Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Musculoskeletal System
Caricato da
simonedarling0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
341 visualizzazioni6 pagineHormonal Control of bone Parathyroid hormone Important Ca and phosphate regulator helps release of Calcium (Ca) from bone tissue. Released from thyroid gland. Vitamin D Steroid hormone, helps absorb Calcium from intestine, get from intestinal digestion and sun. Activates Parathyroid hormone.
Descrizione originale:
Titolo originale
Musculoskeletal+System
Copyright
© Attribution Non-Commercial (BY-NC)
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoHormonal Control of bone Parathyroid hormone Important Ca and phosphate regulator helps release of Calcium (Ca) from bone tissue. Released from thyroid gland. Vitamin D Steroid hormone, helps absorb Calcium from intestine, get from intestinal digestion and sun. Activates Parathyroid hormone.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
341 visualizzazioni6 pagineMusculoskeletal System
Caricato da
simonedarlingHormonal Control of bone Parathyroid hormone Important Ca and phosphate regulator helps release of Calcium (Ca) from bone tissue. Released from thyroid gland. Vitamin D Steroid hormone, helps absorb Calcium from intestine, get from intestinal digestion and sun. Activates Parathyroid hormone.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 6
Musculoskeletal System
Monday, July 06, 2009
9:27 AM
• Osteoblast
○ bone marrow forming cells
○ Lay down new bone and become…
• Osteocytes
○ Parathyroid hormone.
○ Osteoblast - trapped in bone matrix
○ Maintains bone makers.
• Osteoclast
○ Removes bone during repair and remodeling process
○ Reabsorb bone - use citric and lactic acid to do it.
• Bone Matrix
○ Collagen fibers
• Give bone matrix strength
○ Proteoglycans
• Large polysacchrides give strength to bone.
• Important for movement of ions.
○ Glycoprotein complexes
• Bone Mineralization
○ Synthesized and bone minerals are laid down.
○ Final hardening of bone
• Types of bone
○ Compact Bone
• Highly organized, very strong
• Organized by haviristim system.
○ Spongy Bone
• Less complex organization of bone tissue
○ Periosteum
• Double layer of CT
Outer layer has blood vessels and nerves.
Inner layer has collagen fibers that penetrate into bone.
• Hormonal Control of Bone
○ Parathyroid Hormone
• Important Ca & phosphate regulator
• Helps Ca and phosphate be released from bone tissue.
○ Calcitonin
• Helps regulate release of Calcium (Ca) from bone.
• Released from thyroid gland.
○ Vitamin D
• Steroid hormone, helps absorb Ca from intestine, get from intestinal
digestion and sun.
• Activates Parathyroid Hormone.
• Maintenance of Bone Integrity
○ Remodeling: maintains internal structure
Used for microscopic injuries in bone
• Phase 1 (activation)
Stimulis - hormone, drug, physical stressor activates body to form
osteoclasts.
• Phase 2 (resorption)
Osteoclasts gradually reabsorb bone
• Phase 3 (Formation)
Laying down of new bone by Osteoblasts lining walls of injured
site.
○ Repair
Larger wounds
• Hematoma formation
Blood clot over ends of bony tissue
• Formation of procallus by osteoblasts
Sits up from bone tissue, forms seal over end of bone (by
osteoblasts)
Happens within days of injury
Form bone matrix
• Callus formation
Takes a few weeks to form.
Structural integrity
• Replacement and contour modeling
Can take years (up to 4 yrs)
Bone broken down (lysed), then mineralized.
• Structure and Function of Joints
• Stabilize and move
○ Synarthrosis
• Completely immovable, i.e. Skull.
○ Amphiarthrosis
• Slightly movable, where sternum and ribs come together
○ Diarthrosis
• Freely movable, knees, hips, elbows.
○ Fibrous Joints
• Connected by fibrous CT, usually synarthrosis.
• Depends on how far apart the two bones are.
• Radius ulna, teeth to mandible.
○ Cartilaginous Joints
• Connected by cartilage.
• 2 types
Symphysis type joints (pad or disc b/t bones, pubis, intervertebral
discs)
Synchondrosis type joints (have hyaline cartilage, costal cartilage
b/t ribs and sternum)
○ Synovial Joints
• Diarthrosis joints, most movable and most complex.
