Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
The Prevention and Treatment of Recurrent Spontaneous Miscarriage
Caricato da
peter911xCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
The Prevention and Treatment of Recurrent Spontaneous Miscarriage
Caricato da
peter911xCopyright:
Formati disponibili
1
Chinese Medicine Times - Volume 5 Issue 1 - Spring 2010
The Prevention and Treatment Of Recurrent Spontaneous Miscarriage
by Li Qin Zhao
Abstract iscarriage is becoming a common condition for pregnant women, especially in recent years where miscarriage rates have progressively increased as women try to conceive later in life and more and more patients seek IVF treatment. Traditional Chinese Medicine (TCM) has demonstrated that it can prevent and treat recurrent spontaneous miscarriage (RSM) effectively and successfully. In this article, the author analyses the aetiology and pathology of RSM and discuss the differentiation and general modifications according to her clinical experience. The author will also introduce the modern Western medicine approach regarding the diagnosis and treatment of RSM, particularly in with immunological reactions, and report two case studies. Introduction RSM is a term used when three or more consecutive miscarriages have occurred. It is also known as Habitual Abortion. Miscarriage affects around 25% of all pregnancies [1]. Recurrent miscarriage occurs in at least 15% of confirmed pregnancies during the first trimester (12 weeks) [2]. 21% of IVF pregnancies are miscarried spontaneously [1], and women around the age of 40 experience nearly 50% pregnancy loss with IVF alone [3]. In Western medicine, there are three stages to a miscarriage or spontaneous miscarriage: threatened miscarriage, incomplete miscarriage and complete miscarriage. There is little to prevent or treat recurrent miscarriage in western medicine. On the contrary, TCM has been treating it for thousands of years, not only preventing miscarriage but also maintaining the pregnancy until full term, and therefore increase the live birth rate. TCM Aetiology and Pathology 4. According to TCM philosophy, therefore we focus on determining the underlying causes of RSM. There are six main factors according to my clinical experience and the TCM literature that I have researched. Yin deficiency with blood heat 1. Deficiency of kidney and spleen, disharmony of chong and ren channels
The kidney is considered as the origin of congenital constitution, it stores essence, dominates growth, development and reproduction. The spleen is the material basis of the acquired constitution, and the source of qi and blood. The chong channel is the sea of blood, and the ren channel is the sea of yin channels, arising from the uterus in women and is related to conception. Both of them are responsible for blood supply to the foetus. A kidney and spleen deficiency will lead to an inadequate quantity of essence and blood and a disharmony of the chong and ren channels. As a consequence, the foetus cannot be nourished and miscarriage occurs. 2. Deficiency of kidney qi with blood stagnation in the uterus
Women born with a constitutional kidney qi deficiency; or those who have taken the oral contraceptive pill long term; or have had more than one consecutive miscarriage; or many failed IVF attempts, or several strong hormonal drugs have been used can impair the kidney qi, causing kidney qi deficiency and inadequate essence, blood stagnation in the uterus, where the foetus is devoid of blood supply and stops growing, eventually miscarrying. 3. Deficiency of qi and blood:
The spleen and stomach transport and transform the food we eat into usable nutrients and energies, and are considered as the source of qi and blood. A spleen or stomach deficiency could cause inadequate blood production and the sinking of qi, consequently failing to nourish and hold the foetus, leading to a miscarriage.
