Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Q-18-Jul-FIMS CBL - IHD
Caricato da
rieuxCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Q-18-Jul-FIMS CBL - IHD
Caricato da
rieuxCopyright:
Formati disponibili
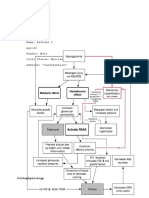
CBL 1 Ischemic heart disease Chapter 243
What are the three major determinants of myocardial o2 demand? Heart rate Myocardial contractility Myocardial wall tension (stress)
What are the three major components to coronary blood flow resistance and what is their relative contribution? R1 large epicardial arteries R2 pre-arteriolar vessels R3 Intra-myocardial small vessels
In the absence of significant atherosclerotic obstruction, resistance in R1 is trivial, with R2 & 3 the major determinants
What factors determine the ischemic changes are reversible or permanent? The severity and duration of imbalance between myocardial oxygen supply and demand. <20 min for total occlusion in the absence of collaterals reversible >20 min myocardial necrosis
What does the term ischaemic cardiomyopathy refer to? Patients with IHD who present with cardiomegaly and heart failure secondary to ischaemic damage to the LV myocardium, that may have caused no symptoms prior to the development of heart failure
What does the typical patient with stable angina pectoris present like? Man >50 or woman >60 Complains of episodes of chest discomfort o Described as heaviness, pressure, squeezing, smothering or choking and rarely as flank pain When asked to localise pain, patient often places a clenched fist over the sternum (Levines sign)
How does angina pain present? The pain is usually crescendo-decrescendo in nature Last 2-5 mins
Can radiate to either shoulder and to both arms, especially the ulnar surfaces of forearm and hand Can also arise in or originate in to the back, intra-scapular region, root of neck, teeth and epigastrium Angina is rarely localised below the umbilicus or above the mandible
What important questions need to be asked to assess whether stable angina is progressing to the unstable syndrome? Is the pain occurring with less exertion than in the past? Is the pain occurring at rest? Is the pain or symptoms awakening you?
How what is the positive predictive value of a positive stress test in a male over 55 years with a history or typical angina pectoris like chest pain? 98% likelihood of CAD in this patient Decreased likelihood if atypical or no chest pain by history and/or during the test
In what populations are the rates of false positive stress tests increased? In pts with low probability of IHD, such as assymptomatic men <40 yrs, or premenopausal women with no risk factors of premature atherosclerosis. Also increased in pts taking cardioactive drugs, such as digitalis, and antiarrythmic agents, and those with intraventricular conductance disturbances, resting ST segment and T-wave abnormalities, ventricular hypertrophy or abnormal K+ level
Which patients may be at an increased risk of false negative results? Patients with disease confined to the circumflex artery as the lateral potion of the heart that this vessel supplies is not well represented on a 12 lead ECG
What is the overall sensitivity of stress testing? What is less likely given a negative stress test? Overall sensitivity of 75% Three vessel disease or left main disease is extremely unlikely given a negative stress test
What are the important parameters recorded by the physician at completion of an exercise stress test? Total duration of test The time to onset of ischemic ST-segment change and chest discomfort The external work performed (generally expressed as stage reached) Internal cardiac work performed (product of HR and BP) Depth of ST-segment depression and the time needed for this to recovery on ECG
