Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Biology 310 Assignment Osteoporosis
Caricato da
Mohd IzwanTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Biology 310 Assignment Osteoporosis
Caricato da
Mohd IzwanCopyright:
Formati disponibili
BIOLOGY 310 ASSIGNMENT OSTEOPOROSIS
NAME: MOHD IZWAN IBRAHIM LECTERURES NAME: SIR ABDUL RAZAK B ABDUL RAHMAN
Abstract Osteoporosis is a common age-related disorder manifested clinically by skeletal fractures, especially fractures of the vertebrae, hip, and distal forearm. The major cause of these fractures is low bone mass, although an increase in trauma due to falls in the elderly also contributes. There are multiple causes for the low bone mass which, in any given individual, may contribute differently to the development of the osteopenia. The most important groups of causes are failure to achieve adequate peak bone mass, slow bone loss due to processes relating to aging, the menopause in women, and a variety of sporadic behavioral, nutritional, and environmental factors that affect bone mass in some but not in other individuals. The most important approach is prevention. Drugs and behavioral factors known to cause bone loss should be eliminated and perimenopausal women should be evaluated for possible preventive administration of estrogen. For patients with fractures due to established osteoporosis, the only drugs approved by the Food and Drug Administration are the antiresorptive agents calcium, estrogen, and calcitonin. Formation-stimulating regimens, however, are being developed and may be available for clinical use in the foreseeable future. These regimens may be capable of increasing bone mass to above the fracture threshold, thereby resulting in a clinical cure of the osteoporosis.
INTRODUCTION
History of Osteoporosis Osteoporosis has haunted human since the dawn of history. Egyptian mummies from 4,000 years ago have been found with the telltale dowagers hump. Most young women today can expect to spend their old age standing as straight and tall as they ever were, thanks to recent dramatic improvements in the diagnosis, prevention, and treatment of osteoporosis. An early medical pioneer, the eighteenth century English surgeon John Hunter discovered that as new bone is laid down in the body, old bone is destroyed, or resorbed. This process is now known as remodeling and was later shown to play a critical role in osteoporosis, though it wasnt even a recognized disease for more than 100 years after his death. In the 1830s the French pathologist Jean Georges Chretien Frederic Martin Lobstein noticed that some patients bones were riddled with larger than normal holes, and he coined the term osteoporosis (porous bone) to describe such deteriorated human bone. In the 1930s Fuller Albright Fuller Albright of Massachusetts General Hospital couldnt help but ponder what it was about being postmenopausal that made women particularly susceptible to having frail bones. Somewhere around 1940 he defines postmenopausal osteoporosis and begins treating women with the condition with estrogen. But estrogen therapy can only prevent damage to the skeleton by stemming bone loss. In the 1940s it was virtually impossible to detect the minimal bone loss seen in the early stages of the disease. Fortunately, starting in the 1960s, researchers developed more sensitive devices for detecting bone loss, including densitometers, which can determine bone density by measuring changes in the absorption of energy passing through bones in the hand, spine, hip, or other body part. This technique enables physicians to detect osteoporosis in its early stages, well before fractures occur. Also in the 1960s Herbert Fleisch discovered compounds known as bisphosphonates that inhibit bone resorption. Other researchers discover that compounds known as selective estrogen receptor modulators (SERMs) can simultaneously block breast tumors and trigger the growth of
uterine cells. At that time though, limited funding was available and the seriousness of the disease was not quite recognized or acknowledged. In 1984, the National Institutes of Health publicized this disease, citing it as a significant threat to health and emphasizing that bone loss could be reduced by estrogen therapy, calcium, good nutrition and exercise. In the 80s and 90s Researchers discovered cytokines that influence the development and activity of osteoclasts. Such discovery then led to bisphosphonates alendronate and risedronate entering the market as anti-osteoporosis drugs. The selective estrogen receptor modulator drug Raloxifene entered the market as a drug to treat and prevent postmenopausal osteoporosis in 1998. Around this time people were also urged to increase their calcium intake. Despite its long history, osteoporosis remains a formidable challenge to medicine.
Definition of Osteoporosis Osteoporosis was come from Greek words Ostoun meaning bone and Poros meaning pore. Osteoporosis is a systemic skeletal disease, which can be described as a condition leading to loss of the required normal density of bones. This disease leads to the bones becoming fragile which in turn leads to risks of fractures, for the smallest of injuries. is a medical condition in which there is a break in the continuity of the bone. A bone fracture can be the result of high force impact or stress, or trivial injury as a result of certain medical conditions that weaken the bones, such as osteoporosis, bone cancer, or osteogenesis imperfecta, where the fracture is then properly termed a pathologic fracture. Patients diagnosed with Osteoporosis, have a disorder in the skeleton leading to abnormally porous bone structure unlike the normal dense structure of bones.
