Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
BM Paper
Caricato da
Vidyavati Krishnan KumaranTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
BM Paper
Caricato da
Vidyavati Krishnan KumaranCopyright:
Formati disponibili
The Use of Antibiotics after Mandibular Third Molar SurgeryIs it Useful in Preventing Post Extraction Complications?
Medyan Al-Rousan BDS*, Gadeer Mukatash BDS*, Maan Alfar BDS*, Ahmad Tarawneh BDS*, Samer Ghazawi MD**, Zuhair Mhaidat BDS*
ABSTRACT Objective: To determine whether the administration of postoperative antibiotics following extraction of a asymptomatic soft tissue impacted lower wisdom teeth is necessary to reduce the incidence of dry socket, and post operative morbidity such as pain, swelling and trismus. Method: This study including 441 patients (208 males, 233 females) who required surgical extraction of lower wisdom teeth. Patients were divided into three groups; (G1) patients received Metronidazole, (G2) patients received Amoxicillin, and (G3) patients did not receive antibiotics at all. All patients received the same analgesic regimen. The incidence of dry socket, swelling, and the intensity of pain was recorded. The chi-squared test was employed to compare the results in the three treated groups Results: No significant difference was found between the three groups regarding the evaluated parameters in
the postoperative sequelae, i.e. pain, swelling and alveolar osteitis (dry socket).
Conclusion: This study showed that prescribing postoperative oral prophylactic antibiotic treatment following the removal of soft tissue impacted lower third molars does not contribute to less pain, less swelling, increased mouth opening or a lower incidence of dry socket, therefore it is not recommended for routine use. Key words: Antibiotics, Dry socket, Pain, Swelling, Third molar.
JRMS September 2011; 18(3): 47-51
Introduction
The routine use of postoperative prophylactic antibiotic therapy in patients undergoing surgical extraction of the lower third molars as an essential measure against infection and postoperative complications such as swelling, limitation of mouth opening and alveolar osteitis is still a widespread practice and a very controversial issue.(1,2) It is believed now by many surgeons that the advantages of using such prophylaxis seem to be
marginal, as shown in the audit undertaken at the University Dental Hospital National Health Service Trust in Cardiff (UK) about the usage of antibiotic prophylaxis practices in case of dental extraction and demonstrated the ''potential for saving large sums of money while apparently incurring no clinical disadvantage''.(3) Also, Monaco G et al, found no difference in patients undergoing surgical third molar extractions between those receiving postoperative amoxicillin and the control group who
From the Departments of: *Dentistry, King Hussein Medical Center, (KHMC), Amman-Jordan **General Surgery, (KHMC) Correspondence should be addressed to Dr. M. Al-Rousan, P. O. Box 3030 Amman 11821 Jordan, E-mail: malrousan@hotmail.com Manuscript received April 9, 2009. Accepted August 6, 2009
JOURNAL OF THE ROYAL MEDICAL SERVICES Vol. 18 No. 3 September 2011
47
did not receive antibiotics in terms of prevention of postoperative complications i.e. fever, pain, swelling and alveolar osteitis.(4) Iciar Arteagoitia et al, demonstrated clearly in their study that studied the efficacy of amoxicillin/clavulanic acid in preventing infectious and inflammatory complications following extraction of soft tissue vertically impacted mandibular third molar teeth, they found out that antibiotics are probably inefficacious, and they stated that antibiotics might be of value in cases where third molars are partially covered by bone and those in a horizontal position, they concluded this based on the fact that the frequency of postoperative complication without antibiotics was 12.9%, which in all cases was resolved using the rescue antibiotic.(5) Also, Leslie R et al in their question whether prophylactic administration of systemic antibiotics prevent postoperative inflammatory complications after third molar surgery, they hypothesized that only mandibular third molars requiring bone removal are at higher risk for post operative complications and antibiotics are better limited to this group and so limiting the exposure of patients to antibiotics and their associated risks and costs, also they recommended that more multicenter research need to be done in this field to determine the necessity for antibiotics and what type of antibiotics to be administered.(6) T. Kaczmarzyk et al evaluated the significance of administration of clindamycin applied in a single preoperative dose of 600 mg with or without subsequent 5-day therapy in prevention of postoperative complications after third molar surgery; again they could not demonstrate any significance for antibiotic prophylaxis that should affect the post operative sequalae in lower third molar surgery.(7) In another study, two different types of antibiotics were tested in patients undergoing surgical removal of third molar teeth, two groups of patients given amoxicillin (with calvulanic acid) and clindamycin respectively compared to another group of patients given placebo, no significant difference was found between the three different groups in the potoperative sequel, as no specific postoperative oral prophylactic antibiotic treatment after the removal of lower third molars could prevent the cases of inflammatory problems after surgery, as it did not contribute to a better wound healing, less
pain, or increased mouth opening, and therefore a conclusion made that routine use of antibiotics in these cases is not recommended.(8) From the literature review in the recent years, it is well noted that surgeons tend to avoid using prophylactic antibiotics following the surgical removal of the non infected third molars, and to start focusing on more important local factors that may play an important role in avoiding postoperative complications. The aim of this paper is to evaluate the actual need for the administration of postoperative oral antibiotics following the removal of asymptomatic soft tissue impacted lower third molars, and the efficacy of antibiotic therapy in preventing postoperative complications.
