Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
0008 - JRS - Waring - Standard Graphs For Reporting Refractive Surgery
Caricato da
Kyros1972Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
0008 - JRS - Waring - Standard Graphs For Reporting Refractive Surgery
Caricato da
Kyros1972Copyright:
Formati disponibili
SPECIAL ARTICLE
Standard Graphs for Reporting Refractive Surgery
George O. Waring III, MD, FACS, FRCOphth
ne of the most difcult problems facing refractive surgeons is comparison of results among refractive surgical procedures. The need for accurate comparisons among different studies is especially acute because of the increasing variety of refractive surgical techniques and procedures. For example, how can refractive surgeons know how to compare the outcomes of laser in situ keratomileusis (LASIK) surgery with the Nidek EC-5000 scanning excimer laser to those with an Autonomous LadarVision ying spot laser or a Bausch & Lomb 217Z Zyoptics wavefront-guided laser? If the refractive results with the Nidek laser are reported as the number of eyes 0.50 diopter (D) of desired outcome, those with the Autonomous laser as the mean spherical equivalent refraction, and those with the Bausch & Lomb as the number of eyes 1.00 D of desired outcome, the surgeon has no basis for comparison of these refractive outcomes, and is left guessing. In 1992, I published a monograph suggesting standard methods for reporting refractive surgical procedures (Waring GO. Standardized data collection and reporting for refractive surgery. Refract Corneal Surg 1992;8(suppl):1-42). These standards were never widely adopted, and authors and companies reported their ndings in a variety of ways, sometimes confusing. For example, some reported only the number of eyes that saw 20/25 uncorrected, obviously because the results looked much better than they would if the standard 20/20 or better criterion were used. None of the ophthalmic societies or standards organizations have made a formal proposal for standardized reporting of refractive surgery results. No journal has required its authors to present material in a standardized manner that would allow comparison among articles (Koch D,
From Inview, Atlanta, Ga. Correspondence: George O. Waring III, MD, FACS, FRCOphth, Inview, 301 Perimeter Center North, Ste 600, Atlanta, GA 30346. Tel: 678.222.5102; Fax: 404.250.9006; E-mail: drgeorge@georgewaring.com
Kohnen T, Obstbaum S, Rosen ES. Format for reporting refractive surgical data. J Cataract Refract Surg 1998;24:285-287). Therefore, to simplify matters, I propose here a set of six standard graphs* that should be included in any paper reporting the results of a series of cases. The idea is simple for authors to adopt, easy for editors to insist upon, and friendly for readers to digest. Graphs from different papers can be arranged side by side, allowing a direct visual comparison of the outcomes of different procedures and techniques. This idea was proposed initially by Thomas Neuhann, MD. The specic graphs and their presentation have been developed by joint efforts of the editorial staffs of the Journal of Refractive Surgery and the Journal of Cataract and Refractive Surgery, including Drs Wallace Chamon, Daniel Epstein, Jack Holladay, Michael Knorz, Thomas Kohnen, Doug Koch, Ron Krueger, Stephen Obstbaum, Jeffrey Robin, Emanuel Rosen, Jonathan Talamo, and myself. Such a requirement imposes an additional burden on the authors, but assists them in their ultimate goal clear communication of their ndings. The Table (pg. 465) presents sources of software that authors can use to generate these graphs. All graphs can be created easily except the scattergram, which requires some special consideration. Each gure is arranged with clearly labeled X and Y axes with the units of measure. Relevant numerical information is present within the graph itself so that the numbers can be read directly from the graph, rather than requiring the reader to search along the Y axis for the actual number. A box within the graph presents the number of eyes and follow-up time (112 consecutive eyes at 3 months in the examples), so the population reported is immediately identied. Relevant summary numbers are presented in a second box to allow the reader to see the answer at a quick glance.
*Updated June 2005.
