Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
CVS MCQs
Caricato da
Thana AlAnsariCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
CVS MCQs
Caricato da
Thana AlAnsariCopyright:
Formati disponibili
The Cardiovascular System
Question .1. A 1-mo-old female infant is presented with a chief complaint of poor feeding and lethargy. Parents report that the child was well until 3 days earlier, when poor feeding began. Pulse rate is 280 beats/min, respiratory rate is 50/min, and blood pressure is 80/50 mm Hg. Physical examination shows a gallop rhythm and an enlarged liver palpable 2-3 cm below the right costal margin. The most appropriate diagnostic test for this patient would be: A. Chest radiograph B. CBC C. ECG Explanation: This is a very high heart rate for a simple sinus rhythm. The child is in heart failure, but the excessively high heart rate may be the cause, not the result, of heart failure. (See Chapter 428 in Nelson Pediatrics, 17th ed.) D. ABG analysis E. Blood culture
Question . 2. What would be the most likely diagnosis in the case in Question 1? A. Reentrant SVT Explanation: This is a classic presentation of supraventricular tachycardia in infancy. It is usually idiopathic and transient but does require rapid diagnosis and treatment. It may also be present in utero. Always be sure the parents are not giving the child over-the-counter cold remedies that contain sympathomimetic agents, which may include "herbal" remedies that could contain ephedra. (See Chapter 428 in Nelson Textbook of Pediatrics, 17th ed.) B. Ventricular tachycardia C. Sepsis D. Anemia E. Pneumonia
Question . 3. What would be the most appropriate next step in treatment for the case in Question 1? A. Electrical defibrillation B. IV verapamil C. Adenosine therapy Explanation: Intravenous rapid push adenosine is the drug treatment of choice for all cases of SVT, in infants and in patients of all ages. Verapamil was once used in older patients, but in infants in heart failure, verapamil has serious adverse effects (cardiac arrest) owing to its negative inotropic effects on an already failing myocardium. (See Chapter 428 in Nelson Textbook of Pediatrics, 17th ed.) D. Antibiotic therapy Blood transfusion
The CVS System Nelson Self Assessments website 17th Edition
Question . 4. Chest pain at rest in a 10-yr-old boy is most likely to be due to all of the following Except: A. B. C. D. Asthma Overuse injury Musculoskeletal trauma Coronary atherosclerosis Explanation: Unless there is a strong family history of premature myocardial infarction or sudden death, or unless symptoms are exacerbated by exercise, chest pain in children is often due to musculoskeletal or pulmonary disorders. Children may complain of chest pain after an adult family member has a myocardial infarction. This is less likely to be coronary vessel disease and more likely to be anxiety. Nonetheless, the clinician should be aware of more serious causes in children with chest pain, dyspnea, or syncope with exercise. (See Chapter 415 in Nelson Textbook of Pediatrics, 17th ed.) E. Anxiety
Question . 5. The best management approach in a 10-yr-old with an ostium secundum atrial septal defect with a 3:1 shunt is: A. Observation until heart failure is present B. Prophylaxis for endocarditis each month C. Transvenous device closure Explanation: Although surgical closure is highly successful, experience with device closure in the cardiac catheterization laboratory has been quite successful, and this procedure is now approved by the FDA. (See Chapter 419 in Nelson Textbook of Pediatrics, 17th ed.) D. Observation until pulmonary hypertension develops E. Phlebotomies for recurrent polycythemia
Question . 6. Pulmonary stenosis is associated with all of the following Except: A. Noonan syndrome B. Tetralogy of Fallot C. Rheumatic fever Explanation: Pulmonary valve lesions in rheumatic fever are very unusual. This lesion is common as a dysplastic valve in Noonan syndrome and in Alagille syndrome, which is due to mutations in Jagged 1. Isolated PS is also noted to have an increased frequency of Jagged 1 mutations without Alagille syndrome. (See Chapter 420 in Nelson Textbook of Pediatrics, 17th ed.) D. Alagille syndrome E. Mutations of Jagged 1 gene
The CVS System Nelson Self Assessments website 17th Edition
Question . 7. Complications of vascular rings include all of the following Except: A. B. C. D. Recurrent emesis Chronic wheezing Tracheomalacia Heart failure Explanation: The vessels involved in vascular rings do not produce a shunt or excessive blood flow. The main problems are mechanical impingement on the trachea and/or esophagus and the symptoms resulting from these points of obstruction. (See Chapter 425 in Nelson Textbook of Pediatrics, 17th ed.) E. Cough Question . 8. A 10-yr-old white girl has a history of increasingly severe exercise intolerance and fatigability. The day of admission she had a syncopal event. On examination, she has a systolic ejection click and a loud, narrowly split second heart sound. This is a soft systolic murmur. The chest radiograph demonstrates prominent pulmonary arteries and an enlarged right ventricle. The peripheral pulmonary vascular markings are greatly decreased. The most likely diagnosis is: A. B. C. D. E. Tetralogy of Fallot Stills murmur Rheumatic fever Cor pulmonale Primary pulmonary hypertension Explanation: Primary pulmonary hypertension is an idiopathic disorder. Some familial cases have mutations in the gene for bone morphogenetic protein receptor II. (See Chapter 426 in Nelson Textbook of Pediatrics, 17th ed.)
