Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Sputum Examination
Caricato da
Dr. Ashish JawarkarCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Sputum Examination
Caricato da
Dr. Ashish JawarkarCopyright:
Formati disponibili
1
SPUTUM EXAMINATION
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
OVERVIEW 1. 2. 3. 4. Indications Collection of sputum Sample transport Sample analysis a. Physical examination b. Microbiological examination 1. Gram stain 2. Culture and sensitivity 3. Examination for acid fast bacilli a. Zn stain b. Fluorescent stain c. Culture on conventional media d. Commercial automated culture system e. Molecular methods 4. Examination for other specific organisms c. Cytological examination
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
* Indications 1. Smear and culture Identification of causative organism in a suspected infection - like pneumonia, TB, fungal infection, P. carinii in HIV, bronchiectasis 2. Cytological examination 1. for malignant cells 2. Looking for viral inclusions 3. asbestosis
* Collection of sputum 1. Early morning deep cough sample is preferred 2. If unable to cough, induction of sputum can be done by a. 15% NaCl aerosol spray & propylene glycol for 20 min or b. Nebulized hypertonic saline and distilled water Collected in: 1. dry wide mouthed container with 25 ml capacity 2. leak proof to prevent aerosols 3. break resistant to prevent dessication
* Sample transport 1. samples should be immediately transported to laboratory as such if nearby 2. if distant laboratory, transport in 25 ml of the following solution N acetyl pyridinium chloride 5g Sodium chloride 10g Distilled water 1 lt If sputum is allowed to stand without medium a. rapid proliferation of contaminating bacterial flora from oral cavity and throat b. H. influenzae donot survive for long Donot refrigerate in any case
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
* SAMPLE ANALYSIS
(i) Physical appearance
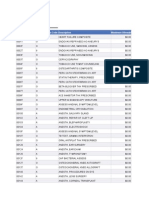
Bloody (hemoptysis) Pulmonary TB Lung abcess Bronchiectasis Bronchogenic carcinoma Mitral stenosis Pulmonary infarction Pneumococcal lobar pneumonia Klebsiella Pseudomonas Pneumonia, lung abcess Pulmonary edema
Rusty Red currant jelly Green Purulent Pink and frothy
(ii) Microbiological examination
#GRAM STAIN:
Prerequisites 1. There should not be squamous cells covered with masses of bacteria indicates sample is mostly from mouth or throat 2. If PMNs are <10 per epithelial cell no need for culture 3. Knowledge of flora of mouth and pharynx necessary before analyzing Normal flora of oral cavity and pharynx GRAM POSITIVE 1. staphylococcus aureus and epidermidis 2. streptococcus viridans and pneumonia 3. diphtheroids 4. enterococci 5. micrococci 6. lactobacilli 7. yeasts (candida) GRAM NEGATIVE 1. neiserria 2. H. influenzae 3. fusobacterium 4. coliforms 5. m. catarrhalis
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
Analysis Streptococcus Pneumoniae Staphylococcus aureus Candida H. influenzae M. catarrhalis Actinomyces Gram positive diplococci with surrounding clear space Gram positive cocci in grape like clusters Gram positive yeast cells with budding yeasts and pseudohyphae Gram negative coccobacilli Gram negative diplococci both intra and extracellular Large granules with center gram negative and periphery gram positive
#CULTURE:
Ideal sample for culture 1. should contain <25 squamous cells per low power filed or <10 squamous cells per high power field 2. sample should contain alveolar macrophages 3. neutrophils should be >10 per epithelial cell or >5 per high power field 4. bronchial epithelial cells present 5. sample should be washed with normal saline to wash the saliva Method: Inoculate the sample on blood agar and chocolate agar
Incubate in an atmosphere of extra CO2
Inspect plates after 18 hours
If growth is significant, antibiotic sensitivity testing is carried out
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
#EXAMINATION FOR ACID FAST BACILLI
!. ZEIHL NEELSON STAINING (AFB stain) Sample: 1. According to RNTCP guidelines, 2 samples are collected, one stat and one early next morning sample. It should be deep cough sputum sample 2. for children, gastric aspirate can be used as they often swallow sputum Preparation: smear is prepared with blood tinged/opaque/grayish/yellowish portion of the sputum
stained with ZN stain
Examined under microscope Reporting guidelines (RNTCP): 1. Mycobacteria appear as bright red, slightly curved or red beaded rods, 2-4 m in length and 0.2 to 0.5 m wide, against a blue green background. 2. Atleast 100 fields should be examined before declaring negative.
