Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Spineadbfvkad
Caricato da
likusajaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Spineadbfvkad
Caricato da
likusajaCopyright:
Formati disponibili
Sholahuddin Rhatomy,MD
ORTHOPAEDIC
SPINE
Sholahuddin Rhatomy MD Orthopaedi UI
1 Orthopaedi UI
Sholahuddin Rhatomy,MD
1. Spine Anatomy 3 2. Spinal injury 13 3. Cervical spine injury 26 4. Thoracolumbal spine trauma 38 5. Sacral fracture 52 6. Cervical disc disease 54 7. Cervical radiculopathy 55 8. Cervical myelopathy 62 9. Rheumatoid spondylitis 68 10. Back pain 73 11. Intravertebral disc disease 74 12. Discogenic pain 75 13. Thoraxic disc prolapse 79 14. Lumbar disc prolapsed79 15. Spondilolisthesis 84 16. Spinal stenosis 88 17. Ankylosing spondylitis95 18. Spine infection 98 19. Spinal metastase 107 20. Prof Brotos lecture 115
2 Orthopaedi UI
Sholahuddin Rhatomy,MD
Spine Anatomy & Biomechanics
BONY ELEMENTS Counteract compressive forces
Cervical Vertebra
3 Orthopaedi UI
Sholahuddin Rhatomy,MD
Thoracic Vertebra
Lumbar Vertebra
SPINAL LIGAMENTS
Resist distractive forces
4 Orthopaedi UI
Sholahuddin Rhatomy,MD
Anterior longitudinal ligament Strongly attached to vertebral body but loosely attached to annulus
Posterior longitudinal ligament Strongly attached to annulus with its fibres penetrating annulus to attach to underlying vertebral body
Ligamentum Flavum (flavum = yellow) Short thick ligament that attaches to laminae & forms anterior capsule of zygoapophyseal joint Histologically contains 80% elastin, 20% collagen
Interspinous ligament Fibres have wide range of orientation with only few passing from 1 spinous process to another Many fibres parallel to spinous processes therefore cannot resist forward bending movements
Supraspinous ligament Not a true ligament, & affords little resistance to separation of spinous processes Terminates at L4 in majority of people A continuation of tendinous fibres of back muscles
INTERVERTEBRAL DISC
5 Orthopaedi UI
Sholahuddin Rhatomy,MD
Annulus fibrosus
Collagen fibres (type I) in lamellae are orientated at an angle ( = 30) to horizontal plane Fibre direction changes in alternating layers by180 This allows motion to be resisted as shown below
Distraction Nucleus pulposus
Shear
Rotation
Thin framework of collagen fibres (type II) with proteoglycan matrix (similar to articular cartilage but with much more fluid consistency) Embedded within this matrix are chondrocytes which are found predominantly in regions of vertebral end plate which serve to maintain components of disc
6 Orthopaedi UI
Sholahuddin Rhatomy,MD
FORAMINAL RELATIONSHIPS
7 Orthopaedi UI
Sholahuddin Rhatomy,MD
DERMATOMES
With advent of fluoroscopically assisted nerve root block there has been accurate assessments made of dermatomal anatomy in neurologically intact individuals They can vary between individuals as to their extent but there are consistent concentric patterns within individuals Diagram below demonstrates dermatomal distribution in different individuals (percentage values are for those in whom at least exhibit particular pattern) Black area: 75% Shaded area: 50% Stippled area: 25%
8 Orthopaedi UI
Sholahuddin Rhatomy,MD
GROWTH
Longitudinal growth effected by growth plate Horizontal growth via periosteal new bone formation Ring apophysis does not contribute to growth
MOTION COUPLING
Instant axis of rotation & centrodes in lumbar spine
9 Orthopaedi UI
Sholahuddin Rhatomy,MD
FREE BODY DIAGRAM
MUSCLE ACTIVITY
In full flexion, very little muscle activity Abdominal muscles have been implicated in aid for back muscle function - intra-abdominal balloon theory but not substantiated For abdominal muscles to offer enough anti-flexion moment, pressure generated would exceed maximal hoop tension of abdominal muscles, & pressure would be so high as to obstruct aorta, & finally they must also exert a flexion moment which would negate any anti-flexion value of raised intra-abdominal pressure
SACROILIAC JOINT
No muscles are designed to act directly in SI joint, as all muscles that cross SIJ act on hip or lumbar spine Studies have been performed to delineate exactly how much movement occurs at SI joint These have included "RSA" type studies where tantalum spheres have been implanted & biplanar radiography has been used to monitor movement seen when patients moved from supine to prone, prone to standing, standing on 1 leg, & standing with maximal lumbar lordosis Other studies using rigidly fixed external fixators have been performed with subjects doing similar movements
10 Orthopaedi UI
Sholahuddin Rhatomy,MD
They concluded that there is between 1 & 2 of movement; this is total magnitude of movement!! Movements are consistent with pelvis being distorted & SI joint acting as a stress reliever for pelvic ring
SPINAL CORD ANATOMY
Motor Cell bodies are in anterior horn cells & innervate skeletal muscle Sensory Cell bodies lie within dorsal root ganglia Fibres arise in pain, thermal, tactile & stretch receptors Proprioception, fine touch & vibration from extremities & trunk Fibres pass cephalad in dorsal columns & do not synapse until reaching cervicomedullary junction Pathway for pressure & crude touch from extremities & trunk Fibres enter, synapse & cross & ascend into contralateral ventral spinothalamic tract Pain & temperature Fibres synapse in spinal cord, & cross to ascend in lateral spinothalamic tract Some area of neuronal overlap explained by branches that ascend or descend via dorsolateral column/fasciculus of Lissauer Sympathetic Sympathetic component of all 31 spinal nerves leaves spinal cord along only 14 motor roots (from T1 to L2) Between T1 & L2 there are white rami containing sympathetic fibres to ganglions of sympathetic chain Synapses occur somewhere along sympathetic chain & then postganglionic fibres reenter mixed spinal nerves through grey rami
Vascular Structures Blood supply to spinal cord
1 anterior median spinal artery & 2 posterior spinal arteries Anterior spinal artery supplies 85% of blood supply to cord throughout its length Radicular or segmental arteries
11 Orthopaedi UI
Sholahuddin Rhatomy,MD
Enter spinal canal through intervertebral foramina Divide into anterior & posterior radicular arteries to feed anterior & posterior spinal arteries, respectively ~8 radicular feeders to anterior spinal artery & ~12 to posterior spinal artery throughout length of cord Cervical spine Majority of radicular arteries arise from vertebral artery Basilar artery also anastomoses with anterior spinal artery Thoracic spine Radicular arteries branch off intercostal arteries at level of costotransverse joint Radicular artery of Adamkiewitz Largest segmental artery Major blood supply to lower cord Originates from left side in 80% Usually accompanies ventral root of thoracic nerves 9, 10 or 11 but may originate anywhere from T5 to L5 Watershed region Limited numbers of segmental arteries supply thoracic cord Branches of anterior spinal artery -> ventral 2/3 of cord Branches of posterior spinal artery -> dorsal 1/3 of cord Region where these 2 zones meet relatively poorly vascularised Critical vascular zone Zone between 4th & 9th thoracic vertebrae has least profuse blood supply Also narrowest region of spinal canal Segmental arteries should be divided as far anteriorly as possible during surgery
Lumbar Spine
Blood supply to bodies Each vertebra by a lumbar segmental artery Segmental arteries for L1-4 arise from aorta L5 from iliolumbar artery Towards intervertebral foramina, divides into 1. Anterior branch -> anterior abdominal wall 2. Posterior branch -> paraspinous muscles & facets 3. Foraminal branch -> spinal canal & its contents Venous supply parallels arterial supply Batson's venous plexus A system of valveless veins within spinal canal & around vertebral body Communication with pelvic plexus Alternative route for venous drainage to IVC Any increase in abdominal pressure -> blood flow preferentially to spinal canal Also preferential pathway for metastasis & infection to lumbar spine
12 Orthopaedi UI
Sholahuddin Rhatomy,MD
Spinal Injury
Introduction Bimodal age distribution 15-24 yrs Secondary peak incidence in people age 55 yrs or older Of those patients surviving cervical spine injury, up to 40% have neurologic deficit 10-38% of adults with thoracolumbar spine injuries have neurologic injury to spinal cord or cauda equina Patients with a spinal injury at 1 level may have another noncontiguous traumatic spinal injury 520% of time Upper C-spine injuries (esp. # of occipital condyle, atlas, odontoid process, & axis body) -> high incidence of additional C-spine injuries
Anatomy Spinal cord Fills ~35% of canal at level of atlas & ~50% of canal in lower cervical spine (C2C7) & in thoracolumbar segments Variable diameter with enlargement of cervical & lumbar regions to supply nerve roots of brachial & lumbosacral plexi Measures ~11 mm at lumbar region Myelomere, or segment of cord from which a nerve root arises Lies 1 level above same-numbered vertebral body until 10th thoracic vertebral segment Lumbar myelomeres are concentrated between T11 & L1 vertebral bodies Conus medullaris, containing sacral & coccygeal myelomeres, is dorsal to L1 body & L2 disk Spatial relationships of gray & white matter structures remain consistent throughout length of cord, but proportions change based on level Pathways Upper motor neurons Originate in cerebral cortex, cross to opposite side in midbrain, then descend in lateral corticospinal tract to synapse with their respective lower motor neurons in anterior horn of gray matter Corticospinal tracts demonstrate polarity, with cervical fibers distributed centrally & sacral fibers peripherally Ascending sensory input Originates in an axon from a cell body located in dorsal root ganglion within vertebral foramen Sensory afferents enter posterior horn of gray matter & travel cephalad in different areas of spinal cord, depending on type of sensation Pain & temperature sensation immediately cross to opposite side of cord & ascend in lateral spinothalamic tract Pressure & crude touch crosses immediately & ascends in a diffuse manner, but primarily in ventral spinothalamic tract Proprioception, light touch & vibratory sensation ascend in fibers of posterior column & cross in brain stem; fasciculus gracilis (lower extremities) is medial to fasciculus cuneatus (upper extremities)
13 Orthopaedi UI
Sholahuddin Rhatomy,MD
Cauda equina (motor & sensory roots of lumbosacral myelomeres) Below level of conus medullaris (L1-L2 disk), spinal canal is filled with cauda equina They exit caudally through respective foramina Middle thoracic spine -> vascular watershed, vascular insult can cause cord ischaemia (Artery of Adamkiewitz) Neurological injury Neurological deficits secondary to skeletal injury from T1-T10 frequently complete, primarily related to cord injury with varying levels of root injury Proportion of root injury increases with more caudal injuries Lesions below L1 have better prognosis Nerve roots, not cord affected Cauda equina less likely to be injured: more room in canal & not tethered to same degree as spinal cord Motor nerve root is composed of lower motor neuron axons, which are more resilient to trauma than brain & spinal cord
Mechanisms of injury Hyperextension Common in neck Anterior ligaments & disc may be damaged Flexion If posterior ligaments intact, wedging of vertebral body occurs If posterior ligaments torn, may cause subluxation Axial compression Causes burst # Bony fragments may be pushed into spinal canal Flexion, with posterior distraction May disrupt middle & posterior columns Flexion with rotation Causes dislocation with or without # Shear
Complications of spinal injury Neurological damage Damage to vertebral column -> deformity & pain Injury may be stable or unstable Stable injuries Vertebral components will not be displaced by normal movement An undamaged spinal cord not in danger No development of incapacitating deformity or pain Unstable injuries Criteria Clinical Progressive neurological deficit Radiological Loss of 50% of vertebral height (25% in C-spine) Failure of at least 2 of Deniss 3 columns
14 Orthopaedi UI
Sholahuddin Rhatomy,MD
Adjacent vertebral # o Angulation of thoracolumbar junction of >20 Burst # Further displacement of injury may occur Compression # of 3 sequential vertebrae can lead to posttraumatic kyphosis 10% of spinal # unstable & <5% a/w cord damage
SPINAL SHOCK Spinal cord nervous tissue dysfunction based on physiologic rather than structural disruption Absence of all distal motor & sensory function as well as loss of sacral spinal reflexes Has resolved when reflex arcs below level of injury begin to function again (eg. bulbocavernosus reflex) Generally lasts several hrs to days Signs Diaphragmatic breathing Warm periphery Decreased BP + decreased pulse rate = neurogenic Decreased body temperature Flaccid limbs Reduced reflexes Decreased pain sensation Erection Urinary retention Return of bulbocavernosus reflex at 24 hrs = end of spinal shock
Neurologic injury May involve spinal cord, nerve roots, or both Neurologic injuries following spine # can be divided into Primary injuries Occur at time of injury 4 basic mechanisms 1. Contusion 2. Compression 3. Stretch 4. Laceration Secondary injuries Occur later Result of ischemia & swelling that accompany all spinal injuries Ischemia secondary to both vascular injury at time of accident & release of vasoactive substances -> local vasoconstriction Inflammatory response accompanies all neurologic injuries & produces edema -> compression of neurologic structures & compromise of spinal microvasculature Cord injury Complete deficit No function (motor or sensory) caudad to cord injury after return of bulbocavernosus reflex +ve bulbocavernosus reflex -> S3-S4 region of conus medullaris both physiologically & anatomically functional
15 Orthopaedi UI
Sholahuddin Rhatomy,MD
99% of patients have return of bulbocavernosus reflex within 24 hrs Return signals end of spinal shock If no neurologic function below level of spinal column injury, lesion is a complete one Can expect up to 1 or 2 levels of additional root return, but prognosis for recovery bleak Bulbocavernosus reflex has no bearing on lesions caudad to conus Incomplete deficit Some neurologic function persists below level of injury after return of bulbocavernosus reflex Sacral sparing Represents at least partial structural continuity of white matter long tracts Evidenced by perianal sensation, voluntary rectal motor function, & great toe flexor activity May be only sign in emergency department that lesion is incomplete Incomplete neurologic deficit has a good prognosis for at least some functional motor recovery Functional motor recovery is seen in only 3% of complete injuries in 1st 24 hrs & virtually never after 24-48 hrs As a general rule, the greater the function distal to lesion & the faster the recovery, the better the prognosis A well-established method of recording functional degree of neurologic deficit: Frankel classification aka ASIA impairment scale Function Complete paralysis Sensory function only below injury level Incomplete motor function below injury level (1 or 2/5) Fair to good motor function (3-4/5) below injury level Normal function below injury level Incomplete deficits tend to fall into 1 of 4 patterns: central cord, anterior cord, posterior cord, or Brown Squard syndromes
Frankel grade A B C D E
Syndrome Anterior cord
Injury/pathology Flexion compression
Features Motor, pain & temp loss Dorsal columns spared
Prognosis Poor 10-15% functional recovery
16 Orthopaedi UI
Sholahuddin Rhatomy,MD
Central cord
Most common Extension injuries to OA spine (>50 yrs) Pincer effect between anterior osteophytes & posterior infolding of ligamentum flavum
Affects upper limbs (flaccid) more than lower limbs (spastic) Motor & sensory loss
Fair Majority functional recovery
Posterior cord Brown Sequard Penetrating trauma
Loss of deep pressure, deep pain & proprioception Loss of ipsilateral motor function, vibration & position sense, contralateral loss of pain & temp Best 90% bladder & bowel control & ability to walk
Conus medullaris syndrome Seen in T12-L1 injuries Loss of voluntary bowel & bladder control (S2-4 parasympathetic control) with preserved lumbar root function May be complete or incomplete; bulbocavernosus reflex may be permanently lost Uncommon as a pure lesion; more common with associated lumbar root lesion (mixed conus-cauda lesion) Nerve root lesions Isolated root lesions may occur at any level May accompany spinal cord injury May be partial or complete May result in radicular pain, sensory dysfunction, weakness, hyporeflexia, or areflexia Cauda Equina Syndrome Caused by multilevel lumbosacral root compression within lumbar spinal canal Clinical manifestations: saddle anesthesia, bilateral radicular pain, numbness, weakness, hyporeflexia or areflexia, & loss of voluntary bowel/bladder function
INITIAL MANAGEMENT OF SPINAL INJURY
ABC, spinal board, hard collar History Strongly suspect spinal injury if any major accident, unconscious patient, fall from a height, sudden jerk of neck after rear end car collision, facial injuries or head injury Ask about neck or back pain, numbness, tingling, weakness, ability to pass urine
Examination Logroll - look for bruising, palpate for step, tenderness Repeated neurological examination to determine neurological damage (complete/incomplete) & its progression/resolution Thorough overall examination for # etc as patient may not feel pain
17 Orthopaedi UI
Sholahuddin Rhatomy,MD
Imaging X-rays C-spine AP, lateral including C7/T1, open mouth view of odontoid, Swimmer's view or pull arms down AP & lateral view of other tender areas of spine CT scan Shows bony injury Better visualization of vertebral arches, facet joints, & neural canal Differentiation of neural elements from other soft tissues requires intrathecal administration of contrast medium MR scan Shows soft tissue involvement Extramedullary compression by disc, hematoma, & bone also readily apparent
If neurological damage Catheterise Note reduced BP & bradycardia due to neurogenic shock (temporary generalised sympathectomy) Rule out hypotension due to haemorrhage elsewhere May need Rx with vasopressors, not fluid resuscitation Invasive monitoring required Give methylprednisolone IV to reduce inflammation & preserve blood flow to spinal cord 30 mg/kg over 15 min Then 5.4mg/kg/hr for Next 23 hrs if within 3 hrs of injury Next 48 hrs if between 3 & 8 hrs of injury Attend to skin by turning
Pharmacologic Treatment of Spinal Cord Injury Medications with potential benefit to spinal cord injury Glucocorticoids or corticosteroids Opiate antagonists (eg. thyrotropin releasing hormone) Opiate receptor antagonists (eg. naloxone) GM-1 gangliosides Other agents Animal studies with all of these have shown significantly greater recovery from neurologic injury than in controls Methylprednisolone Relative contraindications to high-dose steroid Rx Pregnancy Age <13 yrs Concomitant infection Penetrating spinal wounds Uncontrolled diabetes Naloxone & corticosteroids after 8 hrs of injury ineffective GM-1 gangliosides
18 Orthopaedi UI
Sholahuddin Rhatomy,MD
Membrane glycolipids When administered within 72 hrs of injury, result in significant increase in motor scores Administer 100 mg/day for up to 32 days postinjury Not recommended for simultaneous use with methylprednisolone Gastrointestinal hemorrhage Higher incidence a/w patients with head & spinal cord injury than with those with other types of trauma Incidence higher in cervical cord injuries & complete deficits A causative relationship between short-term use of corticosteroids & gastrointestinal hemorrhage suggested but controversial Because of risk of gastric bleeding from stress ulcerations in cases of acute, severe trauma & concomitantly administered high-dose corticosteroids, Rx with acid suppressors eg. proton pump inhibitors recommended
NASCIS II (1990) SCI conceptualized as occuring in stages Following initial mechanical injury, a secondary injury cascade -> additional cell death NASCIS II (1990) Patients treated with methylprednisolone within 8 hrs of injury had significantly better neurologic recovery cf placebo Patients treated after 8 hrs from time of injury had worse outcome cf placebo, attributed to Cx a/w high-dose steroids Current recommendations A bolus of 30 mg/kg administered over 15 min, with a maintenance infusion of 5.4 mg/kg per hr If initiated within 3 hrs of injury -> infusion for 23 hrs If initiated between 3-8 hrs of injury -> infusion for 48 hrs
DEFINITIVE MANAGEMENT Objectives 1. Preserve neurological function 2. Relieve reversible nerve or cord compression 3. Stabilise spine 4. Rehabilitate patient 2 questions 1. ? neurological deficit 2. ? stable/unstable injury Mx
19 Orthopaedi UI
Sholahuddin Rhatomy,MD
Neurological deficit No
Stable Yes
Mx Pain relief Collar or brace Exception can be a burst #, ? operatively stabilise Reduce Hold secure until bone/ligaments heal with ORIF, tong traction, or halo vest Early operative stabilisation to help with nursing, prevent spinal deformity & pain, & speed up rehab Only consider conservative Mx for high thoracic injuries Pain relief Best rest Collar or brace Exception can be a burst #, ? operatively stabilise Early reduction & stabilisation
No Complete Usually no
Incomplete
Yes
No
NEUROLOGICAL ASSESSMENT IN SPINAL INJURIES Aims To determine level of lesion - counted as lowest level at which neurological function is intact bilaterally To determine whether damage is complete or incomplete To determine prognosis May be difficult until period of spinal shock (flaccidity, areflexia) is over (24-48 hrs after injury)
1. Tone 2. Power Diaphragm Shrugging shoulders Flex elbows Extend elbows Abduct fingers Active chest expansion Hip flexion Knee extension Ankle dorsiflexion Ankle plantar flexion Eversion of foot Inversion of foot C3-4-5 C4 C5,6 C7 C8 T1-T12 L2 L3-4 L5-S1 S1-S2 L5 L4
0 1 2 3
MRC Power Grading No active contraction Visible contraction without movement Movement with gravity eliminated Movement against gravity
20 Orthopaedi UI
Sholahuddin Rhatomy,MD
4 5
Movement against resistance but weak Normal power
3. Reflexes Biceps Triceps Supinator Knee jerk Ankle jerk Plantar response Abd cutaneous reflexes Bulbocavernosus reflex C5-6 C6-7 C5-6 L3-4 L5-S1 If upgoing = UMN lesion If lost = UMN lesion Pull penis -> anal sphincter tightening If returned, period of spinal shock over
4. Sensation
5. PR Always perform this to assess S2, 3, 4
ASIA Standard Neurological Classification of SCI Assess Motor Key muscles C5, C6, C7, C8, T1 L2, L3, L4, L5, S1 Score: 0, 1, 2, 3, 4, 5 & NT (not testable) Voluntary anal contraction Sensory
21 Orthopaedi UI
Sholahuddin Rhatomy,MD
Determine Neurological level = most caudal segment with normal function Sensory Motor Complete or incomplete (any sensory or motor function in S4-S5) ASIA impairment scale Zone of partial preservation = caudal extent of partially innervated segment Sensory Motor
Pin prick & light touch Score 0 = absent 1 = impaired 2 = normal NT Any anal sensation
LONG TERM CARE OF NEUROLOGICALLY INJURED SPINAL PATIENTS Frankel grade - useful in monitoring functional improvement from spinal cord injury Frankel grade A B C D E Function Complete paralysis Sensory function only below injury level Incomplete motor function below injury level (1 or 2/5) Fair to good motor function (3-4/5) below injury level Normal function below injury level
Highest mortality in 1st 2/52 Most common causes of morbidity & mortality 1. Respiratory insufficiency Atelectasis & pneumonia Any deficit proximal to T10 causes increased reliance on diaphragm Treat with physio, IPPV, tracheostomy & suction, repeated bronchoscopy 2. Paralytic ileus Keep NBM initially for 24 hrs IV fluids 3. GI bleeds from haemorrhagic gastritis ? due to unopposed parasympathetic activity Give H2 antagonists 4. Urological Cx UTI - main cause of mortality UMNL of bladder - catheterise intermittently to stop urinary stasis & infection LMNL - may manage with suprapubic pressure to relieve bladder Bladder training Stroking/squeeing Assess residual urine at 9/12 -> <100 ml -> continue training 5. Pressure sores
22 Orthopaedi UI
Sholahuddin Rhatomy,MD
6.
7.
