Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Renal Physiology
Caricato da
Andhita Satya Pratama GiovanniCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Renal Physiology
Caricato da
Andhita Satya Pratama GiovanniCopyright:
Formati disponibili
Renal Physiology
I. Introduction
II. Functional Aspects of the Renal System A. Renal Vasculature --parallel vs. series arrangement --relationship between pressure, flow and resistance
B. Glomerular Filtration 1. Determinants of filtration
EFP = Pc - Pt - IIc 2. Normal values Pt = 10 mmHg IIt = 0 mmHg
EFP = effective filtration pressure
*Pc = 45 mmHg *IIc = 27 mmHg
EFP = 45 - 10 - 27 = 8 mmHg
GFR = 120 ml/min
3. Materials filtered the following are easily filtered: a. electrolytes b. metabolic waste products like urea, creatinine, and organic acids c. glucose and inulin d. amino acids e. lower weight proteins and peptides like growth hormone and inulin albumin and other plasma proteins are not filtered negative charge on the filtering membrane inhibits the filtering of anions
**fluid entering the tubule is an ultrafiltrate of plasma, i.e., filtrate has the same concentration of dissolved substances as plasma except proteins 300 mOsm 4. Factors affecting GFR and filtration fraction (FF) FF = GFR RPF RPF = renal plasma flow FF = 20%
2 main factors 1. filtration pressure 2. renal blood (plasma) flow effects of afferent arteriole constriction filtration pressure plasma flow GFR effects efferent arteriole constriction filtration pressure plasma flow GFR? FF capillary II net reabsorption pressure of peritubular capillaries effects of sympathetic system (afferent and efferent constricted) GFR FF
6. Filtration and filtered load The filtration rate (load) of a freely filtered substance is equal to: GFR X Px Px = plasma concentration of substance
Question:
Given the following information: = = = = = 120 ml/min 100 mg/100ml 140 mM 5 mM 24 mM
GFR plasma glucose plasma sodium plasma potassium plasma bicarbonate
What is the filtration rate (load) of the preceding substances? Questions 1-2. Select all the correct answers. 1. Which of the following would tend to increase glomerular filtration rate? 1. 2. 3. 4. an increase in glomerular-capillary oncotic pressure vasoconstriction of the afferent arteriole an increase in hydraulic pressure in Bowmans capsule an increase in renal blood flow
2. Which of the following would be expected to cause a large reduction in glomerular filtration rate? 1. 2. 3. 4. a reduction in mean arterial pressure from 100 to 95 mmHg a reduction in plasma oncotic pressure by one-half a decrease in sympathetic activity complete urethral obstruction
3. The glomerulus: A. is permeable to all molecules with a molecular weight (M) over 5000 B. contains no active transport systems (pumps) that produce an important effect on the composition of the glomerular filtrate C. produces a filtrate with a lower concentration of amino acids than found in plasma D. produces a filtrate with a higher concentration of urea than found in plasma E. all of the above statements are correct
4. The glomerular filtration rate: A. is greater than 50% of the plasma flow to the glomeruli B. falls to approximately 25% of normal when mean arterial pressure changes from 100 to 25 mmHg C. is decreased by a decrease in plasma colloid osmotic pressure D. increases ipsilateral to a ureteral obstruction E. none of the above statements are true Question 5. Select all the correct answers. 5. Sympathetic stimulation of the renal arterioles causing a marked reduction in renal blood flow results in: 1. 2. 3. 4. increased reabsorption of fluid by the nephron decreased glomerular filtration rate decreased peritubular hydrostatic pressure a decreased filtration fraction
6. Sympathetic stimulation of the renal arterioles results in: A. B. C. D. a greater percentage of filtrate being absorbed by the renal tubule a decreased renal filtration fraction increased peritubular hydrostatic pressure in the kidney an increased glomerular filtration rate
Question 7, true or false. 7. The filtration fraction of the kidney is normally about 20%, and is increased due to the vasoconstrictor effects of angiotensin II. 8. In a healthy individual, what percentage of the effective renal plasma flow would you expect to pass into the glomerular capsule? A. B. C. D. E. less that 5% between 15% and 20% between 40% and 50% between 70% and 80% greater than 90%
C. Tubular Reabsorption and Secretion 1. Tubular reabsorption processes involved: diffusion, facilitated diffusion, primary active transport, secondary active transport (co-transport, counter transport) a. transport maximum (Tm) systems e.g., proximal tubule glucose - carrier easily saturated
carrier high affinity for substrate low back leak
everything filtered is reabsorbed until carrier saturated, then excess excreted
b. gradient time system e.g., proximal tubule sodium - carrier never saturated - carrier low affinity for substrate - high back leak approximately a constant percentage of filtered sodium reabsorbed (70-75%_ O2 consumption of the kidney to sodium reabsorption in the proximal tubule
2. Tubular secretion a. transport maximum systems e.g., PAH
b. secretion not exhibiting Tm e.g., potassium 3. Net effects of reabsorption and secretion
filtered load = CFR x Px GFR = glomerular filtration rate (ml/min) Px = plasma concentration of substance excretion = Ux x V Ux = urine concentration of substance V = urine flow rate (ml/min)
net transport rate = filtration rate - excretion rate = (0) no tubular modification = (+) net reabsorption = (-) net secretion
Question: Given the following information: GFR = 120 ml/min plasma glucose = 300 mg/100 ml plasma sodium = 140 mM plasma potassium = 5 mM plasma bicarbonate = 24 mM urine flow = 2 ml/min urine glucose = 10 mg/ml urine sodium = 180 mM urine potassium = 8 mM urine bicarbonate = 0 Calculate the reabsorption rate of the preceding.