CONTENTS
Condition of Osteoporosis The osteoporosis can be classified into two classes; the first one is Primary Type 1, Primary Type 2, or secondary. The primary type of osteoporosis is most common occur among the women after menopause in range of the ages between 50 and 75. Although it is more likely to occur in women, postmenopausal osteoporosis also occurs in men with low levels of testosterone. Primary osteoporosis can be subdivided into Type I is found in the post-menopause stage. Up to 80% of the women in the United States affected by Osteoporosis in the age group of 50 and 75 are of primary Type I. This is because of the sudden postmenopausal decrease in estrogen levels, which results in a rapid depletion of calcium from the skeleton. It is associated with fractures that occur when the vertebrae compress together causing a collapse of the spine, and with fractures of the hip, wrist, or forearm caused by falls or minor accidents. Primary Type 1 osteoporosis accounts for the significantly greater risk for osteoporosis in women than in men. The type II Primary Osteoporosis is more or less related to age. Type II osteoporosis (senile osteoporosis) typically happens after the age of 70 and affects women twice as frequently as men. Type II osteoporosis results when the process of resorption and formation of bone are no longer coordinated, and bone breakdown overcomes bone building. It may result from agerelated reduction in vitamin D synthesis or resistance to vitamin D activity (possibly mediated by decreased or unresponsive vitamin D receptors in some patients). he second type of Osteoporosis is the Secondary type. This type affects both the young and middle age group of people. Secondary osteoporosis is caused by other conditions, such as hormonal imbalances, certain diseases, or medications (such as corticosteroids). Details on the many other causes of secondary disease are included throughout this report. Secondary osteoporosis accounts for < 5% of osteoporosis cases. Causes include endocrine disease for examples glucocorticoid excess, hyperparathyroidism, hyperthyroidism, hypogonadism, hyperprolactinemia, diabetes mellitus.
Symptoms of Osteoporosis
Usually, osteoporosis does not cause any symptoms at first. Osteoporosis is often called the "silent" disease, because bone loss occurs without symptoms. People often don't know they have the disease until bone breaks, frequently in a minor fall that wouldn't normally cause a fracture. Osteoporosis develops very slowly over a period of many years. The condition may creep up on the patient without any obvious symptoms initially - it can take several months, and even several years to become noticeable. Early signs of osteoporosis may include:
Joint pains Difficulty standing Difficulty sitting up straight. The stooping position often seen among elderly people is a visible sign of possible osteoporosis. As the person's bone density or bone mass continues to go down fractures of the hip, wrist or bones in the spine become more common. Even a cough or a sneeze may fracture a rib or cause partial collapse of one of the spinal bones. Elderly people suffer greatly if they fracture a bone, because the bone cannot repair itself properly. Bones that do not effectively repair themselves are more likely to trigger arthritis, eventually leaving the patient seriously disabled. A large percentage of elderly patients who break a bone are not able to live independently afterwards. Although osteoporosis is not painful in itself, the condition cause bone to break more easily, and broken bones are very painful. The most common cause of chronic pain linked to the osteoporosis is a spinal fracture.
Risk Factors That Can Causes and Link to Osteoporosis The two major determinants of risk in the development of osteoporosis are peak bone mass and rate of bone loss. These two determinants are influenced by a number of genetic and environmental factors. Roughly 70% of cases of osteoporosis are probably the result of genetic predisposition, including the role of genetics in dictating how an individual will respond to various exogenous stressors. The remaining 30% of cases are probably triggered by environmental influences. A risk factor is something that increases a person's chances of developing a disease or condition. A number of factors can raise the probability of developing osteoporosis. They include: 1. The patient's sex. Women are twice as likely to develop osteoporosis as men. Experts say there are two reasons for this: I. II. III. Women start life with a lower bone life than men. Women live longer than men. The menopause causes a sudden drop in estrogen in women which speeds up bone loss.
2. Age. A person's bone mass lowers each year as he/she gets old. The falling bone mass continues until the person dies. The average loss of bone mass every year after age 50 is 0.5%
in both male and female.
3. Vertigo. Korean scientists found a link between people who suffer from vertigo and osteoporosis. This is a study of vertigo (Dizziness) among people who have Osteoporosis. The study analyzes the Osteoporosis patients by their gender and age, drugs used, and common conditions other than Osteoporosis. In total 87,013 Osteoporosis patients are studied. The study is created by eHealthMe based on reports from Food and Drug Administration (FDA) and is updated regularly. On Sep, 12, 2013: 87,013 people who have osteoporosis are studied. Among them, 6,855 (7.88%) have vertigo.
4. Human immunodeficiency virus (HIV). People with HIV/AIDS have a significantly higher risk of developing osteoporosis, as this study found. Studies have documented that osteopenia and osteoporosis are more common among HIV-positive patients, compared to HIV-negative individuals of the same sex and age. HIV infection can increase certain proteins in the body including interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-a) that may also be responsible for accelerated bone loss. It's also possible that the constant level of T-cell activation in the body may have an effect on bones. Some researchers have also speculated that HIV's ability to infect cells in the bone marrow may be to blame.