Turn every 2 hrs Teach to relieve pressure later Joint contractures Spasticity Begins 6/52 after cervical & 12/52 after thoracic injury Flexion or extension depends on stimuli Spasticity -> muscle fibrosis -> joint contracture Passive movements +/- splintage 2x per day Remove stimuli Drugs Diazepam Baclofen Nerve block using alcohol or phenol Neurectomy Rhizotomy Psychological withdrawal Multidisciplinary approach Peer support
Rehab o Aims Minimise Cx Maximise remaining functions Achieve higher degree of independence Return to work o T2-T12 will have totally independent ADL & wheelchair mobilisation o T12 & below have possibility of walking with calipers with good hip hiker & quadratus lumborum o L3 & below will be able to walk with short leg brace & crutches o Includes 1. Selfcare 2. ADL 3. Transfer 4. Mobility 5. Education 6. Occupation
23 Orthopaedi UI
Sholahuddin Rhatomy,MD
Summary
24 Orthopaedi UI
Sholahuddin Rhatomy,MD
Cervical Spine Injuries
X-RAYS When to X-ray? 1. High energy multiple injuries 2. Head injury with neck pain 3. Hyperflexion/extension injury with neck tenderness (over midline) 4. ?? drunk or uncooperative patients Which X-rays? 1. Lateral 2. AP 3. Open mouth (odontoid peg) view 4. +/- Oblique views 5. +/- Flexion-extension views to diagnose instability, reserved for symptomatic patient after 7-10/7 when spasm has subsided 6. +/- CT scan if unclear or doubtful lesions 7. +/- MR scan Sensitivity of o Lateral C-spine X-ray alone 70-85% o 3 series (AP, lateral & open mouth views) 80-95% o If CT added 95-100% If a C-spine # is found o 50% have # at an adjacent level o 15% have # in another part of C-spine o 10% have # in thoracic or lumbar spine Reading C-spine X-rays AABCS o Adequacy Lateral - should show from occiput to T1 (swimmers' view or pull arms down) AP - should be symmetrical Open mouth - should show odontoid peg o Alignment On lateral view 4 lordotic curves 1. Anterior vertebral bodies 2. Anterior spinal canal 3. Posterior spinal canal 4. Spinous process tips
25 Orthopaedi UI
Sholahuddin Rhatomy,MD
Step of >3 mm indicates subluxation Step <25% vertebral width -> unilateral facet joint dislocation Step >25-50% vertebral width -> bilateral facet joint dislocation Unduly wide interspinous space -> anterior luxation Assess spinal canal; if <12 mm consider spinal stenosis Atlanto dens interval (ADI) - distance between posterior aspect of anterior arch of C1 to dens of C2 should be <3 mm (<5 mm in children)
On odontoid peg view There should be an equal gap between odontoid peg & articular masses of atlas Lateral edge of articular mass should align with lateral edge of shoulder of C2 body If both gaps widened = disruption of C1 ring On AP view, spinous processes should be in line On oblique view There should be symmetrical shingling of lamina If not = sublux or # of lamina
Bones
Odontoid process, look for lucency Trace round each bone Vertebral body: anterior height 3 mm < posterior height = compression # Tip of spinous process Facet joints Superior & inferior facets should be parallel If not = facet joint dislocation or # Cartilage Intervertebral disc space should be equal anteriorly & posteriorly, no more than o 11 anglulation Soft tissues Prevertebral soft tissue shadow Increase indicates bleeding or swelling >6 mm at C2 > width of vertebra at below level of larynx or 22 mm at C6 If normal, does not exclude injury Difficult to interpret in crying infant, NG tube/intubation, penetrating injury Interspinous space should not be increased
CT Indications 1. Unconscious patient with suspicious or inadequate cervical radiographs
26 Orthopaedi UI
Sholahuddin Rhatomy,MD
2. All cervical # or suspected # on initial plane films 3. Delineating injuries to atlantoaxial complex, esp rotatory subluxation & C-1 ring # 4. To examine Jefferson #, rotatory dislocation, burst #, cervicothoracic level injuries
Discussion o Plain films may not reveal posterior arch #, # & subluxations of articular facets, # of C1 & C2, & interspinal bony fragments o Plain films may not pick up coronally oriented vertebral body # resulting in large separate anterior tear drop fragment o To evaluate mid sagittal # through posterior vertebral wall o Best method for determining encroachment into bony canal Technique o Request thin sections (1.5-3 mm thickness) o Begins 1 level above # & continue 1 level below # Disadvantages o Much less sensitive for detecting # in transverse plane eg. articular process # o Oblique views more sensitive than reformatted, overlapping, transverse CT cuts for detecting certain articular process injuries, & certainly more readily available Tomography o For visualization of lateral masses using either linear or nonlinear motion patterns o Helpful in defining extent of facet # or subluxation o Particularly helpful in determining anatomic level of dens #
MRI For visualizing soft tissue & neural elements, & unsuspected disc herniations in presence of Cspine # Useful for delineating SCIWORA syndrome For visualizing widening of interspinous, interlaminar, or facet distances, prevertebral soft tissue prominence In patients with neurologic deficit - differentiate a compressive, extradural lesion from an intramedullary lesion, eg. cord contusion Differentiates cord edema from hemorrhage or vascular infarction
MANAGEMENT OF CERVICAL SPINE INJURIES Initial Mx See acute Mx of spinal injuries Definitive Mx 1. Preserve neurological function, by immobilising & giving steroids 2. Relieve reversible nerve or cord compression by reduction of #/dislocation 3. Stabilise spine 4. Rehabilitate patient Reduction o Can Improve comfort Relieve nerve tension Decompress neural structures o Traction Gardner Wells tongs Pin placement: below temporal ridge, ~2 cm above external auditory canal & temporal muscle
27 Orthopaedi UI
Sholahuddin Rhatomy,MD
2 kg increments with X-ray assessment & neurological examination after each increment Halo rings - can later be converted into halo vest config to hold neck as definitive Rx Halter traction for C1/2 subluxations Ideally MRI compatible Amount of traction needed for reduction of cervical # or dislocation can be estimated as 10 pounds to distract head & 5 pounds for each interspace Thus C4-C5 #-dislocation would probably require 30 lbs of traction Initially start out with less than this & work upwards after serial radiographs o Open at surgery Fixation till healing 0. External fixation - hard SOMI collar (Sternum Occipital Mandibular Immobilisation), if stable # 1. Halo vest, if unstable Safe, effective Can be used from acute situation to end of Rx Not preferred Rx if neurological deficit 2. Continued traction in supine position, rarely used these days, but can be used if delay in going to theatre, or patient refuses surgery 3. Internal fixation - anterior or posterior fusion (see below) Surgery o Urgent surgery recommended when 1. Progressive neurological deficit with persistent dislocation or neurocompression not corrected by closed traction 2. Persistence of incomplete spinal cord injury with continued impingement on neural elements o Less urgent surgery recommended when Unstable dislocations which have been reduced (ligamentous injuries less likely to heal -> fusion indicated) Complete spinal injury with unstable #, to enable early rehab Rehab & prevention of other Cx o See long term Mx of spinal cord injuries
SPECIFIC CERVICAL SPINE INJURIES INJURIES TO C1-2
28 Orthopaedi UI
Sholahuddin Rhatomy,MD
Functional anatomy Atlanto-occipital joint Synovial Ligaments Alar ligaments restrict rotation of occiput on dens Tectorial membrane Anterior & posterior atlanto-occipital membrane 0-C1 joint capsues Apical ligament Allows nodding movement (1/2 of all cervical flexion-extension) Atlantoaxial joint 3 synovial joints: paired lateral mass articulation, articulation between dens & anterior C1 arch & transverse ligament Ligaments Transverse ligament - primary stabilizer Crucifrom ligament Anterior & posterior atlanto-axial ligaments Alar ligament Apical ligament Allows mainly rotation (1/2 of all cervical rotation), but some flexion, extension & lateral bending
Atlanto-Occipital disarticulation Rarely seen in surviving patients Severe associated head trauma Deficits at cranial nerves VII, VIII, IX, & X as well as brainstem dysfunction may be observed
29 Orthopaedi UI
Sholahuddin Rhatomy,MD
Burst # of C1 (Jeffersons)
# ring of atlas behind & in front of lateral masses Mechanism - axial compression (diving) Rarely causes neurological symptoms Relatively larger space available for cord at C1 level # tend to displace centrifugally Instability a/w C1 # depends on integrity of transverse atlantal ligament 50% a/w other C-spine # especially odontoid # & spondylolisthesis of axis Clinically Patient c/o unstable neck Rarely neurological symptoms Cranial nerve lesions of VI-XII Symptoms of basilar artery insufficiency or vertebral artery injuries X-rays True Jeffersons is 4 part Widening of spaces on either side of odontoid on peg view Rx Central issue: transverse ligament If intact -> SOMI collar If disrupted (sideways spreading of lateral masses) -> 6/52 skull traction then 6/52 firm collar or halo vest Only fuse C1 to C2 if fails to heal after 2/12 or instability, as stiffness will ensue
Transverse ligament rupture Rare, usually fatal Mechanism - forced flexion Can occur in isolation or in combination with atlantoaxial subluxation or atlas # Types of TAL injuries I - bony avulsion II - purely ligamentous Clinically, severe neck pain to complete neurologic compromise Rupture of transverse ligament may be determined by 1. ADI >3 mm in adults; ADI >5 mm in adults also implies rupture of alar ligaments 2. Atlantoaxial offset (lateral displacement of C1 lateral masses) >7 mm on odontoid radiograph 3. Flexion-extension X-rays 4. Visualizing avulsed lateral mass fragment on CT 5. Direct visualization of rupture on MRI Rx
30 Orthopaedi UI
Sholahuddin Rhatomy,MD
o o
If bony avulsion, halo vest till bone healing If midsubstance, C1-C2 fusion Gallie - places wires under posterior arch of C1 & around spinous process of C2 Brooks - places wires under lamina of C1 & C2 In presence of C1 ring # -> transarticular or lateral masses screws
Atlantoaxial rotatory subluxation Mechanism Unknown May occur spontaneously or after trauma Fielding classification (based on degree of anterior translation of atlas on axis) Injury Transverse lig intact, ADI <3 mm Insufficient transverse lig, ADI >3-5 mm Alar lig failure, ADI >5 mm Complete displacement Rx Halter traction for 48 hrs then collar once reduced C1 C2 fusion C1 C2 fusion C1 C2 fusion
Type 1 2 3 4
Clinically, patient's head tilted to 1 side X-ray: unequal gap on open mouth odontoid peg view
Odontoid Peg Fractures Vascular supply arrives through apex of odontoid & through base with watershed area in neck of odontoid Mechanism - forced extension & rotation Cord damage up to 25% High association with other C-spine # Anderson & DLanzo Classification Type 1 2 Injury Through tip of process (avulsion Stable of alar ligament) Hard collar At junction of peg with body (base of dens) Most common Separation in body of axis Nonunion rate 36% (lack of periosteum & cancellous bone) even if in Halo vest Give patient choice: Halo vest or posterior fusion of C1-C2 or anterior screw fixation (80-95% union rate) Halo vest 12/52 -> 80% union rate Rx
31 Orthopaedi UI
Sholahuddin Rhatomy,MD
Hangmans Fractures Traumatic spondylolisthesis of C2/C3 # pars interarticularis of C2 Mechanism - hyperextension & axial loading Bilateral C2 pars # inherently decompress spinal cord -> not usually a/w neurologic deficit May be a/w cranial nerve, vertebral artery, craniofacial injuries 30% incidence of concomitant C-spine # Levine & Edwards Classification Type I II Minimally displaced >3 mm translation Features Rx Stable, treat in hard collar Unstable, treat in traction then halo vest, heal by fusion of C2 on C3, KIV fusion Treat with halo vest with compression, KIV fusion Treat with open reduction & posterior fusion C2-C3 & halo vest for immobilisation
II-A Less translation but more angulation, traction can worsen deformity III Severe angulation & translation, with unilateral or bilateral facet disarticulation of C2 on C3
32 Orthopaedi UI
Sholahuddin Rhatomy,MD
INJURIES TO C3-7
Vertebral bodies: superior cortical surface concave laterally & convex anteroposteriorly, allowing for flexion, extension, & lateral tilt by gliding motion of facets Facet joints Superior articular process is anterior & inferior to inferior articular process o o 45 in sagittal & 0 in coronal plane Uncinate process projects superiorly from lateral aspect of vertebral body; with degenerative changes, these may articulate with superior vertebra -> uncovertebral joint (of Luschka) Ligaments ALL - resists hyperextension & gives stability to anterior aspect of disc space PLL - resists hyperflexion & reinforces discs from herniation Ligamentum flavum Interspinous & supraspinous ligaments Radiology If C-spine instability suspected, flexion-extension views may be obtained in a willing, conscious, & cooperative patient without neurologic compromise A "stretch" test (Panjabi & White) with longitudinal cervical traction -> abnormal test: >1.7 o mm interspace separation or >7.5 change between vertebrae CT with reconstructions to characterize # pattern & degree of canal compromise MRI to further delineate spinal cord, disc, & canal abnormalities
Cervical strain (whiplash) Soft tissue injury when neck suddenly jerked into hyperextension Usually due to rear-end collision Anterior longitudinal ligament strained or torn & disc damaged Pain & stiffness but no physical signs Analgesics & physioRx
Wedge compression # C3-C7 Mechanism of injury - flexion Body compressed but posterior ligaments intact -> # stable Rx If <25% -> rigid collar If >25%
33 Orthopaedi UI
Sholahuddin Rhatomy,MD
Halo vest or posterior fusion as posterior elements likely to be involved Anterior & posterior fusion may be necessary
Teardrop # dislocations C3-C7 Mechanism of injury - severe axial compression or axial compression combined with flexion 1 or more fragments forced into spinal canal Rx - highly unstable, so fusion required
Unilateral facet joint dislocations Mechanism Flexion distraction + rotation Injury involves forward rotation of 1 side of vertebra about contra-lateral facet joint Interfacetal joint on side of direction of rotation is pivot Superior facet on contralateral side rides upward, forward, & over tip of inferior facet of involved joint, coming to rest in intervertebral foramen anterior to inferior facet of joint Central portion of vertebral body subluxates ~25% of AP body diameter Associated injuries Inferior facet of dislocated joint frequently fractured Capsule of non dislocated joint frequently disrupted Can also occur with concomitant # of either facet or entire lateral mass Partial tearing of posterior longitudinal ligament on affected side(s) Clinical Torticollis Axial rotation to contralat side & lateral bend to injured side X-ray - 25% anterior subluxation Rx Without disc widening or subluxation, unilateral facet dislocation is stable injury Reduction + halo vest/fusion
Bilateral facet joint dislocations Mechanism Severe flexion distraction + rotation Integrity of all ligaments of cervical canal lost, including posterior ligaments, anterior & posterior longitudinal ligaments, disc, & articular facet joints Articular facets ride forward over facets below & become locked -> 50% anterior subluxation at involved level Usually 1 or both articular masses # Spine is unstable Often cord damage Associated injuries Disc herniation May occur in 10% who have facet subluxation or dislocation Catastrophic compression of spinal cord can result from an uncontrolled facet reduction Epidural hematoma May result in neurologic comprimise once reduction achieved
34 Orthopaedi UI
Sholahuddin Rhatomy,MD
Ix Rx
Look for blood collection posterior to cord
X-ray - 50% anterior subluxation MRI for associated injuries
Displacement must be reduced by heavy skull traction or manipulation or open reduction Once reduced, options Traction 6/52 & collar 6/52 Halo vest 12/52 Posterior fusion Potential problems include redislocation, inadequate healing, & scapular or other decubiti in patients with insensate skin
Clay Shovellers # Avulsion of spinous process of C3-C7 Treat symptomatically
Principles of upper cervical arthrodesis Remind patient that there will be loss of function whether fused or not Goals 1. Protection of neural structures 2. Pain free stable spine Positioning o Careful planning o If prone, position whilst patient awake Electrophysiological monitoring can be used Bony structures need decortication Autogenous cancellous bone Stable fixation o Posterior fusion MR compatible cable systems (titanium) Cables allow exact tension control & better tightening mechanisms than surgical wire o Anterior fusion with plates
HALO APPLICATION Most effective orthosis for controlling motion at C1-C2 articulation Contra-indications Unstable skull # Traumatized skin overlying pin sites Positioning of patient
35 Orthopaedi UI
Sholahuddin Rhatomy,MD
Position patient (still on spine board & with semirigid collar in place) at end of bed so that head overhangs bed Head stabilized manually with axial distraction A back panel is slid under patient's back between scapulae in direct line with his neck Occipital support, is then attached to back panel & tightly secured Semirigid collar left in place throughout Size of halo Once head supported, appropriate sized halo ring selected Placed in approximate position desired, & secured to occipital support by means of halo suction cups Selection of holes Optimum positioning of halo critical to ensure stability, durability & patient comfort 4 holes placed in scalp, 2 anteriorly & 2 posteriorly Anterior pin sites Centered in groove at upper margin of eyebrows, between supraciliary ridge & frontal prominences Sagittally, just superior to outer half of eyebrows, to avoid supraorbital, supratrochlear nerves & vessels, & frontal sinus Should be placed as close to midline of eyebrow as possible, as thickest mass of bone is central Dangers Placed too inferiorly, pins might encroach on orbit Placed too medially, however, pins might encroach on frontal sinus Some surgeons place pins lateral to eyebrows under hairline, to avoid scarring but may cause 3 problems Since pins penetrates temporalis muscle, chewing may be uncomfortable Temporal bone thin in this area & pentration or loosening may occur Since posterior pins are placed opposite anterior pins, this lateral position causes posterior pins to be very close to anterior pins, & multiplane stability decreased Posterior pin sites Placed about 1/4 inch above ears This ensures that it will be below maximum diameter of skull & will not migrate superiorly Pin insertion Not necessary to incise skin, & posteriorly not necessary to shave hair Have patient close eyes during pin insertion Each pin should be placed until they just touch skin 1 front pin & diagonally opposite back pin tightened to maximum finger tension Other pins likewise tightened Torque screwdriver then used to tighten pins, again tightening them in pairs 1st Consider 6-8 in-lbs of tightness (10 in-lbs will begin to pass through outer table) Unequal tension should not be used as halo will migrate in direction of pin of least tension Pin care Pins should be tightened carefully once a day for 3 days, then checked for tightness every 3 days 3 more times Pins should not routinely be tightened more than a full turn at any visit This may indicate loose pin which has migrated into skull's inner table If such a pin has a torque far less than optimum, it should be removed & a new one placed; in this case, diagonal opposite must be changed Cx Palsy of 6th cranial nerve (abducens)
36 Orthopaedi UI
Sholahuddin Rhatomy,MD
Loosening - if pin does not appear to be infected, it can be retightened by carefully apply a few turns up to desired 8 in-lbs
Bibliography ATLS handbook Current Orthopaedics Vol 9 No. 4 211-282 Miller Rockwood and Green Wheeless
Thoracolumbar Spine Trauma
Anatomy & biomechanics Thoracolumbar spine consists of 12 thoracic & 5 lumbar vertebrae Thoracic level is kyphotic, whereas lumbar region is lordotic At thoracolumbar junction there is a fulcrum of increased motion -> increased risk of injury Kinematics Upper thoracic spine (T1-T10) protected by ribs, sternum & facet joint orientation Thoracic spine much stiffer than lumbar in flexion-extension & lateral bending due to thoracic cage & thinner intervertebral discs (average 20% of vertebral body height vs 40% in lumbar spine), which restrict arc of motion Rotation about craniocaudal axis is greater in thoracic spine, maximum at T8-9 In lumbar spine, rotation is limited by orientation of facets & anterior portion of annulus to only 10 for entire lumbar spine vs ~75 in thoraci c spine Denis 3-column model
Neurology Spinal cord Fills ~35% of canal at level of atlas & ~50% of canal in lower cervical spine (C2C7) & in thoracolumbar segments Variable diameter with enlargement of cervical & lumbar regions to supply nerve roots of brachial & lumbosacral plexi Measures ~11 mm at lumbar region Myelomere, or segment of cord from which a nerve root arises Lies 1 level above same-numbered vertebral body until 10th thoracic vertebral segment Lumbar myelomeres are concentrated between T11 & L1 vertebral bodies Conus medullaris, containing sacral & coccygeal myelomeres, is dorsal to L1 body & L2 disk
37 Orthopaedi UI
Sholahuddin Rhatomy,MD
