Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Rhizoma Extracts On Methicillin-Resistant Staphylococcus Aureus
Caricato da
Juan Favela HernandezDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Rhizoma Extracts On Methicillin-Resistant Staphylococcus Aureus
Caricato da
Juan Favela HernandezCopyright:
Formati disponibili
African Journal of Biotechnology Vol. 11(47), pp. 10799-10803, 12 June, 2012 Available online at http://www.academicjournals.org/AJB DOI: 10.5897/AJB11.
3471 ISSN 1684-5315 2012 Academic Journals
Full Length Research Paper
Antibacterial and synergistic effects of Nardostachytis rhizoma extracts on methicillin-resistant Staphylococcus aureus
Dae-Ki Joung1, Young-Hwa Kim1, Kyung-Hee Lee1, Dong-Yeul Kwon2, Jang-Gi Choi2, Dong-Soo Ha3, Dong-Young Shin1, Kee-Tae kweon4 and Dong-Won Shin1*
Department of Oriental Medicine Resources, College of Bio Industry Science, Sunchon National University, Sunchon Jeonnam 540-742, Republic of Korea. 2 Department of Oriental Pharmacy, College of Pharmacy, Wonkwang Oriental Medicines Research Institute, Wonkwang University, Jeonbuk 570-749, Republic of Korea. 3 Department of Chemistry Education, College of Education, Sunchon National University, Sunchon Jeonnam 540-742, Republic of Korea. 4 Ministry of Health and Welfare Office for Healthcare Policy Division of Traditional Korean Medicine Industry, 75 Yulgong-ro, Jongro-gu, Seoul 110-793, Korea.
Accepted 4 June, 2012
1
Methicillin-resistant Staphylococcus aureus (MRSA) is a serious clinical problem worldwide. Few new drugs are available against MRSA, because it has the ability to acquire resistance to most antibiotics which consequently increases the cost of medication. In the present study, the antibacterial activity of Nardostachytis rhizoma was investigated. The most effective method is to develop antibiotics from the natural products without having any toxic or side effects. Therefore, there is a need to develop alternative antimicrobial drugs for the treatment of infectious diseases. The use of two drugs in combination is a good alternative to slow the process of developing drug resistance and to restore the effectiveness of drugs that are no longer prescribed. Combination therapy is the most commonly recommended empirical treatment for bacterial infections in intensive care units, where monotherapy may not be effective against all potential pathogens, and for preventing the emergence of resistant. Five clinical isolates (MRSA) were obtained from five different patients at Wonkwang University Hospital (Iksan, South Korea). The other two strains were S. aureus ATCC 33591 (methicillin-resistant strain) and S. aureus ATCC 25923 (methicillin-susceptible strain). Antibacterial activity (minimal inhibitory concentrations, MICs) was determined by broth dilution method, disc diffusion method, MTT test and checkerboard dilution test. Antimicrobial activity of n-hexane fraction of N. rhizoma was significant. Against the seven strains, the disc diffusion test was in the range of 14 to 18 mm and had a MICs ranging from 31.25 to 125 g/ml. FICI values for n-hexane fraction (HFL) of N. rhizome + ampicillin (AM) and HFL + oxacillin (OX) were 0.1875 and 0.078125-0.09375, showing the increase of synergistic effect. When combined together, these antibiotic effects were dramatically increased. These effective combinations could be new promising agents in the management of MRSA and MSSA. Key words: Nardostachytis rhizoma, synergism, antibacterial, methicillin-resistant Staphylococcus aureus (MRSA). INTRODUCTION Staphylococcus aureus is a bacterium that grows in the human nose and skin and is a major pathogen for the skin and soft-tissue infections. Methicillin antibiotics have been used against S. aureus however, since its detection in 1961, methicillin-resistant S. aureus (MRSA) has become the most problematic Gram-positive bacterium in
10800
Afr. J. Biotechnol.
the public health field (Witte, 1999). This pathogen is associated with a variety of infectious diseases (Baltch et al., 2007) and has an average mortality rate of 36 to 50% (Dancer, 2008). With increasing antimicrobial resistance to various drugs, combination therapy appears to be a useful option, particularly in developing countries where the availability of drugs is limited (Aqil et al., 2006; Kastoris et al., 2010; Miranda-Novales et al., 2006). Furthermore, MRSA strains are resistant not only to betalactam antibiotics, but also to fluoroquinolones and other antibiotic families (Aqil et al., 2006). The primary purpose of this study was to investigate the in vitro effect on MRSA. Nardostachytis rhizoma is a perennial herb that grows in West and Northwest China. In traditional Chinese medicine, the roots and rhizomes of Nardostachys chinensis Batal are used for their stomachic and sedative effects (Lu, 1986). This plant is known to be rich in sesquiterpenoids, which were found to exhibit antimalarial, antinociceptive and cytotoxic activities (Itokawa et al., 1993) as well as have the ability to enhance neurite outgrowth, promoting activity (Lee et al., 2006). The chemical composition of the essential oils from roots and rhizomes of the N. chinensis obtained by hydrodistillation were analyzed by GC and GC-MS. Calarene (25.31%), aristolone (13.35%), -selinene (7.32%) and -maaliene (6.70%) were the major compounds of the 23 identified components which accounted for 92.76% of the total oil of N. rhizoma (Jihua et al., 2010).