• Uniaxial
Move in one direction
• Biaxial
Move in two directions - finger
• Multi Axial
Multiple planes - Hip
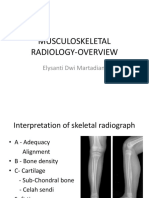
• MSK injuries and Skeletal Trauma classification
○ Fractures
• Complete Fracture
• Incomplete Fracture
• Open Fracture
• Closed Fracture
• Comminuted Fracture
2 or more areas
• Liner Fracture
Parallel to axis of bone
• Oblique Fracture
Oblique angel to bone
• Spiral Fracture
Encircles bone
• Tansverse Fracture
Goes straight across bone
○ Pathologic Fracture
• Break in bone tissue where there has been a preexisting abnormality
or underlying disease issue.
Tumors, osteoporosis, infex of bone, metabolic bone disorders.
○ Stress Fracture
• Occurs in normal or abnormal bones.
• Repeated stress on bone.
• Often in athletes
○ Repair is as described earlier.
• Fractures
○ Clinical Manifestations
• Pain, swelling, loss of function, deformity if not treated.
○ Diagnosis
• Xray and full history
• Underlying cause.
• Mechanism of injury
○ Treatment
• Reduction and internal fixation, manual pressure/manipulation, closed
procedure.
• Surgically, controlled situation
• Immobolization, splints, calfs, traction, external fixation devices
○ Bone Healing
• See above
• Osteoporosis
○ Pourous bone
• Structural integrity compromised, decreased mineralization.
• Usually in cortical (compact) bones (more porous, thinner to start with)
Compact bones - makes up majority of bone structure. Femur,
radius, ulna.
• More prone to fracture.
○ Peak bone mass reached at age 30
• Start to reabsorb bone mass.
• Slow at first, then increases as we age.
○ Progressive bone loss
• Can fracture spontaneously
• Most pronounced in wrist, hip, spine.
Will scan in wrist to check (cheaper)
○ Risk Factors?
• Post-menopausal women.
Possibly due to Drop in Estrogen production, increases amount of
osteoclasts.
• Increased age
• Not active.
• Women.
• Caucasian or Asian increased chance.
• Smaller body build.
○ Manifestations: pain and bone deformity.
• Silent process - don't know unless get a scan. Until bone deformity
occurs. Microfractures in spine, shorter, pain.
• Simple fall can break hip, shoulder, arm, etc.
• Osteomyelitis
• Infex of bone tissue
○ Endogenous and Exogenous source
• From in or outside body.
• Usually by bacteria, sometimes funguses, parasites, viruses.
• From skin, sinus, ear, and dental infex's.
○ Travel by arteries, veins, lymph
○ Provokes and intense inflammatory response in bone tissue
○ Disrupts/weakens the (bone) cortex, predisposing to fracture.
○ Manifestations vary with age, site, initiating event, infecting organism, and
whether it is acute, sub-acute, or chronic.
• Fever, malaise, fatigue, some anorexia, weight loss, pain around
infected area, edema at area (maybe).
• Common in people with Wounds that don't heal.
• Ankle, toe, knee.
• Osteoarthritis (OA)
○ Degenerative Joint Disease
• Non-inflammatory joint disease.
• Loss of articular cartilage.
○ Pathologic Characteristics
• Erosion of Articular Cartilage
• Sclerosis of bone underneath the cartilage
Cause pain.
• Formation of bone spurs.
Cause pain.
○ Risk Factors?
• More severe in women.
• Joint stress, repetitive
• Trauma leading to joint instability.
• Idiopathic forms - don't know why it occurs (most common)
• Age increases risk.
○ Signs/Symptoms?
• Neck and back, wrists/hands, legs feet.
• Larger joints then moving to smaller joints.
○ A slow progressive disease
○ Affects weight-bearing joints.
○ Pain with activity
○ <30 minutes of morning stiffness
○ Crepius
• Popping sensation
• Rheumatoid Arthritis (RA)
○ A Systemic. chronic auimmune disorder of unknown etiology
• Think neutrophils, macrophages, etc come to effected joints and start
phagocytosis on immune complexes at joint, releasing enzymes that
destroy joint cartilage.
