Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ajustes Posturales Anticipatorios y Compensatorios en PC
Caricato da
Pamela DíazDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Ajustes Posturales Anticipatorios y Compensatorios en PC
Caricato da
Pamela DíazCopyright:
Formati disponibili
Human Movement Science 30 (2011) 648657
Contents lists available at ScienceDirect
Human Movement Science
journal homepage: www.elsevier.com/locate/humov
Anticipatory and compensatory postural adjustments in sitting in children with cerebral palsy
Aline Bigongiari a, Flvia de Andrade e Souza a, Patrcia Martins Franciulli a, Semaan El Razi Neto a, Rubens Correa Araujo a, Luis Mochizuki b,
a b
Laboratory of Biomechanics, University So Judas Tadeu, Brazil Escola de Artes, Cincias, e Humanidades, Universidade de Sao Paulo, Avenida Arlindo Btio, 1000 So Paulo, SP 03828 000, Brazil
a r t i c l e
i n f o
a b s t r a c t
The aim of this study was to examine postural control in children with cerebral palsy performing a bilateral shoulder exion to grasp a ball from a sitting posture. The participants were 12 typically developing children (control) without cerebral palsy and 12 children with cerebral palsy (CP). We analyzed the effect of ball mass (1 kg and 0.18 kg), postural adjustment (anticipatory, APA, and compensatory, CPA), and groups (control and CP) on the electrical activity of shoulder and trunk muscles with surface electromyography (EMG). Greater mean iEMG was seen in CPA, with heavy ball, and for posterior trunk muscles (p < .05). The children with CP presented the highest EMG and level of co-activation (p < .05). Linear regression indicated a positive relationship between EMG and aging for the control group, whereas that relationship was negative for participants with CP. We suggest that the main postural control strategy in children is based on corrections after the beginning of the movement. The linear relationship between EMG and aging suggests that postural control development is affected by central nervous disease which may lead to an increase in muscle co-activation. 2011 Elsevier B.V. All rights reserved.
Article history: Available online 31 March 2011 PsycINFO classication: 2520 3297 Keywords: Anticipatory postural adjustment Cerebral palsy Postural control
1. Introduction Adequate postural control is necessary for an appropriate voluntary movement performance (Liao, Yang, Hsu, Chan, & Wei, 2003; Rose et al., 2002; Woollacott et al., 1998). Lobo and Galloway (2008)
Corresponding author.
E-mail address: alinebigongiari@usp.br (L. Mochizuki). 0167-9457/$ - see front matter 2011 Elsevier B.V. All rights reserved. doi:10.1016/j.humov.2010.11.006
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
649
showed that infants with postural experience likely had improved head and trunk strength and control for visual exploration and reaching, had more appropriate muscle responses to maintain balance, and had increased perceptual-motor experiences in a variety of positions. Therefore, these authors considered factors both internal (age and development) and external (environment) to the infants. However, different problems affect movement performance, such as motor disorders (Levin, Cirstea, Archambault, Son, & Roby-Brami, 2002; Mewasinh et al., 2002) or neuromuscular injuries (Rose et al., 2002; Woollacott; 2002). Cerebral palsy (CP) is a non-progressive motor disorder caused by development damage or an immature brain which leads to impaired postural control (Gianni, 2005; Rose et al., 2002). Several neural factors constrain balance control in children with CP: spasticity, hyperactive stretch reexes, and problems with muscle coordination including poorly organized postural responses and increased muscle coactivation at individual joints (Woollacott et al., 1998). Dynamic balance control includes proactive or anticipatory postural adjustments (APA), and reactive or compensatory postural adjustments (CPA) to enhance balance (Aruin, 2003; Massion, 1998). By APA we mean movements that reduce the effects of a perturbation to posture caused by voluntary control. On the other hand, CPA are reactive responses to postural perturbations. Since CP children may have signicant balance problems, an evaluation of both APA and CPA seems warranted. Several changes occur in the postural control of children with CP. During reaching, children with CP show direction-specic postural adjustments (Hadders-Algra, van der Fits, Stremmelaar, & Touwen, 1999; van der Heide et al., 2004) and during standing they show abnormalities in muscle timing and increased levels of coactivation (Brogren, Hadders-Algra, & Forssberg, 1996; Woollacott et al., 1998). Postural control develops differently in children with and without CP. While standing balance usually improves with age in typically developing children, it does not improve with age in children with CP (Rose et al., 2002; Shumway-Cook, Hutchinson, Kartin, Price, & Woollacott, 2003). The APA during reaching in sitting posture in typically developing children is consistently present from 15 months of age onwards (van der Fits, Otten, Klip, van Eykern, & Hadders-Algra, 1999). However, in children with CP, the APA during reaching while sitting is variable in its development (Rose et al., 2002; Woollacott et al., 1998). Both children (without and with CP) show a large variation in the neck and trunk muscles activation latencies (van der Heide et al., 2004). Children with moderate and serious outcomes due to CP show visible decits in postural control. Their motor and functional capacities need to be improved for the maintenance of standing and sitting position through the head and trunk stabilization and alignment (Liao, Yang, Hsu, Chan, & Wei, 2003). The variety of results across different experiments and the lack of postural studies in sitting position take us to this question: how do central motor disorders affect the postural adjustments? In order to answer this question, the main purpose of this study was to investigate the postural adjustments in children with CP performing shoulder exion to grasp a ball. We compared the postural adjustments across different groups and task conditions to test if the importance of anticipatory and compensatory adjustments performed by children with and without CP to postural control are different. We hypothesized that there would be a difference in the anticipatory and compensatory postural adjustments between the children with CP and typically developing children. The children with CP have less anticipatory and greater compensatory adjustments.
2. Methods 2.1. Participants The participants in this study were 12 typically developing children (4 boys and 8 girls) and 12 spastic diplegic children (6 boys and 6 girls). Their main characteristics are presented in Table 1. The typically developing children were recruited from physiotherapy undergraduate students relatives who were without any physical or neurological problems and they served as control group. The spastic diplegic children served as the experimental group (CP). The children with CP were recruited from the physiotherapy service of the University. All parents gave informed consent according to the procedures approved by the Ofce for Regulatory Compliance of the Institution.