A woman born with a constitutional yin deficiency, or long term emotional factors such as stress, worry, anxiety, fear, anger or grief, can cause liver qi stagnation, which eventually turns into liver fire and blood heat ; or suffers from heat syndromes such as
Chinese Medicine Times - Volume 5 Issue 1 - Spring 2010
infection during pregnancy. The heat will attack the foetus in the uterus and cause a miscarriage. 5. Damp heat stagnating in the uterus
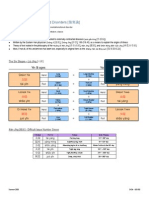
Dried herbs or concentrated powders Tu Si Zi, Xu Duan, Sang Ji Sheng, Du Zhong, Shu Di Huang, Chao Bai Zhu, Dang Shen, Ai Ye and Gui Zhi. 2. Kidney qi deficiency with blood stasis
Severe endometriosis or fibroids that have been inflamed or urinary tract infections (UTI) during pregnancy can produce excessive heat and damp in the body, stagnating in the uterus. This can affect the development of a foetus. It may eventually lead to a miscarriage if left untreated. 6. External factors-Traumatic injury
It is more likely to occur in women who have autoimmune disorders or anti-phospholipid syndrome (blood clotting disorders). Miscarriage can happen at any stage of the pregnancy. Signs and symptoms Backache or sore back; fatigue; vaginal bleeding or spotting with dark brown blood; slow developing and growing foetus; pink tongue with black spots and a deep and thready pulse Treatment principle
Any falls, accidents, impacts, or physical work may impair the chong and ren channels, causing disharmony of qi and blood. As a consequence, foetus growth and development may be affected and threaten a miscarriage. Differentiation and Treatment Traditionally there are four patterns of miscarriage. However, I have modified them according to my clinical experience and divided them into six patterns. 1. Kidney yang and spleen qi deficiency
Strengthen the kidney qi; invigorate the blood and dispel blood stasis; nourish the foetus. Acupuncture points Baihui (DU 20), Geshu (UB 17), Ganshu (UB 18), Shenshu (UB 23), Xiehai (SP 10), Fuliu (KI 4). Patent herbs Shou Tai Wan (Foetus Longevity Pill) combined with Gui Zhi Fu Ling Wan (Cinnamon Twig and Poria Pill). Dried herbs and concentrated powders
It is commonly seen in women with Luteal Phase Defect (LPD), which can cause infertility initially and miscarriage in the early stage if a pregnancy is achieved. Signs and symptoms Pain in the lower back; sinking sensation in the lower abdomen; vaginal bleeding during early pregnancy; dizziness; frequent urination and feeling cold; pale tongue and a weak pulse. Treatment principle Strengthen kidney yang and spleen qi; warm the uterus to calm and nourish the foetus. Acupuncture points Baihui (DU 20), Geshu (UB 17), Pishu (UB 20), Shenshu (UB 23), Zusanli (ST 36), Taixi (KI 3) and moxa on Yinbai (SP 1). Patent herbs
Tu Si Zi, Sang Ji Sheng, Xu Duan, Du Zhong, Ji Xie Teng, Dan Shen, Chuan Xiong, Huang Qi, Gui Zhi, Mu Dan Pi, Chi Shao Yao. 3. Qi and blood deficiency
It often occurs in early pregnancy for women with hypothyroidism, LPD, or incompetent cervix. Signs and symptoms Tired and weak; shortness of breath; sinking sensation in the lower abdominal area; bloated stomach; light bleeding with a pink colour; pale complexion; pale tongue; fine and slippery pulse. Treatment principle
Shou Tai Wan (Foetus Longevity Pill), Nuan Gong Yun Zi Wan (Warm Uterus to Support Conception Pill), or Tai Shan Pan Shi San (Taishan Bedrock Powder); Bu Shen Gu Chong Wan (Strengthen the Kidney to Secure the Chong Channel Pill) if the woman has had previous miscarriages.
Tonify the Qi and blood, strengthen the kidney to boost the essence and nourish the foetus. Acupuncture points: Baihui (DU 20), Yintang (EXHN3), Neiguan (PC 6), Zusanli (ST 36) and moxa on Geshu (UB 17), Ganshu (UB 18), Pishu (UB 20) and Yinbai (SP 1).
