Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Description:: Shock, Circulatory
Caricato da
Putri Nurul HidayahDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Description:: Shock, Circulatory
Caricato da
Putri Nurul HidayahCopyright:
Formati disponibili
Shock, circulatory DESCRIPTION: Inadequate perfusion (oxygen supply) of tissues which results in organ dysfunction, cellular and organ
damage and, if not corrected quickly, death of the patient. Classification of shock: ypo!olemic shock " cardiac output is se!erely reduced due to loss of intra!ascular !olume which results in reduced return of !enous #lood to the heart. $ost often caused #y #lood loss. Cardiogenic shock " cardiac output is se!erely reduced due to a loss of myocardial muscle function, !al!ular dysfunction or arrhythmia. $ost often caused #y large myocardial infarctions. %#structi!e shock " cardiac output is se!erely reduced #y !ascular o#struction of !enous return to the heart (!ena ca!a syndrome), compression of the heart, (pericardial tamponade, tension pneumothorax) or outflow from the heart (aortic dissection, pulmonary em#olism) &istri#uti!e shock " maldistri#ution of #lood flow 'enous pooling (most often due to spinal shock or drug o!erdose) #eha!es much like hypo!olemic shock, cardiac output se!erely reduced #ecause #lood is pooled in peripheral !eins rather than #eing returned to the heart igh output or !asodilating shock (most often due to sepsis or septic like states such as toxic shock) is unique in that cardiac output is normal or ele!ated, #ut not distri#uted appropriately, resulting in o!er perfusion of some tissues and underperfusion (to the point of critical ischemia) of other tissues. Predominant age: (ll ages. &etermined #y underlying diseases causing shock. $ore frequent and less well tolerated in the elderly. Predominant sex: $ale ) *emale +I,-+ (-& +.$/0%$+: 1nderlying disease: 1pper gastrointestinal (1,I) #leeding (ulcer pain, hematemesis, melena) +epsis (fe!er, chills, dysuria and2or costo!erte#ral angle 3C'(4 tenderness with urinary tract infection) $yocardial infarction (chest pain, diaphoresis, nausea, !omiting, +5 or +6 gallop, new heart murmur, rales due to pulmonary edema) 1nderperfusion of organ systems: 7rain: confusion, anxiety, agitation, coma only if se!ere 8idney: oliguria +kin: peripheral cyanosis, sluggish capillary refill, mottling, coolness, may #e o!erly perfused
(flushed) in high output (septic) shock ,I: a#sence of #owel sounds Circulation: thready pulses, tachycardia, hypotension (mean arterial pressure 9 :; torr or systolic pressure 9 <; torr or #lood pressure = 5; torr less than usual #lood pressure in chronic hypertension), secondary cardiac ischemia (+0 depression) or heart failure may occur due to underperfusion of the heart during shock. >ugular" !enous distention (>'&), pulsus paradoxus in pericardial tamponade. CAUSES: ypo!olemic shock 7lood loss due to trauma or gastrointestinal #leeding 0hird space loss of plasma !olume (pancreatitis, #owel o#struction, infarction, anaphylaxis) &iarrhea (e.g., in cholera like states) 7urns Cardiogenic shock (cute myocardial infarction (= 5;? of @' mass) (rrhythmia (heart #lock, !entricular tachycardia, atrial fi#rillation with rapid !entricular response, etc.) (cute !al!ular dysfunction (mitral !al!e due to papillary muscle rupture following inferior $IAs or chordal rupture) aortic or mitral !al!e due to #acterial endocarditis 'entricular septal rupture following anterior2septal $IAs %#structi!e shock /ericardial tamponade Inferior2superior !ena ca!al o#struction usually due to neoplasms (ortic dissection $assi!e pulmonary em#olism &istri#uti!e shock 'enous pooling is due to a loss of !enous tone caused #y loss of sympathetic ner!ous system acti!ity due to acute spinal inBury, general or spinal anesthesia or o!erdose of sedati!e drugs igh output shock is due to sepsis, toxic shock or anaphylaxis (once plasma !olume normaliCed) RISK FACTORS: Included with Causes