• Inflammatory response - perpetuates immune response.
○ Primary site of pathology is the synovium of the joints
○ Begins Insidiously
• Slower onset
○ Pain with movement and joint tenderness
○ Criteria for RA
• Morning stiffness for at least an hour.
• Symmetrical, happens on both wrists.
• Often effects hands
• Get subcutaneous nodules
• Positive blood markers (rheumatoid factor)
• Fibromyalgia
○ Chronic M/S Syndrome
• Unknown cause, flu like symptoms beforehand.
• Some tie in to chronic fatigue syndrome.
• Some also have HIV, Lime's disease.
○ Diffuse Pain, Fatigue, Tender points
• Parts on body, buttocks, shoulder where pain is diffuse, won't correlate
with any other process that is occurring.
• Debilitating chronic lfatigue syndrome.
○ Always have normal lab test (ESR.ANA,RA)
○ Other Symptoms?
• Headache, memory loss, irritable bowel symptoms
• Sensitivity to cold (Reynod's Syndrome?), hands blanch.
• Depression and anxiety.
• Congenital Defects Osteogenesis Imperfecta
• Brittle bone Disease
• Genetic, either autosomal dominant or autosomal recessive process
determines how disease is classified and how severe.
○ Clinical Maniestations
• Osteopenia
Recurring fractures, can happen when picking up child.
Short triangular shaped face.
Blue sclera (white part of eye), poor dentition of teeth.
Increased rate of aortic aneurisms.
• Increased rate of fractures
○ Treatment: Surgery
○ Often mistaken as child abuse in mild cases of OI.
• Juvenile Rheumatoid Arthritis
○ Like adult version
○ Large joints most commonly affected
• Can stiffen and contracture.
• Can be damaged or altered altering how joint grows as child ages.
• Joint stiffness following rest.
• Decreased physical activity, weakness in muscles.
• Effects all children differently - some will have many symptoms, some
will have mild cases.
○ Chronic Uveitis (in eye) is common
○ Serum test for RF (Rheumatoid Factor) may be negative
○ Subluxation and ankolysis may occur in cervical spine
• Deformity of cervical spine, not aligned properly.
○ RA that continues through adolescence can have severe effects in growth
and morbidity.
Potrebbero piacerti anche
- Lecture 11aDocumento33 pagineLecture 11amukhtarjaballaNessuna valutazione finora
- Osteoarthritis of The Knee HKDocumento31 pagineOsteoarthritis of The Knee HKFira Wahidah FirdausNessuna valutazione finora
- FractureDocumento52 pagineFractureCob CornNessuna valutazione finora
- Muskuloskeletal 2012 NaufalDocumento53 pagineMuskuloskeletal 2012 Naufaldahlia kharisma wardhaniNessuna valutazione finora
- Basics of FractureDocumento12 pagineBasics of Fracturecimahmudraju100% (2)
- FractureDocumento302 pagineFractureMaryjoy Gabriellee De La CruzNessuna valutazione finora
- 1-22 Osteoporosis & Hip PainDocumento79 pagine1-22 Osteoporosis & Hip PaintarikeopsNessuna valutazione finora
- Musculoskeletal System Disorders f03Documento34 pagineMusculoskeletal System Disorders f03Marianne LayloNessuna valutazione finora
- Myositis Ossificans: Causes, Symptoms and TreatmentDocumento20 pagineMyositis Ossificans: Causes, Symptoms and TreatmentsarathNessuna valutazione finora
- Musculoskeletal Trauma FracturesDocumento47 pagineMusculoskeletal Trauma FracturesLydia Lopz MsnrncdNessuna valutazione finora
- Osteoarthritis: - Typically Affects The Fingers, Spine, Hips andDocumento36 pagineOsteoarthritis: - Typically Affects The Fingers, Spine, Hips andsuyatmiNessuna valutazione finora