650
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
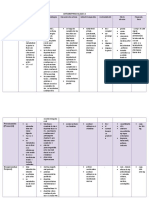
Table 1 The description of the main characteristics of the participants (GMFCS scale, sex, age, weight and height), divided into control group (children without CP) and children with CP. Participants 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Sex Girl Boy Boy Boy Girl Boy Girl Girl Boy Girl Boy Girl Boy Girl Girl Girl Boy Girl Girl Boy Boy Girl Girl Girl Group CP CP CP CP CP CP CP CP CP CP CP CP Control Control Control Control Control Control Control Control Control Control Control Control GMFCS III I II III II III III I I I III III Age (year) 7 8 8 8 8 9 9 9 9 10 11 11 7 8 8 9 9 9 10 10 10 11 11 11 Weight (kg) 20.4 21.5 22.0 25.2 22.8 28.4 28.5 30.7 27.6 29.9 28.8 41.0 24.0 25.2 25.9 28.2 29.0 30.1 31.6 34.5 36.2 37.3 38.3 40.5 Height (m) 1.11 1.19 1.19 1.20 1.22 1.29 1.26 1.42 1.30 1.33 1.26 1.40 1.23 1.25 1.25 1.29 1.33 1.36 1.38 1.39 1.42 1.45 1.44 1.46
The inclusion criteria for the control group were: (1) to be between 7 and 11 years old and (2) to present typical physical and motor developing condition. The exclusion criteria for the control group were: (1) to have any physical, motor and cognitive impairment and (2) to be unable to understand the instructions to perform the motor task. On the other hand, to be included in the experimental group, children with CP had to be able to stand in the sitting position by itself and to grasp a throwing ball with their both hands and to be between 7 and 11 years old. The exclusion criteria for the experimental group were: to be unable to understand the instructions to perform the motor task; be receiving Botox treatments up to six months ago, and to be unable to sit and stand quiet without any external assistance.
2.2. Procedure One senior physiotherapist performed the GMFCS test at the CP children group. When she performed the tests she was not aware of the hypothesis of this study. For the experimental trials, the participants sat on a stable bed without back or foot support. They were instructed to grasp a thrown ball with both hands. The participants were instructed to hold their arms at their sides. After a warning signal, they were told to raise their arms and grasp the ball with their arms parallel to the oor. After the children had grasped the ball, the raw signal was observed and only the signal, that demonstrated APA, was recorded. Two criteria were important: 1 to grasp a thrown ball and 2 to show APA. The order of the ball conditions was randomized across participants. In each ball condition, 10 practice trials were given to familiarize the children with the task. The 10 practice trials were enough for all participants. Some children had learned before to complete 10 trials, but additional trials were not necessary for any of the participants. For each ball (light and heavy), 10 successful measurement trials were performed (van der Heide, Otten, van Eykern, & Hadders-Algra, 2003; Morris & Allison, 2006; Yiou, Schneider, & Roussel, 2007) and recorded. In both ball conditions, the children were aware of the mass of the ball.
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
651
2.3. Data processing and statistical analysis The electromyographic signals (EMG) were recorded with bipolar surface electrodes (Myosystem 1400, Noraxon Inc., Scottsdale, Arizona, USA) on the following muscles: anterior deltoid (DE), biceps brachii (BB), sternocleidomastoid (SC), neck extensor (NE level C7), thoracic extensor (TE level T10), lumbar extensor (LE level L3), and rectus abdominis (RA). The beginning of movement was detected with a bi-dimensional exible electrogoniometer (Noraxon Inc., Scottsdale, Arizona, USA). The axes of the electrogoniometer were aligned to the center of shoulder rotation. Two balls of the same size were thrown to the children (light: 0.180 kg and heavy: 1 kg). All data were collected on a microcomputer via an A/D converter. Data sampling was accomplished at 1000 Hz. The EMG data were amplied 1000 times and band-pass ltered (10200 Hz) using a 4th order Butterworth lter. The angular position data were low-pass ltered (20 Hz) using a 4th order Butterworth lter. The ltered EMG was then full-wave rectied. The integrated signals (iEMG) were calculated for each task and muscle at two time windows. For APA, the window began 200 ms before the initiation of movement to 50 ms after the initiation of movement (see Fig. 1). For CPA, the integration window ranged from 50 ms after movement initiation to 300 ms after movement initiation. iEMG ranging from 400 ms before movement initiation to 300 ms before movement initiation was referred to as pre-APA. The times dening both APA and CPA were derived from previous literature (Shiratori & Latash, 2000). The iEMG during the pre-APA period was subtracted from the APA period to remove the baseline iEMG activity. We normalized iEMG of each muscle by its maximum value and classied it into three EMG levels of activity: mild, from 0% to 30%; moderate, from 30% to 70%; and strong, from 70 to 100%. 2.4. Variables For the description and analysis of postural control of the control and experimental groups, we used the following variables: (a) The intensity of muscular activation: the iEMG was calculated during the APA and the CPA for the selected muscles. (b) The degree of reciprocal inhibition: the iEMG activity of the dorsal muscles (LE, NE) was subtracted from the ventral muscles (RA, SC) to determine the degree of reciprocal inhibition (R).
Fig. 1. Schematic indicating the denitions for anticipatory (APA) and compensatory (CPA) postural adjustments. The top graph indicates the angular position of the shoulder while the bottom graph illustrates a typical EMG time pattern. The dot lines show the time limits of APA, CPA and pre-APA.