DIAGNOSIS DIFFERENTIAL DIAGNOSIS:
-2( @(7%D(0%D.: +pecific to shock Ele!ated lactate (= F mmol2@) indicates anaero#ic meta#olism due to underperfusion of tissues Deduced mixed !enous /;F (9 FG mm g) (9 6.H k/a) o#tained from the pulmonary artery indicates !igorous extraction of oxygen from tissues due to underperfusion 1nderlying diseases responsi#le to shock EC,, C/8 (serial) Chest x"ray (rterial #lood gases ,ram stain and culture of infected sites 7lood cultures C7C (serial determination of g#2 ct in #leeding patients) Drugs that may alter lab results: -2( Disorders that may alter lab results: -2( PATHOLOGICAL FINDINGS: -2( SPECIAL TESTS: Certain tests are essential to making correct and prompt diagnosis in order to dictate specific therapy of disease states producing shock. *or example: Endoscopy2Dadioisotope #leeding scans ena#le localiCation of ongoing #leeding which may direct surgical inter!ention. 0he endoscopist may inter!ene directly !ia the endoscope. (e.g., inBection of sclerosants into !arices or ulcers). Echocardiograms may detect and2or quantify pericardial effusions in shock due to pericardial tamponade. /ericardiocentesis can then #e performed under echocardiographic guidance. (lso useful for detection of !al!ular failure. @ung scans and2or pulmonary arteriography for the detection of massi!e pulmonary em#olism /ulmonary artery (+wan",anC) catheteriCation for serial measurement of cardiac output, central !enous, pulmonary arterial and pulmonary arterial occlusion pressures (left atrial pressure) and !ascular resistance. $ixed !enous #lood gases can #e drawn from the catheter. Indicated when the etiology of shock is uncertain, in cardiogenic and septic shock, or when initial therapy of shock fails to pro!ide for rapid correction of perfusion failure. TREATMENT
APPROPRIATE HEALTH CARE: Emergency room or intensi!e or coronary care unit Continuous electrocardiographic monitoring with frequent assessment of #lood pressure, respiratory status, and urine output GENERAL MEASURES: 0herapy must proceed quickly #efore extensi!e damage to !ital organs occur. 0herapy is directed simultaneously to correct #oth the deficit in tissue perfusion and the underlying disease causing shock (see (ssociated conditions). $aintain +a%F = <I? with supplemental oxygen. Intu#ate and mechanically !entilate patient if patient cannot #e oxygenated with J;;? oxygen or has markedly increased #reathing effort (excessi!e oxygen cost of #reathing). $aintain p a#o!e H.6 (#ut less than H.I) to preser!e !ascular responsi!eness to endogenous or exogenous catecholamines. Correct plasma !olume deficits rapidly #y !olume expanders consisting of isotonic saline (.<-s or DingerAs lactate) with or without colloid (al#umin I? or hydroxyethyl starch :?) /acked red #lood cell transfusion to correct or pre!ent anemia. 7 maintained at or a#o!e J; grams2dl. (dminister coagulation factors (fresh froCen plasma, cryoprecipitate) and platelets if coagulopathy (prolonged /0, /00 or platelet count 9 I;,;;;) is present in a patient who is #leeding 0achyarrhythmias (other than sinus tachycardia) should #e promptly corrected #y electrocardio!ersion. 0rans!enous pacemakers should #e placed to correct #radyrhythmias. 'asopressors (see $edications) to correct hypotension or low cardiac output due to myocardial failure or hypotension due to low !ascular resistance End points of resuscitation: adequate #lood pressure (= :; mm g 3G.; k/a4 mean or = <; mm g 3JF.; k/a4 systolic or within 5; mm g 3I.6F k/a4 of patientAs normal #lood pressure). /atient is awake2alert, urine output adequate, heart rate 9 J;;, warm skin with #risk capillary refill, #owel sounds present. @actate 9 F mmol2@, mixed !enous /%F = 6; mm g.
