Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Rovamycin 3868 DR 1256036243912
Caricato da
Ahmed El AlfyTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Rovamycin 3868 DR 1256036243912
Caricato da
Ahmed El AlfyCopyright:
Formati disponibili
09 "
Rovamycin - SUMMARY OF PRODUCT CHARACTERISTICS
1. TRADE NAME OF THE MEDICINAL PRODUCT ROVAMYCIN 1.5 M.I.U film-coated tablet 2. QUALITATIVE AND QUANTITATIVE COMPOSITION
Active ingredient: each tablet contains 1.5 MIU spiramycin. Excipients: Magnesium stearate; Pregelatinized corn starch; Hydroxypropylcellulose; Croscarmellose sodium; Colloidal anhydrous silica; Microcrystalline cellulose; Methylhydroxypropylcellulose; Polyethylene glycol 6000; Titanium dioxide.
3.
PHARMACEUTICAL FORM Film-coated tablet
4.
CLINICAL PARTICULARS
Therapeutic indications Respiratory tract infections, infections caused by clamydia, cryptosporidiosis pregnancy toxoplasmosis. Posology and Method of Administration Posology In patients with normal renal function: Routine dose: Adults: 6 to 9 million IU/24 hours, i.e. 4 to 6 tablets per day in 2 to 3 intakes. Children: 1.5 to 3 million IU per 10 kg of body weight per day in 2 to 3 intakes. Sore throats should be treated for 10 days. Meningococcal meningitis prophylaxis Adults: 3 million IU/12 hours. Children: 75 000 IU/kg/12 hours. for 5 days. In patients with renal insufficiency: No dose adjustment is necessary.
Method of Administration
Tablets should be swallowed whole with a glass of water. Contraindications Hypersensitivity to spiramycin , other macrolids or any of the excipients It is not recommended for breast-feeding mothers (see 4.6 Pregnancy and Lactation).
Warnings and Precautions For Use If, at the start of treatment, patients experience generalized erythema and pustules, accompanied by fever, acute generalized exanthematous pustulosis should be suspected (see Section 4.8 Undesirable effects); if such a reaction occurs, treatment must be discontinued and any further administration of spiramycin alone or in combination is contraindicated.
Administration of tablets is contraindicated in children under 6 years of age because of the risk of choking.
Since the compound is not excreted via the kidney, there is no need to adjust dosage in patients with renal insufficiency. Very rare cases of hemolytic anemia have been reported in patients with glucose-6phosphate-dehydrogenase deficiency. Spriamycin is therefore not recommended for such patients. Interactions with other medicinal products and other forms of interaction
Interactions requiring precautions for use
+Levodopa (associated with carbidopa): inhibition of carbidopa absorption with decreased plasma concentrations of levodopa. Clinical monitoring and possible adjustment of levodopa dosage. Specific problems with INR imbalance Many cases of increased activity in oral anticoagulants have been reported for patients taking antibiotics. The marked infectious or inflammatory picture, age and general condition of the patient would appear to be risk factors. Under these circumstances, it is difficult to distinguish between the effect of the infection and its treatment in the onset of INR imbalance. However, certain classes of antibiotics are more involved; principally fluoroquinolones, macrolides, cyclines, cotrimoxazole and certain cephalosporins. Pregnancy and lactation
Pregnancy
Spiramycin can be used during pregnancy if necessary. Extensive use of spiramycin during pregnancy has shown no evidence of malformation or fetotoxicity to date.
Lactation
Spiramycin Is excreted into breast milk. Gastrointestinal disorders in neonates have been reported. Consequently, breast-feeding is not recommended to women taking spiramycin. Effects on ability to drive and use machines Not relevant. Undesirable effects
Gastrointestinal system: Skin and appendages:
. gastralgia, nausea, vomiting, diarrhea and, very rarely, pseudo-membranous colitis. - rash, urticaria, pruritis. - very rarely Quinckes edema, anaphylactic shock.