Question . 9. Wolff-Parkinson-White syndrome is associated with all of the following Except: A. Short P-R interval B. Slow upstroke of QRS complex C. Renal tubular acidosis Explanation: There are rarely any extracardiac problems in patients with WPW. The ECG features of the delta wave (slow upstroke of the QRS complex, also known as preexcitation) are not seen during the SVT and are visible only in sinus rhythm. (See Chapter 428 in Nelson 17th ed.) D. Ebstein anomaly E. Episodes of supraventricular tachycardia Question . 10. The initial management of a hemodynamically stable 2-mo-old infant with supraventricular tachycardia should include: A. Vagal stimulation Explanation: In infants, the vagal maneuver of choice is placing a plastic bag containing iced saline completely over the nose and mouth. If this is unsuccessful, intravenous adenosine is the next step. Vagotonic maneuvers in older children include doing a Valsalva maneuver, straining, breath holding,
The CVS System Nelson Self Assessments website 17th Edition
B. C. D. E.
squatting, drinking iced water, coughing, vomiting, and gagging. (See Chapter 428 in Nelson, 17th ed.) Cardioversion Defibrillation Digitalization Intravenous verapamil
Question . 11. Disorders associated with complete heart block include all of the following Except: A. Maternal systemic lupus erythematosus B. Kearns-Sayre syndrome C. Rheumatoid arthritis Explanation: Rheumatoid arthritis primarily involves the pericardium and not the conduction system. Another cause of complete heart block is injury to the conduction system during reparative surgery for congenital heart disorders. (See Chapter 428 in Nelson Textbook of Pediatrics, 17th ed.) D. Cardiac rhabdomyoma E. Endocarditis Question . 12. A previously healthy 7-yr-old girl has a 3-wk history of fever, myalgias, and a positive blood culture for Staphylococcus aureus. The past medical history is negative including a normal camp physical examination 6 mo ago, which did not reveal any heart murmur. After repeating a blood culture, the next step in her evaluation should be: A. Chest radiograph B. Complete blood count C. Echocardiogram Explanation: This patient has bacterial endocarditis of a previously normal valve. S. aureus is a common pathogen producing endocarditis of a native valve. The duration of the illness is too long for a simple viral illness, and in the absence of bone or soft tissue findings, any person with a positive blood culture for S. aureus should be considered as having endocarditis until proven otherwise. (See Chapter 429 in Nelson Textbook of Pediatrics, 17th ed.) D. Bone scan E. Dental clinic appointment Question . 13. Major findings in the Duke criteria for the diagnosis of endocarditis include all of the following Except: A. B. C. D. Two separate positive blood cultures for common bacteria Intracardiac mass on a valve seen with echocardiography Dehiscence of a prostatic valve Osler nodes Explanation: Immune complex phenomena and embolic events are minor criteria. Two major or one major and 3-5 minor criteria suggest definite endocarditis. (See Chapter 429 in Nelson Textbook of Pediatrics, 17th ed.) E. More than two positive blood cultures for unusual bacteria
The CVS System Nelson Self Assessments website 17th Edition
Question . 14. An 8-yr-old boy presents with fever of 2 weeks' duration, shortness of breath, ankle edema, intermittent painful swelling of the wrists, elbows, and knees unrelated to edema, and a new systolic murmur. One month ago he had a sore throat that lasted for 5 days, which resolved spontaneously. The most likely diagnosis is: A. B. C. D. E. Endocarditis Rheumatoid arthritis Meningococcal sepsis Glomerulonephritis Rheumatic fever Explanation: The sore throat represented an untreated episode of group A streptococcal pharyngitis. Rheumatic fever presents acutely as a migrating polyarthritis, pancarditis (valves, myocardium, pericardium), and erythema marginatum (not in this patient). Delayed or chronic manifestations include chorea or subcutaneous nodules. These all represent major criteria for the diagnosis, but documentation of a previous streptococcal infection is also required. (See Chapter 430 in Nelson Textbook of Pediatrics, 17th ed.)
