Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
8-5-09 The Superbill - November-December 1972 Issue of MGMA Journal
Caricato da
Bruce W. McKinnon MBA0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
73 visualizzazioni7 pagineIntroduction to my article entitled "The Super Bill" that appeared in the November/December 1972 issue of Medal Group Management, Journal of the MGMA (Vol 20, #1, pp 21-26). While a Medical practice Administrator in Minnesota, member of Medical Group Management Association and as Chairman of Minnesota Medical Group Management Association's "Clinic-Third Party Billing Procedures Committee", I had become frustrated with a growing proliferation of insurance company forms and promoted the idea of a physician generated standardized billing system for physician services that, as a by-product, would also serve the needs of the Insurance industry including Medicare and Medicaid. With the help of another medical practice administrator and Committee member, John Stehlow, we envisioned and portrayed system that would implement a nationwide coding system for medical, surgical & ancillary services and diagnosis. The concept was revolutionary at the time because it would be developed and implemented by the physician side of the health care industry rather than by the insurance industry which had become bogged down in their attempts to develop a standardized insurance claim form that would satisfy that industry. Given my background as a Medicare Part B Unit Supervisor (Travelers), it was apparent that this new concept address both out-patient services (not then covered by private insurance company contracts) and in-patient services. Following a two year (1970-1971) effort to promote this concept in Minnesota (which John and I labeled as the Superbill, a name conceived prior to a Super Bowl game), it was apparent that it would have to cross state lines to be successful. John and I were appointed to the MGMA Clinic Procedures Committee. This article provides a detailed description of the Superbill concept and the two year road that led to the publication. BWM
Titolo originale
8-5-09 the Superbill - November-December 1972 Issue of MGMA Journal
Copyright
© Attribution Non-Commercial (BY-NC)
Formati disponibili
PDF o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoIntroduction to my article entitled "The Super Bill" that appeared in the November/December 1972 issue of Medal Group Management, Journal of the MGMA (Vol 20, #1, pp 21-26). While a Medical practice Administrator in Minnesota, member of Medical Group Management Association and as Chairman of Minnesota Medical Group Management Association's "Clinic-Third Party Billing Procedures Committee", I had become frustrated with a growing proliferation of insurance company forms and promoted the idea of a physician generated standardized billing system for physician services that, as a by-product, would also serve the needs of the Insurance industry including Medicare and Medicaid. With the help of another medical practice administrator and Committee member, John Stehlow, we envisioned and portrayed system that would implement a nationwide coding system for medical, surgical & ancillary services and diagnosis. The concept was revolutionary at the time because it would be developed and implemented by the physician side of the health care industry rather than by the insurance industry which had become bogged down in their attempts to develop a standardized insurance claim form that would satisfy that industry. Given my background as a Medicare Part B Unit Supervisor (Travelers), it was apparent that this new concept address both out-patient services (not then covered by private insurance company contracts) and in-patient services. Following a two year (1970-1971) effort to promote this concept in Minnesota (which John and I labeled as the Superbill, a name conceived prior to a Super Bowl game), it was apparent that it would have to cross state lines to be successful. John and I were appointed to the MGMA Clinic Procedures Committee. This article provides a detailed description of the Superbill concept and the two year road that led to the publication. BWM
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato PDF o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
73 visualizzazioni7 pagine8-5-09 The Superbill - November-December 1972 Issue of MGMA Journal
Caricato da
Bruce W. McKinnon MBAIntroduction to my article entitled "The Super Bill" that appeared in the November/December 1972 issue of Medal Group Management, Journal of the MGMA (Vol 20, #1, pp 21-26). While a Medical practice Administrator in Minnesota, member of Medical Group Management Association and as Chairman of Minnesota Medical Group Management Association's "Clinic-Third Party Billing Procedures Committee", I had become frustrated with a growing proliferation of insurance company forms and promoted the idea of a physician generated standardized billing system for physician services that, as a by-product, would also serve the needs of the Insurance industry including Medicare and Medicaid. With the help of another medical practice administrator and Committee member, John Stehlow, we envisioned and portrayed system that would implement a nationwide coding system for medical, surgical & ancillary services and diagnosis. The concept was revolutionary at the time because it would be developed and implemented by the physician side of the health care industry rather than by the insurance industry which had become bogged down in their attempts to develop a standardized insurance claim form that would satisfy that industry. Given my background as a Medicare Part B Unit Supervisor (Travelers), it was apparent that this new concept address both out-patient services (not then covered by private insurance company contracts) and in-patient services. Following a two year (1970-1971) effort to promote this concept in Minnesota (which John and I labeled as the Superbill, a name conceived prior to a Super Bowl game), it was apparent that it would have to cross state lines to be successful. John and I were appointed to the MGMA Clinic Procedures Committee. This article provides a detailed description of the Superbill concept and the two year road that led to the publication. BWM
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato PDF o leggi online su Scribd
Sei sulla pagina 1di 7
November/December, 1972
Vol. 20 No. 1
MEDICAL GROUP
MANAGEMENT
Journal of the M.G.M.A.