3
- Very rarely, acute generalized exanthematous pustulosis (see Section 4.4 Special warnings and special precautions for use)
Central and peripheral nervous system:
. occasional and transient paresthesia.
Hepatic signs:
. very rare abnormal results to liver function tests.
Blood cell line:
. very rare cases of hemolytic anemia have been reported (see 4.4. Warnings and special precautions for use). 4.9 Overdose There is no known toxic dose for spiramycin. Expected signs of overdose are gastrointestinal: nausea, vomiting, diarrhea. Lengthening of the QT interval, resolving on discontinuation of treatment, has been observed in neonates treated with high doses of spiramycin, and also after IV administration to people at risk of QT lengthening. In the event of overdose, the QT interval should be determined, especially where other risk factors are present (hypokalemia, congenital lengthening of QT interval, other medicinal products lengthening QT interval and/or inducing torsades de pointes). There is no specific antidote. Symptomatic treatment is recommended. 5. PHARMACOLOGICAL PROPERTIES Pharmacodynamic properties Pharmacotherapeutic class: SYSTEMIC ANTIBACTERIAL AGENT ATC code: J01FA02 Antibacterial antibiotic belonging to the macrolides family. ANTIBACTERIAL ACTIVITY SPECTRUM Critical concentrations differentiate sensitive from moderate strains, and both from resistant ones: S < 1 mg/l and R > 4 mg/l For certain species, the prevalence of acquired resistance may vary according to place and time. It is useful, therefore, to have information on the prevalence of local resistance, particularly when treating severe infections. These data can only provide an indication of the sensitivity of a bacterial strain to this antibiotic. When the variability in the prevalence of resistance for a given species of bacteria is known in France, it is shown in the table below:
Categories SENSITIVE SPECIES
Frequency of acquired resistance in France (> 10%) (extreme values)
Bacillus cereus Corynebacterium diphtheriae
Enterococci
Gram positive aerobic organisms 50% 70% 70 80% 30 40% 35 70% 16-31%
Rhodococcus equi Methicillin-sensitive staphylococcus Methicillin-resistant staphylococcus* Streptococcus B Streptococcus (not classifiable) Streptococcus pneumoniae Streptococcus pyogenes Bordetella pertussis Branhamella catarrhalis Campylobacter Legionella Moraxella
Gram negative aerobic organisms
Anaerobic organisms
Actinomyces Bacteroides Eubacterium Mobilincus Peptostreptococcus Porphyromonas Prevotella Propionibacterium acnes
30 60% 30 40%
Categories
Others Borrelia burgdorferi Chlamydia Coxiella
Leptospires
Frequency of acquired resistance in France (> 10%) (extreme values)
Mycoplasma pneumoniae Treponema pallidum
MODERATELY SENSITIVE SPECIES (of intermediary sensitivity in vitro)
Neisseria gonorrhoeae
Gram negative aerobic organisms
Anaerobic organisms
Clostridium perfringens
Others
Ureaplasma urealyticum
RESISTANT SPECIES Gram positive aerobic organisms
Corynebacterium jeikeium Nocardia asteroides Acinetobacter
Gram negative aerobic organisms
Haemophilus Pseudomonas
Enterobacteria
Anaerobic organisms
Fusobacterium
Others
Mycoplasma hominis
Spiramycin is active against Toxoplasma gondii in vitro and in vivo. * The frequency of acquired resistance to methicillin is between about 30 50 % for all staphylococci and is usually found in the hospital environment. Pharmacokinetic properties
Absorption
Spiramycin is rapidly but incompletely absorbed and is not modified by food intake.
Distribution
After oral administration of 6 million IU of spiramycin, the peak serum concentration is 3.3 g/ml. Plasma half-life is about 8 hours. Spiramycin does not enter the CSF and is excreted into breast milk. Plasma protein binding is low (10%).
