Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Perforantes para Poland
Caricato da
Angela GarciaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Perforantes para Poland
Caricato da
Angela GarciaCopyright:
Formati disponibili
ORIGINAL ARTICLE
Congenital Breast Deformity Reconstruction Using Perforator Flaps
Abhinav K. Gautam, BS,* Robert J. Allen, Jr., BS, Maria M. LoTempio, MD, Timothy S. Mountcastle, MD,* Joshua L. Levine, MD,* Robert J. Allen, MD, FACS,* and Ernest S. Chiu, MD*
Background: Congenital breast deformities such as Poland syndrome, unilateral congenital hypoplasia, tuberous breast anomaly, and amastia pose a challenging plastic surgical dilemma. The majority of patients are young, healthy individuals who seek esthetic restoration of their breast deformities. Currently, both implant and autologous reconstructive techniques are used. This study focuses on our experience with congenital breast deformity patients who underwent reconstruction using a perforator ap. Methods: From 1994 to 2005, a retrospective chart review was performed on women who underwent breast reconstruction using perforator aps to correct congenital breast deformities and asymmetry. Patient age, breast deformity type, perforator ap type, ap volume, recipient vessels, postoperative complications, revisions, and esthetic results were determined. Results: Over an 11-year period, 12 perforator aps were performed. All cases were for unilateral breast deformities. The patients ranged from 16 to 43 years of age. Six patients had undergone previous correctional surgeries. Eight (n 8) aps were used for correction of Poland syndrome and its associated chest wall deformities. Four (n 4) aps were used for correction of unilateral breast hypoplasia. In all cases, the internal mammary vessels were the recipient vessels of choice. No aps were lost. No vein grafts were used. All patients were discharged on the fourth postoperative day. Complications encountered included seroma, hematoma, and nipple malposition. Revisional surgery was performed in 30% of the cases. Esthetic results varied from poor to excellent. Conclusions: Perforator aps are an acceptable choice for patients with congenital breast deformities seeking autologous breast reconstruction. Deep inferior epigastric artery (DIEP) or supercial inferior epigastric artery (SIEA) aps are performed when adequate abdominal tissue is available; however, many young patients have inadequate abdominal tissue, thus a GAP ap can be used. Perforator aps are a safe, reliable surgical technique. In the properly selected patient, donor-site morbidity and functional compromise
are minimized, improved self-esteem is noted, postoperative pain is decreased, and excellent long-term esthetic results can be achieved. Key Words: breast, reconstruction, autologous, SIEA, DIEP, IGAP, SGAP, perforator, Poland, syndrome, tuberous, hypoplasia (Ann Plast Surg 2007;58: 353358)
Received February 20, 2006, and accepted for publication, after revision, August 2, 2006. From the *LSU Health Sciences Center, Division of Plastic and Reconstructive Surgery, New Orleans, LA; and the Medical University of South Carolina, Division of Plastic and Reconstructive Surgery, Charleston, SC. Reprints: Robert J. Allen, MD, MUSC Plastic Surgery, 125 Doughty Street, Suite 480, Charleston, SC 29401. E-mail: boballen@diepap.com. Copyright 2007 by Lippincott Williams & Wilkins ISSN: 0148-7043/07/5804-0353 DOI: 10.1097/01.sap.0000244006.80190.67
ongenital breast deformities occur in a wide spectrum of anatomic breast/chest wall abnormalities, from mild to severe cases. Poland syndrome, unilateral congenital hypoplasia, tuberous breast anomaly, and amastia all pose a challenging plastic surgical dilemma. Poland syndrome, rst described by Poland1 in 1841, is the most common cause of congenital breast hypoplasia/aplasia. Patients may present with absence of the sternal head of the pectoralis major, absence of axillary fold, rib cage anomalies, deciency of subcutaneous fat and axillary hair, and symbrachydactyly.2 Although the etiology of Poland syndrome is unknown, many researchers believe that it is caused by a circulatory defect of the subclavian