Chinese Medicine Times - Volume 5 Issue 1 - Spring 2010
Patent herbs Tai Yuan Yin (Foetal Source Beverage), Gui Pi Wan (Restore the Spleen Pill), or Bu Zhong Yi Qi Wan (Tonify the Middle to Augment the Qi Pill), or the combination of two of them. Dried herbs or concentrated powders: Dang Shen, Chao Bai Zhu, Shu Di Huang, Bai Shao, Huang Qi, Dang Gui, Du Zhong, Sheng Ma, Sha Ren, Zhi Gan Cao. 4. Yin deficiency with blood heat
Treatment principle Clear excess heat and remove the dampness, detoxifies the blood to nourish the foetus. Acupuncture points Yintang (EX-HN3), Neiguan (PC 6), Quchi (LI 11), Xiehai (SP 10), Zusanli (ST 36), Yinlingquan (SP 9); Geshu (UB 17), Ganshu (UB 18), Pishi (UB 20), Taichong (LIV 3). Dried herbs or concentrated powders Huang Qin, Jin Yin Hua, Lian Qiao, Chi Shao Yao, Sheng Di Huang, Dan Shen, Mu Dan Pi, Huang Bai, Fu Ling, Yin Chen. 6. Traumatic injuries
It is likely to occur in women producing anti-sperm antibodies, natural killer cells or hyperthyroidism. Signs and symptoms Vaginal bleeding in the early pregnancy with bright red blood; restless foetus; abdominal pain; constipation; irritation and restlessness; anxiety; disturbed sleep; hot palms; hectic fevers; night sweats; red tongue with a yellow coating or no coating at all; taut, slippery and rapid pulse. Treatment principle
Signs and symptoms Lower abdominal pains with a sinking sensation; backache; restless foetus; vaginal bleeding for the worst cases; pale complexion; lethargy and a weak pulse. Treatment principle
Nourish the yin and blood, clear the heat and calm the foetus. Acupuncture points Yintang (EX-HN3), Xiehai (SP 10), Quchi (LI 11), Neiguan (PC 6), Shenmen (HT 7), Taixi (KI 3); Taichong (LIV 3), Geshu (UB 17), Ganshu (UB 18). Patent herbs Bao Yin Jian (Protect the Yin Beverage) and Yang Xie An Shen Wan (Nourish the Blood to Calm the Shen Pill). Dried herbs or concentrated powders Sheng Di Huang, Huang Qin, Bai Shao Yao, Han Lian Cao, Mai Men Dong, Shan Yao, Xu Duan, Dan Shen, Suan Zao Ren, Fu Ling, Gan Cao. 5. Damp heat stagnation in the uterus
Tonify the Qi and nourishes the blood; invigorate the kidney; calm the foetus; tranquilise the spirit; ease the mind. Acupuncture points Baihui (DU 20), Si Shen Cong (EX-HN1), Yintang (EX-HN3), Neiguan (PC 6), Zusanli (ST 36), Shenmen (HT 7). Patent herbs Gui Pi Wan (Restore the Spleen Decoction) combined with Shou Yai Wan (Foetus Longevity Pill).
Dried herbs and concentrated powders Ren Shen, Huang Qi, Bai Shao Yao, Gan Cao, Shu Di Huang, Tu Si Zi, Sang Ji Sheng, Xu Duan, Long Yan Rou, Chao Bai Zhu, Fu Shen, Du Zhong. General Modifications It is often the case that patients have more complicated conditions. Therefore, modifications are necessary and can make a significant impact on the outcome. Here I summarised the general modifications according to my clinical experience:
This is likely to occur in the second or third trimester after having been infected. Signs and symptoms Abdominal pain; bloated stomach; fever; itchy skin; headaches; restlessness; slow developing foetus (or even stop growing); dark, red tongue with a yellow greasy coating; slippery and rapid pulse.
Chinese Medicine Times - Volume 5 Issue 1 - Spring 2010
For blood deficiency, add Dang Gui, Shu Di Huang, Gou Qi Zi, He Shou Wu, Ji Xie Teng, and needle Geshu (UB 17) and Ganshu (UB 18). For Qi deficiency, add Huang Qi, Dang Shen, Sheng Ma, Chai Hu, and needle Zusanli (ST 36), Baihui (DU 20), use moxa on Qihai (Ren 6) and Guanyuan (Ren 4). For spleen deficiency, add Fu Ling, Shan Yao, Bai Zhu, and needle Zusanli (ST 36), Yinlingquan (SP 9), use moxa on Pishu (UB 20) and Weishu (UB 21). For kidney Yang deficiency, add Du Zhong, Xu Duan, Tu Si Zi, Gui Zhi, and use moxa on Shenshu (UB 23) and Mingmen (DU 4). For kidney Yin deficiency, add Shu Di Huang, Han Lian Cao, Shan Zhu Yu, Sang Shen Zi, Huang Jing, Mai Men Dong, and needle Taixi (KI 3), Shenmen (HT 7), Shenshu (UB 23) and Neiguan (PC 6). For abdominal pains, add Bai Shao Yao, Gan Cao, and use moxa on Zusanli (ST 36), Pishu (UB 20) and Ganshu (UB 18). For the sinking sensation in the lower abdomen, add Huang Qi, Sheng Ma, Chai Hu, and use moxa on Pishu (UB 20), Baihui (DU 20), Zusanli (ST 36). For bleeding due to heat, add Han Lian Cao, Huang Qin, and needle Xiehai (SP 10), Dadun (LIV 1) and Quchi (LI 11) acupuncture points. For bleeding due to cold, add Ai Ye, Jing Jie Sui, and use moxa on Baihui (DU 20) and Yinbai (SP 1). For nausea and poor appetite, add Sha Ren, Chen Pi, Bai Zhu, Sheng Jiang, and needle Neiguan (PC 6), Zusanli (ST 36), Zhongwan (Ren 12) and Shenque (Ren 8). For stress, anxiety and insomnia, add Chai Hu, Bai Shao Yao, Suan Zao Ren, Wu Wei Zi, Fu Shen, Long Yan Rou, Bai Zi Ren, and needle Baihui (DU 20), Si Shen Cong (EX-HN1), Yintang (EXHN3), Neiguan (PC 6) and Shenmen (HT 7).