Tissue and saliva diffusion is excellent (lungs: 20-60 g/g, tonsils: 20-80 g/g, infected sinuses: 75-110 g/g, bones: 5-100 g/g). Ten days after the end of treatment, there is 5 to 7 g/g of active substance in the spleen, liver and kidneys. Macrolides penetrate and accumulate in phagocytes (polynuclear neutrophils, monocytes, peritoneal and alveolar macrophages). Intra-phagocyte concentrations are high in man. These properties explain macrolides activity against intra-cellular bacteria.
Metabolism
Spiramycin is metabolised in the liver with the formation of chemically unknown but active metabolites.
Excretion
-
Preclinical safety data
urine: 10% of the administered dose. extensive biliary excretion: concentrations 15 to 40 times higher than serum concentrations. small amounts of spiramycin are present in feces.
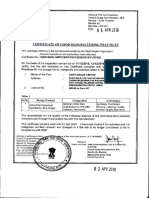
Not relevant. MANUFACTURER Famar Lyon, France for Aventis, France Marketing Authorization Holder sanofi-aventis Israel ltd P.O.box 8090 Netanya 42504 Registration number: 465923868
Potrebbero piacerti anche
- Satorius A210P Balance Users ManualDocumento18 pagineSatorius A210P Balance Users ManualJim McMicanNessuna valutazione finora
- In-Process Testing of Infusions: Novamed Pharmaceutical Quality Control Department Standard Operating ProcedureDocumento5 pagineIn-Process Testing of Infusions: Novamed Pharmaceutical Quality Control Department Standard Operating Procedurenaeem186Nessuna valutazione finora
- Alusim SuspensionDocumento5 pagineAlusim SuspensionAhmad HussainNessuna valutazione finora
- VeerDocumento19 pagineVeerRam KprNessuna valutazione finora
- Microbiological Best Lab Practices & Environmental MonitoringDocumento26 pagineMicrobiological Best Lab Practices & Environmental MonitoringNurul Hardiyanthi SadikinNessuna valutazione finora
- Paracetamol and Ibuprofen Suspension Analytical Method ValidationDocumento3 pagineParacetamol and Ibuprofen Suspension Analytical Method ValidationAmik TuladharNessuna valutazione finora
- Revital Heathcare (Epz) Limited Quality Control Department Sterility Test Raw Data SheetDocumento2 pagineRevital Heathcare (Epz) Limited Quality Control Department Sterility Test Raw Data SheetMusyoka UrbanusNessuna valutazione finora
- Annexure - II Product DevelopmentDocumento50 pagineAnnexure - II Product DevelopmentLife PearlNessuna valutazione finora
- Preparation of Culture Suspension SOPDocumento9 paginePreparation of Culture Suspension SOPMichaelNessuna valutazione finora
- 001 AbbrevationsDocumento86 pagine001 AbbrevationssreeniNessuna valutazione finora
- Pharmacogenomics: Learning ObjectivesDocumento16 paginePharmacogenomics: Learning ObjectivesJamilNessuna valutazione finora
- STP of Ethifen SyrupDocumento5 pagineSTP of Ethifen SyrupBejoy KarimNessuna valutazione finora
- Omcl Management of Environmental Conditions Paphomcl1686r6Documento8 pagineOmcl Management of Environmental Conditions Paphomcl1686r6Hans LeupoldNessuna valutazione finora
- SOP For Automatic Batch Printing MachineDocumento5 pagineSOP For Automatic Batch Printing MachineAshok KumarNessuna valutazione finora
- Catalogue SOP OrthomedDocumento58 pagineCatalogue SOP OrthomedInstrulife OostkampNessuna valutazione finora