artery around the 45th gestational day.3 The frequency of manifestation varies in different ethnic backgrounds, with the highest incidence (1:17,213) seen in Japanese school children4 to the lowest (1:52,530) seen in Hungary.5 Men are affected more often by a ratio of 2:1, and the effects are seen more often on the right side, with a ratio of 5:3.3 In women, patients can also present with ipsilateral breast and nipple hypoplasia and/or aplasia, which may also require reconstruction. Poland syndrome is more common on the right side.6,7 Implant reconstruction has been used routinely for breast asymmetry cases. In 1989, Rintala and Nordstrom8 presented a series of 49 women with breast asymmetry (19/49 cases were Poland syndrome). A subcutaneous prosthesis was used in 76% of their procedures with functionally satisfactory results (ie, ap survival) but relatively poor esthetic symmetry. Thirty-seven of 49 patients received implant reconstruction to correct their breast asymmetry. Complications included capsular contractures (n 5) and infection (n 1). Fodor and Khoury9 reported a woman with Poland syndrome who underwent multiple (n 3) implant reconstruction procedures over a 4-year period that cosmetically failed due to capsular contracture. The failed cosmesis was corrected
Annals of Plastic Surgery Volume 58, Number 4, April 2007
353
Gautam et al
Annals of Plastic Surgery Volume 58, Number 4, April 2007
with a latissimus dorsi ap with submuscular implant to enhance breast mound projection. Long-term results of implant reconstruction have been satisfactory but have a number of associated complications such as capsular contracture, with resulting pain and deformity, rupture/deation, infection, and migration.10,11 Autologous tissue with/without implant prosthesis can also be used for reconstruction of the deformity. The 2 most commonly used myocutaneous aps are the ipsilateral latissimus dorsi aps11,12 and TRAM aps.11,13,14 The latissimus dorsi ap has been well described for use in Poland chest-wall and breast deformity and almost always requires the use of a submuscular implant to provide adequate projection for the breast reconstruction.10,12,13 Cochran et al15 have reported Poland syndrome cases that present with combined hypoplasia of the latissimus dorsi muscle. Free tissue transfer procedures (eg, TRAM ap) have been reported, with excellent results.11 However, TRAM aps can have detrimental, long-term effects on the abdominal wall in young, active patients. A trend towards minimizing donor-site morbidity has evolved into using musclesparing autologous tissue to reconstruct the breast defect. Perforator free aps provide an alternative method of autologous reconstruction that uses the patients excess adipose tissue and skin. Several types of perforator aps currently used, including deep inferior epigastric artery (DIEP),16 supercial inferior epigastric artery (SIEA), superior gluteal artery perforator (SGAP),1719 and inferior gluteal artery perforator (IGAP)17 aps, all make use of different donor sites. Since these autologous perforators do not sacrice any muscle, the patient typically has a lower incidence of donor-site morbidity, abdominal weakness, pain, and has faster recovery time.20
CASE REPORTS Case 1
A 16-year-old female presented with hypoplasia of the left breast. Her past medical history included hormonal therapy started by her gynecologist without improvement of her breast asymmetry. When discussing breast reconstructive options, the patient and her parents were not interested in breast implants. Examination revealed a 5 foot 7 inch, 140-pound female with a normal 36C-sized right breast. The patients left breast was hypoplastic, but no other muscular or chest-wall deformities were present (Fig. 1A). The left breast was reconstructed using a SIEA perforator ap. A low surgical incision was chosen to avoid a scar around the umbilicus in this young female. The SIEA vessels were anastomosed to the internal mammary recipient vessels under the microscope. The nal weight of the left breast ap was 329 g (Fig. 1B). Long-term follow-up shows a continued esthetically pleasing result with good symmetry of the breasts (Fig. 1C).