Question . 15. A 3-mo-old female infant has a history of poor feeding, shortness of breath during feedings, failure to thrive, and chronic cough. Physical examination reveals tachycardia and a gallop rhythm but no murmur. There is hepatomegaly but no cyanosis. A chest radiograph reveals cardiomegaly. The most appropriate diagnostic test is: A. Echocardiogram Explanation: The differential diagnosis includes myocarditis, cardiomyopathies, anomalous coronary arteries, and arteriovenous malformations in the liver or brain. The echocardiogram reveals poor contractibility and a dilated cardiomyopathy. (See Chapter 431 in Nelson) B. Electrocardiogram C. Blood culture D. Serum amino acids E. Urine pH Question . 16. After further evaluation and treatment for heart failure, the child described in Question 15 should also be started on: A. B. C. D. Selenium Vitamin B1 Thyroid hormone Carnitine Explanation: Although deficiencies of all of these nutrients (or hormone) may produce heart failure, the clinical picture and history are not compatible with A-C. Many believe that all infants with cardiomyopathy should receive a trial of carnitine after being evaluated for metabolic inborn errors of metabolism associated with cardiomyopathy. (See Chapter 431 in Nelson Textbook of Pediatrics, 17th ed.) E. None of the above
The CVS System Nelson Self Assessments website 17th Edition
Question . 17. A 20-day-old previously well full-term infant is presented with fever, tachypnea, tachycardia of severity out of proportion to the fever, a gallop rhythm, and hepatomegaly. Important steps in the evaluation of this neonate include all of the following Except: A. Head ultrasonography Explanation: This neonate has a febrile illness with heart failure. (See Chapter 431 in Nelson Textbook of Pediatrics, 17th ed.) B. Echocardiography C. Viral cultures and PCR assay D. ECG E. Liver function tests F. Blood culture
Question . 18. The echocardiogram for the patient in Question 17 reveals myocarditis, and the viral cultures reveal an enterovirus. In addition to medications to treat the heart failure, which additional therapy is now indicated? A. Heart transplantation B. Pleconaril Explanation: Pleconaril is a potent antiviral agent that is very effective against enteroviruses. It is the agent of choice for treatment of severe enteroviral infections. (See Chapter 431 in Nelson Textbook of Pediatrics, 17th ed.) C. Ribavirin D. Intravenous immunoglobulins E. Oseltamivir
Question . 19. A 1-day-old infant is noted to be cyanotic. Physical examination reveals a grade 2-3/6 systolic murmur and a single loud second heart sound. The chest radiograph reveals a normal-sized heart and decreased pulmonary vascular markings. The electrocardiogram (ECG) reveals left ventricular dominance. The next step in the management of this neonate is to administer: A. Sodium bicarbonate B. Morphine C. Prostaglandin E1 Explanation: The murmur may represent a patent ductus arteriosus (PDA). If the PDA closes, marked cyanosis would supervene, resulting in acidosis, shock, and death. Prostaglandin E1 (PGE1) maintains patency of the ductus arterious between the pulmonary artery and the aorta. (See Chapter 423 in Nelson Textbook of Pediatrics, 17th ed.) D. Digoxin E. Positive pressure ventilation
The CVS System Nelson Self Assessments website 17th Edition
Question . 20. The most likely diagnosis for the patient described in Question 19 is: A. B. C. D. Persistent pulmonary hypertension Transposition of the great arteries Truncus arteriosus Pulmonary atresia Explanation: Pulmonary atresia is manifested by a small right ventricle, decreased pulmonary vascular markings, early and marked cyanosis without heart failure, and ductal dependence to maintain some pulmonary blood flow. (See Chapter 423 in Nelson Textbook of Pediatrics, 17th ed.) E. Total anomalous venous return
Question . 21. An 18-mo-old child is noted to assume a squatting position frequently during playtime at the daycare center. The mother also notices occasional episodes of perioral cyanosis during some of these squatting periods. The day of admission, the child becomes restless, hyperpneic, and deeply cyanotic. Within 10 min, the child becomes unresponsive. The most likely underlying lesion is: A. Cardiomyopathy B. Anomalous coronary artery C. Tetralogy of Fallot Explanation: The child described has tetralogy of Fallot with exercise-induced cyanosis. The more serious episode is a cyanotic, blue, or "tet" spell and may be due to decreased systemic vascular resistance, increased pulmonary artery pressure, or right ventricular outflow tract obstruction. The murmur of tetralogy (the pulmonary stenosis) often disappears or lessens during a spell. (See Chapter 423 in Nelson Textbook of Pediatrics, 17th ed.) D. Constipation E. Breath-holding spell
Question . 22. Therapy of a "blue" or "tet" spell could include all of the following Except: A. Epinephrine Explanation: Epinephrine is potentially dangerous because it may exacerbate inotropy and contractile forces, which may obstruct the right ventricular infundibulum. Indeed, propranolol has been used to treat "tet" spells. (See Chapter 423 in Nelson Textbook of Pediatrics, 17th ed.) B. Knee-chest position C. Oxygen D. Morphine E. Sodium bicarbonate F. Phenylephrine
The CVS System Nelson Self Assessments website 17th Edition
