Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
The Addition of Clonidine To Bupivacaine in Combined Femoral-Sciatic Nerve Block For Anterior Cruciate Ligament Reconstruction
Caricato da
pshz92Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
The Addition of Clonidine To Bupivacaine in Combined Femoral-Sciatic Nerve Block For Anterior Cruciate Ligament Reconstruction
Caricato da
pshz92Copyright:
Formati disponibili
www.aana.com/members/journal/ AANA Journal/August 2004/Vol. 72, No.
4 273
A
nterior cruciate ligament (ACL) recon-
struction is associated with significant
postoperative pain that can last as long as
48 hours, often resulting in immobility and
a decrease in effective early mobilization.
1,2
Furthermore, this postoperative immobility can result
in the development of adhesions, weakened ligament
insertion, and muscle atrophy.
3
Therefore, it is impor-
tant that effective postoperative pain management
techniques be used to decrease the incidence of these
preventable postoperative complications. Traditionally,
oral and parental opioids and nonsteroidal anti-inflam-
matory agents are used to control the pain following
ACL reconstruction. While these pharmacological
agents have been shown to adequately control the
pain, large doses often are required, which can result in
a multitude of undesirable side effects.
4,5
In an attempt to provide effective postoperative
analgesia while minimizing untoward effects, anesthe-
sia providers are continually exploring alternative
methods. Of these alternative methods, one technique
Clonidine has been shown to prolong sensory analgesia
when given as an adjunct to peripheral nerve blocks but has
not been evaluated when given in conjunction with a
femoral-sciatic nerve block. The purpose of this investiga-
tion was to determine whether the addition of clonidine to
a femoral-sciatic nerve block would prolong the duration of
sensory analgesia in groups of patients undergoing ante-
rior cruciate ligament (ACL) reconstruction.
This prospective, randomized, double-blind investiga-
tion was performed on 64 subjects undergoing ACL recon-
struction. Patients were assigned randomly to receive a
femoral-sciatic nerve block using 30 mL of 0.5% bupiva-
caine with 1:200,000 epinephrine (control group) or 30 mL
of 0.5% bupivacaine with 1:200,000 epinephrine and 1
g/kg of clonidine (experimental group). Variables meas-
ured included demographics, timed pain intensity measure-
ments, postoperative analgesic consumption, duration of
analgesia, and patient satisfaction.
No significant differences were noted between groups
for pain intensity scores, duration of sensory analgesia,
postoperative analgesic requirements, or overall patient
satisfaction. Both groups reported minimal amounts of
postoperative pain and high analgesic satisfaction scores.
Based on our results, we do not recommend the addition
of clonidine to a femoral-sciatic nerve block when given to
facilitate postoperative analgesia in patients undergoing
ACL reconstruction.
Key words: Anterior cruciate ligament reconstruction,
femoral-sciatic nerve block, postoperative pain manage-
ment, regional anesthesia.
The addition of clonidine to bupivacaine in
combined femoral-sciatic nerve block for
anterior cruciate ligament reconstruction
LT Darren J. Couture, CRNA, MSN, NC, USNR
Bremerton, Washington
LT Heather M. Cuniff, CRNA, MSN, NC, USNR
LCDR Joseph F. Burkard, CRNA, MSN, NC, USN
San Diego, California
LCDR John P. Maye, CRNA, PhD, NC, USN
CDR Joseph Pellegrini, CRNA, DNSc, NC, USN
Bethesda, Maryland
that has been shown to be highly effective in control-
ling postoperative pain in patients undergoing ACL
reconstruction is the lower extremity peripheral nerve
block.
6,7
Lower extremity peripheral nerve blocks in
patients undergoing ACL reconstruction have been
shown to significantly decrease postoperative anal-
gesic requirements, improve postoperative knee reha-
bilitation, and decrease the length of time required in
the hospital.
6,7
Because of these advantages many
practitioners advocate placing a lower extremity
peripheral nerve block in all patients undergoing ACL
reconstruction. The most common nerves blocks per-
formed to facilitate this analgesia are the femoral
nerve block and the combined femoral-sciatic nerve
block. However, it has been noted that after initial
block resolution, patients must rely on oral analgesics
that are associated with undesirable side effects.
Therefore, many clinical investigations have been per-
formed to determine ways to increase the duration of
analgesia from peripheral nerve blocks. These investi-
gations have analyzed the use of combinations of local
274 AANA Journal/August 2004/Vol. 72, No. 4 www.aana.com/members/journal/
anesthetics or supplemental medications to prolong
anesthetic duration with traditional and nontradi-
tional medications.
8-12
One of the nontraditional med-
ications that has shown some promise is the a
2
-adren-
ergic agonist clonidine.
Clonidine has been shown to have an analgesic neu-
raxial effect and is well described in the literature, but
its use is limited by side effects that include an impact
on hemodynamic variables.
13
Studies also have shown
that clonidine can be administered as an adjunct to
local anesthetics in the performance of a peripheral
nerve block without having a detrimental effect on
hemodynamics.
8-12
However, it has been noted that
there are limited studies on what effect clonidine will
have when added to a femoral-sciatic nerve block, and,
to our knowledge, no study has been performed to
date evaluating the effect when given in conjunction
with a femoral-sciatic nerve block in patients undergo-
ing ACL reconstruction. Therefore, the purpose of this
investigation was to examine whether the addition of
1 g/kg of clonidine would prolong the duration of
analgesia and improve patient outcomes when admin-
istered with bupivacaine in a femoral-sciatic block for
ACL reconstruction.