Case 2
A 25-year-old woman presented with left sided Poland syndrome. She was 5 feet 6 inches, 153 pounds, with a bra size of 36B. At age 16, she had reconstruction with a polyurethane-coated silicone prosthesis for correction of her chest-wall deformity. At age 18, she presented with continued asymmetry and underwent a tissue expander with subsequent stacked prostheses. By age 23, she developed severe capsular contracture and, as a result, had both implants removed. On further examination, she revealed the absence of the sternal head of pectoralis major and a large-volume deciency of the left breast. A normal nipple was present. A plaster of paris mold of the right breast was made to determine the volume needed for symmetrical reconstruction (Fig. 2A). Via a horizontal tennis racquet incision, the internal mammary vessels were prepared. A SGAP ap weighing 394 g was harvested and anastomosed to the recipient vessels (Fig. 2B). Following the anastomosis, she developed a hematoma at the recipient site, which was successfully evacuated intraoperatively. The rest of her hospitalization was unremarkable, and she was discharged on postoperative day 4. Three years later, she continued to have an esthetically
MATERIALS AND METHODS
From 1994 to 2005, a retrospective study using a prospectively maintained database was performed on women who underwent perforator aps to correct congenital breast deformities and asymmetry. The clinical data evaluated included patient age, congenital breast deformity type, perforator ap type performed, ap volume, recipient vessels, postoperative complications, revisions, esthetic results, and patient satisfaction.
FIGURE 1. A, 16-year-old with hypoplasia of the left breast, with normal right breast. The low surgical incision was used to avoid scarring around the umbilicus. B, Left breast flap weighing 461 g. The superficial inferior epigastric vessels can be visualized exiting the flap inferiorly. C, One-year follow-up of 16-year-old patient status post reconstruction of hypoplastic left breast with SIEA flap.
354
2007 Lippincott Williams & Wilkins
Annals of Plastic Surgery Volume 58, Number 4, April 2007
Congenital Breast Deformity Reconstruction
FIGURE 2. A, Twenty-five-year-old with left-sided Poland syndrome. B, Preoperative Doppler markings of superior gluteal perforators. Horizontal oblique flap design. C, Three-year follow-up S-GAP flap reconstruction of left-sided Poland syndrome. D, Three-year follow-up of S-GAP flap donor site used in reconstruction for left-sided Poland syndrome.
pleasing result and had resumed a rigorous workout schedule (Fig. 2C, D).
Case 3
A 23-year-old female with congenital hypoplasia of the right breast desired breast reconstruction and an abdominoplasty. Examination revealed a 5 foot 6 inch, 170-pound female with a moderately hypoplastic right breast without associated chest-wall deformity, along with a normal left breast (Fig. 3A). The patient underwent right breast reconstruction using a DIEP perforator ap. While the ap was being harvested, a tissue expander was used to expand the breast pocket for the insertion of the free ap (Fig. 3B). The ap was inset through an inframammary incision and was anastomosed to the internal mammary vessels. The harvested DIEP ap weighed 515 g (Fig. 3C). Her postoperative course was unremarkable. At her 7-month follow-up, the patient was very pleased with her results esthetically and functionally (Fig. 3D).
formities. SIEA (n 2) and DIEP aps (n 2) were used for unilateral breast hypoplasia. Seven of 12 (58%) of the cases were secondary reconstructions after implant failure. In all cases, the internal mammary vessels were the recipient vessels of choice. The size of the internal mammary arteries ranged from 1.5 to 3.5 mm on the right side and from 1.5 to 2.0 mm on the left side. The internal mammary veins ranged from 2.5-4 mm on the right side; 2-3 mm on the left side. No vein grafts were necessary. Operating times varied between 5.5 hours and 7 hours. All patients were discharged on the fourth postoperative day. The patients rated the results as good to excellent; however, the surgeons felt the results ranged from poor to good.