- OA Pathology, Diagnosis and TreatmentDocumento31 pagineOA Pathology, Diagnosis and Treatmentinternship nganjukNessuna valutazione finora
- Care of Patients with Musculoskeletal TraumaDocumento7 pagineCare of Patients with Musculoskeletal TraumaJosephine Navarro100% (1)
- Osteo Arthit IsDocumento19 pagineOsteo Arthit IsShaa ShawalishaNessuna valutazione finora
- MUSCULOSKELETALTERMSDocumento3 pagineMUSCULOSKELETALTERMSapi-3822433Nessuna valutazione finora
- MS 36Documento7 pagineMS 36jefrocNessuna valutazione finora
- Pharmacotherapy of Osteoarthritis: Abera J. (Bpharm., MSC in Clinical Pharmacy), School of Pharmacy, CHMS, HuDocumento31 paginePharmacotherapy of Osteoarthritis: Abera J. (Bpharm., MSC in Clinical Pharmacy), School of Pharmacy, CHMS, HuAbera JamboNessuna valutazione finora
- Musculoskeletal AssesmentDocumento72 pagineMusculoskeletal AssesmentSuci MayveraNessuna valutazione finora
- Surgery - Dychioco - Musculo Skeletal InjuriesDocumento79 pagineSurgery - Dychioco - Musculo Skeletal Injuries3rd yrsNessuna valutazione finora
- Malunion Delayed Union and Nonunion FracturesDocumento31 pagineMalunion Delayed Union and Nonunion FracturesKalayo100% (1)
- Malunion Delayed Union and Nonunion FracturesDocumento31 pagineMalunion Delayed Union and Nonunion FracturesAzmi FarhadiNessuna valutazione finora
- Malunion Delayed Union and Nonunion FracturesDocumento31 pagineMalunion Delayed Union and Nonunion FracturesRasjad ChairuddinNessuna valutazione finora
- Malunion Delayed Union and Nonunion FracturesDocumento31 pagineMalunion Delayed Union and Nonunion FracturesutisuryanjNessuna valutazione finora
- Malunion Delayed Union and Nonunion FracturesDocumento31 pagineMalunion Delayed Union and Nonunion Fracturessatya yudhayanaNessuna valutazione finora
- FractureDocumento30 pagineFractureFarida LaksitariniNessuna valutazione finora
- Osteoarthritis (OA) - Definition, Risk Factors, Symptoms, Diagnosis and Nursing ManagementDocumento39 pagineOsteoarthritis (OA) - Definition, Risk Factors, Symptoms, Diagnosis and Nursing ManagementMourian AmanNessuna valutazione finora
- Fracture 140717081851 Phpapp02Documento63 pagineFracture 140717081851 Phpapp02Jaylord VerazonNessuna valutazione finora
- Complication of FractureDocumento79 pagineComplication of FractureAhmad SyahmiNessuna valutazione finora
- Fracture: Presented By: Ms. Durga Joshi M. SC NursingDocumento63 pagineFracture: Presented By: Ms. Durga Joshi M. SC NursingSanjaya PutraNessuna valutazione finora
- OSTEOARTHRITISDocumento4 pagineOSTEOARTHRITISapi-3822433100% (2)
- Complications of FracturesDocumento55 pagineComplications of FracturesMina SamirNessuna valutazione finora
- Fracture ManagementDocumento50 pagineFracture ManagementCharLes OdalNessuna valutazione finora
- OADocumento27 pagineOADarkKnighthere100% (1)
- Musculoskeletal Disorders 21 dec. 2021Documento61 pagineMusculoskeletal Disorders 21 dec. 2021sofiamansoorNessuna valutazione finora
- 23 Principle of Fractures AGSDocumento31 pagine23 Principle of Fractures AGSNgurah AndhikaNessuna valutazione finora
- Musculoskeletal disorders in childrenDocumento73 pagineMusculoskeletal disorders in childrenMuhammadNessuna valutazione finora
- OSTHEOARTHIRITISDocumento25 pagineOSTHEOARTHIRITISOndari gisemba OSINDENessuna valutazione finora
- Types of FracturesDocumento50 pagineTypes of FracturesMariah Rosette Sison HandomonNessuna valutazione finora