- Sop For Bio-BurdenDocumento5 pagineSop For Bio-BurdenMusyoka UrbanusNessuna valutazione finora
- Meclizine HCLDocumento10 pagineMeclizine HCLChEng_Nessuna valutazione finora
- Testing Procedure of Caps: Ferozsons Laboratories Limited Work InstructionsDocumento8 pagineTesting Procedure of Caps: Ferozsons Laboratories Limited Work InstructionsaKureishiNessuna valutazione finora
- Spec-Shilajit Extract-50%Documento1 paginaSpec-Shilajit Extract-50%marketing splsgroupNessuna valutazione finora
- Magnehelic Gauge CalibrationDocumento7 pagineMagnehelic Gauge CalibrationgrajukankayyaNessuna valutazione finora
- 2.25 PA CTD Jun11 v3Documento38 pagine2.25 PA CTD Jun11 v3Snezana Smileva LazovaNessuna valutazione finora
- Report ErythromycinDocumento26 pagineReport ErythromycinKraken UrNessuna valutazione finora
- Assay Determination: General IndexDocumento10 pagineAssay Determination: General IndexDavid SanabriaNessuna valutazione finora
- WHO Certificate E120 2019Documento4 pagineWHO Certificate E120 2019Risen ChemicalsNessuna valutazione finora
- Cilastati Imipenem Drug InfoDocumento19 pagineCilastati Imipenem Drug InfoCosmina GeorgianaNessuna valutazione finora
- Salom Pharmacy LTD: Quality Control Laboratory SPL-SOP-QC-DISS-001 Operation of Dissolution Rate ApparatusDocumento2 pagineSalom Pharmacy LTD: Quality Control Laboratory SPL-SOP-QC-DISS-001 Operation of Dissolution Rate ApparatusPaolo Peps100% (1)
- Operational Manual: DGYF-S500 Type Electromagnet Induction Sealing MachineDocumento8 pagineOperational Manual: DGYF-S500 Type Electromagnet Induction Sealing MachineHaroldNessuna valutazione finora
- Bromelain MonographDocumento5 pagineBromelain MonographLizbeth Aura CebrianNessuna valutazione finora
- Sanfuliq PVP RegistrasiDocumento25 pagineSanfuliq PVP RegistrasiFajarRachmadiNessuna valutazione finora
- The Sex Influence On PharmacokineticDocumento106 pagineThe Sex Influence On PharmacokineticIuliaCNessuna valutazione finora
- Validation of Chromatographic Methods of AnalysisDocumento17 pagineValidation of Chromatographic Methods of AnalysisRoberto TorrezNessuna valutazione finora
- Enumeration of Coagulase-Positive StaphylococciDocumento23 pagineEnumeration of Coagulase-Positive Staphylococcianil_hod8353Nessuna valutazione finora
- Microbiological Media Preparation SOPDocumento4 pagineMicrobiological Media Preparation SOPAzura Salsabila100% (1)
- Sop For Vitamin K3Documento3 pagineSop For Vitamin K3Ganesh KashinathNessuna valutazione finora
- Development and Evaluation of New DrugsDocumento26 pagineDevelopment and Evaluation of New DrugsAncient Ethiopia TigrayNessuna valutazione finora
- Vostem REPORT RegistDocumento22 pagineVostem REPORT RegistFajarRachmadiNessuna valutazione finora
- Method Development For The Analysis of Anthocyanins in AroniDocumento45 pagineMethod Development For The Analysis of Anthocyanins in Aronimarkiza07Nessuna valutazione finora
- 08 SOP Tatal Microbial CountDocumento5 pagine08 SOP Tatal Microbial CountNoor JavedNessuna valutazione finora
- Amendment 1: Replacement of 3Kl Uf Storage Tank & Installation of New 500 Ltr. Brine TankDocumento8 pagineAmendment 1: Replacement of 3Kl Uf Storage Tank & Installation of New 500 Ltr. Brine TankprakashNessuna valutazione finora