1. The following data are obtained from a patient: 24-hour urine sample total volume sodium concentration potassium concentration creatinine concentration urea concentration
1440 ml 120 mEq/liter 100 mEq/liter 200 mg/100ml 2050 mg/100 ml
plasma sample taken at the midpoint during the urine collection sodium concentration potassium concentration creatinine concentration urea concentration What is the rate of potassium excretion? A. B. C. D. E. less than 0.2 mEq/min 0.2 mEq/min 0.3 mEq/min 0.4 mEq/min more than 0.4 mEq/min 140 mEq/liter 5 mEq/liter 1 mg/100 ml 25 mg/100 ml
2. Toward the end of World War II, Karl Beyer and his associates noted that the injection of PAH decreased the excretion of penicillin in the urine. What would you suggest was its mechanism of action? The PAH: A. competes with penicillin for a site on a carrier molecule in one of the reabsorptive mechanisms B. prevents active reabsorption C. either of the above could be correct D. increases filtration E. competes with penicillin for a site on a carrier molecule in one of the secretory mechanisms
3. If a substance has a transport maximum (Tm) for absorption, this means: A. B. C. D. E. reabsorption is only passive only a constant fraction of the substance will be reabsorbed statements A and B are both correct below a threshold level, all of the substance will be reabsorbed phlorhizin blocks reabsorption
4. Which one of the following substances does not have a Tm value: albumin, arginine, beta hydroxybutyrate, glucose, hemoglobin, phosphate, sulfate, urea, uric acid?
D. Regional Transport along the Nephron
Proximal Tubule Cell tubule blood
Summary of proximal tubule alterations approximately 75% of the sodium that is filtered is reabsorbed here (requires ATP) about 75% of the filtered H2O, K+, C1- follow sodium and the osmolarity of urine at the end of the proximal tubule is 300 mOsm all CHO, protein, peptides, and aa reabsorbed here via secondary active transport (require luminal sodium) all filtered bicarbonate reabsorbed here a loop of henle
Loop of Henle
the mechanisms of the counter current multiplier produce the high interstitial osmolarity in the medulla fluid leaving it hypotonic the vasa recta are counter current capillary loops, flow is slow
Distal Tubule Cell
distal tubule-collecting duct sodium reabsorption-aldosterone K+ secretion acidification of urine = H+ lost as 2 forms a. H2PO4 - titratable acid b. NH4+ - nontitratable acid or ammonium water reabsorption - ADH
1. Increased blood flow through the vasa recta of the kidney allows less time for equilibrium between the medullary interstitium and the blood. This would be expected to: A. increase the solute concentration gradient between the medullary interstitial fluid and collecting duct B. concentrate the urine C. facilitate the action of anti-diuretic hormone D. reduce the osmolarity of the urine
2. The following description is most characteristic of which renal tubular segment: A. B. C. D. proximal tubule thick ascending limb of Henles loop distal convoluted tubule medullary collecting duct
Questions 3 - 7. Select all the correct answers 3. Which of the following describe glucose reabsorption by the kidney? 1. secondary active co-transport at the luminal membrane 2. characterized by a transport maximum of approximately 200 mg per 1200 ml of plasma 3. the filtered load and reabsorption rate are the same at plasma concentrations below threshold 4. active extrusion of glucose across the contraluminal membrane by the Na+ - K+ ATPase
4. A person in previously normal potassium balance maintains neurotic hyperventilation for several days. During this period, what happens to potassium balance? 1. 2. 3. 4. hyperkalemia is observed aldosterone stimulates potassium reabsorption renal excretion of potassium is unchanged renal tubular secretion of potassium is increased
5. Potassium: 1. reabsorption occurs primarily in the late distal and collecting tubule 2. excretion would be expected to increase in response to a diuretic which inhibits reabsorption of sodium chloride in the proximal tubule 3. secretion is under the control of aldosterone, by inhibiting sodium-potassium ATPase activity in the renal proximal tubule 4. has a direct effect on cells of the zona glomerulosa of the adrenal cortex to secrete aldosterone
6. Which of the following are co-transported with sodium in the renal proximal tubule? 1. 2. 3. 4. phosphate amino acids glucose potassium
7. An osmotic diuretic would be expected to: 1. 2. 3. 4. increase urine flow reduce net reabsorption of sodium in the renal proximal tubule enhance sodium excretion increase back-diffusion of sodium in the renal proximal tubule
8. Reabsorption of filtered bicarbonate: A. B. C. D. contributes to excretion of titratable acid is reduced during respiratory acidosis, resulting in increased excretion of bicarbonate is accomplished by net secretion of sodium is enhanced by carbonic anhydrase
9. Potassium: A. reabsorption occurs primarily in the late distal and collecting tubule B. excretion would be expected to increase in response to a diuretic which inhibits reabsorption of sodium chloride in the proximal tubule C. reabsorption in under the direct control of vasopressin, which stimulates sodiumpotassium ATPase activity in the renal proximal tubule D. has a direct effect on cells of the zona glomerulosa of the adrenal cortex to prevent secretion of aldosterone
Questions 10-13.