Spatial relationships of gray & white matter structures remain consistent throughout length of cord, but proportions change based on level Pathways Upper motor neurons Originate in cerebral cortex, cross to opposite side in midbrain, then descend in lateral corticospinal tract to synapse with their respective lower motor neurons in anterior horn of gray matter Corticospinal tracts demonstrate polarity, with cervical fibers distributed centrally & sacral fibers peripherally Ascending sensory input Originates in an axon from a cell body located in dorsal root ganglion within vertebral foramen Sensory afferents enter posterior horn of gray matter & travel cephalad in different areas of spinal cord, depending on type of sensation Pain & temperature sensation immediately cross to opposite side of cord & ascend in lateral spinothalamic tract Touch also crosses immediately & ascends in a diffuse manner, but primarily in ventral spinothalamic tract Proprioception & vibratory sensation ascend in fibers of posterior column & cross in brain stem; fasciculus gracilis (lower extremities) is medial to fasciculus cuneatus (upper extremities) Cauda equina (motor & sensory roots of lumbosacral myelomeres) Below level of conus medullaris (L1-L2 disk), spinal canal is filled with cauda equina They exit caudally through respective foramina Middle thoracic spine -> vascular watershed, vascular insult can cause cord ischaemia (Artery of Adamkiewitz) Neurological injury Neurological deficits secondary to skeletal injury from T1-T10 frequently complete, primarily related to cord injury with varying levels of root injury Proportion of root injury increases with more caudal injuries Lesions below L1 have better prognosis Nerve roots, not cord affected Cauda equina less likely to be injured: more room in canal & not tethered to same degree as spinal cord Motor nerve root is composed of lower motor neuron axons, which are more resilient to trauma than brain & spinal cord
Complications of spinal injury Neurological damage Damage to vertebral column -> deformity & pain Injury may be stable or unstable Stable injuries Vertebral components will not be displaced by normal movement An undamaged spinal cord not in danger No development of incapacitating deformity or pain Unstable injuries Criteria Clinical
38 Orthopaedi UI
Sholahuddin Rhatomy,MD
Progressive neurological deficit Radiological Loss of 50% of vertebral height (25% in C-spine) Failure of at least 2 of Deniss 3 columns Adjacent vertebral # o Angulation of thoracolumbar junction of >20 Burst # Further displacement of injury may occur Compression # of 3 sequential vertebrae can lead to posttraumatic kyphosis 10% of spinal # unstable & <5% a/w cord damage
SPINAL SHOCK Spinal cord nervous tissue dysfunction based on physiologic rather than structural disruption Absence of all distal motor & sensory function as well as loss of sacral spinal reflexes Has resolved when reflex arcs below level of injury begin to function again (eg. bulbocavernosus reflex) Generally lasts several hrs to days Signs Diaphragmatic breathing Decreased BP + decreased pulse rate = neurogenic Decreased body temperature Warm periphery Flaccid limbs Reduced reflexes Decreased pain sensation Erection Urinary retention 99% of patients have return of bulbocavernosus reflex at 24 hrs = end of spinal shock
Neurologic injury May involve spinal cord, nerve roots, or both Neurologic injuries following spine # can be divided into Primary injuries Occur at time of injury 4 basic mechanisms 1. Contusion 2. Compression 3. Stretch 4. Laceration Secondary injuries Occur later Result of ischemia & swelling that accompany all spinal injuries Ischemia secondary to both vascular injury at time of accident & release of vasoactive substances -> local vasoconstriction Inflammatory response accompanies all neurologic injuries & produces edema -> compression of neurologic structures & compromise of spinal microvasculature Cord injury Complete deficit
39 Orthopaedi UI
Sholahuddin Rhatomy,MD
No function (motor or sensory) caudad to cord injury after return of bulbocavernosus reflex +ve bulbocavernosus reflex -> S3-S4 region of conus medullaris both physiologically & anatomically functional Return signals end of spinal shock If no neurologic function below level of spinal column injury, lesion is a complete one Can expect up to 1 or 2 levels of additional root return, but prognosis for recovery bleak Bulbocavernosus reflex has no bearing on lesions caudad to conus Incomplete deficit Some neurologic function persists below level of injury after return of bulbocavernosus reflex Sacral sparing Represents at least partial structural continuity of white matter long tracts Evidenced by perianal sensation, voluntary rectal motor function, & great toe flexor activity May be only sign in emergency department that lesion is incomplete Incomplete neurologic deficit has a good prognosis for at least some functional motor recovery Functional motor recovery is seen in only 3% of complete injuries in 1st 24 hrs & virtually never after 24-48 hrs As a general rule, the greater the function distal to lesion & the faster the recovery, the better the prognosis A well-established method of recording functional degree of neurologic deficit: Frankel classification Function Complete paralysis Sensory function only below injury level Incomplete motor function below injury level (1 or 2/5) Fair to good motor function (3-4/5) below injury level Normal function below injury level
Frankel grade A B C D E
Incomplete deficits tend to fall into 1 of 4 patterns: central cord, anterior cord, posterior cord, or Brown Squard syndromes
40 Orthopaedi UI
Sholahuddin Rhatomy,MD
Syndrome Anterior cord
Injury/pathology Flexion compression
Features Motor, pain & temp loss Dorsal columns spared
Prognosis Poor 10-15% functional recovery Fair Majority functional recovery
Central cord
Most common Extension injuries to OA spine (>50 yrs) Pincer effect between anterior osteophytes & posterior infolding of ligamentum flavum
Affects upper limbs (flaccid) more than lower limbs (spastic) Motor & sensory loss
Posterior cord Brown Sequard Penetrating trauma
Loss of deep pressure, deep pain & proprioception Loss of ipsilateral motor function, vibration & position sense, contralateral loss of pain & temp Best 90% bladder & bowel control & ability to walk
Conus medullaris syndrome Seen in T12-L1 injuries Loss of voluntary bowel & bladder control (S2-4 parasympathetic control) with preserved lumbar root function May be complete or incomplete; bulbocavernosus reflex may be permanently lost Uncommon as a pure lesion; more common with associated lumbar root lesion (mixed conus-cauda lesion) Nerve root lesions Isolated root lesions may occur at any level May accompany spinal cord injury May be partial or complete May result in radicular pain, sensory dysfunction, weakness, hyporeflexia, or areflexia Cauda Equina Syndrome Caused by multilevel lumbosacral root compression within lumbar spinal canal Clinical manifestations: bilateral radicular pain, numbness, weakness, hyporeflexia or areflexia, saddle anesthesia, & loss of voluntary bowel/bladder function
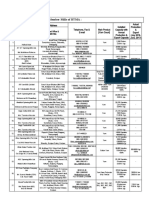
Classification of acute thoracolumbar spinal injuries
Consideration of spinal stability forms basis of thoracolumbar injury classification & Mx Studies suggest that spine consists of 3 columns, each contributing variably to overall stability depending on spinal segment level
Denis 3-column model Based on analysis of both plain X-rays & CT Anterior Anterior 1/2 of vertebral body Anterior longitudinal ligament
41 Orthopaedi UI
Sholahuddin Rhatomy,MD
Middle Posterior 1/2 of vertebral body Posterior longitudinal ligament Posterior Posterior neural arches (pedicles, facets & laminae) Posterior ligamentous complex
Useful in understanding mechanism of injury & assessing stability Instability exists with disruption of any 2 of columns Thoracolumbar stability usually follows middle column; if it is intact, then injury is usually stable Columns can fail individually or in combination by 4 basic mechanisms of injury: compression, distraction, rotation, & shear Resulting thoracolumbar spine injuries are of 4 major types - Furgeson & Allen mechanistic classification 1. Compression 2. Burst 3. Flexion-distraction (seat belt type) 4. #-dislocation Each of these injuries may be divided into subgroups
42 Orthopaedi UI
Sholahuddin Rhatomy,MD
Compression # o Result from anterior or lateral flexion causing failure of anterior column o Middle column remains intact & may act as center of rotation o Radiographically Anterior height of vertebral body diminished Posterior height normal o Normally stable & rarely a/w neurologic compromise o 4 types according to Denis classification Type A - involvement of both end plates Type B - involvement of superior end plate Type C - involvement of inferior end plate Type D - buckling of anterior cortex with both end plates intact Burst # o Involve compressive failure of vertebral body both anteriorly & posteriorly, with failure of both anterior & middle columns o Typical mechanism: fall from a height, landing on one's feet o Axial loading on intervertebral discs -> increased nuclear pressure & hoop stresses in annulus -> high shear stress on vertebral end-plate at inner border of annulus, away from center of disc -> typical large central & posterior fragments of burst # o Typically, posterior column remains intact -> stable burst # o However, as with compression injuries, anterior angulation may damage posterior o ligamentous complex -> kyphotic deformity >20 -> unstable burst # o X-rays Lateral: decreased vertebral body height, retropulsion of bony fragments into canal AP: increased interpedicular distance 25% misdiagnosed as compression # -> CT important o 5 subtypes of burst #, depending on whether 1 or both end-plates are fractured & on amount of rotation or lateral flexion
43 Orthopaedi UI
Sholahuddin Rhatomy,MD
McAfee Researchers -> burst # can be unstable with early progression of neurologic deficits & spinal deformity, & late onset of neurologic deficits & mechanical back pain Factors indicative of instability in burst # >50% canal compromise o >15-25 of kyphosis >40% loss of anterior body height
Flexion-Distraction Injuries (Seat Belt Types) o Occur secondary to distractive disruption of posterior, middle, & anterior columns, usually with anterior column acting as center of rotation o Typical mechanism: head-on motor vehicle collision while wearing a lap seat belt o Failure of all 3 columns may involve primarily bone (Chance #) or ligaments & may extend to >1 spinal level o Radiographically Increased interspinous process distance on AP view Increased posterior height of vertebral body on lateral film o Chance # seldom a/w neurologic compromise unless significant amount of translation occurs o 45% a/w intra-abdominal (bowel) injuries
Fracture-dislocation o Involve disruption of all 3 columns by a combination of compression, tension, rotation, or shear o Both bony & ligamentous disruptions usually present o Neurologic deficit in >70% of cases
44 Orthopaedi UI
Sholahuddin Rhatomy,MD
Denis' subtypes Flexion-rotation type Anterior column fails by compression & rotation while middle & posterior columns fail primarily by rotation Failure may occur through disc or vertebral body Flexion-distraction type Distinguished from Chance-type injury by presence of significant translation Highly unstable, often a/w neurologic deficit, dural tears, & intraabdominal injury Extreme shear type All 3 bony columns fail by shear forces 2 types of shear #: posteroanterior shear & anteroposterior shear
Load Sharing Classification - Gaines Factor Comminution/Involvement (on Little = <30% sagittal CT) More = 30-60% Gross = >60% Apposition of fragments (on axial CT) Minimal displacement Spread = at least 2 mm displacement of <50% of cross section of body Wide = at least 2 mm displacement of >50% of cross section of body Deformity correction (kyphotic Little = <3 correction) o More = 4-9 Most = >10
o o
Amount
Point 1 2 3 1 2 3 1 2 3
Total point 7 or more -> pedicle screw breakage Cannot be used to make decisions on surgical indication because it does not grade ligament injury Recommendations Short segment posterior approach in patients with flexion-distraction injuries or mild burst # with point totals of 6 or less Short segment posterior approach, 2nd stage anterior vertebrectomy & strut fusion in patients with higher-point injuries
INITIAL MANAGEMENT OF SPINAL INJURY ABC, spinal board & hard collar History Strongly suspect spinal injury if any major accident, unconscious patient, fall from a height, sudden jerk of neck after rear end car collision, facial injuries or head injury
45 Orthopaedi UI
Sholahuddin Rhatomy,MD
Ask about neck or back pain, numbness, tingling, weakness, ability to pass urine
Examination Logroll - look for bruising, palpate for step, tenderness Repeated neurological exam to determine neurological damage & its progression/resolution Thorough overall exam for # etc as patient may not feel pain
Imaging X-rays C-spine AP, lateral including C7/T1, open mouth view of odontoid, Swimmer's view or pull arms down AP & lateral view of other tender areas of spine CT scan Shows bony injury Better visualization of vertebral arches, facet joints, & neural canal Differentiation of neural elements from other soft tissues requires intrathecal administration of contrast medium MR scan Shows soft tissue involvement Extramedullary compression by disc, hematoma, & bone also readily apparent
If neurological damage Catheterise Note reduced BP & bradycardia due to neurogenic shock (temporary generalised sympathectomy) Rule out hypotension due to haemorrhage elsewhere Volume replacement, then vasopressors if hypotension without tachycardia persists despite volume expansion Fatal pulmonary edema can result from overinfusion of hypotensive spinal cord injury patient Degrees of hypotension & bradycardia & incidence of cardiac arrest directly related to Frankel grade Invasive monitoring required Give methylprednisolone IV 30 mg/kg over 15 min Then 5.4mg/kg/hr for Next 23 hrs if within 3 hrs of injury Next 48 hrs if between 3 & 8 hrs of injury /Neurological Stable deficit No Yes Mx Pain relief Collar or brace Exception can be a burst #, ? operatively stabilise
46 Orthopaedi UI
Sholahuddin Rhatomy,MD
No Complete
Reduce Hold secure until bone/ligaments heal with ORIF, tong traction, or halo vest
Usually Early operative stabilisation to help with nursing, prevent spinal deformity & pain, & no speed up rehab Only consider conservative Mx for high thoracic injuries Yes Pain relief Best rest Collar or brace Exception can be a burst #, ? operatively stabilize Early reduction & stabilization
Incomplete
No
Attend to skin by turning
DEFINITIVE MANAGEMENT Objectives 1. Preserve neurological function 2. Relieve reversible nerve or cord compression 3. Stabilise spine 4. Rehabilitate patient 2 questions 1. ? neurological deficit 2. ? stable/unstable injury Mx
Surgical Rx Offers significant advantages in selected cases 1. Restores sagittal plane alignment, corrects translation, & decompresses neural structures Soreff reviewed results of nonoperative Rx of 147 thoracolumbar spine # >8 yrs after injury Significant complaints of progressive spinal deformity & that spinal deformity correlated with patient's symptoms & impairment High incidence of flexion-type deformities: compression (40%), gibbus (23%), disc collapse (23%), scoliosis (23%) & spondylosis (46%) 2. Resulted in increased amount of neurologic improvement (53% vs 44%) 3. Tends to decrease rehab time compared with recumbent Rx Higher rate of Cx
Specific injuries Compression # Middle column intact -> no retropulsion -> neurologic dysfunction unlikely Nonsurgical Most patients can be treated symptomatically with short period of bed rest until pain is diminished Immobilization in hyperextension orthosis Early ambulation encouranged
47 Orthopaedi UI
Sholahuddin Rhatomy,MD
Avoidance of compression overloads for a period of 12/52 Close radiographic follow-up Combined anterior & posterior column failure -> compression # with 50% or more collapse in anterior vertebral height or evidence of posterior ligamentous disruption -> acute or delayed kyphotic deformity -> hyperextension orthosis (TLSO) or body cast Surgical Progressive loss of sagittal plane alignment >50% collapse Neurologic deterioration
Burst # Thoracic burst # stability directly related to competency of posterior ligamentous structures Criteria for stable burst # Neurologically intact Posterior arch remains intact: pedicle widening implies posterior arch disruption with instability <25-35 of kyphosis <50% anterior body height collapse Canal compromise <50% Stable burst # without posterior column disruption -> equivalent radiographic & clinical outcomes following surgical & nonsurgical Rx Unstable burst # Often require surgical reduction & stabilization A localized kyphotic deformity of 20-30 or more - > poor outcome with nonsurgical Mx Nonsurgical Most stable burst # & most lumbar burst # can be treated non operatively With non operative Rx, significant remodeling & reabsorption (~50%) of retropulsed fragments can be expected Relative contra-indications Unstable burst # Morbid obesity Presence of associated conditions which would preclude brace wear Short period of bed rest until pain is diminished Immobilization TLSO or hyperextension body cast with or without cervical extension for at least 3/12, depending on # stability Leg extension must be added for # below L3 Typically patients allowed out of bed 3-14/7 after injury, unless other concomitant injuries eg. pelvic # Close radiographic follow-up - with long term follow up, radiographs need to be taken standing to evaluate for kyphosis Surgical Goals 1. Decompression indicated if neurological deficit 2. Realignment 3. Stabilization Incomplete neurologic dysfunction in presence of thecal sac compression often requires surgical decompression in addition to spinal stabilization Indirect decompression Distraction through posterior spinal instrumentation Posterolateral decompression
48 Orthopaedi UI
Sholahuddin Rhatomy,MD
Most indicated for unstable burst # with cord impingement along with dural tear & nerve root entrapment from # of posterior elements Fragments impinging on neural elements pushed away anteriorly Anterior decompression & fusion Most indicated for unstable burst # with cord impingement caused by bone fragments off postero-superior vertebral body Entire vertebral body may be removed Bone graft used to reconstruct anterior spinal column Anterior, posterior, or circumferential fusion chosen depending on level of injury & degree of neurologic & osteoligamentous instability Posterior approach used most often Anterior approach & instrumentation Indications T11-L3 # with incomplete neurological deficit & spinal canal compromise Significant kyphotic deformity Limitations Difficult above T11 & below L3 due to local anatomy Laminar # not accessible Care with significant posterior ligament disruption & osteoporotic bone Significant translational deformity & noncompliance -> contraindications Flexion-distraction (seat belt type) Nonsurgical Injured bony spinal elements have more predictable healing potential than do discal or ligamentous disruption Bony Chance # may be treated nonsurgically with closed reduction in extension o & external immobilization if kyphosis <15 Surgical Adults, however, have not enjoyed same healing success as bony Chance # in children -> recommendation of posterior surgical stabilization in all flexiondistraction injuries In all other flexion-distraction injury variants, posterior reduction & fusion with compressive segmental fixation 1 level above & 1 level below injury often undertaken Care must be taken to avoid significant posterior compression in patients with comminuted posterior vertebral body to prevent iatrogenic bony fragment retropulsion into spinal canal #-dislocation Early surgical reduction & stabilization allows for prompt patient mobilization regardless of neurologic status, thereby decreasing overall morbidity & mortality Decompression of spinal cord often achieved by realignment of spine through posterior approach Subsequent anterior decompression & reconstruction may be necessary if residual thecal sac compression & incomplete neurologic deficit
49 Orthopaedi UI
Sholahuddin Rhatomy,MD
Site for Pedicle Screw Insertion
A horizontal line that bisects transverse process A vertical line that connects lateral edge of facet
LONG TERM CARE OF NEUROLOGICALLY INJURED SPINAL PATIENTS Frankel grade - useful in monitoring functional improvement from spinal cord injury Frankel grade A B C D E Function Complete paralysis Sensory function only below injury level Incomplete motor function below injury level (1 or 2/5) Fair to good motor function (3-4/5) below injury level Normal function below injury level
Highest mortality in 1st 2/52 Most common causes of morbidity & mortality 1. Respiratory insufficiency Atelectasis & pneumonia Any deficit proximal to T10 causes increased reliance on diaphragm Treat with physio, IPPV, tracheostomy & suction, repeated bronchoscopy 2. Paralytic ileus Keep NBM initially for 24 hrs IV fluids 3. GI bleeds from haemorrhagic gastritis ? due to unopposed parasympathetic activity Give H2 antagonists 4. Urological Cx UMNL of bladder - catheterise intermittently to stop urinary stasis & infection LMNL - may manage with suprapubic pressure to relieve bladder Bladder training Stroking/squeeing Assess residual urine at 9/12 -> <100 ml -> continue training 5. Pressure sores Turn every 2 hrs Teach to relieve pressure later 6. Joint contractures Spasticity Begins 6/52 after cervical & 12/52 after thoracic injury Flexion or extension depends on stimuli Spasticity -> muscle fibrosis -> joint contracture Passive movements
50 Orthopaedi UI
Sholahuddin Rhatomy,MD
7.