Drawbacks: 1. sensitivity 60-80% 2. minimum 5000-10000 bacilli / ml should be present for smear to be positive Bleaching technique: 1. A solution of sodium hypochlorite is added to sputum sample it leads to liquefaction of mucous and killing of microbes 2. smears are prepared from sediment and stained with ZN stain
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
2. FLUORESCENCE MICROSCOPY 1. Slides are stained with fluorescent auramine-rhodamine or auramine O 2. Observed under fluorescent microscope mycobacteria appear bright yellow against green background 3. CULTURE ON CONVENTIONAL MEDIA Indications: 1. drug susceptibility testing 2. species identification if other than M. tuberculosis suspected 3. sputum smear negative and strong clinical suspicion Prerequisites: 1. 4% NaOH should be added before inoculation 2. this is because sputum samples are contaminated with normal flora, which grow and digest the media before MTB can grow 3. 4% NaOH kills this flora Media used: 1. solid media LJ media (egg based) or Middle brook (agar based) 2. Liquid media middle brook, TH9, TH 12 Advantage: 1. sensitivity 80-85% 2. can detect as low as 10-100 bacteria/ml Drawbacks: 1. expensive 2. requires 6 weeks for results
4. COMMERCIAL AUTOMATED CULTURE METHODS (BACTEC) 1. Can give results in 2 weeks 2. mycobacteria are inoculated in a broth containing 14C palmitate 3. mycobacteria metabolise 14C palmitate and release 14CO2 which is detected by the instrument 5. MOLECULAR METHODS (PCR) 1. 2. 3. 4. DNA sequences identified in MTB genome by PCR can detect bacteria as low as 10-100 organisms / ml of sputum direct sputum sample or culture samples can be used laboratory cross contamination is an important issue here
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
#EXAMINATION OF OTHER ORGANISMS ON SMEAR P. carinii Yersinia Fungus Histoplasma Aspergillus Paragonimus SPECIFIC INVESTIGATIONS Use BAL and stain with silver stain and giemsa Giemsa stain SDA/KOH mount Giemsa KOH Saline wet mount of sputum for eggs
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
(iv) Cytological examination
Prerequisites: 1. 2. 3. 4. fresh morning sample transport without delay for suspected lung Ca collect sample for 5 consecutive days if delay anticipated, prefix with Saccomanos fixative (50% ethyl alcohol and 2% carbowax)
Method: 1. smears are made from blood tinged portion or tissue fragments and stained with pap stain 2. to be adequate, bronchial epithelial cells and alveolar macrophages must be seen Drawback: Sensitivity is only 65% This sensitivity is more if 1. smears are examined from multiple samples 2. lesion is located centrally 3. larger tumor size 4. histologic type is SCC rather than adenocarcinoma
Notes on sputum examinationBy Dr. Ashish V. Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
Potrebbero piacerti anche
- Practical Manual for Detection of Parasites in Feces, Blood and Urine SamplesDa EverandPractical Manual for Detection of Parasites in Feces, Blood and Urine SamplesNessuna valutazione finora
- Urine Culture: D.M.M. LabDocumento15 pagineUrine Culture: D.M.M. LabTomi RahmadaniNessuna valutazione finora
- Accurate Diagnosis of Parasitic Infections Is Important To Decrease The Prevalence andDocumento4 pagineAccurate Diagnosis of Parasitic Infections Is Important To Decrease The Prevalence andManulat VicaiiNessuna valutazione finora