Select all the correct answers
10. If renal tubular carbonic anhydrase were completely inhibited, you would expect increased excretion of which of the following? 1. 2. 3. 4. sodium water bicarbonate potassium
11. Reabsorption of filtered bicarbonate: 1. 2. 3. 4. contributes to excretion of titratable acid is accompanied by net secretion of sodium reduces the pH of the extracellular fluid is enhanced by carbonic anhydrase
12. The renal countercurrent multiplier is characterized by: 1. 2. 3. 4. a low water permeability in the thick ascending limb of Henles loop permeability of the descending limb of Henles loop to water active salt reabsorption in the thick ascending limb of Henles loop tubular fluid in the thick ascending limb of Henles loop which is more concentrated than the interstitial fluid at that level
13. An osmotic diuretic would be expected to: 1. 2. 3. 4. enhance net reabsorption of sodium in the proximal tubule increase urine volume reduce potassium excretion increase back-diffusion of sodium in the proximal tubule
14. Which of the following structures in the kidney would you expect to be most involved in concentrating the urine? A. B. C. D. E. superficial nephrons the proximal tubule Bowmans capsule the glomerulus juxtamedullary nephrons
15. Potassium: A. reabsorption occurs primarily in the late distal and collecting tubule B. excretion would be expected to decrease in response to a diuretic which inhibits reabsorption sodium chloride in the proximal tubule C. reabsorption is under the control of anti-diuretic hormone, which stimulates sodiumpotassium ATPase activity D. has a direct effect on cells of the zona glomerulosa of the adrenal cortex to secrete aldosterone
E. Clearance concept and renal calculations 1. clearance definition C = U x V P U = urine concentration V = urine flow rate P = plasma concentration
= ml/min Clearance = the minimum volume of plasma at the prevailing plasma concentrations that could have supplied the material appearing in the urine in the given time interval. List the following from the least to the greatest clearance: sodium glucose creatinine inulin PAH
2. GFR measurements GFR = Cin = Uin x V Pin inulin freely filtered, not metabolized, not secreted, not reabsorbed substances used instead of inulin: mannitol, sucrose, creatinine* (*some secreted in humans*)
Cx > Cin - substance filtered and secreted (e.g., PAH) Cx < Cin - substance filtered and reabsorbed or not freely filtered (e.g., glucose) concentration of inulin in the tubule is an index of water reabsorption
3. Renal blood flow measurement PAH - filtered + completely secreted
Cpah = ERPF (effective renal plasma flow)
ERPF = Vpah x V Ppah renal blood flow = ERPF (1 Hct)
4. Filtration fraction (FF) FF = GFR = Cin RPF Cpah 5. Free water clearance - denotes the volume of pure water that must be removed from or added to the flow of urine to make it isosmotic with plasma Cosm - Vosm x V Posm
C C C
H2O = V - Cosm H20 (+) = plasma being concentrated, dilute urine is formed H20 (-) = plasma diluted, concentrated urine is formed
6. Fraction of filtered material excreted (Fractional excretion) FE = Ux / Px = excretion filtered load Uin / Pin = clearance of x clearance of inulin
> <
1 1
= =
net secretion net reabsorption
1. Which of the following substances has the greatest renal clearance? A. B. C. D. E. inulin sodium urea creatinine glucose
2. Determine the excretion of glucose given the following data: urine glucose concentration urine inulin concentration plasma glucose concentration plasma inulin concentration urine flow rate A. B. C. D. 112 mg/min 98.5 mg/min 200 mg/min 2.5 mg/min 125 mg/100ml 56 mg/100ml 90 mg/100ml 1 mg/100ml 2 ml/min
3. The following data are obtained for a patient: inulin clearance plasma bicarbonate concentration urine bicarbonate concentration urine pH titratable acid in urine ammonium ion in urine 170 L/day 25 mmol/L 0 mmol/L 5.8 26 mmol/day 48 mmol/day