+/- splintage 2x per day Remove stimuli Drugs Diazepam Baclofen Nerve block using alcohol or phenol Neurectomy Rhizotomy Psychological withdrawal Multidisciplinary approach Peer support
Rehab o Aims Minimise Cx Maximise remaining functions Achieve higher degree of independence Return to work o T2-T12 will have totally independent ADL & wheelchair mobilisation o T12 & below have possibility of walking with calipers with good hip hiker & quadratus lumborum o L3 & below will be able to walk with short leg brace & crutches o Includes 1. Selfcare 2. ADL 3. Transfer 4. Mobility 5. Education 6. Occupation
Sacral Fractures
Imaging Plain radiographs AP & outlet views Difficult to discern on plain radiographs; 70% may be missed Sacral arcuate lines Will help delineate anatomy of # of upper sacrum Composed of inferior surfaces of costal elements that form roofs of anterior sacral canals (foramina) & neural grooves Arcuate lines easily visible on AP view of pelvis & are symmetrical Asymmetry or discontinuity of sacral arcuate lines may be caused by uncomplicated sacral # Disorganized or marked disruption of sacral arcuate lines indicative of comminuted sacral # CT scan better delineates these injuries
51 Orthopaedi UI
Sholahuddin Rhatomy,MD
Classification Pattern of sacral # Vertical Oblique Transverse Avulsion Vertical Most common Denis classification
Sacral # may occur Lateral to neural foramina (zone 1) Through foramina (zone 2) Medial to foramina (zone 3) Zone 3 # involve central sacral canal, & >50% of these injuries occur with neurologic impairment (cauda equina) Zone 2 injuries a/w neurologic deficits in >25% of cases, usually from nerve root injury Zone 1 sacral ala # may result in sciatic nerve or L5 nerve root injury in ~6% of cases
Transverse Less common High-energy injuries Neurologic deficit, dural tear, & rectal perforation commonly associated
Management Assess for potential instability Stable # includes impacted vertical # of sacrum, nondisplaced # of posterior sacroiliac complex, or subtle # of upper sacrum as seen by asymmetry of sacral arcuate lines Unstable #, is characterized by # diastasis of >0.5-1 cm, along with unstable anterior injury Healing potential If type I # reduces with traction, then unstable # would be expected to become sticky in ~4/52 & complete healing expected in 3/12 Usually managed with closed or surgical reduction & stabilization with a variety of fixation strategies eg. sacroiliac screws, transiliac bars, or plate & screw fixation Closed reduction & percutaneous screw fixation for displaced longitudinal sacral # an option Neurologic deficit should lower threshold to perform decompression (laminectomy) & exploration of involved nerve roots at time of surgical stabilization
52 Orthopaedi UI
Sholahuddin Rhatomy,MD
Cervical Disc Disease
Categorization by Odom et al Aetiology Unilateral soft disc protrusion Osteophytes/hard disc Medial soft disc protrusion Cervical spondylosis
Pathology Nerve root compression/radiculopathy Nerve root compression/radiculopathy Spinal cord compression/myelopathy Spinal cord compression/myelopathy
CERVICAL SPONDYLOSIS A non-specific term Refers to any lesion of cervical spine of a degenerative nature
Pathology Results from an imbalance between formation & degradation of proteoglycans & collagen in disc With aging, a -ve imbalance with subsequent loss of disc material -> degenerative changes Factors influencing severity of degeneration Heredity Trauma Metabolic Certain occupational exposures Other environmental effects, eg. smoking Degeneration -> Disc herniation Stenosis Instability Spine unable to withstand physiologic loads -> significant risk for neurologic injury, progressive deformity & long-term pain & disability Not common in cervical spondylosis except those with stiffness in middle & lower segments who develop compensatory hypermobility at C3-4 or C4-5 -> myelopathy
Clinical Patients may present with neck pain (axial pain), cervical radiculopathy, or myelopathy Most patients have little or no pain Segmental ROM decreased
X-rays
53 Orthopaedi UI
Sholahuddin Rhatomy,MD
X-rays changes Narrowing of intervertebral disc Sclerosis of endplates Osteophyte formation Similar changes may occur in facet joints Most frequently in C5-6 & C6-7 Incidence of spondylosis on X-rays in asymptomatic patients 80% in 51-60 age group 95% in 61-70 age group Incidence of spondylosis on MRI in asymptomatic patients <40 yr Cervical disc herniation Degenerative disc changes Cervical stenosis 10% 25% 4% >40 yr 5% 60% 20%
Cervical spinal instability Radiographic criteria of White o >11 angulation >3.5 mm translation of adjacent subaxial segments
CERVICAL RADICULOPATHY
A condition caused by compression of a nerve root in cervical spine Involves a specific spinal level with sparing of levels immediately above & below
Incidence Annual incidence 83.2 per 100 000 population (Radhakishran, Minnesota, 1994) Age Not common in under 30s Most common in 40s & 50s Cervical degeneration tends to begin 10 yrs later than lumbar degeneration F:M = 3:2
Pathology Causes Lateral disc herniation ~50% (soft disc) Osteophyte formation in Lushka - intervertebral body - joint or facet joint ~50% (hard disc) Only 5% also have developmental spinal stenosis (AP diameter of spinal canal of 12 mm or less) Compression occurs mostly at entrance or just medial to foramen where nerve roots pass ventrally to superomedial edge of superior articular process
54 Orthopaedi UI
Sholahuddin Rhatomy,MD
Occasionally a herniated disc will migrate into intervertebral foramen Frequency of nerve root compressed: C7 > C6 > C8 > C5 Nerve root of inferior vertebra of a given motion segment is the one usually affected by a herniated disc, eg. C6 for C5-C6 disc
Clinical Symptoms Unilateral neck pain, nape pain & pain at suprascapular, scapular or interscapular, usually precedes other symptoms Radiating arm pain Finger parasthesia Weakness Signs Motor weakness Diminished deep tendon reflexes Sensory disturbance C5 Suprascapular None/lateral upper arm None C6 Suprascapular Lateral arm Thumb C7 Scapular/interscapular Posterior arm Index/long C8 Scapular/interscapular Medial arm Little
Neck pain Arm pain Sensory change in fingers Motor weakness Diminished tendon reflexes
Deltoid (biceps) Biceps
Biceps (deltoid) Biceps
Triceps Triceps
Intrinsics (triceps) Triceps
Spurling's neck compression test Downward pressure applied to head with neck extended & rotated towards painful side -> narrowing of neuroforamen +ve if radicular symptoms reproduced or worsened Usually +ve but may be -ve in chronic cases Shoulder abduction test Decreases tension in nerve root -> relief of radicular symptoms Adson's test Distinguishes thoracic outlet syndrome from radiculopathy Arm abducted, extended & externally rotated at shoulder while examiner feels radial pulse Patient turns head towards affected side & takes a deep breath +ve if radial pulse diminishes or lost -> compression of subclavian artery Tinel's sign In radiculopathy, direct palpation or percussion over exiting nerve root may provoke patient's familiar limb or axial pain If tenderness or Tinel's sign elicited more laterally, eg. supraclavicular fossa, then diagnosis should be questioned Scoring system Developed by Tanaka et al Japan
55 Orthopaedi UI
Sholahuddin Rhatomy,MD
Normal score = 20 Has 4 categories: subjective symptoms, ability to work, finger function, objective signs
Differential diagnosis Neck pain preceding other symptoms helps distinguish this from Thoracic outlet syndrome Pancoast tumour Brachial plexus pathology Shoulder pathology Cubital tunnel syndrome Tennis elbow de Quervain's disease Spurling's sign pathognomonic If no neck pain, & Spurlings -ve, diagnosis can be made if symptoms & signs confined to a single nerve root
Investigations In contrast to spinal cord in myelopathy, compressed root can rarely be depicted even with MRI Detection of either spondylosis or laterally herniated disc at involved root level leads to diagnosis Plain X-rays Look for changes in alignment, osteophytes, disc space narrowing, endplate sclerosis, uncovertebral & facet joints Measure sagittal canal diameter Absolute (AP canal diameter <10 mm) or relative (10-13 mm) stenosis are risk factors for myelopathy, radiculopathy, or both Pavlov's ratio (canal/vertebral body width) Should be 1.0, with <0.85 indicating stenosis Ratio of <0.80 is a significant risk factor for lateral neurologic injury This identifies a congenitally narrow canal Only spurs at involved nerve root can be assumed to cause symptoms Spurs of superior articular process more likely to be compressive factor than spurs of Luschka joint Disc spaces at levels of herniation usually preserved Therefore a disc space of normal height at affected level suggests disc herniation as cause of compression CT Most useful for detecting bony spondylitic spurs Slice just cranial to disc space most informative MRI Most useful for herniated disc However disc protrusions are seen in 20% of asymptomatic patients 45-54 yrs old, 57% in those >64 CT myelogram with low-dose water-soluble contrast media Electrodiagnostic studies High false-negative rate Helpful in differentiating peripheral nerve compression from central compression or disease
56 Orthopaedi UI
Sholahuddin Rhatomy,MD
Treatment
Conservative More effective with acute cases Collar & NSAIDs If acute, try bed rest with or without halter traction Poor mans traction - with head (which weighs ~10 lbs) hanging over end of bed (prone in flexion/supine in extension) for several minutes several times a day Cervical epidural injection Direct cervical nerve root block Lees et al 50 out of 51 patients improved But at 2-19 yrs 29% mild residual symptoms 27% moderate symptoms Tanaka et al At 1-3 yrs 49% mild residual symptoms 37% moderate symptoms
Surgery Indications 1. Failure of conservative Rx 2. Increasing neurological deficit 3. Unbearable pain Western surgeons more likely to operate than Eastern surgeons, but selection criteria poorly defined
Surgical Procedures Approach should be determined by position & type of lesion Soft lateral discs easily removed by posterior approach Spurs & more paramedian discs via anterior approach Options Single level Anterior foramenotomy without discectomy Posterior foramenotomy with discectomy 2 levels Smith Robinson anterior discectomy & interbody fusion (graft + anterior cervical plate/cage) With more extensive anterior decompression - discectomy & corpectomy with strut graft fusion Posterior approach General anaesthetic Positioning Prone with face in a headrest Neck flexed Shoulders retracted inferiorly with tape Landmarks: spinous process of C2, C7 & T1 most prominent
57 Orthopaedi UI
Sholahuddin Rhatomy,MD
Incision - midline 2.5 cm lower than interspace to be explored Division of ligamentum nuchae Blunt dissection of paraspinal muscles Fenestration of ligamentum flavum Identify nerve root Excision of osteophytes to free nerve &/or retraction & protection of nerve root to remove disc tissue through cruciate incision in PLL Ensure nerve root is free through intervertebral foramen with a probe Results 90% good Very few Cx Anterior approach Allows exposure to anterior aspect of vertebral bodies from C3-T1 Recurrent laryngeal nerve most important structure at risk Left recurrent laryngeal nerve Ascends in neck between trachea & oesophagus, having branched off vagus nerve at level of arch of aorta Less at risk Right recurrent laryngeal nerve Runs alongside trachea after hooking around right subclavian artery Crosses from lateral to medial in lower part of neck & can be vulnerable Personal preference as to which side to use General anaesthetic Positioning Supine with extension of neck Head ring Turn patients head away from planned incision o Elevate head of table 30 to reduce bleeding Arm by side NG tube to enable identification of oesophagus Check level with X-rays Incision Make a oblique skin crease incision at level of pathology using landmarks described in table Landmarks Hard palate Lower border of mandible Hyoid bone Thyroid cartilage Cricoid cartilage/carotid tubercle Vertebral level Arch of atlas C2-3 C3 C5 C6
Extend it from midline to posterior border of sternocleidomastoid Superficial Incise fascia over platysma in line with skin incision Split platysma with fingers in line of fibres or cut in line of incision Identify anterior border of sternocleidomastoidand & incise fascia immediately anterior to it
58 Orthopaedi UI
Sholahuddin Rhatomy,MD
Deep
Using fingers retract sternocleidomastoid laterally, & sternohyoid & sternothyroid strap muscles with trachea & oesophagus medially Divide omohyoid (omohyoid lies over carotid sheath + transverse cervical artery landmarks to brachial plexus) Palpate carotid artery, develop a plane between medial edge of carotid sheath & midline structures (thyroid, trachea & oesophagus), cutting through pretracheal fascia
Superior & inferior thyroid arteries may limit exposure but can be divided - note reccurent laryngeal nerve between 2 forks of inferior thyroid artery (on the right mainly) Cevical vertebrae covered by longus colli muscle & prevertebral fascia - enter this 'valley' between longus colli muscles ALL is white & gleaming in midline, cut here, as sympathetic chain is on longus colli just lateral to vertebral bodies
59 Orthopaedi UI
Sholahuddin Rhatomy,MD
Structures at risk Main dangers: recurrent laryngeal nerve & sympathetic chain Thoracic duct on the left Excise anterior annulus fibrosis Remove as much disc material as can be seen Insert an interspace spreader Remove posterior annulus & extruded disc &/or any associated bone spurs Posterior longitudinal ligament can be removed for a better view of dura & nerve roots Interbody grafting then performed using Smith Robinson fusion Cloward fusion Bailey Badgely fusion Bloom Raney modification of Smith Robinson fusion Moss cage Moss cage & plate
60 Orthopaedi UI
Sholahuddin Rhatomy,MD
Cx Pseudoarthrosis rates 1 level - 0-5% 2 levels - 10-20% 3 levels - 30-60% Adjacent motion segment degeneration up to 50% Progression of underlying degenerative process Increased load & stress transfer Others Soft tissue injury - airway, esophagus, recurrent laryngeal nerve, Horner's syndrome, thoracic duct, dysphagia Neurologic injury Vertebral artery injury
Surgical results No difference in results reported for anterior or posterior approaches No significant differences between results of surgery for soft disc or for osteophytes
CERVICAL MYELOPATHY
Characterized by Weakness (upper > lower extremity) Sensory changes Ataxic broad based shuffling gait Rarely urinary retention
61 Orthopaedi UI
Sholahuddin Rhatomy,MD
Incidence May be under reported in western countries In Japan, Kokubun 5.7 per 100 000 people Half of patients in 50s or 60s M:F = 2:1
Anatomy of compression Anterior cord compression from protruding disc or posterior osteophytes Anterolateral compression from joints of Luschka Lateral compression from cervical facets Posterior compression from ligamentum flavum
Pathology 7 spinal factors can be causative of spinal cord compression 1. Developmental stenosis: AP diameter of spinal canal of 12 mm or less made with a tube to film distance of 1.8 m 2. Dynamic stenosis: defined as Pennings jaw diameter - distance from posterior inferior corner of vertebral body, to anterior margin of subjacent lamina, 12 mm or less, a/w 2 mm of retrolisthesis with neck in extension 3. Disc herniation: median & paramedian 4. Segmental OPLL (Ossification of posterior longitudinal ligament) 5. Continuous OPLL 6. Posterior spur 7. Calcification of ligamentum flavum (CLF): tends to occur in elderly women 1 & 2 most common
Most commonly affects C5-6 > C4-5 > C3-4 > C6-7 (cf cervical radiculopathy most common at C6-7) This is because cervical enlargement of spinal cord is at C4-5 & C5-6 levels Retrolisthesis on extension (dynamic instability) rarely seen at C7 because of its anterior tilt, so dynamic stenosis rarely affects C6-7 disc Grey matter more vulnerable to compression than white matter
62 Orthopaedi UI
Sholahuddin Rhatomy,MD
Classification of symptomatology - Crandall Central cord syndrome Transverse lesion syndrome Brown-Sequard syndrome Motor system syndrome without sensory disturbance Brachialgia & cord syndrome/radiculomyelopathy Localisation of symptomatic disc level Cervical discs compromise next numbered spinal cord segment This may vary within a range of 1 level Not as easy in myelopathy to diagnose level as it is in radiculopathy Upper limb pain predominates, with associated long tract involvement Symptoms & signs in upper extremities > lower Symptoms & signs in upper & lower extremities Ipsilateral motor & proprioception loss; contralateral pain & temperature loss
Clinical Symptoms In usual order of appearance 1. Funicular pain - characterized by central burning & stinging 2. Paraesthesia of fingers 3. Clumsiness of hands 4. Tightness, hot or cold sensations in trunk 5. Tingling in legs 6. Gait disturbance due to spasticity 7. Urinary disturbance 10-20% 1st notice leg symptoms 1/3 notice electric shock sensations on extending neck indicating an early stage to disease Signs Upper motor neuron findings Jaw jerk Controlled by 5th cranial nerve Performed by tapping on slightly opened jaw Normal reflex contraction of masseter (no or slight) effectively rules out pathology above foramen magnum Upper extremity - mixed upper & lower motor neuron findings Myelopathy can initially present with hand dysfunction with loss of fine motor function eg. writing Hyper-reflexia Hoffman's sign Elicited by flipping either volar or dorsal surfaces of middle finger & observing reflex contraction of thumb & index finger Specific to UMNL of cervical spine Inverted radial reflex (C5-C6) Demonstrated by tapping brachioradialis tendon
63 Orthopaedi UI
Sholahuddin Rhatomy,MD
Diminished reflex noted along with reflex contraction of spastic finger flexors This specific reflex occurs due to cord compression of C5-6 level (from disc or spur) which allows upper motor neuron reflex to occur May be present when cord & root compression are present at C5 level Biceps reflex Primarily indicates neurologic integrity of C5; also has C6 component Scapulohumeral reflex Elicited by tapping tip of spine of scapula in a caudal direction -> scapula elevation or humerus abduction Suggests UMNL above C4 level Finger escape sign Small finger spontaneously abducts due to weak intrinsics, indicating cervical myelopathy 20-seconds finger count Clumsiness or spider fingers Lower extremity - upper motor neuron signs Decline in ability to walk, apparent ataxia Hyper-reflexia Frank clonus Babinski's sign May not be present until myelopathy becomes severe Pathology anywhere along entire cord -> +ve sign Loss of lower extremity proprioception Lhermitte's sign Paraesthesias or leg weakness exacerbated by neck flexion 90% have +ve Hoffman's sign Clonus, upgoing plantars & easily elicited Hoffmann's sign are indicative of advanced disease
Differential diagnosis Multiple sclerosis (patchy demyelination throughout white matter of CNS) - unlike cervical myelopathy there is abnormal cranial nerves, & jaw jerk Amyotrophic lateral sclerosis - affects both upper & lower motor neurons, & no alterations in sensation SCIWORA syndrome Spinal cord tumor Infection Tumor Syringomyelia Subacute combined degeneration - in cervical myelopathy there is more sensory loss in upper extremities & more spastic lower extremities Cerebral hemisphere lesion - low pressure hydrocephalus
Investigations Plain X-ray for stenosis
64 Orthopaedi UI
Sholahuddin Rhatomy,MD
MRI
Normal = ~17 mm Absolute (AP canal diameter <10 mm) or relative (10-13 mm) stenosis are risk factors for myelopathy, radiculopathy, or both Pavlov's ratio (canal/vertebral body width) Should be 1.0, with <0.85 indicating stenosis Ratio of <0.80 is a significant risk factor for lateral neurologic injury This identifies a congenitally narrow canal OPLL
Shows cervical disc prolapse well Demonstrates spinal cord well High intensity signal can be found in spinal cord on T2, representing myelomalacia (necrosis/cavity formation) CT shows OPLL & bone spurs best
MRI showing myelopathy Treatment Conservative Natural history poorly understood but most get worse if not treated Slow stepwise worsening with periods of neurologic plateau preceeding another episode of deterioration In early phases, try NSAIDS, collar, muscle relaxants
Surgical Indications Absolute indication = neurological deficit which is progressing Patients with cord compression on MRI but no objective symptoms or findings of myelopathy best treated nonoperatively Herniation shows better improvement after surgery, older patients & those with dynamic stenosis show less improvement Surgical approaches No controlled prospective studies comparing anterior & posterior approaches Approach depends on 1. Location of pathology 2. Levels of involvement 3. Stability of spine
65 Orthopaedi UI
Sholahuddin Rhatomy,MD
4. Presence of kyphotic deformity Anterior decompression & fusion Indications Generally recommended if disc herniation or posterior spur causing compression at 1 or 2 levels Also indicated if there is kyphotic deformity, so that correction can be achieved See cervical radiculopathy for technique Options Anterior discectomy & interbody fusion with anterior spinal instrumentation With more extensive anterior decompression involving excision of osteophytes discectomy & corpectomy with strut graft fusion Posterior decompression +/- fusion Generally recommended if there is compression of spinal cord at 3 levels or more, in developmental stenosis or calcification of ligamentum flavum Options Laminoplasty Directly decompresses cord posteriorly & indirectly decompresses cord anteriorly Requirements Straight or lordotic cervical spine Stable spine Multilevel cord compression Long term improvement in 60-75% Morbidities C5 motor neuropraxia, often within 24-48 hrs postop Loss of ROM Chronic neck pain Recurrent stenosis Laminectomy - poor outcome due to spinal instability & kyphosis Laminectomy & posterior fusion with posterior instrumentation
Operative Results JOA score Criteria for evaluation of operative results of patients with cervical myelopathy Looks at Upper extremity function Lower extremity function Sensory function Bladder function Total score = 17 points Recovery rate = [Postop score - preop score]/[17 - preop score] x 100%
66 Orthopaedi UI
Sholahuddin Rhatomy,MD
Summary
References Current Orthopaedics, 1998 Campbell's Miller
Rheumatoid Spondylitis
INTRODUCTION 90% of rheumatoids have cervical spine involvement Indications for surgical stabilisation 1. Instability 2. Pain
67 Orthopaedi UI
Sholahuddin Rhatomy,MD
3. Neurological deficit due to nerve compression
ATLANTOAXIAL SUBLUXATION 50-80% of rheumatoid C-spine disorders, but frank dislocation occurs in ~25% 11% will develop cord compression from atlantoaxial subluxation Anterior instability much more common More often in men
Aetiology Pannus formation at synovial joints between dens & ring of C1 Destruction of transverse ligament & dens Anterior subluxation of C1 on C2
Risk factors Corticosteroid use Seropositivity RA nodules Erosive & deforming disease
Clinical Reduced ROM 'Clunk' with neck flexion (Sharp & Purser sign - not recommended!) Rheumatoid compression of spinal cord or nerve roots -> long tract signs (myelopathy) & root pain Root pain Caused by anterior subluxation of atlas on axis -> suboccipital (C2) root pain Can be severe Usually episodic Provoked by sudden movement
Radiology Including patient-controlled flexion & extension views Steele's Rule of Thirds Spinal cord, odontoid process, & free space for cord ~1 cm in diameter each Anterior displacement of atlas >1 cm may jeopardize adjacent segment of spinal cord Atlas-Dens Interval (ADI) >3 mm difference between flexion & extension views -> instability >6 mm difference -> disruption of alar ligaments (attach dens to skull) >9 mm difference -> neurological injury Space Available for Cord (SAC) <10 mm a/w higher risk of neurological damage
68 Orthopaedi UI
Sholahuddin Rhatomy,MD
Flexion & Extension views
MRI showing myelopathy Management Aims
To prevent development of irreversible neurological deficit To prevent sudden death from unrecognised spinal cord compression Avoid unnecessary surgery: 50% of patients with instability but no symptoms should not have surgery Conservative Soft or hard collars for pain relief, not for instability Most severe instability takes place in flexion, therefore main goal is to prevent flexion with an orthosis Surgery
69 Orthopaedi UI
Sholahuddin Rhatomy,MD
Indications 1. Progressive instability 2. Neurological impairment 3. ADI >6 mm or SAC <13 mm means spine should be stabilised prior to GA for other procedures Options Posterior C1-C2 fusion with wires & halo vest immobilisation - Brooks technique Transarticular screw across C1-C2 - Magerl technique Cx Pseudoarthrosis (20%) Recurring myelopathy ADI >6 mm & SAC <10 mm = relative contraindication to surgery in other areas, until spine has been stabilised 1st
Posterior Fusion Compare to Atlantoaxial Subluxation in Childhood
CRANIAL SETTLING (BASILAR INVAGINATION/Atlanto-axial Impaction)
= cranial migration of dens from erosion & bone loss between occiput & C1/C2 Ranawat's line <5 mm is diagnostic May affect up to 5-10% of patients who have C-spine disease
Aetiology Lateral masses of atlas may collapse secondary to erosive changes in atlantooccipital & atlantoaxial synovial joints This leads to vertical subluxation of odontoid process through foramen magnum Tip of odontoid process, which may be expanded by surrounding pannus, is brought into contact with cervicomedullary junction
Clinical Need to rule out myelopathy Headaches due to compression of greater occipital branch of C2
70 Orthopaedi UI
Sholahuddin Rhatomy,MD
Loss of pain/touch sensation over trigeminal nerve distribution Sleep apnea Down beat nystagmus & inter-nuclear ophthalmoplegia Facial diplegia Dysphagia (due to CN IX dysfunction)
X-rays McRae's line Defines opening of foramen magnum Tip of dens may protrude slightly above this line, but if dens is below this line then impaction is not present Chamberlain's line Hard palate to posterior rim of foramen magnum Dens >6 mm above this line consistent with impaction McGregor's line Hard palate to posterior occipital curve Diagnosis is based on tip of dens being >8 mm above this line in men & >10 mm above the line in women Ranawat's line Center of C2 pedicle to C1 arch Normal >17 mm <13 mm consistent with impaction
Treatment May require occiput-C2 fusion
LOWER CERVICAL SPINE Involved in 20% of cases More common in males, steroid use, severe RA Joints of Lushka & facet joints involved Subluxation can occur at multiple levels
71 Orthopaedi UI
Sholahuddin Rhatomy,MD
Subluxation >4 mm with intractable pain & neurological compromise indications for posterior fusion & wiring
Back Pain
Prevalence 60-80% of people will have LBP sometime in their lives 30% referred to Ortho; 3% admitted; 0.5% operated 90% LBP resolves in 6/52, 75% may experience symptoms & disability 1 yr after initial consultation Prevalence of LBP has changed little over years, but associated disability has increased 4x since 1970s In UK certified incapacity for LBP was 120 million days in 1996/7 Overall cost of LBP was 6 billion with 14 million consultations in 1993