MATERIALS AND METHODS Plant material and sample preparation N. rhizoma was purchased from on oriental drug store Well-being Hanyakkuk (Suncheon, korea), in April 2011. Samples were identified by Prof. Dong-Young Shin of the Department of Development in Plant Resources. A voucher specimen was deposited in the Laboratory of Oriental Pharmacology (N.1366). N. rhizoma was air-dried, and boiled in ethanol (2 L for 3 h). The ethanol extract of N. rhizoma (9.78% w/w) was partitioned with organic solvents of different polarities to yield n-hexane, EtOAc, nBuOH and water fractions, in sequence. The samples were stored at 4C.
ATCC 33591 (methicillin-resistant strain) and S. aureus ATCC 25923 (methicillin-susceptible strain). Before use, all bacteria were stored in 30% glycerol and frozen at -70C. The bacteria were cultured in Mueller-Hinton Broth (MHB) and Mueller-Hinton Agar (MHA) (Difco Laboratories, Baltimore, MD, USA). Bacteria were suspended in Mueller-Hinton Broth and then incubated at 37C for 24 h.
Antibiotics Ampicillin (AM) and oxacillin (OX) (Sigma Chemical Co. St. Louis, M0, USA) were used.
Disc diffusion method The disc diffusion method was described by the Clinical and Laboratory Standards Institute Standards and by using a modified agar-well diffusion method (CLSI, 2001). Bacterial strains grown on MHA at 37C for 18 h were suspended in MHB and adjusted to a turbidity of 0.5 McFarland standard scale (approximately 1.5 x 108 CFU/ml). The MHA was poured into Petri dishes and inoculated with 100 l of the suspension. Holes sterile paper discs (diameter 6 mm: Tokyo Roshi Kaihsa, Japan) were punched in the agar and filled with 500 and 250 g extracts. The dissolution of the organic extracts was facilitated with the addition of 50% (v/v) DMSO Sigma, USA (50% DMSO was not active against all strains). AM and OX (DMSO, Sigma, USA) were used as positive controls, and the discs treated with DMSO were used as the negative control. The plates were placed in an incubator at 37C for 18 h. The inhibition zone diameter around each of the discs was measured and recorded at the end of the incubation period.
Minimum inhibitory concentration The minimum inhibitory concentration (MIC) was determined using the broth microdilution method according to the Clinical and Laboratory Standards Institute Guideline (CLSI, 2000). Briefly, a preparation of the bacterial suspension was prepared by growing microorganisms in broth for 24 h and the suspensions were adjusted to a 0.5 McFarland standard turbidity (approximately 1.5 x 108 CFU/ml). Final inoculums were adjusted to the 1.5 x 106 CFU/ml. These serially diluted extracts were then incubated together with inoculum at 37C for 18 h. MIC was defined as the lowest concentration of AM, OX, N. rhizoma extracts and fractions (n-hexane, EtOAc, n-BuOH, aqueous) that inhibited the bacterial growth. At the end of the incubation period, the well plates were visually examined for turbidity. Cloudiness indicated that bacterial growth has not been inhibited by the concentration of antimicrobial agent contained in the medium.
Equipment An incubator (vision, Korea) was used. Checkerboard dilution test The synergistic combinations were investigated in the preliminary checkerboard method performed using the MRSA, MSSA and one clinical isolate strains via MIC determination, according to the published standards (Miranda-Novales et al., 2006; Odds, 2003). The MIC was defined as the lowest concentration of drug alone or in combination that inhibited the visible growth. The in vitro interaction was quantified by determining the fractional inhibitory concentration (FIC). The FIC index was calculated as follows: FIC = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone). FIC indices (FICI) were interpreted as follows: <0.5, synergy; 0.5 to 0.75, partial synergy; 0.76 to 1.0, additive effect; > 1.0 to 4.0, indifference; and >4.0,
Test microorganisms Five clinical isolates (MRSA), namely DPS1 to DPS5, were obtained from five different patients at W onkwang University Hospital (Iksan, South Korea). The other two strains were S. aureus
*Corresponding author. E-mail: sdw@sunchon.ac.kr. Tel: +8261-750-3665.
Joung et al.
10801
Table 1. Antimicrobial activity of N. rhizoma ethanol extract against S. aureus strain ATCC 33591 and ATCC 25923, DPS1, DPS2, DPS3, DPS4, DPS5 under dark.
Parameter S. aureus strain Dark
a
ATCC33591 500
Minimal inhibitory concentration (MIC) (g/ml) a ATCC25923 DPS1 DPS2 DPS3 DPS4 250 1000 250 1000 1000
DPS5 1000
DPS1 indicates Staphylococcus strains from the Department of Plastic Surgery, Wonkwang University Hospital; ND, no detected activity at this concentration.