Autoimmune disorders - lack of the blocking antibody to pregnancy:
In couples that are a close genetic match, there is a lack of the Blocking antibody to pregnancy. The embryo or foetus is rejected and the pregnancy fails. The treatment for this is Lymphocyte immune therapy (LIT). Development of antibodies to Phospholipids
Antiphospholipid antibodies can cause placental thrombosis (thrombophilias), starving the embryo or foetus, resulting in a miscarriage. This is called Antiphospholipid Syndrome (APS) or Blood clotting disorder. The use of low doses of Aspirin and Heparin in the cycle and through pregnancy has been shown to improve pregnancy outcome [7]. Development of anti-sperm antibodies and antinuclear antibodies
Women can develop anti-sperm antibodies which kill the sperm as it enters the vagina, or kills the developing embryo preventing implantation. Anti-nuclear antibodies can directly attack the embryo or foetus and cause it to abort. The treatment for this is steroids such as Prednisolone or Dexamethasone, started on day six of the menstrual cycle and continued until at least 13 weeks of pregnancy. Elevated Natural Killer (NK) cells and elevated Cell Designation (CD) cells and Altered Th-1/Th-2 ratios
All these factors can attack the fertilized eggs and prevent implantation, resulted in a miscarriage. Possible treatment for this may include LIT, Intravenous Immunoglobulins (IVIg), Humira, low dose Aspirin or Prozac. Hypothyroidism and hyperthyroidism
Western Medicine Approach on Diagnosis and Treatment Immunological reactions Recent research has been suggested that in some cases of human reproductive failure (RSM and infertility), they may be the consequence of immunological abnormalities [4]. Approximately 80% of miscarriages are caused by an immunologic reaction [5]. Dr. George Ndukwe has developed the reproductive immunology programme at CARE for RSM in collaboration with the immunology laboratory at the Chicago Medical School in the USA. There are five categories of immunologic problems that can cause pregnancy loss [6] .
Approximately 23-35% of women with RSM have anti-thyroid antibodies [8], which may be indicative of these thyroid disorders. The medication for this is Thyroxine. However, this research is still in the experimental stages and the therapeutic effect has not been clearly established. These drugs can be very expensive, and there are potentially serious adverse reactions. Other possible causes of RSM 70% of defected conceptions are caused by Chromosomal abnormalities and genetic diseases [2] .
Chinese Medicine Times - Volume 5 Issue 1 - Spring 2010
Endocrine disorders Premature ovarian failure (POF): high follicle stimulating hormone (FSH). Luteal phase defect (LPD): inadequate progesterone production.
