Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
QLF Review Caries
Caricato da
Eliza DNCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
QLF Review Caries
Caricato da
Eliza DNCopyright:
Formati disponibili
The Official Journal of the Academy of Laser Dentistry
2008 2008 Vol. Vol. 16 16 No. No. 1 1
Caries Detection by Quantitative Light-Induced Fluorescence
See the technology review article on page 6
Scientific Report: Er,Cr:YSGG Laser Effects on Dentin and Collagen Case Reports: Treatment of Moderate Chronic Periodontitis; Gingivoplasty, Frenectomy, and Second-Stage Implant Recovery; Establishing a Gingival Smile Line; Treatment of Lip Hemangiomas
Academy of Laser Dentistry 3300 University Drive, Suite 704 Coral Springs, FL 33065
Journal of Laser Dentistry
The official journal of the Academy of Laser Dentistry Editor in Chief John D.B. Featherstone, MSc, PhD San Francisco, CA
TA B L E O F C O N T E N T S
jdbf@ucsf.edu
Managing Editor Gail S. Siminovsky, CAE, Executive Director Coral Springs, FL siminovsky@laserdentistry.org Consulting Editor John G. Sulewski, MA Huntington Woods, MI john.sulewski@we-inc.com Associate Editors Donald J. Coluzzi, DDS Portola Valley, CA don@laser-dentistry.com Steven P.A. Parker, BDS, LDS RCS, MFGDP Harrogate, Great Britain thewholetooth@easynet.co.uk Editorial Board John D.B. Featherstone, MSc, PhD Gail S. Siminovsky, CAE John G. Sulewski, MA Donald J. Coluzzi, DDS Steven P.A. Parker, BDS, LDS RCS, MFGDP Alan J. Goldstein, DMD Donald E. Patthoff, DDS Peter Rechmann, Prof. Dr. med. dent. Publisher Max G. Moses Member Media 1844 N. Larrabee Chicago, IL 60614 312-296-7864 Fax: 312-896-9119 max@maxgmoses.com Design and Layout Diva Design 2616 Missum Point San Marcos, TX 78666 512-665-0544 Fax: 512-392-2967 kkolstedt@austin.rr.com Editorial Office 3300 University Drive, Suite 704 Coral Springs, FL 33065
E D I TO R S V I E W
Understanding Our Laser Tools to Better Serve Our Patients ..................5 John D.B. Featherstone, MSc, PhD
C O V E R F E AT U R E CLINICAL REVIEW
Supplementary Methods for Detection and Quantification of Dental Caries........................................................................................................6 Lena Karlsson, RDH; Sofia Tranus, DDS, PhD
SCI ENTI F IC R EPORT
Effect of Er,Cr:YSGG Laser on Human Dentin Collagen: A Preliminary Study ............................................................15 Eleftherios-Terry Farmakis, DDS, MDSc, PhD; Konstantinos Kozyrakis, DDS, PhD; Evangelos G. Kontakiotis, DDS, PhD; Kouvelas Nikolaos DDS, PhD
A DVA N C E D P R O F I C I E N C Y C A S E ST U D I E S
Introduction ............................................................................................................22 Nd:YAG Laser-Assisted Treatment of Moderate Chronic Periodontitis........................................................................23 Mary Lynn Smith, RDH; McPherson, Kansas Use of an 810-nm Diode Laser in a Combined Gingivoplasty, Frenectomy, and Second-Stage Implant Recovery Procedure ................30 Steven Parker, BDS, LDS RCS, MFGDP; Harrogate, North Yorks, Great Britain Establishing a Maintainable Esthetic Gingival Smile Line with an Er:YAG Laser ......................................................................37 Charles R. Hoopingarner, DDS, Houston, Texas Use of an 810-nm Diode Laser in the Treatment of Multiple Hemangiomata of the Lip ............................................................43 Steven Parker, BDS, LDS RCS, MFGDP; Harrogate, North Yorks, Great Britain
954-346-3776 Fax 954-757-2598 www.laserdentistry.org laserexec@laserdentistry.org The Academy of Laser Dentistry is a not-for-profit organization qualifying under Section 501(c)(3) of the Internal Revenue Code. The Academy of Laser Dentistry is an international professional membership association of dental practitioners and supporting organizations dedicated to improving the health and well-being of patients through the proper use of laser technology. The Academy is dedicated to the advancement of knowledge, research and education and to the exchange of information relative to the art and science of the use of lasers in dentistry. The Academy endorses the Curriculum Guidelines and Standards for Dental Laser Education. Member American Association of Dental Editors
Laser Treatment of Vascular Lesions of the Lip ..........................................48
The Journal of Laser Dentistry The mission of the Journal of Laser Dentistry is to provide a professional quarterly journal that helps to fulfill the goal of information dissemination by the Academy of Laser Dentistry. The purpose of the Journal of Laser Dentistry is to present information about the use of lasers in dentistry. All articles are peer-reviewed. Issues include manuscripts on current indications for uses of lasers for dental applications, clinical case studies, reviews of topics relevant to laser dentistry, research articles, clinical studies, research abstracts detailing the scientific basis for the safety and efficacy of the devices, and articles about future and experimental procedures. In addition, featured columnists offer clinical insights, and editorials describe personal viewpoints.
JOU R NAL OF L ASER DENTI STRY
R ESEARCH AB STR ACTS
20 0 8 VO L 16 , N O . 1
Journal of Laser Dentistry: Guidelines for Authors
The Academy of Laser Dentistry Welcomes Your Articles for Submission
The Journal of Laser Dentistry publishes articles pertaining to the art, science, and practice of laser dentistry and other relevant light-based technologies. Articles may be scientific and clinical in nature discussing new techniques, research, and programs, or may be applications-oriented describing specific problems and solutions. While lasers are our preferred orientation, other high-technology articles, as well as insights into marketing, practice management, regulation, and other aspects of dentistry that may be of interest to the dental profession, may be appropriate. All articles are peer-reviewed prior to acceptance, modification, or rejection. These guidelines are designed to help potential authors in writing and submitting manuscripts to the Journal of Laser Dentistry, the official publication of the Academy of Laser Dentistry (ALD). Please follow these instructions carefully to expedite review and processing of your submission. Manuscripts that do not adhere to these instructions will not be accepted for consideration. The Academy of Laser Dentistry and the editors and publisher of the Journal of Laser Dentistry endorse the Uniform Requirements of Manuscripts Submitted to Biomedical Journals (www.icmje.org). The Journal reserves the right to revise or rescind these guidelines. Authors are advised to read the more comprehensive Guidelines for Authors and required forms available by mail or online at www.laserdentistry.org. Manuscript Eligibility Submitted manuscripts must be written clearly and concisely in American English and appropriate for a scholarly journal. Write in active voice and use declarative sentences. Manuscripts will be considered for publication on the condition that they have been submitted exclusively to the Journal, and have not been published or submitted for publication in any part or form in another publication of any type, professional or lay, or in any language elsewhere, and with the understanding that they will not be reprinted without written consent from both the managing editor and the author. Permissions Direct quotations of 100 or more words, and illustrations, figures, tables, or other materials (or adaptations thereof) that have appeared in copyrighted material or are in press must be accompanied by written permission for their use in the Journal of Laser Dentistry from the copyright owner and original author along with complete information regarding source, including (as applicable) author(s), title of article, title of journal or book, year, volume number, issue number, pages. Photographs of identifiable persons must be accompanied by valid signed releases indicating informed consent. When informed consent has been obtained from any patient, identifiable or not, it should be noted in the manuscript. The appropriate Permission Letters must be submitted with the manuscript. Suggested template letters are available online. Copyright All manuscript rights shall be transferred to the Journal of Laser Dentistry upon submission. Upon submission of the manuscript, authors agree to submit a completed Copyright Transfer Agreement form, available online. If the manuscript is rejected for publication, all copyrights will be retained by the author(s). Commercialism ALD members are interested in learning about new products and service offerings, however ALD stresses that submitted manuscripts should be educational in nature. The emphasis is on scientific research and sound clinical and practical advice, rather than promotion of a specific product or service. Disclosure of Commercial Relationships According to the Academys Conflict of Interest and Disclosure policy, manuscript authors and their institutions are expected to disclose any economic or financial support, as well as any personal, commercial, technological, academic, intellectual, professional, philosophical, political, or religious interests or potential bias that may be perceived as creating a conflict related to the material being published. Such conditions may include employment, consultancies, stock ownership or other equity interests, honoraria, stipends, paid expert testimony, patent ownership, patent licensing arrangements, royalties, or serving as an officer, director, or owner of a company whose products, or products of a competitor, are identified. Sources of support in the form of contracts, grants, equipment, drugs, material donations, clinical materials, special discounts or gifts, or other forms of support should be specified. The roles of the study or manuscript sponsor(s), if any, are to be described. Disclosure statements are printed at the end of the article following the authors biography. This policy is intended to alert the audience to any potential bias or conflict so that readers may form their own judgments about the material being presented. Disclosure forms are to be signed by each author. Manuscripts will not be reviewed without the Journal having this form on file. The Academy of Laser Dentistry also requires that authors disclose whether any product discussed in their manuscript is unlabeled for the use discussed or is investigational. The Disclosure Statement form is available online and must be submitted with the manuscript. Manuscript Types Submissions to the Journal should be limited to one of the types indicated below. Scientific / Technology / Clinical Review Case Reports and Clinical Case Studies Scientific / Clinical Research Randomized Clinical Trials Advances in Dental Products Trends Practice Management Guest Editorials and Essays Letters to the Editor Book Reviews Manuscript Preparation and Submission Format All submitted manuscripts should be double-spaced, using 12 pt. font size with at least 6 mm between lines. Submit manuscripts in Microsoft Word (.doc), using either the Windows or Macintosh platform. Manuscripts must be submitted electronically in this format. Hard copy-only submissions will not be accepted. Unacceptable Formats The following submission formats are unacceptable and will be returned: Manuscripts submitted in desktop publishing software PowerPoint presentations Any text files with embedded images Images in lower than the minimum prescribed resolution. Manuscript Components Title Page The title page of the manuscript should include a concise and informative title of the article; the first name, middle initial(s), and last name of each author, along with the academic degree(s), professional title(s), and the name and location (city, state, zip code) of current institutional affiliation(s) and department(s). Authors who are private practitioners should identify their location (city, state, and country). Include all information in the title that will make
electronic retrieval of the article sensitive and specific. Titles of case studies should include the laser wavelength(s) and type(s) utilized for treatment (for example, 810-nm GaAlAs diode). Identify the complete address, business and home telephone numbers, fax number, e-mail address, and Web site address (if any) for all authors. Identify one author as the corresponding author. Unless requested otherwise, the e-mail address is published in the Journal. Abstract A self-standing summary of the text of up to 250 words should precede the introduction. It should provide an accurate summary of the most significant points and be representative of the entire articles content. Provide the context or background for the article, basic procedures, main findings and conclusions. Emphasize new or important aspects. Do not use abbreviations (other than standard units of measurement) or references in the abstract. Author(s) Biography Provide a brief, current biographical sketch of each author that includes professional education and professional affiliations. For authors who hold teaching positions, include the title, department, and school. For authors who are in federal service, include rank or title and station. References References are to be cited in the text by number in order of appearance, with the number appearing either as a superscript or in brackets. The reference list should appear at the end of the manuscript with references in order of first appearance in the text of the manuscript. The reference list must be typed double-spaced on a separate page and numbered in the same sequence as the reference citations appear in the text. Prior to submission, all references are to be properly prepared in the correct format, checked for completeness, carefully verified against their original documents, and checked for accurate correspondence between references cited in the text and listed in the References section. For journal citations, include surnames and all initials of all authors, complete title of article, name of journal (abbreviated according to the U.S. National Library of Medicine (www.nlm.nih.gov/services/ lpabbrev.html), year of publication, volume, issue number, and complete inclusive page numbers. If abstracts are cited, add the abstract number after the page number. For book citations, specify surnames and initials of all authors, chapter number and title (if applicable), edi-
tors surnames and initials, book title, volume number (if applicable), edition number (if applicable), city and full name of publisher, year of publication, and inclusive page numbers of citation. For government publications or bulletins, identify the author(s) (if given); title; department, bureau, agency, or office; the publication series, report, or monograph number; location of publisher; publisher; year of publication; and inclusive page numbers. For articles published online but not yet in print, cite with the papers Digital Object Identifier (DOI) added to the end of the reference. For Web citations, list the authors and titles if known, then the URL and date it was accessed. For presentations, list the authors, title of presentation, indication that the reference is a lecture, name of conference or presentation venue, date, and location.