Methods
This study was conducted to assess the clinical efficacy of two antibiotics regimens (amoxicillin 500 mg tds and Metronidazol 250 mg tds) in two groups of patients compared with a third group of patients who were not given antibiotics in the setting of surgical extraction of a soft tissue impaction of third mandibular molar teeth. The study was conducted in accordance with Good Clinical Practice as approved by the ethical committee of the Royal Medical Services in Jordan. A written, dated informed consent was obtained from all patients prior to study entry. The study was carried out in the period between July 2008 till March 2009 at Prince Ali Hospital in Karak, see Table I showing demographic, objective and subjective measurement data. Four hundred forty one patients, 208 males (47.2%), 233 females (52.8%) requiring surgical extraction of a soft tissue impacted lower wisdom teeth were enrolled in this study. All patients were adults above 18 years old with mean age of 24.6 (age range 19-29 years). All patients were referred to our department by their treating dentists. No patient showed any sign of pain, inflammation, or swelling at the time of surgery. Clinical and radiologic factors were recorded for each case; all patients were medically free, as patients with any chronic illness such as diabetes mellitus or any other medical problem were excluded from the trial. The rationale for assigning the patients to the groups was strictly random and was done after surgery by using prepared randomizations in sealed envelopes. The standard surgical procedure was the same in all
48
JOURNAL OF THE ROYAL MEDICAL SERVICES Vol. 18 No. 3 September 2011
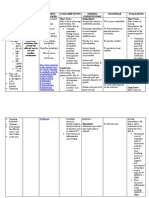
Table I. Demographic, objective and subjective measurement data G (1) patients on G (2) patients on Metronidazol Amoxicillin Number of patients 143 (33.4%) 140 (32.7%) Age (mean) 24.5 24.9 Gender 65 M 78 F 66 M 74 F Mean duration of surgery (mint) 15.4 14.7 Table II. Postoperative pain scoring in the three groups of patients Pain score Group 1 (143) Group 2 (140) Mild 78 (54%) 66 (47%) Moderate 45 (31%) 56 (40%) Sever 20 (14%) 18 (12%) Table III. Postoperative swelling Group Number of patients Table IV. Incidence of dry socket Group Number of patients
G (3) placebo patients 145 (33.8%) 24.1 67 M 78 F 15.9
Group 3 (145) 73 (50%) 51 (35%) 21 (14%)
Group 1 43 (30%)
Group 2 38 (27%)
Group 3 41 (28%)
Group 1 12 (8%)
Group 2 14 (10%)
Group 3 13(8.9%)
cases and only one lower third molar was removed at a time. A mouth rinse of 0.2% chlorhexidine solution for 1 minute was used before surgery. Patients were divided into three groups, group one (G1) received Metronidazole as 250 mg tds, group two (G2) received Amoxicillin 500 mg tds, and the third group (G3 did not receive antibiotics at all. The first and second groups had their antibiotics for 5 days postoperatively. All patients in the three groups had the same regimen of analgesia that consisted of 50 mgs tablet of diclofenac sodium taken one hour preoperatively, followed by diclofenac 50 mg of sodium tds orally for five days postoperatively. Also patients were asked to review the oral surgery clinic or in case of any emergency regarding pain or any other postoperative complication. Patients were asked not to take any other drugs during the trial and not to seek any other medical help except from our oral surgery clinic. The incidence of dry socket (alveolar osteitis), swelling, and the intensity of pain was recorded for all patients. The occurrence of dry socket was judged by both the signs and symptoms, and clinical examination. Dry socket was defined as absence of clot with necrotic remains present in the alveolus accompanied by severe persisting mandibular pain or increasing 48 h after surgery accompanied by intraoral inflammation and erythema. Swelling was subjectively measured, as patients
