Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Skema Hipertensi
Caricato da
Andri wijayaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Skema Hipertensi
Caricato da
Andri wijayaCopyright:
Formati disponibili
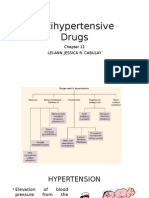
HYPERTENSION 1.
Pathophysiology of Hypertension Secondary to Chronic Renal Failure a) Adults Renal clearance of sodium and water is reduced causing accumulation of intravascular fluid contributing to hypertension. In some patients there is diminished renal perfusion causing inappropriate activation of the renin-angiotensin system. Angiotensin II produces vasoconstriction and increased vascular resistance causing increased blood pressure. Further reduced renal perfusion results in further increased sodium and fluid retention. b) Children Usually due to primary hypertension 2. Therapy for Hypertension in Chronic Renal Failure a) Goals of Therapy Prevent or slow further decline in renal function Prevent atherosclerosis, stroke, and cardiovascular disease Usual adult goal blood pressures: Systolic blood pressure < 130 mm Hg Diastolic blood pressure < 85 mm Hg Usual pediatric goal blood pressures are based on weight, sex and age.
b) Lifestyle modifications Salt restriction Weight reduction Avoid tobacco Limit alcohol consumption If appropriate, start a regular exercise program
c) Pharmacotherapy Empiric Drug Selection for Chronic Renal Insufficiency General Predialysis Population Diuretics Children Calcium Channel Blockers or ACE inhibitors Comorbid Conditions Diabetics ACE inhibitors Bilateral Renal Artery Stenosis Calcium Channel Blockers Heart Failure ACE inhibitors Isolated Systolic Hypertension Calcium Channel Blockers Post MI Beta Blockers Angina Beta Blockers or Calcium Channel Blockers 3. Clinical Pearls Goal blood pressure should be achieved gradually to allow adaptation to reduced perfusion pressures and to prevent ischemic episodes. Antihypertensive doses may be held or reduced on hemodialysis days. Patients may be on multiple antihypertensives at large doses. 4. Clinical Drug Reviews Diuretics Diuretics have the added advantage of helping to control sodium and water retention in addition to blood pressure. The more proximal the site of action the greater the potency of the diuretic Loop diuretics > Thiazides > Potassium Sparing Diuretics Diuretics with different sites of action work together synergistically. Profound diuresis can be a concern. Thiazides (chlorthalidone, hydrochlorothiazide, metolazone, etc.) Thiazides inhibit Na reabsorption at the distal portion of the ascending Loop of Henle. Natriuresis results in reduced peripheral vascular resistance Alone they are not effective at creatinine clearances below 30 mL /min, but metolazone may still be useful for synergy with Loop Diuretics, since metalazone may also block proximal tubule sodium resorption.
Loop Diuretics (ethacrynic acid, furosemide) Na reabsorption in the proximal portion of the Loop of Henle is inhibited by loop diuretics. Loop diuretics have some vasodilating properties which result in reduced renal vascular resistance. High doses are effective even at relatively low creatinine clearances. Loop diuretics are frequently discontinued when dialysis is initiated. Potassium Sparing Diuretics (amiloride, triamterene) Reabsorption at the distal site of the renal tubule is inhibited by potassium sparing diuretics. This is the least potent class of diuretics. They are used with thiazides or loop diuretics to counteract the hypokalemic effect of the more potent diuretic. Potassium sparing diuretics are usually avoided in renal failure due to hyperkalemia and poor efficacy.
Beta-Blockers (acebutolol, atenolol, labetolol, metoprolol, propranolol) Beta blockers inhibit stimulation of beta-adrenergic receptors by catecholamines Beta blockers can reduce renal blood flow secondary to negative cardiac inotropic effects. Angiotensin Converting Enzyme Inhibitors and Angiotensin II Receptor Antagonists These agents cause vasodilation and dilation of efferent arteriole. In some patients, these agents can increase renal blood flow. These agents reduce proteinuria and the rate of progression of renal failure, especially in diabetics (Class A evidence). Hyperkalemia can be a problem during initial stages of renal dysfunction. The complete loss of renal function however, also produces the loss of the mechanism causing hyperkalemia. Calcium Channel Blockers (amlodipine, diltiazem, felodipine, nifedipine, verapamil) Calcium channel blockers reduce renal vascular resistance and increase renal blood flow. Nifedipine SL is reserved for hypertensive crisis in children. Alpha-Blockers (prazosin, terazosin) Alpha-blockers block the activation of alpha receptors, and thus prevent catecholamine induced vasoconstriction.
