Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Defining and Diagnosing Burning Mouth Syndrome PDF
Caricato da
Faheemuddin MuhammadTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Defining and Diagnosing Burning Mouth Syndrome PDF
Caricato da
Faheemuddin MuhammadCopyright:
Formati disponibili
Defining and diagnosing burning mouth syndrome: Perceptions of directors of North American postgraduate oral medicine and orofacial
pain programs Gary D. Klasser, Andres Pinto, Jonathan M. Czyscon, Carl K. Cramer and Joel Epstein JADA 2013;144(10):1135-1142 The following resources related to this article are available online at jada.ada.org ( this information is current as of October 7, 2013):
Downloaded from jada.ada.org on October 7, 2013 Updated information and services including high-resolution figures, can be found in the online version of this article at:
http://jada.ada.org/content/144/10/1135
This article cites 63 articles, 6 of which can be accessed free: http://jada.ada.org/content/144/10/1135/#BIBL Information about obtaining reprints of this article or about permission to reproduce this article in whole or in part can be found at: http://www.ada.org/990.aspx
Copyright 2013 American Dental Association. All rights reserved. Reproduction or republication strictly prohibited without prior written permission of the American Dental Association.
CLINICAL
PRACTICE
Defining and diagnosing burning mouth syndrome
Perceptions of directors of North American postgraduate oral medicine and orofacial pain programs
Gary D. Klasser, DMD, Cert. Orofacial Pain; Andres Pinto, DMD, MPH; Jonathan M. Czyscon, BSc; Carl K. Cramer, DMD, MSc; Joel Epstein, DMD, MSD, Dip ABOM, FRCD(C), FDS RCS(Edin)
he International Association for the Study of Pain1 (IASP) defines burning mouth syndrome (BMS) as a burning pain in the tongue or other oral mucous membrane persisting for at least four months and associated with normal oral mucosa and normal laboratory findings.2,3 The IASP diagnostic criteria are as follows: burning sensation in the tongue or other parts of the oral mucosa, usually bilateral and associated with dysgeusia, dry mouth and denture intolerance. The International Headache Society4 (IHS) described BMS as an intraoral burning sensation for which no medical or dental cause can be found. The IHS further noted that pain may be confined to the tongue (glossodynia) with associated symptoms that include subjective dryness of the mouth (xerostomia), paresthesia and altered taste. The IHS provided the following diagnostic criteria for BMS: pain in the mouth present daily and persisting for most of the day, oral mucosa of normal appearance and exclusion of local and
AB STRACT
Background. The authors conducted a study to ascertain participants perceptions of and confidence in their responses regarding the definition and diagnosis of burning mouth syndrome (BMS). Methods. The authors developed an eight-question questionaire with input from several experienced clinicians in the fields of oral medicine (OM) and orofacial pain (OFP) and sent it to directors (n = 20; OM = 10; OFP = 10) of accredited postgraduate training programs in North America. They used descriptive statistics to analyze the results. Results. The response rate was 65 percent (n = 13; OM = 6; OFP = 7). Participants reported a mean of 7.3 cases of BMS in any given three-month period, with 89 percent of these cases managed within the programs. They identified, with a high degree of confidence, overall criteria for establishing a definition and definitive diagnosis of BMS. Conclusions. There were multiple similarities among participants responses regarding the elements to be included in the definition and diagnosis of BMS. Practical Implications. These data provide information on current status of definitions and diagnostic guidelines and may assist in development of future consensus statements on BMS that incorporate additional geographical representation and appropriate methodology. Key Words. Burning mouth syndrome; diagnosis; respondents perceptions; confidence rating scale. JADA 2013;144(10):1135-1142.
Dr. Klasser is an associate professor, Division of Diagnostic Sciences, School of Dentistry, Louisiana State University Health Sciences Center, 1100 Florida Ave., Box 140, New Orleans, La. 70119, e-mail gklass@lsuhsc.edu. Address reprint requests to Dr. Klasser. Dr. Pinto is an associate professor, University Hospitals Case Medical Center and Department of Oral and Maxillofacial Medicine and Diagnostic Sciences, School of Dental Medicine, Case Western Reserve University, Cleveland. Mr. Czyscon is a third-year student, College of Dentistry, University of Illinois at Chicago. Dr. Cramer was a clinical assistant professor, Department of Oral Biological and Medical Sciences, Faculty of Dentistry, University of British Columbia, Vancouver, British Columbia, Canada, when this article was written. He now is deceased. Dr. Epstein is the director, Oral Medicine, and an adjunct professor, Division of Otolaryngology and Head and Neck Surgery, City of Hope, Duarte, Calif.
JADA 144(10) http://jada.ada.org October 20131135
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL
PRACTICE
systemic diseases. In light of these somewhat imprecise definitions and descriptions, it is easy to understand the challenge facing health care practitioners when evaluating patients with BMS and the barriers to achieving an accurate and reliable diagnosis. The prevalence of BMS is reported to be between 0.7 percent and 5.0 percent of the general population, depending on the methodology (survey or clinical assessment) being used in and the geographical setting of the study.5-8 BMS is reported most commonly by women in the fifth to seventh decade3,9,10 and usually manifests in a period between three years before and 12 years after the onset of menopause.3 It rarely manifests before the age of 30 years.11,12 Investigators report female-to-male ratios ranging from 3:1 to 16:1.3,8,13-15 The pain commonly occurs bilaterally, involving the anterior two-thirds of the tongue, followed by the dorsum and lateral borders of the tongue, the anterior aspect of the hard palate and the labial mucosa of the lips. The burning pain also may occur simultaneously at multiple sites.3,11,14-18 Other symptoms that manifest with the burning complaint include taste alterations,3,19 often described as the presence of a constant foul, bitter or metallic taste sensation, which may be equally as disturbing as or more disturbing than the oral burning pain itself.5 Intriguingly, there are conflicting objective data regarding decreased salivary flow rates in people with BMS.20-23 Nevertheless, findings in some studies have shown qualitative changes in salivary composition.21,23,24 Several classification schemes have been proposed to assist in the diagnosis of BMS. One such classification, proposed by Lamey25 and Lamey and Lewis,26 contains three subtypes according to variations in pain intensity over 24 hours. This classification has not been validated and does not appear to be widely accepted by the scientific community. Jaaskelainen27 proposed three distinct subclasses that were based on neurophysiological, psychophysical and functional imaging studies. Gremeau-Richard and colleagues,28 using a double-masked crossover design, reported there to be two distinct groups of people with BMS, who could be classified on the basis of the location of neuropathic changes (that is, mediated by the peripheral or the central nervous system). A more pragmatic clinical approach is to separate BMS into two distinct categories: primary (essential or idiopathic) BMS, in which there is a lack of evidence of any other disease, and secondary BMS, in which an oral burning sensation is identified secondary to other clinical abnormalities or to systemic condi1136JADA 144(10)http://jada.ada.orgOctober 2013
tions such as anemia, diabetes, thyroid disease or gastroesophageal reflux disorder. Therefore, the clinician bases a diagnosis of BMS on clinical presentation and on the exclusion of local and systemic factors. To date, there is a lack of qualitative and quantitative analyses regarding clinicians understanding of the diagnosis of BMS. We approached these limitations by soliciting opinions (via a confidence rating scale [CRS]) from experienced health care practitioners who treat BMS. This technique engages the resources of all participants and results in an enhanced decision-making ability among members of the group with regard to resolution of the clinical problem addressed.29 This process has been used with an array of oral health issues, including decision support for diagnosis, and has led to improved outcomes for the conditions under investigation (such as outcomes assessment for periodontal therapy, referral criteria in pediatric dentistry and indications for use of radiography).30 Our aim in this study was to gather data about the perceptions of a group of oral medicine and orofacial pain training program directors from the United States and Canada in terms of the definition of BMS and the various factors and variables used in, and assisting with, the determination of its definitive diagnosis.
