful metabolites accumulate, they can cause ischemia of the tissues. If these alterations are not interrupted or reversed in time, long-term changes in neck structure may arise, and disability can result. Clinical Manifestation sharp shooting pain dizziness or lightheadedness difficulty swallowing headache facial pain upper extremity paresthesias pain worsened by movement LOM Stiff neck
Differential Diagnosis Amyotrophic lateral sclerosis Multifocal motor neuropathy Multiple sclerosis Syringomyelia Peripheral neuropathy Pharmacological Management Tricyclic Antidepressants (TCAs) Muscle Relaxants Nonsteroidal Antiinflammatory Drugs (NSAIDs) Acetaminophen Opioids PT Management A. Objective of care: Decrease pain Increase ROM To preserve the integrity of the muscles and all the surrounding structures of the neck To bring back functional mobility of the structures involved To regain the normal alignment of the altered curvature of the cervical spine B. Appropriate Interventions and Rationale of each action Massage- to allow or increase blood flow on the affected area and to avoid adhesion Mobilization exercises- to avoid spasticity or atrophy of the muscles of the cervical spine Relaxation exercises- to decrease muscle tension Biofeedback- to be aware and to have control of the proper posture and processes of the body. C. Relevant Teaching Proper rest Patient should be taught the proper posture for the neck Avoid forces that may exacerbate symptoms Protection of the affected structures Wearing of soft collars if needed
Cervical Sprain/ Strain Definition A cervical strain is a musculotendinous injury produced by an overload injury resulting from excessive forces imposed on the cervical spine. In contrast, cervical sprains are overstretching or tearing injuries of spinal ligaments Anatomy Cervical sprain involves the ligamentous and capsular structures that stabilize and connect the vertebrae and their facet joints. Cervical strain involves levator scapula, trapezius, rhomboids, SCM, scalenes and the extensor muscle group. Muscular strains are seen most frequently because many cervical muscles do not terminate in tendons, but rather attach directly to bone via myofascial tissue that blends seamlessly with periosteum. Etiology Abnormal stresses applied in the cervical spine Acceleration and deceleration injuries Traumatic blows Repetitive motions Epidemiology Cervical sprain and strain injuries account for approximately 85% of neck pain resulting from acute, repetitive, or chronic neck injuries. The incidence is higher in women and individuals aged 30 to 50 years. Pathophysiology Physiologic forces acting on a relatively normal cervical spine result in typical soft tissue strain seen in nonathletes. In individuals with thoracic kyphosis and consequential cervical lordosis and extension, strain occurs in the levator scapulae, superior trapezius, sternocleidomastoid, scalene, and suboccipital muscles. Traumatic blows often incurred in sporting injuries can result in a more acute cervical strain or sprain. Repetitive motions, as occur in recreational activities, can tax shortened and deconditioned cervical rotators, extensors, and lateral flexors that are frequently present in those with cervical spondylosis Clinical manifestation
Headaches that are sharp or dull and localize to the cervical or shoulder girdle musculature. Neck fatigue or stiffness that lessens with gradual activity. Aggravating factors include passive or active motion. Decreased cervical range of motion.
Essentials of Diagnosis Pain is the chief complaint Local tenderness; decreased range of motion; headaches, typically occipital; blurred or double vision Dysphagia, hoarseness, jaw pain, difficulty with balance, vertigo. Roentgenographic evaluation is indicated Differential Diagnosis Fractures Subluxations and dislocations Herniated disk Degenerative disk disease Rheumatoid arthritis Ankylosing spondylitis Infection Factors associated with a poor prognosis: Presence of occipital headaches Interscapular pain Reversal of cervical lordosis Involvement in litigation or workers compensation claims Women have a worse prognosis than men. Pharmacological Management Nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (paracetamol) aid in controlling pain and nurturing restorative sleep patterns. If patients complain of substantial spasm not improved by analgesics and proper positioning, tizanidine or tricyclic antidepressants might be helpful. PT Management A. Objectives of care: Initial rest, bed rest if necessary, and soft collar immobilization are indicated, along with use of antiinflammatory medications
Encourage early mobilization with progressive range of motion and preventing from external supports Frequent reassurance is often necessary because symptoms may be long lasting
B. Appropriate interventions: Physical modalities such as massage, superficial and deep heat, electrical stimulation, and a soft cervical collar can be used in the treatment program.
