Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Kanker Uterus
Caricato da
Jacob Trisusilo SaleanDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Kanker Uterus
Caricato da
Jacob Trisusilo SaleanCopyright:
Formati disponibili
INFORMATION SHEET
Cancer of the Uterus
This Information Sheet has been written to provide you with information about cancer of the uterus. The Sheet has information about diagnosis, treatment, practical support and the emotional impact of cancer.
Menopause is when a womans periods stop and she is no longer able to have a baby. Her body stops releasing the hormones that cause ovulation and periods.
What is cancer of the uterus?
Cancer of the uterus is the most common gynaecological cancer affecting women. Most cancers of the uterus are cancers of the lining of the uterus (the endometrium). Cancers can also develop in the muscle layers of the uterus.
The uterus
The female reproductive system
EGG OVARY
How common is cancer of the uterus?
UTERUS (womb) FALLOPIAN TUBE LIGAMENTS ENDOMETRIUM (lining of the uterus) CERVIX (neck of the uterus) VAGINA (birth canal) LABIA (inner and outer lips)
In New Zealand, cancer of the uterus is the fifth most common cancer for women. Around 385 women are diagnosed with cancer of the uterus in New Zealand each year. It is more common in women aged over 50.
Causes of cancer of the uterus
The exact cause of cancer of the uterus is not known. Some things seem to put women at more risk: age menopause never having children endometrial hyperplasia (thickening) being overweight high blood pressure diabetes a family history of endometriosis breast or bowel cancer
The uterus (womb) is about the size and shape of an upside-down pear. The uterus sits quite low in the abdomen and is held there lightly by muscle. The uterus is joined to the vagina by the cervix, or neck of the womb. Each month, in women who are able to have children, hormones are released in the body that causes ovulation and periods (menstruation). The lining of the uterus is called the endometrium. The endometrium is made up of several layers that include skin-like cells (surface epithelium), blood vessels, tissue spaces and glands. Each month the endometrium grows thicker to prepare for pregnancy. If a woman does not become pregnant, the top layers of the endometrium are shed and flow out through the vagina in the monthly period.
CANCER SOCIETY OF NEW ZEALAND TE KAHU MATEPUKUPUKU O AOTEAROA
Cancer of the Uterus
being on oestrogen hormone replacement without progesterone being on tamoxifen for treatment of breast cancer.
Biopsy
Biopsy means removing some tissue so it can be looked at under a microscope. The biopsy is taken by stretching the cervix open and inserting a device like a telescope (a hysteroscope).
Cancer of the uterus is not caused by sexual activity and cannot be passed on this way.
Symptoms
The most common symptom is unusual bleeding or a watery, bloody discharge from the vagina. Sometimes, this discharge can be smelly. Other symptoms can include discomfort or pain in the abdomen, difficult or painful urination and pain during sex. Unusual bleeding or discharge can happen before and after menopause. It is usually not due to cancer of the uterus. However, all women with unusual bleeding or discharge should see their doctor for a check-up.
Dilation and curettage (D&C)
Sometimes, most of the uterus lining is scraped out. This is called a D&C. This procedure does not take very long. You will probably have a light general anaesthetic. After, you may have period-like cramps and light bleeding that can last for a few days.
Computerised tomography (CT) scan or magnetic resonance imaging (MRI)
These scans give pictures of the organs and other structures (including any cancers) in your body. They are usually done at a hospital or radiology clinic.
How cancer of the uterus is diagnosed
A number of tests will be performed to help find out if you have cancer of the uterus. You may have some or all of the following tests.
Staging
The tests will show whether you have cancer. They can also show if the cancer has spread to other parts of your body. This helps your doctor stage the disease so they can work out the best treatment for you. Stage 1: The cancer is confined to the uterus. Stage 2: The cancer has spread to the cervix. Stage 3: The cancer has spread beyond the uterus/ cervix to the ovaries, fallopian tubes, vagina or nearby lymph nodes. Stage 4: The cancer has spread further, to the inside of the bladder or rectum, throughout the abdomen or to other body parts.
