Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Jcedv3i5p435 PDF
Caricato da
Max FaxTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Jcedv3i5p435 PDF
Caricato da
Max FaxCopyright:
Formati disponibili
J Clin Exp Dent. 2011;3(5):e435-40.
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis.
Journal section: Oral Surgery Publication Types: Research
doi:10.4317/jced.3.e435
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis A Clinical Study.
Ashok Bansal 1, Shivani Jain 2, Srimathy Arora 2, Shipra Gupta 3, Amaninder Singh 4, Deepti Prashar 4
MDS, Professor and Head, Department of Oral & Maxillofacial Surgery, Swami Devi Dyal Hospital & Dental College, Barwala, Haryana, India. 2 MDS, Professor, Department of Oral & Maxillofacial Surgery, Swami Devi Dyal Hospital & Dental College, Barwala, Haryana, India. 3 MDS, Associate Professor, Department of Periodontics, Dr H S Judge Institute of Dental Sciences and Hospital, Panjab University, Sector 25, Chandigarh, India. 4 Senior Lecturer, Department of Oral & Maxillofacial Surgery, Swami Devi Dyal Hospital & Dental College, Barwala, Haryana, India.
1
Correspondence: House number 1472, Near Government Dispensary, Sector 21, Panchkula, Haryana, India. Email: teena1472@yahoo.in
Bansal A, Jain S, Arora S, Gupta S, Singh A, Prashar D. Costochondral Grafts in the treatment of Temporomandibular joint ankylosis A Clinical Study. J Clin Exp Dent. 2011;3(5):e435-40. http://www.medicinaoral.com/odo/volumenes/v3i5/jcedv3i5p435.pdf
Article Number: 50568 http://www.medicinaoral.com/odo/indice.htm Medicina Oral S. L. C.I.F. B 96689336 - eISSN: 1989-5488 eMail: jced@jced.es
Received: 01/02/2011 Accepted: 08/05/2011
Abstract
Background: Treatment of temporomandibular joint (TMJ) ankylosis usually requires adequate excision of the involved ankylotic block (arthroplasty) without interposing any material (gap arthroplasty) or interpositional arthroplasty using autogenous or alloplastic materials. The objective of this paper was to note the potential of the costochondral graft (CCGs) as an interpositional material and to see whether they induce normal growth potential in the reconstructed mandible. Materials and method: The ankylosed temporomandibular joint was reached by a preauricular incision with or without angulation and exposed. In the first 4 cases, arthroplasty was done using a bur. The bony mass was detached of its muscle attachments and removed. In the 5th case, condylectomy was performed. In all cases, this was followed by immediate costochondral grafting. Results: The maximal incisal opening in the pre-operative period ranged from 0- 2mm and in the immediate postoperative period from 15- 20mm. at the end of the follow up period it ranged from 20- 35 mm. The increase in SNB angle, SND angle, ramus length and mandibular body length all showed linear growth of mandible on the side where costochondral grafting was done. Conclusion: The articular reconstruction with costochondral grafts for the treatment of TMJ ankylosis is efficient in relation to post- operative maximal incisal opening, recurrence and articular function. Key Words: Temporomandibular joint, Ankylosis, Surgery, Costochondral graft.
e435
J Clin Exp Dent. 2011;3(5):e435-40.
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis.
Ankylosis may be defined as the fusion of joint surfaces. Temporomandibular joint (TMJ) ankylosis is a rare disorder due to the fusion of mandibular condyle at the cranial base. It is mainly caused by trauma, systemic diseases, or infections. Clinically, the patient presents with severe limitation of mouth opening resulting in compromised oral hygiene procedures. It can also cause disturbances of facial and mandibular growth, and acute compromise of the airway invariably resulting in physical and psychological disability (1). A number of techniques have been described for the treatment of this condition in the literature. These include adequate excision of the involved ankylotic block (arthroplasty), without interposing any material (gap arthroplasty) or interpositional arthroplasty using autogenous or alloplastic materials (2, 3, 4, 5). Autologous rib grafting in craniofacial surgery dates back to the early twentieth century. Poswillo was the rst surgeon to truly establish the physiologic compatibility of costochondral grafting for the TMJ ankylosis. The bony part of the rib is used to replace the condylar neck or ramus and to affix the graft to the mandible, while the cartilaginous portion rests in the existing or newly constructed glenoid fossa. The bone cartilage junction provides a center with growth potential.