foetus was developing well all the way through. Unfortunately, she was involved in a car accident at 29 weeks, had suffered from severe pain on her neck, back, shoulder and chest, headache, stomach cramps, anxiety and insomnia. However, an ultrasound scan showed that the baby was fine. I altered the acupuncture prescription as follows: Baihui (DU 20), Sishencong (EX-HN1), Yintang (EXHN3), Neiguan (PC 6), Shenmen (HT 7), Zusanli (ST 36), Taichong (LIV 3), Tanzhong (Ren 17), Jingbailao (EX-HN15), Jianzhongshu (SI 15), Tianzong (SI 11) and a few Ashi points. The herbal prescription was: Dang Shen, Huang Qi, Bai Shao Yao, Gan Cao, Suan Zao Ren, Shu Di Huang, Tu Si Zi, Xu Duan, Sang Ji Sheng, and Du Zhong. One bag a day for 10 days. She went on to deliver a healthy baby boy naturally at full term. Case two: Yin deficiency with blood heat Natalie, 33 years old, company manager. She had been trying to conceive for four years, had achieved five pregnancies, including one natural pregnancy and four IUI pregnancies. Unfortunately, she miscarried one at 9 weeks, and the other four at 4-5 weeks. She had blood tests for immunological reactions and chromosomal defects, the results were normal. She was referred to me when she was undergoing IVF treatment from CARE Fertility hospital. She always had painful and clotty periods ever since she was young and had to take painkillers for pain relief. She also went on the contraceptive pill for five years before trying for a family. She was physically healthy, but mentally very stressed and busy with her business. She also went to the gym 3-4 times weekly, the excessive exercise leading to profuse sweating. She drank 5-6 cups of tea and coffee each day. She had a red tongue with a thin coating, thread and rapid pulse. Treatment Before egg collection, acupuncture was given to tonify qi and nourish blood, improve egg quality, and prepare her body while she was on the IVF drugs. The points used: Yintang (EX-HN3), Neiguan (PC 6), Hegu (LI 4), Tianshu (ST 25), Guanyun (Ren 4), Zigong (EX-CA1), Xiehai (SP 10), Sanyinjiao (SP 6), Taixi (KI 3), Taichong (LIV 3), Shenshu (UB 23), Geshu (UB 17). Meanwhile, I advised her to stop drinking tea and coffee, to exercise in moderation, and work fewer hours.
Uterine problems Uterine abnormalities. Uterine adhesion or cervical lesion. Endometriosis or fibroids. Incompetent cervix.
Maternal infections Rubella, toxoplasmosis, appendicitis, pneumonia, or urinary tract infection (UTI).
Typical Cases Case one: Kidney yang and spleen qi deficiency, together with traumatic injury. Jane, 31 years old, solicitor. She had achieved five pregnancies, one resulting in a live birth, one miscarried at 12 weeks, and another three miscarried at 5-6 weeks. She conceived again five months later after the last miscarriage, and went to see the consultant in the Early Pregnancy Assessment Unit (EPAU) at the hospital. She was told that they could neither conduct any investigation during pregnancy, nor offer preventative treatment. Instead, they advised her to try alternative medicine. She was five weeks pregnant and felt tired and cold, extremely stressed and anxious, experienced lower abdominal pain and backache, frequent urination, pale complexion. She also had a pale tongue with patched coating, and a deep, thin pulse. Treatment Acupuncture points: Baihui (DU 20), Yintang (EXHN3), Neiguan (PC 6), Shenmen (HT 7), Zusanli (ST 36). Moxa on Guanyuan (Ren 4), Qihai (Ren 6), Shenshu (UB 23) and Mingmen (DU 4). This was done weekly until 14 weeks, and then once every 4 weeks until 29 weeks. Herbal prescription: Huang Qi, Dang Shen, Chao Bai Zhu, Dang Gui, Bai Shao Yao, Sang Ji Sheng, Xu Duan, Du Zhong, Tu Si Zi, Shu Di Huang, Ai Ye, Sha Ren and Zhi Gan Cao. Six bags a week until 8 weeks, then four bags a week until 12 weeks. Meanwhile, she was advised to work part time. She had no complains at all after two weeks of treatment, apart from feeling a bit tired and nauseas. She had blood tests and ultrasound scans regularly every 2-3 weeks until 17 weeks, and had found that the
Chinese Medicine Times - Volume 5 Issue 1 - Spring 2010