least 5 inches (127 mm) in width. The image must be submitted in the size it will be printed, or larger. Illustrations are to augment, not repeat, material in the text. Graphs must not repeat data presented in tables. Clinical photographs must comply with ALDs Guidelines for Clinical Photography, available online. Authors are to certify in a cover letter that digitized illustrations accurately represent the original data, condition, or image and are not electronically edited. Publisher and Copyright Holder The Journal of Laser Dentistry is published by Max G. Moses, Member Media, 1844 N. Larrabee, Chicago, IL 60614, Telephone: (312) 296-7864; Fax: (312) 896-9119. The Journal of Laser Dentistry is copyrighted by The Academy of Laser Dentistry, 3300 University Drive, Suite 704, Coral Springs, FL 33065, Telephone: (954) 346-3776; Fax: (954) 757-2598. Articles, Questions, Ideas Questions about clinical cases, scientific research, or ideas for other articles may be directed to John D.B. Featherstone, Editor-in-Chief, by e-mail: jdbf@ucsf.edu. Submission of Files by E-mail: Send your completed files by e-mail (files up to 10 MB are acceptable). If files are larger than 10 MB, they may be compressed or sent as more than one file, with appropriate labels. Files should be submitted to: John D.B. Featherstone, Editor-in-Chief by e-mail: jdbf@ucsf.edu. By Federal Express or Other Insured Courier: If using a courier, please send the file as a CD-ROM, include a hard copy of your manuscript and also send a verification by e-mail to Gail Siminovsky (laserexec@laserdentistry.org). Gail Siminovsky Academy of Laser Dentistry 3300 University Drive, Suite 704 Coral Springs, FL 33065 Phone: (954) 346-3776.
Illustration Captions and Legends All illustrations must be accompanied by individual explanatory captions which should be typed double-spaced on a separate page with Arabic numerals corresponding to their respective illustration. Tables Tables must be typewritten doublespaced, including column heads, data, and footnotes, and submitted on separate pages. The tables are to be cited in the text and numbered consecutively in Arabic numerals in the order of their appearance in the text. Provide a concise title for each table that highlights the key result. Illustrations Illustrations include photographs, radiographs, micrographs, charts, graphs, and maps. Each should be numbered and cited in the text in the order of appearance and be accompanied by explanatory captions. Do not embed figures within the manuscript text. Each figure and table should be no larger than 8-1/2 x 11 inches. Digital files must measure at
Summary of Illustration Types and Specifications Illustration Type Definition and Examples Preferred Format Required Resolution
Line Art and Black and white graphic with no EPS or JPG 1200 DPI Vector Graphics shading (e.g., graphs, charts, maps) Photographs, drawings, or painting with fine shading (e.g., radi- TIFF or ographs, micrographs with scale JPG bars, intraoral photographs) 300 DPI (black & white) 600 DPI (color)
Halftone Art
Combination Art
Combination of halftone and line art (e.g., halftones containing EPS or JPG 1200 DPI line drawing, extensive lettering, color diagrams)
Editorial Policy The Journal of Laser Dentistry is devoted to providing the Academy and its members with comprehensive clinical, didactic and research information about the safe and effective uses of lasers in dentistry. All statements of opinions and/or fact are published under the authority of the authors, including editorials and articles. The Academy is not responsible for the opinions expressed by the writers, editors or advertisers. The views are not to be accepted as the views of the Academy of Laser Dentistry unless such statements have been expressly adopted by the organization. Information on any research, clinical procedures or products may be obtained from the author. Comments concerning content may be directed to the Academys main office by e-mail to laserexec@laserdentistry.org Submissions We encourage prospective authors to follow JLDs Instructions to Authors before submitting manuscripts. To obtain a copy, please go to our Web site www.laserdentistry.org/press.cfm. Please send manuscripts by e-mail to the Editor at jdbf@ucsf.edu. Disclosure Policy of Contributing Authors Commercial Relationships According to the Academys Conflict of Interest and Disclosure policy, authors of manuscripts for JLD are expected to disclose any economic support, personal interests, or potential bias that may be perceived as creating a conflict related to the material being published. Disclosure statements are printed at the end of the article following the authors biography. This policy is intended to alert the audience to any potential bias or conflict so that readers may form their own judgments about the material being presented. Disclosure Statement for the Academy of Laser Dentistry The Academy of Laser Dentistry has no financial interest in any manufacturers or vendors of dental supplies. Reprint Permission Policy Written permission must be obtained to duplicate and/or distribute any portion of the Journal of Laser Dentistry. Reprints may be obtained directly from the Academy of Laser Dentistry provided that any appropriate fee is paid. Copyright 2008 Academy of Laser Dentistry. All rights reserved unless other ownership is indicated. If any omission or infringement of copyright has occurred through oversight, upon notification amendment will be made in a future issue. No part of this publication may be reproduced or transmitted in any fom or by any means, individually or by any means, without permission from the copyright holder. The Journal of the Academy of Laser Dentistry ISSN# 1935-2557. JLD is published quarterly and mailed nonprofit standard mail to all ALD members. Issues are also mailed to new member prospects and dentists requesting information on lasers in dentistry. Advertising Information and Rates Display rates are available at www.laserdentistry.org/press.cfm and/or supplied upon request. Insertion orders and materials should be sent to Bill Spilman, Innovative Media Solutions, P.O. Box 399, Oneida, IL 61467, 877-878-3260, fax: 309-483-2371, e-mail bill@innovativemediasolutions.com. For a copy of JLD Advertising Guidelines go to www.laserdentistry.org/press_advguide_policy.cfm. The cost for a classified ad in one issue is $50 for the first 25 words and $2.00 for each additional word beyond 25. ALD members receive a 20% discount. Payment must accompany ad copy and is payable to the Academy of Laser Dentistry in U.S. funds only. Classified advertising is not open to commercial enterprises. Companies are encouraged to contact Bill Spilman for information on display advertising specifications and rates. The Academy reserves the right to edit or refuse ads.
Editors Note on Advertising: The Journal of Laser Dentistry currently accepts advertisements for different dental laser educational programs. Not all dental laser educational courses are recognized by the Academy of Laser Dentistry. ALD as an independent professional dental organization is concerned that courses meet the stringent guidelines following professional standards of education. Readers are advised to verify with ALD whether or not specific courses are recognized by the Academy of Laser Dentistry in their use of the Curriculum Guidelines and Standards for Dental Laser Education.
E D I TO R S V I E W
Understanding Our Laser Tools to Better Serve Our Patients
John D.B. Featherstone, MSc, PhD, San Francisco, California
J Laser Dent 2008;16(1):5
SYNOPSIS
John Featherstone, editor-in-chief, describes some of the highlights of this issue of the Journal of Laser Dentistry, illustrating how we must understand what we are doing to better serve our patients.
AUTHOR BIOGRAPHY
Dr. John D.B. Featherstone is Professor of Preventive and Restorative Dental Sciences and Interim Dean in the School of Dentistry at the University of California, San Francisco (UCSF). He has a PhD in chemistry from the University of Wellington (New Zealand). His research over the past 33 years has covered several aspects of cariology (study of tooth decay) including fluoride mechanisms of action, de- and remineralization of the teeth, apatite chemistry, salivary dysfunction, caries (tooth decay) prevention, caries risk assessment, and laser effects on dental hard tissues with emphasis on caries prevention and early caries removal. He has won numerous national and international awards including the T.H. Maiman award for research in laser dentistry from the Academy of Laser Dentistry in 2002, and the Norton Ross Award for Clinical Research from the American Dental Association in 2007. In 2005 he was honored as the first lifetime honorary member of the Academy of Laser Dentistry. Dr. Featherstone has published over 200 papers. He is the editor-in-chief of the Journal of Laser Dentistry.