5. Ethnicity. People who are Caucasian, or of South Asian descent are more likely to develop osteoporosis than people of African or North/South American Indian descent. However, the risk is still significant for everybody.
6. Family history. People who have a close relative which meant parent or sibling who has or had osteoporosis are much more likely to develop it themselves. This is especially the case if the close relative had fractures. A study found that a gene called Duffy Antigen Receptor for Chemokines (DARC) negatively regulates bone density in mice.
7. People with small frames. People who have small body frames, as well as people who are very thin tend to have a higher risk of developing osteoporosis when they get older. This is because their bone mass is lower than other people's when they start to age and bone density begins to fall.
8. Estrogen exposure. Women who have a late menopause, when estrogen levels drop significantly, have a lower risk of developing osteoporosis compared to women whose menopause arrives early or at an average age. Conversely, women whose menopause arrived early are at a higher risk.
9. Anorexia and/or bulimia. People of both sexes who have, or have had eating disorders have a higher risk of developing osteoporosis. International Osteoporosis Foundation warns of bone damage from anorexia.
Treatment For Osteoporosis Hormone Replacement Therapy (HRT) For women going through the menopause HRT helps prevent bone density loss, thus reducing the risk of fractures during treatment. In many cases, though, HRT is not recommended as the first osteoporosis treatment, because it can raise her risk of having a stroke, heart disease and breast cancer. It is important that the patient discuss this option with a doctor.
Testosterone Treatment When a man has osteoporosis because of low testosterone production, testosterone treatment may be recommended. However, as with breast cancer, testosterone may accelerate the growth of prostate cancer as well as increasing the risk of prostate cancer recurrence.
Bisphosphonates These help prevent bone density loss and are non-hormonal drugs. The breakdown rate of bone by osteoclasts is slowed down while the production of new bone is speeded up. If bisphosphonates are unsuitable strontium ranelate might be a good alternative. Taking just one pill per month may help slow down bone loss, this study revealed. Side effects may include abdominal pain, nausea, inflamed esophagus, esophageal ulcers (especially for patients who have had acid reflux) - side effects may be severe. A study revealed that short term use of oral bisphosphonates may leave the jaw vulnerable to devastating necrosis (death of bone tissue).
Calcitonin This inhibits the cells that break down bone. Calcitonin is a hormone made by the thyroid gland. It may be prescribed for women who are more than 5 years beyond menopause and who do not tolerate bisphosphonate medicines. Calcitonin can be used in men with osteoporosis who have normal levels of the male sex hormone testosterone or whose osteoporosis does not get better with testosterone treatment. Calcitonin may relieve pain caused by spinal compression fractures. Calcitonin slows thinning of bone, and may help relieve pain from broken bones caused by osteoporosis. It may also decrease the risk of fractures in the spine.
Calcium and vitamin D supplements These may help older patients lower their risk of hip fractures. Sunlight is the best source of vitamin D. If patients do not have access to sunlight, as may be the case during the winter in some countries, the doctor may recommend a supplement. A Canadian study found that less than half (43%) of patients in Europe with osteoporosis are claiming to take both calcium and vitamin D supplementation with their osteoporosis treatment.
Selective Estrogen Receptor Modulators (SERMs) These drugs help prevent bone density loss. They mimic the beneficial effects of estrogen on bone density in postmenopausal women - however, without the risk of triggering cancers. Raloxifene is an example of this type of drug. Patients who have a history of blood clots should not take this medication. A common side effect is hot flashes. This drug is only approved for women with osteoporosis, not men.
Stem Cell Therapy Stem cell therapy is not a futuristic dream; these therapies are being performed every day by doctors in facilities across the country. There is no need to suffer with the debilitating effects of osteoporosis. Stem cell therapy can free you once again to live without fear that a fracture will cause irreversible damage. Stem cells are the foundation of all other cells in the body. They have no function other than to heal and regenerate damaged areas. These stem cells can take on the job of any other cell including the bone cells that are being lost or damaged due to osteoporosis. Stem cell therapy works by manipulating these stem cells so that they will strengthen and rebuild bones with greater structural health and significantly decreased risk of fracture due to bone loss.
Preventations from Osteoporosis Disease Osteoporosis is more or less preventable for most people. Prevention is very important because, while treatments are available for osteoporosis, no cure currently exists. Prevention of osteoporosis involves several aspects, including nutrition, exercise, lifestyle, and others.
Nutrition Eating the right foods is essential for good nutrition. Our bodies need the right vitamins, minerals, and other nutrients to stay healthy. Getting enough calcium and vitamin D is important for strong bones as well as for proper function of the heart, muscles, and nerves. The best way to get enough calcium and vitamin D is through a balanced diet.