C. Rationale of treatment: Light massage causes sedation, reduction of adhesions, muscular relaxation, and vascular changes Superficial heat and deep heat with ultrasound produce analgesia and muscle relaxation help resolve inflammation, and increase connective tissue elasticity. Transcutaneous electrical nerve stimulation can also be effective in modulating musculoskeletal pain. A soft cervical collar can be prescribed to ease painful sleep disturbances and reduce further neck strain. The collar can be worn while awake, but should be restricted to the first 72 hours after the injury to minimize interference with healing and prevent development of soft tissue tightening. D. Relevant health teachings to patient and family: A gradual return to activities should be initiated by 2 to 4 weeks after injury, and should include a functional restoration program to address postural reeducation. Proper spinal biomechanics must be restored with the establishment of proper movement patterns. Proprioceptive retraining, balance, and postural conditioning should be incorporated into the exercise regimen. Flexibility and range of motion are improved by mobilization and stretching exercises Cervical Spondylosis Definition The age-related, degenerative changes that begin at the intervertebral disk and subsequently involve other tissues,
such as the articular cartilage of the apophyseal joints, and the bone of the spine, including the unciform process. Cervical Spondylotic myelopathy - Is compromise of the spinal cord within the spinal canal as a result of degenerative changes of the cervical spine, is the most serious consequence of cervical intervertebral disc degeneration and the most common cervical spinal cord disorder after middle age. Etiology - Narrowing of the disk height - Presence of osteophytes arising from the disk margins - Ostheoarthritic changes in the posterior zygopophyseal joints. Epidemiology Report upon findings in autopsies of 4253 spines found evidence of spondylosis in 60% of women and 80% in men by the age of 49years and 95% incidence in both sexes ate age 70 years. Significant structural changes in the disk have been reported in most studies of pathological disks in patients past the age of 30 to 35 years. Pathophysiology Cervical spondylosis begins with a decrease in hydration and in water-binding capacity of the nucleus pulposus. This change in hydration capacity typically begins during the third decade. Because the decrease in hydration lessens the intradiscal pressure- the pressure exerted by the hydrophilic nucleus pulposus against the inner walls of the annulus fibrosus- tension cannot be maintained within the annular rings and they buckle as they become excessively loaded in compression. As a result, the annulus fibrosus fibrillates and weakens. The margins of the optimal loading zone for the intervertebral disc are now altered. Clinical Manifestation Neck pain Neck pain with proximal referral Radicular pain Myelopathy Essentials of Diagnosis Generalized disease of the cervical spine related to disk degeneration; myelopathy, radiculopathy, or both may occur
In 90% of men >50 y/o and women >60 y/o, radiographs show cervical degeneration: disk changes, then facet arthropathy, and osteophyte formation and ligament instability Patients often present with complaints of shoulder, elbow, wrist, or hand pain and may report headache (if upper cervical spine is affected) and stiff neck Multiple nerve roots may be involved in radicular symptoms, causing arm pain and distal paresthesias Myelopathy may present with radicular symptoms but also loss of balance, broad-based gait, and lower extremity weakness Reflexes are hypoactive in the upper extremity but hyperactive in the lower; possible Babinski reflex and clonus Clinical picture depends on the anatomic level involved
Differential Diagnosis Cervical radiculopathy due to cervical disk Spinal cord tumor Rheumatoid arthritis Multiple sclerosis Syringomyelia Treatment Depends on symptoms (e.g, neck pain alone, radiculopathy, or myelopathy); initial management is soft collar, NSAIDs, and physical therapy; epidural steroids may be helpful Consider surgical intervention if unresponsive to conservative therapy or if neurologic status deteriorates; surgical decompression of cord through an anterior approach allows anterior fusion; cervical disk replacement is probably not appropriate for the generalized disease occurring in spondylosis. PT Mangement A. Objectives of care: An MRI or a CT scan may be of value, but usually a though clinical examination and routine x-ray studies suffice to confirm the diagnosis. Restore physiological posture a) Decrease the forward-head posture b) Decrease excessive lordosis
Instruction in exercises, ADL, and traction
B. Rationale of action: Supine traction with the angle, force, and duration of traction determined by the tolerance and response reaction of the patient. Neck brace or custom-fitted collar to restrict motion and to ensure proper posture. Either of these should be used for sufficient length of time to assure diminution of inflammation but not so long as to cause dependence or disuse. C. Relevant health teachings to patient and Family: Avoidance of any movement that causes or aggreviates the radicular symptoms Avoidance of excessive range of motion exercises Judicious use of oral inti-inflammation medicine, antidepressant Modification of ADL considered to be aggravating
Tortocollis Definition Idiopathic cervical dystonia, the most common form of adultonset focal dystonia, is an involuntary twisting and turning of the neck caused by abnormal involuntary muscle contractures. Cervical dystonia has also been known as spasmodic torticollis, which implies head jerking or neck spasms. Etiology The only risk factor for progression of dystonia to other body parts was longer duration of disease. Epidemiology The prevalence of cervical dystonia has been estimated at 9 per 100,000, but this low frequency is based on a retrospective chart review.3 The incidence is sex and age related. Women are affected 1.5 to 1.9 times more often than men are 2.4. In 70% to 90% of cases, the disease begins between the fourth and sixth decades, with a peak incidence in the fifth decade of life. Pathophysiology The pathogenic mechanisms of cervical dystonia is most often influenced by genetic factors.