Journal of Refractive Surgery Volume 16 July/August 2000
459
Standard Graphs for Reporting Refractive Surgery/Waring
-16 -14 -12 -10
112 eyes 3 months postop
OVERCORRECTED
Achieved (D)
-8 -6 -4 -2 0
0 -2 -4 -6 -8 -10 -12 -14 -16
UNDERCORRECTED
Attempted (D)
16 14 12
Achieved (D)
112 eyes 3 months postop
OVERCORRECTED
10 8 6 4 2 0 0 2 4 6 8 Attempted (D) 10 12 14 16 UNDERCORRECTED
B
Figure 1. Scattergrams of attempted vs. achieved refraction Scattergrams have the advantage of presenting the outcome of every eye, so that nothing is lost in means or averages and outliers can be easily identied. Since the most important outcome of refractive surgery is the refraction, we selected the scattergram of the attempted refractive change vs. the achieved refractive change for each eye. For a scattergram to accurately represent the outcome visually, the scale of the X and Y axes must be the same (A). Unfortunately, many software programs do not allow this presentation, usually allowing a larger spread along the X axis than along the Y axis (B). Authors should make every attempt to keep the X and Y axes on the same scale (A), but it may be necessary to accept disparate axis scales (B). Source of Data for Example Graphs
The data displayed in the various graphs are from the Emory Vision Correction Center, Atlanta, Georgia, an early series of eyes done with the Nidek EC-5000 laser and the Chiron Automated Corneal Shaper microkeratome for the correction of myopia. The series of 112 consecutive eyes at 3 months after laser in situ keratomileusis (LASIK) are part of a larger study, and the data are not presented to represent overall clinical results from the series, but rather are selected only to create the graphic examples.
460
journalofrefractivesurgery.com
Standard Graphs for Reporting Refractive Surgery/Waring
100 90 80 70
112 eyes 3 months postop
0.50 D: 60% 1.00 D: 79%
% of Eyes
60 50 40 30 20 10 0
0 4 15 10 4 0 0 50
-3 to -2.10
-2 to -1.10
-1 to -0.51
-0.50 to +0.1 to +0.51 to +1.10 to 0.00 +0.50 +1 +2
+2.10 to +3
Postoperative Spherical Equivalent Refraction (D)
Figure 2. Spherical equivalent refractive outcome bar graph
This bar graph represents the postoperative spherical equivalent refraction in small steps. It is possible to take the data in the graph and see easily how many eyes fall within whatever categories the reader wishes to quantify: plano to 0.50 D, 0.50 D, 1.00 D. The full range of refractive results is also presented. At the present time, the gold standard for refractive outcome is to be within 0.50 D of the desired result, and this number is displayed in the summary box. In the future, a more exact summary number may be used.
Journal of Refractive Surgery Volume 16 July/August 2000
461
Standard Graphs for Reporting Refractive Surgery/Waring
100 90 80 70
% of Eyes 87.4 112 eyes 3 months postop 63
95.8
98.3
100
< 0.50 D: 35% < 1.00 D: 63%
60 50 40 30 20 10 0
0.50 34.5
Postoperative Defocus Equivalent Refraction (D)
Figure 3. Defocus equivalent bar graph
Refractive outcome is commonly reported as the spherical equivalent refraction, which is computed as the spherical component added to one-half of the cylindrical component, respecting the sign of the cylinderbut this can be misleading. For example, two eyes after a refractive surgical procedure may have refractions of: Eye #1, 1.00 2.00 90, and Eye #2, 1.00 2.00 180; the spherical equivalent refraction of Eye #1 is plano clearly a perfect result, whereas the spherical equivalent refraction of Eye #2 is 2.00 D, not a very good outcome. Of course, the plano representation of Eye #1 is misleading because of the residual astigmatism. This problem is solved by computing the defocus equivalent, which is simple to compute. To get the spheroequivalent, take the sphere [respecting sign], and add half the cylinder [respecting sign]. Then, to calculate the defocus equivalent, take the spheroequivalent and add one-half of the cylinder, ignoring the sign. Thus, in the above example, the defocus equivalent of Eye #1 is 1.00 D, and the defocus equivalent of Eye #2 is 3.00 D (note there is no sign); the defocus equivalent values more accurately represent the reality of the refractive state of the two eyes. The defocus equivalent bar graph is presented as a cumulative graph, building in one direction and presenting the number of eyes with a given defocus equivalent value. The defocus equivalent was rst dened by Holladay et al in 1991 (Holladay JT, Lynn MJ, Waring GO, Gemmill M, Keehn CG, Fielding B. The relationship of visual acuity, refractive error, and pupil size after radial keratotomy. Arch Ophthalmol 1991;109:70-76) to eliminate the inequity between eyes that had similar spheroequivalent refractions but different amounts of astigmatism. The defocus equivalent is proportional to the area of the blur circle of the conoid of Sturm. [Updated 5/2001]