A Diet High in Calcium Not getting enough calcium during a lifetime significantly increases the risk of developing osteoporosis and is associated with low bone mass, rapid bone loss, and broken bones. Good sources of calcium include low-fat dairy products, such as milk, yogurt, cheese, and ice cream; dark green leafy vegetables, such as broccoli, collard greens, and spinach; sardines and salmon with bones; tofu; almonds; and foods with added calcium, such as orange juice, cereals, soy products, and breads. Calcium supplements and vitamins are also available.
Recommended Calcium Intake by the National Academy of Sciences (1997) Age Birth-6 months 6 months-1 year 1-3 years 4-8 years 9-13 years 14-18 years 19-30 years 31-50 years 51-70 years 70 years or older Pregnant or lactating mg/day 210 270 500 800 1,300 1,300 1,000 1,000 1,200 1,200 See ages above
A Diet High in Vitamin D Vitamin D is important for the body to absorb calcium from the diet. Without enough vitamin D, the body is unable to absorb calcium from the foods that are eaten, and the body has to take calcium from the bones, making them weaker. Vitamin D comes from two sources. It is made in the skin through direct exposure to sunlight, and it comes from the diet. Many people get enough vitamin D naturally. Vitamin D is also found in fortified dairy products, egg yolks, saltwater fish, and liver. However, vitamin D production decreases with age, in people who are housebound, with the use of sunscreens, and during the winter when sun exposure is decreased. In these cases, people may need vitamin D supplements to ensure a daily intake of 400-800 IU of vitamin D.
Exercise Exercise is important to prevent osteoporosis. Although bones may seem like hard and lifeless structures, bones are more like muscle; bones are living tissue that respond to exercise by becoming stronger. Physical activity during childhood and adolescence increases bone density and strength. This means that children who get exercise are more likely to reach a higher peak bone density (maximum strength and solidness), which usually occurs by 30 years of age. People who reach higher peak bone densities are less likely to develop osteoporosis. The best exercise to prevent osteoporosis is weight-bearing exercise that works against gravity. Weight-bearing exercises include walking, hiking, jogging, climbing stairs, playing tennis, jumping rope, and dancing. A second type of exercise is resistance exercise. Resistance exercises include activities that use muscle strength to build muscle mass, and these also help to strengthen bone. These activities include weight lifting, such as using free weights and weight machines found at gyms and health clubs. Exercise has additional benefits in older people as well because exercising increases muscle strength, coordination, and balance and leads to better overall health.
Elderly people, people with osteoporosis, people with heart or lung disease, and people who have not exercised for most of adulthood should check with their health care professional before beginning any exercise program.
Quit Smoking Smoking is bad for the bones as well as for the heart and lungs. In women, nicotine inhibits the bone protective effect of estrogen. Women who smoke often go through menopause earlier, which hastens the development of osteoporosis because bone density decreases more rapidly after menopause. Women who smoke and choose hormone replacement therapy after menopause may require higher doses of hormones and have more complications. Smokers may absorb less calcium from their diets. Smokers have a higher lifetime risk of hip fracture than nonsmokers. Men smokers are at risk of developing osteoporosis.
Limit Alcohol Intake Regular consumption of 2-3 ounces of alcohol a day may be damaging to bones, even in young women and men. Heavy drinkers are more likely to have bone loss and fractures. This is related to both poor nutrition and increased risk of falling.
Therapeutic Medications Currently, bisphosphonates, such as alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronate (Reclast) are approved by the U.S. Food and Drug Administration (FDA) for the prevention and treatment of postmenopausal osteoporosis in women. As men age, they are also susceptible to osteoporosis. Alendronate is approved to increase bone mass in men with age-related osteoporosis. Alendronate and risedronate are
approved to treat men and women with steroid-induced osteoporosis. Adequate calcium and vitamin D intake is essential for bisphosphonates to be effective.
Raloxifene (Evista) . This medication approved for the prevention of osteoporosis only in postmenopausal women who are not taking hormone replacement therapy. Teriparatide is approved for the treatment of the disease in postmenopausal women and men who are at high risk for fracture. Estrogen/hormone therapy (ET/HT) is approved for the prevention of postmenopausal osteoporosis, and calcitonin is approved for treatment. Both alendronate and risedronate are approved for use by men and women with glucocorticoid-induced osteoporosis. See Understanding Osteoporosis Medications for more information.