Calculate the total amount of hydrogen ions secreted: A. B. C. D. 4250 mmol/day 26 mmol/day 74 mmol/day 4324 mmol/day
4. Given the following data: urine flow rate urine osmolarity plasma osmolarity What is the free-water clearance? A. B. C. D. 2 L/24 hours -0.5 L/24 hours -4 L/24hours 1 L/24 hours 0.5 liters/24 hours 600 mosmol/L 300 mosmol/L
5. Given the following data: urine concentration of sodium urine concentration of inulin plasma concentration of sodium plasma concentration of inulin What is the fractional excretion of sodium? A. B. C. D. 1.0 0.5 0.1 0.25 1400 mEq/1 1 mg/ml 140 mEq/1 .01 mg/ml
6. Calculate the renal filtered load of sodium: glomerular filtration rate: urine flow rate urine concentration of inulin plasma concentration of sodium A. B. C. D. 20 ml/min 100 mg/min 12 mEq/min 50 ml/min 100 ml/min 2.4 ml/min 1 mg/ml 0.12 mEq/ml
7. Renal clearance of inulin provides a measure of: A. B. C. D. renal blood flow cardiac output glomerular filtration rate renal plasma flow
8. Calculate the free-water clearance in a patient with the following laboratory date: urine output glomerular filtration rate osmolarity of the urine osmolarity of the plasma A. B. C. D. 2.25 L/24hours 1.5 L/24 hours 3.0 L/24 hours 0.75 L/24 hours 1.5 L/24 hours 125 ml/min 150 m0smol/L 300 m0smol/L
9. calculate the bicarbonate reabsorption in a patient with the following data: clearance in inulin: plasma bicarbonate urine bicarbonate urine pH titratable acid in urine urine ammonium ion 175 L/day 25 mmol/L 0 5.8 26 mmol/day 48 mmol/day
A. B. C. D.
4449 mmol/day 74 mmol/day 26 mmol/day 4375 mmol/day
10. How much new bicarbonate has been added to the blood of the above patient? A. B. C. D. 48 mmol/day 26 mmol/day 4449 mmol/day 74 mmol/day
11. Calculate the renal plasma flow of a patient given the data below: effective renal plasma flow 585 ml/min uncorrected measured hematocrit 45% renal extraction of PAH 0.90 (i.e., 90% of PAH is removed from the plasma by the kidney in a single passage) A. B. C. D. 1064 ml/min 961 ml/min 1066 ml/min 650 ml/min
Question 12. Select all correct answers.
12. Regarding the fractional excretion of a freely filtered susbstance: 1. a value greater than one suggests that net secretion of the substance has occurred 2. in hypernatremia (high sodium in plasma) the fractional excretion of sodium is greater than one 3. the renal clearance of a substance X divided by the inulin clearance is a measure of the fractional excretion of substance X 4. it is necessary to measure urine flow rate to determine the fractional excretion of a substance
DIRECTIONS: (Questions 13-14). Answer true or false to the following statements by marking A for true and B for false.
13. The renal clearance of glucose is less than that of inulin 14. Inulin is present at the same concentration in the glomerular filtrate and the final urine.
15. Which one of the following statements is most consistent with a filterable substance being actively reabsorbed from the renal tubular lumen? A. its renal clearance value is lower than that of inulin B. its renal clearance value is higher than that of inulin C. the ratio of its rate of urinary excretion/plasma concentration is the same as that for glucose D. the ratio of its rate of urinary excretion/plasma concentration is greater than that for glucose E. its concentration in the distal tubule is higher than that in plasma
16. During the infusion of PAH into a patient, the concentration of PAH in the cephalic vein stabilized at 0.02 mg/ml of plasma (=PPAH). At this time, the two kidneys were producing 1 ml of urine per minute (=VU), and the concentration of PAH in the urine was 16 mg/ml (=UPAH). What was the PAH clearance (=CPAH)? What was the effective renal plasma flow (=ERPF)?