Disclosure: Dr. Featherstone has no personal financial interest in any company relevant to the Academy of Laser Dentistry. He consults for, has consulted for, or has done research funded or supported by Arm & Hammer, Beecham, Cadbury, GSK, KaVo, NovaMin, Philips Oralcare, Procter & Gamble, OMNII Oral Pharmaceuticals, Oral-B, Wrigley, and the National Institutes of Health.
JOU R NAL OF L ASER DENTI STRY
Last month we had articles that described how light, including laser light, can be used in everyday dental practice. The article on laser fluorescence for caries detection described just one of the novel new techniques that are becoming available. This month a review of several other techniques is presented. The bottom line is that we must understand how each of these instruments works so that we can make an assessment of what the results mean for our patients. There is no step-by-step cookbook with recipes to work from. The practitioner must be able to interpret the output to best use the information. Many dentists who use lasers in their practice use them for ablation of dental hard tissues, for the removal of decay, and for cavity preparations. In this issue we have an applied research article that helps us understand what the erbium lasers are doing. Again, a better understanding of the tools that we have in our hands is essential for the best treatment plan and the best outcome for our patients. The case studies are presented as examples of how to put into practice the understanding that the authors have of the lasers that they are using for the various tasks. Laser dentistry is
not the only way to tackle any of these clinical problems. However, each of the cases presented demonstrates an elegant use of laser technology in clinical practice. These articles cover the use of Er:YAG, Nd:YAG, and diode lasers for primarily soft tissue applications. In every case the authors have chosen the laser that they considered, from their understanding, to be the best one for the task at hand. We are all dental professionals, each with our own skills and experience. The common message that runs through all of the articles in this issue is that we must understand what we are doing in clinical dentistry in order to decide on the laser, or light source to use, and to interpret what is happening as we use it. Our education and experience together must guide us to do the very best that we can for the oral and general health of our patients. In conclusion, I looked back on my editorial from the last issue and I find it worth repeating the ending statement: We must all be continual learners and work out how to apply our learning to whatever we do each day. Please enjoy this issue of the journal. Feel free to e-mail me with suggestions, criticisms, or compliments at jdbf@ucsf.edu.
20 0 8 VO L 16 , N O . 1
Featherstone
C O V E R F E AT U R E
Supplementary Methods for Detection and Quantification of Dental Caries
Lena Karlsson, RDH; Sofia Tranus, DDS, PhD Department of Cariology and Endodontology, Institute of Odontology, Karolinska Institute, Huddinge, Sweden
J Laser Dent 2008;16(1):6-14
SYNOPSIS
This article reviews the modes of action and clinical application of novel caries detection methods including digital imaging fiber-optic transillumination, laser fluorescence, quantitative light-induced laser fluorescence, and alternating current impedance spectroscopy.
AB STR ACT
There is a need for objective instrumental caries detection methods to supplement traditional visual assessment by the clinician. These methods should be used as supplements to aid in making appropriate decisions about the clinical management of the individual lesion, such as whether to use invasive therapy or a more conservative, noninvasive approach. Objective, reliable, quantitative measures for longitudinal monitoring of lesion response to preventive measures would allow flexibility in selecting intervention appropriate to the individual patient, before lesion progression reaches a stage requiring invasive therapy. This paper reviews some novel and commercially available caries detection methods: FiberOptic Transillumination, Digital Imaging Fiber-Optic Transillumination, Laser Fluorescence, Quantitative Light-induced Fluorescence, and Electronic Caries Measurement.
INTRODUCTION
Our efforts to make the concept of caries prevention popular, and to preserve the dentition into old age are continuously successful.1-5 However, despite the dramatic decline in dental caries, particularly in industrialized countries and among children and young adults, the disease persists, albeit with highly skewed distribution.6-7 The following major changes have occurred in the pattern of the disease: progression of enamel caries is now slower, and allows preventive intervention before irreversible destruction of tooth substance. There is also a pronounced reduction in lesion development on the smooth surfaces, which are readily accessible to fluoride.8-11 Diagnostic techniques to support appropriate clinical decisions about management of the individual lesion, whether invasive therapy or a more conservative, noninvasive approach is indicated,12 are predominantly based on subjective interpretation of visual information: visual inspection, bitewing radiography, and the use of a dental explorer. Longitudinal monitoring of lesions has been hampered by the lack of appropriate diagnostic techniques,
JOU R NAL OF L ASER DENTI STRY
i.e., techniques of high sensitivity and specificity that reflect the slow lesion progression. The aim is to arrest or reverse the disease process, and to intervene before operative restorative dentistry is needed. Objective, reliable quantitative data on the outcome of this strategy, i.e., lesion response to preventive measures, would allow flexibility in selecting intervention appropriate for the individual patient, before lesion progression to a stage requiring expensive invasive therapy. Optimal dental care and treatment will increasingly involve a shift of emphasis and a change of the education and training of oral health personnel, and dental providers need to keep abreast of new approaches and technological advances for diagnoses and therapies of dental caries. In this context, there is a need for complementary methods for detection and quantification of dental caries. There are certain requirements that should to be met by the methods; they have to meet all safety regulations; detect early, shallow lesions; differentiate between shallow and deep lesions; give a low proportion of false positive readings; present data in a
20 0 8 VO L 16 , N O . 1
quantitative form so that activity can be monitored; be precise so that measurements can be repeated by several operators; be cost-effective and user-friendly. Clinically applicable methods for detection of a very early phase of mineral loss and quantification of caries lesions have emerged. In this paper, some novel and commercially available supporting caries detection methods will be summarized; FiberOptic Transillumination, Digital Imaging Fiber-Optic Transillumination, Laser Fluorescence, Quantitative Light-Induced
Karlsson and Tranus
C O V E R F E AT U R E
Figure 1: Clinical FOTI setup. There are several types of probes on the market. This illustrates a quite thick probe.
et al.,19 which showed low sensitivity (0.39) and high specificity (0.92), i.e., the risk for false positive observations was low, and the risk for missed carious lesions was high. There is a need for training and calibration of operators, but few clinical factors influence the readings. Clinical perspective: FOTI is essentially a refinement of traditional visual observation that can enhance caries detection by a trained and experienced clinician, but is not quantitative and has the same limitations as traditional visual methods for assessing lesion extent and following lesions over time. Digital Imaging Fiber-Optic Transillumination (DIFOTI) A recently marketed method based upon the same principles as FOTI is the digitized DIFOTI method. In this method the white light is delivered through an optical fiber via a specially designed handpiece that has a mirror on the opposite side of the tooth, thereby channelling the image back to a digital camera and visualizing the image on a monitor via a computer system. An ordinary computer setup with specially designed software creates a real-time image of the illuminated tooth on the computer screen. The images can be stored for later retrieval and comparative examination. Two disposable mouthpieces are available, one for proximal and one for occlusal surfaces, in an adult as well as a pediatric size. The DIFOTI method is still qualitative. Figure 2 shows a DIFOTI image of a molar occlusal surface. As can be seen tooth defects are readily visualized, such as the unusual morphology in this image. As with regular FOTI, the users level of experience is essential. Only limited research has so far been performed.20-22 Clinical perspective: The DIFOTI technique essentially picks
Figure 2: An occlusal surface on a molar, viewed through DIFOTI. The tooth is illuminated from the buccal surface. Dark areas around the fissures indicate caries lesions.
Fluorescence, and Electronic Caries Measurement.
TH E M ETHODS
Fiber-Optic Transillumination (FOTI) FOTI is a technique that uses light transmission through the tooth13-18 and has been available on the market for more than 40 years, in contrast to the other more novel methods described below that have only recently been developed. FOTI is based on the theory that demineralized dental hard tissues scatter and absorb light more than sound tissue. White, cold light is transmitted from a light source through an optical fiber to a handpiece with a thin probe that is applied to the tooth surface. Figure 1 shows the clinical FOTI setup. It detects and visualizes the caries lesions, so demineralized regions appear darker compared to the surrounding sound tissue, and the contrast between sound and carious tissue is then used for detection of lesions on occlusal, approximal, and smooth surfaces, on enamel as well as dentin. This technique relies on the human eye as the detector and is not quantitative. The majority of the FOTI studies show the same tendency as the well-performed in vitro study on occlusal surfaces by Grossman
up surface scattering of the visualizing light and readily indicates the presence of very early carious lesions, cracks, or imperfections in the tooth surface. From a clinical perspective, however, this information is very limited in its usefulness. The method gives no indication of lesion depth, severity, or progress over time, and cannot be used in the determination of how deep the lesion is and whether surgical intervention is necessary. This problem was highlighted in the recent study by Young and Featherstone.22 Laser Fluorescence (LF) When a caries lesion in enamel and dentin is illuminated with red laser light ( = 655 nm), organic molecules that have penetrated porous regions of the tooth, especially metabolites from oral bacteria, will create an infrared (IR) fluorescence. The enamel is essentially transparent to red light. The IR fluorescence is believed to originate from porphyrins and related compounds from oral bacteria. These molecules are chiefly responsible for the absorption of red light.23 The laser instrument, DIAGNOdent (DD) (KaVo Dental GmbH, Biberach, Germany), is based on research by Hibst and Gall,24 was introduced in the late 1990s, and is today marketed in two versions. Apart from smooth and occlusal surfaces, the latest version,
20 0 8 VO L 16 , N O . 1 JOU R NAL OF L ASER DENTI STRY |
Karlsson and Tranus
C O V E R F E AT U R E
JOU R NAL OF L ASER DENTI STRY
the DD-pen, also aims to readily access approximal surfaces. There is as yet limited information on the usefulness of the latter device. As described in a recent review by Hibst,23 red light from a 655-nm diode is transmitted through an optical fiber to a hand probe. This light beam is used to irradiate the tooth, with the red light transmitting readily through sound enamel. When the light reaches a carious lesion and interacts with appropriate organic molecules that have been absorbed into the porous structure, the light is re-emitted as invisible fluorescence in the nearinfrared region. The emitted light is channelled through the handpiece to a detector and presented to the operator as a digital number on a display (0-99). A higher number indicates more fluorescence and by inference a more extensive lesion below the surface. The first version of the LF device has shown good performance and reproducibility for detection and quantification of occlusal and smooth surface carious lesions in in vitro studies,25-27 but with somewhat more contradictory results in vivo, both in the primary and permanent dentition.28-34 It has also been tried for longitudinal monitoring of the caries process, and for assessing the outcome of preventive interventions.25,35-37 The DD-pen (Figure 3) might be a useful additional tool in detecting approximal caries, but has so far only been evaluated in three in vitro studies.38-40 Factors that may influence the outcome of the measurements in different ways are: presence of plaque, calculus and/or staining on the tooth surface,18,25 and the degree of dehydration of tooth tissue.26 The system detects fluorescent organic molecules that can be present in any surface deposits, thereby readily producing false positives. For measurements on occlusal surfaces, it is also of great importance that the tip is tilted over a range of several different angles to
Figure 3: Approximal measurement with the DIAGNOdent pen. The red laser light can be seen through the dental hard tissue.