Materials and methods
This double-blind prospective investigation was con-
ducted at the Naval Medical Center San Diego (San
Diego, Calif), from August 2001 to April 2002. Fol-
lowing approval from the institutional review board
and an exemption from the US Food and Drug
Administration (IND #63077) to conduct this investi-
gation of a new drug, a total of 64 patients assessed as
ASA class I or II were approached and enrolled in the
study. After initial consent was obtained, subjects
were assigned randomly to a control or experimental
group by using a computer-generated random num-
bers table. Following randomization, an anesthesia
provider ( J.F.B. and J.P.M.) prepared local anesthetic
admixtures and placed them into syringes labeled
with subject number and date and delivered these
syringes to one of the investigators in the study. The
anesthesia provider preparing the solutions main-
tained custody of the randomization list and was not
involved in data collection or block performance,
thereby ensuring that investigators and subjects
remained blinded as to group assignments until con-
clusion of the study. Subjects assigned to the control
group received medications from syringes containing
30 mL of 0.5% bupivacaine with 1:200,000 epineph-
rine, while those in the experimental group received
medications from syringes containing 30 mL of 0.5%
bupivacaine with 1:200,000 epinephrine and 1 g/kg
of clonidine. All subjects then had a femoral-sciatic
nerve block performed with the respective syringes by
one of the investigators (D.J.C. and H.M.C.)
The femoral-sciatic nerve block was performed in
the preoperative block area located immediately adja-
cent to the operative suites. All subjects were placed
in the Sims position on a standard operative gurney,
and standard monitors were used, including a nonin-
vasive blood pressure device, a continuous electrocar-
diogram, and a pulse oximeter. The operative leg was
positioned superiorly and flexed at the knee, and a
line was drawn from the posterior superior iliac spine
to the greater trochanter of the femur. A second line
was drawn from the sacral hiatus to the greater
trochanter, and a third line was drawn perpendicular
to and bisecting the first line. The intersection of the
second and third lines was the point of needle entry
for placement of the sciatic nerve block. The identi-
fied area was prepped with povidone iodine (Beta-
dine) solution and infiltrated with 2 to 3 mL of 1%
lidocaine solution subcutaneously. A 22-gauge, 10-
cm, insulated, B-bevel needle, aimed perpendicular to
the skin, was advanced until posterior tibial nerve dis-
tribution was elicited with the aid of a peripheral
nerve stimulator. A stimulation frequency of 2 Hz and
an intensity level of 1.0 mA were used until a plantar
flexion motor response was elicited. The intensity
level was decreased to less than 0.5 mA while main-
taining the identified motor response. Fifteen milli-
liters of the local anesthetic solution was injected in 5-
mL increments with intermittent syringe aspiration.
After placement of the sciatic nerve block, subjects
were placed in a supine position for placement of the
femoral nerve block. The site of injection was 1 cm
lateral to the femoral artery and 1 cm inferior to the
inguinal ligament. The identified area was prepped
with povidone iodine solution and infiltrated with 2
to 3 mL of 1% lidocaine solution subcutaneously. A
22-gauge, 4-cm, insulated, B-bevel needle was
advanced perpendicular to the skin just lateral to the
artery until femoral nerve distribution was elicited
with the aid of a peripheral nerve stimulator. With a
stimulation frequency of 2 Hz, the intensity level was
set at 1.0 mA until quadriceps extension was elicited,
then decreased to less than 0.5 mA. Fifteen milliliters
of the local anesthetic solution was injected in 5-mL
increments with intermittent syringe aspiration.
Before transport to the operative suite, all blocks
were assessed using pinprick to determine sensory
levels and a modified Bromage scale to determine the
degree of motor blockade. Blocks were considered
successful if no sensation was noted along the femoral
and sciatic dermatomes and a lack of motor strength
www.aana.com/members/journal/ AANA Journal/August 2004/Vol. 72, No. 4 275
was noted when tested. If it was noted that complete
sensory or motor blockade was not present 30 min-
utes following block placement, the block was deter-
mined to be a failure. All data were obtained and
recorded on a data collection sheet. Vital signs,
including blood pressure, heart rate, and oxygen satu-
ration level, were noted and recorded at 5-minute
intervals in the preoperative and operative settings
and recorded on the data collection sheet.
Following block placement, all subjects were taken
to the operating room suite where standard monitors
were reapplied. General anesthesia was administered
according to the following induction protocol: fen-
tanyl, 2 to 3 g/kg intravenously; 2% lidocaine, 1
mg/kg intravenously; and propofol, 2.0 mg/kg intra-
venously. Rocuronium, 0.6 to 1.2 mg/kg intra-
venously, was used to facilitate tracheal intubation.
Anesthesia was maintained with isoflurane, 0.6% to
1.2%, in combination with 50% nitrous oxide and
50% oxygen. Upon completion of the surgical proce-
dure, subjects were transferred to the postanesthesia
care unit. Postoperative pain, if it occurred, was
treated with intravenous fentanyl or intravenous mor-
phine as needed per subject request while subjects
remained in the hospital.
A 0-to-100 numeric rating scale (NRS) was used to
measure pain. Subjects were asked to rate their pain
on the scale; a score of 0 indicated no pain and a
score of 100 indicated the worst pain imaginable.
Subjects were asked to rate their pain preoperatively
and at 5, 7, 9, 11, 13, 15, 17, and 19 hours after place-
ment of the block.