- Stool Exam - Routine, Conc. Method - Students'Documento27 pagineStool Exam - Routine, Conc. Method - Students'AnastasiaNessuna valutazione finora
- (Document Title) : Group 4: Ilarde, Judegarcia, Krllopez, Klim Casing, Rychele BSN4 2019Documento8 pagine(Document Title) : Group 4: Ilarde, Judegarcia, Krllopez, Klim Casing, Rychele BSN4 2019qwerty24Nessuna valutazione finora
- Sputum AnalysisDocumento4 pagineSputum AnalysisGlenn PerezNessuna valutazione finora
- Examination of Specimens For ParasitesDocumento32 pagineExamination of Specimens For ParasitesJhost Clinton PurbaNessuna valutazione finora
- Sputum AnalysisDocumento12 pagineSputum AnalysisAdriana GarciaNessuna valutazione finora
- Sjogren'S Syndrome: Guided By: Dr. Richa MohanDocumento17 pagineSjogren'S Syndrome: Guided By: Dr. Richa MohanAnkyNessuna valutazione finora
- Stool ExaminationDocumento5 pagineStool ExaminationFrinkaWijayaNessuna valutazione finora
- Chapter15 StreptococciDocumento66 pagineChapter15 StreptococciNursheda Abangon AzisNessuna valutazione finora
- Diagnostic Microbiology: CampylobacterDocumento25 pagineDiagnostic Microbiology: Campylobacteranon_914901469Nessuna valutazione finora
- Practical 4 Staphylococci PresentationDocumento24 paginePractical 4 Staphylococci PresentationPatrisha BuanNessuna valutazione finora
- Histopathology InstrumentsDocumento6 pagineHistopathology InstrumentsLawrence LeeNessuna valutazione finora
- Serology & Immunology - INTRODUCTION (SC)Documento31 pagineSerology & Immunology - INTRODUCTION (SC)Aira Kim ReotutarNessuna valutazione finora
- Introduction To ParasitologyDocumento44 pagineIntroduction To ParasitologyRIC JOSEPH PONCIANONessuna valutazione finora
- Pap Smear: Dr. Monika NemaDocumento114 paginePap Smear: Dr. Monika NemafadoNessuna valutazione finora
- Acid Fast StainingDocumento4 pagineAcid Fast Stainingchaudhary TahiraliNessuna valutazione finora
- Pathogenesis of Bacterial InfectionDocumento6 paginePathogenesis of Bacterial InfectionStephen Jao Ayala UjanoNessuna valutazione finora
- UrineDocumento52 pagineUrineMohammed Tahoun100% (1)
- Specimen Collection & Transport GuideDocumento168 pagineSpecimen Collection & Transport Guidesinghranjanr5748100% (1)
- Appropriate Clinical Specimens Collection and Transport For Diagnostic VirologyDocumento48 pagineAppropriate Clinical Specimens Collection and Transport For Diagnostic Virologylong thomNessuna valutazione finora
- GPHT1 Lab 3 Shift Reviewer Pap's Smear Prepared By: C Papanicolau'S MethodDocumento5 pagineGPHT1 Lab 3 Shift Reviewer Pap's Smear Prepared By: C Papanicolau'S MethodCatherine MerillenoNessuna valutazione finora
- Mycobacteria: Nocardia, Rhodococcus, Tsukamurella and GordoniaDocumento7 pagineMycobacteria: Nocardia, Rhodococcus, Tsukamurella and Gordonia20C – Gorospe, Rhai Chezka V.Nessuna valutazione finora
- 11 PathologyDocumento26 pagine11 PathologyRocky BullNessuna valutazione finora
- His To PathologyDocumento2 pagineHis To PathologypixiedustNessuna valutazione finora
- Parasitology ProtozoansDocumento13 pagineParasitology ProtozoansMay LacdaoNessuna valutazione finora
- Hematoxylin and Eosin StainingDocumento6 pagineHematoxylin and Eosin StainingRaja Sharma100% (1)