Introduction
This paper presents a clinical case series of the immediate correction of the deformity and asymmetry of the face associated with temoromandibular joint ankylosis with costochondral grafts (CCGs) as an interpositional material for arthroplasty.
Materials and Method
This study was conducted by analyzing 5 cases of unilateral temporomandibular joint ankylosis (4 males, 1 female) in children aged from 3 to 12 years. The duration of ankylosis at the time of the presentation ranged from 2 to 8 years. Four of them gave a history of local infection like otitis media and pre auricular abscess. The 5th case had a history of poliomyelitis with residual lower limb paralysis. No history and clinical evidences of systemic arthritis/ trauma was seen in any of the cases. A consistent finding was the asymmetry of the face with fullness of the affected side and flattening of the normal side, deviation of midline of the chin to the side of ankylosis and the prominence of antegonial notch on the affected side. Rampant caries and crossbite on affected side was seen in four out of five cases (Figures 1A-C). The diagnosis of temporomandibular joint ankylosis was established by clinical and radiological examination. Informed consent of the parents was obtained to click their photographs. General anesthesia with endotracheal tube passed by
Fig. 1. A: Pre- operative lateral view B: Pre- operative front view C: Intraoral view showing severe occlusal disturbance D: Pre-auricular skin incision e436
J Clin Exp Dent. 2011;3(5):e435-40.
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis.
Fig 2: A: The ankylotic block in the temporomandibular joint. B: Incision for costochondal graft. C: Rib exposed for obtaining costochondral graft. D: The excised costochondral graft. E: The costochondral graft bone plated to the lower border of the mandible by submandibular approach. F: Suturing done of the pre-auricular and the submandibular incisions
blind intubation technique was used in all cases. In 3 cases, the joint was reached by a preauricular incision with angulation and in two cases without angulations (Figure 1D). The ankylosed TMJ was exposed (Figure 2A). In the first 4 cases, osteoarthrectomy was done using a bur. The lower cut was made first, followed by the superior cut. The bony mass was then detached of its muscle attachments and removed. A minimum length of 1.5 cm of length was removed in all the cases. In the 5th case, condylectomy was performed. Surgical treatment at the donor site consisted of harvesting the 6th or the 7th rib with one cm of its attached costal cartilage. With the help of thoracic surgeon, the 6th or 7th rib with 1 cm of attached costal cartilage was harvested subperiosteally (Figures 2B-D). Length of the rib varied in the 5 cases depending on the correction of the vertical height of the ramus. The periosteum was reconstituted and the wound was closed in layers. The cartilage was shaped so that the mediolateral dimension was more than the anteroposterior dimension so as to mimic the original condyle of the mandible. Access to and preparation of the recipient site for the rib graft was made through a submandibular approach. Decortication of the posterior border and lower border of the mandible was then carried out. The rib was tightly fixed to the recipient site using bone plates (Figure 2E). The wound was then irrigated with normal saline and closed in layers (Figure 2F).