‘Medical City Dellas
Dolls, Texas
Iston—p, 28)
ARTICLES PAGE
© Change and the Challenge for Associations .. ‘
© Price and Wage Controls and the Economics of the Health
Care Industry .. 9
© What's New with Professional Corporations .
© The Super Bill .
BRUCE W. McKINNON
@ THE SUPER BILL
the mombership. of M.GM.A- icles I emt
‘concep? ipesition™ can ‘be. token. The following
Inovetive approach to the billing of third parties
BRUCE W. McKINNON graduated from Hamline University in St. Paul, Minnesota
with a B.A. degree in 1964, majoring in history and political science, He worked as a
claims adjuster and Medicare office unit supervisor for Travelers Insurance Company
jor five years, He joined the Medical Education and Research Foundation at St, Paul
Ramsey Hospital, a hospital based group practice of medicine, in June of 1960, as
Assistant Director. In March of 1972 he became Administrator of the Hattiesburg
Clinic, P.A. of Hattiesburg, Mississippi. Mr. McKinnon was the former chairman of
the “Clinio—Third Party Billing Procedures Committee” of Minnesota Medical Group
Management Association and has recently been appointed to the “Clinic Procedures
Committee” of MG.MA.
©
One bill — “THE SUPER BILL” — for all billing, from
all doctor's offlees (solo or group), to all patients and to all
‘third party carriers (local, state and federal; Medicare,
Medicaid, welfare, commereial insurance companies, indus-
‘rial, efe') . . . one code — and only one — for services
rendered . ... one code — and only one— for diagnosis
the elimination of physician and patient signature require:
ments,
‘This is the big 1973 project for the CLINIC PROCEDURES,
COMMITTEE: Borrowing a theme from the M.G.M.A, Na-
tional Conference in Atlanta this year, we intend to be
“visible and physieal” with the new concept on your behalf
If successful (and we intend. to be), the Super Bill concept
could well save millions of dollars in health care costs an-
ually. “Goodbye, Gertrude” (see MGM, July, 1969) was the
first step in this’ direction. Now it is time for “The Super
Bill”,
‘Most administrators are aware that there are numerous
state cline manager organizations, TLE.W., HIC, AMA, the
Blues, and others working on (or have completed) standard
insurance claim forms and procedure coding systems. Cer.
tainly, thls Is a step in the right direction, but whose form,
or what system, are we going to adopt? Will these creations
‘cut across statelines and will there be universal acceptance?
What we see in the future is a battle over “pride of author.
ship," but not necessarily any solutions. Therefore, in pre-
paring this article, your Clinic Procedures Committee has
borrowed what we feel are the best ideas from such states
‘as Washington, Wisconsin, Minnesota, and California and
‘have summarized them into a new concept called the “Super
Bll” We are asking for your comments, pro or con, in de-
veloping this concept, rather than putting the “eart before
the horse” and developing yet another form,
‘The following outline details for you the idea we have in
‘mind; that js, the abolishment of all insurance claim forms
nd the substitution of a statement which will satisfy the
needs of third parties. This eoncopt would allow all options
assignment, nomassignment, federal or commercial insur-
“ance, but mast of all, just 2 bill. In other words, all doctors
Dills are automatically insurance claim forms whether the
patient does or does not have insurance, The ingredients are
(Q) common language, (2) common format, (3) complete
elimination of all signature requirements replaced by legal
falsification notices, (4) versatility in completion by any
process, and (5) the right for the physician to bill the pa-
tient and/or third party direct, according to individual prefer-
I. Adoption of a “Standardized Bill” (one piece of paper)
Which can serve as a Dill or balance forward state-
‘ment to the patient, or, as @ natural byproduct, would
serve the needs of the insurance industry, welfare,
Medicare, and other third parties,
‘The adoption of the standard bill eliminates the cost
of storing and completing varied third party payor
forms and internal forms such as bills and separate
balance forward statements. This allows for physician
business office billing manually, or via typewriter,
ookikeeping machine, and off-line or on-line computer
systems. Immediate ‘savings are extended to third
arty payors since one piece of paper is completely
interchangeable and the need to supply policyholders
with “physicigns claim forms” is virtually eliminated,
since any doctor's bill is automatically the claim form.