- Histochemistry Chapter 5Documento48 pagineHistochemistry Chapter 5Zelalem DejazmachNessuna valutazione finora
- My Co BacteriumDocumento15 pagineMy Co BacteriumPatrickNessuna valutazione finora
- Rickettsia eDocumento10 pagineRickettsia eDeep Iyaz100% (1)
- Sample CollectionDocumento20 pagineSample Collectionmaan khanNessuna valutazione finora
- Medical LaboratoryDocumento5 pagineMedical LaboratoryvictorasaurasNessuna valutazione finora
- CSF and Other Body FluidsDocumento9 pagineCSF and Other Body FluidsJobelle0% (1)
- Respiratory Cytology: DR Mohammed Shahin, JR (Academic), Dept of Pathology & Lab Medicine, AIIMS BhubaneswarDocumento62 pagineRespiratory Cytology: DR Mohammed Shahin, JR (Academic), Dept of Pathology & Lab Medicine, AIIMS BhubaneswarShruthi N.RNessuna valutazione finora
- Stool ExaminationDocumento38 pagineStool ExaminationARIF AHAMMED P100% (1)
- Pap StainingDocumento2 paginePap StainingDrManish KumarNessuna valutazione finora
- AUBF Online Quiz SET ADocumento2 pagineAUBF Online Quiz SET AEricka GenoveNessuna valutazione finora
- Hacek GroupDocumento24 pagineHacek GroupHanna Isabela Bausin0% (1)
- Bacteriology Handouts From Sir PalmaresDocumento30 pagineBacteriology Handouts From Sir PalmaresTin BabistaNessuna valutazione finora
- Rheumatoid Factor Latex Test PartolanDocumento15 pagineRheumatoid Factor Latex Test Partolanchocoholic potchiNessuna valutazione finora
- Gram Negative Rods of Enteric TractDocumento2 pagineGram Negative Rods of Enteric TractJohn TerryNessuna valutazione finora
- Hypersensitivity ReactionsDocumento25 pagineHypersensitivity Reactionsbpt2100% (3)
- Bacteriology Laboratory OrganizationDocumento65 pagineBacteriology Laboratory Organizationtummalapalli venkateswara rao100% (1)
- Elisa & RiaDocumento4 pagineElisa & Riadihajum3Nessuna valutazione finora
- Blood Specimen Collection: Elaine M. KeohaneDocumento15 pagineBlood Specimen Collection: Elaine M. KeohanePrince Guevara100% (1)
- Opportunistic MycosesDocumento36 pagineOpportunistic MycosesTrinain ChakravartiNessuna valutazione finora
- Histopath Lec (Module 1) : Iintroduction To PathologyDocumento17 pagineHistopath Lec (Module 1) : Iintroduction To PathologyAngela ReyesNessuna valutazione finora
- 4th Shifting Micro Lab ReviewerDocumento154 pagine4th Shifting Micro Lab ReviewerJade MonrealNessuna valutazione finora
- Fixation & FixativesDocumento64 pagineFixation & FixativesMadhura Shekatkar100% (1)
- 3 SEMR421 Bacteriology Part 3Documento14 pagine3 SEMR421 Bacteriology Part 3Micah Daniel TapiaNessuna valutazione finora
- Tissue NematodesDocumento33 pagineTissue NematodesJessiNessuna valutazione finora
- Haemophilus SPPDocumento109 pagineHaemophilus SPPJamie CañebaNessuna valutazione finora
- MicroparasitologyDocumento28 pagineMicroparasitologyMj BrionesNessuna valutazione finora
- Antimicrobial Susceptibility TestDocumento4 pagineAntimicrobial Susceptibility TestMATTHEW EARL MALUMAY100% (1)
- Mycology: Rochelle D. Darlucio-Yabut, RMT, MPH Our Lady of Fatima University College of Medical Laboratory ScienceDocumento59 pagineMycology: Rochelle D. Darlucio-Yabut, RMT, MPH Our Lady of Fatima University College of Medical Laboratory ScienceClaire GonoNessuna valutazione finora