Results
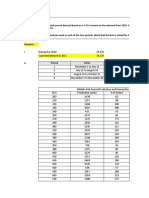
The follow up period varied from 6 months to eighteen months. The maximal incisal opening in the pre-operae437
tive period ranged from 0- 2mm and in the immediate post-operative period from 15- 20mm. At the end of the follow up period the mean maximal incisal opening was 25mm, with a range of 20- 35 mm. The interincisal opening of each case in the pre-operative period, in the immediate post-operative period and at the end of follow up is presented in Table 1. The mouth opening was found to increase gradually with the use of exercisers. Dynamic splints were found to be the most effective tool. Temporary facial nerve injury occurred in 1 out of 5 cases. Preoperative and postoperative cephalograms were taken in all the cases and analysed. Cephalogram of the case 1 and the relevant measurements are depicted in Table 1. The increase in angle SNB, SND ramus length and mandibular body length all show linear growth of mandible on the side where costochondral grafting was done. All the 5 cases showed marked improvement with restoration of normal symmetrical faces. The facial deformity had been reduced in all the cases due to increase in the facial height and shift of the midline of the face to normal. They also had significant improvement in their occlusal patterns. At the end of follow up, there were no signs of any recurrence in any of the cases. Temporary paresis of the temporal branch of the facial nerve occurred in 1 out of the 5 cases. According to the House and Brackmann grading system (6), it was classified as grade III, which means there was a slight to moderate movement of the forehead and slight weakness with maximum effort of the mouth. This patient recovered within 4 months.
J Clin Exp Dent. 2011;3(5):e435-40.
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis.
Case number 1 2 3
Onset age 5y 3y 2y
Age 9y 10 y 6y
Sex M M M
Etiology infection infection infection
Side involved left right right
Pre-op. MIO mm 0 0.5mm 0
Immediate post op. MIO mm 20mm 15mm 15mm
Follow up period 18 m 12 m 8m 6m 6m
MIO at the end of follow up 35mm 25mm 20mm 25mm 20mm
Facial nerve injury No No Till 4 months No No
4 2y 12 y M infection left 2mm 20mm 5 1y 3y F unknown right 0 15mm y- years, MIO maximum incisal opening, M- male, F- female, m- months Cephalogram readings of Case 1 Measurements ANGLE SNA ANGLE SNB ANGLE SND ANGLE FMA ANGLE Ar Go Gn Angle of facial convexity Body length Ramus length Y axis Pre-operative 79 69 66 31 127 19 49.5mm 36mm 68 Post- operative 79 73 69 39 125 12 54mm 40mm 67
Difference between pre- and postoperative readings Nil 4 3 8 2 7 4.5mm 4mm 1
SNA- angle formed by the intersection of sella- nasion plane and a line joining nasion and point A, SNB- angle between the sella-nasion plane and a line joining nasion to point B, SND- angle obtained by joining the sella nasion with the center of the symphysis, FMA- angle formed by the intersection of Frankfort horizontal plane with the mandibular plane, Ar Go Gn- angle obtained by joining Articulare, Gonion, Gnathion point, Angle of facial convexity- angle formed by the intersection of a line from nasion to point A and a line from point A to pogonion, Y axis- angle obtained by joining the sella gnathion line with the Frankfort horizontal plane.
Table 1. Patients data. Ankylosis characteristics according to age of onset of the ankylosis, age at the day of operation, sex, etiology, side involved, pre- and post-operative maximal incisal opening, follow up period and nerve injury after surgery; Cephalogram readings of Case 1
Discussion
The main causes of TMJ ankylosis are trauma and infection (3, 4, 7). Estimates of a traumatic origin range from 26% to 75% and of infection from 44% to 68% (7). In the present study the main cause was infection, especially otitis media which is common in young children. This may be because most of our patients were from a less well-informed population without easy access to the specialty. The ensuing ankylosis could therefore be a reflection of misdiagnosis, or non diagnosis of infections, which were not managed appropriately or received no treatment at all. Also, the children were too young at the time the TMJ ankylosis set in, to have experienced trauma, for it to be the main cause. Use of the autogenous costochondral interpositional graft is an effective procedure for the prevention of reankylosis following the surgical release of TMJ ankylosis (8, 9). Replacement of the condyle with a costochondral graft restores the altered biomechanics after condylectomy or gap-arthroplasty procedures (10). In case of growing child the interpositional material should
e438
not only fill the gap but should also reduce the facial deformity and induce normal growth potential of the mandible. Various growth centre transplants have been used but costochondral junction graft has been found to be the material of choice as an interposition in ankylosis in growing children (11). The rib cartilage has capabilities similar to that of the condylar cartilage and when a costochondral graft is used to replace TMJ apparatus and subjected to functional movements; it can function as a replacement for the mandibular condyle both histologically and physiologically. The cartilaginous portions of such grafts adapts well to the function of the reconstructed temporomandibular joint and to the ramus vertical dimension by reproducing condylar morphology. According to MacIntosh (1), the advantages of this graft are its biological compatibility, workability and functional adaptability. The growth potential of the costochondral graft makes it the ideal choice in children (1). This graft has also the advantage of a predicable behavior (1). With the release of the ankylosis and growth of the costochondral graft, a good functional and esthetic result
J Clin Exp Dent. 2011;3(5):e435-40.