After the embryos had been transferred, acupuncture points were altered to support implantation: Baihui (DU 20), Neiguan (PC 6), Shenmen (HT 7), Zusanli (ST 36), Taixi (KI 3). Auricular points: Naodian (Brain), Neifenmi (Endocrine). She was prescribed Clexane injection and Progesterone pessaries at the hospital. I advised her to stop exercising completely for 12 weeks and take it easy. When she successfully conceived, treatment was changed to maintain the pregnancy: she had a bit of brownish spotting at 6 weeks for one day, but with no abdominal pain or backache. She received an ultrasound scan the next day and the foetus heartbeat was detected. I modified the acupuncture points again accordingly during pregnancy. She was fine until 17 weeks when she experienced light bleeding, which was found to be caused by a polyp in her uterus. We monitored her closely, the polyp stopped growing and she had no more bleeding. She eventually gave birth to a healthy baby daughter at full term. Discussion Spontaneous miscarriage can be very heart-breaking, especially after a woman has suffered from fertility difficulties in the past, and gone through years of treatment to achieve the pregnancy. The most overwhelming loss a woman can experience is the reoccurrence of consecutive miscarriages. In some countries, they would not be investigated until it happened at least three times. All they could do is wait and see. Whenever they managed to conceive, they would go through an emotional roller coaster and wait with tremendous stress and anxiety, which would worsen their condition even further and increase the risk of miscarriage. Therefore when we treat these patients, it is crucial that we strengthen the kidney and tonify the blood to encourage their body to be more conceptive and maintain the pregnancy to full term. Soothing liver qi and nourishing heart blood to ease their mind must also be considered. When a pregnant woman experiences lower abdominal pain or vaginal bleeding during the early stages of pregnancy, they should be checked to ensure that it is not an ectopic pregnancy. To be able to treat the patients effectively, we must understand their TCM diagnosis and differentiation. The most important rule to remember in treating miscarriage is not to move the qi too forcefully or quicken the blood. Any Chinese herbs or acupuncture points with those functions should be used carefully or completely avoided. For those women who have had previous miscarriages, receiving TCM treatment to prepare their body before conception is just as important as the treatment during pregnancy. It is necessary to sometimes combine Chinese medicine with Western medicine to achieve the best possible
result. However, when we treat pregnant women who have conceived through IVF, ICSI or IUI, I would suggest that we must be extra cautious about prescribing Chinese herbs, especially if they have immunological disorders (which are often prescribed the aforementioned medication). In these cases, I strongly recommend using acupuncture only, unless the patient insists on taking herbs. Biography Dr. Zhao graduated from the Henan University of TCM in 1985, and has practised in the Second TCM Hospital of Luoyang city for 10 years as a consultant, specialising in gynaecological and reproductive medicine. She has been practising TCM in the UK since 1995 and founded her clinic in 1997. She has developed her special TCM programme for infertility and recurrent miscarriage, and has been working in collaboration with CARE, the largest independent fertility treatment provider in the UK and some gynaecological and reproductive consultants in the local hospitals. She has successfully treated hundreds of infertile couples across the country. She has also been featured several times on the presses and on television. For further information, please contact: fertilitycare@zhongjing.co.uk References 1. West Z. (2001). Acupuncture in Pregnancy and Childbirth. Churchill Livingstone, Elsevier Limited. Lewis T. & Chamberlain G.V.P (1990). Obstetrics by 10 Teachers. Hodder & Stoughton, London. Liang L. (2003). Acupuncture & IVF. Blue Poppy Press, London. Scientific Advisory Committee (Oct. 2003). Royal College of Obstetricians and Gynaecologists. Shen G. and Huang K. (1999). Treating Infertility with the combination of TCM and Western Medicine. Scientific and Technological Documents Publishing House, Beijing. Ndukwe G. Reproductive Immunology at CARE. Rai R, Cohen H, Dave M and Regan L. BMJ 1997. Randomised controlled trial of aspirin plus heparin in pregnant women with recurrent miscarriage associated with phospholipid antibodies (or antiphospholipid antibodies). Lewis R. (2004). The Infertility Cure. Little, Brown and Company, London.
2.
3. 4.
5.
6. 7.
8.