Question . 23. A 2-day-old infant experiences cyanosis, hypotension, and metabolic acidosis. On examination, the infant is lethargic, tachycardic, and gray-blue, with hepatomegaly, a grade 2-3/6 systolic murmur, and poor radial and femoral pulses. A chest radiograph reveals cardiomegaly, and an ECG demonstrates right ventricular dominance with markedly reduced R waves in V5 and V6. The most likely diagnosis: A. Myocarditis B. Hypoplastic left heart syndrome Explanation: Poor pulses, reduced left ventricular forces on ECG, cardiogenic shock, and severe cyanosis are typical of hypoplastic left heart syndrome. (See Chapter 424 in Nelson Textbook of Pediatrics, 17th ed.) C. Anomalous coronary arteries D. Total anomalous venous return E. Tetralogy of Fallot
Question . 24. A previously well 3-mo-old presents with poor feeding, diaphoresis during feeding, and poor growth. Vital signs reveal a respiratory rate of 70/min, pulse of 175/min, and blood pressure of 90/65 mm Hg in the upper and lower extremities. The cardiac examination reveals a palpable parasternal lift and a systolic thrill. A grade 4 holosystolic murmur and a mid-diastolic rumble are noted. The chest radiograph reveals cardiomegaly. The most likely diagnosis is: A. Cardiomyopathy B. Myocarditis C. VSD Explanation: A large VSD with a large left-to-right shunt produces significant heart failure. The age at onset usually corresponds to the time when the normally high fetal pulmonary vascular resistance declines in the first 1-3 mo of life. With decreasing pulmonary artery pressure, the left-to-right shunt increases. (See Chapter 419.6 in Nelson Textbook of Pediatrics, 17th ed.) D. Coarctation of the aorta E. Transposition of the great arteries
Question . 25. The initial treatment of choice for a symptomatic patient with isolated pulmonic stenosis is: A. Closed surgical blade valvotomy B. Open surgical valvotomy C. Balloon catheter valvuloplasty Explanation: Balloon valvuloplasty has greatly improved the management of stenotic lesions of the pulmonic and aortic valves. (See Chapter 420 in Nelson Textbook of Pediatrics, 17th ed.) D. Blalock-Taussig shunt E. Valve replacement
The CVS System Nelson Self Assessments website 17th Edition
Question . 26. Pulsus paradoxus is associated with: A. Pericarditis Explanation: Paradoxic pulse is also noted in asthma. (See Chapter 432 in Nelson Textbook of Pediatrics, 17th ed.) B. Endocarditis C. Rheumatic fever D. Myocarditis E. Postperfusion syndrome Question . 27. The radiographic finding of notching of the ribs is associated with: A. Pulmonary hypertension B. Anomalous pulmonary venous return above the diaphragm C. Coarctation of the aorta Explanation: Rib notching is caused by increased collateral arteries trying to supply the lower trunk and extremities and bypass the aortic coarctation. (See Chapter 420.6 in Nelson Textbook of Pediatrics, 17th ed.) D. Systemic hypertension E. Aortic insufficiency Question . 28. An atrioventricular septal defect is different from an ostium secundum ASD because the AV septal defect: A. B. C. D. Does not manifest heart failure Does not create volume overload Has the same ECG findings Produces an early tendency for pulmonary hypertension Explanation: The atrial and the atrial-ventricular defects both are associated with a higher tendency for an earlier and more rapid onset of pulmonary hypertension. The ECG of an A-V septal defect is characteristic because of the superior left deviation of the QRS axis. (See Chapter 419 in Nelson, 17th ed.) E. Creates an atrial-level shunt
Question . 29. A 5-mo-old previously well infant is found to have a loud holosystolic murmur (4/6) at the left sternal border. The first and second heart sounds are normal; there is no tachycardia, rumble, or gallop; and hepatomegaly is not noted. The child feeds well and has grown adequately. You suspect: A. A restrictive VSD Explanation: A small VSD (<0.5 cm2) produces a loud murmur, with perhaps a thrill but no other abnormalities, owing to the limited left-to-right shunt. Many of these defects will close spontaneously. (See Chapter 419 in Nelson Textbook of Pediatrics, 17th ed.) B. Anomalous left coronary artery C. A VSD with a 4:1 shunt D. Tetralogy of Fallot E. Single ventricle
The CVS System Nelson Self Assessments website 17th Edition
Question . 30. A 6-mo-old is presented with tachycardia, tachypnea, and poor feeding for 3 mo. Physical examination reveals a continuous machinery murmur and a wide pulse pressure with a prominent apical impulse. The most likely diagnosis is: A. B. C. D. Pulmonic stenosis Aortic stenosis Ventricular septal defect Patent ductus arteriosus Explanation: A PDA often presents like a large VSD except that there is a continuous murmur as well as the diastolic runoff, which produces the wide pulse pressure and bounding pulses. (See Chapter 419 in Nelson, 17th ed.) E. Anomalous coronary artery Question . 31. The differential diagnosis for the lesion in Question 30 includes all of the following Except: A. B. C. D. E. Truncus arteriosus Aorticopulmonary window Sinus of Valsalva aneurysm rupture Aortic valve insufficiency Critical aortic stenosis from a bicuspid valve Explanation: Aortic stenosis without significant aortic regurgitation (insufficiency) produces an inactive precordium, normal or weak pulses, and pressure overload of the left ventricle. (See Chapter 419 in Nelson, 17th ed.)