- Chapter 65 FracturesDocumento43 pagineChapter 65 FracturesBenjamin SchauerteNessuna valutazione finora
- Osteochondroma 150907182521 Lva1 App6891Documento22 pagineOsteochondroma 150907182521 Lva1 App6891bucculuNessuna valutazione finora
- Seminar W4 - Bone & Soft Tissue TumoursDocumento123 pagineSeminar W4 - Bone & Soft Tissue TumoursUN EPNessuna valutazione finora
- Fraktur Patologis EngDocumento11 pagineFraktur Patologis EngAisya IndiraNessuna valutazione finora
- Fracture: Edfran Jed A. Serino MSN 303Documento34 pagineFracture: Edfran Jed A. Serino MSN 303Edfran Jed SerinoNessuna valutazione finora
- UntitledDocumento23 pagineUntitledwieka mawieNessuna valutazione finora
- Fracture 190706114534Documento61 pagineFracture 190706114534Precious BlessingNessuna valutazione finora
- NCM 116 - Musculoskeletal Conditions Part 3Documento21 pagineNCM 116 - Musculoskeletal Conditions Part 3Gabrielle Frances FernandezNessuna valutazione finora
- Dr. K.B.Sudhikumar Prof. & HOD Dept. of Salyatantra, GAC, TripunithuraDocumento69 pagineDr. K.B.Sudhikumar Prof. & HOD Dept. of Salyatantra, GAC, Tripunithuraapi-73271717Nessuna valutazione finora
- OSTEOARTHRITISDocumento61 pagineOSTEOARTHRITISARYAN THAPANessuna valutazione finora
- Degenerative Spinal Cord Diseases: Rizal Daulay Orthopaedic SurgeonDocumento43 pagineDegenerative Spinal Cord Diseases: Rizal Daulay Orthopaedic SurgeonDELA MARSELANessuna valutazione finora
- DR - Jimmy-Blok Semester 2-Minilecture Muskuloskeletal OADocumento55 pagineDR - Jimmy-Blok Semester 2-Minilecture Muskuloskeletal OATutde SedanaNessuna valutazione finora
- Fracture PP Ahmad Aqel 2013Documento32 pagineFracture PP Ahmad Aqel 2013ahmadNessuna valutazione finora
- Musculoskeletal System Teacher Ppts1Documento47 pagineMusculoskeletal System Teacher Ppts1anaflaviaaguiarNessuna valutazione finora
- Degenerative Sport (Autosaved)Documento71 pagineDegenerative Sport (Autosaved)Elisabeth Permatasari SidabutarNessuna valutazione finora
- 6 Kuliah Radiology of MSKDocumento46 pagine6 Kuliah Radiology of MSKDesak PratiwiNessuna valutazione finora
- Pathological Fracture 1Documento38 paginePathological Fracture 1Wan Muhammad Mulkan0% (1)
- Dr. Luthfi Hidayat, SP - OTDocumento39 pagineDr. Luthfi Hidayat, SP - OTadystiNessuna valutazione finora
- Osteoarthritis and Joint Diseases 2023Documento29 pagineOsteoarthritis and Joint Diseases 2023Abdullah MelhimNessuna valutazione finora
- Osteoarthritis 191016103144Documento49 pagineOsteoarthritis 191016103144dr.abouzaid098Nessuna valutazione finora
- MSK RADIOLOGY OVERVIEWDocumento42 pagineMSK RADIOLOGY OVERVIEWRisma Ari PertiwiNessuna valutazione finora
- A Simple Guide to Back Pain and Other Spine DisordersDa EverandA Simple Guide to Back Pain and Other Spine DisordersNessuna valutazione finora
- UCSF PRDG Purchasing Letter 9-1.2010 1Documento1 paginaUCSF PRDG Purchasing Letter 9-1.2010 1simonedarlingNessuna valutazione finora
- Student Evaluation of Clinical Setting 3-29-10 JSBDocumento1 paginaStudent Evaluation of Clinical Setting 3-29-10 JSBsimonedarlingNessuna valutazione finora
- Pediatric Nursing AssessmentDocumento1 paginaPediatric Nursing AssessmentsimonedarlingNessuna valutazione finora
- N144 MSK Burns Abuse LectureDocumento15 pagineN144 MSK Burns Abuse LecturesimonedarlingNessuna valutazione finora
- Calendar Winter For Moodle-4Documento2 pagineCalendar Winter For Moodle-4simonedarlingNessuna valutazione finora