Cervical dystonia develop secondary to head, neck, and shoulder trauma. Impaired inhibition of sensory Ia afferent fibers, impairment of central sensory pathways, and increased spindle responsiveness secondary to overactive gamma-spindle efferent fibers Clinical Manifestation Symptoms usually begin insidiously with complaints of a pulling or drawing in the neck or an involuntary twisting or jerking of the head. (sensory in nature) In extracervical dystonia, the jaw (oromandibular), eyelids (blepharospasm), arm or hand (writers cramp,) and trunk (axial) are the most frequently affected parts. A postural or kinetic hand tremor is present. Most notable is the use of a sensory trick or geste antagonistique. Gently touching the chin, back of the head, or top of the head relieves the symptoms. Pain was commonly described as tiring, radiating, tugging, aching, and exhausting. Functional Limitation Severity of disabilities ranged from: - Mild (subjective feeling of discomfort in social conditions without objective consequences on social life) - Severe (qualitative and quantitative modifi cation of the occupational level with resulting impairment of social life) Pain is associated with constant head turning, greater severity of head turning, and the presence of spasms. Disability is also caused by task-specific limitations (e.g., inability to drive) and avoidance of social interaction due to abnormal posture. Diagnosis Screening biochemical studies (blood chemistry screening test, complete blood count, thyroid function) in addition to a ceruloplasmin level should be performed. Magnetic resonance imaging of the brain and cervical spine should be considered in all patients with a fixed painful neck posture. If there is scoliosis, it may be evaluated with plain radiographs to document the baseline abnormality.
Differential Diagnosis Atlantoaxial dislocation Cervical fracture Degenerative disc Osteomyelitis Klippel-Feil syndrome Congenital torticollis associated with absence of fibrosis of the cervical muscles Post irradiation fibrosis Acute stiff neck Pharyngitis Painful lymphadenopathy, adenitis Vestibulo-ocular dysfunction (head tilt with fourth nerve paresis or labyrinthine disease) Posterior fossa tumor Arnold-Chiari syndrome Nystagmus Sandifer syndrome Spinal cord tumor or syrinx Extraocular muscle palsies, strabismus Head thrusts with oculomotor apraxia Hemianopia Focal seizures Prognosis The prognosis of patients with cervical dystonia has been radically changed after the introduction of chemodenervation with botulinum toxin. Compared with all previous therapies, botulinum toxin benefits the highest percentage of patients in the shortest time, has been proved effective in many doubleblind placebo-controlled and open trials and has fewer side effects than other pharmacologic therapies. For idiopathic cervical dystonia, serotype A is most widely used. The use of serotypes B and F is under investigation in patients who have become immunologically resistant to serotype A. Complications Patients may develop cervical spondylosis with resulting radiculopathy or myelopathy. Extra cervical spread of dystonia is a progression of dystonia to a segmental pattern of dystonia. Isolated cervical dystonia can typically spread to the face, jaw, arms, or trunk
Pharmacological Management Chemodenervation with botulinum toxin. (Medications are generally used as adjuncts to botulinum toxin.) Anticholinergics Benzodiazepines Baclofen Other medications are available, and many patients will require combination therapy. If therapy with botulinum toxin and oral medications fails, surgery may be required
Head Postures and the Muscles Most Commonly Responsible for the Posture Head Posture Responsible Muscles Rotational torticollis Contralateral SCM Ipsilateral SC With or without contralateral SC Laterocollis Retrocollis Ipsilateral SCM, SC, TPZ Bilateral SC
PT Management Physical therapy is recommended as an adjunct to botulinum toxin injection. After treatment, there is less opposition from the dystonic musculature. The goal is to facilitate the patients increased control over head movement and posture once the antagonists are weakened. In a case report, reduction of the effective dose of botulinum toxin was also possible when physiotherapy management was added to a long-term treatment regimen.