access all relevant subsurface regions. Clinical perspective: The LF device is a useful adjunct to traditional visual examination, especially in occlusal surfaces, for the detection of hidden lesions below the surface. However, the device detects organic molecules that have penetrated into surface deposits or subsurface porosities, such as carious lesions. It does not directly detect demineralization. Results must be interpreted with caution by understanding how the device works and how false positive readings can be misleading. The digital number displayed indicates the amount of fluorescence, which is not necessarily a measure of lesion size or depth. Quantitative LightInduced Fluorescence (QLF) The phenomenon of tooth auto fluorescence has long since been suggested to be useful as a tool for the detection of dental caries.41 Fluorescence is a property of some manmade and natural materials that absorb energy at certain light wavelengths and emit
20 0 8 VO L 16 , N O . 1
light at longer wavelengths. An increased porosity due to a subsurface enamel lesion, occupied by water, scatters the light either as it enters the tooth or as the fluorescence is emitted, resulting in a loss of its natural fluorescence. Consequently the demineralized area appears opaque. The strong light scattering in the lesion leads to shorter light path than in sound enamel, and the fluorescence becomes weaker. Bjelkhagen and Sundstrm42 and later de Josselin de Jong et al.43 developed a technique based on this optical phenomenon, making the difference in fluorescence radiance between the carious and sound tooth structure quantitative. This has been termed quantitative light-induced fluorescence (QLF). The QLF method can readily detect lesions to a depth of approximately 500 m. on smooth and occlusal enamel surfaces. In the currently marketed systems (Inspector Pro, Inspektor Dental Care, Amsterdam, The Netherlands) the illumination system consists of a 50-Watt microdischarge arc lamp equipped with an optical bandpass filter with a peak intensity of 370 nm, transmitted through an optical fiber from the light source to a handpiece with a micro CCD video camera. A high-pass filter in front of the camera blocks the excitation light together with the ambient light, so
Figure 4: Principal setup of the Quantitative LightInduced Fluorescence method.
Karlsson and Tranus
C O V E R F E AT U R E
Figure 6: Clinical use of Electronic Caries Measurement (ECM).
JOU R NAL OF L ASER DENTI STRY
The QLF method has been tested in several in vitro,44-46 in situ,47 and in vivo43, 48-53 studies for smooth surface caries lesions. The possibility of adapting the QLF method for occlusal caries diagnosis is under investigation54-55 as well as modification for detection and quantification of secondary caries,56-58 but has yet to be tested clinically. Application for quantification of dental fluorosis has also been investigated.59 Higham et al.60 concluded QLF has the potential to detect, diagnose, and longitudinally monitor occlusal caries and provide useful information to the clinician with regard to the severity of the lesion and likely treatment. Eggertsson et al.61 reported good reproducibility of QLF methods clinically with inter- and intra-examiner reliability greater than 0.95 after training. Factors that may influence the outcome of the measurements are: presence of plaque, calculus and/or staining,62 ambient light, daylight or office light, and the degree of dehydration of tooth tissue.63 The newly designed handpieces on the commercially available devices have largely overcome the ambient light problems. Certain errors in the capturing stage of the method, such as differences in x- or y-axis, or rotation of the image, may be adjusted during the analytical stage of the method. The QLF method can also measure and quantify the red fluorescence (RF) from microorganisms in plaque. The RF observed in plaque can be of use when monitoring oral hygiene; removing infected dentin; detecting a leaking sealant or caries at the margin of a restoration. Two quantities are obtained, R (average change in red Figure 5: The analytical interface of the QLF method. fluorescence, %), and The lesion is color-coded so that the operator can get a area (mm2). So far there quick impression of the area and the depth. that only wavelengths above 520 nm are transmitted to the detector. Figure 4 shows the principal setup for the QLF-technique. The preferred image is captured and saved by the operator by pressing a foot switch, and is later processed. Details about the tooth and the surface examined are set in the program, and the position and orientation of the processed image is thereafter automatically stored in a preset pattern so that when the patient comes back on recall, a contour guides the operator to the right position again. The program offers an automatic repositioning facility, which can be set at any level, and when correlation between the reference image and the real-time image is satisfactory, it can be saved automatically. The fluorescence image is first converted into a black-and-white image so that thereafter the lesion site can be reconstructed by interpolating the grey level values in the sound enamel around the lesion. The difference between measured and reconstructed values gives three quantities: F (average change in fluorescence, %), lesion area (mm2), and Q (area x F), the latter giving a measure of the extent and severity of the lesion. Figure 5 shows the analytical part of the QLF method, as calculated by the specially designed software.
are a very limited number of studies performed with this feature.64 Clinical perspective: The QLF system that has recently come on the market (Inspektor Pro) in several countries can be used as a quantitative measure of enamel lesions in smooth surfaces. It is likely that is will also be useful for occlusal surfaces but this has yet to be proven. The sophisticated computer-driven repositioning feature enables lesion progression or arrestment to be followed over time. This system appears to be a useful adjunct to traditional visual examination. Electronic Caries Measurement (ECM) and Alternating Current Impedance Spectroscopy The ECM technique is based on the theory that sound dental hard tissue, especially the enamel, shows very high electrical resistance or impedance. Demineralized enamel becomes porous, and the pores fill with saliva, water, microorganisms, etc. The more demineralized the tissue, the lower the resistance becomes. In the impedance measurement system a circuit of a very weak alternating current is closed through the patient. From the device, a fiber leads to a probe, which is placed on the site that is to be measured.
| Karlsson and Tranus
20 0 8 VO L 16 , N O . 1
C O V E R F E AT U R E
10
JOU R NAL OF L ASER DENTI STRY
Figure 6 shows clinical use of an Electronic Caries Measurement device. The patient holds a groundunit in the hand, and from the ground-unit, a fiber leads back to the device. Compressed air that is led through the probe isolates the measuring site from the surrounding saliva. The result of the measurement is presented on a display as a number between 1 and 13, and the higher the number, the deeper the lesion. Site-specific measurements have been evaluated in a number of in vitro studies65-71 and in vivo studies.72-73 The reported sensitivity for ECM in detecting dentinal caries lesions of permanent premolar and molar teeth ranges from 0.93 to 0.95, and the specificity ranges from 0.53 to 0.70, in clinical studies, which gives a moderate risk for false positive readings, and a low risk of missed carious lesions. Surface-specific electrical conductance measurements have been investigated under in vitro conditions,74 which showed moderate sensitivity and specificity. Factors that may influence the outcome of the measurements are the degree of dehydration of tooth tissue,75 the degree of maturation of the enamel,76 and temperature variations.77 Another impedance/conductance-based method is Alternating Current Impedance Spectroscopy (ACIST). It is based on the same assumptions about electrical circuits and dental hard tissues as the ECM instrument. Apart from the forward conductance (resistance values, representing continuous conduction/diffusion pathways) it also measures transverse conductance (capacitative conductance pathways). This could give more information than the ECM.78-79 A commercially manufactured impedance measurement device has recently come on the market in the United Kingdom (CarieScan, IDMoS PLC, Dundee,
United Kingdom) and is likely to reach the United States in the near future. Clinical perspective: The electrical conductance or impedance measurement devices have had limited success in the past. The new ACIST system shows considerable promise as a method with good ability to detect lesions with a low level of false positives. However, the device gives a lesion/no lesion answer rather than an image, extent of the lesion, position of the lesion measure. This technique is likely to be a useful adjunct to traditional examination provided the clinician uses the information wisely in combination with other observations to determine an intervention or restorative treatment plan.