Potrebbero piacerti anche
- Warm Disease Made SimpleDocumento8 pagineWarm Disease Made Simplefloreslac100% (2)
- ConcussionDocumento5 pagineConcussionpeter911xNessuna valutazione finora
- Collarbone FractureDocumento1 paginaCollarbone Fracturepeter911xNessuna valutazione finora
- Concussion & Closed Head InjuriesDocumento4 pagineConcussion & Closed Head Injuriespeter911xNessuna valutazione finora
- Abnormal Sweating 1Documento4 pagineAbnormal Sweating 1peter911xNessuna valutazione finora
- Concussion SyndromeDocumento2 pagineConcussion Syndromepeter911xNessuna valutazione finora
- Mental Diseases by Acupuncture and Herbal MedicineDocumento4 pagineMental Diseases by Acupuncture and Herbal Medicinepeter911x100% (1)
- Swelling of The Lymph NodesDocumento5 pagineSwelling of The Lymph Nodespeter911x100% (3)
- 6 StagesDocumento3 pagine6 Stagespeter911x75% (4)
- Tumor FeverDocumento1 paginaTumor Feverpeter911x100% (1)
- The Acute Appendicitis Is AppendixDocumento1 paginaThe Acute Appendicitis Is Appendixpeter911xNessuna valutazione finora
- Gui Pi TangDocumento5 pagineGui Pi Tangpeter911xNessuna valutazione finora
- 4 LevelsDocumento2 pagine4 Levelspeter911cm100% (2)
- Phlegm Misting-Disturbing EJOMDocumento6 paginePhlegm Misting-Disturbing EJOMpeter911x100% (1)
- Disease Patterns of HTDocumento2 pagineDisease Patterns of HTpeter911xNessuna valutazione finora
- Heart TCM Pathology PatternsDocumento6 pagineHeart TCM Pathology Patternspeter911xNessuna valutazione finora
- Heart Syndromes QuizletDocumento2 pagineHeart Syndromes Quizletpeter911xNessuna valutazione finora
- Kidney and PsycheDocumento16 pagineKidney and Psychepeter911x100% (2)
- Kidney and PsycheDocumento16 pagineKidney and Psychepeter911x100% (2)
- Internal Medicine HEARTDocumento10 pagineInternal Medicine HEARTpeter911xNessuna valutazione finora
- QuizletDocumento1 paginaQuizletpeter911xNessuna valutazione finora
- Counseling PatientsDocumento16 pagineCounseling Patientspeter911xNessuna valutazione finora
- Counseling PatientsDocumento16 pagineCounseling Patientspeter911xNessuna valutazione finora
- Herbs Combos For Heart ProblemsDocumento1 paginaHerbs Combos For Heart Problemspeter911xNessuna valutazione finora
- Heart Patterns Functions English EnglishDocumento8 pagineHeart Patterns Functions English Englishpeter911xNessuna valutazione finora
- 4 - Fire - Heart Manage & TreatmentDocumento19 pagine4 - Fire - Heart Manage & Treatmentpeter911xNessuna valutazione finora
- Acupuncture For Memory LossDocumento3 pagineAcupuncture For Memory Losspeter911xNessuna valutazione finora
- FeverDocumento7 pagineFeverpeter911xNessuna valutazione finora
- Hepatic HemangiomatosisDocumento5 pagineHepatic Hemangiomatosispeter911xNessuna valutazione finora
- Gonorrhea by Acupuncture Plus DrugsDocumento2 pagineGonorrhea by Acupuncture Plus Drugspeter911xNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- On The Wings of EcstasyDocumento79 pagineOn The Wings of Ecstasygaya3mageshNessuna valutazione finora
- HPSC HCS Exam 2021: Important DatesDocumento6 pagineHPSC HCS Exam 2021: Important DatesTejaswi SaxenaNessuna valutazione finora
- Week 1 Familiarize The VmgoDocumento10 pagineWeek 1 Familiarize The VmgoHizzel De CastroNessuna valutazione finora
- A-1660 11TH Trimester From Mcdowell To Vodafone Interpretation of Tax Law in Cases. OriginalDocumento18 pagineA-1660 11TH Trimester From Mcdowell To Vodafone Interpretation of Tax Law in Cases. OriginalPrasun TiwariNessuna valutazione finora
- Project Analysis - M5 - MotorwayDocumento6 pagineProject Analysis - M5 - MotorwayMuhammad Haroon ArshadNessuna valutazione finora
- Chrysler CDS System - Bulletin2Documento6 pagineChrysler CDS System - Bulletin2Martin Boiani100% (1)