Estrogen or Hormone Therapy After menopause, bone strength and density decreases rapidly in women. Studies show that estrogen therapy/hormone therapy (ET/HT) reduces bone loss, increases bone density in both the spine and hip, and reduces the risk of broken bones (especially the hip and spine). Currently, ET/HT is approved to prevent osteoporosis from developing after menopause. This therapy is most commonly available in the form of a pill or skin patch. See Hormone Replacement and Osteoporosis for more information. When estrogen therapy (ET) is taken alone, it increases a woman's risk of developing cancer in the uterus (cancer of the uterine lining, called endometrial cancer). Therefore, for women who have not had their uterus removed (have not had a hysterectomy), doctors prescribe an additional hormone, either natural progesterone or a synthetic similar substance called progestin. Progestin or progesterone in combination with estrogen is called hormone therapy (HT), and it reduces the risk of endometrial cancer in women who have not had a hysterectomy.
A large study from the National Cancer Institute (NCI) has recently indicated that long-term use of ET (estrogen alone) may also be associated with an increase in the risk of ovarian cancer. The Women's Health Initiative (WHI) study recently demonstrated that HT is associated with increases in the risk of breast cancer, ovarian cancer, stroke, and heart attack. No studies have determined whether ET (estrogen alone) is associated with an increase in the risk of breast cancer or whether it has an effect on cardiovascular events (like heart attack). Doctors prescribe any estrogen therapy only for the shortest period of time possible. ET/HT used to prevent osteoporosis after menopause should only be considered for women with menopausal symptoms who at significant risk of developing osteoporosis, and other nonestrogen medications should be considered if osteoporosis is the primary concern.
CONCLUSION
Conclusion. Lastly we can conclude that the osteoporosis will start develope when we take less calcium on our daily life and also the risk rapidly increases due to age. So we need to have a healthy lifestyle to prevent this disease from getting us trouble. Besides, we need to avoid taking alcohol especially for pregnency women. It can cause your baby to have a range of lifelong health conditions. Drinking alcohol during pregnancy can cause miscarriage, preterm birth and stillbirth. To get a healthy bone we need to follow the preventation steps as us mention in this report scuh as quick smoking, exercise, and other. So we can have a goood and healthy day in our late age time.
REFRENCES
Refrences. 1. http://www.medscape.com/viewarticle/410461_3. 2. Brian K Alldredge; Koda-Kimble, Mary Anne; Young, Lloyd Y.; Wayne A Kradjan; B. Joseph Guglielmo (2009). Applied therapeutics: the clinical use of drugs. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 1013. 3. Body, JJ (2011 NovDec). "How to manage postmenopausal osteoporosis?". Acta clinica Belgica 66 (6): 4437. 4. Background Document for Meeting of Advisory Committee for Reproductive Health Drugs and Drug Safety and Risk Management Advisory Committee. 5. Neurology;Dizziness Linked to Bone HealthPublished: Mar 23, 2009By Crystal Phend , Staff Writer, MedPage Today Reviewed by Robert Jasmer, MD; Associate Clinical Professor of Medicine, University of California, San Francisco. 6. Osteoporosis Treatment Following HipsFracture: How Rate Vary by Servis;Southern Medical Journal. 103(10):977-981, October 2010. 7. New Guidlines for the Preventation and Treatment of Osteoporosis; Lewiecki, E Michael; Watts, Nelson B. Southern Medical Journal. 102(2):175-179, February 2009. 8. Vitamin D: Important for Prevention of Osteoporosis, Cardiovascular Heart Disease, Type 1 Diabetes, Autoimmune Diseases, and Some Cancers; Holick, Michael F. Southern Medical Journal. 98(10):1024-1026, October 2005. 9. Recommended Calcium and Vitamin D Intakes;Food and Nutrition Board, Institute of Medicine, National Academy of Sciences, 2010. 10. Vogel VG, et al. (2006). Effects of tamoxifen vs. raloxifene on the risk of developing invasive breast cancer and other disease outcomes: The NASBP study of tamoxifen and raloxifene (STAR) P-2 trial. JAMA, 295(23): 2727-2741.