462
journalofrefractivesurgery.com
Standard Graphs for Reporting Refractive Surgery/Waring
102 eyes 3 months postop
Preop SCVA Postop UCVA
97 89 99 100 93 95 96 98 99 100
100 90 80
% of Eyes
81
72
85
70 60 50 40 30 20 10 0
10 2 4 35 45
17 4 12.5 16 20 25 30 40 50 60 80 100 200 400
10
Cumulative Snellen Visual Acuity (20/_)
Figure 4. Uncorrected visual acuity bar graph The bar graph depicting visual acuity has two components. Component #1 is the spectacle-corrected visual acuity at baseline; this is important because it is helpful to know the overall visual potential of the population before looking at the postoperative vision. For example, consider a group of eyes with a baseline refraction of 1.00 to 4.00 D that are receiving intracorneal ring segments; the vast majority of these eyes will be able to see 20/20 or better with spectacle correction before surgery. Contrast this to a group of eyes with a refraction of 15.00 to 25.00 D that are receiving a phakic intraocular lens. It is likely that less than half of these eyes can see 20/40 or better with spectacle correction before surgery. Thus, interpreting the postoperative uncorrected visual acuity results would be different in these two populations, the number of eyes seeing 20/20 or better without correction being a fair and appropriate criterion to apply to the low myopia eyes receiving intracorneal ring segments, but a less appropriate criterion applied to high myopia eyes that receive phakic intraocular lens. Component #2 is a cumulative bar graph of uncorrected visual acuities after surgery. The visual acuities begin at 20/10 and proceed in log units. This is important because as refractive surgery improves, the goal is to identify accurately the number of eyes that see 20/10, 20/12.5, 20/16, and 20/20; these ner distinctions will be used more and more to differentiate among refractive surgery procedures. The X axis represents the full spectrum of visual acuities as demonstrated on the National Eye Institute Vision charts, and as more ofces and clinics adopt these charts as the standard for measuring visual acuity, it will be easier to make sense of the measurement. As long as different studies use different visual acuity charts under different testing circumstances, comparison of visual acuities among studies will be somewhat awed. Of course, if one wishes to eliminate the effects of magnication and optical distortion and vertex power imposed by spectacle lenses, especially in high ametropes, a preoperative contact lens-corrected visual acuity would be the most appropriate standard for comparison to postoperative uncorrected visual acuity.
Journal of Refractive Surgery Volume 16 July/August 2000
463
Standard Graphs for Reporting Refractive Surgery/Waring
60 50
% of Eyes 112 eyes 3 months postop
58.8
40 30 20 10 0
2 or more lines lost 0.8%
25.4
10 5 0 -3 0.8 -2 -1 0 1 2 0 3
Change in Snellen lines of visual acuity
Figure 5. Change in spectacle-corrected visual acuity bar graph The bar graph depicts the change in spectacle-corrected visual acuity from baseline to the postoperative examination in terms of the number of Snellen lines changed. This is the most commonly used measure of safety because it answers the question, If the refractive outcome is not totally acceptable, can the patient put glasses on again and see as well as they did before surgery? A change of 1 Snellen line is within the range of normal biological variability for repeated measures, and therefore is not a meaningful change. A change of 2 or more Snellen lines has been generally adopted as the standard for safety, and is reported in the summary box. Some groups recommend reporting a loss of more than 2 lines as the standard, which of course makes it easier to have a safe procedure. Ideally, this change would be measured by counting the total number of letters seen on the chart and computing a Snellen line equivalent.