Methods
We designed a structured questionnaire with input from four experienced clinicians in oral medicine and orofacial pain (two from each field) who did not participate in the study directly. (The study protocol was approved by an accredited institutional review board.) Most questions were open-ended to facilitate variability of responses. This broad approach captured the most information regarding the respondents opinion without limiting answers or leading him or her. The only question with designated response categories involved specific diagnostic testing for conditions associated with oral burning sensation that excluded BMS. We derived these categories from the current literature on BMS and the knowledge of the four experienced clinicians. The questionnaire (Figure) contained eight questions pertaining to the diagnosis of BMS,
ABBREVIATION KEY. BMS: Burning mouth syndrome. CRS: Confidence rating scale. IASP: International Association for the Study of Pain. IHS: International Headache Society. OFP: Orofacial pain. OM: Oral medicine.
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL
PRACTICE
and the responses to these list the mean number of patients with burning mouth syndrome questions were analyzed in this 1 Please (BMS) seen every three months. study. We addressed the followlist the most common characteristic(s) to be used in a definition ing items: assessment of the 2 Please of BMS. respondents clinical experience as it pertained to BMS; the most list the criteria (including signs and symptoms) necessary for a common characteristics to be 3 Please definitive diagnosis of BMS. used in a definition of BMS; the list the local factors needing to be ruled out before a definitive criteria necessary (including 4 Please diagnosis of BMS can be made. signs and symptoms) to make a definitive diagnosis of BMS list the systemic factors needing to be ruled out before a definitive while addressing local, systemic 5 Please diagnosis of BMS can be made. and psychological factors that need to be ruled out; diagnostic list the psychological factors needing to be ruled out before a 6 Please definitive diagnosis of BMS can be made. tests used to support a diagnosis of BMS; and perception diagnostic tests are used to rule out local factors, systemic factors 7 What regarding the etiopathogenesis or both to support a definitive diagnosis of BMS? Please circle appropriate of BMS. Because the majority of letter(s). questions were in an open-ended a. salivary flow rates b. taste testing format, thereby allowing mulc. serologic studies tiple responses from each pard. soft-tissue biopsy ticipant, we grouped responses e. microbiological cultures according to consensus into f. medication substitution broader, more inclusive categories for discussion purposes. All 8 Please describe the etiopathogenesis of BMS. responses, with the exception of those related to Figure. Questionnaire used in the study. the participants clintABLE 1 ical experience, were measured according Characteristics respondents most commonly to a CRS. The CRS is chose to be used in a denition of burning mouth a Likert-like numeric rating scale with ansyndrome. chors of 1 (meaning I CHARACtERIStIC MEAN (SD) 95 PERCENt NO. OF am very uncertain) CONFIDENCE RESPONDENtS CRS SCORE INtERVAL (PERCENtAGE OF and 7 (I am very certHE tOtAL*) tain), and we includ10 (77) 6.1 (1.10) 5.42-6.78 Burning in the Oral Mucosa ed it to enhance the Absence of Clinical Findings 7 (54) 6.1 (1.07) 5.35-6.93 certainty of (strength Burning in the tongue 4 (31) 6.3 (0.96) 5.31-7.19 of belief in) responses Chronic Pain (Burning Pain 4 (31) 6.8 (0.50) 6.26-7.24 and reduce ambiguLasting Longer than three Months) ity (imprecision in * Total number of respondents = 13. the judged probabili SD: Standard deviation. ties).30-32 Respondents CRS: Confidence rating scale. used this categorical scale to rate their level of confidence in their selection of each option, time of questionnaire distribution, there were and we averaged all answers to produce a mean 20 accredited postgraduate OM and OFP trainscore with appropriate confidence intervals and ing programs in the United States and Canada standard deviations. We considered a high confi(n = 20; OM = 10; OFP = 10). The questionnaire dence rating as a 6.0 or greater. was delivered either electronically or via postal We obtained information about directors of service to all training program directors in the postgraduate oral medicine (OM) and orofacial United States and Canada. We made a second pain (OFP) programs through our personal attempt to deliver the questionnaire to those knowledge, as well as through consulting with who did not respond to the initial inquiry. We the American Academy of Oral Medicine and calculated and recorded descriptive statistics for the American Academy of Orofacial Pain. At the the CRS ratings.
JADA 144(10) http://jada.ada.org October 20131137
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL tABLE 2
PRACTICE
Criteria respondents reported most frequently as necessary for a denitive diagnosis of burning mouth syndrome.
CRItERION NO. OF RESPONDENtS* 10 7 4 4 4 3 MEAN (SD) CRS SCORE 6.2 (0.63) 6.1 (0.69) 6.0 (0.82) 6.0 (0.82) 5.3 (1.70) 6.3 (0.58) 95 PERCENt CONFIDENCE INtERVAL 5.81-6.59 5.63-6.65 5.20-6.80 5.20-6.80 3.58-6.92 5.68-6.98 Subjective Sensation of Intraoral Altered Sensory Symptoms Absence of Mucosal Pathology or Abnormalities Absence of Dental Etiology Presence of Burning Pain Xerostomia (Dryness of the Mouth) Absence of Salivary Gland Hypofunction, Dysfunction or Both (Objective Lack of Salivary Flow Measured According to Weight or Volume) * Total number of respondents = 13. SD: Standard deviation. CRS: Confidence rating scale. Criterion with a mean CRS score < 6.0.
Results
Thirteen (OM = 6; OFP = 7) of the 20 postgraduate directors responded, representing a response rate of 65 percent. The survey results showed that a mean of 7.3 cases of BMS had been diagnosed in each postgraduate program in any given three-month period (Figure, question 1), and approximately 89 percent of those cases had been managed within the postgraduate clinics. Table 1 describes the characteristics that respondents most commonly indicated should be used in a definition of BMS (Figure, question 2). Table 2 describes the criteria respondents reported most frequently as being necessary for a definitive diagnosis of BMS (Figure, question 3). The CRS results (Tables 1 and 2) demonstrated an overall elevated degree of confidence (6.0 or greater) among participants in their responses to the question about the most common characteristics to be used in a definition of BMS (Figure, question 2) and to the question regarding the criteria necessary for a definitive diagnosis of BMS (Figure, question 3), with the exception of xerostomia (Table 2). Respondents reported various factors (Figure, questions 4-6) as needing to be ruled out before they could provide a definitive diagnosis of BMS (Table 3). The majority of respondents indicated measurement of salivary flow rates (n = 11; mean [standard deviation {SD}] CRS score, 6.2 [0.60], 95 percent confidence interval [CI], 5.826.54) as a diagnostic test to rule out a diagnosis of BMS (Figure, question 7). This was followed by serologic studies (n = 8; mean [SD] CRS score, 6.1 [0.64]; 95 percent CI, 5.69-6.57), medication substitution (n = 7; mean [SD] CRS score, 6.1 [0.69]; 95 percent CI, 5.63-6.65), microbiological cultures (n = 5; mean [SD] CRS score,
1138JADA 144(10)http://jada.ada.orgOctober 2013
6.6 [0.55]; 95 percent CI, 6.12-7.08), soft-tissue biopsy (n = 3; mean [SD] CRS score, 6.3 [0.58]; 95 percent CI, 5.68-6.98) and taste testing (n = 2; mean [SD] CRS score, 6.0 [0.0]). Table 4 illustrates that the majority of respondents (54.5 percent) associated BMS with a neuropathic etiopathogenesis (Figure, question 8). Interestingly, participants displayed uncertainty in their responses when defining the etiopathogenesis for BMS (Figure, question 8) as idiopathic or unknown or psychological or psychosocial (Table 4).