- Calcium chloride dihydrate tests and propertiesDocumento2 pagineCalcium chloride dihydrate tests and propertiesMulayam Singh YadavNessuna valutazione finora
- Alternative Methods for Real-Time Microbiological Quality ControlDocumento10 pagineAlternative Methods for Real-Time Microbiological Quality ControlLEPESANTNessuna valutazione finora
- Tamsulosina + DutasterideDocumento13 pagineTamsulosina + DutasterideJavier Hernandez100% (1)
- Operating Procedure Fume HoodDocumento4 pagineOperating Procedure Fume HoodBejoy KarimNessuna valutazione finora
- 01 Disintegration Test For Tablets and CapsulesDocumento30 pagine01 Disintegration Test For Tablets and CapsulesmefroNessuna valutazione finora
- Sls-Mic 032Documento7 pagineSls-Mic 032vpnarashimmanNessuna valutazione finora
- Certificate of Quality: Cayman Pharma S.R.O. Ul. Práce 657, 277 11 NERATOVICE Czech Republic Tel. +420 315 665 360Documento3 pagineCertificate of Quality: Cayman Pharma S.R.O. Ul. Práce 657, 277 11 NERATOVICE Czech Republic Tel. +420 315 665 360amin138irNessuna valutazione finora
- Assay and Dissolution EtoricoxibDocumento8 pagineAssay and Dissolution Etoricoxibsesilia dyah novitrianiNessuna valutazione finora
- Pharmaceutical Country Profile PeruDocumento147 paginePharmaceutical Country Profile PeruNethcy JapNessuna valutazione finora
- XXXX Pharma Stability RegisterDocumento1 paginaXXXX Pharma Stability Registerkanji63Nessuna valutazione finora
- RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES CLEANING VALIDATIONDocumento10 pagineRAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES CLEANING VALIDATIONkumar_chemicalNessuna valutazione finora
- Ethical Drugs LTD.: Siddhirganj, NarayanganjDocumento10 pagineEthical Drugs LTD.: Siddhirganj, NarayanganjBejoy Karim100% (1)
- Analytical Method Development and Validation of Minoxidil in Pharmaceutical Dosage Forms by UV SpectrophotometryDocumento4 pagineAnalytical Method Development and Validation of Minoxidil in Pharmaceutical Dosage Forms by UV SpectrophotometryBil Sonador100% (1)
- Understanding API Assay, Potency, and PurityDocumento17 pagineUnderstanding API Assay, Potency, and PurityAngel FloresNessuna valutazione finora
- Microemulsion Process For The Preparation of Sucrose Esters Osipow1967Documento3 pagineMicroemulsion Process For The Preparation of Sucrose Esters Osipow1967Alfonso Dominguez GonzalezNessuna valutazione finora
- Certificate of Analysis: Apigenin Biochemika 10798 Fluka C15H10O5 270.24 520-36-5Documento1 paginaCertificate of Analysis: Apigenin Biochemika 10798 Fluka C15H10O5 270.24 520-36-5Danang ArdiyantoNessuna valutazione finora
- European Journal of Biomedical AND Pharmaceutical SciencesDocumento14 pagineEuropean Journal of Biomedical AND Pharmaceutical SciencesSACHIN BHASKAR NARKHEDENessuna valutazione finora
- Cleaning and disinfection of food factories: a practical guideDa EverandCleaning and disinfection of food factories: a practical guideNessuna valutazione finora
- ICH Quality Guidelines: An Implementation GuideDa EverandICH Quality Guidelines: An Implementation GuideAndrew TeasdaleNessuna valutazione finora
- Mupirocin Cream Reduces Bacterial InfectionsDocumento7 pagineMupirocin Cream Reduces Bacterial InfectionsVinay KumarNessuna valutazione finora
