Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Dysfunctional Uterine Bleeding
Caricato da
Bubblets Margaux GoldiDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Dysfunctional Uterine Bleeding
Caricato da
Bubblets Margaux GoldiCopyright:
Formati disponibili
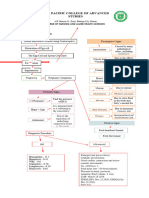
Dysfunctional uterine bleeding (DUB) is abnormal uterine bleeding in terms of amount, duration, or timing during the menstrual cycle,
with no discernible organic cause. The normal menstrual cycle is dependent on the influence of four hormones: estrogen, which predominates during the proliferative phase (generally days 1 to 14); progesterone, which predominates during the secretory phase (generally days 15 to 28); and follicle-stimulating hormone (FSH) and luteinizing hormone (LH), both of which stimulate the ovarian follicle to mature. Disrupting the balance of these four hormones usually results in anovulation and dysfunctional uterine bleeding. During an anovulatory cycle, the corpus luteum does not form and thus progesterone is not secreted. Failure of progesterone secretion allows continuous unopposed production of estradiol, which stimulates the overgrowth of the endometrium. This results in an overproduction of the uterine blood flow. Complications of dysfunctional uterine bleedinginclude anemia, infection from prolonged use of tampons, and in rare situations, hemorrhagicshock. As many as 10% of women with normal ovulatory cycles experience dysfunctional uterine bleeding. The cause of dysfunctional uterine bleeding is unknown. The term dysfunctional uterine bleedingindicates that abnormal bleeding is occurring without an organic cause. It is associated with polycystic ovarian disease and obesity; in both of these conditions, the endometrium is chronically stimulated by estrogen. Other possible associated factors are: cancer of the vagina, cervix, ovaries, and uterus; polyps, ectopic pregnancy, or molar pregnancy; and excessive weight gain, stress, and increased exercise performance. Nursing care plan assessment and physical examination Determine the duration of the present bleeding, the amount of blood loss, and the presence of associated symptoms such as cramping, nausea, and vomiting, fever, abdominal pain, or passing of blood clots. Ask the patient to compare the amount of pads or tampons used in a normal period with the amount they are presently using. Obtain a menstrual and obstetric history. Recent episodes of easy bruising or prolonged, heavy bleeding may indicate abnormal clotting times. The use of contraceptives, especially an intrauterine device (IUD), may contribute to abnormal uterine bleeding. Other possible causative factors, such as pregnancy, pelvic inflammatory disease, or other medical conditions, can be ruled out through a complete history. A complete examination is essential to eliminate organic causes of bleeding. A pelvic speculum and bimanual examination should be done, with particular attention to the presence of cervical erosion, polyps, presumptive signs of pregnancy, masses, tenderness or guarding, or other signs of pathology that may cause abnormal uterine bleeding. Assess for petechiae, purpura, and mucosal bleeding (gums) to rule out hematologic pathology. Check for pallor and absence of conjunctival vessels to gauge anemia. For many women, dysfunctional uterine bleeding results in distress related to the uncertainty of the timing, duration, and amount of bleeding. A woman may feel that her usual activities need to
be curtailed, a situation that may contribute to feelings of loss of control. Assess the womans concerns and coping patterns to establish a framework for determining appropriate interventions. Nursing care plan primary nursing diagnosis: Fluid volume deficit related to blood loss. Nursing care plan intervention and treatment The patient may be confronted with a prolonged evaluation and a variety of treatments before uterine bleeding resumes a more normal pattern or stops completely. Activities are not restricted and can be continued as the woman tolerates them. If infection or anemia is identified, appropriate pharmacologic therapy is initiated. Hormonal manipulation may be indicated, requiring careful dosing and attention to compliance with the treatment plan. Surgical management typically begins with dilation and curettage to remove excessive endometrial buildup, but may include intrauterine cryosurgery, laser ablation of the endometrium, or as a last resort, a hysterectomy. Important interventions include strategies to assist the woman in maintaining normal activities during the evaluation. Instruct the woman about the signs and symptoms of toxic shock syndrome (fever, joint and muscle aches, malaise, weakness) if she continues to use tampons; more frequent than normal changes of the tampon may be indicated. The use of incontinence pads may be more beneficial than the standard feminine napkin in the presence of heavy bleeding. Issues related to sexuality, especially if hysterectomy is indicated, require an accepting, open attitude of the nurse. The woman may feel her femininity is threatened but may have difficulty expressing these feelings. You may need to initiate discussions regarding the impact of evaluation and treatment on the woman. If appropriate, consider the effect on the womans partner and include the partner in all discussions. Nursing care plan discharge and home health care guidelines Provide a list of prescribed medications, if any, that includes the name, dosage, route, and side effects and the signs and symptoms of potential complications, including hypotensive episodes. Explain the need for careful monitoring and follow-up of the bleeding. Encourage the patient to keep a menstrual calendar and record daily bleeding patterns. Teach the patient to have appropriate laboratory follow-up of the complete blood count if indicated.