References Cervical Pain: Braddom, R.L., Physical Medicine & Rehabilitation. 4th ed.,p. 787-796 DeLisa, J.A., Rehabilitation Medicine: Principles & Practice, 4th ed., p 632-648 Frontera, W.R., Silver, J.L. & Rizzo Jr., T. D., Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation, 2nd ed., p. 3-6 OYoung, B., Young, M. A., Stiens, S. A., PM&R Secrets, p. 303 Rakel, D., Integrative Medicine, 3rd ed., pp 599-606 Shultz, S. J., Houglum, P. A., Perrin, D. H., Assesment of Athletic Injuries, p. 53 Warfield, C.A., Principles and Practice of Pain Management, p. 110
Cervical Sprain/ Strain Braddom, R.L., Physical Medicine & Rehabilitation. 4th ed.,p. 794 Frontera, W.R., Silver, J.L. & Rizzo Jr., T. D., Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation, 2nd ed., p. 23-25
Cervical Spondylosis Cailliet., R., Neck and Arm Pain, 3rd ed., pp 165, 180 Frontera, W.R., Silver, J.L. & Rizzo Jr., T. D., Essentials of Physical Medicine and Rehabilitation:
Musculoskeletal Disorders, Pain, and Rehabilitation, 2nd ed., p. 11-15 Porterfield, J.A., DeRosa, C., Mechanical Neck Pain: Perspective in Functional Anatomy, pp., 18-19
Torticollis Frontera, W.R., Silver, J.L. & Rizzo Jr., T. D., Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation, 2nd ed., pp. 579-582
Potrebbero piacerti anche
- Low Back PainDocumento8 pagineLow Back PainLev KalikaNessuna valutazione finora
- Hip Disorders, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentDa EverandHip Disorders, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentNessuna valutazione finora
- The Effect of Cervical Traction Combined With Neural Mobilization On Pain and Disability in Cervical RadiculopathyDocumento5 pagineThe Effect of Cervical Traction Combined With Neural Mobilization On Pain and Disability in Cervical RadiculopathyJORGE MANÇONessuna valutazione finora
- IvdpDocumento89 pagineIvdpFelix SabuNessuna valutazione finora
- Upper Limb OrthosisDocumento83 pagineUpper Limb OrthosisAwaisNessuna valutazione finora
- Wrist Anatomy: Bones Quiz - What Bones Comprise The Wrist? Joints Quiz - What Joints Comprise The Wrist?Documento63 pagineWrist Anatomy: Bones Quiz - What Bones Comprise The Wrist? Joints Quiz - What Joints Comprise The Wrist?Mnn SaabNessuna valutazione finora
- Rehab Plans and Exercises Minor Rotator Cuff Repair Protocol For Physiotherapy Following SurgeryDocumento11 pagineRehab Plans and Exercises Minor Rotator Cuff Repair Protocol For Physiotherapy Following SurgeryTech How AssamNessuna valutazione finora
- Cauda Equina and Conus Medullaris Syndromes Clinical PresentationDocumento9 pagineCauda Equina and Conus Medullaris Syndromes Clinical PresentationhoneyworksNessuna valutazione finora
- Kamars RadiologyDocumento135 pagineKamars RadiologyNayantara Nair100% (1)
- Cinahl Rotator Cuff InjuriesDocumento11 pagineCinahl Rotator Cuff InjurieslizardbeeNessuna valutazione finora
- Cervicogenic Headache Diagnosis and Symptoms Compared to Migraine and Tension HeadachesDocumento10 pagineCervicogenic Headache Diagnosis and Symptoms Compared to Migraine and Tension Headachespuchio100% (1)
- Neck PainDocumento1 paginaNeck PainHasan RahmanNessuna valutazione finora
- Total Hip Arthroplasty PDFDocumento10 pagineTotal Hip Arthroplasty PDFWindy ZeniccNessuna valutazione finora
- Brachial Plexus Injury GuideDocumento19 pagineBrachial Plexus Injury GuideAisyah AzaniNessuna valutazione finora
- SpondylodistitisDocumento32 pagineSpondylodistitisNurul Sakinah RosliNessuna valutazione finora