The duration of analgesia was defined as the time
from placement of the femoral-sciatic block to the
first request for analgesic medication. Data about the
first request for analgesics were obtained from the
hospital record if the request was made while the sub-
ject remained in the hospital or, if the patient had
been discharged from the hospital, in a telephone
interview approximately 24 hours postoperatively.
Opioid consumption was measured for the first 24
hours following block placement. Data about anal-
gesic requirements were obtained from the postanes-
thesia care unit and same-day surgical unit records
while subjects remained in the hospital. In addition,
subjects were asked to maintain a record of analgesic
requirements following discharge from the hospital.
These data were obtained in the follow-up telephone
interview approximately 24 hours postoperatively.
Total opioid consumption for the first 24 hours was
calculated and converted to morphine equivalents.
14
Patient satisfaction, as a measure of overall satisfac-
tion with the quality of anesthesia and analgesia pro-
vided, was measured by asking subjects to rate their
satisfaction level based on a 1-to-5 Likert satisfaction
scale that used the following grading criteria: 1, com-
pletely dissatisfied; 2, dissatisfied; 3, somewhat satis-
fied; 4, satisfied; and 5, completely satisfied. This sur-
vey was conducted during a follow-up phone call
approximately 24 hours after placement of the block.
Descriptive statistics were used to analyze demo-
graphic variables. Mean NRS scores between groups
recorded preoperatively and at 5, 7, 9, 11, 13, 15, 17,
and 19 hours following block placement were com-
pared by using t test analysis, as were the mean times of
duration of analgesia between groups and the mean
amounts of analgesic requirements between groups in
24 hours measured in morphine equivalents. Median
patient satisfaction scores measured with a 1-to-5 Lik-
ert scale between groups were compared by using the
Mann-Whitney U test. A P value of less than .05 was
considered significant. Before the investigation, a
power analysis determined that a sample size of 27 sub-
jects per group would be sufficient to detect a difference
in postoperative sensory analgesia of 180 minutes
when a power of 0.8 and an a of .05 were used. After
factoring in an attrition rate of 15%, the final sample
size was set at 64 subjects, or 32 subjects per group.
Results
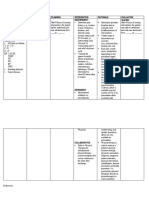
We enrolled 64 subjects in this double-blind investi-
gation. Five subjects in the control group and 4 in the
experimental group experienced failed blocks, and
their data were not included in the analysis. Statistical
analysis was performed on data for the remaining 55
subjects, 27 in the control group and 28 in the exper-
imental group. No significant differences were noted
between groups in the demographic variables of age,
height, weight, sex, or ASA classification (Table).
There were no significant differences between
Bupivacaine Bupivacaine with
(n = 27) clonidine (n = 28)
Age (y) 25.2 4.1 28.5 6.1
Height (cm) 176.9 9.1 176.1 9.0
Weight (kg) 83.1 12.7 86.4 12.1
Sex
Male 26 27
Female 1 1
Table. Demographic data for the study groups*
* Data are given as mean SD, except for sex, which is given as number of
subjects.
276 AANA Journal/August 2004/Vol. 72, No. 4 www.aana.com/members/journal/
groups in mean NRS scores measured preoperatively
or on arrival to the postanesthesia care unit. In addi-
tion, no significant differences were noted between
groups at any of the 2-hour intervals from 5 to 19
hours following block placement (Figure 1).
No statistically significant differences were noted in
the mean duration of analgesia between groups. The
mean duration of analgesia for the control group (bupi-
vacaine without clonidine) was 755 minutes, in com-
parison with 714 minutes for the experimental group
(bupivacaine with clonidine) (P = .758) (Figure 2).
A statistically significant difference was not
observed between groups in the total opioid con-
sumption during the first 24 hours postoperatively.
The control group (bupivacaine without clonidine)
used a mean of 6.98 mg of morphine, compared with
5.1 mg of morphine in the experimental group (bupi-
vacaine with clonidine) (P = .171) (Figure 3).
Patient satisfaction scores reported for the 2 groups
demonstrated no statistically significant differences.
The control group (bupivacaine without clonidine)
reported a median satisfaction score of 4, in compari-
son with 5 for the experimental group (bupivacaine
with clonidine) (P = .063) (Figure 4).
Vital signs were similar between the groups, and no
hemodynamic instability was noted in the preopera-
tive, operative, or postoperative settings. No differ-
ence in the incidence of nausea, vomiting, or somno-
lence was noted between the groups.
Discussion
The addition of 1 g/kg of clonidine to a mixture of
0.5% bupivacaine with 1:200,000 epinephrine in a
combined femoral-sciatic nerve block for patients
undergoing ACL reconstruction did not significantly
decrease NRS scores in this investigation. One possi-
ble explanation for this finding was that reported NRS
scores were surprisingly low at all postblock place-
ment intervals. It is difficult to detect a difference in
pain intensity between groups when subjects in both
groups reported little or no pain. A possible flaw in
the design of this investigation was that NRS scores
Time intervals
M
e
a
n
n
u
m
e
r
i
c
r
a
t
i
n
g
s
c
a
l
e
s
c
o
r
e
s
0
20
40
60
80
100
Bupivacaine
Bupivacaine with clonidine
A
t
f
i
r
s
t
c
o
m
p
l
a
i
n
t
o
f
p
a
i
n
D
i
s
c
h
a
r
g
e
t
o
h
o
m
e
1
9
h
r
1
7
h
r
1
5
h
r
1
3
h
r
1
1
h
r
9
h
r
7
h
r
5
h
r
P
r
e
o
p
e
r
a
t
i
v
e
s
c
o
r
e
Figure 1. Comparison of mean pain intensity scores between groups
Based on a 0-100 numeric rating scale: 0, no pain; 100, worst pain imaginable. No statistically significant difference was
observed between the control (bupivacaine) and experimental (bupivacaine with clonidine) group at each separate time
interval (P > .05). The line extending above each bar represents standard deviation.