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis.
can be achieved without further surgery (12), and the masticatory function is restored (13). However, there is a possibility of excessive growth of the graft, resulting in deviation of the chin and mandibular prognathism years later (14). However in the present study no patients developed clinically significant malocclusion. The 7-step protocol in the treatment of temporomandibular joint ankylosis consists of: a) Aggressive excision of the fibrous and/or bony ankylotic mass, b) Coronoidectomy on the affected side, c) Coronoidectomy on the contralateral side, if steps a and b do not result in a maximal incisal opening greater than 35 mm or to the point of dislocation of the unaffected TMJ d) Lining of the TMJ with a temporalis myofascial flap or the native disc, if it can be salvaged, e) Reconstruction of the ramus condyle unit with either distraction osteogenesis or costochondral graft and rigid fixation f) Early mobilization of the jaw. If distraction osteogenesis is used to reconstruct the ramus condyle unit, mobilization begins the day of the operation. In patients who undergo costochondral graft reconstruction, mobilization begins after 10 days of maxillomandibular fixation. g) Aggressive physiotherapy. A mandibular opening of 30mm is sufficient to leave patients with little or no functional deficit following reconstruction (15). This was achieved in 82% of their cases (15). In this study only 20% of the patients achieved this mouth opening. In the remaining 80% of patients despite that the opening was from 20-30 mm, still it was satisfactory especially for those with severe degree of long standing ankylosis. In all the cases the final result was more than that achieved intraoperatively. This can be explained by the presence of reversible pathology in the other joint as minimal fibrosis or contraction of the temporalis muscle. This emphasizes the fact that no forcible opening of the mouth should be done as this will lead to rupture of the fibrosis or temporalis musculature and subsequent scarring with ankylosis of the contralateral side. In our series, all cases were of unilateral involvement and all showed marked improvement in the functional and aesthetic appearance. Occlusal harmony was also achieved. Neither patient had any signs of recurrence or limitation of mandibular movements. Irrespective of the technique chosen by the surgeon, aggressive resection of the bony or fibrous ankylotic segment is crucial to avoid recurrence. Regardless of the surgical approach used to gain access to the TMJ, the final dissection places the facial nerve at risk for damage. A loss of function of the frontalis and orbicularis oculi muscles is always a possibility. The incidence of complications such as permanent injury
e439
of the facial nerve is very low, with rate varying from 1.5 to 32%, usually disappearing within 6 months. It is possible that the difficulty of the surgical procedure in relation to the type of ankylosis may increase the risks of damage to the facial nerve, especially because the longer the duration of surgery, the longer tissues are separated, thereby increasing the risk of such damage (16). The incidence of facial injury in this series it was 20% (1 out of 5 cases) and it resolved by itself in 4 months. Hence, the articular reconstruction with CCGs for the treatment of ankylosis is shown to be efficient in relation to the post-operative maximal incisal opening, recurrence and articular function.
Conclusion
Autogenous costochondral interpositional graft is an effective procedure for treatment of TMJ ankylosis by articular reconstruction technique; especially if it is associated with mandibular hypoplasia.