Question . 32. For the patient described in Questions 30 and 31, treatment is best performed by which of the following method(s)? A. Intravenous indomethacin B. Surgical closure Explanation: A PDA manifesting in any patient other than a premature infant does not close spontaneously. Surgery carries low morbidity and even lower mortality. However, the availability of transcatheter closure with coils or umbrellas has reduced the need for surgery in most patients. (See Chapter 419) C. Catheter coil closure D. Digoxin until the PDA closes spontaneously E. Angiotensin-converting enzyme inhibitor Question . 33. A neonate manifests cyanosis and hepatomegaly. There is a grade 4/6 systolic ejection murmur without an audible ejection click. The ECG reveals tall, spiked P waves and right ventricular hypertrophy. The best method to evaluate this patient is to perform: A. Chest x-ray examination B. Vector cardiography C. Immediate cardiac catheterization D. MRI E. Echocardiogram Explanation: Echocardiology has replaced most methods of visualizing the anatomy of congenital and other heart lesions. In many circumstances, the
The CVS System Nelson Self Assessments website 17th Edition
10
echocardiographic diagnosis is all that is needed before surgery or other therapies. (See Chapter 416 in Nelson Textbook of Pediatrics, 17th ed.)
Question . 34. The most likely diagnosis in the patient described in Question 33 is: A. Patent ductus arteriosus B. Critical aortic stenosis C. Critical pulmonic stenosis Explanation: Critical pulmonic stenosis often presents in the neonate. Cyanosis is due to elevated right-sided pressures and right-to-left shunting at the patent foramen orale. (See Chapter 420 in Nelson of Pediatrics, 17th ed.) D. Tetralogy of Fallot E. Truncus arteriosus
Question . 35. The treatment of choice for the lesion in the neonate described in Questions 33 and 34 is: A. B. C. D. Digoxin Propranolol (Inderal) Surgical shunt Balloon valvuloplasty Explanation: Balloon pulmonary valvuloplasty is a remarkable nonsurgical method to dilate the valve and partially relieve the obstruction to right ventricular outflow. (See Chapter 420 in Nelson of Pediatrics, 17th ed.) E. Valve replacement
Question . 36. A 12-yr-old boy tries out for a middle school hockey team. He has a history of a heart murmur as an infant, but the doctor thought it would go away. During the tryout, he experiences severe dyspnea and becomes light-headed. At your office, he has a normal rhythm, pulse, and blood pressure and is no longer dizzy. There is a grade 4/6 systolic ejection murmur that radiates to the neck. There is also an ejection click. An ECG reveals left ventricular hypertrophy. The next step in his management should be:
A. B. C. D.
Chest x-ray examination Exercise test Digitalization Echocardiography Explanation: Echocardiography is essential to identify valve disease, estimate gradients, and detect signs of endocardial fibroelastosis. (See Chapter 420 in Nelson Textbook of Pediatrics, 17th ed.) E. Tilt table testing
The CVS System Nelson Self Assessments website 17th Edition
11
Question . 37. The patient described in Question 36 most probably has: A. Pulmonic stenosis B. Mild aortic stenosis C. Severe aortic stenosis Explanation: Severe aortic stenosis may develop gradually, progressing over 5-10 yr. (See Chapter 420 in Nelson Textbook of Pediatrics, 17th ed.) D. Patent ductus arteriosus E. Williams syndrome Question . 38. For the patient described in Question 36, treatment is best accomplished with A. B. C. D. E. Immediate valve replacement A shunt Digoxin Propranolol Balloon valvuloplasty Explanation: Balloon dilatation valvotomy and surgically splitting the valve are treatments of choice. (See Chapter 420 in Nelson of Pediatrics, 17th ed.)
Question . 39. An 8-yr-old boy from the former Soviet Union is brought to your office because of a heart murmur and dusky blue skin. He has marked clubbing of the fingers and toes, and his hematocrit is 70%. He has a grade 4/6 holosystolic murmur. His chest film reveals a normal pulmonary blood flow as well as a right-sided aortic arch. The most likely diagnosis is: A. Total anomalous venous return B. Tetralogy of Fallot Explanation: TOF includes a VSD, pulmonary stenosis, right ventricular hypertrophy, and an overriding aorta between the two ventricles and above the VSD. In addition, 25% of patients have a right-sided aortic arch. (See Chapter 423 in Nelson Textbook of Pediatrics, 17th ed.) C. Eisenmenger syndrome D. Transposition of the great vessels E. Single ventricle Question . 