Discussion
To our knowledge, this is the first study in which investigators have garnered clinicians perceptions and described their degree of confidence in their responses regarding the diagnostic criteria for BMS across emerging diagnostic disciplines such as oral medicine and orofacial pain. The results of our study support the assumption that the 13 postgraduate program directors (OM = 6; OFP = 7) who responded to our survey had experience in the clinical management of BMS (for instance, a mean of 7.3 cases of BMS had been diagnosed in their clinics in any given three-month period), thereby justifying their participation as a sample of clinicians qualified to render perceptions regarding this condition. Participants displayed overall confidence in their responses and consistency with the current literature1-4 with respect to the most common characteristics to be used in a definition of BMS (Table 1). Notably, only four of the 13 program directors reported a burning sensation in the tongue and chronic pain as characteristics that should be used in a definition of BMS. Perhaps many of
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL tABLE 3
PRACTICE
Factors respondents indicated as needing to be ruled out before a denitive diagnosis of burning mouth syndrome could be made.*
FACtOR (tOtAL NO. OF RESPONSES) NO. OF RESPONSES (PERCENtAGE OF tOtAL RESPONSES) 11 (20.0) 10 (18.2) 9 (16.4) 8 (14.5) 8 (14.5) 4 (7.3) 5 (9.1) MEAN (SD) CRS SCORE 95 PERCENt CONFIDENCE INtERVAL 5.96-6.76 5.81-6.59 5.93-6.51 5.76-6.74 5.89-6.37 5.93-7.07 5.92-6.88 Local (n = 55) Oral mucosal lesions (lichen planus, benign migratory glossitis, benign mucous membrane pemphigoid, pemphigus, oral ulcers, oral cancer, leukoplakia) Microbial infection (fungal, viral or bacterial) Dental issues (poorly tting dental prostheses, mechanical irritations, dental caries, periodontal or pulpal disease) Salivary gland hypofunction/dysfunction Contact allergy/mucosal contact irritants (contact allergy or allergy to dental materials, mouthwash, spices, food ingredients, additives or preservatives) Parafunctional habits of tongue or lips Other (nerve trauma or neuropathy, toxic environmental exposure, taste disorder) Systemic (n = 31) Autoimmune disorders (Sjgren syndrome, connective tissue disease, systemic lupus erythematosus) Vitamin or nutritional deciencies Endocrine disorders (diabetes, metabolic diseases) Medication adverse effects Other (hematologic disorder, gastrointestinal condition, cancer, psychopathology) Psychological (n = 28) Anxiety Depression Somatoform disorder Other (psychosis, obsessive-compulsive disorder) *
6.4 (0.67) 6.2 (0.63) 6.2 (0.44) 6.3 (0.71) 6.1 (0.35) 6.5 (0.58) 6.4 (0.55)
8 (25.8) 6 (19.4) 6 (19.4) 4 (12.9) 7 (22.6) 11 (39.3) 9 (32.1) 4 (14.3) 4 (14.3)
6.4 (0.52) 6.3 (0.52) 6.3 (0.52) 6.8 (0.50) 6.4 (0.79) 6.0 (0.77) 5.9 (0.78) 6.0 (0.82) 6.5 (0.58)
6.02-6.74 5.92-6.74 5.92-6.74 6.26-7.24 5.85-7.01 5.54-6.46 5.38-6.40 5.20-6.80 5.93-7.07
Multiple responses were allowed from a single participant. SD: Standard deviation. CRS: Confidence rating scale. There were six responses (each with a CRS score = 6.0) endorsing fungal infection as a local factor, which composed 60 percent of the responses in the microbial infection category.
tABLE 4
Etiopathogenetic theories for burning mouth syndrome.
NAtuRE OF HYPOtHEtICAL EtIOPAtHOGENESIS* NO. OF RESPONSES (PERCENtAGE OF tOtAL RESPONSES [N = 33]) 18 (54.5) 5 (15.2) 3 (9.1) 2 (6.1) 5 (15.2) MEAN (SD) CRS SCORE 95 PERCENt CONFIDENCE INtERVAL 5.66-6.46 4.60-6.60 4.68-5.98 NA NA
Neuropathic (Peripheral or Central Neuropathies or Sensitization) Idiopathic or unknown Psychological or Psychosocial Hormonal Other (taste Dysfunction or Dysregulation, Nutritional Deciency, Chronic ulceration) * Multiple responses were allowed from a single participant. SD: Standard deviation. CRS: Confidence rating scale. Hypotheses with a mean CRS score < 6.0. NA: Not applicable.