DISCUSSION
Quantitative dental caries detection methods may take subjective interpretations of visual, tactile, and radiographic methods to evidence-based clinical practice. A shift from traditional diagnostic methods to advanced and more sensitive methods will improve caries diagnostic routines and hence the dental care and treatment for our patients benefit: minimize the use of unavoidable hazards of ionizing radiation, detect caries in an early stage, obtain a more precise estimation of lesion depth and severity, reveal a dentinal lesion obscured by superimposed sound tissue, monitoring de- or remineralization, evaluate the outcome of different preventive strategies, and detect and quantify bacterial activity. The caries detection methods reviewed in this article meet general clinical needs and although significant promise is seen in these techniques, there is not enough evidence currently available to recommend any one of them as a substitute for conventional methods. However, each of them can be valuable in its own way, as
summarized above as a supplement to traditional methods. Each of the new methods reviewed brings additional information about lesions in a manner specific to the technology used. Nevertheless, traditional methods of caries assessment, which discriminate lesions at the cavitation stage, are not always clinically appropriate, and are obsolete for clinical research requiring detection of a very early phase of mineral loss, which allow a reduction in the duration of experimental periods and the number of subjects required, saving both time and money. To develop and test a new medical technical device is a long-term commitment; it takes time, scientific research, and evidence from the time of the first idea to a validated commercially available device, and even though laboratory findings show strong results, caution is indicated when extrapolating these into clinical conditions. The QLF method is today the most promising technology of those currently on the market, due to its close correlation to the enamel mineral content, but with limitations such as the inability to detect approximal (and occlusal) caries lesions, and dentinal caries. One of the upcoming methods and devices, based on different physical theories that is expected to appear on the market in the future is Optical Coherence Tomography (OCT) which can produce two- or threedimensional images of demineralized regions in dental enamel. When a tooth with a carious lesion is illuminated with infrared light at 1310 nm, OCT technology can produce a quantitative image of the subsurface lesion to the full depth of the enamel.80-81 The OCT method is, however, still yet far from a marketed device for everyday use in the dental office. All improvements require change, but not all change is improvement. Evidence-based care
20 0 8 VO L 16 , N O . 1
Karlsson and Tranus
C O V E R F E AT U R E
is by definition the conscientious, explicit, and judicious use of the current best evidence in making decisions about the care of individual patients, which includes integrating individual clinical expertise with the best available external clinical evidence.82 It is therefore important to emphasize the need for clinical trials to support critical appraisal and decision making in using these techniques, by theory and empirical evidence. In summary, there are several devices currently on the market and more to come that can be used by the clinician as valuable supplements to the traditional caries detection and assessment methods. All of the new methods require a basic understanding of how they work so that the results can be correctly interpreted for the benefit of the patient, especially to aid in the decision as to how to treatment plan, which lesions can be reversed, which chemical therapy should be used, how to assess success or not, and when to intervene with restorative work.
Disclosure: Lena Karlsson has received research funding from independent organizations including the Karolinska Institutet, the Swedish Patent Revenue Fund for Research in Preventive Dentistry, and the Swedish Dental Society. She has also received research funding or free use of technical devices from Inspektor Research Systems BV (The Netherlands), KaVo Scandinavia AB (Sweden), and KaVo Dental GmbH (Germany).
3. Marthaler TM. Changes in dental caries 1953-2003. Caries Res 2004;38(3):173-181. 4. Shay K. The evolving impact of aging America on dental practice. J Contemp Dent Pract 2004;5(4):101110. 5. Hugoson A, Koch G, Gthberg C, Helkimo AN, Lundin SA, Norderyd O, Sjdin B, Sondell K. Oral health of individuals aged 3-80 years in Jnkping, Sweden during 30 years (1973-2003). II. Review of clinical and radiographic findings. Swed Dent J 2005;29(4):139-155. 6. Vehkalahti M, Tarkkonen L, Varsio S, Heikkil P. Decrease in and polarization of dental caries occurrence among child and youth populations, 1976-1993. Caries Res 1997;31(3):161-165. 7. Petersen PE. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century The approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2003;31 Suppl 1:3-23. 8. Newbrun E. Preventing dental caries: Current and prospective strategies. J Am Dent Assoc 1992;123(5):68-73. 20 0 8 VO L 16 , N O . 1 JOU R NAL OF L ASER DENTI STRY | 9. Mejre I, Kllestl C, Stenlund H, Johansson H. Caries development from 11 to 22 years of age: A prospective radiographic study. Prevalence and distribution. Caries Res 1998;32(1):10-16. 10. Maupom G, Shulman JD, Clark DC, Levy SM, Berkowitz J. Toothsurface progression and reversal changes in fluoridated and nolonger-fluoridated communities over a 3-year period. Caries Res 2001;35(2):95-105. 11. Mejre I, Stenlund H, ZeleznyHolmlund C. Caries incidence and lesion progression from adolescence to young adulthood: A prospective 15-year cohort study in Sweden. Caries Res 2004;38(2):130-141. 12. Featherstone JDB. Prevention and reversal of dental caries: Role of low level fluoride. Community Dent Oral Epidemiol 1999;27(1):31-40. 13. Mitropoulos CM. The use of fibreoptic transillumination in the
AUTHOR B IOGR AP H I ES
Lena Karlsson is a registered dental hygienist and a PhD student at Karolinska Institute, Sweden. She works as a lecturer at the Institute of Odontology, unit of Cariology and Endodontics, and is involved in the dental hygienist and the dental student educational programs. In the late 1990s she began to undertake research in the field of diagnosis, prevention, and management of dental caries with a focus on the interaction between laser light and dental hard tissues, supervised by Professor Birgit Angmar-Mnsson. Today she is one of Dr. Sofia Tranuss doctoral students and her thesis work involves studies of different methods for detection and quantification of carious lesions at their earliest stages. She may be contacted by e-mail at lena.karlsson@ki.se.
Dr. Sofia Tranus is a senior lecturer in the Department of Odontology at the Karolinska Institute in Stockholm, Sweden. She has spent the past 10 years developing and testing new techniques for detection and quantification of dental caries. Dr. Tranus completed her PhD in 2002 at the Karolinska Institute, with her thesis entitled Clinical application of QLF and DIAGNOdent Two new methods for quantification of dental caries. Currently, she is on a temporary 2-year assignment at SBU The Swedish Council on Technology Assessment in Health Care. Dr. Tranus may be contacted by email at sofie.tranaeus@ofa.ki.se.
Disclosure: Dr. Tranus has received research funding from independent organizations including the Karolinska Institutet, the Swedish Patent Revenue Fund for Research in Preventive Dentistry, and the Swedish Dental Society. She has also received unrestricted research funding from Inspektor Research Systems BV (The Netherlands), KaVo Scandinavia AB (Sweden), and KaVo Dental GmbH (Germany).
R EER ENCES
1. Marthaler TM, chairman. Caries status in Europe and predictions of future trends. Caries Res 1990;24(6):381-396. 2. Marthaler TM, OMullane DM, Vrbic V. The prevalence of dental caries in Europe 1990-1995. ORCA Saturday afternoon symposium 1995. Caries Res 1996;30(4):237-255.
Karlsson and Tranus
11
C O V E R F E AT U R E
diagnosis of posterior approximal caries in clinical trials. Caries Res 1985;19(4):379-384. 14. Pine CM. Fibre-optic transillumination (FOTI) in caries diagnosis. In: Stookey G. Early detection of dental caries: Proceedings of the first annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 1996:51-65. 15. Vaarkamp J, ten Bosch JJ, Verdonschot EH, Bronkhoorst EM. The real performance of bitewing radiography and fiber-optic transillumination in approximal caries diagnosis. J Dent Res 2000;79(10):1747-1751. 16. Deery C, Care R, Chesters R, Huntington E, Stelmachonoka S, Gudkina Y. Prevalence of dental caries in Latvian 11- to 15-year-old children and the enhanced diagnostic yield of temporary tooth separation, FOTI and electronic caries measurement. Caries Res 2000;34(1):2-7. 17. Davies GM, Worthington HV, Clarkson JE, Thomas P, Davies RM. The use of fibre-optic transillumination in general dental practice. Br Dent J 2001;191(3):145-147. 18. Crtes DF, Ellwood RP, Ekstrand KR. An in vitro comparison of a combined FOTI/visual examination of occlusal caries with other caries diagnostic methods and the effect of stain on their diagnostic performance. Caries Res 2003;37(1):8-16. 19. Grossman ES, Cleaton-Jones PE, Crtes DF, Daya NP, Parak RB, Fatti LP, Hargreaves JA. Accurate diagnosis of occlusal carious lesions A stereo microscope evaluation of clinical diagnosis. SADJ 2002;57(6):215-220. 20. Vaarkamp J, ten Bosch JJ, Verdonschot EH, Tranus S. Quantitative diagnosis of small approximal caries lesions utilizing wavelength-dependent fibre-optic transillumination. J Dent Res 1997;76(4):875-882. 21. Schneiderman A, Elbaum M, Shultz T, Keem S, Greenebaum M, Driller J. Assessment of dental caries with Digital Imaging Fiber-Optic TransIllumination (DIFOTI): In vitro study. Caries Res
1997;31(2):103-110. 22. Young DA, Featherstone JDB. Digital imaging fiber-optic transillumination, F-speed radiographic film and depth of approximal lesions. J Am Dent Assoc 2005;136(12):1682-1687. 23. Hibst R. Detection of caries by DIAGNOdent: Scientific background and performance. J Laser Dent 2007;15(3):130-134. 24. Hibst R, Gall R. Development of a diode laser-based fluorescence caries detector. Caries Res 1998;32(4):294, abstract 80. 25. Lussi A, Imwinkelried S, Pitts N, Longbottom C, Reich E. Performance and reproducibility of a laser fluorescence system for detection of occlusal caries in vitro. Caries Res 1999;33(4):261-266. 26. Shi X-Q, Welander U, AngmarMnsson B. Occlusal caries detection with KaVo DIAGNOdent and radiography: An in vitro comparison. Caries Res 2000;34(2):151-158. 27. Shi X-Q, Tranus S, AngmarMnsson B. Validation of DIAGNOdent for quantification of smooth-surfaces caries: An in vitro study. Acta Odontol Scand 2001;59(2):74-78. 28. Rocha RO, Ardenghi TM, Oliveira LB, Rodrigues CR, Ciamponi AL. In vivo effectiveness of laser fluorescence compared to visual inspection and radiography for the detection of occlusal caries in primary teeth. Caries Res 2003;37(6):437-441. 29. Astvaldsdttir A, Holbrook WP, Tranus S. Consistency of DIAGNOdent instruments for clinical assessment of fissure caries. Acta Odontol Scand 2004;62(4):193198. 30. Tranus S, Lindgren LE, Karlsson L, Angmar-Mnsson B. In vivo validity and reliability of IR fluorescence measurements for caries detection and quantification. Swed Dent J 2004;28(4):173-182. 31. Bamzahim M, Aljehani A, Shi XQ. Clinical performance of DIAGNOdent in the detection of secondary caries lesions. Acta Odontol Scand 2005;63(1):26-30.