Complications
Recipient-site complications encountered included venous congestion (n 2), hematoma (n 1), cellulitis (n 1), and partial fat necrosis (n 1). Three patients had complications (venous congestion and hematoma), which required return to the OR within the rst 24 hours postsurgery. One patient with previous implant reconstruction required surgical evacuation for bleeding. One patient was taken back for venous congestion. Her recipient vessels had been previously radiated for mediastinal lymphoma. The congestion was corrected by reanastomosing the ap to the thoracodorsal system. The cellulitis complication was managed nonoperatively with antibiotics. The patient that devel-
RESULTS
Over an 11-year period, 12 perforator aps were performed on 12 patients whose mean BMI was 22.5 and age ranged from 16 to 44 (Table 1). Eight patients had Poland syndrome with right-sided predilection (n 5). S-GAP (n 4), I-GAP (n 2), SIEA (n 1), and DIEP (n 1) aps were performed for Poland syndrome breast/chest-wall de 2007 Lippincott Williams & Wilkins
355
Gautam et al
Annals of Plastic Surgery Volume 58, Number 4, April 2007
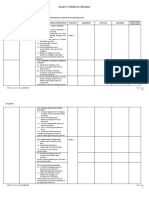
FIGURE 3. A, Twenty-three-yearold female with hypoplasia of the right breast prior to DIEP flap reconstruction. Doppler signals of the perforators are marked with xs. Standard abdominoplasty flap design. B, Intraoperative picture showing temporary tissue expander. C, DIEP flap weighing 515 g with arrow pointing to deep inferior epigastric perforator vessels. D, Seven-month follow-up status postDIEP flap reconstruction of right breast hypoplasia. TABLE 1. Congenital Breast Reconstruction Using Perforator Flaps
Patient 1 2 3 4 5 6 7 8 9 10 11 12 Age 43 16 20 40 25 21 39 22 21 44 17 18 Side L L R L L R R R R L R R Diagnosis PS BH PS PS PS PS PS BH BH BH PS PS Previous Surgeries 1 (implant) 0 0 2 (implants) 1 (implant) 5 (implants, LD ap) 2 (implants) 1 (implant) 0 1 (implant) 0 0 Flap SIEA SIEA SGAP IGAP SGAP IGAP DIEP SIEA DIEP DIEP SGAP SGAP Preop Nipple Presence Present Present Absent Present Present Absent Present Present Present Present Present Present Final Flap Weight (grams) 549 329 311 329 394 538 658 334 663 689 300 317 Complications Donor site seroma Venous congestion hematoma Hematoma Fat necrosis Venous congestion Cellulitis/wound dehiscence
PS, Poland Syndrome; BH, breast hypoplasia; SIEA, supercial inferior epigastric artery; IGAP, inferior gluteal artery perforator; DIEP, deep inferior epigastric perforator; SGAP, superior gluteal artery perforator.
oped partial fat necrosis was taken back to the operating room 3 weeks postoperatively, where 80 g of tissue was removed from the DIEP ap. All aps survived. Complications were successfully corrected without further sequelae. Donor-site complications included hematoma, seroma, and cellulites, all of which were managed nonoperatively. Seventeen percent
(2/12) underwent revisional surgeries at donor sites for symmetry, dog ears, or contour deformity.
DISCUSSION
Congenital-breast-deformity patients may present with a wide spectrum of anatomic chest-wall and thoracic abnor 2007 Lippincott Williams & Wilkins
356
Annals of Plastic Surgery Volume 58, Number 4, April 2007
Congenital Breast Deformity Reconstruction
malities. A number of surgical techniques have been developed and rened over the past 20 years to reconstruct these defects. Prosthetic implant reconstruction has been the mainstay of treatment10 14,21; however, the long-term results have been disappointing. Complications encountered include capsular contracture, implant migration, local tissue erosion, and adverse cosmesis.10,12,13,21 Thus, implant reconstruction may not be the ideal technique for these patients. Autologous reconstruction offers patients the opportunity to use their own tissue, which can provide long-lasting, esthetically natural results without the problems associated with implant reconstruction (Hellman et al, unpublished data). It seems logical that young patients would benet from surgery that is permanent, with few physiologic problems. However, donor-site morbidity such as abdominal hernia/ bulging, infected abdominal wall mesh, prolonged pain, and prolonged hospitalization has dampened the enthusiasm to use autologous techniques. In this study, we present our experience using microvascular perforator aps to reconstruct congenital breast deformities. Perforator free aps are a safe, reliable treatment option for both the plastic surgeon and patient. The technique reduces many of the autologous reconstruction sequelae such as abdominal wall bulge/weakness, pain, and prolonged OR and hospitalization time. Many of these young women are concerned not only about their physical appearance but also of the functional effects and recovery time, which may negatively impact their normal activities. The evaluation of a congenital-breast-deformity patient can be challenging due to severe breast asymmetry and the lack of donor sites for perforator aps. In general, we prefer DIEP and SIEA aps for reconstruction with excess abdominal tissue. Both DIEP and SIEA aps can be harvested using a low, transverse, bikini-line incision, which is well hidden like an abdominoplasty scar. If the patient does not have adequate abdominal tissue, as is the case in many of the younger patients, gluteal tissue is the preferred donor site. Either a superior or IGAP ap can be used. Typically, the SGAP allows for more tissue to be harvested (50 100 g greater than IGAP), but there is a higher chance for buttock contour deformity, requiring a secondary revisional procedure. In contrast, the IGAP ap scar can be hidden in the crease, which patients tend to prefer (Babineaux et al, unpublished data). However, wound dehiscence has been observed since it is an important anatomic area for sitting and movement.