6.1 (0.87) 5.6 (1.10) 5.3 (0.58) 6.0 (0.0) 6.0 (0.0)
the respondents believed the definition of BMS should be more encompassing, including the entire oral mucosa (n = 10) rather than being restricted to the tongue region (n = 4). Certainly, the presence of a burning sensation in the entire
oral mucosa as compared with that only in the tongue region is more consistent with the clinical findings described in the literature.3,14,16-18 It is possible the majority of respondents did not endorse the inclusion of chronic pain (n = 4) in
JADA 144(10) http://jada.ada.org October 20131139
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL
PRACTICE
the definition of BMS because they considered that an acute onset of an oral burning sensation would be an acceptable criterion to be included in a definition of BMS. Alternatively, they may have believed that the concept of chronic pain, as defined in our study (pain lasting longer than three months), was not consistent with their perception of chronic pain, which possibly involved a longer period (for instance, six months). The nature of these responses may reflect, in part, the nature of the referral network and the delay in patients referral to OM and OFP clinics and programs.33 We did not investigate further the issue of the temporal component regarding chronic pain in this study. To assist the health care practitioner in providing a definitive diagnosis and to assist with consistency among clinical trials, it is important to standardize diagnostic criteria. Overall, participants in this study were confident in their responses in this regard in identifying the key diagnostic criteria, and they reported criteria similar to those published in the literature (Table 2) as being necessary for a definitive diagnosis of BMS.5,34-39 It is of paramount importance for the health care practitioner to understand that BMS is a diagnosis supported by the nature of the symptomatic complaint and the exclusion of various local and systemic factors (Table 3). A detailed discussion of these factors is beyond the scope of this article; however, reviews regarding them appear in the literature.36-41 The results of our study (Table 3) indicate that participants responses were consistent with the current literature regarding the factors that need to be ruled out in the diagnosis of BMS. These were reported with a moderate to high level of confidence (range of mean CRS scores, 5.9-6.8; 95 percent CI, 5.20-7.24). The emphasis on the need to rule out fungal infection may be due to the often associated elevated prevalence of Candida species reported in people with BMS.42-47 The presence of a fungal infectionoften associated with a bitter or metallic taste (a symptom also commonly reported by patients with BMS) and clinical findings of erythema (erythematous candidiasis) or pseudomembranes (pseudomembranous candidiasis) on the oral mucosaoften represents the true source of oral burning pain.45 Patients with these symptoms may report increased pain on eating, likely because of irritation of the mucosa.48,49 The importance of ruling out the presence of a fungal infection cannot be understated and if such an infection is identified, a diagnosis of secondary BMS would be appropriate, with
1140JADA 144(10)http://jada.ada.orgOctober 2013
symptoms managed accordingly for an infection of this type. Before diagnosing BMS, the health care practitioner would be prudent to obtain a thorough history and perform a comprehensive examination involving the use of adjunctive tests, imaging or both when deemed necessary. The use of certain diagnostic tests assists in ruling out factors that may be responsible for the oral burning symptoms, thus distinguishing primary from secondary BMS. Eleven respondents endorsed the measurement of salivary flow rates as an important diagnostic test to determine salivary gland hypofunction or dysfunction. Although there is controversy among clinicians regarding the role of salivary flow in BMS, our data suggest that health care practitioners should incorporate into their diagnostic armamentarium and decisionmaking processes a means of objectively measuring salivary flow rates and methods of ruling out salivary conditions before they provide a definitive diagnosis of BMS. Participants did not indicate the need for use of imaging (dental or medical) in the diagnosis of BMS. This was most likely because we did not provide participants with the option of endorsing this diagnostic test, having deliberately excluded it from the designated response categories (Figure, question 7). There may have been additional diagnostic testing alternatives that we overlooked and did not include in the questionnaire. Furthermore, owing to the nature of the methodology, by which we forced respondents to choose a response from a prescribed menu, we were not able to elicit these other possibilities (we provided no space in which they could record diagnostic tests not present in the menu supplied), thereby introducing the potential for bias to the responses. It is interesting that three participants endorsed the use of soft-tissue biopsy as an important diagnostic test to rule out a diagnosis of BMS. Although there is no established consensus regarding the sampling of soft tissue (for example, to rule out mucosal disease or to observe smallfiber axonal degeneration in the tongue) for a definitive diagnosis of BMS, it is possible these participants responded in this manner because they suspected other soft-tissue diseases (Table 3) causing oral burning sensations that could be misconstrued as BMS. Although the precise etiology and pathophysiology of BMS still is elusive (Table 4), the results of this survey are representative of the current published literature regarding BMS involving both central50-53 and peripheral10,54-56 neuropathic mechanisms. More than one-half
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL
PRACTICE
of the total number (n = 33) of responses (54.5 percent) supported the concept of BMS having a neuropathic etiopathogenesis. Additionally, theories involving psychological and psychosocial issues25,57-63 and hormonal factors3,8,64,65 reported in the literature also were reported by the respondents. Generally, in comparison with other responses regarding the various topics addressed in the study, participants displayed a lower level of confidence in their responses in this category. This may be explained by the lack of strong scientific evidence supporting any one particular theory for the etiopathogenesis of BMS (perhaps with the exception of the neuropathic component). Limitations. This study was limited by being based on self-reports gathered via a mainly open-ended survey. The open-ended format required categorization of responses by the investigators, which may have introduced misclassification bias. Furthermore, because the number of people surveyed was limited by the number of accredited programs (that is, 20 programs), the actual number of participants (n = 13, providing a response rate of 65 percent) was small. Although we did not conduct a formal assessment of each participants knowledge regarding BMS and did not control for variability in participants education, these individuals had considerable clinical education and experience in the diagnosis and management of BMS and were active in caring for patients with these symptoms. The CRS technique allowed us to gauge their level of confidence in their responses. Involving a greater number of participants by expanding the survey beyond North America or recruiting a greater number of experienced clinicians in the disciplines of OM and OFP and applying nominal techniques for consensus building would be of great benefit and should be a consideration in future studies. We did not perform a formal sample-size calculation, as our intent in this study was to capture the universe of all training program directors in North America. Furthermore, the reliability of the CRS technique, owing to its cross-sectional nature, could not be demonstrated in this study.
Conclusions
and management of BMS. We observed similarities among respondents who had a high degree of confidence regarding variables associated with the diagnosis of BMS, such as neuropathic etiopathogenesis and objective assessment of salivary flow. Global standardization of the defining criteria for BMS and necessary diagnostic algorithms can be formulated by convening leaders in the field from different geographical regions. This worthwhile exercise, in addition to following strict methods for the development of a comprehensive consensus statement that expands the current definitions of BMS described earlier in this article, certainly would aid in the advancement of our knowledge of this condition to the benefit of both health care practitioners and the patients they serve. n
Disclosure. None of the authors reported any disclosures. 1. Merskey H, Bogduk N, eds. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Seattle: IASP Press; 1994:74-75. 2. Grinspan D, Fernandez Blanco G, Allevato MA, Stengel FM. Burning mouth syndrome. Int J Dermatol 1995;34(7):483-487. 3. Grushka M. Clinical features of burning mouth syndrome. Oral Surg Oral Med Oral Pathol 1987;63(1):30-36. 4. Lance JW, Olesen J, eds; International Headache Society. The International Classification of Headache Disorders. 2nd ed. Cephalalgia 2004;24(suppl 1):9-160. 5. Grushka M, Epstein JB, Gorsky M. Burning mouth syndrome. Am Fam Physician 2002;65(4):615-620. 6. Klausner JJ. Epidemiology of chronic facial pain: diagnostic usefulness in patient care. JADA 1994;125(12):1604-1611. 7. Grushka M, Sessle BJ. Burning mouth syndrome. Dent Clin North Am 1991;35(1):171-184. 8. Basker RM, Sturdee DW, Davenport JC. Patients with burning mouths: a clinical investigation of causative factors, including the climacteric and diabetes. Br Dent J 1978;145(1):9-16. 9. Zakrzewska JM. The burning mouth syndrome remains an enigma. Pain 1995;62(3):253-257. 10. Lauria G, Majorana A, Borgna M, et al. Trigeminal smallfiber sensory neuropathy causes burning mouth syndrome. Pain 2005;115(3):332-337. 11. Bergdahl M, Bergdahl J. Burning mouth syndrome: prevalence and associated factors. J Oral Pathol Med 1999;28(8):350-354. 12. van der Waal I, ed. The Burning Mouth Syndrome. Copenhagen: Munksgaard; 1990:5-90. 13. Main DM, Basker RM. Patients complaining of a burning mouth: further experience in clinical assessment and management. Br Dent J 1983;154(7):206-211. 14. van der Ploeg HM, van der Wal N, Eijkman MA, van der Waal I. Psychological aspects of patients with burning mouth syndrome. Oral Surg Oral Med Oral Pathol 1987;63(6):664-668. 15. Gorsky M, Silverman S, Chinn H. Clinical characteristics and management outcome in the burning mouth syndrome: an open study of 130 patients. Oral Surg Oral Med Oral Pathol 1991;72(2): 192-195. 16. Gorsky M, Silverman S, Chinn H. Burning mouth syndrome: a review of 98 cases. J Oral Med 1987;42(1):7-9. 17. Svensson P, Bjerring P, Arendt-Nielsen L, Kaaber S. Sensory and pain thresholds to orofacial argon laser stimulation in patients with chronic burning mouth syndrome. Clin J Pain 1993;9(3):207-215. 18. Sardella A, Lodi G, Demarosi F, Tarozzi M, Canegallo L, Carrassi A. Hypericum perforatum extract in burning mouth syndrome: a randomized placebo-controlled study. J Oral Pathol Med 2008;37(7):395-401. 19. Eguia Del Valle A, Aguirre-Urizar JM, Martinez-Conde R, Echebarria-Goikouria MA, Sagasta-Pujana O. Burning mouth syndrome in the Basque Country: a preliminary study of 30 cases. Med Oral 2003;8(2):84-90. 20. Lamey PJ, Lamb AB. Prospective study of aetiological
The findings in this study present an initial exploration of the perceptions of program directors of OM and OFP postgraduate programs in North America regarding diagnostic paradigms, clinical presentations and etiologic and pathophysiological theories regarding BMS. The participants were postgraduate program directors who were clinicians experienced in the diagnosis
JADA 144(10) http://jada.ada.org October 20131141
Copyright 2013 American Dental Association. All Rights Reserved.