Differential Diagnosis According to Age LOOK OUT FOR RED FLAGS Children 1. Congenital disorders 2. Developmental disorders 3. Infection 4. Primary tumours - eosinophilic granuloma, Ewing's sarcoma, metastatic neuroblastoma, spinal cord tumours Young adults 1. Disc disease 2. Spondylolisthesis 3. # 4. Scheuermann's disease 5. Ankylosing spondylitis Older adults 1. Spinal stenosis 2. Metastatic disease 3. Osteopaenic # 4. Infection
Types of Back Pain DRRIP Discogenic back pain
72 Orthopaedi UI
Sholahuddin Rhatomy,MD
Pain from innervated ligamentous layer of annulus fibrosus when it is stretched by a bulging disc Midline & worse with lordotic postures, bending & lifting Radicular back pain Pain extending to buttock &/or leg Associated with disc herniation or spinal stenosis or intraspinal pathology Referred back pain Aortic aneurysm Visceral (ulcer, PID, endometriosis, gallbladder disease, pleural disease) Infection UTI Hip arthritis Iatrogenic back pain Dural adhesions Post surgical instability Post operative discitis; arachnoiditis Psychogenic back pain Must exclude organic pathology Waddell's inappropriate signs often present
Waddell's Inappropriate/Nonorganic Signs (1984) Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine 1980;5:117-25
Superficial (light pinch) Non anatomic (tender to palpation over LS, pelvis, & TS) 2. Simulation Axial loading - vertical loading on a standing patient's skull -> LBP Rotation - passive rotation of shoulders & pelvis in same plane -> LBP 3. Distraction SLR - discrepancy between findings on sitting & supine straight leg raising tests 4. Regional disturbances Weakness - "cogwheel" (give-way) weakness, resisted hip flexion Sensory - non-dermatomal sensory loss 5. Overreaction (most important Waddell criteria) Disproportionate facial expressions, verbalisation or tremor during examination 3 or more signs present = be wary of operating; nonorganic features According to Waddell et al o Nonorganic signs by themselves should not be equated with malingering or presence of psychological problem o Rather, finding of nonorganic signs should alert clinician to need for more comprehensive testing
1. Tenderness
73 Orthopaedi UI
Sholahuddin Rhatomy,MD
Intervertebral Disc Disease
Pathophysiology of lumbar degenerative disease Degenerative process of spine occurs at level of functional spinal unit, or motion segment, which consists of 2 adjacent vertebral bodies Intervertebral disc & facet joints Ligamentous supports: ligamentum flavum, interspinous, supraspinous, & intertransverse ligaments, & facet joint capsule Kirkaldy-Willis classification describes 3 stages of degenerative process 1. Dysfunction of support tissues of motion segment (15-45 yrs), with facet joint synovitis, annular & ligament stretching & minor tearing, & minor reducible subluxations 2. Unstable stage (35-70 yrs): progressive annular & ligament tearing & laxity, decrease in proteoglycan & water content of nucleus pulposus which further alters kinematics of motion segment -> altered facet joint forces & hypermobility, with secondary degenerative bone formation & facet enlargement 3. Motion segment stabilization (>60 yrs), resulting from disc height loss & osteophyte formation along vertebral end plates -> disc space narrowing results in overriding of facet joints, & narrowing of lateral portion of spinal canal & foramen As degenerative process proceeds o Annulus fibrosus may undergo progressive radial tearing -> radial tears may accumulate & focal defect may -> true disc herniation o Segmental spinal instability may develop as a result of progressive incompetence of disc & facet joints to oppose shear, bending, torsional, & axial forces o Spondylolisthesis may occur, with secondary lateral recess & then central canal stenosis caused by intact posterior neural arch o Degenerative scoliosis May result in narrowing of foramina & lateral recesses within concavity of curve Fractional curve stenosis, with low lumbar extremity pain on side of convexity of main curve
Age related changes in intervertebral disc
74 Orthopaedi UI
Sholahuddin Rhatomy,MD
Intervertebral disc has blood supply up to age of 8 yrs Nutrition after this time is by imbibition & requires movement of spinal column Proteoglycan synthesis decreases with age, thus concentration will diminish from 65% in early adult life to 30% by 60 yrs Proteoglycans that persist are smaller in size & concentration of chondroitin sulphate falls (keratan sulphate concentrations remain constant) This causes a drop in water content from 88% at birth to 65% by age 75 However most of this dehydration occurs in childhood & early adolescence, with a decrease of only 6% from early adult life to old age Collagen content increases in both nucleus & annulus but concentration of elastin falls Loss of water & increase in collagen content -> discs stiffer & less resistant to deformation & also less able to recover from creep deformation As nucleus dries out & becomes more fibrous it is less able to transmit forces to annulus & annulus then has to play a greater role in load transmission therefore subjecting it to greater stresses Contrary to popular belief, disc height does not decrease with age but stays constant, with any loss of disc height representing a degenerative process as opposed to an age related change
Discogenic pain
Normal discs have sensory nerve endings in outer 1/3 of annulus -> potential source of back pain Disc stimulation studies (using either hypertonic saline or contrast media) -> normal discs do not cause pain Disc stimulation is specific for painful discs & in particular for radial annular tears Reproduction of pain does not correlate with whether or not disc is degenerated, only with degree of fissuring of disc
Causes Discogenic pain can result from Torsional injury (circumferential tear of annulus) Internal disc disruption (acute traumatic annular tear) Degenerative disc disease Infection (discitis)
Diagnosis Diagnosis of discogenic pain is one of exclusion, as presence of degenerated lumbar disc on Xrays or MRI very common, even in asymptomatic controls Internal disc disruption Cannot be diagnosed clinically but only after post-discography CT Correlation between reproduction of pain & grade 3 tear very strong Grade 0 No disruption evident
75 Orthopaedi UI
Sholahuddin Rhatomy,MD
Grade 1 Grade 2 Grade 3
Disruption to inner 1/3 Disruption to middle 1/3 Disruption to outer 1/3
Intervertebral provocative discography Single most important test in diagnosing painful internal disc disruption Walsh et al JBJS 72A: 1081-1088, 1990 -> in 10 asymptomatic volunteers with discography at 3 lumbar levels there were no cases of provocation of pain ie. specificity 100% 2 components Provocation of patient's typical pain with a pressurized contrast injection Back pain alone or back pain > leg pain Increased back pain with increased intradiscal pressure Morphologic abnormalities on post-discography radiographs or CT Must be seen for test to considered +ve Dye extending into epidural space or to periphery of disc Post-discography CT scanning increases ability to diagnose radial tears of annulus not seen on MRI Indicated when patient has back pain but MRI shows >1 'black' discs or equivocal findings Useful to identify painful levels when contemplating spinal fusion so that remaining black discs can be saved Colhoun etal JBJS 70B: 267-271, 1988 -> 89% of patients in whom discography had demonstrated disc disease & provoked symptoms had significant & sustained benefit from operation
Clinical Back pain Midline Usually mechanical, being accentuated with prolonged sitting & standing, bending & lifting Either alone or in excess of leg pain PE Lacks features identifying other pain syndromes No neurologic deficit
76 Orthopaedi UI
Sholahuddin Rhatomy,MD
Management Conservative Most patients with back pain believed to be disc-related are successfully treated with aggressive nonsurgical Mx Active rehab, medication, & other aspects of pain Mx Surgery As last resort for individuals who are highly motivated, carefully selected (preferably 1 level disease), & without significant psychosocial magnification of symptoms Usually involves spinal fusion Rationale - immobilisation of offending motion segment will alleviate pain Indications Chronic & disabling LBP +/- leg pain severe enough to prevent work or other physical activities Failure of conservative Rx (incl exercise program) Pain min 6/12 Pathology well localised on Ix (MRI, discography) Realistic patient expectations Contraindications No definite pathology to explain symptoms Multiple level degeneration where symptoms cannot be localised Major psychological stress Results - overall ~66% patients have satisfactory outcome from fusion Options Posterior fusion with instrumentation - gold standard for rare patient with true lumbar segmental instability Those patients with painful lumbar spondylosis LS are best served with a disc ablative procedure eg. ALIF & PLIF Circumferential fusions should be reserved for patients with significant canal pathologies, where revision is required, & other situations in which additional stabilization is required
Disc replacement surgery Not proven in Rx of discogenic pain, mainly because of considerable difficulty in identifying painful level (or levels) Intradiscal electrothermal coagulation
77 Orthopaedi UI
Sholahuddin Rhatomy,MD
Alternative to avoid fusion Attempt to denervate posterior annulus & cause thermal shrinkage of lax annular tissue Indication: discogram +ve degenerative disc disease with annular tears unresponsive to nonsurgical care for at least 6/12 Contraindication: focal disc herniation
Aetiology of disc degradation & herniation Not exactly clear why discs degrade, but not simply related to normal age changes Theories put forward include 1. End plate # which then causes disruption of delicate nuclear homeostasis 2. Autoimmune process analogous to sympathetic ophthalmia (not proven) Process of disc degeneration is believed to have biochemical basis, with inhibition of nuclear proteoglycan synthesis & enhanced matrix degradation caused by chemical mediators eg. IL-1, IL-6, nitric oxide (NO), PGE-2, & matrix metalloproteinases (MMPs) Intervertebral discs are able to withstand large forces (load to failure = 10,000 N) & 1st structure to fail will normally be vertebral end plate If a normal disc is loaded in presence of a radial tear or experimentally produced annular cut, the nucleus, because of its intrinsic cohesiveness, does not herniate; only a degraded disc will herniate
Natural history of disc degradation is either isolated disc resorption or disc herniation
78 Orthopaedi UI
Sholahuddin Rhatomy,MD
Disc pressure/failure Sitting-leaning forward > sitting > standing > lying on side > supine Rotation combined with flexion worst positions for disc injury Elevated by bending forward, bending to side, lifting, coughing, sneezing, & straining Asymmetric & cyclic loading combined with lateral bend, compression, & flexion risk factors for disc herniation
Thoracic disc prolapse
Very rare, only 0.5% of all prolapsed discs Cord compression & thoracic back pain from malignancy more common Most common in 4th decade 75% occur below T8; very rare above T4 Thoracic back pain radiating round chest with UMN signs in lower limbs MRI Rx Posterior surgery with laminotomy possible but spinal cord does not tolerate retraction Disc can be approached via a costotransversectomy, or transthoracic approach with fusion of affected level with rib strut graft
Lumbar disc prolapse
80% of population affected at some stage in their lives Most patients 30-50 yrs of age M:F = 2:1 Most herniations occur at L4-5 & L5-S1 interspaces
Pathology Disc herniation may vary in severity from disc protrusion to disc extrusion, to finally disc sequestration Disc containment Contained disc herniation - disc material herniated through inner annulus but not outer annulus, but still can distort path of nerve Non contained herniation - disc material penetrates both inner & outer layers of annulus > may reside beneath PLL or penetrate through it, or can be sequestered as a free fragment Posterolateral disc herniation Protruded disc usually compresses next lower nerve as that nerve crosses level of disc in its path to its foramen Note that each nerve emerges through upper part of foramen & lies against body of vertebra above
79 Orthopaedi UI
Sholahuddin Rhatomy,MD
Central (posterior) herniation In lower lumbar segments, central herniation may result in S1 radiculopathy Less frequently, a protruded disc above L2 vertebra may compress spinal cord itself or may result in cauda equina syndrome Far lateral disc herniation May compress nerve root above level of herniation Pressure on a normal nerve root will not cause pain, but pressure on an inflamed root will Depending on site of disc prolapse, nerve involvement will be as follows Nerve Root Affected Disc Prolapse L2/3 L3/4 L4/5 L5/S1 Posterolateral L3 L4 L5 S1 Far Lateral L2 L3 L4 L5
Features "Rules of Three" (Apley) 3 guidelines 1. Very young & very old seldom have acute disc prolapse In adolescents look for infection, benign tumours & spondylolisthesis In elderly look for vertebral compression # & malignancy 2. An ill patient has a more serious disorder 3. In disc prolapse, episodes of pain are generally punctuated by intervals of normality 3 warnings 1. Sciatica is referred pain which can also come from facet joints, SI joints or infection 2. Disc prolapse at most occurs at 2 levels; if multiple levels affected then suspect a neurological cause 3. Severe, unrelenting pain is not a feature of disc prolapse; suspect tumour or infection 3 major disorders to exclude 1. Inflammatory disorders eg. infection, ankylosing spondylitis
80 Orthopaedi UI
Sholahuddin Rhatomy,MD
2. Vertebral tumours cause severe pain & spasm 3. Nerve tumours eg. neurofibromata of cauda equina may cause sciatica but pain
is continuous Clinical Disc prolapse can cause both radiculopathy &/or radicular pain Varying amounts of back &/or leg pain; leg pain (nerve pain) > back pain (usually annular pain) Activities that increase intraspinal & intradiscal pressure eg. coughing, sneezing, & Valsalva maneuver often accentuate pain Symptoms usually subside in a few days or weeks & while present there is usually a list or scoliosis which may be towards the side of lesion (if prolapse is in axilla of root) or away from it (if it is lateral to root) Usually loss of lumbar lordosis & para-vertebral muscle spasm Typical radicular pain may be accompanied by paresthesias as well as varying degrees of motor, sensory, & reflex loss SLR Radicular lower extremity pain reproduced with between 35-70 of extremity elevation Key finding in sciatica, but is also found in Myogenic pain Ischial burisitis Annular tear Hamstring tightness Critical distinction made by sciatic stretch test Generally indicative of L5 or S1 compression Femoral stretch test indicative of L4 radiculopathy Neuro exam -> weakness, reflex changes, or segmental sensory loss Posterolateral disc herniation Protrusion is usually posterolateral, where it may compress roots of a spinal nerve Far lateral disc herniation 6-10% L4 nerve root most often involved Typically intense radicular pain (sciatic 25% & femoral 75% of time) Central disc prolapse At L5/S1 may cause bilateral S1 radiculopathy More proximally -> caudal equina syndrome Bilateral LMN weakness in legs Loss of perianal sensation: "saddle anaesthesia" Loss of anal tone: faecal incontinence Sphincteric disturbance Inability to sense bladder filling, painless retention & overflow: urinary incontinence This is a surgical emergency requiring emergency MRI & subsequent decompression within 24 hrs of onset of symptoms Meta-analysis of Literature on Cauda Equina Syndrome - Spine 2000
Investigations
81 Orthopaedi UI
Sholahuddin Rhatomy,MD
X-rays List or scoliosis may be evident Exclude bony pathology (Macnab) Traction spur 2-3 mm from distal border of anterior & lateral surfaces of vertebral bodies at point of attachment of outermost anular fibres denotes segmental instability Knuttson's sign of gas in disc (disc vacuum sign) MRI Ix of choice 29% prevalence of disc herniation in asymtomatic individuals Characterized by extension of disc beyond margins of adjacent vertebral bodies Changes in disc Normal, hydrated NP has an increased proton signal on T2 With increasing desiccation, this signal blends with that of surrounding annulus With further degeneration, a dark, isointense signal may be seen on T2 An increased T2 signal may be noted in some areas, where it is thought to represent free fluid in annular tears & fissures Changes in endplate Modic Type I Associated with acute end-plate disruption & fissuring with ingrowth of vascularized fibrous tissue into adjacent vertebral body marrow Decreased signal intensity on T1 & increased signal intensity on T2 Seen in ~5% of patients who undergo MRI scanning for disk disease Modic Type II In chronic degeneration, hematopoietic (red) peridiscal marrow undergoes fatty degeneration Increased signal intensity on T1 & slightly increased signal intensity on T2 Seen in ~16 % of patients Modic Type III Sclerosis is caused by presence of woven bone End-plate defect sometimes with Schmorl's nodules (intraosseous herniation of disc material) Can be a/w sclerosis within vertebral body adjacent to intravertebral herniated disc Hypointense signal on both T1 & T2 CT myelography if patient cannot have MRI eg. intra-cranial clips, pacemaker
Natural History Up to 90% of patients, gradual & progressive resolution of symptoms without surgical intervention within 3/12 of onset of symptoms After 1st episode 90% improve & do not relapse 2nd episode 90% improve & 50% relapse 3rd episode 90% improve & 100% relapse Regardless of Rx, impaired motor function had good prognosis whereas sensory deficits remained in almost one half of all patients
Treatment MAJORITY REQUIRE NO SURGICAL INTERVENTION - 90%
82 Orthopaedi UI
Sholahuddin Rhatomy,MD
Non-operative NSAIDs Short period of bed rest Activity modification Physiotherapy: back classes helpful Epidural injections of LA steroid -> 60-85% success in short term & 30-40% in long term (6/12)
Operative Indication 1. Unrelenting leg pain despite adequate conservative measures 2. Neural damage 3. Cauda equina syndrome Goals o Alleviate neural compression without further injury to affected nerve root(s) o Minimal disruption of surrounding normal tissues & maintenance of spinal stability Fenestration of ligamentum flavum & laminotomy with excision of disc o Standard operative Rx o Excellent for eradicating leg pain but not for back pain o Risk of reherniation at same level on same side 5% o Addition of spinal fusion at same time as discectomy not proven to be superior to simple discectomy & adds considerable morbidity Disc replacement surgery o Not proven in Rx of discogenic pain, mainly because of considerable difficulty in identifying painful level (or levels) Cx o Periop: incidental durotomy, wrong-level & wrong-sided surgery, retained disk fragments with persistent radiculopathy, wound infections o Late: disc space infection, recurrent disc herniation (5-10%), postop instability Cochrane Review o Standard discectomy (fenestration & discectomy) better than microdiscectomy better than chemonucleolysis o Use of gel foam, free fat grafts, or ADCON-L gel has been studied - no difference between free fat grafts or gel foam, but free fat caused less dural scarring o Multi-centre trials in USA & Europe -> lower incidence of scar formation following use of gel Weber et al Spine 1983 o Only trial that compared surgical Rx of lumbar disc prolapse with any form of natural history, conservative Rx, or placebo o Prospective controlled trial which compared long-term outcomes of Rx by discectomy vs initial conservative Mx followed by surgery if conservative therapy failed o Trial not blinded & considerable crossover o Both patient & observer ratings showed that Discectomy significantly better than 'conservative therapy' at 1 yr But no significant differences in outcomes at 4 & 10 yrs o Malter re-analysed Weber's data & suggested that discectomy was highly cost-effective, at ~$29,000 per QALY gained
83 Orthopaedi UI
Sholahuddin Rhatomy,MD
COMPARISON TABLE Disc herniation Age Levels Symptoms Prognosis 30-50 L4-5, L5-S1 Leg > back 90% improve Degenerative disc disease Spondylolisthesis All ages L4-5, L5-S1 Asymptomatic Spinal stenosis 70-80 L4-5, L3-4 Leg > back Unchanged in 70% Worse in 15% Improved in 15% Majority Severe neurologi cal symptom s Failed conserva tive + impaired ADL
LBP
Conservativ e Surgical
90% Unrelenting leg pain Neural damage, CES
Most Chronic disabling LBP +/- leg pain Failed conservativ e Pathology well localised Realistic patient expectation s
Mainstay Slip >50% or progressing in adolescents Back &/or leg pain unresponsive to nonoperative Rx Functionally significant neurological deficit
Spondylolysis & Spondylolisthesis
SPONDYLOLYSIS
A defect in pars interarticularis (between superior articular process & remainder of lamina), most often involving L5 Can occur independently or be a cause of spondylolisthesis Most common cause of LBP in adolescents Aetiology Usually fatigue # from repetitive hyperextension stresses (gymnasts) Genetic tendency for stress # of pars to occur in first years of upright posture Family members of affected individuals Certain Eskimo tribes Sacral spina bifida & sacralisation of 5th lumbar vertebrae Patients with thoraco-lumbar Scheuermann's disease & thought to be a/w compensatory increase in lumbar lordosis Radiology Plain X-rays demonstrate 80% of lesions Oblique views - additional 15% picked up - 'Scottie dog' sign (Lachapelle)
84 Orthopaedi UI
Sholahuddin Rhatomy,MD
CT - may miss # Bone scan - increased uptake indicates an acute/recent lesion which will probably heal Non-union common
SPONDYLOLISTHESIS
"Spondy" refers to vertebrae & "listhesis" means "to slip" Displacement of a cephalad vertebra on an adjacent caudal vertebra Slippage can be anterior, posterior, or lateral When spondylolysis is bilateral, superior articular processes are attached to body by pedicles, but most of lamina, spinous process, & inferior articular processes are detached; body of involved vertebra may displace anteriorly Usually L4/5 & L5/S1 Normally laminae & facets constitute a locking mechanism preventing forward slippage
Classification (Newman, Wiltse, McNab)
Dysplastic/Congenital (20%) Isthmic (50%)
Child
5-50
Degenerative (25%) Post-traumatic Pathological Post-operative
Older Young Any Adult
Superior articular facets of S1 are congenitally defective Associated with spina bifida occulta Caused by spondylolysis (L5/S1) A. Lytic - fatigue # of pars interarticularis B. Elongated but intact pars interarticularis C. Acute # of pars interarticularis Degenerative disc disease & degenerated facet joints (L4/L5) -> subluxation From acute # in some other portion of vertebra that allows a slip to occur An isolated pars # is not seen with this lesion Tumours, infections, Paget's... Direct: excessive resection of neural arches/facets Indirect: transition above or below a previously fused segment
85 Orthopaedi UI
Sholahuddin Rhatomy,MD
Severity of Slip Percentage of slip of AP diameter of vertebra below (Meyerding classification) Grade I <25% Grade II 25-50% Grade III 50-75% Grade IV 75-100% Grade V >100% (spondyloptosis) Slip angle o Normal = >0
Clinical Rarely symptomatic May be discovered only incidentally on X-rays Injury may aggravate any symptoms Usually pain begins insidiously during 2nd or 3rd decade with walking & standing Flattening of back Spinous process step-off & buttocks appear heart-shaped Restricted motion of lumbar spine Tight hamstrings -> inability to bend at hips with knees fully extended Claudication may signal development of lateral stenosis
Radiology Plain X-rays should be taken standing Grade slip Slip angle Oblique X-rays Bone scans - see above CT - evaluates osseous architecture & provides better view of pars interarticularis & posterior elements MRI Evaluates disc But can see a pseudodisc herniation due to rotatory element of slip
86 Orthopaedi UI
Sholahuddin Rhatomy,MD
Treatment Non-operative Rule out other causes of low back discomfort, eg. disk herniation, bone or spinal cord tumors, or disc space infection in Rx of low-grade spondylolisthesis Mainstay of Rx in patients with <50% slip progression Combination of activity modification, trunk strengthening, & bracing Bracing If symptoms persist in spite of activity modification, bracing or surgery might be indicated Painful spondylolysis, but no slip, should be treated by bracing for 6-8/12 then gradual brace removal Adolescents - X-rays every 6/12 until maturity Risk factors for slip progression 1. Young age at presentation 2. Females 3. Slip angle > -10o 4. High grade slip (>50% slip progression) 5. Dome shaped sacrum 6. Inclined sacrum (>30o beyond vertical)
Operative Indications Slip >50% or progressing in adolescents Back &/or leg pain unresponsive to non-operative Rx Functionally significant neurological deficit Grade I & II In situ L5-S1 posterolateral fusion (& decompression) Repair of pars defect & fixation using a lag screw or wires has been described for low grade slips (<25%) Grade III, IV & V Extended in situ posterolateral fusion from L4 to S1 (& decompression) Fusion to L4 required, for increased stability & because L4 disc will become degenerative by middle age Try reduce kyphosis Children - posterior intertransverse fusion without instrumentation Adults - decompression without fusion used for elderly degenerative spondylolisthesis as likelihood of progression very low Instrumented fusion Debatable Decompression Carragee, 1997 -> addition of decompression to posterolateral arthrodesis may actually increase rate of pseudoarthrosis & clinical failure Reduction Most children & adolescents with grade III & even grade IV slips do not require reduction Potential advantages Decreased pseudarthrosis rate Stabilization of deformity Minimization of length of fusion Improved cosmesis
87 Orthopaedi UI
Sholahuddin Rhatomy,MD
Prevention of acute postop cauda equina syndrome Techniques include femoral traction, cast reduction, instrumented reduction, combined anterior-posterior approach Cx Most significant - traction on L5 nerve root Nerve root injuries not only occur at level of spondylolisthesis but may also occur throughout lumbosacral plexus because of trunk lengthening that occurs with reduction Anterior interbody fusion for failed posterior fusions, salvage procedures
Spinal Stenosis
Introduction Narrowing of spinal canal, nerve root canal or intervertebral foramen producing root ischemia & neurogenic claudication Lumbar spinal stenosis is 1 manifestation of general process of spinal degeneration that occurs with aging, & often becomes symptomatic in 7th & 8th decades of life L4-L5 segment most commonly affected, followed by L3-L4 Men > women, because their spinal canals narrower at L3-L5 levels