had just been asked if a significant swelling occurred or not and for how many days it lasted. The assessment of the intensity of post operative pain was done by employing a 100 mm visual analogue scale, and then results were classified into three categories, i.e. mild, moderate and severe. All patients were operated by the same surgeon (the main author) and the same surgical technique was employed in all cases, i.e. envelope mucopereosteail flap with minimal buccal bone removal if needed. All cases were done in the oral surgery outpatient clinics in our department at the Prince Ali Hospital in Karak (South of Jordan). All cases were performed under local anesthesia (zylocaine with adrenaline). The follow-up period was for two weeks, patients were reviewed on the second postoperative day, on day seven after the surgery and finally on day 14 postoperatively. Statistical analysis was performed by using 1-way analysis of variance, Students t test, and chi-square test. A value of P < 0.05 was considered statistically significant.
Results
Among the 441 patients who entered the trial, 13 did not check in for the follow-up examination and complete data sets were obtained only from 428 patients, for whom statistical analysis was performed. The three main parameters i.e. pain, swelling and alveolar osteitis (dry socket) had been
JOURNAL OF THE ROYAL MEDICAL SERVICES Vol. 18 No. 3 September 2011
49
evaluated and analyzed independently in the three groups of patients (G1, G2, G3). For the evaluation of post operative pain, see Table II that illustrates the numbers of patients who experienced mild, moderate or sever pain in the three groups of patients. The chi-squared test was employed to compare the results in the three treated groups, no statistically significant difference was found between the three groups (P > 0.05). Regarding the postoperative reactionary swelling, the number of patients who experienced a significant swelling that was associated with limitation of mouth opening and lasted more than 48 hours was as follows: in Group one (43 patients 30%), in Group two (38 patients 27%) and in Group 3 (41 patients 28%), see Table III. Again no statistically significant difference was found between the data in the three tested groups (P > 0.05). The incidence of alveolar osteitis (dry socket) in the three groups was as follows: in Group one (12 patients 8%), in Group two (14 patients 10%) and in Group 3 (13 patients 8.9%), see Table IV. Again no statistically significant difference was found between the three tested groups (P > 0.05). Among the patients who experienced dry socket, 68% of the cases were males, and 32% were females. Another significant finding was that 85% of the patients who experienced dry socket were heavy smokers; they even smoked at the day of surgery. Discussion We conducted this study in view of the growing concerns about the over-prescription of antibiotics, considering the implications regarding adverse effects in individual patients and increasing antimicrobial resistance within the community, a very high price to pay, this becomes very true when patients get exposed to a life threatening infections and antibiotics fail to play their expected role, also a significant financial implications should be considered when considering the high price spent on unjustified prescription of antibiotics, and the need for more expensive antibiotics when serious infections happen. Piecuch J et al, in their clinical trial to answer the question "should antibiotics be used for third molar surgery?" They found that the practice of oral surgeons of giving antibiotics to patients is usually led by one or more of the following reasons: 1) Presence of infection; 2) the patient is medically