CLINICAL
PRACTICE
litus. J Oral Pathol Med 2003;32(1):46-50. 44. Chen Q, Samaranayake LP. Growth of the fungal pathogen Candida in parotid saliva of patients with burning mouth syndrome. Microbios 2000;102(401):45-52. 45. Kurnatowska AJ. Search for correlation between symptoms and signs of changes in the oral mucosa and presence of fungi. Mycoses 2001;44(9-10):379-382. 46. Osaki T, Yoneda K, Yamamoto T, Ueta E, Kimura T. Candidiasis may induce glossodynia without objective manifestation. Am J Med Sci 2000;319(2):100-105. 47. Terai H, Shimahara M. Glossodynia from Candida-associated lesions, burning mouth syndrome, or mixed causes. Pain Med 2010; 11(6):856-860. 48. Terai H, Shimahara M. Tongue pain: burning mouth syndrome vs Candida-associated lesion. Oral Dis 2007;13(4):440-442. 49. Terai H, Shimahara M. Atrophic tongue associated with Candida. J Oral Pathol Med 2005;34(7):397-400. 50. Jaaskelainen SK, Rinne JO, Forssell H, et al. Role of the dopaminergic system in chronic pain: a fluorodopa-PET study. Pain 2001;90(3):257-260. 51. Jaaskelainen SK. Clinical neurophysiology and quantitative sensory testing in the investigation of orofacial pain and sensory function. J Orofac Pain 2004;18(2):85-107. 52. Hagelberg N, Forssell H, Aalto S, et al. Altered dopamine D2 receptor binding in atypical facial pain. Pain 2003;106(1-2):43-48. 53. Forssell H, Jaaskelainen S, Tenovuo O, Hinkka S. Sensory dysfunction in burning mouth syndrome. Pain 2002;99(1-2):41-47. 54. Heckmann SM, Heckmann JG, HiIz MJ, et al. Oral mucosal blood flow in patients with burning mouth syndrome. Pain 2001; 90(3):281-286. 55. Formaker BK, Mott AE, Frank ME. The effects of topical anesthesia on oral burning in burning mouth syndrome. Ann N Y Acad Sci 1998;855:776-780. 56. Nagler RM, Hershkovich O. Sialochemical and gustatory analysis in patients with oral sensory complaints. J Pain 2004;5(1):56-63. 57. Browning S, Hislop S, Scully C, Shirlaw P. The association between burning mouth syndrome and psychosocial disorders. Oral Surg Oral Med Oral Pathol 1987;64(2):171-174. 58. Bogetto F, Maina G, Ferro G, Carbone M, Gandolfo S. Psychiatric comorbidity in patients with burning mouth syndrome. Psychosom Med 1998;60(3):378-385. 59. Zilli C, Brooke RI, Lau CL, Merskey H. Screening for psychiatric illness in patients with oral dysesthesia by means of the General Health Questionnaire: twenty-eight item version (GHQ-28) and the Irritability, Depression and Anxiety Scale (IDA). Oral Surg Oral Med Oral Pathol 1989;67(4):384-389. 60. Rojo L, Silvestre FJ, Bagan JV, De Vicente T. Psychiatric morbidity in burning mouth syndrome: psychiatric interview versus depression and anxiety scales. Oral Surg Oral Med Oral Pathol 1993;75(3):308-311. 61. Al Quran FA. Psychological profile in burning mouth syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97(3): 339-344. 62. Eli I, Baht R, Littner MM, Kleinhauz M. Detection of psychopathologic trends in glossodynia patients. Psychosom Med 1994; 56(5):389-394. 63. Abetz LM, Savage NW. Burning mouth syndrome and psychological disorders. Aust Dent J 2009;54(2):84-93. 64. Santoro V, Caputo G, Peluso F. Clinical and therapeutic experience in twenty eight patients with burning mouth syndrome. Minerva Stomatol 2005;54(9):489-496. 65. Woda A, Dao T, Gremeau-Richard C. Steroid dysregulation and stomatodynia (burning mouth syndrome). J Orofac Pain 2009;23(3):202-210.