652
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
(c) The amount of co-contraction: the iEMG activity of the muscle pairs RA-LE and SE-NE were added to represent the amount of co-contraction (C). The children with CP were classied within Gross Motor Function Classication System for Cerebral Palsy (GMFCS) (Palisano et al., 1997). Each individual result is presented in Table 1. This scale is applied to classify the participants functional abilities (level I: participant walks without restrictions and has restriction to perform more advanced gross motor skills; level II: participant walks without assistive devices and has limitation to walk outside; and level III: participant needs assistive mobility devices to walk and has constraints to walk outside). Multiple Analysis of Variance (MANOVA) was applied to verify the effect of postural adjustment (APA and CPA), group (control and CP), ball (light and heavy) and muscle (DE, SC, NE, TE, LE, BB, and RA). Tukeys HSD was applied for post-hoc comparisons where appropriate. Multiple linear regression analysis was applied to test the relationship between the iEMG of the trunk muscles and aging. Lastly, multiple linear regression analysis was performed between GMFCS scale and postural adjustment (APA and CPA). 3. Results iEMG amplitude during APA increased compared to the resting level in four muscles (DE, SC, TE, and LE) during both the light and heavy ball conditions in both the control and CP groups (Table 2). The rectus abdominus (RA) decreased compared to the resting level in the light ball condition of the control group and in both ball conditions of the CP group. Both the BB and the NE muscles decreased in the light ball condition of the control group and heavy ball condition of the CP group respectively. The magnitudes of the iEMG for postural adjustment, group, ball and muscles are presented in Fig. 2. The MANOVA on these effects indicated that there were no signicant interactions in this analysis. We found that all factors affected iEMG (p < .001). That is, the iEMG magnitude was greater for the CPA than the APA, the CP group than the control and the heavy ball than the light ball. The post-hoc analysis revealed the highest iEMG for SC, TE, and LE muscles (p < .001). The mean values of both the co-contraction (C) and reciprocal inhibition (R) indices are presented in Table 3. For both indices, there were no signicant interactions between postural adjustment, group and ball. However, there was a signicant difference between the main effects of postural adjustment (APA versus CPA), group (control versus CP), and ball (light versus heavy) (p < .0001) for both the neck and trunk muscles. The R index was signicantly different between groups (control and CP) (p < .001) for both the trunk and the neck. The highest R index was found for the trunk muscles and for the control group versus the CP group. MANOVA was used to verify the effect of postural adjustment (APA and CPA), ball (light and heavy), group (control and CP), and EMG activity level (mild, moderate, and strong) on frequency distribution
Table 2 Anticipatory postural adjustment (APA) across muscles (deltoid, sternocleidomastoid, neck extensor, thoracal extensor, lumbar extensor, biceps brachii and rectus abdominis) for the control and cerebral palsy groups during catching a light or heavy ball. Cross (+) means that activity during APA is higher than pre-APA, while trace () means that activity during APA is smaller than pre-APA. Type of anticipatory postural adjustment Group Ball mass Muscle Deltoid Sternocleidomastoid Neck extensor Thoracal extensor Lumbar extensor Biceps brachii Rectus abdominis Control group Light + + + + + Heavy + + + + + + + Cerebral palsy group Light + + + + + + Heavy + + + + +
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
653
Fig. 2. Average iEMG (SD) during anticipatory (APA) and compensatory (CPA) postural adjustments for the muscles of the (a) control and (b) cerebral palsy groups when catching a light or heavy ball. The muscles were anterior deltoid (DE), biceps brachii (BB), sternocleidomastoid (SC), neck extensor (NE), thoracic extensor (TE), lumbar extensor (LE), and rectus abdominis (RA).
Table 3 Neck and trunk co-contraction (C) and reciprocal inhabitation (R) indexes during anticipatory (APA) and compensatory (CPA) postural adjustments for the control and cerebral palsy groups when catching a light or heavy ball. iEMG (% mean) Cerebral palsy APA Light Neck Trunk C-index R-index C-index R-index 38.0 11 5.3 4.2 19.0 9.6 18.3 9.1 Heavy 42.8 10 5.8 4.9 44.9 20 10.6 10 CPA Light 51.9 12 9.3 8.9 58.2 18 13.7 10 Heavy 54.0 10 8.0 6.6 56.9 17 12.2 10 Control APA Light 41.0 12 6.6 4.4 47.0 23 10.6 11 Heavy 40.1 12 7.3 6.2 44.8 21 11.5 9.3 CPA Light 53.4 10 6.7 5.4 52.5 17 10.1 10 Heavy 51.5 10 7.7 7.1 56.2 18 12.6 9.1
of postural responses. This analysis was based on data presented in Fig. 3. There were signicant interactions between muscle activity level and the effects of postural adjustment, ball and group (p < .0001). For mild activity, responses were more frequently with heavy ball, and for control group. For moderate activity, responses were more frequent during CPA and with light ball. For strong activity, responses were more frequent during CPA with light ball and for the CP group. The post hoc analysis indicated that mild activity was the most frequent response while the least frequent response was at the strong level (p < .0001). A multiple linear regression analysis was used to verify the relationship between muscular activity and aging (Fig. 4). For the control group, a positive linear relationship between iEMG and aging during APA was found (R2 = .28, p = .001) and a negative relationship during CPA (R2 = .14, p = .02). For the CP group, a negative relationship between iEMG and aging during APA and CPA (R2 = .39, p = .0001).
654
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
Fig. 3. The muscle activity level during postural adjustments and groups. The muscle activity is presented according to its frequency distribution of iEMG divided into three levels (030%, 3070%, and 70100%) during (a) compensatory (CPA) and (b) anticipatory (APA) postural adjustments for the control and cerebral palsy groups during catching a light or heavy ball.
The GMFCS test resulted in four children (33.3%) classied at level I, two children (16.6%) at level II, and six children (50%) were classied at level III. A regression analysis indicated no relationship between functional ability and APA (R = .04, p = .87) or APC (R = .21, p = .46). 4. Discussion The purpose of this study was to compare anticipatory and compensatory postural adjustments in individuals with CP and typically developing children. We hypothesized that children with CP would have less anticipatory and greater compensatory adjustments than healthy children. In general, we found differences in muscle activity to support our hypothesis. Typically developing children and children with CP raised their arms to catch a ball using different muscular patterns of muscle activation. Mostly, muscle activity increased before this movement for typically developing children (i.e., APA); however, some muscles were tuned differently across group and task conditions. Typically developing children, as well as young adults, show changes in postural adjustments with additional load (Hadders-Algra et al., 1999; Witherington et al., 2002), leading to an increased APA intensity (Bouisset, Richardson, & Zattara, 2000; Vernazza-Martin, Martin, Cincera, & Pedotti, 1999). To catch a more massive ball, our typically developing children increased the activity of all muscles while children with CP tuned some muscles (DE, SC, TE, LE, and BB) and relaxed others (NE and RA). To achieve the postural goal (control of balance) during a motor task, different strategies are applied prior to and/or after the initiation of the movement. The muscle activities are constrained by synergies that help to increase or decrease the task success; therefore, we can identify good or bad synergies. How muscles are switched on or off to accomplish the task can help us to reveal the
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
655
Fig. 4. The main results of multiple linear regression analysis of iEMG of all muscles (deltoid, biceps brachii, sternocleidomastoid, neck extensor, thoracal extensor, lumbar extensor, and rectus abdominis), during anticipatory (APA) and compensatory (CPA) postural adjustments for the control and cerebral palsy groups during catching a ball.