compromised and requires antibiotic prophylaxis against metastatic infection; 3) the patient or the patient's family demands antibiotics; 4) the standard of care in the oral surgery community is to use antibiotics, and hence not to use them violates this standard; and when 5) the risk of postoperative infection is high and, consequently, prophylaxis is needed. But in their analysis of these reasons and their results, they found that in case of erupted mandibular or partially erupted third molars antibiotics are not justified unless an active infection is present, or when prophylaxis is needed in certain cases of medical compromise, including cardiac and immunosuppressive disorders. Also they stated that antibiotics are not justified for wound prophylaxis for maxillary third molar extractions regardless of the level of impaction because the overall infection rate is so low (0.27%). So, they recommended complying with these standards regardless of the patients desires, or even if it was the standard of care in the oral surgery community is to use antibiotics, as usually that standard implicates using antibiotics after surgery and that violates the basic principles of prophylaxis.(9) Also, many supportive opinions are in the literature recommending not to give antibiotics in third molar extraction as shown in the multi center study that involved patients with all four third molars below the occlusal plane, who were divided into two groups, the first group were given intravenous antibiotics just before third molar surgery, the second group (control group) did not receive intravenous antibiotics, and no statistically significant difference found between the two groups in term of the postoperative outcome.(10-13) Also, we should not underestimate the value of some local measures like the application of 0.2% chlorhexidine gluconate mouth rinsing preoperatively for 30 seconds and postoperatively for seven days. It was found to improve the outcome of surgery in terms of patients quality of life and postoperative complication.(14) Another valuable local measure after third molar surgery is local cold compression for 45 minutes postoperatively, as it causes vasoconstriction leading to reduced reactionary oedma and hence decreases the excitability of free nerve endings and peripheral nerve fibers, consequently increasing the pain threshold.(15) Also, the administration of IV corticosteroid with third molar surgery does have a positive impact in improving recovery after third molar surgery.(16) Dentists for decades are used to prescribing
JOURNAL OF THE ROYAL MEDICAL SERVICES Vol. 18 No. 3 September 2011
50
antibiotics routinely after extraction. It is about time to reconsider this, and carry out a more thorough evaluation for the patients, especially those who are asymptomatic prior to extraction. Also, if antibiotics are to be given, they should be given preoperatively, as systemic antibiotic should be present in the tissues before the procedure is begun, and the use of antibiotics only after surgery has no benefit or justification.(17) Patients following surgery usually will suffer pain, and what we really should care about is a very good regimen of analgesics, best started preoperatively, the best undoubtedly are the nonsteroidal antiinflammatory drugs (NSAID), given on regular basis, and toped up by a more potent analgesics when needed, as basically what the patients go through following extraction is an inflammatory state that is best treated by an anti-inflammatory drugs and good analgesics rather than treating it with antibiotics.
Conclusion
The results of our study showed that specific postoperative oral prophylactic antibiotic treatment after the removal of partially erupted or soft tissue impacted lower third molars does not contribute to less pain, less swelling, or decreased incidence of dry socket. And therefore, it is not recommended for routine usage.
References
1. Worrall SF. Antibiotic prescribing in third molar surgery. Br J Oral Maxillofac Surg 1998 Feb; 36(1):74-5. 2. Zeitler DL. Prophylactic antibiotics for third molar surgery: a dissenting opinion. J Oral Maxillofac Surg 1995 Jan;53(1):61-4. 3. Thomas DW, Hill CM. An audit of antibiotic prescribing in third molar surgery. Br J Oral Maxillofac Surg 1997Apr; 35(2):126-8. 4. Monaco G, Staffolani C, Gatto MR, et al. Antibiotic therapy in impacted third molar surgery. Eur J Oral Sci 1999 Dec; 107(6):437-41. 5. Arteagoitia I, Diez A, Barbier L, et al. Efficacy of amoxicillin / calvulanic acid in preventing infectious and inflammatory complications following impacted mandibular third molar extraction. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2005; 100(1):e11-e18.