Table 2. Antimicrobial activity of N. rhizoma ethanol extract, n-hexane, EtOAc, n-BuOH and water fractions against S. aureus strain ATCC33591, ATCC25923, DPS1, DPS2, DPS3, DPS4, DPS5 under dark.
S. aureus strain ATCC33591 ATCC25923 DPS1a DPS2 DPS3 DPS4 DPS5
a
n-hexane 125 62.5 250 31.25 62.5 125 125
Minimal inhibitory concentration (MIC) (g/ml) EtOAc n-BuOH H2O Ampicillin 1000 ND ND 500 500 ND ND 31.25 1000 ND ND 31.25 125 ND ND 1000 1000 ND ND 31.25 1000 ND ND 31.25 1000 ND ND 15.63
Oxacillin 500 500 1000 250 1000 1000 500
DPS1 indicates Staphylococcus strains from the Department of Plastic Surgery, Wonkwang University Hospital; ND, no detected activity at this concentration.
antagonism. Finally, the varying rates of synergy between the two agents were determined (Mazumdor et al., 2005). All experiments were independently repeated three times. Colorimetric assay using MTT test A colorimetric assay based on MTT for rapid detection of the presence of bacteria was performed as previously described (Abate et al., 1998; Scheuber et al., 1983; Shi et al., 2008). Briefly, a stock solution of 5 mg/ml MTT (Sigma) was prepared in phosphatebuffered saline and kept at -70C. A final concentration of 1 mg/ml of MTT was used in the assay. After 24 h of incubation at 37C, 20 l of the yellow MTT was added to the 96-well microtiter plate (0.3 ml volume) and incubated for an additional 20 min. The presence of a blue color indicates the presence of bacteria.
RESULTS AND DISCUSSION Ethanol extract had a MIC of 500 g/ml against S. aureus ATCC 33591 under dark condition, and had a MIC of 250 g/ml against S. aureus ATCC 25923 in the same condition (Table 1). Table 2 shows that the antimicrobial activity of n-hexane fraction was remarkable, and had a MIC of 31.25 to 250 g/ml against S. aureus strains. Antimicrobial activity of n-hexane fraction was remarkable. The n-hexane fraction of N. rhizoma showed antimicrobial activity inhibition zone of 14 to 18 mm against S. aureus strains (Table 3). n-hexane fraction of N. rhizoma lowered the MICs against the MRSA strain and MSSA but FICI values for HFN + AM and HFN + OX
were 0.1875 and 0.078125 to 0.09375, showing the increase of synergistic effect (Table 4). The most effective method is to develop antibiotics from the natural products without having any toxic or side effects. Therefore, there is a need to develop alternative antimicrobial drugs for the treatment of infectious diseases. Combination therapy is the most commonly recommended empirical treatment for bacterial infections in intensive care units, where monotherapy may not be effective against all potential pathogens, and used for preventing the emergence of resistant mutants (Drago et al., 2007). When combined together, these antibiotic effects were dramatically increased. Different drug combinations are reported to treat infections caused by pathogens (Drago et al., 2007; Liu et al., 2000; MirandaNovales et al., 2006). Antimicrobial activity of n-hexane fraction was remarkable, and had a MICs ranging from 31.25 to 250 g/ml and Checkerboard dilution test was performed to determine the action of HFN alone as well as its synergistic action with AM, or OX against the two strains. When tested against ATCC 33591, our data indicate that HFN alone only had moderate inhibitory effect on the growth of MRSA. However, in the presence of a non-growth inhibitory dose of HFN (125 g/ml) or AM (500 g/ml), HFN together with AM was highly effective with a FICI of 0.1875. Similar effects were also observed in MSSA strain. These results show that HFN in combination with these antibiotics could effectively inhibit MRSA growth. It may be partly due to the fact that they
10802
Afr. J. Biotechnol.
Table 3. Antimicrobial activity of N. rhizoma ethanol extract and n- hexane fractions (g/ml) against S. aureus strain ATCC33591, ATCC25923, DPS1, DPS2 DPS3, DPS4, DPS5 under dark.
S. aureus strain ATCC33591 ATCC25923 a DPS1 DPS2 DPS3 DPS4 DPS5
a
ethanol extract 500 250 8 ND 10 8 7 ND 12 9 9 ND 8 ND 8 ND
Zone of inhibitory (mm) n-hexane fractions AM 500 250 500 15 13 12 17 14 10 14 11 16 18 15 21 16 12 19 15 12 16 14 11 20
OX 250 9 8 11 19 11 13 15 500 ND ND ND 20 ND ND ND 250 ND ND ND 12 ND ND ND
DPS1 indicates Staphylococcus strains from the Department of Plastic Surgery, Wonkwang University Hospital; ND, no detected activity at this concentration.
Table 4. Interpreted FICIb response for HFNc + AM and HFN + OX combination against a standard MRSA strain and a standard MSSA strain
under dark.