factors in burning mouth syndrome. Br Med J (Clin Res Ed) 1988;296(6631):1243-1246. 21. Tammiala-Salonen T, Hiidenkari T, Parvinen T. Burning mouth in a Finnish adult population. Community Dent Oral Epidemiol 1993;21(2):67-71. 22. Bergdahl J, Anneroth G, Stenman E. Description of persons with symptoms presumed to be caused by electricity or visual display units: oral aspects. Scand J Dent Res 1994;102(1):41-45. 23. Glick D, Ben-Aryeh H, Gutman D, Szargel R. Relation between idiopathic glossodynia and salivary flow rate and content. Int J Oral Surg 1976;5(4):161-165. 24. Syrjanen S, Piironen P, Yli-Urpo A. Salivary content of patients with subjective symptoms resembling galvanic pain. Oral Surg Oral Med Oral Pathol 1984;58(4):387-393. 25. Lamey PJ. Burning mouth syndrome. Dermatol Clin 1996; 14(2):339-354. 26. Lamey PJ, Lewis MA. Oral medicine in practice: orofacial pain. Br Dent J 1989;167(11):384-389. 27. Jaaskelainen SK. Pathophysiology of primary burning mouth syndrome. Clin Neurophysiol 2012;123(1):71-77. 28. Gremeau-Richard C, Dubray C, Aublet-Cuvelier B, Ughetto S, Woda A. Effect of lingual nerve block on burning mouth syndrome (stomatodynia): a randomized crossover trial. Pain 2010;149(1): 27-32. 29. Carney M. How commitment and involvement influence the development of strategic consensus in health care organizations: the multidisciplinary approach. J Nurs Manag 2007;15(6):649-658. 30. Cramer CK, Klasser GD, Epstein JB, Sheps SB. The Delphi process in dental research. J Evid Based Dent Pract 2008;8(4): 211-220. 31. Curley SP, Young MJ, Yates JF. Characterizing physicians perceptions of ambiguity. Med Decis Making 1989;9(2):116-124. 32. Walter SD, Mitchell A, Southwell D. Use of certainty of opinion data to enhance clinical decision making. J Clin Epidemiol 1995;48(7):897-902. 33. Klasser GD, Epstein JB, Villines D, Utsman R. Burning mouth syndrome: a challenge for dental practitioners and patients. Gen Dent 2011;59(3):210-220. 34. Woda A, Navez ML, Picard P, Gremeau C, Pichard-Leandri E. A possible therapeutic solution for stomatodynia (burning mouth syndrome). J Orofac Pain 1998;12(4):272-278. 35. Sardella A. An up-to-date view on burning mouth syndrome. Minerva Stomatol 2007;56(6):327-340. 36. Mock D, Chugh D. Burning mouth syndrome. Int J Oral Sci 2010;2(1):1-4. 37. Klasser GD, Fischer DJ, Epstein JB. Burning mouth syndrome: recognition, understanding, and management. Oral Maxillofac Surg Clin North Am 2008;20(2):255-271. 38. Minor JS, Epstein JB. Burning mouth syndrome and secondary oral burning. Otolaryngol Clin North Am 2011;44(1):205-219. 39. Lopez-Jornet P, Camacho-Alonso F, Andujar-Mateos P, SanchezSiles M, Gomez-Garcia F. Burning mouth syndrome: an update. Med Oral Patol Oral Cir Bucal 2010;15(4):e562-e568. 40. Suarez P, Clark GT. Burning mouth syndrome: an update on diagnosis and treatment methods. J Calif Dent Assoc 2006;34(8): 611-622. 41. Balasubramaniam R, Klasser GD, Delcanho R. Separating oral burning from burning mouth syndrome: unravelling a diagnostic enigma. Aust Dent J 2009;54(4):293-299. 42. Samaranayake LP, Lamb AB, Lamey PJ, MacFarlane TW. Oral carriage of Candida species and coliforms in patients with burning mouth syndrome. J Oral Pathol Med 1989;18(4):233-235. 43. Vitkov L, Weitgasser R, Hannig M, Fuchs K, Krautgartner WD. Candida-induced stomatopyrosis and its relation to diabetes mel-
1142JADA 144(10)http://jada.ada.orgOctober 2013
Copyright 2013 American Dental Association. All Rights Reserved.
Potrebbero piacerti anche
- Challenge in DiagnosisDocumento6 pagineChallenge in Diagnosissgoeldoc_550661200Nessuna valutazione finora
- Optimizing Advanced Therapies in Ulcerative Colitis: Is Your Practice Up to Date? A Focus on Clinical Evidence and Guideline RecommendationsDa EverandOptimizing Advanced Therapies in Ulcerative Colitis: Is Your Practice Up to Date? A Focus on Clinical Evidence and Guideline RecommendationsNessuna valutazione finora
- The Accuracy of Clinical Diagnosis of Oral Lesions and Patient-Specific Risk Factors That Affect DiagnosisDocumento6 pagineThe Accuracy of Clinical Diagnosis of Oral Lesions and Patient-Specific Risk Factors That Affect DiagnosisAmeloblogNessuna valutazione finora
- Improving Outcomes in Chronic Obstructive Pulmonary Disease: Optimizing Maintenance Therapy Across Health Care SettingsDa EverandImproving Outcomes in Chronic Obstructive Pulmonary Disease: Optimizing Maintenance Therapy Across Health Care SettingsNessuna valutazione finora
- Topical Application in Burning Mouth Syndrome: SciencedirectDocumento6 pagineTopical Application in Burning Mouth Syndrome: SciencedirectlepouletNessuna valutazione finora
- 31priti EtalDocumento4 pagine31priti EtaleditorijmrhsNessuna valutazione finora
- Contemporary Dental Pharmacology: Evidence-Based ConsiderationsDa EverandContemporary Dental Pharmacology: Evidence-Based ConsiderationsNessuna valutazione finora
- Baccaglini Et Al 2010Documento9 pagineBaccaglini Et Al 2010Amanda AiresNessuna valutazione finora
- Burning Mouth Syndrome An Update 2010Documento7 pagineBurning Mouth Syndrome An Update 2010tele6Nessuna valutazione finora
- Screening For Good Health: The Australian Guide To Health Screening And ImmunisationDa EverandScreening For Good Health: The Australian Guide To Health Screening And ImmunisationNessuna valutazione finora
- BrazJOralSci 2013 Vol12 Issue1 p5 10Documento6 pagineBrazJOralSci 2013 Vol12 Issue1 p5 10Taufiqurrahman Abdul DjabbarNessuna valutazione finora
- Rheumatology CPGDocumento21 pagineRheumatology CPGSanNessuna valutazione finora
- Board Review in Preventive Medicine and Public HealthDa EverandBoard Review in Preventive Medicine and Public HealthValutazione: 3.5 su 5 stelle3.5/5 (2)
- Journal Pone 0091059Documento5 pagineJournal Pone 0091059AgusBhaktiNessuna valutazione finora
- Successful Periodontal Therapy: A Non-Surgical ApproachDa EverandSuccessful Periodontal Therapy: A Non-Surgical ApproachNessuna valutazione finora
- P AcutepainmgmtDocumento5 pagineP AcutepainmgmtLeticia Quiñonez VivasNessuna valutazione finora
- Managing Health in the Genomic Era: A Guide to Family Health History and Disease RiskDa EverandManaging Health in the Genomic Era: A Guide to Family Health History and Disease RiskNessuna valutazione finora
- Risk Assessment and Oral Diagnostics in Clinical DentistryDa EverandRisk Assessment and Oral Diagnostics in Clinical DentistryNessuna valutazione finora
- Evidence Based Practise of Oral MedicineDocumento10 pagineEvidence Based Practise of Oral MedicineshrikantNessuna valutazione finora
- Office Based Anesthesia Complications: Prevention, Recognition and ManagementDa EverandOffice Based Anesthesia Complications: Prevention, Recognition and ManagementGary F. BoulouxNessuna valutazione finora