1. Vasconcelos BC, Porto GG, Bessa-Nogueira RV, Nascimento MM. Surgical treatment of temporomandibular joint ankylosis: followup of 15 cases and literature review. Med Oral Patol Oral Cir Bucal. 2009;14: E34-8. 2. Chossegros C, Guyot L, Cheynet F, Blanc JL, Gola R, Bourezak Z, et al. Comparison of different materials for interposition arthroplasty in treatment of temporomandibular joint ankylosis surgery: Long-term follow-up of 25 cases. Br J Oral Maxillofac Surg. 1997; 35:157-60. 3. Elgazzar RF,Abdelhady AI, Saad KA, Elshaal MA, Hussain MM, Abdelal SE, Sadakah AA. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg.2010; 39: 333-42. 4. Manganello-Souza LC, Mariani PB. Temporomandibular joint ankylosis: Report of 14 cases. Int J Oral Maxillofac Surg.2003; 32: 24-9. 5. el-Sheikh MM. Temporomandibular joint ankylosis: the Egyptian experience. Ann R Coll Surg Engl. 1999; 81: 12-8. 6. House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985; 93: 146-7. 7. Chidzonga MM. temporomandibular joint ankylosis: review of thirty- two cases. Br J Oral Maxillofac Surg. 1999; 37: 123-6. 8. Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg.2004; 33: 755-60. 9. Crawley WA, Serletti JM, Manson PN. Autogenous reconstruction of the temporomandibular joint. J Craniofacial Surg. 1993; 4: 2834. 10. Politis C,Fossion E,Bossuyt M. The use of costochondral grafts in arthroplasty of the temporomandibular joint. J Craniomaxillofac Surg.1987; 15: 345-54. 11. El-Sayed KM. Temporomandibular joint reconstruction with costochondral graft using modified approach. Int J Oral Maxillofac Surg. 2008; 37: 897-902. 12. Rahman QB, Molla MR,Islam ME. Temporomandibular joint reconstruction using costochondral graft. MymensinghMed J. 2007; 16: 225-9. 13. Matsuura H,Miyamoto N, Kurita K, Goss AN. The effect of autogenous costochondral grafts on temporomandibular joint fibrous and bony ankylosis: A preliminary experimental study. J Oral Maxillofac Surg.2006; 64: 1517-25. 14. Ko EW, Huang CS, Chen YR. Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac
References
J Clin Exp Dent. 2011;3(5):e435-40.
Costochondral Grafts in the treatment of Temporomandibular joint ankylosis.
Surg.1999; 57: 789-98. 15. Obeid G, Guttenberg SA, Connole PW. Costochondral grafting in condylar replacement and mandibular reconstruction. J Oral Maxillofac Surg. 1988; 3: 177- 82. 16. Weizberg S,Kryshtalskyj B. Facial nerve function following temporomandibular joint surgery using the preauricular approach. J Oral Maxillofac Surg. 1992; 50: 1048-51.
e440
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Anatomy Slide #9Documento18 pagineAnatomy Slide #9Max FaxNessuna valutazione finora
- Neurosurg Focus Article Pe7Documento9 pagineNeurosurg Focus Article Pe7Max FaxNessuna valutazione finora
- Anatomy Slide #3Documento32 pagineAnatomy Slide #3Max FaxNessuna valutazione finora
- A Rare Case of Carcinoma of Unknown Primary in AnDocumento2 pagineA Rare Case of Carcinoma of Unknown Primary in AnMax FaxNessuna valutazione finora
- 51 667 1 PBDocumento2 pagine51 667 1 PBMax FaxNessuna valutazione finora
- Ijd2023 9898446Documento6 pagineIjd2023 9898446Max FaxNessuna valutazione finora
- 8956Documento18 pagine8956Max FaxNessuna valutazione finora
- Treatment Planning of Surgical Orthodontic CasesDocumento173 pagineTreatment Planning of Surgical Orthodontic CasesMax FaxNessuna valutazione finora