Anatomy Central canal of spinal column conveys spinal cord in cervical, thoracic & upper lumbar levels In most individuals, spinal cord ends by L1 level; below this level remaining lumbar & sacral nerve roots travel as cauda equina Nerve roots are more tolerant to chronic pressure than spinal cord -> individual may tolerate higher degree of stenosis in lower lumbar spine than in cervical or thoracic region Boundaries of central canal vary with level of vertebral body At level of a vertebral body Canal is bordered by body itself anteriorly, pedicles laterally, & laminae posteriorly This is the site that is affected in cases of congenital stenosis, where pedicles are typically shortened At level of intervertebral disc Anterior border is formed by annulus, posterolateral borders by facet joints & capsules, & posterior border by ligamentum flavum These are the structures most affected by degenerative processes Dimensions of spinal canal & foramen are influenced by dynamic & postural factors When a person rises from recumbency to standing, resulting axial load on intervertebral disc causes further bulging of annulus, which in turn further compromises central canal & foramen Foramina decrease in size while nerve roots increase in diameter as you move down spine, thus lumbar spine most commonly affected
Aetiology Classification - Arnoldi (1976) Congenital
88 Orthopaedi UI
Sholahuddin Rhatomy,MD
Developmental Achondroplasia Acquired Degenerative Spondylolisthetic Worse if imposed on a developmental narrowing Disc herniation Degenerative & disc herniation Degenerative & congenital Others Paget's Spinal tumour Infection (TB) Post-surgery Trauma
Pathophysiology Narrowing of central canal &/or intervertebral foramina is due to 1. Annular bulging 2. Bone spur formation 3. Facet joint enlargement 4. Ligamentous hypertrophy Compression of neural structures also compresses vascular supply of nerves so that symptoms are predominately those of neural ischemia
89 Orthopaedi UI
Sholahuddin Rhatomy,MD
Because both neural canal & neural foramen are narrowed with spine in extension & opened in flexion, neural compression is most often temporary Pain induces patients to change position & relieve nerve pressure before permanent neurologic damage
Mechanism (Howe et al. Pain, 1977) When standing or walking lumbar lordosis increases stenosis Subarachnoid obstruction occurs Diffusion of fluid from endoneurium into subarachnoid space impaired Increased endoneurial pressure -> 'Compartment Syndrome' in nerve roots Conduction disturbances A nerve which has been repetitively injured becomes more easily irritated by dynamic factors
Classification by site Central stenosis Compression of thecal sac & cauda equina Caused by Arthritic facets with medial encroachment Congenitally narrow canal ('trefoil' shape) Spondylolisthesis Central disc herniation Posttraumatic Post-surgical Lateral stenosis Compression of nerve root Caused by Superior articular facet enlargement Lateral disc herniation Ligamentum flavum hypertrophy Uncinate spurring Types 1. Lateral recess stenosis - affects traversing (lower) nerve root 2. Foraminal stenosis - affects exiting (upper) nerve root 3. Extra-foraminal (far-out)
90 Orthopaedi UI
Sholahuddin Rhatomy,MD
Pathology Minimal cross sectional area is normally at level of facet joints & is least at level of L3/4 Narrowest AP diameter usually from posterior vertebral wall to upper border of spinous process Verbiest defined <10 mm as absolute stenosis & <12 mm as relative stenosis In cervical spine <13 mm AP diameter or <0.8 times AP diameter of adjacent vertebral body is defined as spinal stenosis 3 3 3 Canal area of 180 m +/- 50 m is normal in lumbar spine, <100 m is spinal canal stenosis & 1003 130 m is early or relative canal stenosis Interpedicular distance should be 16 mm & lateral canal usually measures 5 mm diameter & <2 mm indicates stenosis Developmental stenosis or degenerative disease in association with vascular problems (venous hypertension or ischaemia), inflammation of neural elements & irritation of cauda equina, nerve roots, sinu-vertebral nerve & posterior primary rami Central canal stenosis may be exaggerated by hypertrophy (realy just bunching up) of ligamentum flavum, hypertrophy & osteophyte formation of facet joints, annular bulging of disc & thickening of lamina Lateral recess stenosis can result from loss of disc height & over-riding facets, osteophyte formation of facet joints, hypertrophy of ligamentum flavum/capsule of joint (probably not true hypertrophy but bunching up) & posterior annular bulge Impingement may also be caused by extradural arachnoid cysts or perineural cysts
Clinical Virtually all individuals in 70's have some degree of spinal stenosis on imaging studies, but only a fraction manifest true symptoms of central &/or foraminal stenosis Symptoms of stenosis are usually unilateral or bilateral leg pain, with or without back pain Insidious onset & slow rate of progression Pain occurs when upright & particularly when walking Typical symptoms: leg pain, numbness, weakness developing after patient walks a predictable distance Patient seeks relief by sitting, leaning forward to "relieve pressure" putting his foot on a raised rest, or lying down
91 Orthopaedi UI
Sholahuddin Rhatomy,MD
Central stenosis Compression on cauda equina -> neurogenic claudication -> bilateral aching, cramping, or burning sensation in legs Increased unsteadiness or loss of balance Feeling better if they walk stooped forward Rarely urinary incontinence & cauda equina syndrome Foraminal stenosis Radicular signs from narrowing of lateral recess or neural foramen PE can be unimpressive in patients with central stenosis Ambulate with forward-leaning posture & moderately broad-based gait Check distal pulses to screen for vascular causes of claudication Stress test = walk until symptoms occur Phalen test may be specific; with patient upright, bend patient into extension for a full minute Difference to vascular claudication Activity Walking Uphill Walking Rest Bicycling Lying Flat Vascular Claudication Neurogenic Claudication
Distal-proximal pain; calf pain Proximal-distal thigh pain Symptoms develop sooner Relief with standing Symptoms develop Relief -ve Symptoms develop later Relief with sitting or bending No symptoms May increase symptoms +ve
Paraesthesia & weakness after walking
Investigations X-rays Bone spurs, decreased disc height & facet hypertrophy in older patients Degenerative spondylolisthesis & degenerative lumbar scoliosis Instability Dynamic lateral radiographs for abnormal motion or instability at any level Normal anterior & posterior translation from L1 to L5 is ~8% of length of vertebral body or ~4 mm Note that typical degenerative changes of osteophyte formation, decrease in disc height, & ligament calcification will serve to limit motion CT More accurate & detailed picture of bony anatomy Less accurate than MRI in estimating degree of compromise of soft tissue elements, thus can underestimate degree of stenosis Spinal canal <10 mm AP diameter = absolute stenosis MRI (without gadolinium) Currently gold standard in evaluation of central stenosis Allows visualization of disc, neural elements, ligamentum flavum & thecal sac Epiradicular nerve root block Improvement of radicular symptoms after injection of anaesthetic suggestive of lateral (foraminal) stenosis Myelography
92 Orthopaedi UI
Sholahuddin Rhatomy,MD
No longer routinely necessary, although can be useful in selected cases Provides most complete anatomic evaluation of compression of neural elements within lumbar spine Also allows for dynamic assessment of stenosis with spine in maximal flexion & extension -> segmental instability, disc bulging, ligamentum flavum infolding in extension Cx Headaches 20-30% & a few are severe & require blood patch 30% have nausea & seizures may occur if contrast gets around base of skull or brain Anaphylaxis is rare & a/w allergies when contrasts used IV (less so in CSF)
Natural History 2 studies following 49 patients (Hayashi) & 32 patients (Johnsson) for 5 yrs (with non-operative Rx) Symptoms unchanged in 70% Worse in 15% Improved in 15%
Treatment Non-Operative Medications NSAIDs Muscle relaxants Antidepressants for chronic radicular pain Calcitonin Activity modification Physiotherapy Massage, ultrasound, TENS, acupuncture, biofeedback, hot or cold packs, traction, manipulation Can offer symptomatic relief of radicular or low back pain, but not for claudicant symptoms Most useful: therapeutic stretching & strengthening exercises for abdominal & spinal extensor muscles, & aerobic fitness training Flexion brace (Williams brace) - prevents lordosis but not well tolerated Epidural & nerve root block steroid injections - good long-term relief in patients with foraminal or lateral recess stenosis
Operative Indications 1. Severe neurological symptoms: progression of functionally disabling neurologic deficit or CES -> urgent surgical intervention 2. Failed conservative Rx + impaired ADL Surgery reserved for patients with evidence of severe spinal stenosis on imaging studies & have preponderance of lower extremity symptoms Decompression in patients with predominant back pain has poorer outcome than patients with mainly leg pain symptoms
93 Orthopaedi UI
Sholahuddin Rhatomy,MD
Decompression good for relieving leg pain but may not improve back pain & in fact may increase instability problems with occasional need for associated spinal fusion (particularly if major component of symptoms is back pain or if degenerative spondylolisthesis with stenosis - best results if fuse as well as decompress) Decompression procedures o Central stenosis Partial laminectomy for patients without segmental instability (eg. spondylolisthesis) Total laminectomy should be avoided o Lateral recess stenosis Medial facetectomy - medial margin of superior facet, facing spinal canal, is resected only o Foraminal & extra-foraminal stenosis Extra-spinal approach to dorsal root ganglion (in intervertebral foramen) Resect lower lamina laterally & caudally until dural sac is seen; pediculotomy may be required Spinal fusion o With no segmental instability, arthrodesis may not be required (assuming posterior elements have not been destabilized) o Indications Preop instabilty (spondylolisthesis) Instability expected from resection of facet joint Sagittal inclination of facet joint Bilateral discectomy along with laminectomy High demand postop activities o Posterolateral fusion Operative results o Variable due to 1. Not all stenotic sites necessarily cause symptoms -> selecting decompression levels can be difficult 2. Insufficient decompression 3. Incorrect levels 4. Postop instability 5. Regrowth of resected tissue & scarring o Multi-level involvement does not do well due to postop instability (should consider fusion, but very invasive) o Careful attention to patient selection & meticulous operative planning important in optimizing surgical outcome o Central canal stenosis decompression: 65-85% good outcome o Nerve root decompression: 62% complete success & 24% partial success (Crock S1 decompression) o Degenerative spondylolisthesis preop have 40-65% risk of further slipping & 65% good result postop (further slipping not a/w poor prognosis)
References Current Orthopaedics. Mini-Symposium: 13(3). July 1999 Apley Miller
94 Orthopaedi UI
Sholahuddin Rhatomy,MD
Ankylosing Spondylitis
Diagnosis One of seronegative spondyloarthropathies, others being Reiter's disease Behet's disease Psoriatic arthropathy Arthropathy a/w inflammatory bowel disease (Crohn's & ulcerative colitis) Rome criteria for AS Clinical LBP & stiffness >3/12 not relieved by rest Pain & stiffness in thoracic region Limited motion in lumbar spine Limited chest expansion History of evidence of iritis or its sequelae Radiological X-rays - bilateral sacroiliac changes characteristic of AS Diagnosis Radiological criterion + 1 clinical criterion, or 4 clinical criteria in absence of radiological sacroilitis
Incidence Affects spine & sacroiliac joints primarily Prevalence of 2:1000 in Western Europe but much lower in Japan & Negroid races Affects young men (age 15-25 yrs), but may also begin in middle-aged men M:F between 2:1 & 10:1 Strong familial tendency
Aetiology Cause unknown HLA-B27 found in 90% of patients & 50% of their relatives
Pathology Preferential involvement of tendon & ligament insertions has coined term enthesopathy 2 basic lesions 1. Synovitis of diarthrodial joints Synovitis of SI joint & facet joints causes destruction of articular cartilage & periarticular bone Costovertebral joints commonly affected which causes reduced respiratory excursion When other joints affected same changes occur 2. Inflammation of fibro-osseous junctions of syndesmotic joints This affects intervertebral discs, SI joint ligaments, manubriosternal joint, pubic symphysis & bony insertions of large tendons Pathological changes occur in 3 stages 1. Inflammatory reaction with round cell infiltration, granulation tissue & destruction of bone 2. Replacement of granulation tissue with fibrous tissue
95 Orthopaedi UI
Sholahuddin Rhatomy,MD
3. Ossification of fibrous tissue leading to ankylosis of joints
Clinical features Spine
Insidious onset of backache & stiffness in an adolescent or young adult, recurring at a number of intervals over a number of yrs Pain may be referred into buttock & be confused with sciatica Early in disease process, little to find on clinical exam apart from slight loss of lumbar lordosis, limitation of extension of spine & SIJ tenderness Later patients have characteristic posture Loss of lumbar lordosis Thoracic kyphosis Forward thrust of neck Flexed hips & knees Unable to perform "wall test" Patient asked to stand with back against wall Should normally be able to touch occiput, scapulae, buttocks & heels to wall In advanced cases entire spine may be completely ankylosed Chest expansion often markedly reduced <7 cm Peripheral arthritis May involve hips, knees, ankles, toes, (rare upper extremities) in >30% of cases May precede back pain by several years Arthritis is acutely painful but rarely chronic or destrcutive Hip joint Affected in up to 50% of patients with AS Often bilateral Protrusio & hip flexion contractures common Achilles tendon insertion pain Extraskeletal manifestations Eyes: uveitis & conjunctivitis in 20% Heart: aortic valve disease, carditis (rare) Lungs: pulmonary fibrosis (rare) GU: prostatitis Disease is often more severe when it occurs early in life
Spine Fractures in AS X-rays Cardinal sign & earliest feature is sacroiliitis Symmetric, bilateral subchondral erosions, followed by subchondral sclerosis Iliac side affected 1st followed by ankylosis Occult # Loss of reduction Progressive kyphosis Non union Progressive neural deterioration Epidural hematoma - neurologic deficit occuring at higher level than at # site may indicate expanding hematoma which is more common in AS Death in >50% of cases
96 Orthopaedi UI
Sholahuddin Rhatomy,MD
Spine
Disease 1st affects lumbar spine & then ascends to thoracic spine Vertebrae appear squared off on lateral radiographs Later syndesmophytes form between bodies, bridging several levels which can lead to "Bamboo" or "Rugger Jersey" spine Facet joint are simultaneously obliterated Peripheral joints may show erosive arthropathy or ankylosis
Special Investigations Inflammatory markers raised early in disease HLA-B27 present in 90% of cases, but important to note that only a fraction of people with HLAB27 antigen develop ankylosing spondylitis
Treatment Majority of patients despite disease can lead active life Aims 1. General measures to maintain satisfactory posture & preserve movement Physiotherapy & exercise encouraged Sleep in prone position Aim to remain as mobile as possible for as long as possible 2. NSAIDs to help with pain & stiffness These can help patient to perform exercise but do not themselves affect course of disease 3. Surgery to correct deformity & restore mobility Corrective osteotomies of lumbar & cervical spine can be performed if deformity severe enough, but potentially hazardous Total joint replacement, especially THR may be needed Higher infection rate Hetertopic ossification Occurs in 20-40% of THR More common with trochanteric osteotomy To avoid HO, consider insertion of a cemented acetabular component followed by 750 rads around component Careful evaluation needed following cervical spine injury as they can have unstable # with risk of developing non-union
Diffuse Idiopathic Skeletal Hyperostosis (DISH) / Forestier's Disease / Ankylosing Hyperostosis Fairly common disorder which affects older men Characterised by widespread ossification of ligament & tendon insertions Particular involvement of spine but unlike ankylosing spondylitis it is not an inflammatory condition, & spinal pain & stiffness not a feature
97 Orthopaedi UI
Sholahuddin Rhatomy,MD
Spine Infections
Vertebral Osteomyelitis (Pyogenic Spondylitis)
Incidence Uncommon 2-4% of all osteomyelitis ~70% of cases >50 yo Site of infection Lumbar spine = most often affected but uncommonly cause paralysis Thoracic & cervical regions affected less often but have higher incidence of paralysis
Aetiology 70% arise from UTI, chronically ill, elderly adults Due to Batson's venous plexus = communication between pelvic & vertebral plexus (NB surgically) Risk factors Older debilitated patients IV drug addicts (pseudomonas) History of pneumonia, UTI, skin infection Immunocompromised patient Organisms Staph aureus most common (>50%) but MRSA increasing Gram -ve (E. coli, Pseudomonas, Proteus) & anaerobes on the increase Strep viridans Brucellae, candidae, coccidiomycosis (in immunocompromised)
Pathophysiology Thought to be a secondary manifestation of infection elsewhere Haematogenous spread most common (Batson's complex) Organisms settle in metaphyseal region of vertebral body Toxins cause thrombosis, infarct, abscess, blocks nutrition Frequently extend into & destroy adjacent intervertebral discs; usually 2 vertebral bodies & a disc space affected Purulent material may break out of cortex anteriorly to form paravertebral abscess or posteriorly to form epidural abscess Weakening of bone may cause vertebral collapse
Clinical Often significant delay in diagnosis (6-12/52) Insidious course, with back pain developing over 1-3/12 Triad = fever + back pain + tenderness
98 Orthopaedi UI
Sholahuddin Rhatomy,MD
Consider bacterial endocarditis Neurology Incidence of neurological deficit may be as high as 40% Suggests epidural extension of abscess (usually located anterior to neural elements)
Radiology X-rays 2 weeks - disc space narrowing (infections involving vertebral bodies frequently extend into & destroy adjacent intervertebral discs; usually 2 vertebral bodies & a disc space affected) 6 weeks - erosion of vertebral body end-plate; osteolysis 8 weeks - reactive sclerosis due to trabecular collapse 12 weeks - new bone formation - distinct from TB: see soft tissue calcification, less sclerotic response 6-12 months - intervertebral fusion, usually signifies resolution of process Disc destruction is atypical of neoplasms Examine paravertebral soft tissues - retropharangeal & psoas contours
MRI
Very sensitive & specific (for differentiating from tumour) Gadolinium enhances sensitivity High signal on T2 & decreased signal on T1
Investigations Bacteriologic diagnosis essential Blood cultures
99 Orthopaedi UI
Sholahuddin Rhatomy,MD
Percutaneous CT guided needle biopsy +ve in 68-86% of cases Infections of upper cervical spine & sacrum not safely accessible to needle aspiration Do stains for AFB & fungi Open biopsy considered if closed biopsy -ve after 2 attempts Tuberculin skin tests for TB FBC, ESR, CRP, bone biochemistry ASOT Anti-staph titres MSU
Treatment Non-operative 1st line of Rx IV antibiotics for 2/52 then oral for 3/12 Bed rest Spinal brace till 6/52 or healing ESR used to follow Rx effects (gallium scans can also be used) Good prognostic signs Age <60 yrs Normal immune status Decreasing ESR Staph aureus infection Operative Indications 1. Need for open biopsy 2. If neurology not settling 3. Instability due to vertebral collapse 4. Paraspinal or epidural abscess 5. Failure of response to medical Rx Anterior decompression & strut graft Anterior approach provides better exposure for draining associated psoas & paraspinal abscesses With adequate debridement & antibiotics, bone grafts used for stabilisation do well with over 90% fusion Role of spinal instrumentation controversial; with large deformity, posterior instrumentation may be indicated
DISCITIS (JUVENILE)
Occurs primarily in younger patients Lumbar spine most common location Usually self-limiting infection/inflammation of intervertebral disc or end plate Blood-borne or direct infection usually during procedures Probably autoimmune (Bianco), no sepsis to be found May represent extension of subacute vertebral end-plate OM which does not produce progressive vertebral OM
100 Orthopaedi UI
Sholahuddin Rhatomy,MD
Clinical Unlike osteomyelitis, usually no systemic symptoms (children typically afebrile) Child typically c/o back pain & refuses to flex spine May also c/o hip or abdominal pain & may refuse to stand or walk Tenderness over spine, paravertebral muscle spasm, loss of normal lumbar lordosis, limitation of spine motion
Investigations WBC usually normal ESR elevated >40 When a causative organism can be identified, it is most commonly Staph aureus Biopsy indicated only for children who fail to respond to non-operative Mx, & for older children & adolescents in whom a different organism may be suspected or if TB or tumor suspected
Radiology X-rays
May appear normal early on Disc-space narrowing Irregularity involving adjacent vertebral end-plates Later, in adult, disc space usually goes on to fusion, whereas in child disc space usually restored Bone scan Tch bone scan demonstrates increased uptake of isotope in infected disc space - may be useful in early diagnosis MRI More sensitive than bone scans in early discitis Decreased signal on T1 images & increased signal on T2
Treatment Bed rest Use of spinal immobilization with a cast or orthosis depends on severity of symptoms (avoid traction) Empirical systemic antibiotics (although probably make no difference) Since vascular access to disc more abundant in children, antibiotics are usually successful
101 Orthopaedi UI
Sholahuddin Rhatomy,MD
Penicillinase resistant synthetic penicillin or cephalosporin, even if cultures not +ve
TUBERCULOSIS
10% of TB involves bone Spine - most common site of skeletal TB (>50%) Thoracic spine most commonly involved (lumbar for OM & discitis) with T10 commonest Usually involves multiple levels (average ~3) May have 'skip lesions'
Pathology Pathogenesis Usually a secondary infection - primary lesion in lung, GIT or GUT Blood borne infecton usually settles in vertebral body anteriorly adjacent to disc (paradiscal vertebra) Bone destruction & caseation follow Infection then spread to disc space under anterior longitudinal ligament to involve metaphyses of adjacent vertebrae -> destruction of several contiguous levels or skip lesions (15%) or abscess formation (50%) Usually more bone destruction, more sequestra, larger abscess, gaseous pus than pyogenic OM Paraspinal abscess formation more common than pyogenic OM Intervertebral discs, being relatively avascular is relatively spared & preserved until late disease Anterior vertebral body collapse causes sharp kyphosis With progressive kyphosis -> risk of cord compression Risk of cord damage due to Pressure by abscess or displaced bone Ischemia from spinal artery thrombosis Pott's paraplegia 10% of TB spine Early onset paralysis due to pressure by 1. Abscess 2. Caseous material 3. Sequestra Late onset paralysis due to 0. Increasing deformity 1. Reactivation 2. Reduced cord blood supply
Clinical Subacute presentation Non-specific Fever, night sweats, anorexia, weight loss Most common presenting symptom is back pain Deformity, cold abscess, neurology
102 Orthopaedi UI
Sholahuddin Rhatomy,MD
Investigations CXR (2/3 have abnormal CXR) ESR high WBC variable Tuberculin skin test Delayed hypersensitivity reaction In Mantoux test 0.1 ml of purified protein derivative injected intradermally +ve reaction: a papule of >15 mm diameter at 72 hrs In Heaf test Purified protein derivative placed on skin A gun is used to produce multiple punctures +ve reaction: >4 papules at puncture sites at 72 hrs +ve if Active infection BCG vaccination or subclinical exposure to TB -ve does not mean not infected, eg. in immunocompromised Biopsy Definitive diagnosis HPE Central necrotic area surrounded by histiocytes & giant cells with nuclei at margin of cell (= Langerhans giant cells) Microscopy Stain for Acid Fast Bacilli (Ziel-Neelsen stain) Only 50% of cases +ve Culture Requires use of enriched Lowenstein-Jensen medium at 35-37 & adequate oxygenation Cultures only visible at 2-4/52
Radiology X-rays
Include entire spine (skip lesions) No single diagnostic pathognomonic sign Earliest sign: local osteoporosis of 2 adjacent vertebrae with preservation of disc Typically, anterior destruction of 2 adjacent vertebrae & destruction of intervening intervertebral disc Later bone destruction, collapse of adjacent vertebral bodies into each other Paraspinal soft tissue shadows due to paravertebral abscess With healing bone density increases & paravertebral abscesses may calcify Less calcificaton cf pyogenic OM o Kyphosis = angulation >4 at each level
103 Orthopaedi UI
Sholahuddin Rhatomy,MD
Bone scans High false -ve rate with Tch & Gallium scans MRI May distinguish abscess from granulation tissue More difficult to discern between TB & neoplasia Assess cord compression Site & size of abscesses
Treatment Aims
1. To eradicate disease 2. To prevent or correct deformity 3. To prevent paraplegia
Non-operative o Indications Early disease with minimal bone involvement Medical contraindications to operation o Antituberculous drugs Forms basis of Rx (not surgery) Treat for 6-12/12 RIPES - Rifampicin, Isoniazid, Pyrazinamide, Ethambutol, Spectinomycin Regimes Intensive phase Continuation phase o Drug Dly. dose BW. dose Max. dose dly 600 mg BW 600 mg Adverse reaction Orange discolouration of body fluid Hepatitis Flu like reaction Vomiting Thrombocytopenia Drugs EHRZ RH Daily doses x 2 months (total of 56 doses) Biweekly doses x 4 months (total of 32 doses)
Rifampicin
10 mg/kg/day
10-15 mg/kg/day
104 Orthopaedi UI
Sholahuddin Rhatomy,MD
Isoniazid Pyrazinamide
5-8 mg/kg/day
15-20 mg/kg/day
Hepatitis dly 300 mg Peripheral neuritis BW 1200 mg Hypersensitivity dly 2 gm dly 1.2 gm Hepatotoxicity Hyperuricaemia Optic neuritis Gastrointestinal disturbance Hypersensitivity Ototoxicity Nephrotoxicity Skin rash
20-40 mg/kg/day
Ethambutol
15-25 mg/kg/day
Streptomycin
15-20 mg/kg/day
15-20 mg/kg/day
1 gm
o Spinal orthosis to prevent deformity o Bed rest for more advanced disease Surgery o Literature Clinical trials (1978) Anti-TB alone as effective as any other methods (including surgical debridement) in stemming disease o However, in 10-yr follow-up, kyphosis increased by average of >17 MRC Working Party on TB of the Spine 1998 (15 yrs follow-up) A short course of INH & rifampin as effective as standard 18 month regime in uncomplicated TB spine Excellent results with outpatient chemotherapy, with no late relapse or late onset paraplegia No advantage with wearing a plaster jacket nor is there any advantage to bed rest Outcome 87% of favorable outcome in all 3 Rx group ChemoRx alone ChemoRx + debridement ChemoRx + debridement + anteriror fusion Only advantage of radical excision with bone grafting over open debridement was less late deformity Leong 1990 Anterior resection of diseased tissue & ASF -> early & complete eradication of infection, & prevention of deformity o Indications 1. Large abscess palpable posteriorly 2. Neurology 3. Instability 4. No response to medical therapy (no improvement after 2/52) 5. Patients <15 yrs with kyphosis >30o (high risk for progression of kyphosis) o Adjuvant chemotherapy beginning 10 days before surgery essential o Hong Kong Procedure recommended Radical anterior debridement Anterior fusion with iliac strut grafting (allows better correction of kyphosis) o Advantages Adequate material for analysis Prevention of progression of abscess