PACU = Postanesthesia care unit
www.aana.com/members/journal/ AANA Journal/August 2004/Vol. 72, No. 4 277
were performed only until 19 hours following block
placement. Before the initiation of this investigation,
many anesthesia providers at Naval Medical Center
San Diego estimated the duration of analgesia from a
femoral-sciatic nerve block with bupivacaine for an
ACL reconstruction to be approximately 12 to 18
hours. We did not anticipate the duration of analgesia
to be greater than 19 hours. Interestingly, during fol-
low-up appointments in the orthopedic clinic a num-
ber of subjects reported little or no pain more than 24
hours after block placement. However, the number of
subjects of this anecdotal finding was not recorded. A
statistically significant difference between groups may
have been detected if NRS scores were measured at
intervals past 19 hours, as the blocks began to wear
off. In 1 study, a statistically significant decrease in
postoperative pain scores was demonstrated when
clonidine was added to a brachial plexus nerve
block.
10
Subjects receiving 30, 90, or 300 g of cloni-
dine in a brachial plexus block for carpal tunnel
release reported decreased visual analogue scale
scores compared with subjects in the control group.
10
However, this decrease occurred only 200 minutes
following block placement.
Our investigation also demonstrated that clonidine
did not significantly increase the duration of analgesia
for subjects undergoing ACL repair. This finding,
while not in accordance with the findings of previous
investigations, may suggest that postoperative pain
associated with ACL reconstruction exceeds that of
other surgical procedures in which clonidine has been
used.
8-12
Increasing the dose to 1.5 to 2 g/kg of cloni-
dine may prove to be more efficacious for patients
undergoing ACL reconstruction. This observation is
supported by a study conducted by Goldfarb et al
11
that enrolled 30 subjects undergoing femoral osteo-
0
500
1,000
1,500
Bupivacaine with clonidine Bupivacaine
D
u
r
a
t
i
o
n
o
f
a
n
a
l
g
e
s
i
a
(
m
i
n
)
Bupivacaine
with clonidine
Bupivacaine
Figure 2. Comparison of the mean duration of analge-
sia between groups
Measured from the time of block placement to the first
request for rescue analgesic medication. No statistically
significant difference was observed between the control
(bupivacaine) and experimental (bupivacaine with
clonidine) groups (P > .05). The line extending above
each bar represents standard deviation.
0
5
10
15
Bupivacaine with clonidine Bupivacaine
A
n
a
l
g
e
s
i
a
r
e
q
u
i
r
e
m
n
e
t
s
(
m
g
)
Bupivacaine
with clonidine
Bupivacaine
Figure 3. Comparison of the mean postoperative
analgesic requirements between groups in 24 hours
Total analgesic medication consumption was recorded
and converted to morphine equivalents. No statistically
significant difference was observed between the
control (bupivacaine) and experimental (bupivacaine
with clonidine) groups (P > .05). The line extending
above each bar represents standard deviation.
0.0
2.5
5.0
Bupivacaine with clonidine Bupivacaine
M
e
d
i
a
n
p
a
t
i
e
n
t
s
a
t
i
s
f
a
c
t
i
o
n
s
c
o
r
e
s
Bupivacaine
with clonidine
Bupivacaine
Figure 4. Comparison of median patient satisfaction
scores between groups
Overall patient satisfaction was measured by using a 1-5
Likert scale: 1, completely dissatisfied; 2, dissatisfied;
3, somewhat satisfied; 4, satisfied; 5, completely
satisfied. No statistically significant difference was
observed between the control (bupivacaine) and
experimental (bupivacaine with clonidine) groups
(P > .05).
278 AANA Journal/August 2004/Vol. 72, No. 4 www.aana.com/members/journal/
synthesis. All subjects received a femoral and lateral
femoral cutaneous nerve block with 1 of 3 solutions.
The control group received the block with 30 mL of
0.35% bupivacaine and 250 g of epinephrine, which
resulted in a mean duration of analgesia of 349 min-
utes. The 2 study groups received the block with 30
mL of 0.35% bupivacaine and 150 g of clonidine or
30 mL of 0.35% bupivacaine, 250 g of epinephrine,
and 150 g of clonidine, which resulted in a mean
duration of analgesia of 911 minutes and 1,113 min-
utes, respectively (P < .01).
11
No statistically significant difference was observed
between groups in the total amount of opioid con-
sumption during the first 24 hours postoperatively.
The amount of opioids consumed during the first 24
hours was minimal for both groups. Considering the
amount of pain most patients experience after under-
going ACL reconstruction, the mean amount of mor-
phine equivalents used during the first 24 hours post-
operatively was considerably low, less than 8 mg of
morphine for both groups. This finding provides fur-
ther evidence that a femoral-sciatic block is an effec-
tive adjunct in providing postoperative analgesia for
ACL repair. However, the effect of clonidine on reduc-
ing postoperative analgesic requirements when
administered peripherally with a local anesthetic
remains controversial. A few investigations have
found that the addition of clonidine to a local anes-
thetic for a peripheral nerve block does not reduce the
requirement for postoperative analgesic medica-
tions.