- ClinicianDocumento5 pagineClinicianAhmed El AlfyNessuna valutazione finora
- Drug Dosage Calculation PacketDocumento8 pagineDrug Dosage Calculation PacketAhmed El AlfyNessuna valutazione finora
- GcppextrDocumento7 pagineGcppextrAhmed El AlfyNessuna valutazione finora
- Foundations of Taoist PracticeDocumento17 pagineFoundations of Taoist PracticeAlesha Rose100% (11)
- The Mech of AspirinDocumento4 pagineThe Mech of AspirinsabrahimaNessuna valutazione finora
- 1 The Art of Female EjaculationDocumento8 pagine1 The Art of Female EjaculationSzabo Attila100% (2)
- Cardiology 101 150Documento31 pagineCardiology 101 150Ahmed El AlfyNessuna valutazione finora
- 1311Documento6 pagine1311Ahmed El AlfyNessuna valutazione finora
- AspirinDocumento34 pagineAspirinAhmed El AlfyNessuna valutazione finora
- ParofenDocumento3 pagineParofenAhmed El AlfyNessuna valutazione finora
- NEUROLOGY For MRCP Part 1Documento14 pagineNEUROLOGY For MRCP Part 1Appu JainNessuna valutazione finora
- DermatologyDocumento48 pagineDermatologyAhmed El AlfyNessuna valutazione finora
- Eighth Book of MosesDocumento29 pagineEighth Book of MosesCorneliu Meciu100% (4)
- TestosteroneDocumento113 pagineTestosteroneAhmed El AlfyNessuna valutazione finora
- Cardiology 101 150Documento31 pagineCardiology 101 150Ahmed El AlfyNessuna valutazione finora
- Amino Acids Injection Improves Hepatic EncephalopathyDocumento12 pagineAmino Acids Injection Improves Hepatic EncephalopathyAhmed El AlfyNessuna valutazione finora
- Inderal CmiDocumento4 pagineInderal CmiAhmed El AlfyNessuna valutazione finora
- PHYS THER-1995-Ward-526-38Documento15 paginePHYS THER-1995-Ward-526-38Ahmed El AlfyNessuna valutazione finora
- ParofenDocumento3 pagineParofenAhmed El AlfyNessuna valutazione finora
- Amino Acids Injection Improves Hepatic EncephalopathyDocumento12 pagineAmino Acids Injection Improves Hepatic EncephalopathyAhmed El AlfyNessuna valutazione finora
- GeneticsDocumento45 pagineGeneticsAhmed El AlfyNessuna valutazione finora
- 1311Documento6 pagine1311Ahmed El AlfyNessuna valutazione finora
- DermatologyDocumento48 pagineDermatologyAhmed El AlfyNessuna valutazione finora
- DermatologyDocumento48 pagineDermatologyAhmed El AlfyNessuna valutazione finora
- Pharmacology 251 307Documento33 paginePharmacology 251 307Ahmed El AlfyNessuna valutazione finora
- Clinical Haematology 201 256Documento38 pagineClinical Haematology 201 256Ahmed El AlfyNessuna valutazione finora
- Cardiology 101 150Documento31 pagineCardiology 101 150Ahmed El AlfyNessuna valutazione finora
- Endocrinology 101 150Documento29 pagineEndocrinology 101 150Ahmed El AlfyNessuna valutazione finora
- Cardiology 151 200Documento34 pagineCardiology 151 200Ahmed El AlfyNessuna valutazione finora
- Product and Company Identification: Safety Data SheetDocumento7 pagineProduct and Company Identification: Safety Data SheetZirve PolimerNessuna valutazione finora
- RadioisotopesDocumento28 pagineRadioisotopessivagurunathan.P100% (3)
- Method Statement FOR Waste Polymer Slurry Disposal: PT Bauer Pratama IndonesiaDocumento4 pagineMethod Statement FOR Waste Polymer Slurry Disposal: PT Bauer Pratama IndonesiaFendi Rang TigorNessuna valutazione finora