- Speaking RubricDocumento1 paginaSpeaking RubricxespejoNessuna valutazione finora
- Matutum View Academy: (The School of Faith)Documento14 pagineMatutum View Academy: (The School of Faith)Neil Trezley Sunico BalajadiaNessuna valutazione finora
- Big Brother Naija and Its Impact On Nigeria University Students 2 PDFDocumento30 pagineBig Brother Naija and Its Impact On Nigeria University Students 2 PDFIlufoye Tunde100% (1)
- Monster Hunter: World - Canteen IngredientsDocumento5 pagineMonster Hunter: World - Canteen IngredientsSong HoeNessuna valutazione finora
- Charter of The New UrbanismDocumento4 pagineCharter of The New UrbanismBarabas SandraNessuna valutazione finora
- ING C1 CO JUN2016 CorrectorDocumento6 pagineING C1 CO JUN2016 CorrectoraciameNessuna valutazione finora
- P D P: C I D, C M: Design of Coastal RoadsDocumento55 pagineP D P: C I D, C M: Design of Coastal RoadsMohammedNessuna valutazione finora
- Shelly Cashman Series Microsoft Office 365 Excel 2016 Comprehensive 1st Edition Freund Solutions ManualDocumento5 pagineShelly Cashman Series Microsoft Office 365 Excel 2016 Comprehensive 1st Edition Freund Solutions Manualjuanlucerofdqegwntai100% (10)
- Final LUS EvaluationDocumento36 pagineFinal LUS EvaluationNextgenNessuna valutazione finora
- Lesson Plan Letter SDocumento4 pagineLesson Plan Letter Sapi-317303624100% (1)
- KM170, KM171, KM172, F3A21, F3A22: 3 SPEED FWD (Lock Up & Non Lock Up)Documento4 pagineKM170, KM171, KM172, F3A21, F3A22: 3 SPEED FWD (Lock Up & Non Lock Up)krzysiek1975Nessuna valutazione finora
- The Teacher Research Movement: A Decade Later: Cite This PaperDocumento13 pagineThe Teacher Research Movement: A Decade Later: Cite This PaperAlexandre NecromanteionNessuna valutazione finora
- UserProvisioningLabKit 200330 093526Documento10 pagineUserProvisioningLabKit 200330 093526Vivian BiryomumaishoNessuna valutazione finora
- Immobilization of Rhodococcus Rhodochrous BX2 (An AcetonitriledegradingDocumento7 pagineImmobilization of Rhodococcus Rhodochrous BX2 (An AcetonitriledegradingSahar IrankhahNessuna valutazione finora
- CrimDocumento29 pagineCrimkeziahmae.bagacinaNessuna valutazione finora
- Masking Conventional Metallic Cast Post For Enhancing EstheticsDocumento5 pagineMasking Conventional Metallic Cast Post For Enhancing EstheticsleilyanisariNessuna valutazione finora
- Pot-Roasted Beef BrisketDocumento4 paginePot-Roasted Beef Brisketmarcelo nubileNessuna valutazione finora
- Charles Zastrow, Karen K. Kirst-Ashman-Understanding Human Behavior and The Social Environment-Thomson Brooks - Cole (2007)Documento441 pagineCharles Zastrow, Karen K. Kirst-Ashman-Understanding Human Behavior and The Social Environment-Thomson Brooks - Cole (2007)joan82% (17)
- (Ebook - Antroposofia - EnG) - Rudolf Steiner - Fundamentals of TheraphyDocumento58 pagine(Ebook - Antroposofia - EnG) - Rudolf Steiner - Fundamentals of Theraphyblueyes247Nessuna valutazione finora
- Chapter 1 INTRODUCTION TO LITERATUREDocumento4 pagineChapter 1 INTRODUCTION TO LITERATUREDominique TurlaNessuna valutazione finora
- Adigwe J. C.: ATBU, Journal of Science, Technology & Education (JOSTE) Vol. 3 (1), January, 2015 ISSN: 2277-0011Documento16 pagineAdigwe J. C.: ATBU, Journal of Science, Technology & Education (JOSTE) Vol. 3 (1), January, 2015 ISSN: 2277-0011AnnyNessuna valutazione finora
- Lesson 1 Concepts About Educational TechnologyDocumento17 pagineLesson 1 Concepts About Educational TechnologyMarvin ContigaNessuna valutazione finora
- What Is Urban PlanningDocumento33 pagineWhat Is Urban PlanningDivine Grace FernandoNessuna valutazione finora
- Simple Enzymes Kinetics and Kinetics ModelDocumento14 pagineSimple Enzymes Kinetics and Kinetics ModelSidra-tul MuntahaNessuna valutazione finora