Strains ATCC 33591 ATCC 25923
b
MIC of HFN + AM (g/ml) HFN AM Alone With AM Alone With HFN 125 15.625 500 31.25 62.5 7.8 31.25 1.59
c
FICI 0.1875 0.1875
HFN Alone With OX 125 7.8 62.5 3.9
MIC of HFN + OX (g/ml) OX Alone With HFN 500 15.625 500 7.8
FICI 0.09375 0.078125
FICI fractional inhibitory concentration index, HFN n-hexane fraction of N. rhizome, FIC fractional inhibitory concentration.
had abundant monoterpenoids and sesquiterpenoids which contributed to their antimicrobial activity and should be further studied. Antimicrobial and antioxidant mechanisms of the essential oils as well as their active components need to be further studied and clarified. In conclusion, we found that N. rhizoma extracts and nhexane fraction have an antibacterial effect on MRSA and MSSA, showing the increase of synergistic effect.
REFERENCES Abate G, Mshana RN, Miorner H (1998). Evaluation of a colorimetric assay based on 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) for rapid detection of rifampicin resistance in Mycobacterium tuberculosis. Int. J. Tuberc. Lung Dis., 2: 10111016. Aqil F, Ahmad I, Owais M (2006). Evaluation of anti-methicillinresistant Staphylococcus aureus (MRSA) activity and synergy of some bioactive plant extracts. Biotechnol. J., 1: 10931102. Baltch AL, Ritz WJ, Bopp LH, Michelsen PB, Smith RP (2007). Antimicrobial activities of daptomycin, vancomycin, and oxacillin in human monocytes and of daptomycin in combination with gentamicin and/or rifampin in human monocytes and in broth against Staphylococcus aureus . Antimicrob. Agents Chemother., 51: 1559 1562. CLSI (2000). Methods for dilution antimicrobial susceptibitity tests. For bacteria that aerobically Approved standards. CLSI document M7-A5. Wayne, PA. CLSI (2001). Performance standards for antimicrobial disk susceptibility tests. Approved standards. CLSI document M2 A7 Wayne, PA.
Dancer SJ (2008). The effect of antibiotics on methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother., 61: 246253. Drago L, De Vecchi E, Nicola L, Gismondo MR (2007). In vitro evaluation of antibiotics combinations for empirical therapy of suspected methicillin resistant Staphylococcus aureus severe respiratory infections. BMC Infect. Dis., 7: 111. Itokawa H, Masuyama K, Morita H, Takeya K (1993). Cytotoxic sesquiterpenes from Nardostachys chinensis. Chem. Pharm. Bull., 41: 1183-1184. Jihua W, Jianglin Z, Hao L, Ligang Z, Zhilong L, Jingguo W, Jianguo H, Zhu Y, Fuyu Y (2010). Chemical Analysis and Biological Activity of the Essential Oils of Two Valerianaceous Species from China: Nardostachys chinensis and Valeriana officinalis Molecules 15: 64116422; doi:10.3390/molecules15096411. Kastoris AC, Rafailidis PI, Vouloumanou EK, Gkegkes ID, Falagas ME (2010). Synergy of fosfomycin with other antibiotics for Gram-positive and Gram-negative bacteria. Eur. J. Clin. Pharmacol., 66: 359368. Lee SJ, Choi YH, Choi BT (2006). Inhibitory effects of aqueous extracts from Nardostachys chinensis on -melanocyte stimulating hormoneinduced melanogenesis in B16F10 cells. Integr. Biosci., 10: 233-236. Liu IX, Durham DG, Richards RM (2000). Baicalin synergy with betalactam antibiotics against methicillin-resistant Staphylococcus aureus and other beta-lactam-resistant strains of S. aureus. J. Pharm. Pharmacol., 52: 361366. Lu A, Chen S (1986). Flora Reipublicae Popularis Sinicae; Science Press: Beijing, China, Tomus 73. Mazumdor K, Dutta NK, Kumar KA, Dastidar SG (2005). In vitro and in vivo synergism between tetracycline and the cardiovascular agent oxyfedrine HCI against common bacterial strains. Biol. Pharm. Bull. 28: 713-771. Miranda-Novales G, Lean os -Miranda BE, Vilchis-Perez M, Solorzano-Santos F (2006). In vitro activity effects of combinations of cephalothin, dicloxacillin, imipenem, vancomycin and amikacin
Joung et al.
10803
against methicillin-resistant Staphylococcus spp. strains. Ann. Clin. Microbiol. Antimicrob., 5: 25. Odds FC (2003). Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother., 52: 1. Scheuber PH, Mossmann H, Beck G, Hammer DK (1983). Direct skin test in highly sensitized guinea pigs for rapid and sensitive determination of staphylococcal enterotoxin B. Appl. Environ. Microbiol., 46: 13511356.
Shi YJ, Chen J, Xu M (2008). A new method for antimicrobial susceptibility testing of in vitro-cultured bacteria by means of resonance light scattering technique. J. Microbiol. Biotechnol., 18: 118123. Witte W (1999). Antibiotic resistance in Gram-positive bacteria: epidemiological aspects. J. Antimicrob. Chemoth., 44: 1-9.