- 30-3 Rrecurring Oral UlcerDocumento31 pagine30-3 Rrecurring Oral UlcerMax FaxNessuna valutazione finora
- FinalJ IncisionDocumento3 pagineFinalJ IncisionMax FaxNessuna valutazione finora
- NF UkDocumento7 pagineNF UkMax FaxNessuna valutazione finora
- Chapter 2Documento17 pagineChapter 2Max FaxNessuna valutazione finora
- 703-Article Text-966-1-10-20221030Documento4 pagine703-Article Text-966-1-10-20221030Max FaxNessuna valutazione finora
- India Evaluation of Public Awareness, Knowledge andDocumento8 pagineIndia Evaluation of Public Awareness, Knowledge andMax FaxNessuna valutazione finora
- Review of Salivary Gland NeoplasmsDocumento7 pagineReview of Salivary Gland NeoplasmsMax FaxNessuna valutazione finora
- Steroids in Oral SurgeryDocumento9 pagineSteroids in Oral SurgeryMax FaxNessuna valutazione finora
- Anatomy Nose 2Documento23 pagineAnatomy Nose 2Max Fax100% (1)
- Patient's Knowledge Regarding Dental Implants in Tabriz, IranDocumento6 paginePatient's Knowledge Regarding Dental Implants in Tabriz, IranMax FaxNessuna valutazione finora
- Computers in Biology and MedicineDocumento9 pagineComputers in Biology and MedicineMax FaxNessuna valutazione finora
- Autologous Blood Products and Their Roles Within DentistryDocumento6 pagineAutologous Blood Products and Their Roles Within DentistryMax FaxNessuna valutazione finora
- Maxillofacial Fractures: Midface and Internal Orbit - Part I: Classification and AssessmentDocumento6 pagineMaxillofacial Fractures: Midface and Internal Orbit - Part I: Classification and AssessmentMax FaxNessuna valutazione finora
- Dr. Smijal PG Its Year Department of PeriodonticsDocumento98 pagineDr. Smijal PG Its Year Department of PeriodonticsMax Fax100% (1)
- Corticosteroids in Dentistry: Review ArticleDocumento3 pagineCorticosteroids in Dentistry: Review ArticleMax FaxNessuna valutazione finora
- Temporomandibular Joint Arthrocentesis. Review of The LiteratureDocumento7 pagineTemporomandibular Joint Arthrocentesis. Review of The LiteratureMax FaxNessuna valutazione finora
- Oral Oncology: Letter To The EditorDocumento1 paginaOral Oncology: Letter To The EditorMax FaxNessuna valutazione finora
- Steroids in Dentistry: Presented By-Shibani Sarangi Postgraduate Iind Year (Dept of Oral & Maxillofacial Surgery)Documento67 pagineSteroids in Dentistry: Presented By-Shibani Sarangi Postgraduate Iind Year (Dept of Oral & Maxillofacial Surgery)Max FaxNessuna valutazione finora
- Sudan Medical Specialization Board (SMSB) Council of Oral and Maxillofacial SurgeryDocumento31 pagineSudan Medical Specialization Board (SMSB) Council of Oral and Maxillofacial SurgeryMax FaxNessuna valutazione finora
- The Use of Occlusal Splints in Temporomandibular DDocumento7 pagineThe Use of Occlusal Splints in Temporomandibular DMax FaxNessuna valutazione finora
- Fellowship in Maxillofacial Trauma: GoalsDocumento6 pagineFellowship in Maxillofacial Trauma: GoalsMax FaxNessuna valutazione finora
- Neck DissectionsDocumento9 pagineNeck DissectionsMax FaxNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Botswana Ref Ranges PaperDocumento7 pagineBotswana Ref Ranges PaperMunyaradzi MangwendezaNessuna valutazione finora
- Daily Mail 2022-10-25Documento74 pagineDaily Mail 2022-10-25mohsen gharbiNessuna valutazione finora
- 2 - (Accounting For Foreign Currency Transaction)Documento25 pagine2 - (Accounting For Foreign Currency Transaction)Stephiel SumpNessuna valutazione finora