6. Leslie R, Halpern A, Thomas B, et al. Does prophylactic administration of systemic antibiotics prevent postoperative inflammatory complications after third molar surgery? Journal of Oral and Maxillofacial Surgery 2007 February; 65(2): 177-185. 7. Kaczmarzyk T, Wichlinski J, Stypulkowska J, et al. Single-dose and multi-dose clindamycin therapy fails to demonstrate efficacy in preventing infectious and inflammatory complications in third molar surgery. International Journal of Oral and Maxillofacial Surgery 2007 May 36(5): 36, 417-422. 8. Paul W, Eckel D, Poeschl E. Postoperative prophylactic antibiotic treatment in third molar surgery-a necessity? J Oral Maxillofac Surg 2004 62:3-8. 9. Piecuch J, Arzadon J, Lieblich S. Prophylactic antibiotics for third molar surgery: a supportive opinion. J Oral Maxillofac Surg 1995; 53: 53-60. 10. Foy S, Shugars D, Phillips C, et al. The impact of intravenous antibiotics on health-related quality of life outcomes and clinical recovery after third molar surgery. J Oral Maxillofac Surg 2004 Jan; 62(1):1521. 11. Van Gool A, Ten Bosch J, Boering G. Clinical consequences of complaints and complications after removal of the mandibular third molar. Int J Oral Surg 1977 Feb; 6(1):29-37. 12. Bystedt H, Nord CE. Effect of antibiotic treatment on postoperative infections after surgical removal of mandibular third molars. Swed Dent J 1980; 4: 27. 13. Kaziro GSN. Metronidazole (Flagyl) and Arnica Montana in the prevention of post-surgical complications, a comparative placebo controlled clinical trial. Br J Oral Maxillofac Surg1984; 22:42. 14. Delilbasi C, Saracoglu U, Keskin A. Effects of 0.2% chlorhexidine gluconate and amoxicillin plus clavulanic acid on the prevention of alveolar osteitis following mandibular third molar extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94:301-4. 15. Forouzanfar T, Ausems S, Baart J. Effect of ice compression on pain after mandibular third molar surgery: a single-blind, randomized controlled trial. International Journal of Oral and Maxillofacial Surgery 2008; 37(9): 824-830. 16. Tiwana, P, Foy S, Shugars D, et al. The impact of intravenous corticosteroids with third molar surgery in patients at high risk for delayed health-related quality of life and clinical recovery. J Oral Maxillofac Surg 2005; 63:55-62. 17. Lacasa M, Jimene J, Ferras V, et al. Prophylaxis versus pre-emptive treatment for infective and inflammatory complications of surgical third molar removal. International Journal of Oral and Maxillofacial Surgery 2007 April; 36(4): 321-327.
JOURNAL OF THE ROYAL MEDICAL SERVICES Vol. 18 No. 3 September 2011
51
Potrebbero piacerti anche
- IADT Avulsion GuidelinesDocumento9 pagineIADT Avulsion GuidelinesHashem Motahir Ali Al-ShamiriNessuna valutazione finora
- Guidelines BookDocumento16 pagineGuidelines BookAdel ElaroudNessuna valutazione finora
- E Avulsion PDFDocumento8 pagineE Avulsion PDFluckytung07Nessuna valutazione finora
- 1-9 Iadt Guidelines Combined - LR - 11-5-2013Documento27 pagine1-9 Iadt Guidelines Combined - LR - 11-5-2013Pepo BelovedNessuna valutazione finora
- Emergensy in DentistryDocumento49 pagineEmergensy in DentistryVidyavati Krishnan KumaranNessuna valutazione finora
- Traumatic Dental Injury and TreatmentDocumento30 pagineTraumatic Dental Injury and TreatmentfirmansyahddsNessuna valutazione finora
- 1 Management of Medical Emergencies in Dental Practice - 60Documento60 pagine1 Management of Medical Emergencies in Dental Practice - 60Vidyavati Krishnan KumaranNessuna valutazione finora
- CPG Treatment of Periodontal AbscessDocumento26 pagineCPG Treatment of Periodontal AbscessFirda Maulani MawardiNessuna valutazione finora
- Gingival Index Score GisDocumento28 pagineGingival Index Score GisVidyavati Krishnan KumaranNessuna valutazione finora
- SDCEP Drug Prescribing For Dentistry Update Sept 2014Documento6 pagineSDCEP Drug Prescribing For Dentistry Update Sept 2014Vidyavati Krishnan KumaranNessuna valutazione finora
- Recurrent Aphthous StomatitisDocumento2 pagineRecurrent Aphthous StomatitisVidyavati Krishnan KumaranNessuna valutazione finora