MEDICATIONS DRUG(S) OF CHOICE: &opamine, low dose, J"5 Kg2kg2min augments contractility and cardiac output (#eta"J) and
increases heart rate. 0his pro!ides increased #lood flow to kidneys and gut. (lso acts directly on dopaminergic receptors in the renal !asculature to enhance renal #lood flow. &opamine = 5 Kg2kg2min: augments contractility, and cardiac output (#eta"J) and increased heart rate. Increases #lood pressure #y a com#ination of increased cardiac output and !asoconstriction (alpha). -orepinephrine F"JF Kg2min: augments #lood pressure #y increased !ascular resistance (alpha). Deduced #lood flow to splanchnic #ed can #e re!ersed #y low dose dopamine. /henylephrine F;"F;; Kg2min: see norepinephrine &o#utamine I"J; Kg2kg2min augments contractility and cardiac output (#eta"J). as #oth !asoconstricti!e (alpha) and !asodilator (#eta"F) properties. 0hese effects ha!e a minimal effect on systemic !asculature. Contraindications: Defer to manufacturerAs profile of each drug Precautions: $yocardial oxygen consumption is increased #y increased heart rate, afterload, and contractility /ressors can increase myocardial ischemia if present $ay precipitate or worsen tachyarrhythmias +hould #e used in lowest possi#le dose for as limited period of time as possi#le Significant possible interactions: Defer to manufacturerAs profile of each drug
Encephalopathy and2or cere#ro!ascular accident EXPECTED COURSE AND PROGNOSIS: $ortality is determined #y a complex interaction of primary disease causing shock, age, coexisting chronic disease and shock se!erity as marked #y the num#er of acute organ system failures that follow shock 7est outcome (= <;? sur!i!al) in young patient with transient shock due to trauma or gastrointestinal #lood loss without chronic irre!ersi#le illnesses /oor outcome (= <;? mortality) in elderly patient with septic shock, underlying chronic li!er disease, who de!elops acute renal failure, (D&+, and coagulopathy
MISCELLANEOUS ASSOCIATED CONDITIONS: ,astrointestinal #lood loss: may require endoscopic or surgical inter!ention if #leeding doesnAt spontaneously cease, e.g., electrocoagulation or inBecting sclerosant for #leeding peptic ulcers, sclerotherapy in esophageal !arices +epsis: empiric anti#iotic therapy, anti#odies against gram negati!e antigens Cardiogenic shock: therapy should help reduce cardiac ischemia (oxygen, nitrates) and accomplish rapid reperfusion of inBured, #ut potentially !ia#le, myocardium (throm#olysis with fi#rinolytic agents, #alloon angioplasty of stenotic !essels or surgical #ypass grafting) ( #alloon pump may temporiCe #y pro!iding impro!ed coronary #lood flow during and following diagnostic testing and re!asculariCation therapy. If shock is due to acute failure of the mitral or aortic !al!e, surgical !al!e replacement may #e lifesa!ing. /ulmonary em#olism Cardiac tamponade
FOLLOW UP PATIENT MONITORING: Careful monitoring of all life functions in intensi!e care PREVENTION/AVOIDANCE: +hock is #est a!oided #y prompt recognition and treatment of underlying diseases which cause shock (e.g., early anti#iotic therapy for infections) POSSIBLE COMPLICATIONS: $ultiple organs may #e damaged #y underperfusion during shock (cute tu#ular necrosis Ischemic hepatitis Ischemic #owel &isseminated intra!ascular coagulopathy (dult respiratory distress syndrome ((D&+)
Potrebbero piacerti anche
- Kardiogenik SyokDocumento43 pagineKardiogenik SyokGalih Arief Harimurti WawolumajaNessuna valutazione finora
- Patofisiologi Shock CardiogenicDocumento44 paginePatofisiologi Shock CardiogenicGalih Arief Harimurti Wawolumaja100% (1)