- Galvanic Series: Why Metals Corrode?Documento7 pagineGalvanic Series: Why Metals Corrode?Rey Francis FamulaganNessuna valutazione finora
- Astm D1785-15Documento11 pagineAstm D1785-15david franco0% (1)
- 20b. Global S CycleDocumento15 pagine20b. Global S CyclerossydaNessuna valutazione finora
- Big Batch Soap MakingDocumento24 pagineBig Batch Soap MakingAnonymous Vu1R35s4WZ100% (2)
- 11th Chemistry EM - Public Exam 2022 - Model Question Paper - English Medium PDF DownloadDocumento3 pagine11th Chemistry EM - Public Exam 2022 - Model Question Paper - English Medium PDF DownloadAshwini Shankar KumarNessuna valutazione finora
- Process Integration Using Pinch Analysis: A Cement Industry Case StudyDocumento4 pagineProcess Integration Using Pinch Analysis: A Cement Industry Case StudyReggie DueñasNessuna valutazione finora
- Selective MediaDocumento10 pagineSelective Mediaprincess_likemist4Nessuna valutazione finora
- TubingDocumento6 pagineTubingkevin wongNessuna valutazione finora
- A STUDY ON THE ECOFRIENDLY DYES EXTRACTED FROM THREE DIFFERENT SPECIES OF Curcuma LDocumento3 pagineA STUDY ON THE ECOFRIENDLY DYES EXTRACTED FROM THREE DIFFERENT SPECIES OF Curcuma Lanon_285184956Nessuna valutazione finora
- C.02 - Gas-Freeing and Cleaning of TanksDocumento7 pagineC.02 - Gas-Freeing and Cleaning of TanksmkkamarajNessuna valutazione finora
- Syntheses of Soap and DetergentDocumento4 pagineSyntheses of Soap and DetergentChin Castro Zabat100% (2)
- FINALSDocumento8 pagineFINALSSeenpai23Nessuna valutazione finora
- Land Deep Production Casings in Menengai Geothermal FieldDocumento30 pagineLand Deep Production Casings in Menengai Geothermal FieldShafeeq ChappuNessuna valutazione finora
- Food Preservatives and Their Harmful EffDocumento2 pagineFood Preservatives and Their Harmful EffJo ShuNessuna valutazione finora
- Unit 1 - Construction Materials - WWW - Rgpvnotes.inDocumento21 pagineUnit 1 - Construction Materials - WWW - Rgpvnotes.inmadhavi likharNessuna valutazione finora
- MCQ IjsoDocumento20 pagineMCQ IjsommhabgNessuna valutazione finora
- Organic Name Reactions GuideDocumento12 pagineOrganic Name Reactions GuidechinmayaNessuna valutazione finora
- Imp of MicronutrientsDocumento5 pagineImp of MicronutrientsDanish S MehtaNessuna valutazione finora
- Instruction Manual Instruction Manual: HDI 2D949-80Documento30 pagineInstruction Manual Instruction Manual: HDI 2D949-80GeorgianaNessuna valutazione finora
- Bio HGHDocumento19 pagineBio HGHapi-240332064Nessuna valutazione finora
- Solvent Extraction Principles and Practice 2nd Ed - Jan Rydberg Et Al. (Marcel Dekker, 2004)Documento724 pagineSolvent Extraction Principles and Practice 2nd Ed - Jan Rydberg Et Al. (Marcel Dekker, 2004)Milena Katarina Stojiljkovic100% (6)
- DTS Thoracic R4Documento2 pagineDTS Thoracic R4Arief FaqihNessuna valutazione finora
- D94 PDFDocumento8 pagineD94 PDFJuan Diego ArizabalNessuna valutazione finora
- NanotechnologyDocumento28 pagineNanotechnologyCordelia Marisse ReyesNessuna valutazione finora
- Astm 1351 1 REPLICADocumento6 pagineAstm 1351 1 REPLICAmaheshNessuna valutazione finora
- Schunk Carbon Technology Sealring Bearing SiSiC SSiC EN PDFDocumento2 pagineSchunk Carbon Technology Sealring Bearing SiSiC SSiC EN PDFMUHAMMAD ASYRAAF BIN ANUARNessuna valutazione finora