464
journalofrefractivesurgery.com
Standard Graphs for Reporting Refractive Surgery/Waring
+2
Spherical Equivalent Refraction (D)
0 -2
112 eyes
-4 -6 -8
Preop 2 wk Time After Surgery 3 mo 6 mo Eyes change 0.50 D 3.5%, 2 wk to 6 mo
Figure 6. Stability of refraction graph The timeline depicts the mean spherical equivalent refraction and one standard deviation depicted by the error bars at various intervals after surgery. This allows determination of stability of the refraction, but the intervals chosen and the time depicted will depend on examination frequency in any given series. Percent of eyes that changed by 0.50 D is given for the total follow-up time in the summary box. The error bars are important because a wide spread of the standard deviation would show that there is considerable instability in the refraction, even though the means may show minimal change over time.
TABLE
Standard Graph Software Sources*
Outcomes Analysis Software, Inc. PO Box 1097 Rancho Santa Fe, CA 92067, USA Tel/Fax: 858.856.4462; E-mail: garrett23@aol.com Datagraph med (Medical Data Analysis Software) Ingenieurbro Pieger Treidelsweg 8, D-90530 Wendelstein, Germany Tel: 49.9129.27382; Fax: 49.9129.27163; E-mail: pieger@csi.com SigmaPlot, SPSS Science Excel, Microsoft Corporation
The Journal of Refractive Surgery provides no specific endorsement of the above listed software packages.
Journal of Refractive Surgery Volume 16 July/August 2000
465
Standard Graphs for Reporting Refractive Surgery/Waring
-16 -14 -12 -10
100
112 eyes 3 months postop
90 80
% of Eyes
70 60 50 40 30 20
112 eyes 3 months postop
50
0.50 D: 60% 1.00 D: 79%
OVERCORRECTED
Achieved (D)
-8 -6 -4 -2 0
0 -2 -4 -6 -8 -10 -12 -14 -16
15 10 0
-3 to -2.10
UNDERCORRECTED
10 0
4
-2 to -1.10 -1 to -0.51
-0.50 to +0.1 to +0.51 to +1.10 to +2.10 to 0.00 +0.50 +1 +2 +3
Postoperative Spherical Equivalent Refraction (D)
Spherical equivalent refractive outcome bar graph 102 eyes 3 months postop
98.3 100
Attempted (D)
Scattergram of attempted vs. achieved refraction Preop SCVA Postop UCVA
97 89 81 72 85 99 100 93 95 96 98 99 100
100 90 80 70
112 eyes 3 months postop
63 87.4
95.8
100 90 80 70 60 50 40 30 20 10 0
10 2 4 4 17 35 45
% of Eyes
60 50 40 30 20 10 0
0.50
34.5
% of Eyes
< 0.50 D: 35% < 1.00 D: 63%
10
12.5
16
20
25
30
40
50
60
80
100
200
400
Postoperative Defocus Equivalent Refraction (D)
Defocus equivalent bar graph
58.8
Cumulative Snellen Visual Acuity (20/_)
Visual acuity bar graph (SCVA = spectacle corrected visual acuity, UCVA = uncorrected visual acuity)
60 50
112 eyes 3 months postop
% of Eyes
40 30 20 10 0
2 or more lines lost 0.8%
Spherical Equivalent Refraction (D)
+2 0 -2
112 eyes
25.4
-4 -6 -8
Preop 2 wk 3 mo 6 mo
10 5 0
-3
Eyes change 0.50 D 3.5%, 2 wk to 6 mo
0.8
-2 -1 0 1 2
0
3
Change in Snellen lines of visual acuity
Change in spectacle-corrected visual acuity bar graph
Time After Surgery
Stability of refraction graph. Error bars indicate one standard deviation.