- Cardiogenic ShockDocumento49 pagineCardiogenic Shockmaibejose0% (1)
- ShockDocumento64 pagineShockAnusha VergheseNessuna valutazione finora
- Pharmacotherapy - Heart Failure - Dr. Mohammed KamalDocumento62 paginePharmacotherapy - Heart Failure - Dr. Mohammed KamalMohammed KamalNessuna valutazione finora
- Shock Tugas Anestesi ViliaDocumento81 pagineShock Tugas Anestesi ViliaviliaNessuna valutazione finora
- Taufan Arif, S.Kep., NS., M.KepDocumento85 pagineTaufan Arif, S.Kep., NS., M.KepputriNessuna valutazione finora
- ShockDocumento36 pagineShockJohnryan NdiranguNessuna valutazione finora
- Mi CaseDocumento5 pagineMi CaseffaaNessuna valutazione finora
- Atrial Fibrilation GauDocumento39 pagineAtrial Fibrilation GauRANA MOHAMMED HAMOOD AL-HADEQNessuna valutazione finora
- Lecture 8Documento7 pagineLecture 8Grafu Andreea AlexandraNessuna valutazione finora
- 3 ShockDocumento12 pagine3 ShockAiden JosephatNessuna valutazione finora
- Ischemic Heart DiseaseDocumento67 pagineIschemic Heart Diseasealfaz lakhani80% (5)
- Although Shock Has Been Recognised For Over 100 YearsDocumento4 pagineAlthough Shock Has Been Recognised For Over 100 YearsRusty HoganNessuna valutazione finora
- Heart FailureDocumento77 pagineHeart FailureJudy Anne PatricioNessuna valutazione finora
- ShockDocumento22 pagineShockAbdul MajidNessuna valutazione finora
- BAU PTR-Neurology-Lecture 11-StrokeDocumento133 pagineBAU PTR-Neurology-Lecture 11-Strokeerfan mohammadiNessuna valutazione finora
- ShockDocumento9 pagineShockapocruNessuna valutazione finora
- Ntroduction To The Physical ExaminationDocumento4 pagineNtroduction To The Physical ExaminationAngelica NenitaNessuna valutazione finora
- Lec 3Documento17 pagineLec 3Yousef El3alamey0% (1)
- Shock 20231122 213304 0000Documento32 pagineShock 20231122 213304 0000Mikella E. PAGNAMITANNessuna valutazione finora
- Acquired Central Nervous System Vascular Disorders-1Documento39 pagineAcquired Central Nervous System Vascular Disorders-1Jake MillerNessuna valutazione finora
- Athero 2 Dr. Raquid 2021Documento93 pagineAthero 2 Dr. Raquid 2021oreaNessuna valutazione finora
- The Next Sequel: Scarring My HeartDocumento56 pagineThe Next Sequel: Scarring My Heartshmily_0810Nessuna valutazione finora
- PPP v3Documento771 paginePPP v3Steven Lam100% (1)
- Cardiology-6 CADDocumento20 pagineCardiology-6 CADMahmoud RamadanNessuna valutazione finora
- Cardiovascular DisordersDocumento20 pagineCardiovascular DisordersHampson MalekanoNessuna valutazione finora
- Curs 9 Myocarditis CardiomyopathyDocumento41 pagineCurs 9 Myocarditis CardiomyopathyIliescu DenisaNessuna valutazione finora
- 6.0 IDS ShockDocumento4 pagine6.0 IDS ShockEdalyn CapiliNessuna valutazione finora
- Clinical Neurology Answers OnlyDocumento68 pagineClinical Neurology Answers Onlyanas kNessuna valutazione finora
- ShockDocumento18 pagineShocksantokh108Nessuna valutazione finora
- ShockDocumento63 pagineShockAhmedNessuna valutazione finora
- HTN and CHFDocumento29 pagineHTN and CHFkiflomNessuna valutazione finora
- Heart Failure and Pulmonary EdemaDocumento60 pagineHeart Failure and Pulmonary EdemaYosra —Nessuna valutazione finora
- Stroke: Clinical Presentation and Anatomical LocalizationDocumento36 pagineStroke: Clinical Presentation and Anatomical LocalizationYusuf JoganNessuna valutazione finora
- Examination and Investigation of The Cardiovascular System (CVS)Documento27 pagineExamination and Investigation of The Cardiovascular System (CVS)Jake MillerNessuna valutazione finora
- Alteration in Perfusion 2Documento28 pagineAlteration in Perfusion 2Atteya Mogote AbdullahNessuna valutazione finora