- Low BackDocumento7 pagineLow BackMuhammad FahmyNessuna valutazione finora
- Radial Nerve: Rajadurai R Crri, Orthopedics Ii Unit RGGGHDocumento31 pagineRadial Nerve: Rajadurai R Crri, Orthopedics Ii Unit RGGGHrajaeasNessuna valutazione finora
- Assessment of Back Pain-BMJDocumento30 pagineAssessment of Back Pain-BMJMarco Paulo Reyes NaoeNessuna valutazione finora
- Orthosisofhandppt 181202162551Documento65 pagineOrthosisofhandppt 181202162551Khageswar SamalNessuna valutazione finora
- Frozen Shoulder - Adhesive Capsulitis - OrthoInfo - AAOSDocumento6 pagineFrozen Shoulder - Adhesive Capsulitis - OrthoInfo - AAOSpempekplgNessuna valutazione finora
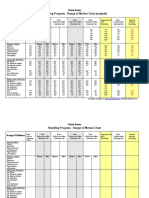
- Standing Program - Range of Motion Chart (Sample) : Client NameDocumento2 pagineStanding Program - Range of Motion Chart (Sample) : Client NameNorMan Albaytar PerezNessuna valutazione finora
- Spondylolisthesis PDFDocumento121 pagineSpondylolisthesis PDFishak_alsophNessuna valutazione finora
- Low Back Pain: Rezki Amalia NurshalDocumento74 pagineLow Back Pain: Rezki Amalia NurshalRezki Amalia NurshalNessuna valutazione finora
- MSK Us ProtocolsDocumento40 pagineMSK Us Protocolsjamir59Nessuna valutazione finora
- MusculoskeletalDocumento119 pagineMusculoskeletalEdissa PangilinanNessuna valutazione finora
- Scoliosis: Degenerative & IdiopathicDocumento34 pagineScoliosis: Degenerative & IdiopathicClaudia MariscaNessuna valutazione finora
- A Patient's Guide To Radial Tunnel SyndromeDocumento4 pagineA Patient's Guide To Radial Tunnel SyndromeKarunya Vk100% (1)
- Fracture Colles Rehabilitation Advice Following WristDocumento4 pagineFracture Colles Rehabilitation Advice Following WristfaprilisaNessuna valutazione finora
- Clinical Signs - NamedDocumento9 pagineClinical Signs - NamedsprapurNessuna valutazione finora
- Scoliosis (Curved Spine)Documento7 pagineScoliosis (Curved Spine)Chow Mun FaiNessuna valutazione finora
- Wrist / Fingers Injuries: DR - Shafaq Shahid Lecturer DPT, Ms-OmptDocumento59 pagineWrist / Fingers Injuries: DR - Shafaq Shahid Lecturer DPT, Ms-OmptNabiha AjmalNessuna valutazione finora
- Lumbar Radiculopathy Medback Castillo Mendez EDITEDDocumento12 pagineLumbar Radiculopathy Medback Castillo Mendez EDITEDSteve ColbertNessuna valutazione finora
- Genu Recurvatum SyndromDocumento7 pagineGenu Recurvatum SyndromRoxana RascaNessuna valutazione finora
- Lumbar Spine AssesmentDocumento8 pagineLumbar Spine AssesmentPavithra SivanathanNessuna valutazione finora
- Ankle Examination Orthopaedics McraeDocumento6 pagineAnkle Examination Orthopaedics McraeHafizah HoshniNessuna valutazione finora
- Musculoskeletal TraumaDocumento103 pagineMusculoskeletal TraumaJona Kristin EnclunaNessuna valutazione finora
- Peripheral Nerve Blocks Lower ExtremityDocumento53 paginePeripheral Nerve Blocks Lower ExtremityArief Hariyadi SantosoNessuna valutazione finora
- Hand PDFDocumento179 pagineHand PDFRadenSiwi Bagus HadhiningratNessuna valutazione finora
- Principles of Tendon Transfer in The Hand and ForearmDocumento9 paginePrinciples of Tendon Transfer in The Hand and Forearm'Ema Surya PertiwiNessuna valutazione finora
- Cervical DisordersDocumento89 pagineCervical DisordersAbdallah Samir Mostafa٢٠١٩٠٢١٥٩Nessuna valutazione finora
- Trochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandTrochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Assessment of Posture: Prepared By: Floriza P. de Leon, PTRPDocumento17 pagineAssessment of Posture: Prepared By: Floriza P. de Leon, PTRPFloriza de Leon100% (1)