- Martin-Harris Et Al (2008) MBS Measurement Tool For Swallow Impairment MBSImpDocumento14 pagineMartin-Harris Et Al (2008) MBS Measurement Tool For Swallow Impairment MBSImpinfoNessuna valutazione finora
- Demoares 2019Documento8 pagineDemoares 2019Diego LemurNessuna valutazione finora
- Concise Epidemiologic Principles and Concepts: Guidelines for Clinicians and Biomedical ResearchersDa EverandConcise Epidemiologic Principles and Concepts: Guidelines for Clinicians and Biomedical ResearchersNessuna valutazione finora
- Burning Mouth Syndrome 2013 Dental Clinics of North AmericaDocumento16 pagineBurning Mouth Syndrome 2013 Dental Clinics of North AmericaazizNessuna valutazione finora
- Treating the Dental Patient with a Developmental DisorderDa EverandTreating the Dental Patient with a Developmental DisorderKaren A. RaposaNessuna valutazione finora
- Diagnostic and Microbiological Tools in Oral and Maxillofacial SurgeryDocumento36 pagineDiagnostic and Microbiological Tools in Oral and Maxillofacial SurgeryrajtanniruNessuna valutazione finora
- Uoi 142 FDocumento9 pagineUoi 142 FbkprosthoNessuna valutazione finora
- Articol 1Documento10 pagineArticol 1Airam MNessuna valutazione finora
- BrazilDocumento7 pagineBrazilkarinagitakNessuna valutazione finora
- Targeted Therapy in Translational Cancer ResearchDa EverandTargeted Therapy in Translational Cancer ResearchApostolia-Maria TsimberidouNessuna valutazione finora
- Multi-Dimensionality of Chronic Pain of The Oral Cavity and FaceDocumento10 pagineMulti-Dimensionality of Chronic Pain of The Oral Cavity and FaceTatiana AlapeNessuna valutazione finora
- Validity Two Methods For Assessing Oral Health Status of PopulationsDocumento9 pagineValidity Two Methods For Assessing Oral Health Status of PopulationsSyarifah HaizanNessuna valutazione finora
- EJMCM Volume 7 Issue 8 Pages 3155-3160Documento6 pagineEJMCM Volume 7 Issue 8 Pages 3155-3160Harnoor GhumanNessuna valutazione finora
- Medical HistoryDocumento9 pagineMedical HistoryCristinaNessuna valutazione finora
- Stress and PeriodontitisDocumento10 pagineStress and PeriodontitisTELVA GALVANNessuna valutazione finora
- Clinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareDa EverandClinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareNessuna valutazione finora
- 1 s2.0 S0278239120310582 MainDocumento9 pagine1 s2.0 S0278239120310582 MainCaio GonçalvesNessuna valutazione finora
- Relationship Between Oral Health Literacy and Oral Health StatusDocumento6 pagineRelationship Between Oral Health Literacy and Oral Health StatusRufai HarunaNessuna valutazione finora
- Impact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyDocumento10 pagineImpact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyKornist BufuNessuna valutazione finora
- Your Dental Health Can Save Your Life: Unlocking the Secrets of Oral-Systemic Health: All About DentistryDa EverandYour Dental Health Can Save Your Life: Unlocking the Secrets of Oral-Systemic Health: All About DentistryNessuna valutazione finora
- The Association Between Depression and Anxiety and Use of Oral Health Services and Tooth LossDocumento12 pagineThe Association Between Depression and Anxiety and Use of Oral Health Services and Tooth LossAhmad Ulil AlbabNessuna valutazione finora
- Burning Mouth Syndrome: Etiology, Clinical Presentations, and Treatment AlternativesDocumento6 pagineBurning Mouth Syndrome: Etiology, Clinical Presentations, and Treatment Alternativessilviana yusufNessuna valutazione finora
- Bell 2012Documento13 pagineBell 2012badria bawazirNessuna valutazione finora
- Sci Transl Med 2015 VassyDocumento3 pagineSci Transl Med 2015 VassyJesus NavarroNessuna valutazione finora
- Introduction To The Oral and Maxillofacial Pathology Focus Issue On "Preneoplastic Oral Epithelial Lesions"Documento11 pagineIntroduction To The Oral and Maxillofacial Pathology Focus Issue On "Preneoplastic Oral Epithelial Lesions"jesus ulises estrada cantuNessuna valutazione finora
- Diabetes Mellitus: Impact on Bone, Dental and Musculoskeletal HealthDa EverandDiabetes Mellitus: Impact on Bone, Dental and Musculoskeletal HealthMeng Hee TanNessuna valutazione finora
- IJCDOral Mucositis 2014Documento11 pagineIJCDOral Mucositis 2014Aarya Haridasan NairNessuna valutazione finora
- Martin Harris Et Al 2021 The Modified Barium Swallow Study For Oropharyngeal Dysphagia Recommendations From AnDocumento10 pagineMartin Harris Et Al 2021 The Modified Barium Swallow Study For Oropharyngeal Dysphagia Recommendations From AnCARLA ARACELI GÓMEZNessuna valutazione finora
- Research Project PaperDocumento6 pagineResearch Project Paperapi-369452069Nessuna valutazione finora
- ESMEILI Et Al Dentist Attitudes and Practice Related in The Dental SetingDocumento7 pagineESMEILI Et Al Dentist Attitudes and Practice Related in The Dental SetingJardelSantosNessuna valutazione finora
- IntroductionDocumento11 pagineIntroductionshrikantNessuna valutazione finora
- Sindrome de SjrogenDocumento10 pagineSindrome de SjrogenWesley RodriguesNessuna valutazione finora
- Laryngopharyngeal Reflux Disease: Integrative ApproachesDa EverandLaryngopharyngeal Reflux Disease: Integrative ApproachesNausheen JamalNessuna valutazione finora
- Antibiotic Prophylaxis in Orthognathic Surgery - An Overview of Systematic ReviewsDocumento12 pagineAntibiotic Prophylaxis in Orthognathic Surgery - An Overview of Systematic ReviewsBruno GuardieiroNessuna valutazione finora
- Dental Implants Are Contraindicated In...Documento5 pagineDental Implants Are Contraindicated In...Lia DietrichNessuna valutazione finora
- Evidence-Based Dentistry for the Dental HygienistDa EverandEvidence-Based Dentistry for the Dental HygienistNessuna valutazione finora
- Oral Health-Related Quality of Life, Sense of Coherence and Dental Anxiety: An Epidemiological Cross-Sectional Study of Middle-Aged WomenDocumento6 pagineOral Health-Related Quality of Life, Sense of Coherence and Dental Anxiety: An Epidemiological Cross-Sectional Study of Middle-Aged WomenAlexandru Codrin-IonutNessuna valutazione finora
- Consensus of Prostho On Implants-2017Documento148 pagineConsensus of Prostho On Implants-2017Faheemuddin MuhammadNessuna valutazione finora
- How To Be Happy - WayToGodDocumento65 pagineHow To Be Happy - WayToGodFaheemuddin MuhammadNessuna valutazione finora
- Modular DenturesDocumento4 pagineModular DenturesFaheemuddin MuhammadNessuna valutazione finora
- Let S Be Your Guide-PoundDocumento8 pagineLet S Be Your Guide-PoundFaheemuddin MuhammadNessuna valutazione finora
- RPH Clasp Assembly - A Simple Alternative To Traditional DesignsDocumento3 pagineRPH Clasp Assembly - A Simple Alternative To Traditional DesignsFaheemuddin Muhammad0% (1)