Potrebbero piacerti anche
- Uterine Bleeding-A Case StudyDocumento4 pagineUterine Bleeding-A Case StudyRoanne Lagua0% (1)
- Dysfunctional Uterine BleedingDocumento7 pagineDysfunctional Uterine BleedingNhorz Love UNessuna valutazione finora
- Abnormal Uterine BleedingDocumento7 pagineAbnormal Uterine BleedingBrian Fry100% (1)
- MenorrhagiaDocumento44 pagineMenorrhagiaHugh Jacobs100% (1)
- Dysfunctional Uterine Bleeding: Prepared By: Sabnam Gurung Roll No:31Documento39 pagineDysfunctional Uterine Bleeding: Prepared By: Sabnam Gurung Roll No:31Sabnam GurungNessuna valutazione finora
- Dysfunctional Uterine Bleedin1Documento15 pagineDysfunctional Uterine Bleedin1Hendy SetiawanNessuna valutazione finora
- Men Orr HagiaDocumento15 pagineMen Orr HagiaJ SNessuna valutazione finora
- Clinical: Section 3 of 10Documento36 pagineClinical: Section 3 of 10coleNessuna valutazione finora
- Yale - Abnormal Uterine Bleeding Preceptor - 389620 - 284 - 45546 - v1Documento12 pagineYale - Abnormal Uterine Bleeding Preceptor - 389620 - 284 - 45546 - v1omegasauron0gmailcomNessuna valutazione finora
- History and Examination: Chapter - 1Documento10 pagineHistory and Examination: Chapter - 1Sameer KhanNessuna valutazione finora
- The Gynecologic History and Pelvic Examination Up To Date 2016Documento14 pagineThe Gynecologic History and Pelvic Examination Up To Date 2016Mateo GlNessuna valutazione finora
- Abnormal Uterine BleedingDocumento3 pagineAbnormal Uterine BleedingNura ZeinNessuna valutazione finora
- Updated InterpretationDocumento4 pagineUpdated InterpretationIRA MONIQUE CABADENNessuna valutazione finora
- Management Abnormal Uterine Bleeding SLCOGDocumento13 pagineManagement Abnormal Uterine Bleeding SLCOGumapathisivanNessuna valutazione finora
- MenorrhagiaDocumento3 pagineMenorrhagiajermie22100% (1)
- Abnormal Uterine Bleeding: The Menstrual CycleDocumento2 pagineAbnormal Uterine Bleeding: The Menstrual CycleindahmahfuzhahNessuna valutazione finora
- Assessment and Management of Female Physiologic ProcessesDocumento4 pagineAssessment and Management of Female Physiologic ProcessesKelseyNessuna valutazione finora
- HP Oct08 AndrogenismDocumento8 pagineHP Oct08 AndrogenismgratianusbNessuna valutazione finora
- LBM 6-Bheta Silfana Ulul AzmiDocumento41 pagineLBM 6-Bheta Silfana Ulul AzminafikayNessuna valutazione finora
- DUB Feb24 - TaggedDocumento22 pagineDUB Feb24 - TaggedsarasamadieNessuna valutazione finora
- Evaluacion de Sangrado UterinoDocumento74 pagineEvaluacion de Sangrado UterinoSaul Gonzalez HernandezNessuna valutazione finora
- AUB StartedDocumento13 pagineAUB StartedIbrahim AbdullahNessuna valutazione finora
- Abnormal Uterine Bleeding in A 39 Year OldDocumento16 pagineAbnormal Uterine Bleeding in A 39 Year OldEliana GerzonNessuna valutazione finora
- January Case AnalysisDocumento20 pagineJanuary Case AnalysisJenny Juniora AjocNessuna valutazione finora
- Hormone Replacement Therapy (HRT) :: DR - FatinDocumento32 pagineHormone Replacement Therapy (HRT) :: DR - FatinAmmarNessuna valutazione finora
- Abnormal Uterine BleedingDocumento8 pagineAbnormal Uterine BleedingEcbNessuna valutazione finora
- Common Problems in Women S Health 19Documento33 pagineCommon Problems in Women S Health 19afifahsalsabilaaaNessuna valutazione finora
- Ectopic PregnancyDocumento36 pagineEctopic PregnancyLorenz BreezNessuna valutazione finora
- OB/Gyn Clinical PearlsDocumento4 pagineOB/Gyn Clinical PearlsD50% (4)
- Abnormal Uterine BleedingDocumento11 pagineAbnormal Uterine BleedingKharmell Waters AndradeNessuna valutazione finora
- Gynecological NursingDocumento329 pagineGynecological Nursingsharon ocharaNessuna valutazione finora
- Background of The Condition:: Those That Put A Person at Risk of Developing A Problem)Documento3 pagineBackground of The Condition:: Those That Put A Person at Risk of Developing A Problem)Genelly Anne Argañoza RamosNessuna valutazione finora