9,12
One investigation demonstrated results in
direct opposition.
15
Clinically, it seems that the most
important determinant of successful postoperative
pain relief after a femoral-sciatic nerve block is the
proximity of the needle to the nerve. Although not
examined in this investigation, it seemed that when
the clinician performing the block was able to elicit a
strong motor response at less than 0.5 mA, subjects
reported a longer duration of analgesia than those
with a weaker motor response at the same setting.
No statistically significant difference was found in
patient satisfaction scores between groups. Subjects
reported high satisfaction scores in both groups. This
investigation was not powered to detect a difference in
patient satisfaction scores using a Likert scale. Despite
this limitation, it was interesting to note that satisfac-
tion scores seemed to be approaching a statistically sig-
nificant difference at the .06 level between groups.
This finding suggests that a femoral-sciatic block for
ACL repair may add to patient satisfaction. Our patient
satisfaction results may have been a misrepresentation
of the data secondary to not including subjects who
experienced failed blocks in the final analysis.
It seems that a femoral-sciatic nerve block alone
provides adequate postoperative analgesia following
ACL reconstruction, and the addition of clonidine to
the block appears to have no additional benefit.
REFERENCES
1. Frost S, Grossfeld S, Kirkley A, Litchfield B, Fowler P, Amendola
A. The efficacy of femoral nerve block in pain reduction for out-
patient hamstring anterior cruciate ligament reconstruction: a
double-blind, prospective, randomized trial. Arthroscopy. 2000;16:
243-248.
2. Edkin BS, Spindler KP, Flanagan JF. Femoral nerve block as an
alternative to parenteral narcotics for pain control after anterior
cruciate ligament reconstruction. Arthroscopy. 1995;11:404-409.
3. Solheim E, Strand T. Postoperative pain after anterior cruciate lig-
ament reconstruction using a transligamentous approach. Am J
Sports Med. 1993;21:507-509.
4. Brown DW, Curry CM, Ruterbories LM, Avery FL, Anson PS. Eval-
uation of pain after arthroscopically assisted anterior cruciate lig-
ament reconstruction. Am J Sports Med. 1997;25:182-186.
5. Tetzlaff JE, Andrish J, OHara J Jr, Dilger J, Yoon HJ. Effectiveness
of bupivacaine administered via femoral nerve catheter for pain
control after anterior cruciate ligament repair. J Clin Anesth. 1997;
9:542-545.
6. Salman MA, Yucebas ME, Coskun F, Aypar U. Day-case
laparoscopy: a comparison of prophylactic opioid, NSAID or local
anesthesia for postoperative analgesia. Acta Anaesthesiol Scand.
2000;44:536-542.
7. Souter AJ, Fredman B, White PF. Controversies in the periopera-
tive use of nonsteroidal anti-inflammatory drugs. Anesth Analg.
1994;79:1178-1190.
8. Eledjam JJ, Deschodt J, Viel EJ, et al. Brachial plexus block with
bupivacaine effects of added alpha-adrenergic agonists: compari-
son between clonidine and epinephrine. Can J. Anaesth. 1991;
38:870-875.
9. Casati A, Magistris L, Fanelli G, et al. Small-dose clonidine prolongs
postoperative analgesia after sciatic-femoral nerve block with 0.75%
ropivacaine for foot surgery. Anesth Analg. 2000;91: 388-392.
10. Bernard JM, Macaire P. Dose-range effects of clonidine added to lido-
caine for brachial plexus block. Anesthesiology. 1997;87:277-284.
11. Goldfarb G, Ang E, Debaene B, Galet C, Jolis P. Duration of anal-
gesia after femoral nerve block with bupivacaine: effect of cloni-
dine added to the anesthetic solution [abstract]. Anesthesiology.
1989;71:A643.
12. .Singelyn FJ, Gouverneur JM, Robert A. A minimum dose of cloni-
dine added to mepivacaine prolongs the duration of anesthesia
and analgesia after axillary brachial plexus block. Anesth Analg.
1996;83:1046-1050.
13. Klimscha W, Chiari A, Krafft P, et al. Hemodynamic and analgesic
effects of clonidine added repetitively to continuous epidural and
spinal blocks. Anesth Analg. 1995;80:322-327.
14. Reisine T, Pasternak G. Opioid analgesics and antagonists. In:
Hardman JG, Limbird LE, Molinoff PB, Ruddon RW, AG, eds.
Goodman & Gilmans The Pharmacological Basis of Therapeutics.
9th ed. New York, NY: McGraw-Hill; 1996:535.
15. Reuben SS, Connely NR. Postoperative analgesia for outpatient
arthroscopic knee surgery with intraarticular clonidine. Anesth
Analg. 1999;88:729-733.
AUTHORS
LT Darren J. Couture, CRNA, MSN, NC, USNR, is a staff nurse anes-
thetist at Naval Hospital Bremerton, Wash.
LT Heather M. Cuniff, CRNA, MSN, NC, USNR, is staff nurse anes-
thetist at Naval Hospital Camp Pendleton, Calif.
LCDR Joseph F. Burkard, CRNA, MSN, NC, USN, is clinical coor-
dinator, Navy Nurse Corps Anesthesia Program, San Diego, Calif.
LCDR John P. Maye, CRNA, PhD, NC, USN, is director of Research,
Naval Postgraduate Dental School, Bethesda, Md.