Central Acting Agents (clonidine) Clonidine stimulates postsymptomatic alpha 2 adrenergic receptors in the CNS, activating inhibitory neurons to produce a decrease in sympathetic outflow. Also has antagonist actions at presynaptic alpha receptors. It is usually a third or fourth line antihypertensive agent. Clonidine can also be used to treat restless leg syndrome, a nervous system disorder of renal failure patients (see nervous system disorders section) Vasodilators (hydralazine, minoxidil) Hydralazine reduces total peripheral resistance by direct action on vascular smooth muscle, with an effect greater on arterioles than on veins. Minoxidil causes direct relaxation of arteriolar smooth muscle, resulting in a reduction in total peripheral resistance
Hypertension: Useful References
1. Anderson S, Jung FF, Ingelfinger JR. Renal renin-angiotensin system in diabetes: fuctional, immunohistochemical, and molecular biological correlations. Am J Physiol 1993; 265: F477F486. 2. Kaplan NM. Renal Parenchymal Hypertension in Clinical Hypertension 7th edition. Williams & Wilkins publishing. Philadelphia, 1998. 3. National High Blood Pressure Education Program. National High Blood Pressure Program Working Group report on hypertension and chronic renal failure. Arch Intern Med 151:128066, 1991. 4. Ruilupe LM, Campo C, Rodriguez-Artalejo F, et al. Blood pressure and renal function: therapeutic inplications. J Hypertens. 1996; 14: 1259-1263. 5. Schlueter WA, Batle DC. Renal effects of antihypertensive drugs. Drugs 37:900-25, 1989. 6. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1997, 157: 2413-2445. 7. Working Group. 1995 Update of the working group reports on chronic renal failure and renovascular hypertension (NIH publication no. 95-3791). Washington DC, Nation Heart, Lung and Blood Institute. Oct 1995.
Potrebbero piacerti anche
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Anti-Hypertensive 2Documento49 pagineAnti-Hypertensive 2pushpaNessuna valutazione finora
- Hypertension and KidneyDocumento34 pagineHypertension and KidneyanandababuNessuna valutazione finora
- Renal Artery Stenosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandRenal Artery Stenosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsValutazione: 5 su 5 stelle5/5 (1)
- Pharmacology 3 - Management of Heart FailureDocumento59 paginePharmacology 3 - Management of Heart Failurealbatros000Nessuna valutazione finora
- Antihypertensive Drugs RTDocumento41 pagineAntihypertensive Drugs RTMaherNessuna valutazione finora
- Pharm CH 11 AntihypertensivesDocumento42 paginePharm CH 11 AntihypertensivesDaniel AdamsNessuna valutazione finora
- Drugs Used in Heart FailureDocumento27 pagineDrugs Used in Heart Failurealeah morenoNessuna valutazione finora
- Cardiovascular Agents PDFDocumento118 pagineCardiovascular Agents PDFgherlethrNessuna valutazione finora
- Emergency Drugs: A Review: Jeselo O. Gorme, RNDocumento71 pagineEmergency Drugs: A Review: Jeselo O. Gorme, RNdodong skyroseNessuna valutazione finora
- Cardiovascular Drugs 4Documento31 pagineCardiovascular Drugs 4ismailaiaibrahimNessuna valutazione finora
- Pharmacology Semi FinalsDocumento269 paginePharmacology Semi FinalsTrishaNessuna valutazione finora
- Anti Hypertensive Drugs - DiureticsDocumento49 pagineAnti Hypertensive Drugs - DiureticsApurba Sarker Apu100% (1)
- Antihypertensives - Nursing 2Documento88 pagineAntihypertensives - Nursing 2Cyril Selorm LotameNessuna valutazione finora
- Important Complications of Chronic Kidney Disease: Continuing Medical EducationDocumento4 pagineImportant Complications of Chronic Kidney Disease: Continuing Medical EducationAn-Nisa Khoirun UmmiNessuna valutazione finora