sion and an additional OR visit. We have had success without pre-expansion when there is skin envelope laxity.
Inadequate Tissue Volume
Restoration of inadequate volume requires clinical analysis of the congenital breast deformity. Frequently, the tissue is decient in the inferior medial or inferior lateral breast pole, thus this must be accounted for in skin envelope preparation and ap insetting. With proper patient selection, perforator aps can have adequate volume for these congenital defects.
High Inframammary Fold (IMF) Position
In any breast reconstruction case, a properly positioned and newly created IMF is necessary to ensure a more predictable result.22 Patients with tuberous breast deformity tend to have a high IMF, which may need to be lowered below the inferior boundary of the contralateral IMF so autologous tissue does not sit high on the chest wall. On the contrary, if the previous expander/implant was positioned too low, it must be repositioned prior to nal ap inset.
Nipple Presence/Position
Existing nipple presence and malposition add to the complexity of breast reconstruction. Nipple-areolar complex may not have developed along normal meridians. As a result, surgical manipulation may be required to position and centralize the nipple/areola complex in esthetically correct locations. This may result in additional risk of unfavorable scarring and further breast parenchymal distortion.
Contralateral Breast Asymmetry
Though the contralateral breast may appear esthetically acceptable, to improve symmetry, a mastopexy/breast augmentation/breast reduction may be considered and discussed.
Recipient Vessel Access/Selection Proper
Recipient vessel selection is important for overall esthetics and ap viability success. It is preferable to extend the incisions from previous scars to gain access to the internal mammary vessels. If no prior scars are noted, an incision slightly above the inframammary fold allows adequate access to the second or third intercostal space (ie, internal mammary vessels) for microsurgery. If needed, the incision can also be extended laterally to reach the thoracodorsal vessels. Other traditional incisions, such as the tennis racquet incision, are also effective in recipient vessel access. Certainly, incisions should be discussed with the patient prior to surgery. Finally, revisional surgery should always be discussed to achieve optimal esthetic results. A single-stage operation result may be disappointing for both the patient and plastic surgeon.
Preoperative Planning and Considerations
Complexities of congenital breast reconstruction include inadequate tissue volume, inadequate skin envelope, nipple absence/malposition, high inframammary fold position, contralateral breast asymmetry, and recipient vessel access/selection.