- National Geographic Traveller India - July 2016-P2PDocumento104 pagineNational Geographic Traveller India - July 2016-P2PPeter100% (2)
- Pratham Bhardwaj: Education SkillsDocumento1 paginaPratham Bhardwaj: Education SkillsashuNessuna valutazione finora
- Affin Bank V Zulkifli - 2006Documento15 pagineAffin Bank V Zulkifli - 2006sheika_11Nessuna valutazione finora
- Robbins FOM10ge C05Documento35 pagineRobbins FOM10ge C05Ahmed Mostafa ElmowafyNessuna valutazione finora
- Assessment On The Efficiency of Technology Use in Teaching and Learning Process at Emilio Aguinaldo College Cavite. ResponsesDocumento14 pagineAssessment On The Efficiency of Technology Use in Teaching and Learning Process at Emilio Aguinaldo College Cavite. ResponsesZAMORA REYMARNessuna valutazione finora
- Communication & Soft Skills: Deepak and Arvind Kumar Pgppe + Mba (Feb'11)Documento19 pagineCommunication & Soft Skills: Deepak and Arvind Kumar Pgppe + Mba (Feb'11)deepaksingh16100% (1)
- Project Definition and DescriptionDocumento9 pagineProject Definition and DescriptionEileen VelasquezNessuna valutazione finora
- Athletic KnitDocumento31 pagineAthletic KnitNish A0% (1)
- 39 Nts General Merit List 22 Mar 18Documento26 pagine39 Nts General Merit List 22 Mar 18Lakshmi VedanarayananNessuna valutazione finora
- GE Money and BankingDocumento110 pagineGE Money and BankingBabita DeviNessuna valutazione finora
- Performance Appraisal System-Jelly BellyDocumento13 paginePerformance Appraisal System-Jelly BellyRaisul Pradhan100% (2)
- Class 8 PPT - Abhijeet Singh GureniyaDocumento16 pagineClass 8 PPT - Abhijeet Singh Gureniyasimran simmyNessuna valutazione finora
- Leading A Multi-Generational Workforce:: An Employee Engagement & Coaching GuideDocumento5 pagineLeading A Multi-Generational Workforce:: An Employee Engagement & Coaching GuidekellyNessuna valutazione finora
- MYPNA SE G11 U1 WebDocumento136 pagineMYPNA SE G11 U1 WebKokiesuga12 TaeNessuna valutazione finora
- Tu 05Documento23 pagineTu 05Yang ElvisQUNessuna valutazione finora
- Chapter 4 Lesson ProperDocumento44 pagineChapter 4 Lesson ProperWenceslao LynNessuna valutazione finora
- Thd04e 1Documento2 pagineThd04e 1Thao100% (1)
- Review - ChE ThermoDocumento35 pagineReview - ChE ThermoJerome JavierNessuna valutazione finora
- V.S.B Engineering College, KarurDocumento3 pagineV.S.B Engineering College, KarurKaviyarasuNessuna valutazione finora
- Part 1Documento14 paginePart 1Jat SardanNessuna valutazione finora
- Karla Beatriz Flores Ochoa 402-12 "C" 20 de Octubre de 2013Documento1 paginaKarla Beatriz Flores Ochoa 402-12 "C" 20 de Octubre de 2013Chabe CaraNessuna valutazione finora
- Family Decision MakingDocumento23 pagineFamily Decision MakingNishant AnandNessuna valutazione finora
- 4aeaconditionals 110228122737 Phpapp01Documento24 pagine4aeaconditionals 110228122737 Phpapp01Luis Fernando Ponce JimenezNessuna valutazione finora
- Venetian Shipping During The CommercialDocumento22 pagineVenetian Shipping During The Commercialakansrl100% (1)
- On Evil - Terry EagletonDocumento44 pagineOn Evil - Terry EagletonconelcaballocansadoNessuna valutazione finora
- Class XI Economics 2011Documento159 pagineClass XI Economics 2011Ramita Udayashankar0% (1)
- Tradingfxhub Com Blog How To Trade Supply and Demand Using CciDocumento12 pagineTradingfxhub Com Blog How To Trade Supply and Demand Using CciKrunal ParabNessuna valutazione finora