postural synergy organization. Considering all task repetitions, the children with CP and typically developing children activated their muscles during APA. The stronger activations were often observed after the initiation of movement when the mass ball was heavy for the children with CP while typically developing children activated their muscles at mild level. Thus, there were different uses of synergies leading to different patterns of activation between groups. We found that children with CP presented stronger single and agonist/antagonist muscle activations than typically developing children. The lack of supraspinal modulation on tonic stretch reex thresholds at segmental levels, spasticity, or central nervous system (CNS) immaturity (Brogren et al., 1996; van der Fits and Hadders-Algra; 1998) are common in children with CP and contribute to strong single muscle responses. As a consequence, those neural problems lead to poorly organized postural responses, including increased muscle coactivation at individual joints and movement restrictions (Aruin & Almeida, 1997; Brogren et al., 1996; Dan et al., 2000, Hadders-Algra et al., 1999; Levin et al., 2002; Woollacott, 2002; Woollacott et al., 1998). Delays in the development of specic neural or musculoskeletal subsystem and sensorial decits contribute to balance difculties (Hadders-Algra et al., 1999; van der Heide et al., 2004; Woollacott, 2002). Our results did not show a linear relationship between GMFCS scale and postural adjustment across participants. The lack of a relationship between functional levels and postural control suggests that more specic scales to describe balance and upper limb movements are necessary. After all, qualitative analyses of standing and gait cannot account for other motor abilities. Maturity and motor experiences improve motor development (Hadders-Algra et al., 1999) and both processes are improved by aging. In fact, postural adjustments change as people get older (Grasso, Assaiante, Prvost, & Berthoz, 1998; Hay & Redon, 1999; Mercer & Sahrmann, 1997; van der Fits & Hadders-Algra, 1998; Woollacott et al., 1998; Witherington et al., 2002). This occurs because participants learn how to use postural adjustments to better achieve the task goals or to avoid postural risks associated with movement perturbation. In this sense, infants develop APA while they learn to get up, stand up, and walk (van der Fits et al., 1999; Witherington et al., 2002). In our results, for typically
656
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
developing children, regression analysis, although producing weak correlations, seemed to indicate two postural processes with aging: APA increases, while CPA decreases. For children with CP, aging affects postural processes in a different fashion. Although children with CP had more difculty in grasping the thrown ball, they also caught it. Contrary to typically developing children, the children with CP decreased both APA and CPA with aging. Facing the task, both feedforward and feedback control may be weakened due to aging and the progression of the disease. Although no specic-direction muscle activation has been observed in children with CP, probably because only severe children with CP show changes in the specic-direction postural responses (Brogren et al., 1996; van der Fits & Hadders-Algra, 1998; van der Heide et al., 2003). In addition, the main problem in a CNS lesion is the ne modulation (temporal and tonic patterns) of postural responses (van der Heide et al., 2004) which may have contributed to the decline in both APA and CPA activities across ages in this study. In conclusion, typically developing children and children with CP showed different patterns of postural activity across load perturbation. As children with CP performed the task with lower muscle activity, efforts should be made to guarantee that such condition does not lead to the increase of postural instability and unbalance situations in daily life activities. We believe the relationship between postural control and development in children with cerebral palsy shows us that on-going functional activity training and neuromuscular rehabilitation are necessary to deal with cerebral palsy impairment. However, to improve postural and motor control, multisensory stimulation tasks should be encouraged during rehabilitation programs. We only showed how the intensity of muscle changes across the experimental conditions. Further analysis is necessary to verify whether muscular latency is different between children with and without CP. This information may be interesting in view of the discussion about how those children coordinates several muscles to perform a postural and movement task. Acknowledgments The authors gracefully acknowledge Joseph Hamill for his invaluable suggestions and discussions and the anonymous reviewers for their helpful comments. References
Aruin, A. S. (2003). The effect of changes in the body conguration on anticipatory postural adjustments. Motor Control, 7, 264277. Aruin, A. S., & Almeida, G. L. (1997). A co-activation strategy in anticipatory postural adjustment in persons with Down syndrome. Motor Control, 1, 178191. Bouisset, S., Richardson, J., & Zattara, M. (2000). Do anticipatory postural adjustment occur in different segments of the postural chain follow the same organizational rule for different task movement velocities, independently of the inertial load value? Experimental Brain Research, 132, 7986. Brogren, E., Hadders-Algra, M., & Forssberg, H. (1996). Postural control in children with spastic diplegia: Muscle activity during perturbations in sitting. Developmental Medicine and Child Neurology, 38, 379388. Dan, B., Bouillot, E., Bengoetxea, A., Noel, P., Kanh, A., & Cheron, G. (2000). Head stability during whole body movements in spastic diplegia. Brain & Development, 22, 99101. Gianni, M. A. C. (2005). Paralisia cerebral. Aspectos clnicos. In E. W. Moura & P. A. C. Silva (Eds.), Aspectos clnicos e prticos da reabilitao (pp. 1325). Artes medicas. Grasso, R., Assaiante, C., Prvost, P., & Berthoz, A. (1998). Development of anticipatory orienting strategies during locomotor tasks in children. Neuroscience and Biobehavioral Reviews, 22, 533539. Hadders-Algra, M., van der Fits, I. B. M., Stremmelaar, E. F., & Touwen, B. C. L. (1999). Development of postural adjustments during reaching in infants with CP. Developmental Medicine & Child Neurology, 41, 766776. Hay, L., & Redon, C. (1999). Feedforward versus feedback control in children and adults subjected to a postural disturbance. Experimental Brain Research, 125, 153162. Levin, M. F., Cirstea, C. M., Archambault, P., Son, F., & Roby-Brami, A. (2002). Impairment and compensation of reaching in patients with stroke and cerebral palsy. In M. L. Latash (Ed.), Progress in motor control (pp. 103122). Champaign-Urbana, IL: Human Kinetics. Liao, S. F., Yang, T. F., Hsu, T. C., Chan, R. C., & Wei, T. S. (2003). Differences in seated postural control in children with spastic cerebral palsy and children who are typically developing. American Journal of Physical Medicine and Rehabilitation, 82, 622626. Lobo, M. A., & Galloway, J. C. (2008). Postural and object-oriented experiences advance early reaching, object exploration, and means-end behavior. Child Development, 79, 18691890. Massion, J. (1998). Postural control system in developmental perspective. Neuroscience and Biobehavioral Reviews, 22, 465472.