Physical examination
Your doctor will feel your abdomen to check for swelling. Your doctor may also look at your vagina and cervix using a speculum (a bit like having a Pap test/smear).
Transvaginal ultrasound
In this test, sound waves are used to create a picture of internal organs. A small device called a transducer is put into your vagina. It makes sound waves and receives echoes. A computer makes a picture of the echoes produced when the sound waves meet something dense, like an organ or a tumour. Using the ultrasound, the doctor can look at the size of your ovaries and uterus and the thickness of the endometrium. If there is anything unusual, your doctor will suggest that you have a biopsy.
Types of cancer of the uterus
Adenocarcinoma is a cancer that starts in glandular tissue. Most women (about 85 percent) who are diagnosed with cancer of the uterus have this type of cancer.
CANCER SOCIETY OF NEW ZEALAND TE KAHU MATEPUKUPUKU O AOTEAROA
Cancer of the Uterus
The less common types of cancer of the uterus are adenosquamous carcinoma, papillary serous carcinoma and, rarely, clear cell carcinoma or uterine sarcoma. These cancers are called high-risk cancers because they are more likely to spread.
External radiation treatment
Radiation from a large machine (a linear accelerator machine) is directed at the part of the body needing treatment. For cancer of the uterus, the lower abdominal area and pelvis are treated. The treatment is carefully planned to do as little harm as possible to your normal body tissue. The treatment is usually given daily for five days each week, for several weeks. The length of treatment will depend on the size and type of cancer and on your general health.
Treatment
Cancer of the uterus is often diagnosed early, before it has spread. This means that many women will not need treatment other than surgery. If the cancer has spread beyond the uterus, then radiation treatment, hormone treatment or chemotherapy may be used in addition to surgery.
Chemotherapy
This is the treatment of cancer by drugs. The aim is to destroy all cancer cells while having the least possible effect on normal cells. The drugs are usually given intravenously via a drip. Chemotherapy is a systemic treatment (treating the whole body). There are different combinations of drugs used for cancer of the uterus.
Surgery
Cancer of the uterus is usually treated by removing the uterus. The operation is called a hysterectomy. The fallopian tubes and ovaries will also be removed. If the cancer has spread into the muscle wall of the uterus, this increases the risk of spread to the abdominal lymph nodes. These nodes may also be removed during surgery. If the cancer has spread to the cervix, a small part of the upper vagina and the ligaments supporting the cervix are also removed. The surgery also causes menopause, so you are no longer able to have children.
Hormone treatment
Some cancers of the uterus depend on hormones for growth. This is one of the reasons womens ovaries are removed during surgery.
Radiation treatment
Radiation treatment uses high-energy radiation to destroy cancer cells and may be used instead of or as well as surgery.
Side effects of treatment
Tiredness
Many women find that tiredness is a major problem. Your tiredness may continue for quite awhile even after treatment has finished. Some women find that it takes them up to one to two years to feel really well again.
Internal radiation treatment (Brachytherapy)
Brachytherapy is a type of radiation treatment where the radiation source is placed close to the cancer. The implant is inserted through the vagina using special applicators. Internal radiation treatment can be done in two ways, either continuously for up to thirty hours as a low dose rate treatment, or, more commonly, as high dose rate treatment given as several short treatments.
Menopause
Women who go through menopause as a result of the cancer treatment will have to adjust to the symptoms and body changes caused by no longer producing large amounts of the female hormones. You will need to discuss these with your doctor.
CANCER SOCIETY OF NEW ZEALAND TE KAHU MATEPUKUPUKU O AOTEAROA
Cancer of the Uterus
Bladder problems
Bladder control may change after treatment. Your doctor or nurse will be able to suggest ways to help with bladder control. These may include exercises to strengthen the muscles of your pelvic floor. You may need a referral to a physiotherapist. Some hospitals have continence nurses who can help you with bladder problems.