- Rehab of Severley Worn Dentition-Using Fixed and RemovableDocumento0 pagineRehab of Severley Worn Dentition-Using Fixed and RemovableFaheemuddin MuhammadNessuna valutazione finora
- 5trial Visits and DentureDocumento12 pagine5trial Visits and DentureFaheemuddin MuhammadNessuna valutazione finora
- Why-When-How - To Increase Ovd PDFDocumento6 pagineWhy-When-How - To Increase Ovd PDFFaheemuddin MuhammadNessuna valutazione finora
- 10 Steps To Overcome Social Anxiety - Chapter 1Documento22 pagine10 Steps To Overcome Social Anxiety - Chapter 1kapilnabarNessuna valutazione finora
- Submergence of Vital Root For Preservation of Residual RidgeDocumento0 pagineSubmergence of Vital Root For Preservation of Residual RidgeFaheemuddin MuhammadNessuna valutazione finora
- Treatment of Grossly Resorbed Mandibular Ridge 1Documento48 pagineTreatment of Grossly Resorbed Mandibular Ridge 1Faheemuddin Muhammad0% (1)
- Modified Pontic Design For Ridge DefectsDocumento11 pagineModified Pontic Design For Ridge DefectsFaheemuddin MuhammadNessuna valutazione finora
- Ridge Defects and Pontic DesignDocumento14 pagineRidge Defects and Pontic DesignFaheemuddin MuhammadNessuna valutazione finora
- PersonalityDocumento77 paginePersonalityFaheemuddin MuhammadNessuna valutazione finora
- Denture Complaint PDFDocumento10 pagineDenture Complaint PDFFaheemuddin MuhammadNessuna valutazione finora
- Saudi Aramco Medical Services Organization: Plan Helper CalendarDocumento1 paginaSaudi Aramco Medical Services Organization: Plan Helper CalendarFaheemuddin MuhammadNessuna valutazione finora
- Curve of Spee in Prostho-Broadrick Flag TechniqueDocumento5 pagineCurve of Spee in Prostho-Broadrick Flag TechniqueFaheemuddin MuhammadNessuna valutazione finora
- Indian Dental Academy - Theories of Impression Making in Complete Denture Treatment PDFDocumento15 pagineIndian Dental Academy - Theories of Impression Making in Complete Denture Treatment PDFFaheemuddin MuhammadNessuna valutazione finora
- Impression Theories in Complete DenturesDocumento2 pagineImpression Theories in Complete DenturesFaheemuddin MuhammadNessuna valutazione finora
- A Review of The Clinical Significance of The Occlusal Plane Variation and Head PostureDocumento74 pagineA Review of The Clinical Significance of The Occlusal Plane Variation and Head PostureFaheemuddin MuhammadNessuna valutazione finora
- Facebow Calliper ReviewDocumento5 pagineFacebow Calliper ReviewFaheemuddin Muhammad100% (3)
- PaperDocumento4 paginePaperFaheemuddin MuhammadNessuna valutazione finora
- Effective Suction-Imporession For Retentive Mand Dentture PDFDocumento24 pagineEffective Suction-Imporession For Retentive Mand Dentture PDFFaheemuddin MuhammadNessuna valutazione finora
- Effective Suction-Imporession For Retentive Mand Dentture PDFDocumento24 pagineEffective Suction-Imporession For Retentive Mand Dentture PDFFaheemuddin MuhammadNessuna valutazione finora
- Leukemia I To 13Documento252 pagineLeukemia I To 13Anel RedzepiNessuna valutazione finora
- Journal Diabetes MellitusDocumento11 pagineJournal Diabetes Mellitusnabila noorNessuna valutazione finora
- LDN (Low Dose Naltrexone) VariousPatentsandPatentApplicationsDocumento47 pagineLDN (Low Dose Naltrexone) VariousPatentsandPatentApplicationsLynn Allison NelsonNessuna valutazione finora
- BRVO PPT by Dr. Chinmay KharadeDocumento31 pagineBRVO PPT by Dr. Chinmay KharadeChinmay KharadeNessuna valutazione finora
- Insights ImmunotherapyDocumento32 pagineInsights Immunotherapy@yuanNessuna valutazione finora
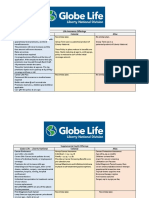
- Life Insurance Offerings Globe Life - Liberty National Colonial AflacDocumento3 pagineLife Insurance Offerings Globe Life - Liberty National Colonial AflacTina Hughes0% (1)
- Assessment of Chest Pain in Primary CareDocumento8 pagineAssessment of Chest Pain in Primary CareVictoria GomezNessuna valutazione finora
- Neuroimaging Clinics of North America 2015 #2 PDFDocumento173 pagineNeuroimaging Clinics of North America 2015 #2 PDFYully gunawan100% (1)
- Radiology 1Documento4 pagineRadiology 1sha100% (3)
- ResearchDocumento26 pagineResearchJhen de Vera83% (12)
- Diabetic Microvascular DiseaseDocumento68 pagineDiabetic Microvascular DiseasePavel GonzálezNessuna valutazione finora
- Androgen Insensitivity Syndrome (AIS)Documento19 pagineAndrogen Insensitivity Syndrome (AIS)arief206_eighteenNessuna valutazione finora
- Heterotopic Bone Formation Final Draft-ZemenfesDocumento5 pagineHeterotopic Bone Formation Final Draft-Zemenfesapi-270166097Nessuna valutazione finora
- Talley Sum UpDocumento51 pagineTalley Sum UpRozana Bawareth100% (1)
- Factors That Affect The Praactice of Exclsuive Breastfeeding Among LactatinDocumento57 pagineFactors That Affect The Praactice of Exclsuive Breastfeeding Among LactatinGideon Owusu Atta100% (1)
- Tilman Family Unfolding Case Cellular Reg Deathdying Osteo NextgenDocumento2 pagineTilman Family Unfolding Case Cellular Reg Deathdying Osteo Nextgenapi-521127784Nessuna valutazione finora
- Improving Outcomes For Breast Cancer SurvivorsDocumento280 pagineImproving Outcomes For Breast Cancer SurvivorsHồ Q. ThuậnNessuna valutazione finora
- Clark Hulda - The Cure For All CancersDocumento662 pagineClark Hulda - The Cure For All Cancersapi-197127630100% (1)
- Cirrhosis Patient Education 2014Documento3 pagineCirrhosis Patient Education 2014Robert G. Gish, MDNessuna valutazione finora
- Common ICD10 Codes For Acupuncture-1Documento1 paginaCommon ICD10 Codes For Acupuncture-1Edwin Alvarez100% (1)
- Nuclear Medicine - Radioactivity For Diagnosis and TherapyDocumento217 pagineNuclear Medicine - Radioactivity For Diagnosis and TherapyPriscila FloresNessuna valutazione finora
- Professor (DR) Rama Kant Biodata Curriculum VitaeDocumento50 pagineProfessor (DR) Rama Kant Biodata Curriculum VitaebobbyramakantNessuna valutazione finora
- Low Back PainDocumento53 pagineLow Back PainSahara EffendyNessuna valutazione finora
- Immunotherapy For Lung CancerDocumento3 pagineImmunotherapy For Lung CancerPongwirat ChantasoontornNessuna valutazione finora
- Research DesignDocumento24 pagineResearch DesignNeza MAe Bulat-ag SalutanNessuna valutazione finora
- Mobiltrans HD-30Documento10 pagineMobiltrans HD-30Sebastian FuentesNessuna valutazione finora
- Hepatitis BDocumento23 pagineHepatitis BAbraham RumayaraNessuna valutazione finora
- Oncology Specialty Pharmaceutical Sales in San Antonio TX Resume Carrie MagnerDocumento2 pagineOncology Specialty Pharmaceutical Sales in San Antonio TX Resume Carrie MagnerCarrieMagnerNessuna valutazione finora
- Phlebotomy Handbook: Blood Collection EssentialsDocumento55 paginePhlebotomy Handbook: Blood Collection EssentialsayooniaNessuna valutazione finora
- Fruitarian Recipe ManualDocumento137 pagineFruitarian Recipe ManualGoodmanBeguel100% (3)