40. The reason that the hematocrit is so high in the patient described in Question 39 is: A. Chronic hypoxia Explanation: Chronic hypoxia produces both the clubbing and the polycythemia. High hematocrits (usually >65% on a central blood sample) usually produce hyperviscosity, which impairs tissue perfusion. Therefore, up to a point, the raised hematocrit improves oxygen delivery; once hyperviscosity develops, the tissue microcirculation is compromised. (See Chapter 427 in Nelson Textbook of Pediatrics, 17th ed.) B. It was taken in a low cardiac output state C. It was a peripheral finger stick D. Polycythemia improves flow through VSD E. Hyperviscosity aids flow to the pulmonary artery
The CVS System Nelson Self Assessments website 17th Edition
12
Question . 41. The patient described in Question 39 experiences a headache and is unable to move the left side of his body. The most likely cause is: A. Embolic stroke B. Cerebral thrombosis C. Cerebral abscess Explanation: Cerebrovascular accidents result from a combination of polycythemia and the right-to-left shunting in patients with TOF. Strokes are more common in children younger than 2 yr and in those with iron-deficiency anemia. Cerebral abscess formation is more common in children older than 2 yr. (See Chapter 427 in Nelson Textbook of Pediatrics, 17th ed.) D. Migraine E. Moyamoya disease
Question . 42. The most likely cause of sudden death in an athlete immediately after forceful blunt trauma to the chest is: A. Commotio cordis Explanation: This unusual event places the heart in asystole, which is unfortunately refractory to almost all resuscitative efforts. At the scene, defibrillation may improve the outcome if done within minutes of the episode. (See Chapter 428 in Nelson Textbook of Pediatrics, 17th ed.) B. Myocardial infarction C. Lacerated coronary artery D. Ruptured cardiac tendineae E. Hemorrhagic pericarditis
Question . 43. An 8-yr-old girl presents with chest pain of 1 day's duration. Five days before onset of the pain, she had fever, chills, and myalgias. Physical examination reveals an uncomfortable, anxious, afebrile patient with tachycardia, no murmur, and distant heart sounds. The chest radiograph shows cardiomegaly without pulmonary edema. There is a paradoxical pulse of 22 mm Hg. The most likely diagnosis is: A. B. C. D. Myocarditis Cardiomyopathy Kawasaki disease Pericarditis Explanation: Pericarditis, in this child due to coxsackievirus infection, often presents as chest pain, tachycardia, narrow pulse pressure, and a pulsus paradoxus. The chest radiograph demonstrates cardiomegaly, which can be enlargement due to myocardial dilatation or expansion of the pericardial space from fluid. (See Chapter 432 in Nelson Textbook of Pediatrics, 17th ed.) E. Sepsis
The CVS System Nelson Self Assessments website 17th Edition
13
Question . 44. The differential diagnosis for the patient described in Question 43 includes all of the following Except:
A. B. C. D. E.
Rheumatic fever SLE Juvenile rheumatoid arthritis Post-meningococcal immune complexes Chronic atrial fibrillation Explanation: Immune complex and other immune mechanisms may produce a pericardial effusion, pericarditis, and rarely cardiac tamponade. (See Chapter 432 in Nelson Textbook of Pediatrics, 17th ed.)
The CVS System Nelson Self Assessments website 17th Edition
14
Potrebbero piacerti anche
- ABHA Coil ProportionsDocumento5 pagineABHA Coil ProportionsOctav OctavianNessuna valutazione finora
- XXX. MCQ Cardiovascular System Book 315-336Documento19 pagineXXX. MCQ Cardiovascular System Book 315-336Maria OnofreiNessuna valutazione finora
- Coronary Atery Disease-Htn-Thrombo QuestionsDocumento38 pagineCoronary Atery Disease-Htn-Thrombo Questionssrivari sriniNessuna valutazione finora
- Cardiac Physiology MCQsDocumento13 pagineCardiac Physiology MCQsالعراقي الصامد100% (2)
- Final Questions 2021Documento8 pagineFinal Questions 2021PatrycjaSkierkaNessuna valutazione finora
- The Original Lists of Persons of Quality Emigrants Religious Exiles Political Rebels Serving Men Sold For A Term of Years Apprentices Children Stolen Maidens Pressed and OthersDocumento609 pagineThe Original Lists of Persons of Quality Emigrants Religious Exiles Political Rebels Serving Men Sold For A Term of Years Apprentices Children Stolen Maidens Pressed and OthersShakir Daddy-Phatstacks Cannon100% (1)
- Blood MCQDocumento24 pagineBlood MCQBijay Kumar MahatoNessuna valutazione finora