Figure 7. Composite plate All six graphs can be presented on one page of a standard sized journal. This would allow the reader to scan easily the six gures to get the overall graphic picture of the major outcome variables. In addition, single pages from different articles could be displayed side by side for rapid visual comparison on the results. 466
journalofrefractivesurgery.com
Potrebbero piacerti anche
- Preschool Sensory Resource - 0Documento3 paginePreschool Sensory Resource - 0Damayanti ThapaNessuna valutazione finora
- Diopsys NOVA Operator's ManualDocumento139 pagineDiopsys NOVA Operator's ManualLuis100% (1)
- Iol Power Calculation Warren HillDocumento4 pagineIol Power Calculation Warren HillMariana Luzardo bravoNessuna valutazione finora
- OCANZ Sept 2007 Paper 2Documento4 pagineOCANZ Sept 2007 Paper 2Ben Joon100% (3)
- The Routine LASIK ProcedureDocumento71 pagineThe Routine LASIK ProcedureLondon Vision Clinic100% (3)
- White Intumescent Cataract Management: My Approach: 2022, #1Da EverandWhite Intumescent Cataract Management: My Approach: 2022, #1Nessuna valutazione finora
- MCQ Ophthalmo WITH AnswersDocumento3 pagineMCQ Ophthalmo WITH AnswersEddie Lim100% (1)
- LASIK Surgery Is Safe in The Long-TermDocumento103 pagineLASIK Surgery Is Safe in The Long-TermLondon Vision Clinic100% (1)
- OtologiDocumento13 pagineOtologimr_curiousityNessuna valutazione finora
- Eye Care CentreDocumento5 pagineEye Care CentreRuni ANessuna valutazione finora
- Phakic Intraocular Lens Implantation Patient Leaflet April2017Documento11 paginePhakic Intraocular Lens Implantation Patient Leaflet April2017Lilianty FauziNessuna valutazione finora
- Understanding Diopsys FfERG Fixed Luminance ReportsDocumento6 pagineUnderstanding Diopsys FfERG Fixed Luminance ReportssalsomanoNessuna valutazione finora
- Contact Lenses For ChildrenDocumento6 pagineContact Lenses For ChildrenmelikebooksNessuna valutazione finora
- 1112CRSTEuro Cs VinciguerraDocumento3 pagine1112CRSTEuro Cs VinciguerraR Andres Plaza ZNessuna valutazione finora
- Effect of Corneal Asphericity and Spherical Aberration On Intraocular Lens Power CalculationsDocumento2 pagineEffect of Corneal Asphericity and Spherical Aberration On Intraocular Lens Power Calculationsr2201cNessuna valutazione finora
- Calculation of Toric Intraocular Lenses Using Multivariate RegressionDocumento9 pagineCalculation of Toric Intraocular Lenses Using Multivariate RegressionRonald PuchaNessuna valutazione finora
- Retrospective Analysis of Wavefront Optimized Myopic LASIK Comparison of Preoperative To Postoperative AstigmatismDocumento9 pagineRetrospective Analysis of Wavefront Optimized Myopic LASIK Comparison of Preoperative To Postoperative AstigmatismAthenaeum Scientific PublishersNessuna valutazione finora
- Laser in Situ Keratomileusis For Astigmatism 0.75 Diopter Combined With Low Myopia: A Retrospective Data AnalysisDocumento9 pagineLaser in Situ Keratomileusis For Astigmatism 0.75 Diopter Combined With Low Myopia: A Retrospective Data AnalysisAris BayuNessuna valutazione finora
- Thesis Topics in Ophthalmology in AiimsDocumento5 pagineThesis Topics in Ophthalmology in AiimsBuyCollegePaperOnlineUK100% (1)
- Intraocular Lens Power Calculation in Eyes With Previous Corneal Refractive SurgeryDocumento10 pagineIntraocular Lens Power Calculation in Eyes With Previous Corneal Refractive Surgerymoni7777Nessuna valutazione finora