Potrebbero piacerti anche
- Article1401275147 - Shah Et AlDocumento6 pagineArticle1401275147 - Shah Et AlGustavo Gutiérrez GómezNessuna valutazione finora
- Immunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsDocumento7 pagineImmunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsUMYU Journal of Microbiology Research (UJMR)Nessuna valutazione finora
- tmp5FC5 TMPDocumento5 paginetmp5FC5 TMPFrontiersNessuna valutazione finora
- Me NTH ADocumento4 pagineMe NTH ASoumitra NathNessuna valutazione finora
- Anti-Fungal 8Documento4 pagineAnti-Fungal 8shubham panditNessuna valutazione finora
- Ahmed 2013Documento5 pagineAhmed 2013sii nuriantiNessuna valutazione finora
- Antimicrobial Activity of Emilia Sonchifolia DC Tridax Procumbens Etc Potential As Food PreservativesDocumento9 pagineAntimicrobial Activity of Emilia Sonchifolia DC Tridax Procumbens Etc Potential As Food Preservativessripathy84Nessuna valutazione finora
- Pasta TripleDocumento7 paginePasta TripleLincoln GarciaNessuna valutazione finora
- HJNHNNDocumento9 pagineHJNHNNProbioticsAnywhereNessuna valutazione finora
- Antibacterial and ModulatoryDocumento6 pagineAntibacterial and ModulatoryevilbioNessuna valutazione finora
- Isolation and Characterization of Actinomycetes From Soil and Evaluation of Antibacterial Activities of Actinomycetes Against PathogensDocumento9 pagineIsolation and Characterization of Actinomycetes From Soil and Evaluation of Antibacterial Activities of Actinomycetes Against PathogensTrương Tấn SangNessuna valutazione finora
- Trab 3Documento10 pagineTrab 3Diogo Luan de OliveiraNessuna valutazione finora
- Antibacterial Effect of Cassia Fistula Extract On Pathogenic Bacteria of Veterinary ImportanceDocumento5 pagineAntibacterial Effect of Cassia Fistula Extract On Pathogenic Bacteria of Veterinary ImportanceAsif MajeedNessuna valutazione finora
- Asian Journal of Pharmaceutical and Clinical ResearchDocumento6 pagineAsian Journal of Pharmaceutical and Clinical ResearchLeandro DouglasNessuna valutazione finora
- tmp9414 TMPDocumento8 paginetmp9414 TMPFrontiersNessuna valutazione finora
- De Lucca 2011Documento9 pagineDe Lucca 2011khadijaNessuna valutazione finora
- Anti-Mycobacterial Activity of Piper Longum L. Fruit Extracts Against Multi Drug Resistant Mycobacterium SPPDocumento9 pagineAnti-Mycobacterial Activity of Piper Longum L. Fruit Extracts Against Multi Drug Resistant Mycobacterium SPPBilici EcaterinaNessuna valutazione finora
- 17 Vol. 2issue 4IJPSR2011Paper 7Documento7 pagine17 Vol. 2issue 4IJPSR2011Paper 7Rea Dela MulongNessuna valutazione finora
- Assessment of Selected Yemeni Medicinal Plants For Their in Vitro Antimicrobial, Anticancer and Antioxidant ActivitiesDocumento11 pagineAssessment of Selected Yemeni Medicinal Plants For Their in Vitro Antimicrobial, Anticancer and Antioxidant ActivitiesvalvemayamNessuna valutazione finora
- Antibacterial Alkaloids From Chelidonium Majus Linn (Papaveraceae) Against Clinical Isolates of Methicillin-Resistant Staphylococcus AureusDocumento5 pagineAntibacterial Alkaloids From Chelidonium Majus Linn (Papaveraceae) Against Clinical Isolates of Methicillin-Resistant Staphylococcus AureusFitrianidilaNessuna valutazione finora
- EJM - Volume 53 - Issue 1 - Pages 49-68Documento20 pagineEJM - Volume 53 - Issue 1 - Pages 49-68seema yadavNessuna valutazione finora
- Parasitology International: ReviewDocumento8 pagineParasitology International: ReviewMarcos SilvaNessuna valutazione finora
- Tmp5a61 TMPDocumento8 pagineTmp5a61 TMPFrontiersNessuna valutazione finora
- Synergistic Antibacterial Activity of Salvia Officinalis and Cichorium Intybus Extracts and AntibioticsDocumento7 pagineSynergistic Antibacterial Activity of Salvia Officinalis and Cichorium Intybus Extracts and AntibioticsSAHID IQBALNessuna valutazione finora
- NIH Public Access: Author ManuscriptDocumento10 pagineNIH Public Access: Author ManuscriptSyahrul Hamidi NasutionNessuna valutazione finora