- Management L Low Back PainDocumento7 pagineManagement L Low Back PainelsyamelindaNessuna valutazione finora
- Lumbar Spine AssessmentDocumento26 pagineLumbar Spine Assessmentyoyo_pt2007100% (1)
- Fractures of Spine and Pelvis2007Documento70 pagineFractures of Spine and Pelvis2007api-19916399Nessuna valutazione finora
- Juvenile Idiopathic ArthritisDocumento14 pagineJuvenile Idiopathic ArthritisClaudiaCazacuNessuna valutazione finora
- Carpal Tunnel Syndrome JAAOS 2007 PDFDocumento12 pagineCarpal Tunnel Syndrome JAAOS 2007 PDFStefano Pareschi PasténNessuna valutazione finora
- Tendon TransferDocumento1 paginaTendon TransferPandi Smart VjNessuna valutazione finora
- Cervical Spine EvaluationDocumento9 pagineCervical Spine EvaluationS.Muhaymen HussainNessuna valutazione finora
- B 756 Vertebris GB III10Documento44 pagineB 756 Vertebris GB III10Lukasz Bartochowski100% (1)
- 87 Slides Fundamentals in Orthopedic Surgery 2019Documento88 pagine87 Slides Fundamentals in Orthopedic Surgery 2019Mark Samuel Tanchoco100% (1)
- The Wrist Common Injuries and ManagementDocumento36 pagineThe Wrist Common Injuries and ManagementDan RollorataNessuna valutazione finora
- Spine Fractures and Spinal Cord InjuryDocumento54 pagineSpine Fractures and Spinal Cord InjuryAloy PudeNessuna valutazione finora
- Beighton Hypermobility ScoreDocumento2 pagineBeighton Hypermobility ScoreVishal RautNessuna valutazione finora
- Spondylolisthesis: To Reduce or Not Case Discussion: Early Onset ScoliosisDocumento36 pagineSpondylolisthesis: To Reduce or Not Case Discussion: Early Onset ScoliosisneareastspineNessuna valutazione finora
- Ultrasound Guided Lower Limb Blocks Tony AllenDocumento39 pagineUltrasound Guided Lower Limb Blocks Tony Allenrepre64Nessuna valutazione finora
- Week 1 and 2 PCP Workbook QuestionsDocumento4 pagineWeek 1 and 2 PCP Workbook Questionsapi-479717740100% (1)
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsValutazione: 4 su 5 stelle4/5 (2)
- Balance Dysfunction in Parkinson’s Disease: Basic Mechanisms to Clinical ManagementDa EverandBalance Dysfunction in Parkinson’s Disease: Basic Mechanisms to Clinical ManagementNessuna valutazione finora
- Hip Neck Fracture, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandHip Neck Fracture, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Leprosy PDFDocumento19 pagineLeprosy PDFsteffiecruz06Nessuna valutazione finora
- Coronary Artery DiseaseDocumento5 pagineCoronary Artery Diseasesteffiecruz06Nessuna valutazione finora
- Cardiac RehabDocumento37 pagineCardiac Rehabsteffiecruz06Nessuna valutazione finora
- Overuse SyndromeDocumento20 pagineOveruse Syndromesteffiecruz06Nessuna valutazione finora
- Delayed Onset Muscle Soreness (Doms)Documento2 pagineDelayed Onset Muscle Soreness (Doms)steffiecruz06Nessuna valutazione finora
- Chronic Fatigue Syndrome PDFDocumento22 pagineChronic Fatigue Syndrome PDFsteffiecruz06Nessuna valutazione finora
- FibromyalgiaDocumento20 pagineFibromyalgiasteffiecruz06Nessuna valutazione finora
- Chronic PainDocumento38 pagineChronic Painsteffiecruz06Nessuna valutazione finora
- XL MulticalDocumento2 pagineXL MulticalĐào Huy VănNessuna valutazione finora
- Icmr-National Institute For Research in Tuberculosis-ChennaiDocumento27 pagineIcmr-National Institute For Research in Tuberculosis-Chennaidhanya sriNessuna valutazione finora