- Stages of Chronic Kidney Disease Stage Description GFR Ml/min/1.73mDocumento4 pagineStages of Chronic Kidney Disease Stage Description GFR Ml/min/1.73mMegan SamsonNessuna valutazione finora
- Cardiac DrugsDocumento35 pagineCardiac DrugsCristina Centurion100% (3)
- Diuretics: PHRM 306: Drugs Affecting CVSDocumento51 pagineDiuretics: PHRM 306: Drugs Affecting CVSEjaj SumitNessuna valutazione finora
- Nephrotic Syndrome + ArfDocumento64 pagineNephrotic Syndrome + ArfkrishnasreeNessuna valutazione finora
- AntiHypertensives (Autosaved)Documento64 pagineAntiHypertensives (Autosaved)UsamaNessuna valutazione finora
- Drugs Acting On Cardiovascular SystemDocumento81 pagineDrugs Acting On Cardiovascular SystemevaNessuna valutazione finora
- Pharmacotherapy of Hypertention TerbaruDocumento45 paginePharmacotherapy of Hypertention TerbarulisaNessuna valutazione finora
- HTN Treatment DR - VishvasDocumento46 pagineHTN Treatment DR - VishvasvishvasNessuna valutazione finora
- Heart Diseases Can Be Grouped Into 3 Major Disorders:: - Cardiac Failure - Ischemia - Cardiac ArrhythmiaDocumento24 pagineHeart Diseases Can Be Grouped Into 3 Major Disorders:: - Cardiac Failure - Ischemia - Cardiac Arrhythmiablah4020Nessuna valutazione finora
- Chapter 11 Antihypertensive AgentsDocumento11 pagineChapter 11 Antihypertensive AgentsChristine Annmarie TapawanNessuna valutazione finora
- Antihypertensives Cardiovascular PharmacologyDocumento52 pagineAntihypertensives Cardiovascular PharmacologyAlan LealNessuna valutazione finora
- Chapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsDocumento5 pagineChapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsErika Joy Cabison TamayoNessuna valutazione finora
- Cardiovascular Drugs Gizi DR DianDocumento56 pagineCardiovascular Drugs Gizi DR DianTriana Dessy FitriantiNessuna valutazione finora
- 1 Antihypertensive DrugsDocumento14 pagine1 Antihypertensive DrugsReda SoNessuna valutazione finora
- Anti Hypertensive 20191211Documento35 pagineAnti Hypertensive 20191211helloitsmenadNessuna valutazione finora
- ACE INHIBITORS & ARBsDocumento31 pagineACE INHIBITORS & ARBsMaria khurshidNessuna valutazione finora
- Anti HypertensionDocumento62 pagineAnti HypertensionHazazi Jr Love LoverpoolNessuna valutazione finora
- 10-11 Treatment of HypertensionDocumento11 pagine10-11 Treatment of HypertensionHanif GandohNessuna valutazione finora
- Chapter 13 Drugs Used in Heart FailureDocumento7 pagineChapter 13 Drugs Used in Heart FailureChristine Annmarie TapawanNessuna valutazione finora
- Challenges Diuretics CasebasedDocumento13 pagineChallenges Diuretics CasebasedDaniel MelendezNessuna valutazione finora
- Inhibitors of AngiotensinDocumento37 pagineInhibitors of AngiotensinBoyu GrtrNessuna valutazione finora
- Lecture 6 Anti HypertensionDocumento40 pagineLecture 6 Anti HypertensionMNGS StudioNessuna valutazione finora
- Jurnal Penatalaksanaan EdemaDocumento7 pagineJurnal Penatalaksanaan EdemaMariska Nada Debora100% (1)
- 6 CVS Lecture 5 - Drugs For Heart FailureDocumento55 pagine6 CVS Lecture 5 - Drugs For Heart FailureCraig DuHaneyNessuna valutazione finora
- Anti HypertensivesDocumento21 pagineAnti HypertensivesDivya RanasariaNessuna valutazione finora
- Sec1 Clinical2 (ARF)Documento44 pagineSec1 Clinical2 (ARF)ahmedmohamed01153159469Nessuna valutazione finora
- ACE Inhibitors & Angiotensin II Antagonists: October 1997Documento4 pagineACE Inhibitors & Angiotensin II Antagonists: October 1997indee533Nessuna valutazione finora