105 Orthopaedi UI
Sholahuddin Rhatomy,MD
Relieve pressure on neural tissue Graft under compression - fusion almost sure, thus late kyphosis prevented
Prognosis Good prognosis for recovery in neurological compromise of active disease Poor prognosis in paraplegia of healed disease probably due to causes eg. fibrosis constricting cord, or impingement of cord on hard bony bridge arising from multilevel disease Severe kyphotic deformity may result if a larger number of levels involved
EPIDURAL ABSCESS
Dorsal abscess follows intervention or surgery - most common Ventral abscess when a/w discitis or osteomyelitis More common in immunocompromised, malignancy, DM, alcohol abuse, invasive procedures, vertebral # Thoracic spine most common (little epidural fat in cervical spine) Rapid deterioration with progression to radicular pain, then paralysis over 72-96 hrs Mortality rate 12% Must be kept in mind when investigating a patient for spinal infection or tumour
Treatment A medical & surgical emergency Requires rapid decompression - laminectomy (ventral abscesses require anterior approach)
Poor prognostic factors Rapidly progressing paralysis Complete paralysis Neurological deficits for >36 hrs Immunocompromised, DM, elderly
POST-OPERATIVE INFECTIONS Incidence 0.5% following discectomy 2% following fusion without instrumentation 5% following fusion with instrumentation Postop disciitis may be difficult to diagnose - keep in mind
106 Orthopaedi UI
Sholahuddin Rhatomy,MD
COMPARISON TABLE Osteomyelits Age Region Site Disc involvement ESR WBC Biopsy adult lumbar metaphysis yes high high + Discitis child lumbar end plate, disc yes high N TB any thoracic anterior body no high N + Tumour any lumbar posterior body no (except lymphoma & myeloma) normal N +
Spinal Metastases
Epidemiology Spine is most common site for skeletal metastases Most common tumours of spine Most common primaries: breast, lung, prostate, thyroid, kidney, lymphoma, myeloma >70% of patients who die from malignant disease have evidence of spinal mets & posterior elements are involved only 1/6 as often as vertebral body
Pathogenesis Spread to vertebral body 1st & later to pedicles Batson's venous plexus Spinal metastases can give rise to pain &/or neurological dysfunction Back pain Back pain nearly universal, however absence of back pain does not exclude malignant spinal cord compression Mechanism of back pain Tumour pain Direct tumour invasion of bone -> inflammatory effect & intraosseous hypertension Osteoclast activity, which is a host response to tumour invasion, is thought to be mediator of bone pain Mechanical pain Bony destruction can lead to progressive loss of mechanical stability allowing intravertebral micromotion Loss of rotational stability can occur due to loss of pedicular integrity Neurological dysfunction Mechanisms
107 Orthopaedi UI
Sholahuddin Rhatomy,MD
Direct epidural tumour compression Bony compression as a result of burst # Spinal instability -> vertebral collapse & increased kyphotic deformity at level of epidural compression Vascular accident to cord leading to ischaemia -> rapid onset of paralysis Paralysis at level of spinal cord more common than at level of cauda equina Lower capacity of canal Lower tolerance of upper motor neurons to compression Concept of spinal stability Ability of supporting structures of spine to allow for physiological loading so as to prevent pain & deformity An unstable spine is not necessarily one whereby movement or weight bearing will lead to a catastrophic collapse & paralysis In gross instability this may be true, but spine afflicted with malignancy generally develops a gradual loss of bony stability resulting in mechanical pain &/or rest pain which leads to impairment & diminished quality of life
Clinical
Red flags
History of cancer Recent unexplained weight loss Night pain Age >50
Investigation Most are osteolytic & not seen on plain X-rays until >30% destruction of vertebral body has occured MRI for extent of tumours & neurologic compromise CT-guided needle biopsy often possible & surgery for diagnosis avoided Skeletal survey or bone scan for other metastases
Management Multidisciplinary Mx including pain Mx, steroids, chemotherapy, radiation therapy & surgery
Patient selection & outcome measurement Pain
Wai et al Prospectively evaluated efficacy of surgery in patients with metastatic spinal disease with respect to quality of life Largest improvement to be in pain following surgery Neurological dysfunction Nather et al Evaluated factors which influence prognosis for neurological recovery due to extradural malignancy Good prognosis Incomplete paraplegia Intact sphincter control
108 Orthopaedi UI
Sholahuddin Rhatomy,MD
A long duration of neurologic deficit & a gradual onset of compression Strongest prognostic factor for post-Rx ambulation is pre-Rx neurological status; & most importantly, motor function Mx of instability a/w pain prior to neurological compromise is optimal time for surgery (if technically viable) Once a significant neurological event occurs, chance for recovery is limited but spinal instability may still need to be addressed Survival Improved patient survival after diagnosis of a primary malignancy, due to advances in chemotherapy, radiotherapy, & surgery, has meant that quality of remaining life is of great significance in Rx decisions Survival after surgical Mx of symptomatic spinal metastases Harrington -> 84% at 6/12, 77% at 1 yr, 51% at 2 yrs & 45% at 3 yrs Bauer -> 67% at 3/12 & only 23% at 1 yr Wise et al -> mean survival time of 15.9/12 Factors predicting survival after surgery for spinal metastases Primary cancer type Finkelstein et al Lung, melanoma, upper gastrointestinal tract - poorest survival with median of 87 days, 69.5 days & 56 days, respectively Intermediate survival with prostate (223 days) & breast (346 days) Longest median with lymphoma (706 days) & myeloma (591 days) Overall 1- & 3- month mortality rate of 9% & 29%, respectively Age Finkelstein et al -> for overall survival, each year of advancing age had a 1% increased risk of dying Preop neurological deficit Argenson et al -> patients with preop deficit had significantly lower mean survival at 1 & 3 yrs post-op Finkelstein et al Preop neurological deficit an independent determinant of a worse prognosis 19% more likely to die cf those without deficits Furthermore, 71% more likely to get postop infection, due to administration of preop radiation
Harrington Classification
I No neurological loss or bone involvement II Bone involvement without collapse or neurology III Neurological loss without significant bone involvement IV Vertebral collapse with mechanical back pain but no significant neurological loss V Collapse & neurological loss I & II: chemotherapy +/- radiotherapy III: radiation therapy & steroids IV & V: surgery Tokuhashi score (Spine, 1990) An index to predict survival after surgery for spinal metastases
109 Orthopaedi UI
Sholahuddin Rhatomy,MD
Designed for deciding between excisional or palliative procedures 6 clinical parameters General condition (Karnofsky index) Primary site of cancer Number of metastases in vertebral body Severity of spinal cord palsy Number of extraspinal bone metastases Metastases to major internal organs Score generated correlates to postop survival -> subsequently used in decision making for surgical intervention
Tomita et al (Spine, 2001)
A new surgical strategy for Rx of patients with spinal metastases Designed for deciding on various Rx ranging from wide or marginal excision to palliative Rx Scoring system consists of 3 prognostic factors Grade of malignancy Visceral metastases Bone metastases
1. 2. 3.
This strategy provides appropriate guidelines; however, final decision should be made by individual patient
Radiotherapy Effective for bone pain caused by direct tumour invasion in absence of mechanical instability Mode of action for pain relief by RT is based on direct tumour kill as well as having an antiinflammatory effect RT also effects local osteoclastic activity Bone regeneration can occur following RT & timely Rx can prevent development of mechanical instability Patients who recompress within previous RT field can be considered for reirradiation Risk of radiation myelitis is 1.9% & currently no evidence that any dose fractionation provides superior neurologic outcome
110 Orthopaedi UI
Sholahuddin Rhatomy,MD
Steroids High dose dexamethasone Shown to improve ambulation in malignant spinal cord compression Serious adverse effects
Surgery Indicated for progressive neurological deterioration or incapacitating pain due to mechanical
instability
Anticipated improvement in quality of life from surgery must outweigh risks Surgery may be a/w significant Cx due to immunosuppression, poor nutritional status & medical co-morbidities Considerations in decision making Life span of patient At least 3/12 General medical condition A non-surgical medical Cx will provide no improvement in overall quality of life in otherwise successful spinal procedure Age Each year of advancing age had a 1% increased risk of dying Cancer type Survival Preop embolisation may need to be considered in vascular tumours eg. renal cell carcinoma Number of spinal levels involved Surgical approach Stable instrumentation Radiation status Posterior thoracic surgery through an irradiated field has a significantly higher risk of wound dehiscence Postop radiotherapy should be delayed Surgical considerations Tumour location & level will affect choice of surgical approach Anterior procedures rarely appropriate at cranio-cervical or lumbo-sacral junctions Aside from these extremes, decompression for anterior disease can be achieved from either front or back of spine 85% of tumours are anterior, therefore, majority of decompression procedures should also be anterior as there is a positive correlation between location of extradural metastatic deposit & response to surgical Rx Anterior approach Direct anterior decompression & stabilisation from a transthoracic or retroperitoneal approach most appropriate for single level or occ. 2 level contiguous disease Anterior column support Can be achieved with iliac crest bone graft, cortical allograft, cage or methylmethacrylate Each with supplemental plate fixation for rotational stability Posterior approach
111 Orthopaedi UI
Sholahuddin Rhatomy,MD
Fusion Decision to fuse depends on life expectancy Iliac crest bone graft or bone graft substitutes may be used Postop irradiation should be delayed at least 3/52 allowing for skin healing & bone graft incorporation
Postero-lateral decompression followed by instrumentation provides good opportunity for decompression of anterior aspect of spinal cord & for posterior decompression & stabilisation of unstable spine Fixation factors, extent of disease & radiation status need to be considered as described above Stable instrumentation needs to be achieved, often spanning diseased segments
Percutaneous vertebroplasty 1st described in 1987 Alternative to open surgery for restoring stability to spine For osteoporotic #, complete relief of symptoms & restoration of mobility within 24 hr reported for 90% of patients In Rx of osteolytic bone metastases, results have been similarly encouraging PV may be applicable to patients with pain due to instability who may not be suitable for invasive spinal surgery due to medical co-morbidities, multilevel disease or having a profound neurological deficit Complications Cx rates: 1.3% in osteoporosis, 10% in metastatic disease Include cement entering nerve root foramen or spinal canal -> radiculopathy or spinal cord compression Systemic Cx include embolic events due to marrow fat, tumour fragments or cement entering circulation Extrusion of cement common, but most extrusions are minor & do not lead to neurological sequelae
Hypercalcaemia Serum Ca >2.55 mmol/L Determine if patient is symptomatic - bones, moans, stones & abdominal groans Pruritus Decreased QT interval -> arrhythmias CNS effects: confusion, stupor, lethargy, disorientation, weakness Constipation, anorexia, nausea & vomiting Polyuria, kidney stones Bony resorption +/- fibrous replacement of marrow (osteitis fibrosa cystica) Rx Hydration (saline diuresis) Loop diuretics Dialysis (for severe cases) Mobilization Specific drug therapy (biphosphonates, mithramycin, calcitonin, galium nitrate) Initial Mx Stop All thiazide diuretics - decrease Ca excretion
112 Orthopaedi UI
Sholahuddin Rhatomy,MD
Vit D & Ca supplements Hydration (saline diuresis) Correct volume depletion / expand extracellular volume NS 500 ml IV "wide open" (will dilute Ca/promote excretion) May require up to 4-10 liters of NS per day Establish diuresis >2500 ml/day Loop diuretics Lasix 20-40 mg IV q2-4 hr (will increase Ca excretion) Severe hypercalcemia Life-threatening hypercalcemia (>4.00 mmol/l or >16 mg/dl), unequivocally symptomatic, or both Consider dialysis Calcitonin Most rapid-acting osteoclast inhibitor becomes a first-line drug Given in single dose Pamidonate Much more potent bisphosphonate than etidronate Has also proved to be effective therapy for hypercalcemia Slow IV infusion of 15-45 mg daily for up to 6 days Mithramycin Inhibitor of RNA synthesis in osteoclasts IV 25 microg per kg over 4-6 hrs Serum Ca concentration begins to decrease as early as 12 hrs after administration& maximal reduction occurs in 48-72 hrs Toxic to kidney, liver, hematopoetic system
Psychosocial HyperCa Pain Tumour
TLC H2O, diuretics, biphosphonates Analgesia DXT Instability (IV & V) See instability DXT + steroids See instability Chemo +/- DXT DXT + steroids <3/12 TLC, analgesia, DXT >3/12 Surgery Excisional Palliative Percutaneous vertebroplasty
Neurology
Tumour (III) Instability (IV)
Instability
I & II III IV Assess prognosis & V Age Primary cancer Preop neurology General condition
113 Orthopaedi UI
Sholahuddin Rhatomy,MD
Practise points When considering surgery for metastatic spine disease life span of patient, general medical condition, number of spinal levels involved, age, cancer type & radiation status must be considered Outcomes following surgery should be measured using a global functional outcome scale which takes into account physical, social & psychological domains Surgery in a carefully selected patient population can improve overall quality of life Greatest improvement is with pain relief Neurological improvement has a poorer response to surgery
114 Orthopaedi UI
Sholahuddin Rhatomy,MD
Idiopathic Scoliosis
Definition : Three-dimensional deformity of the spine with lateral curvature plus rotation of the vertebral bodies , sagital coronal and axial The criteria of Cobb > 10 Classification Scoliosis : 1.Non structural scoliosis(reversible,norotation) ~ habitual poor posture ~ pain and muscle spasm ~ lower limb length discrepancy 2.Structural scoliosis(irreversible,rotate ~ idiopat ~ osteopathic ~ neuropathi ~ myopathic
o
4 Types Idiopathic Scoliosis Infantile ( 0 3 y) Juvenile (3 10 y) Adolescence ( 10 -19 y) Adult (> 19 y)
Infantile type : - the onset from birth to 3 years old - etiology : post natal pressure - more common in boys - usually left thoracic scoliosis
Juvenile type : - the onset between 4 and 9 years old - more common in girls
adolescent type :
115 Orthopaedi UI
Sholahuddin Rhatomy,MD
- the most common type - the onset between 10 years old and the end of growth - more common in girls - common pattern : right thoracic scoliosis
Etiology (dari kuliah prof SS) GENETICS TWIN STUDIES FIRST DEGREE RELATIVES- 11 % AFFECTED SEARCH FOR RESPONSIBLE GENES TISSUE DEFICIENCIES BONE - OSTEOPENIA MUSCLE - CALCIUM METABOLISM LIGAMENT/DISCAnatomy VERTEBRAL GROWTH ABNORMALITIES IV. PROGRESSION RELATED TO GROWTH FASTER ANTERIOR GROWTH HYPOKYPOSISS -ROTATIONAL BUCKLING OF SPINE AIS PATIENTS TALLER THAN PIERS INCREASED GROWTH HORMONE (PETERNEWTON SANDIEGO
CNS THEORIES MANY NEUROMUSCULAR CONDITION SYRINX ASSOCIATED WITH SCOLIOSIS MELATONIN DEFICIENCY PINEALECTOMIZED CHICKENS
Physiology Human erect physiologic curvature cervical lordosis, thoraxic kyphosis, lumbar lordosis coronal plain Straight Scoliosis curvature coronal plane and sagital plane most hypokhypotic
Prevalence & Natural History
116 Orthopaedi UI
Sholahuddin Rhatomy,MD
>30 CURVE: 1-3/1000, M : F = 1 : 8 CURVE PROGRESSION IN ADULTHOOD RARE IF < 30O COMMON IF >50-75 THORACIC >30-40 LUMBAR 1 /YEAR
0 0
BACK PAIN HIGHER RATE THAN CONTROLS Curve > 10 0,5 3 % children & adolescent Curve > 30 1,5 3 % per 1000
o o
Risk Factor for Progression Sex ; female : menses determine the growth spurt. Within 12 mo after menses Skeletal growth Risser 1or less, prog 60 70 % Risser 3 reduce to 10%
Curve Location, Apex T12/above > progress than isolated lumbar curve Curve magnitude greater curve, more progress
Evaluation of the Patient History : Development of milestone Growth history medical History
Physical examination : LOOK-FEEL-MOVE WALKING, STANDING (BACK, SIDE, FRONT), FORWARD BENDING, FLEXIBILITY, NEUROLOGICAL EXAMINATION Standing in straight and flexedtrunk & spine Look any asymetri; neck , shoulder, ribs, waist and hips
117 Orthopaedi UI
Sholahuddin Rhatomy,MD
Trunk Balance : Plumb line Shoulder Asymetri Body Arm Distance Adam forward bend test Scoliometry not correlate with cobb angle Scoliosis Leg length discrepancy use a block to eliminate or forward bend in seated position Lateral bending Find any laxity Look for hyperkyfosis
Radiographic At least from T1 L5 should be seen clearly Standing PA / Lateral Supine Force side bending R & L Pelvic AP If cobb > 100 defree STAGNARA VIEW (measure true angle degree of deformity) SIDE BENDING, FULCRUM BENDING ( to predict maximal correction after treatment) MRI : AGE < 10, LEFT THORACIC, NEUROLOGICAL FINDINGS
Assessed : 1. End vertebra 2. Apical 3. Curve location 4. Curve direction 5. Curve magnitude 6. Risser sign 7. Structural curve
118 Orthopaedi UI
Sholahuddin Rhatomy,MD
8. Nonstructural curve 9. Major curve 10. Minor curve 11. Rotation
End Vertebra : The top and bottom vertebrae that tilt maximally into concavity of the curve, they are typically least rotated, least horizontally displaced vertebra within a curve Apical vertebra : the central vertebra within the curve its typically the least tilted, most rotated, and most horizontally displaced
-. Curve location: curve location its defined by its apex Curve CervicoThoraxic Thoraxic Thoracolumbal Lumbar Lumbosacral Apex C7 T1 T2 T11 T12 L1 L2 L4 L5 S1
Curve Direction : it was determined by the side of convexity, curve convex toward to the right are termed right curve Curve magnitude : using cobb lippman technique : the angle formed by the intersection of the two line that are drawn across the superior end plate of the upper end most tilted vertebra and the inferior endplate of the lower end vertebra Curve magnitude : using cobb lippman technique Risser sign : 0 : absent 1 : 0-25 % 2 : 25 50 %
119 Orthopaedi UI
Sholahuddin Rhatomy,MD
3 : 51 75 % 4 : 76 100% 5 : fusion of epiphysis to the ileum
4 : correlate with the end of spinal growth 5 : correlate with the end of height increase
Non Structural Curve : curve that correct completely when patient bend toward the convexity of the curve Structural Curve : curve that do not correct completely when patient bend toward the convexity of the curve Vertebral Rotation Nash and Moe : If the pedicles are equidistant from the sides of the vertebral bodies, no vertebral rotation is present (0 rotation). The grades progress up to grade IV rotation, in which the pedicle is past the center of the vertebral body ( From Nash CL Jr, Moe JH: J Bone Joint Surg 51A:223, 1969)
Plumb line C7 sagittal plumb line is useful measurement of sagittal balance. Plumb line dropped from middle of C7 vertebral body falls close to posterosuperior corner of S1 vertebral body
120 Orthopaedi UI
Sholahuddin Rhatomy,MD
Classification The purpose : Categorizing similar type of curve pattern Communication tool A tool for comparing various report A tool of helping select surgical treatment
Kings classification of the scoliotic curve: * I : Primary lumbar,secondary thoracic * II : Primary thoracic,secondary lumbar * III : Thoracic without structural lumbar * IV : long thoracic curve extending to L4 * V : double thoracic curve with T1 tilting into the upper curve
Lenke Classification More Comprehensive To select level should be fused
121 Orthopaedi UI
Sholahuddin Rhatomy,MD
Curve classification triad 1. Curve type ( 1 through 6) 2. Lumbar spine modifier ( A,B, or C ) 3. Sagittal thoracic modifier ( -,N,+ )
Each of three components should be identified separately and combine to complete classification
Curve Type Type Proximal Thoraxic Main Thoraxic Thoracolumbar/Lumbar Curve Type
NS
S (Mayor)
NS
Main Thoraxic
S (Mayor)
NS
Double Thoraxic
NS
S (Mayor)
Double mayor
S (Mayor)
Triple mayor
NS
NS
S (Mayor)
TL/L
NS Structural Curve
S (Mayor)
TL/L / Main Thoraxic
PT : Side bending Cobb, Coronal > 25 , Sagital / Kyphosis > 20 (T2 T5) MT : Side bending Cobb Coronal, Coronal > 25 , Sagital / Kyphosis > 20 (T10 L2) TL/L : Side bending Cobb, Coronal > 25 , Sagital / Kyphosis > 20 (T10 L2)
o o o o
Lumbar Spine Modifier A : Central Sacral Vertical Line between pedicle B : Central Sacral Vertical Line touches apical bodies C : Central Sacral Vertical Line completely medial
122 Orthopaedi UI
Sholahuddin Rhatomy,MD
Thoraxic Sagital Profile - : Hypokifosis < 10
o
N : Normal 10 40o + : Hyperkifosis > 40
o
Treatment Goal : To prevent progression Correction trunkal Balance Improve quality of live Safe correction
123 Orthopaedi UI
Sholahuddin Rhatomy,MD
Treatment options (Three O): Observation & re-evaluate Orthoses Operation
Non Operative : Observation : < 25 Immature < 50 Mature
o o o o o o
Ro 3 mo after first visit, then 6 mo for < 20 & 4 6 mo for > 20 significant change : progression > 10 for curve < 20 and
o o
progression > 5 for curve > 20
Orthosis Curve 30 40
o
Milwaukee (CTLSO) for apex above T8 Boston (TLSO) up to T8 apex Must be wear 23 hours until 2 years after menarch / risser 4 and wean off in year
Operative treatment The indications : Progressive Curve > 40 45 in growing Children Failure of bracing Progressive Curve beyond 50 o in adult
o
Cottrell Gambar
124 Orthopaedi UI
Sholahuddin Rhatomy,MD
Kalo dilakukan anterion release : 2 minggu sebelum dan sesudah op dilakukan cotrell
Tanpa anterior release 3 bulan pre operasi minimal 3 jam perhari Control tiap 3 minggu Untuk menambah mobilitas saat operasi dilakukan costektomy dan fascetectomy
Perkembangan instrumentasi 1. Harrington Rod di concave side, compression convex side ,. Implant memegang atas dan bawah saja, di fascet superior dan inferior saja. Kompresi di prosessus tranversus. oleh paul Harrington 1960, komplikasi iskemi.ischemic time 3 jam. Di Indonesia 1977 prof SS 2. Dwyre instrumentation (Australian, alan Frederick dwyre, mattress hospital 1974). Shortening not distraction..approach anterior Di Indonesia 1979 3. Luque instrumentation (mexico. Edward luque, 1981, Stamford university)SSI (segmental spinal instrumentation)..tiap segmen diikat dg wire 4. Rectangle (john dove dari RS harsil) modifikasi dari luque..dengan alat calverstein (nama kota) untuk instabilisasi daerah lumbosakral - luque : kawat dibentuk seperti tangga ..double C - calverstein kawat di bentuk curve 5. chicken wire ..wire pada base spinosus ( pertama di singapura),. Karena takut memasang di sublaminar 6. Cottrell duboisset dapat melakukan rotasi selain koreksi 2 dimensi. Alat ini merajai selama 10 th di temukan oleh : is cotrell dari lyon dan dubboiset orthopaed dari paris.dasarnya claw (modifikasi dari hook), superior di fascet dan tranversus inferior di lamina Dari penelitian koreksinya postoperasi dinilai dengan CT scan derotasinya < 10 derajat 7. kombinasi pedicle screw ISOLA (nama kupu-kupu, modifikasi dari CD) .prof lec bartnel. Memakai hook dan screw di L3, claw diatas dan di bawah wire di tengah(songen wire).bisa memutar kemiringan L3 8. full pedicle screw .pioneer : tse ill tsuk dan lenke : periapical translasi Derotasi : periapical translasi : memutar sumbunya di luar implant..mengubah skoliosis menjadi kiposis Translasi sumbunya di tiap vertebra Inserting :
125 Orthopaedi UI
Sholahuddin Rhatomy,MD
1. Roy cammille : langsung lurus , tidak perlu sampai ke korpus 2. magerl : harus ke korpus,1mm medial dan 1 mm chepalad to the center Direct apical translasi oleh lenke ; rotasi langsung pada apeknya
Tuberculosis of the Spine (prof SS)
List of Problem : Infection Poor General Condition Multiple Lesions Cold Abscess Pain Pathologic fracture Instability Neurological Deficit Deformity Kyphus Progression by Growth Socio Economic Psychogenic
Total Treatment : treating TB spondylitis not only the infection but all the existing problems with all methods as required Treatment List : Basic Treatment : anti Tb, drugs, supportive tx, body cast/brace, bed rest Abscess Drainage Costo Transversectomy Thoracoscopic Debridement Anterior Debridement + Fusion ( HongKong Method )
126 Orthopaedi UI
Sholahuddin Rhatomy,MD
Anterior Instrumentation Posterior Instrumentation Transpedicular Debridement & Biopsy Transforaminal Posterior LIF Shortening Procedure Circumferential Decompression Rehabilitation
Steps of Total Treatment Step 1: Step 2: Step 3: treatment Step 4: identify and clarify the existing problems list of all treatment modalities conservative to the most aggressive individual patients : match list of problems to the suitable types of the matching give ten treatment choices or ten alternatives
Step 5: discuss Tx. choice with patient and family explain risks, prognosis, costs of the procedureinformed consent
Aim of Treatment Healing of TB Spondylitis in a stable and painless spine without unacceptable deformity with return of function, return to the society, family and occupation Heal of TB 1. Clinical : increase body weight, accebtable deformity 2. lab : ESR and CRP Normal 3. Radiology : kirkaldy willis criteria (Canadian) : bony ankilosis > callus formation across healthy spine above and below Total Treatment Options
1. Non Operative 2. Decompression of a large abscess 3. Anterior debridement and fusion
127 Orthopaedi UI
Sholahuddin Rhatomy,MD
4. Posterior instrumentation and anterior debridement and fusion (HK method) 5. Posterior shortening and instrumentation and anterior debridement & fusion 6. Posterior only : shortening procedure, transpedicular biopsy, costotransversectomy instrumentation for thorocic spine, kyphosis < 75
0
7. Posterior only : shortening procedure debridement PLIF or TLIF, instrumentation for lumbar spine less than 90
0 0
8. Posterior only kyphosis 75 - 89 - Shortening procedure - Costotransversectomy
- Circumferential decompression - Posterior instrumentation . Poterior only kyphosis > 900 : (Non Distraction) - Shortening procedure - Costo transversectomy - Circumferential decompression - Posterior instrumentation & fusion 10. Posterior with or without anterior debridement and fusion : (Distraction) - Shortening procedure - Costo transversectomy - Circumferential decompression with osteotomy all the way to anterior L.L.