- Antimicrobial Resistance Profile of Helicobacter Pylori Clinical Isolates in Duhok City, Kurdistan Region/IraqDocumento4 pagineAntimicrobial Resistance Profile of Helicobacter Pylori Clinical Isolates in Duhok City, Kurdistan Region/IraqInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Phytochemical Screening and Antimicrobial Activity of Aqueous Stem Extract of Aloe Vera On Some Common Pathogenic BacteriaDocumento8 paginePhytochemical Screening and Antimicrobial Activity of Aqueous Stem Extract of Aloe Vera On Some Common Pathogenic BacteriaUMYU Journal of Microbiology Research (UJMR)Nessuna valutazione finora
- Staphylococcus Aureus, The Most Virulent Staphylococcus Species, Is Also The Prevalent Pathogen IsolatedDocumento6 pagineStaphylococcus Aureus, The Most Virulent Staphylococcus Species, Is Also The Prevalent Pathogen IsolatedVivi RocheNessuna valutazione finora
- Ảnh Hưởng Của Các Sản Phẩm Tự Nhiên Đến Một Số Giai Đoạn Của Chu Kỳ Bào Tử Của Clostridium Difficile in VitroDocumento27 pagineẢnh Hưởng Của Các Sản Phẩm Tự Nhiên Đến Một Số Giai Đoạn Của Chu Kỳ Bào Tử Của Clostridium Difficile in VitroLại Ngọc MaiNessuna valutazione finora
- AnmikDocumento4 pagineAnmikDimas Rinto MahardikaNessuna valutazione finora
- Food Chemistry: A. Sakunpak, P. PanichayupakaranantDocumento6 pagineFood Chemistry: A. Sakunpak, P. PanichayupakaranantSamiantara DotsNessuna valutazione finora
- Vol3 Issue5 03Documento5 pagineVol3 Issue5 03R.G.ManikarajanNessuna valutazione finora
- 11 Oxirane GC MSDocumento6 pagine11 Oxirane GC MSCHRISTIAN FELIPE JIMENEZ MURILLONessuna valutazione finora
- Evaluacion of Diffusion and Dilution Methods To Detemine The Antibacterial Activity of Plants ExtractsDocumento6 pagineEvaluacion of Diffusion and Dilution Methods To Detemine The Antibacterial Activity of Plants ExtractsLuis Alberto AnguianoNessuna valutazione finora
- tmpECD6 TMPDocumento10 paginetmpECD6 TMPFrontiersNessuna valutazione finora
- Phytochemical Study and Antibacterial Activity of Ethanolic and Aqueous Extracts of Barks of Myrianthus Holstii Engl. (Cecropiaceae)Documento8 paginePhytochemical Study and Antibacterial Activity of Ethanolic and Aqueous Extracts of Barks of Myrianthus Holstii Engl. (Cecropiaceae)IJAR JOURNALNessuna valutazione finora
- Characterization of Antimicrobial Antioxidant AntiDocumento7 pagineCharacterization of Antimicrobial Antioxidant AntiHamidun MhydunNessuna valutazione finora
- Fphar 12 746808Documento14 pagineFphar 12 746808Mary Grace LanwangNessuna valutazione finora
- Tamizhazhagan 1Documento3 pagineTamizhazhagan 1TamizhazhaganNessuna valutazione finora
- 9920-Article Text-64618-1-10-20180206Documento6 pagine9920-Article Text-64618-1-10-20180206GioviNessuna valutazione finora
- Bpswinter2011 0218Documento3 pagineBpswinter2011 0218Fahru DinNessuna valutazione finora
- Anti InflammatoryDocumento7 pagineAnti InflammatoryJeylan simboNessuna valutazione finora
- Anti Microbial Activity of ChloxylonDocumento3 pagineAnti Microbial Activity of ChloxylonDr. Ramadevi DevarakondaNessuna valutazione finora
- Agar Well Diffusion MTDDocumento7 pagineAgar Well Diffusion MTDRoland GealonNessuna valutazione finora
- ArticleDocumento6 pagineArticleSalmaNessuna valutazione finora
- In Vitro Antimicrobial Potential of Extracts and PDocumento14 pagineIn Vitro Antimicrobial Potential of Extracts and PWilliam VolmerNessuna valutazione finora
- Phytochemical Screening and Antibacterial Activity of Four Cnidoscolus Species (Euphorbiaceae) Against Standard Strains and Clinical IsolatesDocumento8 paginePhytochemical Screening and Antibacterial Activity of Four Cnidoscolus Species (Euphorbiaceae) Against Standard Strains and Clinical IsolatesÓscar AguirreNessuna valutazione finora
- Activity of Plant Extracts Used in Northern Nigerian Traditional Medicine Against Methicillin-ResistantDocumento8 pagineActivity of Plant Extracts Used in Northern Nigerian Traditional Medicine Against Methicillin-ResistantSukma ArdillaNessuna valutazione finora
- Sambiloto 4Documento8 pagineSambiloto 4Radiksa AzryNessuna valutazione finora
- Abjna 3 2 43 48Documento6 pagineAbjna 3 2 43 48Riskha Febriani HapsariNessuna valutazione finora