- Antihypertensive Drugs: S. Parasuraman, M.Pharm., PH.D.Documento44 pagineAntihypertensive Drugs: S. Parasuraman, M.Pharm., PH.D.Shreya SinhaNessuna valutazione finora
- Uia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREDocumento4 pagineUia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREfadhiliNessuna valutazione finora
- Drugs of CvsDocumento32 pagineDrugs of CvsAgus HaryantoNessuna valutazione finora
- Hypertension Lecture3: Pharmacological TreatmentDocumento25 pagineHypertension Lecture3: Pharmacological TreatmentRam NiwasNessuna valutazione finora
- Drug Induced Kidney DiseasesDocumento34 pagineDrug Induced Kidney DiseasesManhal A AbdulkaderNessuna valutazione finora
- Other Diuretics Final 2017Documento4 pagineOther Diuretics Final 2017Anonymous sSuBudwdNessuna valutazione finora
- Approach ConsiderationsDocumento5 pagineApproach ConsiderationsGunawan SetiawanNessuna valutazione finora
- Blood Pressure Medications Lecture 2020 4 Pod CastsDocumento46 pagineBlood Pressure Medications Lecture 2020 4 Pod CastsfbjsjdfhNessuna valutazione finora
- DiureticsDocumento3 pagineDiureticsCarl Simon CalingacionNessuna valutazione finora
- Pharmacology Assignment 3Documento31 paginePharmacology Assignment 3Tujiyye kooNessuna valutazione finora
- Approach To Patient With HypertensionDocumento64 pagineApproach To Patient With HypertensionAndrassy Twinkle AlineaNessuna valutazione finora
- ObjectivesDocumento39 pagineObjectiveskiranstNessuna valutazione finora
- Lecture 1 antihypertensionSDSDocumento7 pagineLecture 1 antihypertensionSDSSara AbbasNessuna valutazione finora
- Book Review (Writing) : Indriyani (1740601042)Documento8 pagineBook Review (Writing) : Indriyani (1740601042)Indri YaniNessuna valutazione finora
- CVS PharmacologyDocumento60 pagineCVS PharmacologyGølà Sèèñàà–baale irraaNessuna valutazione finora
- Antihypertensive DrugsDocumento37 pagineAntihypertensive Drugsleiann_jessicaNessuna valutazione finora
- Vasodilators by Hiren PatelDocumento28 pagineVasodilators by Hiren PatelHiren_Patel_2427Nessuna valutazione finora
- Evaluating Hospital Strategies For Reducing 30 Day Readmission Rates BDocumento13 pagineEvaluating Hospital Strategies For Reducing 30 Day Readmission Rates BAndri wijayaNessuna valutazione finora
- Cleft Lip in Children - Questions About Treating Cleft Lip in Children On JustAnswerDocumento2 pagineCleft Lip in Children - Questions About Treating Cleft Lip in Children On JustAnswerAndri wijayaNessuna valutazione finora
- SCM 34 440Documento27 pagineSCM 34 440Andri wijayaNessuna valutazione finora
- Types of Cleft LipDocumento2 pagineTypes of Cleft LipAndri wijayaNessuna valutazione finora
- An Initial Description of A Sonographic Sign That VerifiesDocumento5 pagineAn Initial Description of A Sonographic Sign That VerifiesAndri wijayaNessuna valutazione finora
- Morning Report Dokter IGD RSUD Bengkalis: Kamis, 14 Maret 2019 Oleh: Dr. Said Muzani Dr. Dian NoviasariDocumento34 pagineMorning Report Dokter IGD RSUD Bengkalis: Kamis, 14 Maret 2019 Oleh: Dr. Said Muzani Dr. Dian NoviasariAndri wijayaNessuna valutazione finora
- SSH Premix TetanggaDocumento1 paginaSSH Premix TetanggaAndri wijayaNessuna valutazione finora
- ReferencesDocumento3 pagineReferencesAndri wijayaNessuna valutazione finora
- Hematoma EpiduralDocumento15 pagineHematoma EpiduralAndri wijayaNessuna valutazione finora
- Acute Respiratory Distress SyndromDocumento12 pagineAcute Respiratory Distress SyndromAndri wijayaNessuna valutazione finora
- Kurva TB BB 2-20 TahunDocumento1 paginaKurva TB BB 2-20 Tahundibo_malmsteenNessuna valutazione finora