- Self Assessment of Halitosis Among Diabetic Saudi Female PatientsDocumento13 pagineSelf Assessment of Halitosis Among Diabetic Saudi Female PatientsVidyavati Krishnan Kumaran100% (1)
- Dental Health With Oil SwishingDocumento4 pagineDental Health With Oil SwishingVidyavati Krishnan KumaranNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- BST GuidelinesDocumento6 pagineBST GuidelinesAman Raj KNessuna valutazione finora
- CML 2018 - Part I PDFDocumento536 pagineCML 2018 - Part I PDFfinney blessed75% (48)
- The Right To Effective Behavioral TreatmentDocumento4 pagineThe Right To Effective Behavioral TreatmentFrancesca LeograndeNessuna valutazione finora
- Apatarpan-Chikitsa-In-Sthoulya February 2017 1271176680 0516316Documento2 pagineApatarpan-Chikitsa-In-Sthoulya February 2017 1271176680 0516316PNessuna valutazione finora
- Gordon's Functional PatternsDocumento2 pagineGordon's Functional PatternsFatima Love Ariate-ArcasetasNessuna valutazione finora
- LearnEnglish - Professionals Podcasts-English-for-medicine-a-doctors-view - 1Documento6 pagineLearnEnglish - Professionals Podcasts-English-for-medicine-a-doctors-view - 1Cintial_89Nessuna valutazione finora
- Ky For Psychiatric Disorders Shannahof PDFDocumento12 pagineKy For Psychiatric Disorders Shannahof PDFSumit Kumar100% (1)
- Gloves - What Are They For?Documento1 paginaGloves - What Are They For?n4ceNessuna valutazione finora
- Swadesh FoundationDocumento8 pagineSwadesh FoundationKunal RajNessuna valutazione finora
- TI Activity 2 Getting Familiar With My Second HomeDocumento8 pagineTI Activity 2 Getting Familiar With My Second HomeSheila Mae CaballaNessuna valutazione finora
- Edinburgh Postnatal Depression Scale1 HaristaDocumento4 pagineEdinburgh Postnatal Depression Scale1 HaristaHar RealNessuna valutazione finora
- Risk ReportingDocumento3 pagineRisk ReportingMiguel TagustosNessuna valutazione finora
- BFAD Laws and RegulationsDocumento39 pagineBFAD Laws and Regulationsmrk_rlnd100% (2)
- CHN Reviewer Midterm TopicsDocumento19 pagineCHN Reviewer Midterm TopicsSamantha VeraNessuna valutazione finora
- What Are The Parts of A Nursing Diagnosis? Know How To Write An Appropriate Nursing DiagnosisDocumento9 pagineWhat Are The Parts of A Nursing Diagnosis? Know How To Write An Appropriate Nursing DiagnosisNoah ClevengerNessuna valutazione finora
- Early Diagnosis of Childhood Cancer: © Pan American Health OrganizationDocumento45 pagineEarly Diagnosis of Childhood Cancer: © Pan American Health Organizationcindy8127Nessuna valutazione finora
- Gianna Graziani Cover LetterDocumento1 paginaGianna Graziani Cover Letterapi-733890262Nessuna valutazione finora
- First Aid: Immediate and Temporary Care Given byDocumento18 pagineFirst Aid: Immediate and Temporary Care Given byJd Jamolod PelovelloNessuna valutazione finora
- ElephantiasisDocumento21 pagineElephantiasisPutri Anena AyuNessuna valutazione finora
- Corn PresentationDocumento20 pagineCorn PresentationPooja ShrivastavNessuna valutazione finora
- Acute Pain Nursing Care PlanDocumento3 pagineAcute Pain Nursing Care PlanSiafei RabeNessuna valutazione finora
- A Mixed Methods Study of Student Stress in PTADocumento9 pagineA Mixed Methods Study of Student Stress in PTATâm TịnhNessuna valutazione finora
- Health Law ProjectDocumento22 pagineHealth Law ProjectVarun MittalNessuna valutazione finora
- Uremic EncephalopathyDocumento4 pagineUremic EncephalopathySandi BeyNessuna valutazione finora
- Acr On Modular Learning SimulationDocumento4 pagineAcr On Modular Learning SimulationAbba JoyNessuna valutazione finora
- Business Description Key Information: Series CDocumento2 pagineBusiness Description Key Information: Series CYASH AGRAWALNessuna valutazione finora
- EqwDocumento3 pagineEqwHoward SadianNessuna valutazione finora
- Nursing Care PlanDocumento3 pagineNursing Care Plananon_984362Nessuna valutazione finora
- Gaceta Sanitaria 37 Comunica 23 FDocumento21 pagineGaceta Sanitaria 37 Comunica 23 FdsgonzalezNessuna valutazione finora
- FSA - Eligible ExpensesDocumento24 pagineFSA - Eligible ExpensesCatherine MifsudNessuna valutazione finora