What are the contraindications to exercise stress testing? How soon after can an exercise stress test be performed in pts following an uncomplicated MI? Rest angina within 48 hrs Unstable rhythm Severe aortic stenosis Acute myocarditis Uncontrolled heart failure Severe pulmonary hypertension Active infective endocarditis
Stress testing can be performed as early as 6 days following an uncomplicated MI using a modified protocol limited via heart rate rather than symptoms
What ECG changes during a stress test are used to define the ischemic ST-segment response? Defined as flat or downsloping depression of the ST-segment >0.1mV below baseline lasting longer than 0.08s
What other factors lead to discontinuation of a exercise stress test? Evidence of chest discomfort Severe shortness of breath Dizziness Severe fatigue ST-segment depression >0.2mV (2mm) A fall in SBP >10mmHg Development of a ventricular tachyarrhythmia
What is the normal HR and BP response during a graded exercise stress test? What does an absence of these characteristic changes indicate? Normal response is a progressive increase in both HR and BP in response to exercise Failure of blood pressure to increase, or a fall in BP with signs of ischaemia during a stress test is an important prognostic sign, as it may reflect ischaemia-induced global left ventricular dysfunction
What atherosclerotic plaques cannot be visualised during coronary arteriography? This method outlines the lumina of the coronary arteries, thus, only plaques that encroach on the coronary lumen can be detect This is of note as many plaques start growth in the intima and media (causing an outward bulging of the artery) before encroaching into the lumen (process referred to as remodelling)
What are the indications for coronary arteriography? Patients with chronic stable angina pectoris who are severely symptomatic despite medical therapy and are being considered for revascularisation (PCI or CABG) Patients with troublesome symptoms that present diagnostic difficulties in whom there is need to confirm or rule out the diagnosis of IHD Patient with known or possible angina pectoris who have survived sudden cadiac arrest Patients with angina or evidence of ischaemia on non-invasive testing with clinical or laboratory evidence of ventricular dysfunction Patients judged to be high risk of sustaining coronary events based on signs of severe ischaemia on noninvasive testing, regardless of the presence or severity of symptoms
What are the main risk factors that can be addressed in a pt with IHD? Obesity impairs the treatment of other risk factors and is accompanied by o Hypertension, hyperlipidemia and hyperglycemia (T2DM) Diet: low in saturated and trans-saturated fatty acids and a reduced caloric intake to achieve optimal body weight Cigarette smoking accelerates coronary artherosclerosis in both sexes and all ages, increased risk of thrombosis, plaque instability, MI and death. In addition, smoking increases myocardial O2 demands and reduces supply exacerbating angina symptoms. Hypertension increased adverse events, LVH etc. Diabetes mellitus Treatment of dyslipidemia HMG CoA reductase inhibitors, lower LDL cholesterol (25-50%), raise HDL cholesterol (5-9%), lower triglycerides (5-30%)
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Practice StripsDocumento9 paginePractice StripsErica Yamamoto50% (4)
- Shortness of Breath: Checklist PMPF Checklist PMPFDocumento1 paginaShortness of Breath: Checklist PMPF Checklist PMPFanz_4191Nessuna valutazione finora
- 2010 Postgraduate Statement of Fees and General ConditionsDocumento6 pagine2010 Postgraduate Statement of Fees and General ConditionsrieuxNessuna valutazione finora
- ENT CPC - Tonsil ProblemsDocumento3 pagineENT CPC - Tonsil ProblemsrieuxNessuna valutazione finora
- Nephritic NephroticDocumento1 paginaNephritic NephroticrieuxNessuna valutazione finora