- Screening The Anti Gout Traditional Herbs From TCM Using An in VitroDocumento7 pagineScreening The Anti Gout Traditional Herbs From TCM Using An in VitroSanithaaaNessuna valutazione finora
- Apjcp 19 2911Documento6 pagineApjcp 19 2911Arian RahimiNessuna valutazione finora
- TC 15025Documento4 pagineTC 15025MD MuntaharNessuna valutazione finora
- Antimycobacterial Compound From Thai LeavesDocumento20 pagineAntimycobacterial Compound From Thai LeavesMayuriNessuna valutazione finora
- Research Article in Vitro Cytotoxic, Antioxidant, and Antimicrobial Mesua Beccariana (Baill.) Kosterm., Mesua Ferrea Mesua Congestiflora ExtractsDocumento10 pagineResearch Article in Vitro Cytotoxic, Antioxidant, and Antimicrobial Mesua Beccariana (Baill.) Kosterm., Mesua Ferrea Mesua Congestiflora ExtractsKelas B FarmasiNessuna valutazione finora
- With Activities of Amphotericin B and in Vitro Activity of SCH-56592 and ComparisonDocumento4 pagineWith Activities of Amphotericin B and in Vitro Activity of SCH-56592 and ComparisonMaria Marta SampietroNessuna valutazione finora
- Zahedan J Res Med Sci 2012 14 8 74 76Documento3 pagineZahedan J Res Med Sci 2012 14 8 74 76yudhit bessieNessuna valutazione finora
- Textbook on the Bases of Pharmaceutical and Medicinal Chemistry of AntibioticsDa EverandTextbook on the Bases of Pharmaceutical and Medicinal Chemistry of AntibioticsNessuna valutazione finora
- Current Trends in the Identification and Development of Antimicrobial AgentsDa EverandCurrent Trends in the Identification and Development of Antimicrobial AgentsNessuna valutazione finora
- Endophyte Biotechnology: Potential for Agriculture and PharmacologyDa EverandEndophyte Biotechnology: Potential for Agriculture and PharmacologyAlexander SchoutenNessuna valutazione finora
- Antibiotics: Phages in Food Industry Biocontrol and BioremediationDocumento15 pagineAntibiotics: Phages in Food Industry Biocontrol and BioremediationJuan Favela HernandezNessuna valutazione finora
- APJCP - Volume 15 - Issue 15 - Pages 6137-6143 PDFDocumento7 pagineAPJCP - Volume 15 - Issue 15 - Pages 6137-6143 PDFJuan Favela HernandezNessuna valutazione finora
- Effect of Garlic (Allium Sativum) Oil OnDocumento4 pagineEffect of Garlic (Allium Sativum) Oil OnJuan Favela HernandezNessuna valutazione finora
- 1 PDFDocumento6 pagine1 PDFJuan Favela HernandezNessuna valutazione finora
- DM2015 253519Documento9 pagineDM2015 253519Juan Favela HernandezNessuna valutazione finora
- Bicas J.L Et Al., 2008Documento12 pagineBicas J.L Et Al., 2008Juan Favela HernandezNessuna valutazione finora
- Chemistry of Toxic Range Plants. Highly Oxygenated Flavonol Methyl Ethers From Gutierrezza MzcrocephalaDocumento14 pagineChemistry of Toxic Range Plants. Highly Oxygenated Flavonol Methyl Ethers From Gutierrezza MzcrocephalaJuan Favela HernandezNessuna valutazione finora
- 1 s2.0 S0367326X98000446 MainDocumento4 pagine1 s2.0 S0367326X98000446 MainJuan Favela HernandezNessuna valutazione finora
- 1 s2.0 S1751722213002801 MainDocumento4 pagine1 s2.0 S1751722213002801 MainJuan Favela HernandezNessuna valutazione finora
- Microbial PathogenesisDocumento6 pagineMicrobial PathogenesisJuan Favela HernandezNessuna valutazione finora
- Advanced Drug Delivery ReviewsDocumento12 pagineAdvanced Drug Delivery ReviewsJuan Favela HernandezNessuna valutazione finora
- MezquiteDocumento21 pagineMezquiteJuan Favela HernandezNessuna valutazione finora
- Fulltext 1Documento21 pagineFulltext 1Juan Favela HernandezNessuna valutazione finora
- wst1 CelprolDocumento18 paginewst1 CelprolJuan Favela HernandezNessuna valutazione finora
- EvodiaDocumento4 pagineEvodiaJuan Favela HernandezNessuna valutazione finora
- J. Biol. Chem.-2004-Boshoff-40174-84Documento11 pagineJ. Biol. Chem.-2004-Boshoff-40174-84Juan Favela HernandezNessuna valutazione finora
- E. ColiDocumento3 pagineE. ColiJuan Favela HernandezNessuna valutazione finora
- Olea EuropaeaDocumento7 pagineOlea EuropaeaJuan Favela HernandezNessuna valutazione finora
- Citotoxicidad Rosa SalpinoDocumento13 pagineCitotoxicidad Rosa SalpinoJuan Favela HernandezNessuna valutazione finora
- 94Documento95 pagine94lthyaguNessuna valutazione finora