IL, Universal Standardization of Billing Format, Certain
basic information for billing to the patient, responsible
party, and/or third parties should be generated rou-
finely’ through the physician's accounting system and
presented on the bill in the following manner.
‘A. Deseription of services via the 19 CRVS (or
other nationally accepted publications) and two
Gigit modifier, when applicable, with an abbrevi
ated description.
1. At present the 1969 CRVS is the most widely.
used medical deseription publication in the
United States (the AMA CPT is virtually a copy
of this publication)
2, The 1969 CRVS includes an additional 2,000 pro-
cedural deseriptions not indicated in the 1964
November/Decomber 1972 21
CRYS. The California Medical Association ad-
vises that there will be no digits added to the
1969 CRVS number or modifier codes, which
lends to ease in adoption of future revisions. Tt
is imperative that the system be designed to
keep up with the new techniques and discoveries
within the field of medicine, as opposed to lock-
ing into a system guaranteed to become archaic
8. The 1969 CRVS provides the use of modifier
codes which enables the physician to designate
his eustomary fee in those cases where his fee
is reduced or increased. More importantly,
other modifier codes indicate multiple or biv
lateral procedures, assistant surgeons, team sur-
gery, professional components, ete, eliminating
the need for correspondence between third party
payors and the provider requesting clarification
Future additions of the CRVS could expand the
modifiers to include break down between doctor
and supervisory anesthesiology, hospital and
professional components for ancillary services,
injection procedures by attending physicians or
radiologists.
The modifier codes coupled with the CRVS
number, guarantee accuracy in third party pro
files and easily lends to accurate national sta
tistical studies, since all third party payor sta
tisties would be in a common language which is
interchangeable,
4. The contention that the 1969 CRVS is inflationary
or that it promotes the breakdown of services
in order to increase the total charge is invalid.
In view of the Wage-Price Freeze and Phase IT
of the present program, physicians are unable to
increase their prices beyond 25% overall. In
‘other words, for physicians to adopt the 1969
CRYS into their system, they are restricted to
identifying the CRVS number to the services
which they presently render and charge their
current fees.
Secondly, Blue Shield “fee schedules,” all
editions of the CRVS, and the CPT have recog-
nized the billing of nowincidental multiple pro-
cedures at 50% Future revisions of the CRVS
could place more emphasis upon differentiating
Detween incidental and non-ineidental multiple
services. If there has been a problem in this
area, it has been due to the lack of understand:
ing and national direction rather than the use
of the 1969 CRVS or an attempt on the part of
Physicians to defraud the public
‘Note: While we believe the 1969 CRVS is pres-
ently the best coding system in use, the number-
Ing system lacks codes for injections, supplies,
orthopedic appliances, eye glasses, contact
lenses, aphakia lenses, ambulances, many lab
and xray procedures, and a multitude of other
{ng system) could be used for description, At pres:
ent, the medical record in most linies must be
reviewed by clorical personnel in order to extract
this information, Since the physician generally is
not directly involved in the placement of the diag-
nosis on a claim form, insurance companies pres:
ently may be receiving inaccurate information,
while the physician's business office operating
costs are ever increasing due to the necessity of
having to pull the medical record, The revolution
in pre-printed “‘charge tickets” provides the solu.
tion since @ checkoff system is provided on the
front of the ticket for the service which the physi
cian renders, a simple, time saving technique, A
portion of the ticket is preprinted with the ICDA
codes unique to that physlclan's speciality. The
physictan simply checks the diagnosis descrip.
‘ion(s) pertaining to that patient’s treatment, (Or
hhe can select the proper code from a list, then
write it on the’ charge ticket.)