- MCQ CardioDocumento12 pagineMCQ CardioAhmed MahanaNessuna valutazione finora
- Vq40de Service ManualDocumento257 pagineVq40de Service Manualjaumegus100% (4)
- All Past Rounds Cardio MCQs AlexandriaDocumento37 pagineAll Past Rounds Cardio MCQs AlexandriaMahmoud Abouelsoud100% (1)
- Cvs MCQ Exam 2008Documento14 pagineCvs MCQ Exam 2008ZH. omg sarNessuna valutazione finora
- CVS MCQ 2010 PDFDocumento23 pagineCVS MCQ 2010 PDFjuniorebinda60% (5)
- CVS MCQsDocumento21 pagineCVS MCQsMohammed Boyka100% (1)
- Heart McqsDocumento33 pagineHeart McqsNaghman Zuberi75% (16)
- MCQ Cardio 2Documento54 pagineMCQ Cardio 2Dian Paramita100% (1)
- Respiratory MCQDocumento3 pagineRespiratory MCQMarjina Khatoon NipuNessuna valutazione finora
- CPSP Demo Questions With Key - PDF Version 1Documento23 pagineCPSP Demo Questions With Key - PDF Version 1Arshad AliNessuna valutazione finora
- Paper C 2019 With Key andDocumento28 paginePaper C 2019 With Key andaizaz100% (1)
- بنك الأسئلةDocumento775 pagineبنك الأسئلةسماح صلاح100% (1)
- Cardiology Mcq's Part - 1Documento31 pagineCardiology Mcq's Part - 1aymenNessuna valutazione finora
- The DIRKS Methodology: A User GuideDocumento285 pagineThe DIRKS Methodology: A User GuideJesus Frontera100% (2)
- 012 CardiacDocumento41 pagine012 CardiacAhmed Zaghw100% (1)
- CVS MCQDocumento14 pagineCVS MCQNur Hamizah Md FuziNessuna valutazione finora
- Renal MCQ 4Documento10 pagineRenal MCQ 4AzizNessuna valutazione finora
- Quiz Cardiovascular Part 3 of 3Documento60 pagineQuiz Cardiovascular Part 3 of 3MedShare100% (7)
- Ganong Physiology Mcqs & SeqsDocumento193 pagineGanong Physiology Mcqs & SeqsRichardNessuna valutazione finora
- MCQ CVS PDFDocumento22 pagineMCQ CVS PDFGovindaraju Subramani100% (1)
- Neurology Multiple Choice Questions With Explanations: Volume IIIDa EverandNeurology Multiple Choice Questions With Explanations: Volume IIIValutazione: 4.5 su 5 stelle4.5/5 (6)
- Respiratory Failure MCQ and QuestionsDocumento5 pagineRespiratory Failure MCQ and QuestionsChikezie Onwukwe67% (3)
- Exam 2018 PDFDocumento62 pagineExam 2018 PDFWondimu Koy100% (1)
- Physiology McqsDocumento5 paginePhysiology McqsFaisal AwanNessuna valutazione finora
- Cardiovascular MCQs LJDocumento11 pagineCardiovascular MCQs LJYanis Yan100% (1)
- Investment Analysis and Portfolio Management: Frank K. Reilly & Keith C. BrownDocumento113 pagineInvestment Analysis and Portfolio Management: Frank K. Reilly & Keith C. BrownWhy you want to knowNessuna valutazione finora
- Pulm 2005 Exam QuestionsDocumento32 paginePulm 2005 Exam QuestionsItharshan IndreswaranNessuna valutazione finora
- CVS Trial ExamDocumento29 pagineCVS Trial ExamAssale Maen100% (1)
- Cardiology 2015-mcqsDocumento78 pagineCardiology 2015-mcqsAsif Newaz100% (1)
- MCQs PulmonologyDocumento2 pagineMCQs PulmonologySadia Batool86% (7)
- RenalDocumento8 pagineRenalVallesh ShettyNessuna valutazione finora
- MCQ IM DepDocumento183 pagineMCQ IM DepHesham A100% (3)
- Renal Disease McqsDocumento20 pagineRenal Disease McqsShankar Deshmukh100% (1)
- Self-Assessment: BOFs for MRCP(UK) and MRCP(I) Part IDa EverandSelf-Assessment: BOFs for MRCP(UK) and MRCP(I) Part INessuna valutazione finora
- Neurology Multiple Choice Questions With Explanations: Volume IDa EverandNeurology Multiple Choice Questions With Explanations: Volume IValutazione: 4 su 5 stelle4/5 (7)
- Medicine-I Important BCQSDocumento10 pagineMedicine-I Important BCQSShairy SohoNessuna valutazione finora
- Medicine I Past BCQsDocumento25 pagineMedicine I Past BCQsShairy SohoNessuna valutazione finora
- Heart, Nerve and Mucsle, Membrane Transport Mcqs With KeyDocumento8 pagineHeart, Nerve and Mucsle, Membrane Transport Mcqs With KeyMudassar Roomi100% (7)
- Cardio SLE Mcqs With AnswersDocumento37 pagineCardio SLE Mcqs With AnswersAsif Newaz100% (4)
- 47 MCQs On GI and Nutrition PhysiologyDocumento14 pagine47 MCQs On GI and Nutrition Physiologyrazsubedi100% (1)
- Ecg Mcqs 1700 DR - AfsanaDocumento5 pagineEcg Mcqs 1700 DR - AfsanaSamah Khan100% (2)
- 003 Pathology MCQ ACEM Primary CardiovascularDocumento5 pagine003 Pathology MCQ ACEM Primary Cardiovascularbmhsh100% (2)
- 15 Miscellaneous Bacteria PDFDocumento2 pagine15 Miscellaneous Bacteria PDFAnne MorenoNessuna valutazione finora
- Gi Physiology Mcqs 24 Aug 04Documento7 pagineGi Physiology Mcqs 24 Aug 04Ran AccNessuna valutazione finora
- Cardiology MCQDocumento7 pagineCardiology MCQNesma Adel100% (1)
- Lung MCQDocumento7 pagineLung MCQArvinth Guna Segaran100% (2)