- Fall 2009 Hematology Oncology Content Topics and Case StudyDocumento2 pagineFall 2009 Hematology Oncology Content Topics and Case StudysimonedarlingNessuna valutazione finora
- Children With Special Needs and Ethical DilemmasDocumento45 pagineChildren With Special Needs and Ethical DilemmassimonedarlingNessuna valutazione finora
- Community Health Work LogDocumento1 paginaCommunity Health Work LogsimonedarlingNessuna valutazione finora
- Mcgirr 149 Winter 10Documento168 pagineMcgirr 149 Winter 10simonedarlingNessuna valutazione finora
- Sociocultural Presentation MegDocumento1 paginaSociocultural Presentation MegsimonedarlingNessuna valutazione finora
- Asthma That Disappears Between Ages 6-8 - Bronchioles Grew & Resolved The AsthmaDocumento27 pagineAsthma That Disappears Between Ages 6-8 - Bronchioles Grew & Resolved The Asthmasimonedarling100% (1)
- Growth and Development Nature vs. NurtureDocumento6 pagineGrowth and Development Nature vs. NurturesimonedarlingNessuna valutazione finora
- Fall 2009 Endocrine Content Topics and Case Study2Documento2 pagineFall 2009 Endocrine Content Topics and Case Study2simonedarlingNessuna valutazione finora
- Fall 2009 GI Unit Content Topics and Case StudyDocumento3 pagineFall 2009 GI Unit Content Topics and Case StudysimonedarlingNessuna valutazione finora
- Nursing DiagnosesDocumento2 pagineNursing DiagnosessimonedarlingNessuna valutazione finora
- MedSurg - Endocrine IIkaitlynDocumento8 pagineMedSurg - Endocrine IIkaitlynsimonedarlingNessuna valutazione finora
- N145 Hot TopicsDocumento8 pagineN145 Hot TopicssimonedarlingNessuna valutazione finora
- Respiratory October 14, 2009 Once An Endotracheal Tube Is InsertedDocumento2 pagineRespiratory October 14, 2009 Once An Endotracheal Tube Is InsertedsimonedarlingNessuna valutazione finora
- N145Neuro Part 2Documento11 pagineN145Neuro Part 2simonedarlingNessuna valutazione finora
- N145Neuro Part 2Documento11 pagineN145Neuro Part 2simonedarlingNessuna valutazione finora
- Head To Toe AssessmentDocumento2 pagineHead To Toe Assessmentsimonedarling100% (4)
- N145Neuro Part 1Documento6 pagineN145Neuro Part 1simonedarlingNessuna valutazione finora
- Accessory OrgansDocumento7 pagineAccessory OrganssimonedarlingNessuna valutazione finora
- Cancers Sum 2009Documento34 pagineCancers Sum 2009simonedarlingNessuna valutazione finora
- Endocrine Disorders Julie Mann, NP - Case StudyDocumento10 pagineEndocrine Disorders Julie Mann, NP - Case Studysimonedarling75% (4)
- PulmDocumento20 paginePulmsimonedarling100% (2)
- N145 Anemia Cancer HIVDocumento4 pagineN145 Anemia Cancer HIVsimonedarlingNessuna valutazione finora
- Tuesday, July 28, 2009 9:25 PMDocumento8 pagineTuesday, July 28, 2009 9:25 PMsimonedarlingNessuna valutazione finora
- PAthos Exam 3 Disorders of The Abd.Documento9 paginePAthos Exam 3 Disorders of The Abd.simonedarlingNessuna valutazione finora
- Summer 2009 Nutrition Bowel Elimination WhiteLNDocumento7 pagineSummer 2009 Nutrition Bowel Elimination WhiteLNsimonedarling100% (2)
- DynaMed Plus - Stroke (Acute Management)Documento126 pagineDynaMed Plus - Stroke (Acute Management)Sarah Shafa MarwadhaniNessuna valutazione finora
- Subacute, Silent, and Postpartum Thyroiditis 2012Documento11 pagineSubacute, Silent, and Postpartum Thyroiditis 2012YoaNnita GoMezNessuna valutazione finora