After treatment
During your treatment you will be monitored frequently. After the completion of your treatment, you may need to have regular check-ups. Your doctor will decide how often you will need these check-ups as everyone is different. Check-ups will gradually become less frequent if you have no further problems. The Cancer Society has other resources you may find useful, such as Cancer of the Uterus: A guide for women, their families and friends and Sexuality and Cancer/Hkakatanga me te Mate Pukupuku. You can receive copies of both booklets at your local Cancer Society by phoning the Cancer Information Helpline 0800 CANCER (226 237). Being diagnosed with cancer can be very distressing. For more information and support phone the Cancer Information Helpline: 0800 CANCER (226 237), or contact your local Cancer Society.
Bowel problems
After surgery some women have problems with their bowels for a while. You may need to make adjustments with your diet or take medication. Talk to your doctor if your bowel problems dont improve.
Lymphoedema
Lymphoedema is swelling of part of the body, usually the legs or the arms. It may occur after treatment for cancer of the uterus if you have had the lymph nodes in your abdomen removed. Removal of the nodes may prevent normal draining of the lymph fluid from the legs. As a result, fluid can build up in one or both legs causing swelling. Discuss with your doctor your potential risk of developing lymphoedema. Symptoms can be managed if treated early.
This information sheet was written in January 2011 by the Cancer Society. The Cancer Societys information sheets are reviewed every three years.
For cancer information and support phone 0800 CANCER (226 237) or go to www.cancernz.org.nz
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Torso GuideDocumento373 pagineTorso GuideMonica PatracutaNessuna valutazione finora
- Chromosome Mitosis Meiosis Review WorksheetDocumento4 pagineChromosome Mitosis Meiosis Review Worksheetapi-331662907Nessuna valutazione finora
- Medical Terminolog1Documento25 pagineMedical Terminolog1Jullia SollezaNessuna valutazione finora
- Genetics of Human Heterotaxias: ReviewDocumento9 pagineGenetics of Human Heterotaxias: ReviewJacob Trisusilo SaleanNessuna valutazione finora
- Magnesium Sulfate For Preeclampsia: PerspectiveDocumento2 pagineMagnesium Sulfate For Preeclampsia: PerspectiveJacob Trisusilo SaleanNessuna valutazione finora
- Hall Ak 1993Documento5 pagineHall Ak 1993Jacob Trisusilo SaleanNessuna valutazione finora
- Armstrong2007 PDFDocumento5 pagineArmstrong2007 PDFJacob Trisusilo SaleanNessuna valutazione finora
- Early and Late Results of The Modified Fontan Operation For Heterotaxy SyndromeDocumento5 pagineEarly and Late Results of The Modified Fontan Operation For Heterotaxy SyndromeJacob Trisusilo SaleanNessuna valutazione finora
- Nitrofurantoin: From Wikipedia, The Free Encyclopedia NitrofurantoinDocumento18 pagineNitrofurantoin: From Wikipedia, The Free Encyclopedia NitrofurantoinJacob Trisusilo SaleanNessuna valutazione finora
- Peripartum HysterectomyDocumento10 paginePeripartum HysterectomyJacob Trisusilo SaleanNessuna valutazione finora
- MITOCHONDRIAL DNA (mtDNA)Documento2 pagineMITOCHONDRIAL DNA (mtDNA)Jacob Trisusilo SaleanNessuna valutazione finora
- Jacob Trisusilo Salean, MD FK Unair - Rsud DR SoetomoDocumento19 pagineJacob Trisusilo Salean, MD FK Unair - Rsud DR SoetomoJacob Trisusilo SaleanNessuna valutazione finora
- Metabolic Changes: Jacob Trisusilo Salean, MDDocumento9 pagineMetabolic Changes: Jacob Trisusilo Salean, MDJacob Trisusilo SaleanNessuna valutazione finora