Only the diagnosis code number will print on
the standard bill — not the description, This is ab-
solutely essential since the samo piece of paper
(the statement/claim form) goes both to third par-
fies and to the patient, should the patient have in-
surance, (Whether the patient files his own claim
of it is done by the doctor is irrelevant)
Place of service via the Medicare codes
Dates of service — Inpatient services of a like
kind (ie, one procedure code such as follow-up
hospital visits may be lumped together), showing
total charge and the first date and last date of
serviee. It is understood that there will be no lump-
ing together of unlike services, sueh as the initial
‘exam and follow-up hospital visits,
Identification of patient by name, date of birth, and
patient status (adult male, adult female, dependent
male, dependent female.) Date of birth and patient
status are options, dependent upon how the clinic
handles insurance
Tientifieation of Medicare, Welfere, insurance or
other third party contract ‘holder by name, policy
number, subscriber number and/or contract num:
ber. Accurate and efficient identification cannot be
achieved until doctors, hospitals, and third parties
begin using a standard for individual identiication,
‘This will involve a carefully disciplined syntax for
the name and agreed number — most likely the
Social Security number, It is feasible and neces
sary, but its accomplishment will require several
years of cooperative effort and is not necessary for
the approval of this concept, Blanks would be al-
lowed within tho format to indicate this informa-
tion,
Note: This information would be provided by
the patient rather than by the elinie in those eases
where the patient insured will be filing his own
claim (see Roman numeral VD.
6
‘ancillary items which must he billed by many IIL. Other information needed by third party. The bill will
clinics. It is imperative that future revisions of ritGyltelal ace far nace har 2 Gs tape tars
the CRVS take these items into consideration, Plleable and if available by the doctor's otfiee or the
B. Diagnoses via the latest ICDA codes. Use of the patient, dependent upon the option chosen by the clinie
total coding system is preferable and Is encouraged. for billing
However, the “Massachusetts” codes (which iden. ‘A.Is condition employment related?
tify captions of the sections of the total ICDA eod- ‘An answer of “NO” is automatic since the pro-
22 Medical Group Management
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Nar / National Association of Realtors Code of Ethics - Pledge of PerformanceDocumento1 paginaNar / National Association of Realtors Code of Ethics - Pledge of PerformanceBruce W. McKinnon MBANessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The SuperbillDocumento8 pagineThe SuperbillBruce W. McKinnon MBANessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- 2-22-2013: The 1974 Superbill Book Publication Written by Bruce W. McKinnon in Hattiesburg, MS and Published by MGMADocumento55 pagine2-22-2013: The 1974 Superbill Book Publication Written by Bruce W. McKinnon in Hattiesburg, MS and Published by MGMABruce W. McKinnon MBANessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- 9-1-2012 Final Appendix C - With Cover Page - For 18 Nomination Letters From 62, 64 & 65 HU Tennis Team Members For Hall of Fame ApplicationDocumento20 pagine9-1-2012 Final Appendix C - With Cover Page - For 18 Nomination Letters From 62, 64 & 65 HU Tennis Team Members For Hall of Fame ApplicationBruce W. McKinnon MBANessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- 9-1-2012 Rev-Years 2011-2012 HU Hall of Fame Nomination PacketDocumento17 pagine9-1-2012 Rev-Years 2011-2012 HU Hall of Fame Nomination PacketBruce W. McKinnon MBANessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
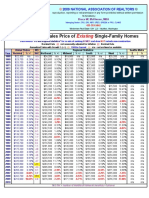
- 3-12-2010 NAR Average and Median Sale Prices For Single Family Homes and Condos 1968-2009Documento4 pagine3-12-2010 NAR Average and Median Sale Prices For Single Family Homes and Condos 1968-2009Bruce W. McKinnon MBANessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- 3-11-2010 Bruce McKinnon's Medical Administration Cirriculum Vitae 1964-1998Documento4 pagine3-11-2010 Bruce McKinnon's Medical Administration Cirriculum Vitae 1964-1998Bruce W. McKinnon MBANessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- 4-03-09 History of Interest Rates-15 Year Fixed Rate Mortgages - Freddie Mac SurveyDocumento2 pagine4-03-09 History of Interest Rates-15 Year Fixed Rate Mortgages - Freddie Mac SurveyBruce W. McKinnon MBANessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- 2008 Totals - Realty Trac Foreclosure Count Stats by StateDocumento1 pagina2008 Totals - Realty Trac Foreclosure Count Stats by StateBruce W. McKinnon MBANessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
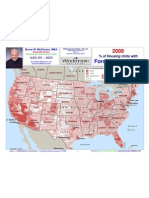
- 2008 Realty Trac Foreclosure Stats Heatmap by StateDocumento1 pagina2008 Realty Trac Foreclosure Stats Heatmap by StateBruce W. McKinnon MBANessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)