Inadequate Skin Envelope
Ideally, the skin envelope is prepared by proper tissue expander placement. This allows the surgeon an opportunity to accurately predict the volume of autologous tissue needed to create an esthetically pleasing breast mound. Unfortunately, this requires multiple hospital visits for tissue expan 2007 Lippincott Williams & Wilkins
CONCLUSION
Perforator aps can be safely performed to reconstruct congenital breast deformities, with minimal functional effects and acceptable esthetic results. These aps have the advantage over traditional musculocutaneous aps in that the donor-site morbidity is lower, functional compromise is mini-
357
Gautam et al
Annals of Plastic Surgery Volume 58, Number 4, April 2007
mized, and recovery time is faster. Microsurgical skills are required. It should be considered in the surgical armamentarium for congenital breast reconstruction. REFERENCES
1. Poland A. Deciency of the pectoral muscles. Guys Hosp Rep. 1841;6: 191. 2. Seyfer AE, Icochea R, Graeber GM. Polands anomaly: natural history and long-term results of chest wall reconstruction in 33 patients. Ann Surg. 1988;208:776. 3. Schwartz T. Polands syndrome: prologue Poland syndrome Web site. Available at: http://www.polands-syndrome.com. Accessed August 3, 2005. 4. Der Kaloustian VM, Hoyme HE, Hogg H, et al. Possible common pathogenetic mechanisms for Poland sequence and Adams-Oliver syndrome. Am J Med Genet. 1991;38:69 73. 5. Sugiura Y. Polands syndrome: clinco-roentgenographic study on 45 cases. Cong Anom. 1976;16:1728. 6. Longaker M, Glat PM, Colen LB, et al. Reconstruction of breast asymmetry in Polands chest-wall deformity using microvascular free aps. Plast Reconstr Surg. 1997;99:429. 7. Shamberger RC, Welch KJ, Upton J. Surgical treatment of thoracic deformity in Polands syndrome. J Pediatr Surg. 1989;24:760 765. 8. Rintala AE, Nordstrom REA. Treatment of severe developmental asymmetry of the female breast. Scand J Plast Reconstr Surg. 1989;23:231. 9. Fodor PB, Khoury F. Latissimus dorsi muscle ap in reconstruction of congenitally absent breast and pectoralis muscle. Ann Plast Surg. 1980; 4:422. 10. Anderl H, Kerschbaumer S. Early correction of the thoracic deformity of Polands syndrome in children with the latissimus dorsi muscle ap: long-term follow-up of two cases. Br J Plast Surg. 1986;39:167.
11. Marks MW, Argenta LC, Izenberg PH, et al. Management of the chest-wall deformity in male patients with Polands syndrome. Plast Reconstr Surg. 1991;87:674. 12. Ohmori K, Takada H. Correction of Polands pectoralis major muscle anomaly with latissimus dorsi musculocutaneous aps. Plast Reconstr Surg. 1980;65:400. 13. Ohjimi Y, Shioya N, Ohjimi H, et al. Correction of a chest wall deformity utilizing latissimus dorsi with a turnover procedure. Aesthetic Plast Surg. 1989;13:199. 14. Hester TR, Bostwick J. Polands syndrome: correction with latissimus muscle transposition. Plast Reconstr Surg. 1982;69:226. 15. Cochran JH, Pauly TJ, Edstrom LE, et al. Hypoplasia of the latissimus dorsi muscle complicating breast reconstruction in Polands syndrome. Ann Plast Surg. 1981;6:402. 16. Allen RJ, Treece P. Deep inferior epigastric perforator ap for breast reconstruction. Ann Plast Surg. 1994;32:32. 17. Guerra AB, Metzinger SE, Bidros RS, et al. Breast reconstruction with gluteal artery perforator (GAP) aps: a critical analysis of 142 cases. Ann Plast Surg. 2004;52:118 125. 18. Blondeel PN. The sensate free superior gluteal artery perforator (S-GAP) ap: a valuable alternative in autologous breast reconstruction. Br J Plast Surg. 1999;52:185. 19. Rosenbaum G, Allen RJ. Treatment of Polands breast deformity using a superior gluteal artery perforator ap. 1995;88:10. 20. Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP aps for breast reconstruction. Plast Reconstr Surg. 2004; 113:11531160. 21. Garcia VF, Seyfer AE, Graeber GM. Reconstruction of congenital chest-wall deformities. Surg Clin North Am. 1989;69:1103. 22. Chun YS, Pribaz JJ. A simple guide to inframammary-fold reconstruction. Ann Plast Surg. 2005;55:8 11.