- Metabolic Changes: Jacob Trisusilo Salean, MDDocumento9 pagineMetabolic Changes: Jacob Trisusilo Salean, MDJacob Trisusilo SaleanNessuna valutazione finora
- Maximum Volume To Which The Lungs Can Be Expanded With The Greatest Possible Inspiratory EffortDocumento6 pagineMaximum Volume To Which The Lungs Can Be Expanded With The Greatest Possible Inspiratory EffortMariz PepitoNessuna valutazione finora
- Abortion - PPT For 2nd MSCDocumento1 paginaAbortion - PPT For 2nd MSCArjesa TakaNessuna valutazione finora
- The Inferior Olivary Nucleus of The Rat A Light and Electron Microscopic StudyDocumento31 pagineThe Inferior Olivary Nucleus of The Rat A Light and Electron Microscopic StudyRafael GutierrezNessuna valutazione finora
- Chapter18 TheCardiovascularSystem TheHeartDocumento7 pagineChapter18 TheCardiovascularSystem TheHeartChelsea CunninghamNessuna valutazione finora
- Infectious Disease NotesDocumento19 pagineInfectious Disease Notesshwetlana rampureNessuna valutazione finora
- Malignant Ovarian TumourDocumento42 pagineMalignant Ovarian TumourJones MarinaNessuna valutazione finora
- SCIENCE 7 Q2 Week 4Documento2 pagineSCIENCE 7 Q2 Week 4Edsel BelbarNessuna valutazione finora
- HYSTERECTOMYDocumento4 pagineHYSTERECTOMYDeepu NairNessuna valutazione finora
- HEMA Lec 03 Bone Marrow Collection Lymphoid Organs 1Documento9 pagineHEMA Lec 03 Bone Marrow Collection Lymphoid Organs 1Patrick AbellaNessuna valutazione finora
- Branchial Cleft CystsDocumento8 pagineBranchial Cleft CystsHere LeafsNessuna valutazione finora
- HeartDocumento28 pagineHeartZahidKhanNessuna valutazione finora
- Bavituximab MOA BrochureDocumento3 pagineBavituximab MOA BrochureinternetforumuserNessuna valutazione finora
- Ann. Din. Biochem.: Regulation of Calcium MetabolismDocumento22 pagineAnn. Din. Biochem.: Regulation of Calcium MetabolismAzmi FarhadiNessuna valutazione finora
- Model Answers: Chapter 13 Homeostasis and The Human Urinary SystemDocumento3 pagineModel Answers: Chapter 13 Homeostasis and The Human Urinary Systemsyed aliNessuna valutazione finora
- MRI TextbookRecommendationsDocumento1 paginaMRI TextbookRecommendationsChris SacconeNessuna valutazione finora
- Immunologic DisordersDocumento156 pagineImmunologic DisordersManny HermosaNessuna valutazione finora
- Circulatory System of CockroachDocumento18 pagineCirculatory System of Cockroachyayeg rajaNessuna valutazione finora
- DX Procedure & Nursing ResponsibilityDocumento3 pagineDX Procedure & Nursing ResponsibilityGwyneth SantiagoNessuna valutazione finora
- Chapter 1 Introduction To Human AnatomyDocumento39 pagineChapter 1 Introduction To Human AnatomyPramisshila Nurnatasha Abd SamatNessuna valutazione finora
- Pex 02 01Documento5 paginePex 02 01auliaNessuna valutazione finora
- TNCT Q4 Module5Documento22 pagineTNCT Q4 Module5Glenn Mendez100% (1)
- Cysts of The Oral Cavity-3Documento33 pagineCysts of The Oral Cavity-3Mostafa El GendyNessuna valutazione finora
- Year 10 DPP Biology Term 3 Exam RevisionDocumento8 pagineYear 10 DPP Biology Term 3 Exam RevisionPoojit VenugopalaNessuna valutazione finora
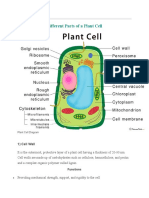
- Cell PlantDocumento7 pagineCell PlantEbiz MarkNessuna valutazione finora
- Electrode Placement enDocumento40 pagineElectrode Placement enRichard HarrisNessuna valutazione finora
- Cell Poster Diagram CADocumento2 pagineCell Poster Diagram CARando AyNessuna valutazione finora
- DIPASREE - ROYCHOWDHURYAnomalous Secondary Growth in Boerhaavia Stem2020!04!03Anomalous Secondary Growth in Boerhaavia StemDocumento2 pagineDIPASREE - ROYCHOWDHURYAnomalous Secondary Growth in Boerhaavia Stem2020!04!03Anomalous Secondary Growth in Boerhaavia StemAkshay KannanNessuna valutazione finora