- Topic:: Unstable AnginaDocumento44 pagineTopic:: Unstable AnginaApurba100% (1)
- IschemicHeartDisease LectureDocumento64 pagineIschemicHeartDisease LectureFerdinand RobertNessuna valutazione finora
- Heartbeat Disorders: by Aisha Sara Tasnim Physician: Dr. SsebulibaDocumento31 pagineHeartbeat Disorders: by Aisha Sara Tasnim Physician: Dr. SsebulibaNinaNessuna valutazione finora
- Stroke: DR Abdirahman AbibDocumento40 pagineStroke: DR Abdirahman AbibMahad IbrahemNessuna valutazione finora
- 115-NCLEX-RN Review Made Incredibly Easy, Fifth Edition (Incredibly Easy Series) - Lippincott-16083 - p53Documento1 pagina115-NCLEX-RN Review Made Incredibly Easy, Fifth Edition (Incredibly Easy Series) - Lippincott-16083 - p53MuhNatsirNessuna valutazione finora
- Trauma and Its ComplicationsDocumento80 pagineTrauma and Its Complicationsjoe BouGhazaliNessuna valutazione finora
- ShockDocumento53 pagineShockHassan Ahmed100% (3)
- Copstead-Kirkhorn: Pathophysiology, 4 Edition: Disease Profiles Cardiogenic ShockDocumento2 pagineCopstead-Kirkhorn: Pathophysiology, 4 Edition: Disease Profiles Cardiogenic ShockadadanNessuna valutazione finora
- Pathophysiology of Pericardial DiseaseDocumento36 paginePathophysiology of Pericardial DiseaseivaniNessuna valutazione finora
- ShockDocumento2 pagineShockYousef El3alameyNessuna valutazione finora
- Electrocardiogram: Electrocardiogram EKG Heart Heart's Electrical Activity DiagnosisDocumento38 pagineElectrocardiogram: Electrocardiogram EKG Heart Heart's Electrical Activity DiagnosislorhenzsoNessuna valutazione finora
- Pemicu 6 Eko Blok KGDDocumento128 paginePemicu 6 Eko Blok KGDEko SiswantoNessuna valutazione finora
- Cardiac TemponadeDocumento18 pagineCardiac TemponadeDIVYA GANGWAR100% (1)
- Prof Univ DR Ion C.Tintoiu FESC Centrul de Cardiologie Al Armatei Universitatea Titu MaiorescuDocumento719 pagineProf Univ DR Ion C.Tintoiu FESC Centrul de Cardiologie Al Armatei Universitatea Titu MaiorescuVioleta Malina Bîrsan HodivoianuNessuna valutazione finora
- Stroke UgDocumento76 pagineStroke Ug74. Shravani VNessuna valutazione finora
- Shock and Circulatory FailureDocumento8 pagineShock and Circulatory FailureOktaviana Sari DewiNessuna valutazione finora
- Syncope: Global Cerebral Blood FlowDocumento7 pagineSyncope: Global Cerebral Blood FlowChananNessuna valutazione finora
- Neurosurgery: UnprotectedDocumento39 pagineNeurosurgery: UnprotectedMaulana Taufik100% (2)
- Stroke CMEDocumento34 pagineStroke CMEKeren Karunya SingamNessuna valutazione finora
- 8.syncope & PresyncopeDocumento11 pagine8.syncope & PresyncopeIbrahim RamizNessuna valutazione finora
- Cardiac Emergencies Cne DelhiDocumento109 pagineCardiac Emergencies Cne DelhiManisha Thakur100% (1)
- Cardiology DR Osama MahmoudDocumento138 pagineCardiology DR Osama MahmoudIsmail Habib100% (4)
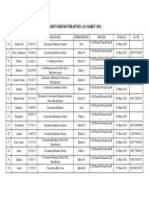
- Pasien Khemoterapi Bulan Maret 2012Documento1 paginaPasien Khemoterapi Bulan Maret 2012Putri Nurul HidayahNessuna valutazione finora
- Pasien Khemoterapi Bulan Maret 2012Documento1 paginaPasien Khemoterapi Bulan Maret 2012Putri Nurul HidayahNessuna valutazione finora
- Daftar PustakaDocumento2 pagineDaftar PustakaPutri Nurul HidayahNessuna valutazione finora
- Obst Sleep Apnea 060515Documento7 pagineObst Sleep Apnea 060515Putri Nurul HidayahNessuna valutazione finora
- Gagal Ginjal KronikDocumento20 pagineGagal Ginjal KronikFendy SuyantoNessuna valutazione finora
- A.R.I Well D-ONE® - InstructionsDocumento9 pagineA.R.I Well D-ONE® - InstructionsHari YantoNessuna valutazione finora
- Diagnosis of Paraprotein DiseasesDocumento29 pagineDiagnosis of Paraprotein DiseasesScarlettMLVNessuna valutazione finora