CDR Joseph Pellegrini, CRNA, DNSc, NC, USN, is director of
Research, Navy Nurse Corps Anesthesia Program, Bethesda, Md.
DISCLAIMER
The views expressed in this article are those of the authors and do not
reflect the official policy or position of the Department of the Navy,
Department of Defense, or the US Government.
Potrebbero piacerti anche
- Eledjam1991 Article BrachialPlexusBlockWithBupivac PDFDocumento6 pagineEledjam1991 Article BrachialPlexusBlockWithBupivac PDFKalpanaNessuna valutazione finora
- 11 LdpopDocumento5 pagine11 LdpopBaru Chandrasekhar RaoNessuna valutazione finora
- Levobupivacaine and Bupivacaine in Spinal Anesthesia For Transurethral Endoscopic SurgeryDocumento7 pagineLevobupivacaine and Bupivacaine in Spinal Anesthesia For Transurethral Endoscopic SurgeryCassandraBussinkNessuna valutazione finora
- Effectiveness of Fascia Iliaca Compartment Block For Post Operative Analgesia After Surgery For Femur Bone FractureDocumento12 pagineEffectiveness of Fascia Iliaca Compartment Block For Post Operative Analgesia After Surgery For Femur Bone FractureIJAR JOURNALNessuna valutazione finora
- Synopsis DR ABCDocumento8 pagineSynopsis DR ABCFiaz medicoNessuna valutazione finora
- JAnaesthClinPharmacol294459-335648 091924 PDFDocumento6 pagineJAnaesthClinPharmacol294459-335648 091924 PDFaltaikhsannurNessuna valutazione finora
- Anesth Essays ResDocumento8 pagineAnesth Essays ResFi NoNessuna valutazione finora
- Bahan KedkelDocumento8 pagineBahan KedkelUliza Nur AiniNessuna valutazione finora
- Cervical Epidural Anaesthesia For Shoulder Arthroscopy and Effective Postoperative Physiotherapy For A Frozen Shoulder: A Case StudyDocumento4 pagineCervical Epidural Anaesthesia For Shoulder Arthroscopy and Effective Postoperative Physiotherapy For A Frozen Shoulder: A Case StudySutiyono TyoNessuna valutazione finora
- Continuous Pericapsular Nerve Group Block For Hip Surgery: A Case SeriesDocumento17 pagineContinuous Pericapsular Nerve Group Block For Hip Surgery: A Case SeriesVivek Vishal SahNessuna valutazione finora
- Tangtiphaiboontana 2021Documento8 pagineTangtiphaiboontana 2021翁嘉聰Nessuna valutazione finora
- Effect of Dexamethasone On The Duration of Interscalene Nerve Blocks With Ropivacaine or BupivacaineDocumento8 pagineEffect of Dexamethasone On The Duration of Interscalene Nerve Blocks With Ropivacaine or BupivacaineIda KatarinaNessuna valutazione finora
- Anes 10 3 9Documento7 pagineAnes 10 3 9ema moralesNessuna valutazione finora
- Small-Dose Ketamine Infusion Improves Postoperative Analgesia and Rehabilitation After Total Knee ArthroplastyDocumento6 pagineSmall-Dose Ketamine Infusion Improves Postoperative Analgesia and Rehabilitation After Total Knee ArthroplastyArturo AlcantaraNessuna valutazione finora
- Bloqueo Pec 2 MamaDocumento9 pagineBloqueo Pec 2 Mamapalomisgarcia1995Nessuna valutazione finora
- JAnaesthClinPharmacol37163-254754 000414Documento4 pagineJAnaesthClinPharmacol37163-254754 000414Ferdy RahadiyanNessuna valutazione finora
- Br. J. Anaesth.-2009-Foss-111-6Documento6 pagineBr. J. Anaesth.-2009-Foss-111-6alejandropst1664Nessuna valutazione finora
- PRM2017 1721460 PDFDocumento6 paginePRM2017 1721460 PDFmikoNessuna valutazione finora
- Musa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim NasseriDocumento6 pagineMusa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim Nasseridebby claudiNessuna valutazione finora
- Comparison of Analgesic Effects of Intravenous Nalbuphine and Pentazocine in Patients Posted For Short-Duration Surgeries A Prospective Randomized Double-Blinded StudyDocumento4 pagineComparison of Analgesic Effects of Intravenous Nalbuphine and Pentazocine in Patients Posted For Short-Duration Surgeries A Prospective Randomized Double-Blinded StudyMuhammad AtifNessuna valutazione finora
- SynopsisDocumento14 pagineSynopsisAqeel AhmadNessuna valutazione finora
- Adjunct Analgesia Reduces Pain and Opioid Consumption After Hip ArthrosDocumento14 pagineAdjunct Analgesia Reduces Pain and Opioid Consumption After Hip ArthrosFelipeSanzanaNessuna valutazione finora
- IJISRT23JUN363Documento7 pagineIJISRT23JUN363International Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- The Effectiveness of Magnesium Sulphate Intravenous Bolus or Added As An Adjunct To Ropivacaine For Brachial Plexus Block in Upper Limb Orthopaedic SurgeriesDocumento7 pagineThe Effectiveness of Magnesium Sulphate Intravenous Bolus or Added As An Adjunct To Ropivacaine For Brachial Plexus Block in Upper Limb Orthopaedic SurgeriesInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Critical AppraisalDocumento13 pagineCritical AppraisalRatna Widiyanti KNessuna valutazione finora