32. Angnes V, Angnes G, Batisttella M, Grande RH, Loguercio AD, Reis A. Clinical effectiveness of laser fluorescence, visual inspection and radiography in the detection of occlusal caries. Caries Res 2005;39(6):490-495. 33. Reis A, Mendes FM, Angnes V, Angnes G, Grande RH, Loguercio AD. Performance of methods of occlusal caries detection in permanent teeth under clinical and laboratory conditions. J Dent 2006;34(2):89-96. 34. Akarsu S, Kprl H. In vivo comparison of the efficacy of DIAGNOdent by visual inspection and radiographic diagnostic techniques in the diagnosis of occlusal caries. J Clin Dent 2006;17(3):53-58. 35. Lussi A, Megert B, Longbottom C, Reich E, Francescut P. Clinical performance of a laser fluorescence device for detection of occlusal caries lesions. Eur J Oral Sci 2001;109(1):14-19. 36. Anttonen V, Sepp L, Hausen H. A follow-up study of the use of DIAGNOdent for monitoring fissure caries in children. Community Dent Oral Epidemiol 2004;32(4):312-318. 37. Aljehani A, Yousif MA, AngmarMnsson B, Shi XQ. Longitudinal quantification of incipient carious lesions in postorthodontic patients using a fluorescence method. Eur J Oral Sci 2006;114(5):430-434. 38. Lussi A, Hack A, Hug I, Heckenberger H, Megert B, Stich H. Detection of approximal caries with a new laser fluorescence device. Caries Res 2006;40(2):97-103. 39. Aljehani A, Yang L, Shi XQ. In vitro quantification of smooth surface caries with DIAGNOdent and the DIAGNOdent pen. Acta Odontol Scand 2007;65(1):60-63. 40. Khnisch J, Bcher K, Hickel R. The intra/inter-examiner reproducibility of the new DIAGNOdent Pen on occlusal sites. J Dent 2007;35(6):509-512. 41. Benedict HC. The fluorescence of teeth as another method of attack on the problem of dental caries. J Dent Res 1929;9:274-275. 42. Bjelkhagen H, Sundstrm F. A clini-
12
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
Karlsson and Tranus
C O V E R F E AT U R E
cally applicable laser luminescence method for the early detection of dental caries. IEEE J Quant Electron 1981;17(12):2580-2582. 43. de Josselin de Jong E, Sundstrm F, Westerling H, Tranus S, ten Bosch JJ, Angmar-Mnsson B. A new method for in vivo quantification of changes in initial enamel caries with laser fluorescence. Caries Res 1995;29(1):2-7. 44. Hafstrm-Bjrkman U, Sundstrm F, de Josselin de Jong E, Oliveby A, Angmar-Mnsson B. Comparison of laser fluorescence and longitudinal microradiography for quantitative assessment of in vitro enamel caries. Caries Res 1992;26(4):241247. 45. Emami Z, Al-Khateeb S, de Josselin de Jong E, Sundstrm F, Trollss K, Angmar-Mnsson B. Mineral loss in incipient caries lesions quantified with laser fluorescence and longitudinal microradiography. A methodologic study. Acta Odontol Scand 1996;54(1):8-13. 46. Al-Khateeb S, ten Cate JM, AngmarMnsson B, de Josselin de Jong E, Sundstrm G, Exterkate RAM, Oliveby A. Quantification of formation and remineralization of artificial enamel lesions with a new portable fluorescence device. Adv Dent Res 1997;11(4):502-506. 47. Al-Khateeb S, Oliveby A, de Josselin de Jong E, Angmar-Mnsson B. Laser fluorescence quantification of remineralization in situ of incipient enamel lesions: Influence of fluoride supplements. Caries Res 1997;31(2):132-140. 48. Al-Khateeb S, Forsberg CM, de Josselin de Jong E, AngmarMnsson B. A longitudinal laser fluorescence study of white spot lesions in orthodontic patients. Am J Orthod Dentofacial Orthop 1998;113(6):595-602. 49. Ferreira Zandon AG, Isaacs RL, van der Veen M, Stookey GK. Indiana pilot clinical study of Quantitative Light Fluorescence. In: Stookey GK, editor. Early detection of dental caries II: Proceedings of the 4th annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 2000:219-230.
50. Tranus S, Al-Khateeb S, Bjrkman S, Twetman S, Angmar-Mnsson B. Application of quantitative lightinduced fluorescence to monitor incipient lesions in caries-active children. A comparative study of remineralisation by fluoride varnish and professional cleaning. Eur J Oral Sci 2001;109(2):71-75. 51. Tranus S, Shi X-Q, Lindgren LE, Trollss K, Angmar-Mnsson B. In vivo repeatability and reproducibility of the quantitative light-induced fluorescence method. Caries Res 2002;36(1):3-9. 52. Pretty IA, Ellwood RP. Comparison of paired visual assessment and software analyses of changes in caries status over 6 months from fluorescence images. Caries Res 2007;41(2):115-120. 53. Yin W, Feng Y, Hu D, Ellwood RP, Pretty IA. Reliability of quantitative laser fluorescence analysis of smooth surface lesions adjacent to the gingival tissues. Caries Res 2007;41(3):186-189. 54. Ferreira Zandon AG, Analoui M, Beiswanger BB, Isaacs RL, Kafrawy AH, Eckert GJ, Stookey GK. An in vitro comparison between laser fluorescence and visual examination for detection of demineralization in occlusal pits and fissures. Caries Res 1998;32(3):210-218. 55. Ando M, Eggertsson H, Isaacs RL, Analoui M, Stookey GK. Comparative studies of several methods for the early detection of fissure lesions. In: Stookey GK, editor. Early detection of dental caries II: Proceedings of the 4th annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 2000:279-299. 56. Hall AF, DeSchepper E, Ando M, Stookey GK. In vitro studies of laser fluorescence for detection and quantification of mineral loss from dental caries. Adv Dent Res 1997;11(4):507514. 57. Tranus S, de Josselin de Jong E, Lussi A, Angmar-Mnsson B. Quantitative light induced fluorescence for assessment of enamel caries around fillings: A pilot study. Caries Res 1997;31(4):324, abstract 132.
58. Gonzlez-Cabezas C, Fontana M, Gomes-Moosbauer D, Ando M, Analoui M, Stookey GK. Comparative studies of several methods for the early detection of secondary caries. In: Stookey GK, editor. Early detection of dental caries II: Proceedings of the 4th annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 2000:317-342. 59. Pretty IA, Tavener JA, Browne D, Brettle DS, Whelton H, Ellwood RP. Quantification of dental fluorosis using fluorescence imaging. Caries Res 2006;40(5):426-434. 60. Higham SM, Smith PW, Pretty IA. Development of an occlusal caries index for quantitative light-induced fluorescence (QLF). In: Stookey GK, editor. Early detection of dental caries III: Proceedings of the 6th annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 2003:195-212. 61. Eggertsson H, Ferreira-Zandon AG, Ando M, Gonzlez-Cabezas C, Fontana M, Martinez-Mier EA, Waskow-Chin JR, Jackson RD, Eckert GJ, Stookey GK, Zero DT. Reproducibility of in vitro and clinical examinations with QLF (Quantitative Light-Induced Fluorescence). Developing guidelines for imaging and analyzing QLF images, and a process for training examiners. In: Stookey GK, editor. Early detection of dental caries III: Proceedings of the 6th annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 2003:213-228. 62. Al-Khateeb S, Exterkate RAM, de Josselin de Jong E, AngmarMnsson B, ten Cate JM. Light-induced fluorescence studies on dehydration of incipient enamel lesions. Caries Res 2002;36(1):25-30. 63. Angmar-Mnsson B, Al-Khateeb S, Tranus S. Quantitative lightinduced fluorescence: Current research. In: Stookey GK, editor. Early detection of dental caries II: Proceedings of the 4th annual Indiana conference. Indianapolis: Indiana University, School of Dentistry, 2000:203-217. 64. van der Veen MH, Thomas RZ, Huysmans MC, de Soet JJ. Red auto-
Karlsson and Tranus
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
13
C O V E R F E AT U R E
fluorescence of dental plaque bacteria. Caries Res 2006;40(6):542-545. 65. White GE, Tsamtsouris A, Williams DL. Early detection of occlusal caries by measuring the electrical resistance of the tooth. J Dent Res 1978;57(2):195-200. 66. Verdonschot EH, Wenzel A, Truin GJ, Knig KG. Performance of electrical resistance measurements adjunct to visual inspection in the early diagnosis of occlusal caries. J Dent 1993;21(6):332-337. 67. Ricketts DN, Kidd EA, Liepins PJ, Wilson RF. Histological validation of electrical resistance measurements in the diagnosis of occlusal caries. Caries Res 1996;30(2):148-155. 68. Ekstrand KR, Ricketts DN, Kidd EA. Reproducibility and accuracy of three methods for assessment of demineralization depth of the occlusal surface: An in vitro examination. Caries Res 1997;31(3):224-231. 69. Ashley PF, Blinkhorn AS, Davies RM. Occlusal caries diagnosis: An in vitro histological validation of the Electronic Caries Monitor (ECM) and other methods. J Dent 1998;26(2):83-88. 70. Wicht MJ, Haak R, Sttzer H, Strohe D, Noack MJ. Intra- and interexaminer variability and validity of laser fluorescence and electrical resistance readings on
root surface lesions. Caries Res 2002;36(4):241-248. 71. Khnisch J, Heinrich-Weltzien R, Tabatabaie M, Stsser L, Huysmans MC. An in vitro comparison between two methods of electrical resistance measurement for occlusal caries detection. Caries Res 2006;40(2):104-111. 72. Rock WP, Kidd EAM. The electronic detection of demineralisation in occlusal fissures. Br Dent J 1988;164(8):243-247. 73. Verdonschot EH, Bronkhorst EM, Burgersdijk RCW, Knig KG, Schaeken MJM, Truin GJ. Performance of some diagnostic systems in examinations for small occlusal carious lesions. Caries Res 1992;26(1):59-64. 74. Huysmans MC, Longbottom C, Hintze H, Verdonschot EH. Surfacespecific electrical occlusal caries diagnosis: Reproducibility, correlation with histological lesion depth, and tooth type dependence. Caries Res 1998;32(5):330-336. 75. Yukizaki H, Kawaguchi M, Egashira S, Hayashi Y. Relationship between the electrical resistivity of enamel and the relative humidity. Connect Tissue Res 1998;38(1-4):53-57, discussion 73-79. 76. Schulte A, Gente M, Pieper K. Posteruptive changes of electrical resistance values in fissure enamel
of premolars. Caries Res 1999;33(3):242-247. 77. Huysmans MC, Longbottom C, Christie AM, Bruce PG, Shellis RP. Temperature dependence of the electrical resistance of sound and carious teeth. J Dent Res 2000;79(7):1464-1468. 78. Longbottom C, Huysmans MC, Pitts NB, Los P, Bruce PG. Detection of dental decay and its extent using a.c. impedance spectroscopy. Nat Med 1996;2(2):235-237. 79. Huysmans MC, Longbottom C, Pitts NB, Los P, Bruce PG. Impedance spectroscopy of teeth with and without approximal caries lesions An in vitro study. J Dent Res 1996;75(11):1871-1878. 80. Fried D, Xie J, Shafi S, Featherstone JD, Breunig TM, Le C. Imaging caries lesions and lesion progression with polarization sensitive optical coherence tomography. J Biomed Opt 2002;7(4):618-627. 81. Jones RS, Darling CL, Featherstone JD, Fried D. Imaging artificial caries on the occlusal surfaces with polarization-sensitive optical coherence tomography. Caries Res 2006;40(2):81-89. 82. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: What it is and what it isnt. BMJ 1996;312(7023):71-72.