- Neuroanesthesia ProposalDocumento2 pagineNeuroanesthesia ProposalPatricio CaballeroNessuna valutazione finora
- Order 157489 - PSC Requisition - Ulta Lab TestsDocumento2 pagineOrder 157489 - PSC Requisition - Ulta Lab Testszarrin77Nessuna valutazione finora
- An Epidemic of DepressionDocumento2 pagineAn Epidemic of DepressionMel Schwartz100% (3)
- Alcohol Binge Drinking in OCDDocumento2 pagineAlcohol Binge Drinking in OCDSuyash DwivediNessuna valutazione finora
- DMDFDocumento22 pagineDMDFsujal177402100% (1)
- Renal Failure and Kidney DiseaseDocumento41 pagineRenal Failure and Kidney Disease12046Nessuna valutazione finora
- Surgical Options in The Management of Inguinal Hernias: Mohammed Al-SaffarDocumento61 pagineSurgical Options in The Management of Inguinal Hernias: Mohammed Al-Saffarsgod34Nessuna valutazione finora
- Low Back Pain SyndromeDocumento244 pagineLow Back Pain Syndromebrunettebomshell100% (4)
- Bahasa Inggris AskepDocumento4 pagineBahasa Inggris AskepMona Indah100% (2)
- Introduction Integrative MedicineDocumento13 pagineIntroduction Integrative MedicineNitin PatilNessuna valutazione finora
- Patient Safety Incident Report Form SummaryDocumento9 paginePatient Safety Incident Report Form SummaryJhun SantiagoNessuna valutazione finora
- Blood Alcohol ContentDocumento6 pagineBlood Alcohol ContentGina Monserrat Gamboa NezNessuna valutazione finora
- Just Culture CommissionDocumento27 pagineJust Culture CommissionAlina PetichenkoNessuna valutazione finora
- Subq and Im InjectionsDocumento2 pagineSubq and Im Injectionsapi-242267470Nessuna valutazione finora
- VUJ ObstructionDocumento2 pagineVUJ ObstructionSheikh Mizanur RahmanNessuna valutazione finora
- Antepartum HaemorrhageDocumento36 pagineAntepartum HaemorrhageAfi RamadaniNessuna valutazione finora
- Artificial Intelligence in HealthcareDocumento3 pagineArtificial Intelligence in HealthcareBaekhyunee PubbyNessuna valutazione finora
- Scientists Study The Benefits of Worms - NewselaDocumento3 pagineScientists Study The Benefits of Worms - NewselaMr WarnockNessuna valutazione finora
- Don't Throw Away The Cane W.P.blountDocumento15 pagineDon't Throw Away The Cane W.P.blountVijay KumarNessuna valutazione finora
- FUROSEMIDEDocumento2 pagineFUROSEMIDEjbespiritu100% (3)
- FibromyalgiaDocumento85 pagineFibromyalgiamariuscornel100% (1)
- Acute Mild Traumatic Brain Injury (Concussion) in Adults - UpToDateDocumento22 pagineAcute Mild Traumatic Brain Injury (Concussion) in Adults - UpToDateZulvina FaozanudinNessuna valutazione finora
- Regulation For Optical Center and Optometry Services FinalDocumento15 pagineRegulation For Optical Center and Optometry Services FinalsafasayedNessuna valutazione finora
- Oxygen-Induced Hypercapnia in COPD PDFDocumento4 pagineOxygen-Induced Hypercapnia in COPD PDFsatyagraha84Nessuna valutazione finora
- FERRIC CARBOXYMALTOSE IMPROVES SYMPTOMS IN HEART FAILURE PATIENTS WITH IRON DEFICIENCYDocumento31 pagineFERRIC CARBOXYMALTOSE IMPROVES SYMPTOMS IN HEART FAILURE PATIENTS WITH IRON DEFICIENCYDanar Fahmi SudarsonoNessuna valutazione finora
- CareMore: Innovative Healthcare DeliveryDocumento30 pagineCareMore: Innovative Healthcare DeliveryPartnership to Fight Chronic DiseaseNessuna valutazione finora
- Approach To Hypoglycemia in Infants and Children - UpToDateDocumento19 pagineApproach To Hypoglycemia in Infants and Children - UpToDateOmar Nayef TaaniNessuna valutazione finora