- Effects of Hand Massage On Anxiety in Cataract Surgery Using Local AnesthesiaDocumento7 pagineEffects of Hand Massage On Anxiety in Cataract Surgery Using Local AnesthesiaJuhendriDwiAGNessuna valutazione finora
- Comparative Study of Intrathecal Sufentanil Bupivacaine Versus Intrathecal Bupivacaine in Patients Undergoing Elective Cesarean SectionDocumento5 pagineComparative Study of Intrathecal Sufentanil Bupivacaine Versus Intrathecal Bupivacaine in Patients Undergoing Elective Cesarean SectiontamiNessuna valutazione finora
- Research ArticleDocumento10 pagineResearch ArticlethiaNessuna valutazione finora
- Low Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate SurgeryDocumento6 pagineLow Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate Surgeryblabarry1109Nessuna valutazione finora
- Amalia 163216 - Journal ReadingDocumento26 pagineAmalia 163216 - Journal ReadingGhifari FarandiNessuna valutazione finora
- Ael 370Documento5 pagineAel 370Devanti EkaNessuna valutazione finora
- Mode of Action of Cupping - Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy SubjectsDocumento14 pagineMode of Action of Cupping - Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy Subjectsdwi putri ratehNessuna valutazione finora
- Continuous Peripheral Nerve Block For PoDocumento5 pagineContinuous Peripheral Nerve Block For PoBinNessuna valutazione finora
- JAnaesthClinPharmacol312191-1284204 033402Documento5 pagineJAnaesthClinPharmacol312191-1284204 033402Rusman Hadi RachmanNessuna valutazione finora
- Hyperbaric Spinal For Elective Cesarean Section: - Ropivacaine Vs BupivacaineDocumento13 pagineHyperbaric Spinal For Elective Cesarean Section: - Ropivacaine Vs BupivacaineYayaNessuna valutazione finora
- Supraclavicular Brachial Plexus BlockDocumento2 pagineSupraclavicular Brachial Plexus BlockmagedemanNessuna valutazione finora
- Celecoxib & Ketoprofen For Pain ManagementDocumento8 pagineCelecoxib & Ketoprofen For Pain ManagementUbaidillah AfiffNessuna valutazione finora
- 1 s2.0 S0883540318311537 MainDocumento6 pagine1 s2.0 S0883540318311537 MainSavNessuna valutazione finora
- Anasthesia 1Documento7 pagineAnasthesia 1Rionald SitompulNessuna valutazione finora
- Toxina en Sindrome Dolor RegionalDocumento7 pagineToxina en Sindrome Dolor RegionalPatricio LoyolaNessuna valutazione finora
- 14Documento10 pagine14Juliana ObandoNessuna valutazione finora
- Comparison of Clonidine and Fentanyl As An Adjuvant To Bupivacaine in Unilateral Spinal AnaesthesiaDocumento11 pagineComparison of Clonidine and Fentanyl As An Adjuvant To Bupivacaine in Unilateral Spinal AnaesthesiaYadin SabudiNessuna valutazione finora
- Anjali Bhure, Neelakshi Kalita, Prasad Ingley, C.P. Gadkari: Research ArticleDocumento5 pagineAnjali Bhure, Neelakshi Kalita, Prasad Ingley, C.P. Gadkari: Research ArticleTedja PrakosoNessuna valutazione finora
- Mode of Action of Cupping Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy Subjects 2014Documento11 pagineMode of Action of Cupping Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy Subjects 2014silkofosNessuna valutazione finora
- Rawal Medical JournalDocumento8 pagineRawal Medical JournalBahRunNessuna valutazione finora
- Which Treatment Approach Is Better For Hemiplegic Shoulder Pain in Stroke PatientsDocumento10 pagineWhich Treatment Approach Is Better For Hemiplegic Shoulder Pain in Stroke PatientsDiego Pinto PatroniNessuna valutazione finora
- 9829 CE (Ra) F (SH) PF1 (SNAK) PFA (P)Documento4 pagine9829 CE (Ra) F (SH) PF1 (SNAK) PFA (P)razaqhussain00Nessuna valutazione finora
- Revista Brasileira DE AnestesiologiaDocumento9 pagineRevista Brasileira DE AnestesiologiayulianiNessuna valutazione finora
- Xia 2018Documento7 pagineXia 2018Jefferson891127Nessuna valutazione finora
- Cont Infusion Vs Mand Bolus W PCEADocumento6 pagineCont Infusion Vs Mand Bolus W PCEAk3 rschNessuna valutazione finora
- Pulsed Radiofrequency ofDocumento8 paginePulsed Radiofrequency ofDiego Pinto PatroniNessuna valutazione finora
- Caudal Anesthesia in PediatricDocumento7 pagineCaudal Anesthesia in PediatricDavid PesireronNessuna valutazione finora
- Spinal Anaesthesia For Ambulatory Arthroscopic Surgery of The KneeDocumento6 pagineSpinal Anaesthesia For Ambulatory Arthroscopic Surgery of The KneeGustavo MosqueraNessuna valutazione finora
- Comparison of Surgical Outcome and Complications Between Spinal and General Anaesthesia For Patients Undergoing Percutaneous NephrolithotomyDocumento5 pagineComparison of Surgical Outcome and Complications Between Spinal and General Anaesthesia For Patients Undergoing Percutaneous Nephrolithotomynaufal12345Nessuna valutazione finora