- Histopathologic Technique: Two KeyplayersDocumento19 pagineHistopathologic Technique: Two KeyplayersHadjar MitmugNessuna valutazione finora
- DehydrationDocumento14 pagineDehydrationChelly JimenoNessuna valutazione finora
- Antigen and Its PropertiesDocumento20 pagineAntigen and Its Propertiestusharpremin92% (12)
- External Examination at AutopsyDocumento87 pagineExternal Examination at AutopsyDr. Ashish JawarkarNessuna valutazione finora
- StreptococciDocumento91 pagineStreptococciDr. Ashish JawarkarNessuna valutazione finora
- Robbins Chapter 1 Cell As A Unit of Health and DiseaseDocumento46 pagineRobbins Chapter 1 Cell As A Unit of Health and DiseaseDr. Ashish Jawarkar0% (1)
- Needle Sticks Sharps Injuries: FactsDocumento31 pagineNeedle Sticks Sharps Injuries: FactsDr. Ashish Jawarkar67% (3)
- Anti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDocumento41 pagineAnti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarNessuna valutazione finora
- Control of Aerosol Transmitted DiseasesDocumento45 pagineControl of Aerosol Transmitted DiseasesDr. Ashish JawarkarNessuna valutazione finora
- Control of Microbial Growth: Dr. Ashish Jawarkar Pathologist Parul Sevashram HospitalDocumento38 pagineControl of Microbial Growth: Dr. Ashish Jawarkar Pathologist Parul Sevashram HospitalDr. Ashish JawarkarNessuna valutazione finora
- Biomedical Waste ManagementDocumento57 pagineBiomedical Waste ManagementDr. Ashish JawarkarNessuna valutazione finora
- Systemic Microbiology: BacteriologyDocumento42 pagineSystemic Microbiology: BacteriologyDr. Ashish JawarkarNessuna valutazione finora
- Sickle Cell AnemiaDocumento13 pagineSickle Cell AnemiaDr. Ashish JawarkarNessuna valutazione finora
- Laboratory Approach To AnemiasDocumento23 pagineLaboratory Approach To AnemiasDr. Ashish JawarkarNessuna valutazione finora
- Semen Analysis (WHO 2010)Documento14 pagineSemen Analysis (WHO 2010)Dr. Ashish Jawarkar100% (1)
- Nosocomial InfectionDocumento31 pagineNosocomial InfectionDr. Ashish Jawarkar0% (1)
- Renal Function TestsDocumento26 pagineRenal Function TestsDr. Ashish Jawarkar100% (1)
- Basics of Microscopy and StainingDocumento29 pagineBasics of Microscopy and StainingDr. Ashish JawarkarNessuna valutazione finora
- Microscopy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDocumento21 pagineMicroscopy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarNessuna valutazione finora
- Bacteria: Morphology and ClassificationDocumento44 pagineBacteria: Morphology and ClassificationDr. Ashish JawarkarNessuna valutazione finora
- Liver Function TestsDocumento28 pagineLiver Function TestsDr. Ashish Jawarkar100% (2)
- NecrosisDocumento6 pagineNecrosisDr. Ashish JawarkarNessuna valutazione finora
- 2009 Fee ScheduleDocumento1.123 pagine2009 Fee ScheduleNicole HillNessuna valutazione finora
- Ispad 2014Documento290 pagineIspad 2014Sheyla Alegre Pariona100% (1)
- Classification of Drugs Are: Hepatoprotective Drugs E.g.: Silymarin Antibiotics E.G.Documento2 pagineClassification of Drugs Are: Hepatoprotective Drugs E.g.: Silymarin Antibiotics E.G.Navya Sara SanthoshNessuna valutazione finora
- OCTA InflammatoryEyediseaseSrivastavaDocumento24 pagineOCTA InflammatoryEyediseaseSrivastavaPriyanka DocNessuna valutazione finora
- Dalay Panishment of FormalinDocumento4 pagineDalay Panishment of Formalinmutiara defiskaNessuna valutazione finora