A. Bigongiari et al. / Human Movement Science 30 (2011) 648657
657
Mercer, V. S., & Sahrmann, S. A. (1997). Age group differences in postural adjustments associated with a stepping task. Journal of Motor Behavior, 29, 243246. Mewasinh, L. D., Demil, A., Christiaens, F. J. C., Missa, A. M., Cheron, G., & Dan, B. (2002). Motor strategies in standing up in leukomalacic spastic diplegia. Brain and Development, 24, 291295. Morris, S. L., & Allison, G. T. (2006). Effects of abdominal muscle fatigue on anticipatory postural adjustments associated with arm raising. Gait and Posture, 24, 342348. Palisano, R., Rosenbaum, P., Walter, S., Russell, D., Wood, E., & Galuppi, B. (1997). Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology, 39, 214223. Rose, J., Wolff, D. R., Jones, V. K., Bloch, D. A., Oehlert, J. W., & Gamble, J. G. (2002). Postural balance in children with cerebral palsy. Developmental Medicine & Child Neurology, 44, 5863. Shiratori, T., & Latash, M. (2000). The roles of proximal and distal muscles in anticipatory postural adjustments under asymmetrical perturbations and during standing on rollerskates. Clinical Neurophysiology, 111, 613623. Shumway-Cook, A., Hutchinson, S., Kartin, D., Price, R., & Woollacott, M. (2003). Effect of balance training on recovery of stability in children with cerebral palsy. Developmental Medicine & Child Neurology, 45, 592602. van der Fits, I. B. M., & Hadders-Algra, M. (1998). The development of postural response patterns during reaching in healthy infants. Neuroscience and Biobehavioral Reviews, 22, 521526. van der Fits, I. B. M., Otten, E., Klip, A. W. J., van Eykern, L. A., & Hadders-Algra, M. (1999). The development of postural adjustment during reaching in 6- to 18month-old infants. Experimental Brain Research, 126, 517528. van der Heide, J. C., Fock, J. M., Otten, E., Stremmelaar, E., van Eykern, L. A., & Hadders-Algra, M. (2004). Postural control during reaching in preterm children with cerebral palsy. Developmental Medicine & Child Neurology, 46, 253266. van der Heide, J. C., Otten, E., van Eykern, L. A., & Hadders-Algra, M. (2003). Development of postural adjustments during reaching in sitting children. Experimental Brain Research, 151, 3245. Vernazza-Martin, S., Martin, N., Cincera, M., & Pedotti, A. (1999). Arm raising in humans under loaded vs. unloaded and bipedal vs. unipedal conditions. Brain Research, 846, 1222. Witherington, D. C., Hofsten, C. V., Rosander, K., Robinette, A., Woollacott, M. H., & Bertenthal, B. I. (2002). The development of anticipatory postural adjustments in infancy. Infancy, 3, 495517. Woollacott, M. H. (2002). Development of balance control in typically developing children and children with cerebral palsy. In M. L. Latash (Ed.), Progress in motor control (pp. 83101). Champaign-Urbana, IL: Human Kinetics. Woollacott, M. H., Burtner, P., Jensen, J., Jasiewicz, J., Roncesvalles, N., & Sveistrup, H. (1998). Development of postural responses during standing in healthy children and children with spastic diplegia. Neuroscience and Biobehavioral Reviews, 22, 583589. Yiou, E., Schneider, C., & Roussel, D. (2007). Coordination of rapid stepping with arm pointing: Anticipatory changes and step adaption. Human Movement Science, 26, 357375.
Potrebbero piacerti anche
- Recent Research in Nutrition and Growth: 89th Nestlé Nutrition Institute Workshop, Dubai, March 2017Da EverandRecent Research in Nutrition and Growth: 89th Nestlé Nutrition Institute Workshop, Dubai, March 2017Nessuna valutazione finora
- Trunk Control TestDocumento20 pagineTrunk Control TestSilaghi CiprianNessuna valutazione finora
- Teaching Exercise to Children: A Complete Guide to Theory and PracticeDa EverandTeaching Exercise to Children: A Complete Guide to Theory and PracticeValutazione: 5 su 5 stelle5/5 (1)
- (129 136) V9N5PTDocumento8 pagine(129 136) V9N5PTAqila NurNessuna valutazione finora
- Physical Activity and Walking Onset in Infants With Down SyndromeDocumento16 paginePhysical Activity and Walking Onset in Infants With Down SyndromeSindy Tatiana Valbuena CasallasNessuna valutazione finora
- Effectiveness of Klapp Exercise To Treat Angle Currence in Children With Scoliosis: Literature ReviewDocumento11 pagineEffectiveness of Klapp Exercise To Treat Angle Currence in Children With Scoliosis: Literature ReviewAlejandra GiraldoNessuna valutazione finora
- Contributions of Trunk Muscles To Anticipatory PosturalDocumento14 pagineContributions of Trunk Muscles To Anticipatory PosturalChristhoper HermosillaNessuna valutazione finora
- Postural Orientation During Standing in Children With Bilateral Cerebral PalsyDocumento7 paginePostural Orientation During Standing in Children With Bilateral Cerebral PalsyRaul Vieira VillarroelNessuna valutazione finora
- Refinement, Reliability, and Validity of The Segmental Assessment of Trunk ControlDocumento12 pagineRefinement, Reliability, and Validity of The Segmental Assessment of Trunk ControlBeverly IgartuaNessuna valutazione finora
- AOPA Handout NewParadigms Sciences IMPDocumento34 pagineAOPA Handout NewParadigms Sciences IMPAnup PednekarNessuna valutazione finora
- Postural Control Performance of Active and Inactive Older AdultDocumento11 paginePostural Control Performance of Active and Inactive Older AdultKhairunnisa Ayu KresnandaNessuna valutazione finora
- Jenna e and Nikki R Ebp Final Alt With Accepted ChangesDocumento14 pagineJenna e and Nikki R Ebp Final Alt With Accepted Changesapi-435782808Nessuna valutazione finora
- Cerebral Palsy Presentation 2Documento13 pagineCerebral Palsy Presentation 2api-664219351Nessuna valutazione finora
- 10 30621-Jbachs 1261701-2996283Documento10 pagine10 30621-Jbachs 1261701-2996283Mina RizqinaNessuna valutazione finora
- Aging, Muscle Activity, and Balance Control: Physiologic Changes Associated With Balance ImpairmentDocumento8 pagineAging, Muscle Activity, and Balance Control: Physiologic Changes Associated With Balance ImpairmentFrancisco Vicent PachecoNessuna valutazione finora