- Threatened Abortion ReportDocumento8 pagineThreatened Abortion ReportMohamad RaisNessuna valutazione finora
- Abnormal MenstruationDocumento18 pagineAbnormal MenstruationDevikha PeremelNessuna valutazione finora
- GG Menstruasi - Dysmenorea DLLDocumento35 pagineGG Menstruasi - Dysmenorea DLLPSC 119 Kota TegalNessuna valutazione finora
- Explo Lap TahbsoDocumento3 pagineExplo Lap TahbsoJustin AlejoNessuna valutazione finora
- Menstrual Disorders 2Documento39 pagineMenstrual Disorders 2Nanang HidayatullohNessuna valutazione finora
- Hyperemesis Gravidarum: By: Solomon Berhe OBGYN ResidentDocumento73 pagineHyperemesis Gravidarum: By: Solomon Berhe OBGYN Residentmuleget haileNessuna valutazione finora
- A Case Study On Ovarian New GrowthDocumento25 pagineA Case Study On Ovarian New GrowthSandra GabasNessuna valutazione finora
- Infertility and Climacteric CrisisDocumento4 pagineInfertility and Climacteric Crisisgeorgeloto12Nessuna valutazione finora
- Investigation and Management of MenorrhagiaDocumento26 pagineInvestigation and Management of MenorrhagiaRahdin Ahmad Faresy Al-HamidiNessuna valutazione finora
- Absent or Irregular PeriodsDocumento6 pagineAbsent or Irregular PeriodsEcbNessuna valutazione finora
- Ectopic Pregnancy Management - 280720Documento10 pagineEctopic Pregnancy Management - 280720SUPRIYA SINGHNessuna valutazione finora
- Infertility PDFDocumento12 pagineInfertility PDFdian_c87100% (1)
- Ectopic Pregancy: Chena B. CurigDocumento35 pagineEctopic Pregancy: Chena B. CurigJaicca Faith Tandih AllasNessuna valutazione finora
- Amenorrhea & Heavy Menstrual BleedingDocumento22 pagineAmenorrhea & Heavy Menstrual BleedingJanesel Plariza PanerioNessuna valutazione finora
- Anovulatory Bleeding - StatPearls - NCBI BookshelfDocumento11 pagineAnovulatory Bleeding - StatPearls - NCBI BookshelfArinilhaquedr.Nessuna valutazione finora
- Postmenopausal Bleeding - StatPearls - NCBI BooksDocumento11 paginePostmenopausal Bleeding - StatPearls - NCBI BooksKalaivathanan VathananNessuna valutazione finora
- 103 Reproductive Disorders & Advanced Techniques IVFDocumento22 pagine103 Reproductive Disorders & Advanced Techniques IVFShital PatelNessuna valutazione finora
- Management of Abnormal Uterine Bleeding - UpToDateDocumento25 pagineManagement of Abnormal Uterine Bleeding - UpToDatePollyannaLimadeCastroNessuna valutazione finora
- Basic Infertility EvaluationDocumento13 pagineBasic Infertility EvaluationRosu GeorgeNessuna valutazione finora
- AmenorrheaDocumento40 pagineAmenorrheaMeraol HusseinNessuna valutazione finora
- AmenorrheaDocumento13 pagineAmenorrheaJanesel Plariza PanerioNessuna valutazione finora
- Dysfunctional Uterine BleedingDocumento8 pagineDysfunctional Uterine BleedingJet BautistaNessuna valutazione finora
- Faq 147Documento3 pagineFaq 147Gaylene Munsayac AldaveNessuna valutazione finora
- Oral Health Care For The Pregnant PatientDocumento6 pagineOral Health Care For The Pregnant PatientDominique Harz FresnoNessuna valutazione finora
- Nursing Management of MenopauseDocumento37 pagineNursing Management of MenopauseSuby Beigh82% (11)
- B23. Pathophysiology of PostpartumDocumento8 pagineB23. Pathophysiology of Postpartumjhon heriansyahNessuna valutazione finora
- Case PresDocumento22 pagineCase Presandrei jinNessuna valutazione finora
- Does Premenstrualsyndrome Induces Change in The ANSDocumento1 paginaDoes Premenstrualsyndrome Induces Change in The ANSSailaja NandennagariNessuna valutazione finora
- Examining A Short Stature ChildDocumento7 pagineExamining A Short Stature ChildKhirren RaoNessuna valutazione finora
- B12 Calibrators: SystemDocumento2 pagineB12 Calibrators: SystemQuyet PhungNessuna valutazione finora