- Bloodborne Pathogens Program: Western Oklahoma State College Employee Training HandbookDocumento35 pagineBloodborne Pathogens Program: Western Oklahoma State College Employee Training HandbookKashaNessuna valutazione finora
- Hepato-Biliary System and Their DisordersDocumento131 pagineHepato-Biliary System and Their DisordersIton BumatayNessuna valutazione finora
- Chapter 1Documento38 pagineChapter 1synap5esNessuna valutazione finora
- Answer Sheet: Name: Test: 70minDocumento3 pagineAnswer Sheet: Name: Test: 70minThanh TâmNessuna valutazione finora
- F U R D C GDocumento33 pagineF U R D C GGiosué Reyes HernandezNessuna valutazione finora
- BMBL-5th EditionDocumento421 pagineBMBL-5th EditionBryan OngNessuna valutazione finora
- Nicky - Human Milk BankDocumento2 pagineNicky - Human Milk BankKaye Tubungbanua - MatunogNessuna valutazione finora
- Gale Mein Dard Khansi Kharash Aur Infection Ka Ilaj Ke UpayDocumento3 pagineGale Mein Dard Khansi Kharash Aur Infection Ka Ilaj Ke UpayGovindNessuna valutazione finora
- Ontimmunol09 01837Documento17 pagineOntimmunol09 01837akshayajainaNessuna valutazione finora
- Diagnostic Imaging ChestDocumento1.485 pagineDiagnostic Imaging ChestMạnh Đình Nguyễn100% (1)
- Date Report Date Name Age/Sex Lab No. Reg. No. Panel Name Slide No. Ref. Dr. Report StatusDocumento2 pagineDate Report Date Name Age/Sex Lab No. Reg. No. Panel Name Slide No. Ref. Dr. Report StatusSaurabh SinghNessuna valutazione finora
- Nano Today: Marcel Alexander Heinrich, Byron Martina, Jai PrakashDocumento21 pagineNano Today: Marcel Alexander Heinrich, Byron Martina, Jai Prakashvishal makadiaNessuna valutazione finora
- CDCDocumento116 pagineCDCRam BasanyNessuna valutazione finora
- Differences Between Staphylococcus and Streptococcus - Microbiology NotesDocumento3 pagineDifferences Between Staphylococcus and Streptococcus - Microbiology NotesSareeya ShreNessuna valutazione finora
- Common Tropical Disease in ThailandDocumento84 pagineCommon Tropical Disease in ThailandDr.Sathaporn KunnathumNessuna valutazione finora
- Parasites & People - Host Parasite Relationship - RumalaDocumento40 pagineParasites & People - Host Parasite Relationship - RumalamicroperadeniyaNessuna valutazione finora
- Biodfence Product InsertDocumento2 pagineBiodfence Product Insertapi-235072265Nessuna valutazione finora
- The Selection and Use of Essential in Vitro Diagnostics: WHO Technical Report SeriesDocumento380 pagineThe Selection and Use of Essential in Vitro Diagnostics: WHO Technical Report SeriesJOSHITHANessuna valutazione finora
- 13.approach To Upper Respiratory Tract InfectionsDocumento3 pagine13.approach To Upper Respiratory Tract InfectionsRed DevilNessuna valutazione finora
- DengvaxiaDocumento1 paginaDengvaxiaAce Bryan Niño LlesolNessuna valutazione finora
- Premarital SexDocumento6 paginePremarital SexArcon AlvarNessuna valutazione finora
- Jurnal SleDocumento2 pagineJurnal SlePratidina Dwinda HENessuna valutazione finora
- Path GitDocumento18 paginePath Gitvnair112Nessuna valutazione finora
- Lecture6 Intro, Classification of ParasitesDocumento38 pagineLecture6 Intro, Classification of ParasitesJumar Villegas100% (1)
- Chapter 3 Infection Control: Phlebotomy, 5e (Booth)Documento13 pagineChapter 3 Infection Control: Phlebotomy, 5e (Booth)Carol Reed100% (1)
- Sapphire Insect Transfection KitDocumento1 paginaSapphire Insect Transfection KitAlleleBiotechNessuna valutazione finora
- Hand Foot Mouth Disease (HFMD) For TeachersDocumento2 pagineHand Foot Mouth Disease (HFMD) For Teachersalbeny j.pNessuna valutazione finora