- 24-Article Text-45-1-10-20180502Documento7 pagine24-Article Text-45-1-10-20180502Nanie Persona AlonsoNessuna valutazione finora
- Fatiga y Control Postural DinamicoDocumento19 pagineFatiga y Control Postural DinamicoPatricio Alejandro Gaete PobleteNessuna valutazione finora
- 2010 - YAP - Determinants of ResponsivenessDocumento8 pagine2010 - YAP - Determinants of ResponsivenessFriendlymeNessuna valutazione finora
- Research Article: The Influence of The The Sagittal Spinal Curvatures in Children With Generalized Joint HypermobilityDocumento7 pagineResearch Article: The Influence of The The Sagittal Spinal Curvatures in Children With Generalized Joint Hypermobilitysaarita lozano piedraNessuna valutazione finora
- Research in Developmental DisabilitiesDocumento12 pagineResearch in Developmental DisabilitiesRun CapNessuna valutazione finora
- Twelve-Week Biomechanical Ankle Platform System Training On Postural Stability and Ankle Proprioception in Subjects With Unilateral Functional Ankle InstabilityDocumento8 pagineTwelve-Week Biomechanical Ankle Platform System Training On Postural Stability and Ankle Proprioception in Subjects With Unilateral Functional Ankle Instability杨钦杰Nessuna valutazione finora
- Timed Up and Down Stairs Validity and ReliabilityDocumento9 pagineTimed Up and Down Stairs Validity and ReliabilityAndrea B DullanoNessuna valutazione finora
- Son 2016Documento4 pagineSon 2016Zaki RiciNessuna valutazione finora
- Physical Activity in Youth With Osteogenesis Imperfecta Type IDocumento6 paginePhysical Activity in Youth With Osteogenesis Imperfecta Type INefri ArshintaNessuna valutazione finora
- Can Physical Training Hsne An Effect On Well Being in Adults With Mild Intellectual Disability PDFDocumento6 pagineCan Physical Training Hsne An Effect On Well Being in Adults With Mild Intellectual Disability PDFKallia KoufakiNessuna valutazione finora
- Lin 2012Documento9 pagineLin 2012Luis Briones Lau.LiNessuna valutazione finora
- Ritmo EH InglesDocumento7 pagineRitmo EH InglesfasckNessuna valutazione finora
- Effect of Group-Task-Oriented Training On Gross and FineDocumento14 pagineEffect of Group-Task-Oriented Training On Gross and FineCarolinaNessuna valutazione finora
- Effectiveness of Proprioceptive Training Over Strength Training in Improving The Balance of Cerebral Palsy Children With Impaired BalanceDocumento14 pagineEffectiveness of Proprioceptive Training Over Strength Training in Improving The Balance of Cerebral Palsy Children With Impaired BalanceDr. Krishna N. SharmaNessuna valutazione finora
- The Association Between Functional Movement and Overweight and Obesity in British Primary School ChildrenDocumento8 pagineThe Association Between Functional Movement and Overweight and Obesity in British Primary School ChildrenHanna RikaswaniNessuna valutazione finora
- Ways To Improve Balance in Cerebral Palsy PatientsDocumento3 pagineWays To Improve Balance in Cerebral Palsy PatientsSakthiVel Ramu100% (1)
- 2017 - Kwon - A Study On The Physical Fitness On Children With JRADocumento6 pagine2017 - Kwon - A Study On The Physical Fitness On Children With JRAkenmitaNessuna valutazione finora
- JurnalDocumento7 pagineJurnalhasriyantiNessuna valutazione finora
- Working With The Older Client Part 1 Article 2016Documento6 pagineWorking With The Older Client Part 1 Article 2016ChrisGellertNessuna valutazione finora
- Chapter 12 Research MusaDocumento12 pagineChapter 12 Research MusaAinie LawisanNessuna valutazione finora
- NIH Public Access: Assessment of Postural Control in Children With Cerebral Palsy: A ReviewDocumento16 pagineNIH Public Access: Assessment of Postural Control in Children With Cerebral Palsy: A ReviewMaria Camila SanabriaNessuna valutazione finora
- Effect of Core Stability Exercise On Postural Stability in Children With DownsyndromeDocumento10 pagineEffect of Core Stability Exercise On Postural Stability in Children With Downsyndromeputri gunaNessuna valutazione finora
- The Efficacy of A 9-Month Treadmill Walking Program On The Exercise Capacity and Weight Reduction For Adolescents With Severe AutismDocumento10 pagineThe Efficacy of A 9-Month Treadmill Walking Program On The Exercise Capacity and Weight Reduction For Adolescents With Severe AutismmarikosvaNessuna valutazione finora
- Haglund-A, Maria - 2007 - Trunk and Center of Mass Movements During Gait in Children With Juvenile Idiopathic ArthritisDocumento10 pagineHaglund-A, Maria - 2007 - Trunk and Center of Mass Movements During Gait in Children With Juvenile Idiopathic ArthritisAwatef FituriNessuna valutazione finora
- Preventive Medicine: Catherine L. Davis, Stephanie CooperDocumento5 paginePreventive Medicine: Catherine L. Davis, Stephanie CooperFrankis De Jesus Vanegas RomeroNessuna valutazione finora
- The Effect of Ankle-Foot Orthoses On Community-Based Walking in Cerebral Palsy: A Clinical Pilot StudyDocumento8 pagineThe Effect of Ankle-Foot Orthoses On Community-Based Walking in Cerebral Palsy: A Clinical Pilot StudyGita TikihaiNessuna valutazione finora
- Manual Therapy: Filip Struyf, Jo Nijs, Stijn Horsten, Sarah Mottram, Steven Truijen, Romain MeeusenDocumento6 pagineManual Therapy: Filip Struyf, Jo Nijs, Stijn Horsten, Sarah Mottram, Steven Truijen, Romain MeeusenJorgeNessuna valutazione finora
- Medicina: Ffect of A Combined Stretching and StrengthDocumento12 pagineMedicina: Ffect of A Combined Stretching and StrengthKimum KimúmNessuna valutazione finora
- Maughan Et Al. (2012) PDFDocumento15 pagineMaughan Et Al. (2012) PDFvabrandaoNessuna valutazione finora
- Effect of Task-Oriented Training and Neurodevelopmental Treatment On The Sitting Posture in Children With Cerebral PalsyDocumento3 pagineEffect of Task-Oriented Training and Neurodevelopmental Treatment On The Sitting Posture in Children With Cerebral PalsyPhysio SauravNessuna valutazione finora