- Articulo Revision Medicina en Ortopedia y TraumaDocumento43 pagineArticulo Revision Medicina en Ortopedia y TraumaAfra Eslis NoatoNessuna valutazione finora
- 4services On DemandDocumento9 pagine4services On DemandDe WiNessuna valutazione finora
- Obstetrical Analgesia Word 2Documento10 pagineObstetrical Analgesia Word 2Top MusicNessuna valutazione finora
- Suprascapular Nerve Block Versus Steroid Injection For Non-Specific Shoulder PainDocumento7 pagineSuprascapular Nerve Block Versus Steroid Injection For Non-Specific Shoulder PainTri KurniawanNessuna valutazione finora
- JurnalDocumento5 pagineJurnalFuchsia ZeinNessuna valutazione finora
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYDa EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNessuna valutazione finora
- Controversiesindental Traumatology: Orrett E. OgleDocumento15 pagineControversiesindental Traumatology: Orrett E. OglechannadrasmaNessuna valutazione finora
- NCP Multple MyelomaDocumento2 pagineNCP Multple Myelomavia macarioNessuna valutazione finora
- Case01.Acute PainDocumento56 pagineCase01.Acute PainshairaorquetaNessuna valutazione finora
- Arero Primary Hospital Pain MGT ProtocolDocumento9 pagineArero Primary Hospital Pain MGT Protocolsami ketemaNessuna valutazione finora
- Lisa Johnson, Ba, SRS, Latg Certification Review Session 2010 Asr Annual Meeting Clearwater Beach, FLDocumento33 pagineLisa Johnson, Ba, SRS, Latg Certification Review Session 2010 Asr Annual Meeting Clearwater Beach, FLAnonymous cCMY2pNessuna valutazione finora
- Bioorganic & Medicinal Chemistry Letters: SciencedirectDocumento6 pagineBioorganic & Medicinal Chemistry Letters: SciencedirectjubvvNessuna valutazione finora
- Memorias LavecDocumento288 pagineMemorias Lavecsbc27Nessuna valutazione finora
- 5863-Article Text-11079-1-10-20130211Documento13 pagine5863-Article Text-11079-1-10-20130211Pram PramonoNessuna valutazione finora
- English Pre-Test: Nat Takes A NapDocumento13 pagineEnglish Pre-Test: Nat Takes A NapJayvee Wynne VergaraNessuna valutazione finora
- Comparison of Octreotide and Hyoscine in Controlling Gastrointestinal Symptoms Due To Malignant Inoperable Bowel ObstructionDocumento4 pagineComparison of Octreotide and Hyoscine in Controlling Gastrointestinal Symptoms Due To Malignant Inoperable Bowel ObstructionThiago GomesNessuna valutazione finora
- What Are The Therapeutic Classes of DrugsDocumento3 pagineWhat Are The Therapeutic Classes of DrugsFrank GomesNessuna valutazione finora
- Drug StudyDocumento5 pagineDrug StudySarie LevitaNessuna valutazione finora
- Maste Med SheetDocumento78 pagineMaste Med SheetBarbie Wiggers100% (1)
- CNS Drugs TextDocumento27 pagineCNS Drugs TextTina TalmadgeNessuna valutazione finora
- Perioperative Nursing Hand Out - Postop-1Documento22 paginePerioperative Nursing Hand Out - Postop-1Jamie NarcisoNessuna valutazione finora
- Syiva Auliya Anjani (Critical Appraisal) JurnalDocumento11 pagineSyiva Auliya Anjani (Critical Appraisal) JurnalRagil SaputroNessuna valutazione finora
- Forensic Medicine & Toxicology - Topical Past PapersDocumento24 pagineForensic Medicine & Toxicology - Topical Past PapersRohama Qubra 279Nessuna valutazione finora
- BURN PAIN - Pain Management Made Incredibly EasyDocumento2 pagineBURN PAIN - Pain Management Made Incredibly EasySakura Kimono100% (1)
- MCQ Pathways9th.IDocumento4 pagineMCQ Pathways9th.Iareej alblowi100% (1)
- KetamineDocumento4 pagineKetamineapi-235915759Nessuna valutazione finora
- PNDFDocumento315 paginePNDFXharisz Dulin100% (3)
- Fact Sheet Painful Peripheral NeuropathyDocumento6 pagineFact Sheet Painful Peripheral Neuropathyasdar fajrinNessuna valutazione finora
- Crash Course - General PharmacologyDocumento62 pagineCrash Course - General PharmacologyDhanesh VijayaraghavanNessuna valutazione finora
- Different Kinds of Drugs and Its EffectsDocumento13 pagineDifferent Kinds of Drugs and Its EffectsSapo KurtNessuna valutazione finora
- Audio AnalgesiaDocumento7 pagineAudio AnalgesiaRisana RahoofNessuna valutazione finora
- College of Arts and Sciences Nursing Department: InstructionDocumento3 pagineCollege of Arts and Sciences Nursing Department: InstructionJoevence Gazo CuaresmaNessuna valutazione finora
- Narcotics ClassificationDocumento23 pagineNarcotics Classificationzohaib hassan100% (2)
- POSTER Tramadol A2 PRINT PDFDocumento1 paginaPOSTER Tramadol A2 PRINT PDFJohnny ZinzNessuna valutazione finora
- PT - Mapeh 6 - Q4Documento8 paginePT - Mapeh 6 - Q4Arnold GradoNessuna valutazione finora
- Multimodal Analgesia A CL 2022Documento14 pagineMultimodal Analgesia A CL 2022Alejandra SanchezNessuna valutazione finora