17. The renal clearance of (select the one best answer): A. B. C. D. a substance is measured in mg/ml a substance is measured in mg/min sodium is decreased by the injection of aldosterone inulin, at a plasma concentration of 60 mg%, is lower than at a plasma concentration of 120 mg% E. para-aminohippurate (PAH) at a plasma concentration of 60 mg% is higher than at a plasma concentration of 120 mg%
18. The clearance of substances f, g and h are studied at different concentrations in the blood. The following data are obtained:
Which of the following statements best characterizes substance f ? Substance f in the nephron is: A. B. C. D. E. secreted reabsorbed filtered filtered and reabsorbed filtered and secreted
19. Which one of the following statements best characterizes substance h in question18. Substance h in the nephron is: A. B. C. D. E. filtered and actively secreted filtered and passively reabsorbed filtered, passively reabsorbed, and actively reabsorbed filtered and synthesized filtered, synthesized, and secreted
20. Which one of the following statements concerning curve h in question 18 is true? the plasma concentration at point: A. B. C. D. E. i represents the transport maximum i represents the splay i represents the threshold j represents the splay j represents the threshold
21. All of the following substances are filtered into the glomerular capsule. Indicate which ones will produce a clearance curve in man similar to f, g or h in question 18. One of these substances has a Tm value of 375 mg/min and another of 1 mg/min. Therefore, in making your comparisons, concentrate on the shape of the clearance-concentration curve, not absolute values of concentration. _____inulin _____glucose _____PAH _____sulfate _____ascorbic acid _____penicillin _____albumin _____arginine _____ketone bodies _____lysine _____hemoglobin _____diodrast _____phosphate
Answers to Renal Questions
Pages 4-5 1. 2. 3. 4. 5. 6. 7. 8. 4 only 4 only B E A A T B
Pages 19-23 1. D 2. D 3. D 4. B 5. C 6. C 7. C 8. D 9. D 10. D 11. D 12. B 13. A 14. B 15. C 16. 800 ml/min 17. C 18. E 19. C 20. C 21. g f h hhh fhf hhh h
Page 10 1. 2. 3. 4. A E D Urea
Pages 14-16 1. D 2. A 3. 1 & 3 4. 4 only 5. 2 & 4 6. 1, 2, 3 7. all 8. D 9. B 10. all 11. 4 only 12. 13. 2 & 4 14. E 15. D
Potrebbero piacerti anche
- Mcqs RenalDocumento19 pagineMcqs RenaldevdsantoshNessuna valutazione finora
- Physio Multiple Choice Body Fluids and Renal and RespDocumento15 paginePhysio Multiple Choice Body Fluids and Renal and Respsac50900Nessuna valutazione finora
- Renal Physiology:: 1. Renal Blood Flow Is Dependent OnDocumento16 pagineRenal Physiology:: 1. Renal Blood Flow Is Dependent OnBlackstarNessuna valutazione finora
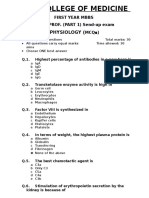
- First Part Exam - March 2021Documento28 pagineFirst Part Exam - March 2021hassan mohamedNessuna valutazione finora
- Renal Physiology RevisionDocumento6 pagineRenal Physiology RevisionramadanNessuna valutazione finora
- MCI Screening Test 2005Documento46 pagineMCI Screening Test 2005Iboyaima SinghNessuna valutazione finora
- PHYSIO MCQsDocumento10 paginePHYSIO MCQsarwa fawzy100% (1)
- 7 RespirationDocumento15 pagine7 RespirationCLEMENTNessuna valutazione finora
- 5 - Cardiac Output - Ass. Prof. Dalia Abd El-Salam - 2020Documento6 pagine5 - Cardiac Output - Ass. Prof. Dalia Abd El-Salam - 2020Hossam BaniisNessuna valutazione finora
- Physiology QuestionsDocumento14 paginePhysiology QuestionsLamis Alhaj KaddamNessuna valutazione finora
- The Fate of Metabolism Andmabolic PathwaysDocumento25 pagineThe Fate of Metabolism Andmabolic PathwaysXuân Vi100% (1)
- (K) Gastroenteritis and Fluid VolumeDocumento1 pagina(K) Gastroenteritis and Fluid Volumeapi-3769252Nessuna valutazione finora
- Respiratory System Study GuideDocumento13 pagineRespiratory System Study GuidebisnumNessuna valutazione finora
- DPP 2 Oesophagus and StomachDocumento4 pagineDPP 2 Oesophagus and StomachDr-Atin Kumar SrivastavaNessuna valutazione finora
- Renal Physiology Practice QuestionsDocumento4 pagineRenal Physiology Practice QuestionsAndiWilkinsNessuna valutazione finora