- Iuliano Et Al., 2015Documento6 pagineIuliano Et Al., 2015luisangelpuertasNessuna valutazione finora
- Intech-Physiotherapy For Children With Cerebral PalsyDocumento24 pagineIntech-Physiotherapy For Children With Cerebral Palsyasfand khanNessuna valutazione finora
- Aerobic ExerciseDocumento9 pagineAerobic Exercisebiahonda15Nessuna valutazione finora
- Stump C Lit Reivew FinalDocumento8 pagineStump C Lit Reivew Finalapi-621438645Nessuna valutazione finora
- Muscle Force and Range of Motion Predictors of Balance in CPDocumento21 pagineMuscle Force and Range of Motion Predictors of Balance in CPshodhgangaNessuna valutazione finora
- Fix Ini StoDocumento31 pagineFix Ini StoMarchelina Benediktin KaunangNessuna valutazione finora
- Literature ReviewDocumento20 pagineLiterature ReviewMira MakramNessuna valutazione finora
- Experimental Gerontology: SciencedirectDocumento11 pagineExperimental Gerontology: SciencedirectFebria Rike ErlianaNessuna valutazione finora
- Fundamental Movement Skills and Physical Fitness As Predictors of Physical Activity: A 6-Year Follow-Up StudyDocumento8 pagineFundamental Movement Skills and Physical Fitness As Predictors of Physical Activity: A 6-Year Follow-Up StudyTúlio MartinsNessuna valutazione finora
- Y Balance Test - 2015Documento8 pagineY Balance Test - 2015JOSÉ MARIA SÁ FREIRE JRNessuna valutazione finora
- The Effects of Therapeutic Taping On Gross Motor Function in Children With Cerebral PalsyDocumento8 pagineThe Effects of Therapeutic Taping On Gross Motor Function in Children With Cerebral PalsyDenise PereiraNessuna valutazione finora
- Lowe 2015Documento9 pagineLowe 2015ﻱﺪﺢ ﺁﻏﻦﻎNessuna valutazione finora
- Bar-Haim Et Al-2006-Developmental Medicine & Child NeurologyDocumento6 pagineBar-Haim Et Al-2006-Developmental Medicine & Child NeurologyGiancarlo Becerra BravoNessuna valutazione finora
- Content ServerDocumento9 pagineContent ServerKennie RamirezNessuna valutazione finora
- Klapp MethodDocumento7 pagineKlapp MethodRJLeddaNessuna valutazione finora
- PTJ 1636Documento10 paginePTJ 1636Pamela DíazNessuna valutazione finora
- Journal of Aerosol Science: Christian J. K Ahler, Rainer HainDocumento11 pagineJournal of Aerosol Science: Christian J. K Ahler, Rainer HainPamela DíazNessuna valutazione finora
- Move To Improve: The Feasibility of Using An Early Mobility Protocol To Increase Ambulation in The Intensive and Intermediate Care SettingsDocumento11 pagineMove To Improve: The Feasibility of Using An Early Mobility Protocol To Increase Ambulation in The Intensive and Intermediate Care SettingsPamela DíazNessuna valutazione finora
- Movilizacion Segura en UCI PDFDocumento19 pagineMovilizacion Segura en UCI PDFGabriela MantillaNessuna valutazione finora
- Research Report: The Physical Function Intensive Care Test: Implementation in Survivors of Critical IllnessDocumento9 pagineResearch Report: The Physical Function Intensive Care Test: Implementation in Survivors of Critical IllnessPamela DíazNessuna valutazione finora
- Sciadv Abd3083 Full PDFDocumento11 pagineSciadv Abd3083 Full PDFjudith retanaNessuna valutazione finora
- Kibler Et Al 2012 Scapula Dyskinesis and Its Relation To Shoulder Injury PDFDocumento9 pagineKibler Et Al 2012 Scapula Dyskinesis and Its Relation To Shoulder Injury PDFPamela DíazNessuna valutazione finora
- Validez y Confiabilidad de Las Escalas de Evaluación Funcional en Pacientes Críticamente Enfermos. Revisión SistemáticaDocumento8 pagineValidez y Confiabilidad de Las Escalas de Evaluación Funcional en Pacientes Críticamente Enfermos. Revisión SistemáticaPamela DíazNessuna valutazione finora
- Safety and Feasibility of A Neuroscience Critical Care Program To Mobilize Patients With Primary Intracerebral HemorrhageDocumento23 pagineSafety and Feasibility of A Neuroscience Critical Care Program To Mobilize Patients With Primary Intracerebral HemorrhagePamela DíazNessuna valutazione finora
- Maeda2018feedforward and Feedback Control Share An Internal Model of The Arm S Dynamics PDFDocumento26 pagineMaeda2018feedforward and Feedback Control Share An Internal Model of The Arm S Dynamics PDFPamela DíazNessuna valutazione finora
- Defining The Clinical Course of MultipleDocumento9 pagineDefining The Clinical Course of MultipleLos Pl DNessuna valutazione finora
- 1 s2.0 S0716864012703346 Main PDFDocumento12 pagine1 s2.0 S0716864012703346 Main PDFPamela DíazNessuna valutazione finora
- The Effect of Increased Mobility On Morbidity in The Neurointensive Care Unit PDFDocumento11 pagineThe Effect of Increased Mobility On Morbidity in The Neurointensive Care Unit PDFPamela DíazNessuna valutazione finora
- Laver Et Al-2020-Cochrane Database of Systematic Reviews PDFDocumento80 pagineLaver Et Al-2020-Cochrane Database of Systematic Reviews PDFPamela DíazNessuna valutazione finora
- Physical and Occupational TherDocumento11 paginePhysical and Occupational TherPamela DíazNessuna valutazione finora
- Khan Et Al-2015-Cochrane Database of Systematic Reviews PDFDocumento46 pagineKhan Et Al-2015-Cochrane Database of Systematic Reviews PDFPamela DíazNessuna valutazione finora
- Kibler 2016 The Role of The Scapula in Preventing and Treating Shoulder Instability PDFDocumento8 pagineKibler 2016 The Role of The Scapula in Preventing and Treating Shoulder Instability PDFPamela DíazNessuna valutazione finora
- Kibler 2016 The Role of The Scapula in Preventing and Treating Shoulder Instability PDFDocumento8 pagineKibler 2016 The Role of The Scapula in Preventing and Treating Shoulder Instability PDFPamela DíazNessuna valutazione finora
- Kibler Et Al 2012 Scapula Dyskinesis and Its Relation To Shoulder Injury PDFDocumento9 pagineKibler Et Al 2012 Scapula Dyskinesis and Its Relation To Shoulder Injury PDFPamela DíazNessuna valutazione finora