- Ort1-1 2 PDFDocumento24 pagineOrt1-1 2 PDFAndri wijayaNessuna valutazione finora
- Pott Disease PDFDocumento5 paginePott Disease PDFAndri wijayaNessuna valutazione finora
- Hemorrhagic Stroke WorkupDocumento10 pagineHemorrhagic Stroke WorkupAndri wijayaNessuna valutazione finora
- Ophthalmia NeonatorumDocumento2 pagineOphthalmia NeonatorumjudssalangsangNessuna valutazione finora
- Hemorrhagic Stroke Clinical PresentationDocumento11 pagineHemorrhagic Stroke Clinical PresentationAndri wijayaNessuna valutazione finora
- JNC 7 (Klasifikasi Hipertensi) PDFDocumento2 pagineJNC 7 (Klasifikasi Hipertensi) PDFAbdur RahmanNessuna valutazione finora
- Unsafe Abortion: Fifth EditionDocumento55 pagineUnsafe Abortion: Fifth EditionAndri wijayaNessuna valutazione finora
- Hubungan Terjadinya Stroke Pada Pasien Diabetes Mellitus Di Rsu Dr. SoetomoDocumento1 paginaHubungan Terjadinya Stroke Pada Pasien Diabetes Mellitus Di Rsu Dr. SoetomoAndri wijayaNessuna valutazione finora
- Hypertension JNC 7Documento7 pagineHypertension JNC 7Syahrurrahman BokowNessuna valutazione finora
- Pengaruh Anestesi Spinal Terhadap Hemodinamik Padapenderita Dengan Seksio SesareaDocumento25 paginePengaruh Anestesi Spinal Terhadap Hemodinamik Padapenderita Dengan Seksio SesareaAndri wijayaNessuna valutazione finora
- Pediatric Cleft Lip and PalateDocumento6 paginePediatric Cleft Lip and PalateAndri wijayaNessuna valutazione finora
- Morning Report TGL 28 - 3 2012Documento23 pagineMorning Report TGL 28 - 3 2012Andri wijayaNessuna valutazione finora
- Target Range For Glycemic Control: 80-140 MG/DL (Generally 110 MG/DL)Documento3 pagineTarget Range For Glycemic Control: 80-140 MG/DL (Generally 110 MG/DL)Otchi Pudtrie Wijaya100% (1)
- Hypertensive Disorders of PregnancyDocumento8 pagineHypertensive Disorders of PregnancyAndri wijayaNessuna valutazione finora
- 108 188 1 SMDocumento7 pagine108 188 1 SMAndri wijayaNessuna valutazione finora
- DIC Pregnancy 2009Documento2 pagineDIC Pregnancy 2009Andri wijayaNessuna valutazione finora
- HELLP SyndromeDocumento4 pagineHELLP SyndromeCésar Javier Adrianzén TelloNessuna valutazione finora
- Makalah Herbal MedicineDocumento8 pagineMakalah Herbal MedicineAndri wijayaNessuna valutazione finora
- A Presentation On Congenital HyperthyroidismDocumento26 pagineA Presentation On Congenital Hyperthyroidismkriti kaushalNessuna valutazione finora
- Pricelist 13 Juli 2020Documento21 paginePricelist 13 Juli 2020Achmad Sya'idNessuna valutazione finora
- SEMINAR 3 Neoplastic, Myeloproliferative and Myelodysplastic DisordersDocumento6 pagineSEMINAR 3 Neoplastic, Myeloproliferative and Myelodysplastic DisordersMICHELLE RAPELONessuna valutazione finora
- Penerapan PMKP RS Arjaty Daud 2022 UPDATEDocumento15 paginePenerapan PMKP RS Arjaty Daud 2022 UPDATERUNI DARYANTI100% (1)
- Diseases of The Skeletal SystemDocumento20 pagineDiseases of The Skeletal Systemlateef ramonNessuna valutazione finora
- Lesson 2 - Administrative Order No. 2021-0037Documento10 pagineLesson 2 - Administrative Order No. 2021-0037Marjan CalzadoNessuna valutazione finora
- Adorio Partograph ScenarioDocumento2 pagineAdorio Partograph Scenariojonathan liboonNessuna valutazione finora
- Pnpa Requirement 2019Documento5 paginePnpa Requirement 2019Michael Angelo SantosNessuna valutazione finora
- Hyper Calc Emi ADocumento31 pagineHyper Calc Emi AFatima SajidNessuna valutazione finora
- Angeles University Foundation: I) Clinical PathologyDocumento20 pagineAngeles University Foundation: I) Clinical PathologyKaye ManalastasNessuna valutazione finora