- Classes of Antibiotics SummaryDocumento1 paginaClasses of Antibiotics Summaryhanzukik100% (1)
- 1-1 Multicolor Fluorochrome Laser ChartDocumento1 pagina1-1 Multicolor Fluorochrome Laser Chartgonococo1Nessuna valutazione finora
- Enhanced Glucan Formation of Filamentous Fungi by Effective Mixing, Oxygen Limitation and Fed-Batch ProcessingDocumento7 pagineEnhanced Glucan Formation of Filamentous Fungi by Effective Mixing, Oxygen Limitation and Fed-Batch ProcessingEdward Marques de SouzaNessuna valutazione finora
- The Mitotic Cell CycleDocumento21 pagineThe Mitotic Cell CycleKulo AchrudinNessuna valutazione finora
- Industrial Production of Beta-Lactam AntibioticsDocumento8 pagineIndustrial Production of Beta-Lactam AntibioticsSyarif AlmubarakNessuna valutazione finora
- Theoretical Correlation Between Viscosities at Dynamic and Steady Flow States in Aureobasidium Pullulans Culture FluidsDocumento3 pagineTheoretical Correlation Between Viscosities at Dynamic and Steady Flow States in Aureobasidium Pullulans Culture FluidsM.Çağrı AltındalNessuna valutazione finora
- Todd O. Yeates, Todd S. Norcross and Neil P. King - Knotted and Topologically Complex Proteins As Models For Studying Folding and StabilityDocumento14 pagineTodd O. Yeates, Todd S. Norcross and Neil P. King - Knotted and Topologically Complex Proteins As Models For Studying Folding and StabilityLokosooNessuna valutazione finora
- Phy 420Documento4 paginePhy 420Muhammad Farooq UmarNessuna valutazione finora
- Food Biotechnology and Food SafetyDocumento3 pagineFood Biotechnology and Food SafetykingsleyesedebeNessuna valutazione finora
- Industrial Production of Soy Sauce: B.S. LuhDocumento5 pagineIndustrial Production of Soy Sauce: B.S. Luhazmi rahmayaniNessuna valutazione finora
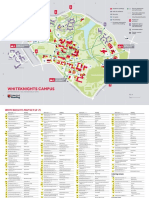
- Whiteknights Campus MapDocumento4 pagineWhiteknights Campus MapRajvirBhogalNessuna valutazione finora
- 15-6411 USD3086 Star-Plus Microcarriers AnDocumento5 pagine15-6411 USD3086 Star-Plus Microcarriers AnDEVESH BHOLENessuna valutazione finora
- 1 Biological Sciences DDocumento2 pagine1 Biological Sciences Derum shomailNessuna valutazione finora
- Course Outline BIOT 423 and 421Documento4 pagineCourse Outline BIOT 423 and 421Ryan ReighnsNessuna valutazione finora
- MIT7 01SCF11 4.5sol PDFDocumento3 pagineMIT7 01SCF11 4.5sol PDFLopamudra BiswasNessuna valutazione finora
- Encyclopedia of Biological Chemistry - Vol - 1Documento895 pagineEncyclopedia of Biological Chemistry - Vol - 1aishbiyaNessuna valutazione finora
- Pres 4381 Fa 324 C 214Documento11 paginePres 4381 Fa 324 C 214Yatharth AnandNessuna valutazione finora
- Single Use Systems - BiotechnologyDocumento22 pagineSingle Use Systems - BiotechnologyRashad SyedNessuna valutazione finora
- Systems and Computational Biology - Molecular and Cellular Experimental SystemsDocumento344 pagineSystems and Computational Biology - Molecular and Cellular Experimental Systemscentroid100% (1)
- 2ND QUARTER WEEK 4 GENETIC ENGINEERING FinalDocumento18 pagine2ND QUARTER WEEK 4 GENETIC ENGINEERING FinalMarylyn MirandaNessuna valutazione finora
- Test - IB Biology 10.1 - QuizletDocumento4 pagineTest - IB Biology 10.1 - QuizletSumi VjNessuna valutazione finora
- 4.1 - Cell Cycle Part 1Documento5 pagine4.1 - Cell Cycle Part 1Deomar Joseph ParadoNessuna valutazione finora
- Tarifa Neb 2011-1Documento19 pagineTarifa Neb 2011-1Antonio Diez JuanNessuna valutazione finora
- B.sc. Hons. Chemistry71-72Documento2 pagineB.sc. Hons. Chemistry71-72calix468Nessuna valutazione finora
- VarII Raspuns BaremeDocumento7 pagineVarII Raspuns BaremeIancu Adina FloricicaNessuna valutazione finora
- Reference Regulatory AuthoritiesDocumento2 pagineReference Regulatory AuthoritiesziadddNessuna valutazione finora
- Competent Cells and TransformationDocumento22 pagineCompetent Cells and TransformationCarinaJongLeeNessuna valutazione finora
- Animal BioreactorDocumento12 pagineAnimal BioreactorBhuvanesh TNessuna valutazione finora
- List of Sub-Themes: International Law and Human RightsDocumento3 pagineList of Sub-Themes: International Law and Human RightsApooNessuna valutazione finora