- Pedicle screw instrumentation with immediate correction and distraction to give room for the dura & cord (no kinking due to the shortening)
Conclusion : Total treatment is the most acceptable, comprehensive, rational and problem solving approach to the management of tuberculosis of the spine CURRENT TREATMENT
128 Orthopaedi UI
Sholahuddin Rhatomy,MD
History Tx TB in Indonesia
1. before anti TB era Px treat at sanatorium at least 2 years with good air, food and rest (dutch period) Cisarua RS Fatmawati 1930 direktur Bp sunyoto Triple drugs Streptomysin, INH and PAS Project HOPE (USA mission commando from hope ship basis, project from Eisenhower 1960) 2. anti TB era a. MRC / medical research council . report I form lyod Griffith (internist) in Rhodesia (gulawayo and madras) conclusion : TB spine is medical case Fatmawati > indication of operation is paraplegia, 1954 prof sukaryo do costotranversectomy to drainage abscess (learn from boston hospital (prof biakto) Reason of operation are > because of medical / body cast tx : No radiological healing Gibbus pain + Just fibrous heal and clinical heal
b. MRC report II (hongkong) by myo salmoon TB spine can operate if 2 level spine and paraplegia 1934 1 operation Ito suchia (jepang) 1954 ischii and condo do 1 operation with hongkong method c. 1956 hodgson and stock develop HM (radical anterior debridement and strut graft) JBJS 1956 popularize by Arthur yau (queen marry hospital hongkong) then he lecture around the world d. Radjsekaran report 15% failure of hongkong method due to : slip of gruft, graft resorption / lysis, tricortical graft > ribs.children with fibula..fusion Cuma 16% yang lain fibrous fusion e. 1969 roland beaton campaign TB spine is surgical cast 3. Instrumentation Era 1971 APOA Spine section kongres di tokyo: New sam moon report used Harrington rod
st st
Indonesia : 1. 1969 prof soelarto 1 do HM + ronald Betham 2. 1989 Prof SS : start Total treatment caused failure of HM high and many problem in TB Spine
st
129 Orthopaedi UI
Sholahuddin Rhatomy,MD
Advantage HM 1. totally evacuate of infection until leave bleeding ( fascilitate to antibiotic0 2. eliminate paraplegia 3. confirm Dx 4. mengurangi lama perawatan Disadvantage HM 1. unstable sehingga perlu eksternal support 6 bulan 2. progression of deformity 3. cannot correct severe kyphosis
Fusion di spine oleh Hip and aldy 1911 (posterior fusion) Paraplegia : Mekanik (abscess, deformity, sequester) Vaskuler ( thrombosis by seddon) Meningomyelocele
Pengambilan PA saat operasi ; Anterior (open , endoscopic) Foraminotomy Transpedicel Costotransversectomy
Konservatif pada TB bisa pada kasus yang mengenai 1-2 level saja. Khususnya TB dari discus (myosam moon)
130 Orthopaedi UI
Potrebbero piacerti anche
- Dissector Answers - Deep Back & Spinal CordDocumento9 pagineDissector Answers - Deep Back & Spinal CordUloko ChristopherNessuna valutazione finora
- Spinal Anatomy & Surgical ApproachesDocumento37 pagineSpinal Anatomy & Surgical Approachestachyonemc2Nessuna valutazione finora
- Spinal CordDocumento59 pagineSpinal Cordveegeer100% (1)
- Neuraxial Blockade Anatomy and LandmarksDocumento10 pagineNeuraxial Blockade Anatomy and LandmarksSedaka DonaldsonNessuna valutazione finora
- Kuliah Spine TraumaDocumento91 pagineKuliah Spine TraumaEvi MaisyariNessuna valutazione finora
- Kuliah Spine TraumaDocumento91 pagineKuliah Spine Traumatutor tujuhNessuna valutazione finora
- Chapter 5 Spinal CordDocumento87 pagineChapter 5 Spinal CordOsman abdilahi nuurNessuna valutazione finora
- Anatomy and Pathology of The Achilles Tendon Tracy MacNairDocumento48 pagineAnatomy and Pathology of The Achilles Tendon Tracy MacNairHusna NadiaNessuna valutazione finora
- Hip Joint Feb 2023Documento66 pagineHip Joint Feb 2023sagarmandal1595Nessuna valutazione finora
- Thoracic Wall 01Documento22 pagineThoracic Wall 01Dr. Saber Ar RaffiNessuna valutazione finora
- SPINAL NERVE Presentation Completed-2Documento51 pagineSPINAL NERVE Presentation Completed-2Sheikh Muhammad MuhallilNessuna valutazione finora
- Cross Sectional Anatomy of SpineDocumento37 pagineCross Sectional Anatomy of SpineAvinash Gupta50% (2)
- The Spinal Cord: Lec-11-Dr - Maysoon AlkazzazDocumento12 pagineThe Spinal Cord: Lec-11-Dr - Maysoon AlkazzazRose ParisNessuna valutazione finora
- Neuraxial AnaesthesiaDocumento12 pagineNeuraxial Anaesthesiakl;kzNessuna valutazione finora
- Week 2 Study Quide Q ADocumento6 pagineWeek 2 Study Quide Q Aapi-479716004Nessuna valutazione finora
- Anatomy and Localization of Spinal Cord DisordersDocumento23 pagineAnatomy and Localization of Spinal Cord DisordersMichael RojasNessuna valutazione finora
- The Spinal Cord,, and Blood Supply To The BrainDocumento78 pagineThe Spinal Cord,, and Blood Supply To The BrainMartha MulusaNessuna valutazione finora
- لقطة شاشة ٢٠٢٣-١٠-٢٨ في ٦.٢٩.٥٩ صDocumento115 pagineلقطة شاشة ٢٠٢٣-١٠-٢٨ في ٦.٢٩.٥٩ صhNessuna valutazione finora
- Lecture 12 Skeletal System Lower Limb (Surface Anatomy)Documento29 pagineLecture 12 Skeletal System Lower Limb (Surface Anatomy)hafiz patahNessuna valutazione finora
- Biomechanical of The SpineDocumento38 pagineBiomechanical of The SpinePap PipNessuna valutazione finora
- Anatomia Da ColunaDocumento59 pagineAnatomia Da ColunaPaula Duarte MarquesNessuna valutazione finora
- Anatomy Revision - Upper LimbDocumento7 pagineAnatomy Revision - Upper LimbroyalvirenNessuna valutazione finora
- Anatomy ReviewDocumento283 pagineAnatomy ReviewmmbrewNessuna valutazione finora
- 5.spinal CordDocumento62 pagine5.spinal CordNishanth LakshmanNessuna valutazione finora
- Spinal Cord InjuriesDocumento31 pagineSpinal Cord Injuriesmariam bassemNessuna valutazione finora
- Cervical AnatomyDocumento41 pagineCervical AnatomythwisemanNessuna valutazione finora
- Spinal Anesthesia - Technique - UpToDateDocumento37 pagineSpinal Anesthesia - Technique - UpToDateSamir Perez CasadiegoNessuna valutazione finora
- Pelvic FractureDocumento22 paginePelvic FractureAgeng BudianantiNessuna valutazione finora
- Human Anatomy & Physiology: Spinal Cord, Spinal Nerves and Somatic ReflexesDocumento41 pagineHuman Anatomy & Physiology: Spinal Cord, Spinal Nerves and Somatic ReflexesSyarif MaulanaNessuna valutazione finora
- Spinal Cord InjuryDocumento37 pagineSpinal Cord Injurylim sjNessuna valutazione finora
- Atlas and AxisDocumento26 pagineAtlas and AxisJane BurtonNessuna valutazione finora
- Chapter 1-Musculoskeletal SystemDocumento113 pagineChapter 1-Musculoskeletal SystemWang Ming YaNessuna valutazione finora
- Membrul Superior MGDocumento118 pagineMembrul Superior MGMihai OpreaNessuna valutazione finora
- Thoracic Segment KpsDocumento77 pagineThoracic Segment Kpskrishna bptNessuna valutazione finora
- Spinal CordDocumento31 pagineSpinal CordMercy DakaNessuna valutazione finora
- Anatomy of Thoracic WallDocumento27 pagineAnatomy of Thoracic WallSamuel Pola Karta Sembiring100% (1)
- Positioning Presentation-VertebraeDocumento156 paginePositioning Presentation-Vertebraeron reteracionNessuna valutazione finora
- Functional Organization & StructureDocumento78 pagineFunctional Organization & StructureNilay PatelNessuna valutazione finora
- The Shoulder Anatomy & Approaches: Abdulaziz F. Ahmed, MBBS PGY-2Documento61 pagineThe Shoulder Anatomy & Approaches: Abdulaziz F. Ahmed, MBBS PGY-2Abdulaziz Al-Akhras100% (1)
- Muscles of The Thoracic Wall, Pectoral Region - 2023 - 1Documento28 pagineMuscles of The Thoracic Wall, Pectoral Region - 2023 - 1202112360Nessuna valutazione finora
- Anatomy Midterm Study GuideDocumento53 pagineAnatomy Midterm Study Guidelovelyc95Nessuna valutazione finora
- Regional AnesthesiaDocumento209 pagineRegional AnesthesiaNatnael ZelalemNessuna valutazione finora
- Spinal Injury1Documento37 pagineSpinal Injury1Selam Tesfaye ShebaNessuna valutazione finora
- Joints of The Lower LimbDocumento63 pagineJoints of The Lower LimbEliud MbuteNessuna valutazione finora
- Cervical DisordersDocumento89 pagineCervical DisordersAbdallah Samir Mostafa٢٠١٩٠٢١٥٩Nessuna valutazione finora
- Anatomy - Pectoral Region and Axilla PDFDocumento4 pagineAnatomy - Pectoral Region and Axilla PDFAngel KimNessuna valutazione finora
- The Anatomy of The Pelvis: Structures Important To The Pelvic Surgeon Workshop 45 Tuesday 24 August 2010, 14:00 - 18:00Documento29 pagineThe Anatomy of The Pelvis: Structures Important To The Pelvic Surgeon Workshop 45 Tuesday 24 August 2010, 14:00 - 18:00Kumah WisdomNessuna valutazione finora
- Hafizah Binti Mohd Hoshni Musculoskeletal Anatomy Skeleton of The ThoraxDocumento28 pagineHafizah Binti Mohd Hoshni Musculoskeletal Anatomy Skeleton of The ThoraxhafizahhoshniNessuna valutazione finora
- Trauma Spinal Wates Dr. WRDocumento68 pagineTrauma Spinal Wates Dr. WRLanlan LesmanaNessuna valutazione finora
- Whiplash Certification CDocumento229 pagineWhiplash Certification CPedro M. BorgesNessuna valutazione finora
- Anatomy of Vertebral CoulmnDocumento30 pagineAnatomy of Vertebral Coulmnsanullah123khan.13Nessuna valutazione finora
- Safe and Logical Radiography of L.S. SpineDocumento39 pagineSafe and Logical Radiography of L.S. SpineSujeet ChandNessuna valutazione finora
- Knee UltrasoundDocumento6 pagineKnee UltrasoundAndrei GianinaNessuna valutazione finora
- Radiology of The SpineDocumento50 pagineRadiology of The SpineAsem AlhazmiNessuna valutazione finora
- Spinal CordDocumento65 pagineSpinal CordDr. Vinod Gupta100% (1)
- Beka Aroshidze 2017Documento48 pagineBeka Aroshidze 2017Rupesh M DasNessuna valutazione finora
- Dams 1Documento76 pagineDams 1jmohideenkadharNessuna valutazione finora
- Os Complete Final AnswerDocumento198 pagineOs Complete Final AnswerDeshini Balasubramaniam100% (4)
- Brachial Plexus InjuriesDocumento46 pagineBrachial Plexus Injuriesnams orthoNessuna valutazione finora
- T Shirt DesignDocumento1 paginaT Shirt DesignlikusajaNessuna valutazione finora
- The Neurological Examination PDFDocumento7 pagineThe Neurological Examination PDFIu Ha SimNessuna valutazione finora
- Language TestingDocumento2 pagineLanguage TestinglikusajaNessuna valutazione finora
- Anging Mamiri in EnglishDocumento1 paginaAnging Mamiri in EnglishlikusajaNessuna valutazione finora
- Go Tell It On The MountainDocumento12 pagineGo Tell It On The MountainlikusajaNessuna valutazione finora
- Proposal by UchicikDocumento15 pagineProposal by UchiciklikusajaNessuna valutazione finora
- Koran Bedah Plastik, Senin 02 JUNI 2014: Unit Luka Bakar No Bed Nama Diagnosis Terapi Hasil Lab Lab 01-06-2014Documento6 pagineKoran Bedah Plastik, Senin 02 JUNI 2014: Unit Luka Bakar No Bed Nama Diagnosis Terapi Hasil Lab Lab 01-06-2014likusajaNessuna valutazione finora
- Jurnal UkuDocumento3 pagineJurnal UkulikusajaNessuna valutazione finora
- DASSDocumento2 pagineDASSNeelam Zafar100% (1)
- T Shirt DesignDocumento1 paginaT Shirt DesignlikusajaNessuna valutazione finora
- Bca CoverDocumento1 paginaBca CoverlikusajaNessuna valutazione finora
- Osteo Kon Drom A TobanDocumento4 pagineOsteo Kon Drom A TobanlikusajaNessuna valutazione finora
- Ats Program at Glance PDFDocumento2 pagineAts Program at Glance PDFlikusajaNessuna valutazione finora
- Koran Fix Rabu BP 3614Documento1 paginaKoran Fix Rabu BP 3614likusajaNessuna valutazione finora
- SBDFJKDocumento6 pagineSBDFJKlikusajaNessuna valutazione finora
- Incidence and Predictors of Difficult Nasotracheal Intubation With Airway ScopeDocumento5 pagineIncidence and Predictors of Difficult Nasotracheal Intubation With Airway ScopelikusajaNessuna valutazione finora
- Neuropathic PainDocumento13 pagineNeuropathic PainEdward ValenciaNessuna valutazione finora
- SBDFJKDocumento6 pagineSBDFJKlikusajaNessuna valutazione finora
- Clubfoot - Ponseti Management. Editor Lynn Stahelli (2003)Documento32 pagineClubfoot - Ponseti Management. Editor Lynn Stahelli (2003)amalia_utami_1Nessuna valutazione finora
- 4 - Crystal adsfdsbadsgSDJBJSdDeposition DisordersDocumento7 pagine4 - Crystal adsfdsbadsgSDJBJSdDeposition DisorderslikusajaNessuna valutazione finora
- MK Giz Slide Malnutrisi Energi ProteinDocumento88 pagineMK Giz Slide Malnutrisi Energi ProteinlikusajaNessuna valutazione finora
- Osteo Kon Drom A TobanDocumento4 pagineOsteo Kon Drom A TobanlikusajaNessuna valutazione finora
- National Geographic - May (2010) (Malestrom)Documento81 pagineNational Geographic - May (2010) (Malestrom)GNessuna valutazione finora
- Zebra Puzzle GuideDocumento3 pagineZebra Puzzle GuideLightFinderNessuna valutazione finora
- A Dark Brown Dog by Stephen CraneDocumento13 pagineA Dark Brown Dog by Stephen CraneDayangFauziah Bt AwangAhetNessuna valutazione finora
- Fairy TaleDocumento7 pagineFairy TaleMiguel Lugia-ZengNessuna valutazione finora
- Student WorkDocumento7 pagineStudent Workapi-316130138Nessuna valutazione finora
- Annotatedbib2 DebockDocumento2 pagineAnnotatedbib2 Debockapi-282281003Nessuna valutazione finora
- Listening - Compare Animal and Human Behavior 2 - Mode - Report - Unit 6 - Lesson 3 - Vantage B2 - MyEnglishLabDocumento1 paginaListening - Compare Animal and Human Behavior 2 - Mode - Report - Unit 6 - Lesson 3 - Vantage B2 - MyEnglishLabAnnuar Florez100% (1)
- Slideshow 3rd Grade Species - Western BluebirdDocumento24 pagineSlideshow 3rd Grade Species - Western Bluebirdapi-553036288Nessuna valutazione finora
- Reading Comprehension For Grade 3 PDFDocumento6 pagineReading Comprehension For Grade 3 PDFIVAN CONRADNessuna valutazione finora
- Unisystem PiratesDocumento8 pagineUnisystem PiratesAnime300100% (1)
- CASE PRE (Intrapartum)Documento6 pagineCASE PRE (Intrapartum)teuuuuNessuna valutazione finora
- Black Caviar Blog 10Documento2 pagineBlack Caviar Blog 10bruce6526Nessuna valutazione finora
- Popcorn Lamb Amigurumi Crochet PDF Free PatternDocumento7 paginePopcorn Lamb Amigurumi Crochet PDF Free Patternami arinta100% (1)
- Animal Diversity 7th Edition Hickman Test Bank 1Documento9 pagineAnimal Diversity 7th Edition Hickman Test Bank 1gregoryNessuna valutazione finora
- Esthetic Rehabilitation of A Severely Worn Dentition With MIPPDocumento22 pagineEsthetic Rehabilitation of A Severely Worn Dentition With MIPPKarla Margine PérezNessuna valutazione finora
- Practice 02Documento5 paginePractice 02Binh MinhNessuna valutazione finora
- The Mystery of Metamorphosis - Foreword by Lynn Margulis and Dorion SaganDocumento5 pagineThe Mystery of Metamorphosis - Foreword by Lynn Margulis and Dorion SaganChelsea Green Publishing100% (1)
- Military Working Dog ProgramDocumento155 pagineMilitary Working Dog Programjojo2486100% (3)
- Fresco Slouchy HatDocumento2 pagineFresco Slouchy HatClaudia CatanaNessuna valutazione finora
- Pulpal Reactions To Caries and Dental ProceduresDocumento58 paginePulpal Reactions To Caries and Dental ProceduresSony RajbhandariNessuna valutazione finora
- Wet & Wild by David EllisDocumento83 pagineWet & Wild by David EllisAustin Macauley Publishers Ltd.Nessuna valutazione finora
- Algeria Country PaperDocumento9 pagineAlgeria Country PaperSandeep MahantaNessuna valutazione finora
- List of Yarn Manufacturing Member Mills of BTMADocumento26 pagineList of Yarn Manufacturing Member Mills of BTMAMd. Monowarul IslamNessuna valutazione finora
- About Us: Vaccination AND Deworming ProgramDocumento1 paginaAbout Us: Vaccination AND Deworming ProgramTolitzjr CatayloNessuna valutazione finora
- Laxative and Purgative HerbsDocumento2 pagineLaxative and Purgative HerbsqueencelNessuna valutazione finora
- Association Between Caesarean Delivery and Isolated Doses of Formula Feeding in Cow Milk AllergyDocumento6 pagineAssociation Between Caesarean Delivery and Isolated Doses of Formula Feeding in Cow Milk Allergyirene aureliaNessuna valutazione finora
- Generic Dungeon WOTCDocumento9 pagineGeneric Dungeon WOTCMark YfjNessuna valutazione finora
- The Nail and Its StructureDocumento22 pagineThe Nail and Its StructureHarlene OzarNessuna valutazione finora
- Cho Han HuDocumento42 pagineCho Han HuprasanthNessuna valutazione finora
- Cunning Linguists Oral Sex in The Song of SongsDocumento16 pagineCunning Linguists Oral Sex in The Song of SongsMisael Vargas100% (2)