- Chapter 70-GuytonDocumento9 pagineChapter 70-Guytonswoljaswol1Nessuna valutazione finora
- Physiology Final Exams JULY 8, 2020Documento17 paginePhysiology Final Exams JULY 8, 2020Ndor BariboloNessuna valutazione finora
- 054 Physiology MCQ ACEM Primary RenalDocumento1 pagina054 Physiology MCQ ACEM Primary RenalYasif AbbasNessuna valutazione finora
- Zanki Respiratory PhysiologyDocumento19 pagineZanki Respiratory Physiologysmian08Nessuna valutazione finora
- MCQ Renal Phys1Documento7 pagineMCQ Renal Phys1Arif Nabeel100% (1)
- 2 K 23 Mbbs CurriculumDocumento300 pagine2 K 23 Mbbs CurriculumAbdullah Nayyar100% (1)
- Respiratory QuestionsDocumento116 pagineRespiratory QuestionsNatukunda Dianah100% (1)
- The HeartDocumento15 pagineThe HeartCLEMENTNessuna valutazione finora
- ABG Exercises 3Documento19 pagineABG Exercises 3REMAN ALINGASANessuna valutazione finora
- MCQs On CVS Pharmacology by Medical Study CenterDocumento47 pagineMCQs On CVS Pharmacology by Medical Study CenterLin YunNessuna valutazione finora
- 1st Year Sendup MCQsDocumento8 pagine1st Year Sendup MCQsTARIQNessuna valutazione finora
- Important Seqs of Biochemistry For 1st Year Mbbs StudentsDocumento7 pagineImportant Seqs of Biochemistry For 1st Year Mbbs Studentsdr saadia anjum0% (1)
- Renal Physiology McqsDocumento1 paginaRenal Physiology Mcqsahmed100% (1)
- Physiology McqsDocumento5 paginePhysiology McqsFaisal AwanNessuna valutazione finora
- Physiology Final Exam - Glory 2017 PDFDocumento14 paginePhysiology Final Exam - Glory 2017 PDFMohammad BarakatNessuna valutazione finora
- Mcq-Heart Conducting SystemDocumento42 pagineMcq-Heart Conducting SystemDan BrightNessuna valutazione finora
- Ganong Physiology 21eDocumento1 paginaGanong Physiology 21eprasun_v0% (1)
- Physiology Final Exam QuestionsDocumento3 paginePhysiology Final Exam QuestionsRohini Selvarajah100% (1)
- Lecture 7 ThermoregulationDocumento30 pagineLecture 7 ThermoregulationLouella Artates100% (1)
- Biochem 2Documento7 pagineBiochem 2Aleena KarimNessuna valutazione finora
- Practical PhysiologyDocumento11 paginePractical Physiologyapi-3728690Nessuna valutazione finora
- Shams Pulmonary Quiz 1Documento9 pagineShams Pulmonary Quiz 1tylermedNessuna valutazione finora
- Physio-DES-6 (Cardiac)Documento56 paginePhysio-DES-6 (Cardiac)Joseph Kim100% (1)
- Respiration:: Mcqs PhysiologyDocumento96 pagineRespiration:: Mcqs PhysiologyAhmedNessuna valutazione finora
- Cardiovascular Physiology - Cardiac Cycle and MurmursDocumento107 pagineCardiovascular Physiology - Cardiac Cycle and MurmursAaron D. Phoenix100% (1)
- 47 MCQs On GI and Nutrition PhysiologyDocumento14 pagine47 MCQs On GI and Nutrition Physiologyrazsubedi100% (1)
- Cvs MCQDocumento52 pagineCvs MCQMiracle For NursesNessuna valutazione finora
- Bone McqsDocumento4 pagineBone McqsAwan1994100% (2)
- TextDocumento14 pagineTextOdigo OfujeNessuna valutazione finora
- Shams Pulmonary Quiz 2Documento16 pagineShams Pulmonary Quiz 2tylermedNessuna valutazione finora
- Endocrine SystemDocumento51 pagineEndocrine SystemMahenor Emad100% (1)
- Biology, 7e (Campbell) : Chapter 41: Animal NutritionDocumento7 pagineBiology, 7e (Campbell) : Chapter 41: Animal Nutrition123456789123456789hiNessuna valutazione finora
- CVS Embryology Questions and Study Guide - Quizlet Flashcards by Hugo - OxfordDocumento5 pagineCVS Embryology Questions and Study Guide - Quizlet Flashcards by Hugo - OxfordAzizNessuna valutazione finora
- Metabolism MCQ ADocumento0 pagineMetabolism MCQ ASurajit BhattacharjeeNessuna valutazione finora
- 1.about Some GIT Hormones (True or False)Documento71 pagine1.about Some GIT Hormones (True or False)JOSEPH NDERITU100% (2)
- Biochem Chapter19a ProfDocumento8 pagineBiochem Chapter19a ProfAnonymous t5TDwdNessuna valutazione finora
- MCQ ChoDocumento31 pagineMCQ Choامجد حسين جواد كاظمNessuna valutazione finora
- MCQs On GITDocumento3 pagineMCQs On GITsamuel waiswaNessuna valutazione finora
- Renal Control of Acid Base BalanceDocumento5 pagineRenal Control of Acid Base BalanceEuniceSimNessuna valutazione finora
- 2006 PhysioDocumento18 pagine2006 Physioanaeshkl100% (1)