- Landscape ArchitectureDocumento9 pagineLandscape Architecturelisan2053Nessuna valutazione finora
- 1 Medicine MCQs - CNSDocumento10 pagine1 Medicine MCQs - CNSDiwakesh C B80% (5)
- Neurology: Self-Assessment for MRCP(UK) Neurology SCEDa EverandNeurology: Self-Assessment for MRCP(UK) Neurology SCEValutazione: 5 su 5 stelle5/5 (1)
- Investigation Data FormDocumento1 paginaInvestigation Data Formnildin danaNessuna valutazione finora
- GIT MCQs DR - Ahmed MowafyDocumento15 pagineGIT MCQs DR - Ahmed Mowafya7wfNessuna valutazione finora
- Advanced Oil Gas Accounting International Petroleum Accounting International Petroleum Operations MSC Postgraduate Diploma Intensive Full TimeDocumento70 pagineAdvanced Oil Gas Accounting International Petroleum Accounting International Petroleum Operations MSC Postgraduate Diploma Intensive Full TimeMoheieldeen SamehNessuna valutazione finora
- CVS MCQsDocumento1 paginaCVS MCQsManisha JindalNessuna valutazione finora
- MCQs and Cases 5th YearDocumento118 pagineMCQs and Cases 5th Yearyoune6Nessuna valutazione finora
- Git & Nutrition McqsDocumento24 pagineGit & Nutrition McqsShahabuddin Shaikh100% (1)
- MCQ CardiologyDocumento2 pagineMCQ Cardiologyvishaljairam100% (1)
- Medical Science MCQs Practice Test 1 PDFDocumento3 pagineMedical Science MCQs Practice Test 1 PDFHazim Rhman AliNessuna valutazione finora
- Lange - Endocrine - Physiology Self-Assessment Study QuestionsDocumento19 pagineLange - Endocrine - Physiology Self-Assessment Study QuestionsDimsy Flora KpaiNessuna valutazione finora
- General Medicine - Surgery IV YearDocumento40 pagineGeneral Medicine - Surgery IV YearCynthia GNessuna valutazione finora
- Hech MCQDocumento9 pagineHech MCQamol dahiphaleNessuna valutazione finora
- Endocrine Pathology Mcqs Set 1Documento1 paginaEndocrine Pathology Mcqs Set 1Ho Yong Wai100% (2)
- EPMS System Guide For Subcontractor - V1 2Documento13 pagineEPMS System Guide For Subcontractor - V1 2AdouaneNassim100% (2)
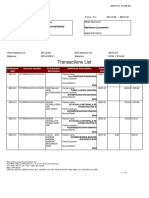
- Transactions List: Marilena Constantin RO75BRDE445SV93146784450 RON Marilena ConstantinDocumento12 pagineTransactions List: Marilena Constantin RO75BRDE445SV93146784450 RON Marilena ConstantinConstantin MarilenaNessuna valutazione finora
- Vendor Registration FormDocumento4 pagineVendor Registration FormhiringNessuna valutazione finora
- Bagian AwalDocumento17 pagineBagian AwalCitra Monalisa LaoliNessuna valutazione finora
- FINAL VERSION On Assessment Tool For CDCs LCs Sept. 23 2015Documento45 pagineFINAL VERSION On Assessment Tool For CDCs LCs Sept. 23 2015Edmar Cielo SarmientoNessuna valutazione finora
- CV Ashish PDFDocumento3 pagineCV Ashish PDFRoshan KejariwalNessuna valutazione finora
- Less Homework More TroubleDocumento7 pagineLess Homework More Troubleg697a0mw100% (1)
- Subeeka Akbar Advance NutritionDocumento11 pagineSubeeka Akbar Advance NutritionSubeeka AkbarNessuna valutazione finora
- Stratum CorneumDocumento4 pagineStratum CorneumMuh Firdaus Ar-RappanyNessuna valutazione finora
- Energy Production From Speed BreakerDocumento44 pagineEnergy Production From Speed BreakerMuhammad Bilal67% (3)
- Formato MultimodalDocumento1 paginaFormato MultimodalcelsoNessuna valutazione finora
- Oil List: Audi Front Axle DriveDocumento35 pagineOil List: Audi Front Axle DriveAska QianNessuna valutazione finora
- Ferobide Applications Brochure English v1 22Documento8 pagineFerobide Applications Brochure English v1 22Thiago FurtadoNessuna valutazione finora
- Catalogo PukangDocumento41 pagineCatalogo PukangClarita Muller LeigueNessuna valutazione finora
- Chapter 4: Thermal ComfortDocumento16 pagineChapter 4: Thermal ComfortWengelNessuna valutazione finora
- P01 - PT in Building & Its AdvantagesDocumento11 pagineP01 - PT in Building & Its AdvantagesPartha Pratim RoyNessuna valutazione finora
- Flight Data Recorder Rule ChangeDocumento7 pagineFlight Data Recorder Rule ChangeIgnacio ZupaNessuna valutazione finora
- Concise Selina Solutions Class 9 Maths Chapter 15 Construction of PolygonsDocumento31 pagineConcise Selina Solutions Class 9 Maths Chapter 15 Construction of Polygonsbhaskar51178Nessuna valutazione finora
- Pediatric Fever of Unknown Origin: Educational GapDocumento14 paginePediatric Fever of Unknown Origin: Educational GapPiegl-Gulácsy VeraNessuna valutazione finora
- Ty Baf TaxationDocumento4 pagineTy Baf TaxationAkki GalaNessuna valutazione finora
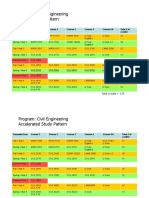
- HKUST 4Y Curriculum Diagram CIVLDocumento4 pagineHKUST 4Y Curriculum Diagram CIVLfrevNessuna valutazione finora