- Laver Et Al-2020-Cochrane Database of Systematic Reviews PDFDocumento80 pagineLaver Et Al-2020-Cochrane Database of Systematic Reviews PDFPamela DíazNessuna valutazione finora
- Sud Dick 2006Documento12 pagineSud Dick 2006Pamela DíazNessuna valutazione finora
- Sud Dick 2007Documento19 pagineSud Dick 2007Pamela DíazNessuna valutazione finora
- Early Mobility and Walking Program For Patients in Intensive Care Units Creating A Standard of CareDocumento11 pagineEarly Mobility and Walking Program For Patients in Intensive Care Units Creating A Standard of CarePamela DíazNessuna valutazione finora
- Maeda2018feedforward and Feedback Control Share An Internal Model of The Arm S Dynamics PDFDocumento26 pagineMaeda2018feedforward and Feedback Control Share An Internal Model of The Arm S Dynamics PDFPamela DíazNessuna valutazione finora
- Khan Et Al-2015-Cochrane Database of Systematic Reviews PDFDocumento46 pagineKhan Et Al-2015-Cochrane Database of Systematic Reviews PDFPamela DíazNessuna valutazione finora
- Stroke Compara Bobath Van VlietDocumento7 pagineStroke Compara Bobath Van VlietPamela DíazNessuna valutazione finora
- Aquatic Therapy ScientificAspects PDFDocumento14 pagineAquatic Therapy ScientificAspects PDFCarlos Ernesto AriasNessuna valutazione finora
- Alcance de Sonido Clave Permanencia Del Objeto en CiegosDocumento8 pagineAlcance de Sonido Clave Permanencia Del Objeto en CiegosPamela DíazNessuna valutazione finora
- 1 s2.0 S000296101300295X MainDocumento6 pagine1 s2.0 S000296101300295X MainPamela DíazNessuna valutazione finora
- Densitometría Osea en PC SeveraDocumento12 pagineDensitometría Osea en PC SeveraPamela DíazNessuna valutazione finora
- The Case of Dora and Her DreamsDocumento5 pagineThe Case of Dora and Her DreamsHardik Motsara100% (1)
- Massage Therapy PDFDocumento1 paginaMassage Therapy PDFVirgilio BernardinoNessuna valutazione finora
- Classification and Patient Selection in Abdominoplasty: Alan Matarasso, MD, FacsDocumento8 pagineClassification and Patient Selection in Abdominoplasty: Alan Matarasso, MD, FacsPopa FlorinNessuna valutazione finora
- Antiaritmice Clasa I A MedicamentDocumento3 pagineAntiaritmice Clasa I A MedicamentAndreea ElenaNessuna valutazione finora
- The 2015 OSDUHS Mental Health and Well-Being Report Executive SummaryDocumento11 pagineThe 2015 OSDUHS Mental Health and Well-Being Report Executive SummaryCityNewsTorontoNessuna valutazione finora
- Patient DatasheetDocumento28 paginePatient DatasheetMohit RajNessuna valutazione finora
- Pediatric LeukemiasDocumento42 paginePediatric LeukemiasslyfoxkittyNessuna valutazione finora
- Etiopathogenesis & Staging of Cancer BreastDocumento25 pagineEtiopathogenesis & Staging of Cancer Breastapi-3701915Nessuna valutazione finora
- Emotional IntelligenceDocumento19 pagineEmotional IntelligenceShweta ShrivastavaNessuna valutazione finora
- MAN ParaTitle-Manuscript - Grace-EpresDocumento80 pagineMAN ParaTitle-Manuscript - Grace-EpresSevered AppleheadNessuna valutazione finora
- Transfusion Reactions and Their ManagementDocumento59 pagineTransfusion Reactions and Their ManagementAida AlaudinNessuna valutazione finora
- CarcinogenDocumento196 pagineCarcinogenJosé RamírezNessuna valutazione finora
- Fibula Stress Fractures: A Treatment Review: Iftach Hetsroni, MD, and Gideon Mann, MDDocumento3 pagineFibula Stress Fractures: A Treatment Review: Iftach Hetsroni, MD, and Gideon Mann, MDJamaluddin HaikhahNessuna valutazione finora
- Schizo QuizDocumento4 pagineSchizo QuizmalindaNessuna valutazione finora
- Clarksville Family Therapy, LLC: 2535 Madison Street, Suite D Clarksville, TN 37043Documento6 pagineClarksville Family Therapy, LLC: 2535 Madison Street, Suite D Clarksville, TN 37043Ken MurrayNessuna valutazione finora
- Buset Na ResearchDocumento5 pagineBuset Na Researchmk soberanoNessuna valutazione finora
- Ileus in Critical Illness Mechanisms And.11Documento6 pagineIleus in Critical Illness Mechanisms And.11albimar239512Nessuna valutazione finora
- NPI Reflects Spring 2013Documento12 pagineNPI Reflects Spring 2013npinashvilleNessuna valutazione finora
- Msif Atlas of Ms 2013 ReportDocumento28 pagineMsif Atlas of Ms 2013 ReporttomrehNessuna valutazione finora
- CystoceleDocumento7 pagineCystocelesandeepv08Nessuna valutazione finora
- Ice TherapyDocumento5 pagineIce TherapyDiane CastillonNessuna valutazione finora
- Artículo Sedación Inhalada Con Óxido Nitroso y OxígenoDocumento6 pagineArtículo Sedación Inhalada Con Óxido Nitroso y OxígenoPaula DanielaNessuna valutazione finora
- A Network Meta-Analysis On The Effects of Information Technology Application On Preoperative Anxiety of PatientsDocumento7 pagineA Network Meta-Analysis On The Effects of Information Technology Application On Preoperative Anxiety of PatientsInternational Journal of Application or Innovation in Engineering & ManagementNessuna valutazione finora
- 15 PsychiatricDocumento35 pagine15 PsychiatricSami Ullah Khan NiaziNessuna valutazione finora
- Pedia ReviewerDocumento27 paginePedia ReviewerEvangeline GoNessuna valutazione finora
- Cholesterol PresentationDocumento28 pagineCholesterol Presentationapi-240098169Nessuna valutazione finora
- Origin of The Universe DLPDocumento9 pagineOrigin of The Universe DLPJeiril DivinoNessuna valutazione finora
- Acupuncture IVFDocumento10 pagineAcupuncture IVFWolfgang Rb100% (1)
- Autologous Rib Microtia Construction: Nagata TechniqueDocumento15 pagineAutologous Rib Microtia Construction: Nagata Techniqueandi ilmansyahNessuna valutazione finora
- Beneficial Effects of Ozone Therapy On Oxidative Stress, Cardiac Functions and Clinical Findings in Patients With Heart Failure Reduced Ejection FractionDocumento8 pagineBeneficial Effects of Ozone Therapy On Oxidative Stress, Cardiac Functions and Clinical Findings in Patients With Heart Failure Reduced Ejection FractionCarlosAlbertoCoutinhoNessuna valutazione finora