Potrebbero piacerti anche
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsValutazione: 4 su 5 stelle4/5 (2)
- Relieve Back Pain with Protruded Disc TreatmentDocumento12 pagineRelieve Back Pain with Protruded Disc TreatmentElvisNessuna valutazione finora
- Chronic GastritisDocumento7 pagineChronic GastritisDivina AquinoNessuna valutazione finora
- Hiatal Hernia: BY MR, Vinay KumarDocumento27 pagineHiatal Hernia: BY MR, Vinay KumarVinay KumarNessuna valutazione finora
- Case Presentation On Chronic Osteomyelitis: Prepared By: Sital Gautam MN1 Year, 2012Documento55 pagineCase Presentation On Chronic Osteomyelitis: Prepared By: Sital Gautam MN1 Year, 2012Rabina RajbanshiNessuna valutazione finora
- Nursing Careplan - Rectal CancerDocumento5 pagineNursing Careplan - Rectal CancerdrugcardrefNessuna valutazione finora
- Burns Assessment - TeachMeSurgeryDocumento5 pagineBurns Assessment - TeachMeSurgeryLaroui HoNessuna valutazione finora
- Compartment Syndrome Diagnosis and TreatmentDocumento3 pagineCompartment Syndrome Diagnosis and TreatmentTantyo Adi P100% (2)
- Feeding Helpless Patient - Types Od Diet and Factors Affecting Dietary PatternDocumento12 pagineFeeding Helpless Patient - Types Od Diet and Factors Affecting Dietary PatternKenje Kate Agripo0% (4)
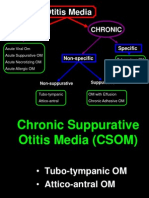
- CSOM TreatmentDocumento21 pagineCSOM TreatmentSarwinder SinghNessuna valutazione finora
- Mrs. D, 37 Yo. Post Modified Radical MastectomyDocumento17 pagineMrs. D, 37 Yo. Post Modified Radical MastectomyElisabethLisyeKonnyNessuna valutazione finora
- Kidney Stones: Causes, Symptoms and TreatmentDocumento26 pagineKidney Stones: Causes, Symptoms and TreatmentPatrascu CristiNessuna valutazione finora
- Bowel Training Guide for Constipation, Diarrhea and IrregularityDocumento2 pagineBowel Training Guide for Constipation, Diarrhea and Irregularitydickie.gdrNessuna valutazione finora
- Hookworm Disease: Ancylostoma Duodenale-Are Anthropophilic Human Hookworms Transmitted From Infected SoilDocumento5 pagineHookworm Disease: Ancylostoma Duodenale-Are Anthropophilic Human Hookworms Transmitted From Infected SoilBrix Valdriz100% (1)
- Dr. Abhimod R's Guide to Developing a Comprehensive School Health ProgramDocumento166 pagineDr. Abhimod R's Guide to Developing a Comprehensive School Health ProgramHarshitha100% (1)
- Cholelithiasis Health EducationDocumento12 pagineCholelithiasis Health Educationmohamad dildarNessuna valutazione finora
- Elimination Pattern (Fecal) MSPDocumento20 pagineElimination Pattern (Fecal) MSPMuhammadNessuna valutazione finora
- Alcohol Dependence SyndromeDocumento61 pagineAlcohol Dependence SyndromeAdrishyaNessuna valutazione finora
- NCP GeDocumento14 pagineNCP GeSuluhTriUtomoNessuna valutazione finora
- Ob Nursing Care Plan For Maternal Database Maternal and NewbornDocumento2 pagineOb Nursing Care Plan For Maternal Database Maternal and Newbornapi-403051801Nessuna valutazione finora
- Sigmoid Volvulus: Rashid Swed S. (Md4) Mwanyingili John A. (Md3)Documento46 pagineSigmoid Volvulus: Rashid Swed S. (Md4) Mwanyingili John A. (Md3)Amani Twaha MsemakweliNessuna valutazione finora
- Patient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDocumento93 paginePatient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDay MedsNessuna valutazione finora
- St. Paul University Nursing Care PlansDocumento6 pagineSt. Paul University Nursing Care PlansRoxanne MariÑas Delvo0% (1)
- A Client Care StudyDocumento27 pagineA Client Care StudyTestimony WilliamNessuna valutazione finora
- INTUSSUSCEPTIONDocumento3 pagineINTUSSUSCEPTIONS GNessuna valutazione finora
- OSCE Subcutaneous Injection SkillsDocumento2 pagineOSCE Subcutaneous Injection SkillsvishnuNessuna valutazione finora
- PBBN 1St Yr Child Health Nursing CBIMNCIDocumento29 paginePBBN 1St Yr Child Health Nursing CBIMNCIcopy smart100% (1)
- Research ProposalDocumento22 pagineResearch ProposalKapil LakhwaraNessuna valutazione finora
- Case 052: Biliary ColicDocumento4 pagineCase 052: Biliary ColicZauzaNessuna valutazione finora
- Hiatal HerniaDocumento3 pagineHiatal HerniaJobelle AcenaNessuna valutazione finora