- Biochem Practical QuestionsDocumento13 pagineBiochem Practical QuestionsBurhan HameedNessuna valutazione finora
- MCQ - Test 2Documento3 pagineMCQ - Test 2Gaurav SinghNessuna valutazione finora
- Quiz - Development of Human Cardiovascular SystemDocumento7 pagineQuiz - Development of Human Cardiovascular Systemlucky mbaselaNessuna valutazione finora
- CVS MCQDocumento14 pagineCVS MCQNur Hamizah Md FuziNessuna valutazione finora
- Hazardous Compounds in Tobacco SmokeDocumento16 pagineHazardous Compounds in Tobacco SmokePutra Dhyatmika100% (1)
- Animals Think and FeelDocumento5 pagineAnimals Think and FeelAndhita Satya Pratama GiovanniNessuna valutazione finora
- 1 PDFDocumento11 pagine1 PDFAndhita Satya Pratama GiovanniNessuna valutazione finora
- Excitatory Inhibitory BalanceDocumento14 pagineExcitatory Inhibitory BalanceAndhita Satya Pratama GiovanniNessuna valutazione finora
- CardiologiaDocumento5 pagineCardiologiaAndhita Satya Pratama GiovanniNessuna valutazione finora
- ReferencesDocumento2 pagineReferencesAndhita Satya Pratama GiovanniNessuna valutazione finora
- c1Documento11 paginec1Andhita Satya Pratama GiovanniNessuna valutazione finora
- CardiologiaDocumento5 pagineCardiologiaAndhita Satya Pratama GiovanniNessuna valutazione finora
- Proteinuria Round TableDocumento16 pagineProteinuria Round TableAndhita Satya Pratama GiovanniNessuna valutazione finora
- UHL Hyperosmolar Non-Ketotic Diabetic State - HONKDocumento5 pagineUHL Hyperosmolar Non-Ketotic Diabetic State - HONKAndhita Satya Pratama GiovanniNessuna valutazione finora
- Optimizing Therapeutics in The Management of Patients With Multiple Sclerosis: A Review of Drug Efficacy, Dosing, and Mechanisms of ActionDocumento12 pagineOptimizing Therapeutics in The Management of Patients With Multiple Sclerosis: A Review of Drug Efficacy, Dosing, and Mechanisms of ActionAndhita Satya Pratama GiovanniNessuna valutazione finora
- An Approach To Interpreting SpirometryDocumento8 pagineAn Approach To Interpreting Spirometrylisa_hayesNessuna valutazione finora
- Spirometer Handbook NacaDocumento24 pagineSpirometer Handbook NacaebrycNessuna valutazione finora
- Abdominal Examination SignsDocumento2 pagineAbdominal Examination SignsAndhita Satya Pratama Giovanni0% (2)
- Ampullary Cancer: Review and Clinical Update: Melissa Chan, MD, and Douglas G. Adler, MD, FACG, FASGEDocumento6 pagineAmpullary Cancer: Review and Clinical Update: Melissa Chan, MD, and Douglas G. Adler, MD, FACG, FASGEAndhita Satya Pratama GiovanniNessuna valutazione finora
- Karnofsky/Lansky Performance StatusDocumento0 pagineKarnofsky/Lansky Performance StatusHanayuki VizureiNessuna valutazione finora
- CheungDocumento104 pagineCheungAndhita Satya Pratama GiovanniNessuna valutazione finora
- AbsDocumento1 paginaAbsAndhita Satya Pratama GiovanniNessuna valutazione finora
- Ampullary Cancer: Review and Clinical Update: Melissa Chan, MD, and Douglas G. Adler, MD, FACG, FASGEDocumento6 pagineAmpullary Cancer: Review and Clinical Update: Melissa Chan, MD, and Douglas G. Adler, MD, FACG, FASGEAndhita Satya Pratama GiovanniNessuna valutazione finora
- Chapters 36, 37Documento80 pagineChapters 36, 37Andhita Satya Pratama GiovanniNessuna valutazione finora
- EndophthalmitisDocumento25 pagineEndophthalmitisAndhita Satya Pratama GiovanniNessuna valutazione finora
- Diabetes and The EyeDocumento7 pagineDiabetes and The EyeAndhita Satya Pratama GiovanniNessuna valutazione finora
- 1300 NobleDocumento39 pagine1300 NobleAndhita Satya Pratama GiovanniNessuna valutazione finora
- PR Tianma Perlieremimi Impactra Final-100220Documento10 paginePR Tianma Perlieremimi Impactra Final-100220jerryNessuna valutazione finora
- Fphar 12 768268Documento25 pagineFphar 12 768268Araceli Anaya AlvaradoNessuna valutazione finora
- Microbial ResistanceDocumento16 pagineMicrobial ResistanceDixa MeNessuna valutazione finora
- Herbal Remedies For Mouth Ulcer: A Review: KeywordsDocumento7 pagineHerbal Remedies For Mouth Ulcer: A Review: KeywordsumapNessuna valutazione finora
- Revision Study Material Unit - X: Anti-Viral & HIV DrugsDocumento16 pagineRevision Study Material Unit - X: Anti-Viral & HIV DrugsMagesh SNessuna valutazione finora