- Team Code 34 PDocumento22 pagineTeam Code 34 PShivam TiwaryNessuna valutazione finora
- What Is Doctor of Physical TherapyDocumento7 pagineWhat Is Doctor of Physical TherapyDebra NajiNessuna valutazione finora
- Paida and Lajin Self Healing PDFDocumento10 paginePaida and Lajin Self Healing PDFMelvin Arvizu100% (1)
- Germany CV Format-Sample OnlyDocumento6 pagineGermany CV Format-Sample Onlydeamhi nursing serviceNessuna valutazione finora
- FASENRA - PFS To Pen Communication Downloadable PDFDocumento2 pagineFASENRA - PFS To Pen Communication Downloadable PDFBrîndușa PetruțescuNessuna valutazione finora
- Medical AbbreviationsDocumento54 pagineMedical AbbreviationsHardeep Singh BaliNessuna valutazione finora
- DR List IshwarDocumento18 pagineDR List IshwarIshwar Rajput100% (1)
- Us HealthcareDocumento49 pagineUs HealthcareJerald FernandezNessuna valutazione finora
- Destination 2Documento4 pagineDestination 2oldhastonian0% (1)
- Silver Book Part A Medication Management ID3104Documento7 pagineSilver Book Part A Medication Management ID3104Anton BalansagNessuna valutazione finora
- Prevalensi Dan Dampak Kecanduan Gadget Pada Remaja: Literature ReviewDocumento10 paginePrevalensi Dan Dampak Kecanduan Gadget Pada Remaja: Literature ReviewfazliahNessuna valutazione finora
- Best of Fives For Dentistry 3 ST Ed (2014)Documento179 pagineBest of Fives For Dentistry 3 ST Ed (2014)chimedbator100% (3)
- CSC FORM 41 Med.Documento5 pagineCSC FORM 41 Med.editha salahayNessuna valutazione finora
- Knowledge and Practice Towards Care and MaintenancDocumento7 pagineKnowledge and Practice Towards Care and MaintenancyunishaNessuna valutazione finora
- Excerpt From The Disease Delusion by Dr. Jeffrey S. BlandDocumento12 pagineExcerpt From The Disease Delusion by Dr. Jeffrey S. BlandRachel Jackson100% (2)
- Hepatic EncephalopathyDocumento5 pagineHepatic Encephalopathyliveconnectionz282Nessuna valutazione finora
- Low Back Pain Guidelines-Reduced2Documento26 pagineLow Back Pain Guidelines-Reduced2ranggadr100% (1)
- Critical Apprasisal 2Documento5 pagineCritical Apprasisal 2api-678326591Nessuna valutazione finora
- Eclampsia Nursing Case AnalysisDocumento38 pagineEclampsia Nursing Case AnalysisMary Justine Nuyad-AfricaNessuna valutazione finora
- Standardization of The Definition and Surgical.9Documento11 pagineStandardization of The Definition and Surgical.9JobelleNessuna valutazione finora
- 322-Article Text-1656-1-10-20230630Documento11 pagine322-Article Text-1656-1-10-20230630Bunga nurmala septiaNessuna valutazione finora
- PDF To WordDocumento284 paginePDF To WordVictoria UrsachiNessuna valutazione finora
- Everest Pharmacy Lists 2022 PDFDocumento13 pagineEverest Pharmacy Lists 2022 PDFSuraj PatilNessuna valutazione finora
- Goboy, Louise Germaine U. BSN 210 Self-Assessment QuestionsDocumento2 pagineGoboy, Louise Germaine U. BSN 210 Self-Assessment QuestionsLouise Germaine100% (1)
- Daptomycin Guidance Note - Revision 20200430Documento6 pagineDaptomycin Guidance Note - Revision 20200430Marcelo UGNessuna valutazione finora
- Hyperthermia (Thurs)Documento1 paginaHyperthermia (Thurs)Christine Esguerra OrozcoNessuna valutazione finora
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 4.5 su 5 stelle4.5/5 (82)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (254)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (60)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDa EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisValutazione: 5 su 5 stelle5/5 (8)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (5)
- To Explain the World: The Discovery of Modern ScienceDa EverandTo Explain the World: The Discovery of Modern ScienceValutazione: 3.5 su 5 stelle3.5/5 (51)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedValutazione: 4 su 5 stelle4/5 (61)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (46)