- Oesophageal Atresia by GabriellaDocumento7 pagineOesophageal Atresia by GabriellaGabrielleNessuna valutazione finora
- Ostomy Care: Esther Hattler, BS, RN, WCCDocumento51 pagineOstomy Care: Esther Hattler, BS, RN, WCCAnita TermasNessuna valutazione finora
- AnorectalmalformationDocumento126 pagineAnorectalmalformationNinaNessuna valutazione finora
- Types of Skin Traction PresentationDocumento16 pagineTypes of Skin Traction PresentationZerjohn Seniorom100% (1)
- Secondary TB Eng 2015Documento124 pagineSecondary TB Eng 2015humanNessuna valutazione finora
- Femur FractureDocumento19 pagineFemur FractureMadx VNessuna valutazione finora
- Care of Eye - FOOT AND NAILS NCPDocumento12 pagineCare of Eye - FOOT AND NAILS NCPchaitali shankarNessuna valutazione finora
- AppendicitisDocumento16 pagineAppendicitisFiras AbusharikhNessuna valutazione finora
- Tracheostomy CareDocumento40 pagineTracheostomy CareSreelekhaNessuna valutazione finora
- Types and Causes of HemorrhageDocumento26 pagineTypes and Causes of HemorrhagepriyagidhuNessuna valutazione finora
- Hookworm Diseases: (Ancylostomiasis /Miner'S Disease/Egyptian Chlorisis)Documento21 pagineHookworm Diseases: (Ancylostomiasis /Miner'S Disease/Egyptian Chlorisis)Mel Izhra N. Margate100% (1)
- Guiilan Barre SyndromeDocumento19 pagineGuiilan Barre SyndromeDhayaneeDruAinsleyIINessuna valutazione finora
- Twenty Four Hour RecallDocumento39 pagineTwenty Four Hour RecallWillow DumpljngNessuna valutazione finora
- Hirschsprung Disease Case Study: Maecy P. Tarinay BSN 4-1Documento5 pagineHirschsprung Disease Case Study: Maecy P. Tarinay BSN 4-1Maecy OdegaardNessuna valutazione finora
- 1.case Presentation CHDDocumento23 pagine1.case Presentation CHDDHARM MEENANessuna valutazione finora
- Leishmania Nursing LectDocumento36 pagineLeishmania Nursing LectA Rhman Al OwaisNessuna valutazione finora
- Presentation Social IsolationDocumento20 paginePresentation Social IsolationMariagmzNessuna valutazione finora
- Care of Casts and Splints - OrthoInfo - AAOSDocumento2 pagineCare of Casts and Splints - OrthoInfo - AAOSSAIFUL ISLAMNessuna valutazione finora
- Hydrocephalus and Spina Bifida: Pathophysiology, Clinical Presentation and ManagementDocumento63 pagineHydrocephalus and Spina Bifida: Pathophysiology, Clinical Presentation and ManagementAjeng Aristiany Rahawarin100% (2)
- Disposable Delivery KitDocumento13 pagineDisposable Delivery Kitapi-3823785100% (1)
- RicketsDocumento5 pagineRicketsNader SmadiNessuna valutazione finora
- GINGIVITISDocumento43 pagineGINGIVITISRamyaNessuna valutazione finora
- Kenya ARV Guidelines 2018Documento230 pagineKenya ARV Guidelines 2018Felix Wafula MusibiNessuna valutazione finora
- Topical Medication ApplicationDocumento40 pagineTopical Medication ApplicationAnn Merlin JobinNessuna valutazione finora
- Otitis Media: Prepared By: - Priyanka ThapaDocumento38 pagineOtitis Media: Prepared By: - Priyanka ThapaKalo kajiNessuna valutazione finora
- Surgical CP ParotidDocumento43 pagineSurgical CP ParotidValarmathiNessuna valutazione finora
- Abnormal LabourDocumento7 pagineAbnormal LabourSaman SarKo0% (1)
- Assessing Newborns EffectivelyDocumento35 pagineAssessing Newborns EffectivelyBaldwin Hamzcorp Hamoonga100% (1)
- Non Viral HepatitisDocumento8 pagineNon Viral HepatitisKeith Wesley YbutNessuna valutazione finora
- BIOPSYDocumento8 pagineBIOPSYASHLEY DAWN BUENAFENessuna valutazione finora
- Gas Chromatography (GC)Documento4 pagineGas Chromatography (GC)Mohd Izwan67% (3)
- Surat Kebenaran Membawa Kereta Dengan Izin (Authorization Letter)Documento1 paginaSurat Kebenaran Membawa Kereta Dengan Izin (Authorization Letter)Mohd Izwan60% (5)
- Disadvantages of Using Internet Among University Student MalaysiaDocumento3 pagineDisadvantages of Using Internet Among University Student MalaysiaMohd IzwanNessuna valutazione finora
- THE NOCTURNAL BITING HABITS OF VARIOUS GENERA OF MOSQUITO IN TAMAN BERSATU, ARAU, PERLIS. (UiTM ARAU PERLIS MALAYSIA)Documento31 pagineTHE NOCTURNAL BITING HABITS OF VARIOUS GENERA OF MOSQUITO IN TAMAN BERSATU, ARAU, PERLIS. (UiTM ARAU PERLIS MALAYSIA)Mohd IzwanNessuna valutazione finora