- World University of Bangladesh: An AssignmentDocumento5 pagineWorld University of Bangladesh: An AssignmentMD REFATNessuna valutazione finora
- Volume of DistributionDocumento11 pagineVolume of DistributionDr. Mushfique Imtiaz ChowdhuryNessuna valutazione finora
- Thoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryDocumento8 pagineThoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryIJAR JOURNALNessuna valutazione finora
- Biliary Tract Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Documento96 pagineBiliary Tract Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Sabbir RaihanNessuna valutazione finora
- Pharmd - 3Y - 3.5 - Medicinal ChemistryDocumento41 paginePharmd - 3Y - 3.5 - Medicinal ChemistrySyed Ali ShahNessuna valutazione finora
- Sustanon '250': Name of The MedicineDocumento7 pagineSustanon '250': Name of The MedicineAmalia WardatulNessuna valutazione finora
- Journal of Ethnopharmacology: Gardenia Jasminoides Ellis: Ethnopharmacology, Phytochemistry, andDocumento28 pagineJournal of Ethnopharmacology: Gardenia Jasminoides Ellis: Ethnopharmacology, Phytochemistry, andeman mamdohNessuna valutazione finora
- Case Study AppendicitisDocumento58 pagineCase Study AppendicitisArianne Joy Balon100% (2)
- Рractical lesson№1.INTRODUCTION TO THE PRESCRIPTIONS.Documento15 pagineРractical lesson№1.INTRODUCTION TO THE PRESCRIPTIONS.Marwan Diaa El BahyNessuna valutazione finora
- CarbamazepineDocumento5 pagineCarbamazepineapi-3797941100% (2)
- 3-Fred Davies (14 Aug 2020) Hawazen - CheckedDocumento3 pagine3-Fred Davies (14 Aug 2020) Hawazen - CheckedDr. Emad Elbadawy د عماد البدويNessuna valutazione finora
- Locuri A 2 A Specialitate NOIEMBRIE 2022Documento2 pagineLocuri A 2 A Specialitate NOIEMBRIE 2022madimadi11Nessuna valutazione finora
- Antifungal Potential of Aqueous Extract of Mondia Whitei Root Bark Phytochemical Analysis and Inhibition StudiesDocumento7 pagineAntifungal Potential of Aqueous Extract of Mondia Whitei Root Bark Phytochemical Analysis and Inhibition StudiesKIU PUBLICATION AND EXTENSIONNessuna valutazione finora
- 2010 AAO's DIARYDocumento99 pagine2010 AAO's DIARYCheri PerezNessuna valutazione finora
- Comparison of The Effects of Citicoline and Piracetam On Hypoxic-Ischemic Brain Damage in Neonatal RabbitsDocumento7 pagineComparison of The Effects of Citicoline and Piracetam On Hypoxic-Ischemic Brain Damage in Neonatal RabbitsAgung WpNessuna valutazione finora
- Ambulatory Urology and Urogynaecology, 2021Documento286 pagineAmbulatory Urology and Urogynaecology, 2021Desmosedici GrenadierNessuna valutazione finora
- National Comprehensive HIV Prevention, Care, and Treatment Training For Pharmacy Professionals-Participant ManualDocumento326 pagineNational Comprehensive HIV Prevention, Care, and Treatment Training For Pharmacy Professionals-Participant ManualAYANA KORSANessuna valutazione finora
- BOMRA Registration Quality GuidelinesDocumento95 pagineBOMRA Registration Quality GuidelinesBK RegulatoryNessuna valutazione finora
- Intravenous Infusion of Lidocaine Reduces PropofolDocumento6 pagineIntravenous Infusion of Lidocaine Reduces PropofolAnonymous lSWQIQNessuna valutazione finora
- MY Hematology MasterclassDocumento32 pagineMY Hematology Masterclassabdul qayyumNessuna valutazione finora
- Extraction and Preliminary Phytochemical Screening of Active Compounds in Morinda Citrifolia FruitDocumento4 pagineExtraction and Preliminary Phytochemical Screening of Active Compounds in Morinda Citrifolia FruitnoviNessuna valutazione finora
- Montair LC TabletsDocumento9 pagineMontair LC Tabletskurutala100% (1)
- Development and Characterization of A New Oral Dapsone Nanoemulsion System: Permeability and in Silico Bioavailability StudiesDocumento8 pagineDevelopment and Characterization of A New Oral Dapsone Nanoemulsion System: Permeability and in Silico Bioavailability StudiesTheva CharaanNessuna valutazione finora
- PHARMA ProblemsDocumento13 paginePHARMA ProblemsEllen Mynelle Mabulac100% (1)
- Asthma Molecular and Drug DevelopmentDocumento17 pagineAsthma Molecular and Drug DevelopmentTira MaharaniNessuna valutazione finora