358
2007 Lippincott Williams & Wilkins
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Cuento en Ingles "Human"Documento11 pagineCuento en Ingles "Human"Angela GarciaNessuna valutazione finora
- Bases Anatomicas PerforantesDocumento12 pagineBases Anatomicas PerforantesAngela GarciaNessuna valutazione finora
- Clinical Atlas of Muscle and Musculocutaneous FlapsDocumento490 pagineClinical Atlas of Muscle and Musculocutaneous FlapsAngela Garcia100% (3)
- Brachial Plexus InjuriesDocumento345 pagineBrachial Plexus Injuriesmohamedwhatever100% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- CH 3 VocabDocumento5 pagineCH 3 VocabAbdirahman Abdullahi OmarNessuna valutazione finora
- Lymphatic Filariasis in The PhilippinesDocumento20 pagineLymphatic Filariasis in The PhilippinesSherlyn Joy Panlilio IsipNessuna valutazione finora
- Wellness at SeaDocumento9 pagineWellness at SeaRam Niwas ChauhanNessuna valutazione finora
- Points To Be DiscussedDocumento4 paginePoints To Be DiscussedShalini ShekharNessuna valutazione finora
- Lesson 4Documento4 pagineLesson 4api-316910625Nessuna valutazione finora
- Assessing The Status of Professional Ethics Among Ghanaian RadiographersDocumento31 pagineAssessing The Status of Professional Ethics Among Ghanaian Radiographersdeehans100% (1)
- 5 Problems (FSPR)Documento6 pagine5 Problems (FSPR)NMDNMSSDNessuna valutazione finora
- Glycerol MsdsDocumento6 pagineGlycerol MsdsJX Lim0% (1)
- Cardiac Science AED G3 Pro - Service ManualDocumento78 pagineCardiac Science AED G3 Pro - Service Manualmisu_stefan6141Nessuna valutazione finora
- Research Paper About Poverty - NSTP Project For FINALSDocumento5 pagineResearch Paper About Poverty - NSTP Project For FINALSLeoNessuna valutazione finora
- Group 2 - Up-Fa1-Stem11-19 - Chapter IiDocumento7 pagineGroup 2 - Up-Fa1-Stem11-19 - Chapter IijamesrusselNessuna valutazione finora
- PBHCI - Mental Health ScreeningDocumento2 paginePBHCI - Mental Health ScreeningRoshin Tejero0% (1)
- NursingDocumento18 pagineNursingKairmela PeriaNessuna valutazione finora
- Part-IDocumento507 paginePart-INaan SivananthamNessuna valutazione finora
- Rule On Adoption AM NO. 02-6-02-SCDocumento16 pagineRule On Adoption AM NO. 02-6-02-SCAnathea Cadagat100% (1)
- Umbar - Performance Task 7Documento3 pagineUmbar - Performance Task 7Bella CiaoNessuna valutazione finora
- Endo Gia Curved Tip Reload With Tri StapleDocumento4 pagineEndo Gia Curved Tip Reload With Tri StapleAntiGeekNessuna valutazione finora
- The Good-Enough Sex Model For Couple Sexual SatisfactionDocumento13 pagineThe Good-Enough Sex Model For Couple Sexual SatisfactionwernikNessuna valutazione finora
- MMO Chat Filter Bad WordsDocumento15 pagineMMO Chat Filter Bad WordsWilliam KravetsNessuna valutazione finora
- High PlateletsDocumento9 pagineHigh PlateletsHemal VyasNessuna valutazione finora
- Bellavista 1000 Technical - SpecificationsDocumento4 pagineBellavista 1000 Technical - SpecificationsTri DemarwanNessuna valutazione finora
- Tle 7 - 8 - FisheryDocumento17 pagineTle 7 - 8 - FisheryRey JavierNessuna valutazione finora
- Good Knight 420 GPatien ManualDocumento30 pagineGood Knight 420 GPatien ManualJose Antonio AlcazarNessuna valutazione finora
- SigmaDur 188-520-550 Msds Hardener PDFDocumento17 pagineSigmaDur 188-520-550 Msds Hardener PDFMarcos LaraNessuna valutazione finora
- PECFASDocumento2 paginePECFASNunik KhoirunnisaNessuna valutazione finora
- Bertam ProfileDocumento8 pagineBertam ProfilesadassanNessuna valutazione finora
- Inc Tnai IcnDocumento7 pagineInc Tnai IcnDeena MelvinNessuna valutazione finora
- Receiving and Storage PDFDocumento12 pagineReceiving and Storage PDFshyamkattiNessuna valutazione finora
- ASYNCHRONOUS-ACTIVITY-Module 1Documento7 pagineASYNCHRONOUS-ACTIVITY-Module 1Grant Wynn ArnucoNessuna valutazione finora
- PDP2 Heart Healthy LP TDocumento24 paginePDP2 Heart Healthy LP TTisi JhaNessuna valutazione finora