- TIFF X DAN 6 Week Shred III Workout Program Schedule v2Documento9 pagineTIFF X DAN 6 Week Shred III Workout Program Schedule v2808ricksmithNessuna valutazione finora
- PHAR 400 Pharmacology I Master 1-3-21Documento5 paginePHAR 400 Pharmacology I Master 1-3-21Zahid Bashir BhattiNessuna valutazione finora
- Procedure Study - Oxygen TherapyDocumento4 pagineProcedure Study - Oxygen TherapyFaye AseoNessuna valutazione finora
- Advanced Life Support (Training Manual)Documento74 pagineAdvanced Life Support (Training Manual)Matt100% (25)
- Autism Spectrum Disorders: A Booklet For Parents and CarersDocumento40 pagineAutism Spectrum Disorders: A Booklet For Parents and CarersAndreea SanduNessuna valutazione finora
- Physical Fitness Test Body Composition/Cardiovascular Tests: Lesson 2 For 1 Hour Day 2 Week 2 Quarter 1Documento36 paginePhysical Fitness Test Body Composition/Cardiovascular Tests: Lesson 2 For 1 Hour Day 2 Week 2 Quarter 1Elmar MariñasNessuna valutazione finora
- Dr. Peter McCullough - COVID Vaccines Have Already Killed 50,000 Americans.Documento7 pagineDr. Peter McCullough - COVID Vaccines Have Already Killed 50,000 Americans.chingatchgook80% (5)
- Brugada SyndromeDocumento5 pagineBrugada SyndromevitriaNessuna valutazione finora
- Theories of NeurosisDocumento170 pagineTheories of NeurosisemilvulcuNessuna valutazione finora
- Description:: Dance Therapy "In The Mood of Dancing"Documento2 pagineDescription:: Dance Therapy "In The Mood of Dancing"kristine_silangNessuna valutazione finora
- HSN CodesDocumento50 pagineHSN CodesManoj T PNessuna valutazione finora
- Guidelines On Dental Record KeepingDocumento8 pagineGuidelines On Dental Record KeepingXubair AhmedNessuna valutazione finora
- Diagnosis and Management of COPD: A Case Study: RespiratoryDocumento4 pagineDiagnosis and Management of COPD: A Case Study: RespiratoryUssy TsnnnNessuna valutazione finora
- Understanding Medical Surgical Nursing - 0843-0843Documento1 paginaUnderstanding Medical Surgical Nursing - 0843-0843Anas TasyaNessuna valutazione finora
- Preliminary Report of Hiv and Toxoplasma Gondii Occurrence in Pregnant Women From MozambiqueDocumento5 paginePreliminary Report of Hiv and Toxoplasma Gondii Occurrence in Pregnant Women From MozambiqueBla BlaNessuna valutazione finora
- NIV - Past, Present and FutureDocumento9 pagineNIV - Past, Present and FutureDejan ŽujovićNessuna valutazione finora
- Orthodontic Treatment in Systemic DisordersDocumento9 pagineOrthodontic Treatment in Systemic DisordersElizabeth Diaz BuenoNessuna valutazione finora
- Daftar PustakaDocumento2 pagineDaftar PustakaS R PanggabeanNessuna valutazione finora
- Afp Surveillance 21st Century 0Documento25 pagineAfp Surveillance 21st Century 0cavmichaelNessuna valutazione finora
- Parafin Sept 2011Documento28 pagineParafin Sept 2011Sarin AvniNessuna valutazione finora
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (169)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (3)
- Gut: the new and revised Sunday Times bestsellerDa EverandGut: the new and revised Sunday Times bestsellerValutazione: 4 su 5 stelle4/5 (392)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDa EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningValutazione: 4 su 5 stelle4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceDa EverandTo Explain the World: The Discovery of Modern ScienceValutazione: 3.5 su 5 stelle3.5/5 (51)
- An Autobiography of Trauma: A Healing JourneyDa EverandAn Autobiography of Trauma: A Healing JourneyValutazione: 5 su 5 stelle5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisDa EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (9)