14
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
Karlsson and Tranus
SCI ENTI F IC R EPORT
Effect of Er,Cr:YSGG Laser on Human Dentin Collagen: A Preliminary Study
Eleftherios-Terry Farmakis, DDS, MDSc, PhD1; Konstantinos Kozyrakis, DDS, PhD2; Evangelos G. Kontakiotis, DDS, PhD3; Kouvelas Nikolaos DDS, PhD4
1Fellow Researcher, Department of Endodontics, Dental School, University of Athens, Greece; 2Lecturer, Department of Endodontics, Dental School, University of Athens, Greece; 3Assistant Professor, Department of Endodontics, Dental School, University of Athens, Greece; 4Associate Professor, Dept of Pediatric Dentistry, Dental School, University of Athens, Greece. J Laser Dent 2008;16(1):15-20
SYNOPSIS
This article reports a study that illustrates how the collagen is affected during ablation of dentin by an Er,Cr:YSGG laser, at clinically relevant fluences.
AB STR ACT
Objective: The objective of this study was to determine the alterations of human dentin proteins (mainly collagen) following the use of an Er,Cr:YSGG laser. Materials & Methods: Fifteen human dentin sections were studied in three equal groups. Half of the surface was irradiated using an energy density of 88 J/cm2 for groups A and C, and 150 J/cm2 for group B. In addition, group C was etched for 15 seconds with 37% phosphoric acid. All sections were then immersed in 5% ninhydrin solution for 3 hours and then examined by light microscopy for collagen assessment. Results: In groups A and B the control untreated surfaces appeared in a blue-reddish color. In group A, the treated surfaces showed circular white areas surrounded by deep blue rings and under magnification the dentin appeared roughened and smear layer-free. In group B, the treated areas showed a roughened surface with no coloration. In group C, both the etched-only and the irradiated and etched surfaces showed a lighter coloration compared to control. Conclusions: From this preliminary study, it is suggested that there was a severe change in human dentin collagen and creation of a roughened dentin surface following the use of this laser. The higher the energy, the greater the effect. Fewer changes occurred after the use of etchant only.
INTRODUCTION
Since the discovery of lasers in 1960, much research has been done in order to investigate the interaction of lasers with the dental tissues.1-2 The early dental lasers for use with hard dental tissue applications often produced a charring effect. A few years ago, a Class IV Erbium Laser was cleared by the U.S. Food and Drug Administration (FDA) for use in dentistry. This type of laser (Er,Cr:YSGG) uses a crystal whose main element is erbium (a rare earth element), in addition to small portions of chromium, yttrium, scandium, gallium, and garnet. This crystal when irradiated emits a characteristic wavelength of 2780 nm that falls within the absorption band of water.3-5 One of the earlier possible explanations, proposed by the manufacturer, for the action of the Er,Cr:YSGG laser on dental hard tissues has to do with the interaction of this specific laser wavelength with the water spray of the laser handpiece. It has been suggested that when water droplets are introduced into the Er,Cr:YSGG laser beam, that the water droplets explode violently
Farmakis et al.
JOU R NAL OF L ASER DENTI STRY
outwards, due to the energy absorption, thus creating a plasma expansion which drives the water droplets to supersonic velocity. The expression of this phenomenon is a production of a pressure of 400 MPa and velocities up to 1000 m/sec from energized water droplets.6 When this stream of water jet is striking the target, it supposedly has enough power to dislodge material but with a very accurate cutting.7 It has been suggested that water is the cutting agent; and in addition that hard dental material that is dislodged, once incorporated into the stream, could act as abrasive particles, thus increasing the efficiency of the cutting field. This abrasive water jet (AWJ) is speculated to be capable of removing hard dental tissues but without the carbonization effect associated with other types of lasers, due to its indirect action. Actually, the temperature at the operating field is reduced,8-9 something that might be expected due to the cooling effect of water. However, it has recently been proposed that the action of the Er,Cr:YSGG laser is similar to the Er:YAG, since their wavelengths are similar (2780 nm for the
20 0 8 VO L 16 , N O . 1
15
SCI ENTI F IC R EPORT
16
JOU R NAL OF L ASER DENTI STRY
Er:YAG, 2940 nm for the Er,Cr:YSSG), both falling within the water absorption band. Accordingly they have similar absorption parameters in the hard dental tissues.10 The most recent explanation for its action is the interaction of this specific laser wavelength with hydrated dentin. Since this wavelength is absorbed very well by the water content of dentin and also by the hydroxyapatite mineral, the water is heated and finally vaporized; the vapors remain inside the dental tissues until the pressure building up in the dental hard tissues is enough to disrupt their integration, causing micro-explosions, thereby ejecting dentin particles (water-induced ablation).11 In cavity preparations made by dental burs, bonding of resin to enamel is achieved via micromechanical retention on the roughened surface, whereas the retention to dentin is based mainly on the hybrid layer formation and to a lesser degree to the micromechanical retention offered by the resin tags embedded in dentin.12-13 In cavities prepared by Er,Cr:YSGG lasers, the associated microroughness on both enamel and dentin does not require a change of approach to resin bonding to the enamel. However, the resulting alteration of collagen may lead to the formation of an inferior hybrid layer zone due to incomplete penetration of the collagen fibrils by the hydrophilic primers and resin monomers.14 In this case, the resin-dentin bond is favored by resin tag formation.15 The objective of this work was to investigate the possible alterations of human dentin proteins (mainly collagen) following irradiation by an Er,Cr:YSGG laser under different clinically relevant settings. These changes in dentin could affect the hybrid layer formation and the subsequent dentin bonding to resin composite restorative materials.
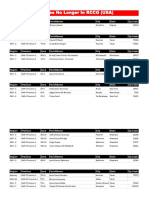
Table 1: Er,Cr:YSGG laser parameters based on the manufacturer* recommendation for treating dentin and enamel
Parameter Power Pulse Energy Frequency Energy Density Dentin 3.5 Watts 175 mJ 20 Hz 88 J/cm2 Enamel 6 Watts 300 mJ 20 Hz 150 J/cm2
*Millennium, Biolase Technology, Inc., San Clemente, Calif., USA
M AT E R I A L S A N D M ETHODS
Fifteen standardized dentin sections (each 2 mm thick) were prepared from sound human molars that had been stored in sterile saline, until they were used. From each tooth, a single disc was obtained by using a low-speed saw (IsoMet, Buehler Ltd., Lake Bluff, Ill., USA) under tap water cooling. The cutting plane was parallel to the occlusal surface of the tooth and in most cases the sections did not interfere with the pulp horns. A groove was made on one side of each section, dividing the surface into two parts. Finally the sections were randomly distributed into three groups. The Er,Cr:YSGG laser handpiece (Millennium, Biolase Technology, Inc., San Clemente, Calif., USA) was securely mounted on a stand so the beam would fall vertically on the section surface at a distance of 5 mm from the end of the tip. The sapphire tip used was 0.7 mm in diameter. Then each section was mounted on a microscope observation glass slide and moved manually at a rate of approximately 5 mm/sec in a sweeping motion, simulating the hand movement during cavity preparation. In groups A and B, one half of each section surface was treated with the settings suggested by the manufacturer for treating dentin and enamel respectively. Settings and calculated energy densities are shown in Table 1. Groups A and C were irradiated at 88 J/cm2, and Group B at 150 J/cm2. In group C, half of the surface
Figure 1: A typical deep blue-reddish appearance of control dentin area after the use of 5% aqueous ninhydrin solution
20 0 8 VO L 16 , N O . 1
Figure 2: A laser-treated specimen using the settings for dentin (Group A) after the use of 5% aqueous ninhydrin solution
was treated with dentin-treating laser irradiation settings and then both halves (the whole surface) were etched for 15 seconds with 37% phosphoric acid (Enamel Prep Etching Gel, Ivoclar Vivadent A.G., Schaan, Liechtenstein) applied by a disposable brush. This procedure was repeated on all five sections of group C, simulating the etching procedure that usually takes place before the use of composite resin filling materials along with the use of priming and bonding agents. The main question was: Do all or any of these procedures affect
Farmakis et al.