- LithiumDocumento2 pagineLithiumrieuxNessuna valutazione finora
- Summary of Medical StandardsDocumento3 pagineSummary of Medical StandardsGuilherme CruzNessuna valutazione finora
- Indian Oil Corporation Ltd. Guidelines and Criteria For Physical Fitness For Pre-Employment Medical ExaminationDocumento11 pagineIndian Oil Corporation Ltd. Guidelines and Criteria For Physical Fitness For Pre-Employment Medical ExaminationShub SamNessuna valutazione finora
- Old CartsDocumento3 pagineOld CartsinggitluthfiazahraNessuna valutazione finora
- Management of Acute Abdomen in Pregnancy Current PerspectivesDocumento16 pagineManagement of Acute Abdomen in Pregnancy Current PerspectivesjessicapxeNessuna valutazione finora
- Cardiac RegenerationDocumento5 pagineCardiac RegenerationBenyam ZenebeNessuna valutazione finora
- Pulmo Viewboxes BLOCK 8Documento251 paginePulmo Viewboxes BLOCK 8U.P. College of Medicine Class 2014100% (2)
- CH 04 Clicker QuestionsDocumento53 pagineCH 04 Clicker QuestionsCharmane Sherisse DumlaoNessuna valutazione finora
- Eisenmenger SyndromeDocumento6 pagineEisenmenger SyndromeWarkah SanjayaNessuna valutazione finora
- Elective Cardioversion: Critical Care Unit (CCU) The Horton General HospitalDocumento8 pagineElective Cardioversion: Critical Care Unit (CCU) The Horton General HospitalEzraGoenadiNessuna valutazione finora
- Weaning Ventilator Protocol For LiberationDocumento3 pagineWeaning Ventilator Protocol For LiberationBonny ChristianNessuna valutazione finora
- Tanaman Beracun Di Sekitar KitaDocumento33 pagineTanaman Beracun Di Sekitar KitaDenny Yogiantara HerlambangNessuna valutazione finora
- SCIENCE 9 (1) - MELC 1 - Reviewed by CommitteeDocumento13 pagineSCIENCE 9 (1) - MELC 1 - Reviewed by CommitteeBayani VicencioNessuna valutazione finora
- EACVI Multimodality Imaging of Native Valvular RegDocumento62 pagineEACVI Multimodality Imaging of Native Valvular RegВенцислав МирчевNessuna valutazione finora
- 13.30 DR Arunraj Navaratnarajah - The Septic PatientDocumento49 pagine13.30 DR Arunraj Navaratnarajah - The Septic PatientagusNessuna valutazione finora
- IV FluidsDocumento7 pagineIV FluidsAmy LalringhluaniNessuna valutazione finora
- Biopsy Interpretation of The Liver First Edition Michael TorbensonDocumento540 pagineBiopsy Interpretation of The Liver First Edition Michael TorbensonByron Gonzalez UsmaNessuna valutazione finora
- Venous Thromboembolism (VTE) : Quality DepartmentDocumento28 pagineVenous Thromboembolism (VTE) : Quality DepartmentDIGITAL 143Nessuna valutazione finora
- CCP Vs NCCPDocumento4 pagineCCP Vs NCCParn0ld21Nessuna valutazione finora
- 5 FAST Facts About Stroke Infographic Ucm500739Documento1 pagina5 FAST Facts About Stroke Infographic Ucm500739roseNessuna valutazione finora
- Thesis Statement Heart DiseaseDocumento7 pagineThesis Statement Heart Diseasexgkeiiygg100% (2)
- Horner'S Syndrome - : Far Eastern University - Nicanor Reyes Medical FoundationDocumento3 pagineHorner'S Syndrome - : Far Eastern University - Nicanor Reyes Medical FoundationVictorija Evania Lucille DeldioNessuna valutazione finora
- NICUDocumento45 pagineNICU렌이비드Nessuna valutazione finora
- TestBank Lewis Medical Surgical Nursing 11th 2020.pdf-282-305Documento24 pagineTestBank Lewis Medical Surgical Nursing 11th 2020.pdf-282-305هدوء النسمةNessuna valutazione finora
- Seminar Conduction System of HeartDocumento61 pagineSeminar Conduction System of HeartKirtishAcharyaNessuna valutazione finora
- Mattox Trauma 8th Edition - PDF 2Documento16 pagineMattox Trauma 8th Edition - PDF 2Meri YeghiazaryanNessuna valutazione finora
- Veratrum VirideDocumento5 pagineVeratrum VirideSuhas IngaleNessuna valutazione finora
- CKD Case StudyDocumento8 pagineCKD Case StudyEspiridionNessuna valutazione finora
- Cardiology MCQDocumento2 pagineCardiology MCQmohamed mowafeyNessuna valutazione finora