- 2024 04 04 SSCP Oversight EC Letter To Daszak 6c867682d6Documento12 pagine2024 04 04 SSCP Oversight EC Letter To Daszak 6c867682d6Jennifer Van LaarNessuna valutazione finora
- Biocontrol Potential of Trichoderma Spp. Against Fusarium Oxysporum in Solanum Lycopersicum LDocumento6 pagineBiocontrol Potential of Trichoderma Spp. Against Fusarium Oxysporum in Solanum Lycopersicum LMartinius TinNessuna valutazione finora
- M010-MSI-HSE-00-PLN-02007 - Rev5 Heat Stress & Summer Working Plan PDFDocumento66 pagineM010-MSI-HSE-00-PLN-02007 - Rev5 Heat Stress & Summer Working Plan PDFEldhose VargheseNessuna valutazione finora
- PEMF Therapy Controls Physical Effects of StressDocumento2 paginePEMF Therapy Controls Physical Effects of StressAndreas LooseNessuna valutazione finora
- Answer: 1Documento4 pagineAnswer: 1Jeffrey ViernesNessuna valutazione finora
- IV. Recognizing National Issues and Concern - E-Substance Abuse EducationDocumento9 pagineIV. Recognizing National Issues and Concern - E-Substance Abuse EducationMicsjadeCastillo0% (1)
- RAD RLE MCN 6 Case StudyDocumento9 pagineRAD RLE MCN 6 Case StudyCathleen Nasis Forrosuelo100% (2)
- Graves DiseaseDocumento13 pagineGraves DiseaseGerald John PazNessuna valutazione finora
- Performing Chest PhysiotherapyDocumento14 paginePerforming Chest PhysiotherapyDivya Chauhan100% (1)
- Bio Toxin PathwayDocumento1 paginaBio Toxin PathwayJackie De Vries100% (1)
- Grade 8 Health Summative Test Alcohol and CigaretteDocumento3 pagineGrade 8 Health Summative Test Alcohol and CigaretteAlbert Ian Casuga100% (1)
- CockroachesDocumento12 pagineCockroachesuma_mounaNessuna valutazione finora
- Bio TherapyDocumento18 pagineBio TherapyChino RamirezNessuna valutazione finora
- Australian Biology Olympiad 2009Documento41 pagineAustralian Biology Olympiad 2009Science Olympiad Blog100% (1)
- 8-Drugs Used in Anxiety and Panic Disprder (Edited)Documento11 pagine8-Drugs Used in Anxiety and Panic Disprder (Edited)ana01210761809Nessuna valutazione finora
- (NH4) 2co3Documento5 pagine(NH4) 2co3MuhafiNessuna valutazione finora
- OSPE DU MedicineDocumento101 pagineOSPE DU MedicinesaifNessuna valutazione finora
- Dispensing, Incompatibilities, and Adverse Drug Reactions Answer Key-PINK PACOPDocumento78 pagineDispensing, Incompatibilities, and Adverse Drug Reactions Answer Key-PINK PACOPBilly Vince AlquinoNessuna valutazione finora
- GI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyDocumento11 pagineGI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyTony LeeNessuna valutazione finora
- Nursing Care For ElderlyDocumento7 pagineNursing Care For ElderlyNeenu Rajput83% (12)
- Legal Aid Society Complaint Re Homeless YouthDocumento65 pagineLegal Aid Society Complaint Re Homeless YouthPaul SchindlerNessuna valutazione finora
- Herniated Nucleus Pulposus (HNP)Documento21 pagineHerniated Nucleus Pulposus (HNP)Kaye100% (1)
- South Carolina Maternal Morbidity and Mortality Review CommitteeDocumento4 pagineSouth Carolina Maternal Morbidity and Mortality Review CommitteeABC15 NewsNessuna valutazione finora
- Chorti DictionaryDocumento285 pagineChorti DictionaryLuis Bedoya100% (1)
- Persuasive Speech Outline - Marijauna FinalDocumento4 paginePersuasive Speech Outline - Marijauna Finalapi-34805003388% (17)