- s12886 022 02620 7Documento8 pagines12886 022 02620 7MarioNessuna valutazione finora
- AUC and ConcordanceDocumento16 pagineAUC and ConcordanceDeepanshu BhallaNessuna valutazione finora
- Long Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofDocumento9 pagineLong Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofayurNessuna valutazione finora
- Understanding Corneal TopographyDocumento12 pagineUnderstanding Corneal TopographyWagner de AvizNessuna valutazione finora
- Catarct SinilisDocumento5 pagineCatarct SinilisAsri Mukti NantaNessuna valutazione finora
- DGH 3000 User ManaualDocumento56 pagineDGH 3000 User ManaualRoberto FalconeNessuna valutazione finora
- Primary Topography Guided Lasik Treating Manifest Refractive Astigmatism Versus Topography Measured Anterior Corneal AstigmatismDocumento13 paginePrimary Topography Guided Lasik Treating Manifest Refractive Astigmatism Versus Topography Measured Anterior Corneal AstigmatismbilalNessuna valutazione finora
- Olsen 2012Documento7 pagineOlsen 2012Camila GuerraNessuna valutazione finora
- Astigmatism Double Angle Plot Tool V130 Spreadsheet InstructionsDocumento8 pagineAstigmatism Double Angle Plot Tool V130 Spreadsheet InstructionsashishNessuna valutazione finora
- Salmon 2003Documento9 pagineSalmon 2003Andrea GilNessuna valutazione finora
- Using The Pentacam™ Calculation: For IOL PowerDocumento4 pagineUsing The Pentacam™ Calculation: For IOL PowerGerardo Felipe Mora ZepedaNessuna valutazione finora
- Opth 14 815Documento8 pagineOpth 14 815Andrés QueupumilNessuna valutazione finora
- OPD-Scan III: Refractive Power / Corneal AnalyzerDocumento6 pagineOPD-Scan III: Refractive Power / Corneal AnalyzerFreeNessuna valutazione finora
- Clinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisDocumento5 pagineClinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisayurNessuna valutazione finora
- Pentcam 5tDocumento16 paginePentcam 5tMarian FasieNessuna valutazione finora
- VA Schivirling2020Documento7 pagineVA Schivirling2020Jordi MasNessuna valutazione finora
- Inside: Quality InsiderDocumento9 pagineInside: Quality Insidertehky63Nessuna valutazione finora
- Ocular Aberrations Before and After Myopic Corneal Refractive Surgery: LASIK-Induced Changes Measured With Laser Ray TracingDocumento8 pagineOcular Aberrations Before and After Myopic Corneal Refractive Surgery: LASIK-Induced Changes Measured With Laser Ray Tracingbonny_07_fk_unsri9248Nessuna valutazione finora
- Driver's Eye State Identification Based On Robust Iris Pair LocalizationDocumento4 pagineDriver's Eye State Identification Based On Robust Iris Pair LocalizationKhalil UllahNessuna valutazione finora
- Pubmed Thesis Topics in OphthalmologyDocumento5 paginePubmed Thesis Topics in Ophthalmologyheidiowensspringfield100% (2)
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocumento10 pagineClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNessuna valutazione finora
- 2007-Supplement Pentacam AAO 2006Documento11 pagine2007-Supplement Pentacam AAO 2006ElBuen JohnNessuna valutazione finora
- Eye TrackingDocumento6 pagineEye Trackingp@bloNessuna valutazione finora
- Problems With Wavefront Aberrations Applied To Refractive Surgery: Developing StandardsDocumento10 pagineProblems With Wavefront Aberrations Applied To Refractive Surgery: Developing Standardsmvs_newNessuna valutazione finora
- Ecop 09 00286Documento11 pagineEcop 09 00286GabrielNessuna valutazione finora