- Retinal Diseases - 5Documento2 pagineRetinal Diseases - 5AkicaNessuna valutazione finora
- Lyme, CF ProtocolDocumento36 pagineLyme, CF ProtocolTheresa Dale100% (1)
- Dengue Case SolutionDocumento9 pagineDengue Case SolutionPRASHANT GUPTA0% (1)
- Serological Diagnosis of Infectious DiseasesDocumento38 pagineSerological Diagnosis of Infectious DiseasesPurple basketNessuna valutazione finora
- KIT Volume XXI No 1 April 2009 PropDocumento16 pagineKIT Volume XXI No 1 April 2009 PropKITexBruderhofCCINessuna valutazione finora
- CA MammaeDocumento30 pagineCA MammaeAlfiany SahrNessuna valutazione finora
- 2005 Coxe Cooper Avian FluDocumento37 pagine2005 Coxe Cooper Avian Flupep59Nessuna valutazione finora
- Endodontic MicrobiologyDocumento9 pagineEndodontic MicrobiologySarah KahilNessuna valutazione finora
- RBI Sees 9.5 PC GDP Contraction in FY21: India S Active Covid-19 Cases Fall Below 9 LakhDocumento12 pagineRBI Sees 9.5 PC GDP Contraction in FY21: India S Active Covid-19 Cases Fall Below 9 LakhGauravNessuna valutazione finora
- Handbook of African Swine Fever in Wild BoarDocumento111 pagineHandbook of African Swine Fever in Wild BoarMayeth MacedaNessuna valutazione finora
- Zygomatic Implants PDFDocumento18 pagineZygomatic Implants PDFgirl33Nessuna valutazione finora
- Ajit Kulkarni - LachesisDocumento8 pagineAjit Kulkarni - LachesisAntonio Andres BergesNessuna valutazione finora
- Flesh-Eating BacteriaDocumento3 pagineFlesh-Eating BacteriaEdward McSweegan, PhD100% (2)
- Fastest way to travel from Misamis Occidental to Camiguin islandDocumento3 pagineFastest way to travel from Misamis Occidental to Camiguin islandNina Romina NavaltaNessuna valutazione finora
- General Veterinary Parasitology and Helminthology PDFDocumento253 pagineGeneral Veterinary Parasitology and Helminthology PDFLakshmi75% (4)
- Micro-Blading PPT GBDocumento55 pagineMicro-Blading PPT GBMarina Koza100% (4)
- STIs Part ADocumento3 pagineSTIs Part AMihaela EneNessuna valutazione finora
- Executive Summary Per Barangay in A Semester For CHN For FacultyDocumento5 pagineExecutive Summary Per Barangay in A Semester For CHN For FacultyAmira Fatmah QuilapioNessuna valutazione finora
- 15 Leave PDFDocumento12 pagine15 Leave PDFKarthiga SelviNessuna valutazione finora
- Integrated Helminth Control Program (IHCP) : Date VenueDocumento31 pagineIntegrated Helminth Control Program (IHCP) : Date VenueAnonymous100% (2)
- Daftar Pustaka: Dermatology, 2Documento3 pagineDaftar Pustaka: Dermatology, 2Kusmantoro HidayatNessuna valutazione finora
- Kisi Soal BHS Inggris KLS Xii Pas GanjilDocumento4 pagineKisi Soal BHS Inggris KLS Xii Pas Ganjilirawan dwi putraNessuna valutazione finora
- Contact Lens Complications and ManagementDocumento10 pagineContact Lens Complications and Managementstrawberry8832850% (2)
- Participatory LectureDocumento5 pagineParticipatory LectureThandiMtungwaNessuna valutazione finora
- Word Formation 2417Documento8 pagineWord Formation 2417Adam BrzostekNessuna valutazione finora
- Cystic Fibrosis Signs and Symptoms ExplainedDocumento3 pagineCystic Fibrosis Signs and Symptoms ExplainedsakthiprimeNessuna valutazione finora
- Cardiovascular Health DrillsDocumento10 pagineCardiovascular Health DrillsnotadagNessuna valutazione finora
- Making System Dynamics Cool II: New Hot Teaching and Testing Cases of Increasing ComplexityDocumento29 pagineMaking System Dynamics Cool II: New Hot Teaching and Testing Cases of Increasing ComplexityAdrian HNessuna valutazione finora