- THE NOCTURNAL BITING HABITS OF VARIOUS GENERA OF MOSQUITO IN TAMAN BERSATU, ARAU, PERLIS. (UiTM ARAU PERLIS MALAYSIA)Documento53 pagineTHE NOCTURNAL BITING HABITS OF VARIOUS GENERA OF MOSQUITO IN TAMAN BERSATU, ARAU, PERLIS. (UiTM ARAU PERLIS MALAYSIA)Mohd IzwanNessuna valutazione finora
- Techniques in Microbiology I PDFDocumento16 pagineTechniques in Microbiology I PDFMohd Izwan67% (3)
- Portable Water PurificationDocumento9 paginePortable Water PurificationAnonymous V5UYBUMaNessuna valutazione finora
- Reglas de Oro en VM en SDRADocumento9 pagineReglas de Oro en VM en SDRADiana Laura Sarmiento VázquezNessuna valutazione finora
- ICE Checklist #4: Cleaning and Disinfection of The Dialysis StationDocumento1 paginaICE Checklist #4: Cleaning and Disinfection of The Dialysis StationAbidi Hichem100% (2)
- 47 439 1 PB PDFDocumento5 pagine47 439 1 PB PDFsrikar13Nessuna valutazione finora
- Ishikawa 2007Documento9 pagineIshikawa 2007Anggi RefinandaNessuna valutazione finora
- Apitherapy PrinciplesDocumento3 pagineApitherapy PrinciplesNikos ManiasNessuna valutazione finora
- Mold ToxinsDocumento7 pagineMold ToxinsMikiatlantul100% (1)
- Ethics & Legal Issues in PsychiatryDocumento91 pagineEthics & Legal Issues in PsychiatryShah OzairNessuna valutazione finora
- Prescription vs OTC Drug RisksDocumento19 paginePrescription vs OTC Drug Risks19-28 Manan PopatNessuna valutazione finora
- Comm 210 Informative Speech OutlineDocumento5 pagineComm 210 Informative Speech Outlineapi-269568046Nessuna valutazione finora
- Acute Phase Proteins As Early Non-Specific Biomarkers of Human and Veterinary DiseasesDocumento420 pagineAcute Phase Proteins As Early Non-Specific Biomarkers of Human and Veterinary DiseasesguadialvarezNessuna valutazione finora
- Strategies Improve Motor LearningDocumento18 pagineStrategies Improve Motor LearningUriel TabigueNessuna valutazione finora
- Evaluating The Training Effects of Two Swallowing Rehabilitation Therapies Using Surface ElectromyographyDocumento11 pagineEvaluating The Training Effects of Two Swallowing Rehabilitation Therapies Using Surface ElectromyographyTahysse Andrea Varela SilvaNessuna valutazione finora
- SMLEQBank 15-12-15 PDFDocumento294 pagineSMLEQBank 15-12-15 PDFIndrajit Barua0% (2)
- Treatment Guidelines (Nigeria)Documento116 pagineTreatment Guidelines (Nigeria)Laarny De Jesus Garcia - Ame100% (1)
- AmoebiasisDocumento2 pagineAmoebiasisJay PeeNessuna valutazione finora
- Dorothea Elizabeth Orem: Self-Care TheoryDocumento3 pagineDorothea Elizabeth Orem: Self-Care TheoryE.R.ONessuna valutazione finora
- Group TherapyDocumento16 pagineGroup TherapyAlpha50% (2)
- MENTAL HEALTH AND MENTAL DISORDERS WordDocumento12 pagineMENTAL HEALTH AND MENTAL DISORDERS WordJeanny YoungNessuna valutazione finora
- Beginners' Guide To Health and FitnessDocumento25 pagineBeginners' Guide To Health and FitnessMahmood HikmetNessuna valutazione finora
- Madness in Buenos AiresDocumento340 pagineMadness in Buenos AiresLaura VanadiaNessuna valutazione finora
- Group5 - Pharmacovigilance CIOMSDocumento386 pagineGroup5 - Pharmacovigilance CIOMSAjay Kumar100% (1)
- Polysaccharides Mucilage PolysaccharidesDocumento4 paginePolysaccharides Mucilage PolysaccharidesRiad SalihNessuna valutazione finora
- Pros and cons of experimental medical treatmentsDocumento3 paginePros and cons of experimental medical treatmentskingfish1021Nessuna valutazione finora
- STI Power Point PresentationDocumento33 pagineSTI Power Point PresentationHervis Fantini100% (1)
- Science Measures The Human Energy FieldDocumento7 pagineScience Measures The Human Energy FieldNICOL JOHANA ANGULO ORTIZNessuna valutazione finora
- Gastric and Duodenal Disorders - Test 4Documento21 pagineGastric and Duodenal Disorders - Test 4Vickie BuckerNessuna valutazione finora
- POSTPARTUM CAREDocumento58 paginePOSTPARTUM CAREGino Al Ballano BorinagaNessuna valutazione finora
- Breech PresentationDocumento40 pagineBreech PresentationShuhada Wahab100% (3)
- UNODCDocumento128 pagineUNODCMohammed Mohammed Shoukry Naiem100% (1)