- Email Not Displaying Correctly? View It in Your Browser Forward To A FriendDocumento5 pagineEmail Not Displaying Correctly? View It in Your Browser Forward To A Friendkyochum5805Nessuna valutazione finora
- Smith Test, Goniolens, Shadow TestDocumento3 pagineSmith Test, Goniolens, Shadow TestJLo100% (1)
- Opd - Scan Ii PDFDocumento6 pagineOpd - Scan Ii PDFDfhos Oftalmo ServiceNessuna valutazione finora
- A New Iris Segmentation Method For Recognition: (Jzhuang, Wangyh, TNT, Jlcui) @NLPR - Ia.ac - CNDocumento4 pagineA New Iris Segmentation Method For Recognition: (Jzhuang, Wangyh, TNT, Jlcui) @NLPR - Ia.ac - CNchinmay2882Nessuna valutazione finora
- III.2 A Package For The Statistical Analysis of Visual FieldsDocumento16 pagineIII.2 A Package For The Statistical Analysis of Visual Fieldssidharth mahotraNessuna valutazione finora
- Comparison Between Femtosecond Laser Mushroom Con Figuration and Manual Trephine Straight-Edge Con Figuration Deep Anterior Lamellar KeratoplastyDocumento6 pagineComparison Between Femtosecond Laser Mushroom Con Figuration and Manual Trephine Straight-Edge Con Figuration Deep Anterior Lamellar KeratoplastyindahdeshakaNessuna valutazione finora
- Delineating Fluid-Filled Region Boundaries in Optical Coherence Tomography Images of The RetinaDocumento17 pagineDelineating Fluid-Filled Region Boundaries in Optical Coherence Tomography Images of The RetinaVenkatraman KalyanakumarNessuna valutazione finora
- PIIS0002939422003841Documento6 paginePIIS0002939422003841Anca Florina GaceaNessuna valutazione finora
- Accuracy of Intraocular Lens Calculation FormulasDocumento10 pagineAccuracy of Intraocular Lens Calculation FormulasHerval Martins filhoNessuna valutazione finora
- Macular Hole Size As A Prognostic Factor in Macular Hole SurgeryDocumento5 pagineMacular Hole Size As A Prognostic Factor in Macular Hole SurgeryArni ZulsitaNessuna valutazione finora
- QB For ADSDocumento12 pagineQB For ADSKunj TrivediNessuna valutazione finora
- Comparison of Total Corneal Astigmatism Between IOLMasterDocumento7 pagineComparison of Total Corneal Astigmatism Between IOLMasterSarah Camacho PinedaNessuna valutazione finora
- Comparative Effects of Various Types of Toric Intraocular Lenses On Astigmatism CorrectionDocumento9 pagineComparative Effects of Various Types of Toric Intraocular Lenses On Astigmatism CorrectionAndrés QueupumilNessuna valutazione finora
- Lab Report Zoology 2Documento4 pagineLab Report Zoology 2Rebecca UyNessuna valutazione finora
- Anterior Segment Parameters Associated To Acute Glaucoma With Slit Lamp Optical Coherence TomographyDocumento6 pagineAnterior Segment Parameters Associated To Acute Glaucoma With Slit Lamp Optical Coherence TomographyRika FitriaNessuna valutazione finora
- Aberraciones Modelo de Ojo 2342Documento11 pagineAberraciones Modelo de Ojo 2342pacaNessuna valutazione finora
- Accuracy of Two Devices and Three Different Calculation Methods For Predicting Residual Astigmatism After Intraocular Lens ImplantationDocumento5 pagineAccuracy of Two Devices and Three Different Calculation Methods For Predicting Residual Astigmatism After Intraocular Lens Implantationjorefe12Nessuna valutazione finora
- Anterior Chamber Angle Imaging With Optical Coherence TomographyDocumento7 pagineAnterior Chamber Angle Imaging With Optical Coherence TomographySouvik BanerjeeNessuna valutazione finora
- 4 PerceptionDocumento8 pagine4 PerceptionDaniel Saadi Hamid RazzaNessuna valutazione finora
- Accommodation Dysfunction: DR Neelu AgrawalDocumento30 pagineAccommodation Dysfunction: DR Neelu AgrawalNeelu MundhadaAgrawalNessuna valutazione finora
- Backwards Design FinalDocumento12 pagineBackwards Design Finalapi-253513324Nessuna valutazione finora
- Visual Perception - Simply PsychologyDocumento9 pagineVisual Perception - Simply PsychologyPapuna ChivadzeNessuna valutazione finora
- Refractive ErrorsDocumento7 pagineRefractive ErrorsJim Jose AntonyNessuna valutazione finora
- Hyperopia: AuthorsDocumento13 pagineHyperopia: AuthorsHana SetianingsihNessuna valutazione finora
- Use of Intraocular Lenses in Children With Traumatic Cataract in South IndiaDocumento5 pagineUse of Intraocular Lenses in Children With Traumatic Cataract in South IndiaYanjinlkham KhNessuna valutazione finora
- Tinnitus Today June 1999 Vol 24, No 2Documento27 pagineTinnitus Today June 1999 Vol 24, No 2American Tinnitus AssociationNessuna valutazione finora
- Clinical Management of Binocular Vision .24Documento1 paginaClinical Management of Binocular Vision .24Ikmal ShahromNessuna valutazione finora
- The Spatial Tuning of Chromatic Adaptation: Annette WernerDocumento13 pagineThe Spatial Tuning of Chromatic Adaptation: Annette WernerUjjayanta BhaumikNessuna valutazione finora
- G8 Lesson Plan - Week 3 Modifiers and InfographicDocumento5 pagineG8 Lesson Plan - Week 3 Modifiers and InfographicIchaac Veracruz100% (1)
- Erum ShahidDocumento5 pagineErum Shahidkhoridatul hasindahNessuna valutazione finora
- Color BasicsDocumento3 pagineColor BasicsEmma Fe Ranis EsclamadoNessuna valutazione finora
- Retinopathy of Prematurity (Rop)Documento21 pagineRetinopathy of Prematurity (Rop)ArinYuniastikaEkaPutriNessuna valutazione finora
- SCIENCE F3 (Chapter 1)Documento49 pagineSCIENCE F3 (Chapter 1)Nurul NasaruddinNessuna valutazione finora
- Notes50 - PEDIATRIC VISION OR HEARING DISORDERSDocumento9 pagineNotes50 - PEDIATRIC VISION OR HEARING DISORDERSTJ ZamarroNessuna valutazione finora
- The Function of The Middle Ear Is ToDocumento3 pagineThe Function of The Middle Ear Is ToRubi MeeajanNessuna valutazione finora
- Listening Practice5Documento8 pagineListening Practice5Phone Myat Pyaye SoneNessuna valutazione finora
- Article Best Lenses Sport P 1Documento5 pagineArticle Best Lenses Sport P 1Umanath R PoojaryNessuna valutazione finora
- Ophthalmology PDFDocumento92 pagineOphthalmology PDFMarwa AhmedNessuna valutazione finora
- Mci Flexalighting Tarifa 2017Documento274 pagineMci Flexalighting Tarifa 2017VEMATELNessuna valutazione finora
- AMsler Grid, It Require To Diagnose Central RetinaDocumento7 pagineAMsler Grid, It Require To Diagnose Central RetinakeshavNessuna valutazione finora
- Aerial PhotographyDocumento48 pagineAerial PhotographySharan Pratap SinghNessuna valutazione finora
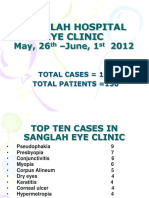
- SanglahDocumento13 pagineSanglahIzzarIzzarNessuna valutazione finora
- Introduction To Sensory Physiology: 1. Mapping The Density of Temperature and Touch-Sensitive Spots of The SkinDocumento4 pagineIntroduction To Sensory Physiology: 1. Mapping The Density of Temperature and Touch-Sensitive Spots of The SkinAshbirZammeriNessuna valutazione finora
- The Human Eye and The Colourful World PPT-Mod-2 (10TH)Documento25 pagineThe Human Eye and The Colourful World PPT-Mod-2 (10TH)SamNessuna valutazione finora
- Sensory 1Documento13 pagineSensory 1Hasnita JaisNessuna valutazione finora