SCI ENTI F IC R EPORT
Figure 3: A laser-treated specimen using the settings for dentin (Group A) after the use of 5% aqueous ninhydrin solution (100X magnification)
Figure 5: Roughened dentin surface after laser irradiation with the settings for treating dentin (Group A, 500X magnification)
Figure 4: A laser-treated specimen using the settings for dentin (Group A) after the use of 5% aqueous ninhydrin solution (200X magnification)
Figure 6: Roughened dentin surface after laser irradiation with the settings for treating dentin (Group A, 1000X magnification). The absence of smear layer is noticeable
R E S U LT S
All control areas of groups A and B, plus the back side of all sections (groups A, B, and C), had the same appearance: deep blue-reddish color, demonstrating that after dentin was cut with a diamond saw, free -amino and carboxyl groups were exposed, originating mainly from the dentin collagen (Figure 1).
Farmakis et al.
JOU R NAL OF L ASER DENTI STRY
dentin collagen, and to what extent? The chosen method for monitoring was the use of 5% ninhydrin solution. Ninhydrin [2, 2-dihydroxy-1H-indene-1, 3(2H)-dione or 2,2-dihydroxy-1,3-indanedione] (Merck & Co, Inc., Whitehouse Station, N.J., USA) comes as a monohydrate molecule, forming pale yellow prisms that freely dissolve in water, producing a yellow-colored solution.16 When used as a reagent, upon the presence of free -amino acids and carboxyl groups (which in this case come from human dentin proteins, mainly collagen), it yields a bluereddish color. The degree of coloration is not only a qualitative method but it can also become a semi-quantitative one with the use of a spectroscope. Thus, changes
can be precisely detected and measured, compared to a control of a given substrate.16 After all procedures were completed, according to the protocol, all sections were embedded in 5% aqueous ninhydrin solution for 3 hours. Then all sections were examined by light microscopy (50X up to 1000X magnification) and photographs were taken.
In the laser-irradiated area of group A macroscopically, the treated area looked pitted (Figure 2). At 100X (Figure 3) and 200X magnification (Figure 4), small circular craters were observed, which were white centrally, and surrounded by deep blue rings. At higher magnification (500X), the dentin surface was observed to be roughened (Figure 5), and at 1000X magnification appeared to be smear layer-free (Figure 6). In the laser-irradiated area of group B, macroscopically, a generally roughened dentin with no coloration was observed (Figure 7). At higher magnification (500X), the surface appeared aggressively roughened compared to the treated area of group A, but the surface was smear layer-free (Figure 8). In the sections of group C, both
20 0 8 VO L 16 , N O . 1
17
SCI ENTI F IC R EPORT
the etched-only and the irradiated/etched areas appeared similar in coloration: not as densely colored as the control area (Figure 9). In the areas that were both laser-irradiated and etched (500X), the surface appeared to be like the laser irradiation-only group, only much smoother, with the residuals of the etching procedure apparent in some areas (Figure 10).
DISCUSSION
Earlier studies with other types of lasers showed carbonizations along with crack lines due to thermal effects during the treatment of dental hard tissues.1-2 The erbium laser energy is primarily absorbed by the water molecules, converted into kinetic energy, resulting in no carbonization of the irradiated
surface and no thermal damage to pulp with clinically relevant energy levels. In this study, the observation that the treated dentin surfaces were smear layer-free was in agreement with other studies.17-18 Collagen alteration was directly related to the energy level used. At the higher energy level studied, more alteration of collagen was observed. Collagen alterations were similarly observed on the surfaces following etching. Other studies that examined the alteration of dentin collagen after acid etching reported a denaturation of collagen,17 a removal of peptides, changes in collagen conformation in situ, and a collapse of the
20 0 8 VO L 16 , N O . 1
Figure 7: A laser-treated dentin specimen using the laser settings for enamel (Group B) after the use of 5% aqueous ninhydrin solution
Figure 9: A dentin specimen of which half of the surface was treated with the settings for dentin (Group C) and then the whole surface was etched with 37% phosphoric acid (Group C) after the use of 5% aqueous ninhydrin solution
fibrils.19 This dentin surface change, prior to bonding agent application, did not seem to negatively affect the formation of a sound hybrid layer. In our study the condition of collagen fibrils of acid-etched or laser-treated dentin was not tested. More research is needed to evaluate the morphological and structural changes of the remaining collagen and the quality of the resulting hybrid layer after the use of this laser under the clinically relevant parameters used. When the lower energy settings were used, the creation of each crater was the effect of internal explosion of vapors inside the dentin. It looked as though in the center of each crater, along with the dentin removal, there was an area that was free from -amino and carboxyl groups, while at the periphery there were remains of collagen. This could be explained by the Gaussian profile distribution of the pulse energy.20 At the higher power settings the treated dentin surface appeared to be collagenfree, and cracked hydroxyapatite crystals remained, giving a rough surface appearance. This roughened surface might not need additional acid etching to achieve a good bond with composite resin filling systems,21 although other studies showed that acid etching,
JOU R NAL OF L ASER DENTI STRY
Figure 8: Roughened dentin surface after laser irradiation with the settings for treating enamel (Group B, 500X magnification) demonstrating the absence of a smear layer
Figure 10: Appearance of laser-irradiated and etched dentin (Group C, 500X magnification) demonstrating a smooth and smear layer-free surface
18
Farmakis et al.
SCI ENTI F IC R EPORT
CO N C LU S I O N
The Er.Cr:YSGG laser, when used on dental hard tissues, may be slow on enamel, but works well on dentin. This study demonstrated that the remaining treated dentin surface is microroughened, smear layer-free, and free of -amino and carboxyl groups, indicating complete removal of collagen. Clinical Relevance Statement: Further investigations should be continued to determine whether the existing adhesives and resin composite filling systems are in harmony with Er,Cr:YSGG laser
4. Vodopyanov KL. Bleaching of water by intense light at the maximum of the 3 micron absorption band. Sov Phys J Exp Theor Phys 1990;70:114121. 5. Hale GM, Querry MR. Optical constants of water in the 200-nm to 200-micrometer wavelength region. Appl Optics 1973;12(3):555-563. 6. Kimmel Al, Rizoiu IM, Eversole LR. Phase Doppler particle analysis of laser-energized exploding water droplets. In: International Laser Congress, September 25-28, 1996, Athens, Greece, abstract 67. 7. Clarkson DM. A review of technology and safety aspects of erbium lasers in dentistry. Dent Update 2001;28(6):298-302.
Farmakis et al.
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
following erbium laser irradiation, should not be omitted.14, 22-23 On the laser-irradiated and etched area there were two observations of particular interest. First, the color was identical to the color of the etched-only surface. Obviously, the laser-irradiated surface was affected by acid etching. The acid removed the free -amino and carboxyl group zone and the cracked hydroxyapatite crystal structures, exposing the collagen underneath toward the surface. The second finding agrees with this hypothesis because under magnification the laser-irradiated and etched surfaces appeared smoother when compared to the laser treatment-only surface, meaning that the acid demineralized the hydroxyapatite crystals that roughened the surface. The question is whether or not this micromechanical roughness following laser treatment is stable and stiff enough for better adhesion. Additional studies are needed to answer these questions. Since there was no difference on the opposite sides of treated and control areas, it was assumed that both energy levels (88 and 150 J/cm2) were safe for the pulp tissue when there is a 2 mm dentinal wall thickness. These findings are in accordance with the findings of other researchers.24
ablation of dentin, or whether new methods and materials should be developed to suit laser applications for hard dental tissues. When the Er,Cr:YSGG laser is used for cavity preparation, the remaining surface is smear layer-free.
AUTHOR B IOGR AP H I ES
Dr. Eleftherios-Terry Farmakis completed his Undergraduate and Postgraduate studies (MDSc and PhD) in Dentistry at the University of Athens, Greece. He specialized in Endodontics and is a member of Greek Endodontic Society (EEE), American Association of Endodontists (AAE), and International Association for Dental Research (IADR). He has several fields of interest, and one of them is lasers in dentistry. Dr. Farmakis can be reached at elefarm@dent.uoa.gr. Dr. Kostas Kozyrakis received both his dental degree and his PhD diploma from the Dental School, University of Athens, Greece, where he serves as a lecturer in the Department of Endodontics. He is a member of the Academy of Laser Dentistry (ALD), the European Society of Oral Laser Applications (ESOLA), and the Hellenic Society of Oral Laser Applications. He has attained the Standard Proficiency status for Er:YAG, diode, and Nd:YAG lasers from the Academy of Laser Dentistry and that of the Second Module of the European Association of Oral Laser Applications. Dr. Kozyrakis presently utilizes tan Nd:YAG laser mainly for endodontic applications, and he is involved with seminars for the Applications of Lasers in Dentistry to Greek Dentists. He has done research concerning the Er:YAG and Nd:YAG applications in dentistry. Dr. Evangelos Kontakiotis received both his dental degree and his PhD diploma from the Dental School, University of Athens, Greece, where he serves as an Assistant Professor in the
Department of Endodontics. He has published more than 80 articles, some of which are in the laser field. Dr. Nikos Kouvelas received his dental degree and PhD from the Dental School, University of Athens, Greece and completed his Pediatric Dentistry specialty in Toronto, Canada. Dr. Kouvelas is an Assistant Professor in the Department of Paediatric Dentistry, Dental School, University of Athens, Greece, and is a member of ESOLA.
Disclosure: The authors have no financial affiliation with any dental laser manufacturer. The research was presented at the 1st Congress of European Society for Oral Laser Application (ESOLA) May 2001, Vienna, Austria.
R EF ER ENCES
1. Goldman L, Gray JA, Goldman J, Goldman B, Meyer R. Effect of laser beam impacts on teeth. J Am Dent Assoc 1965;70(3):601-606. 2. Lobene RR, Bhussry BR, Fine S. Interaction of carbon dioxide laser radiation with enamel and dentin. J Dent Res 1968;47(2):311-317. 3. Walsh JT Jr, Cummings JP. Effect of the dynamic optical properties of water on midinfrared laser ablation. Lasers Surg Med 1994;15(3):295305.
19
SCI ENTI F IC R EPORT
8. Glockner K, Rumpler J, Ebeleseder K, Stdtler P. Intrapulpal temperature during preparation with the Er.YAG laser compared to the conventional burr: An in vitro study. J Clin Laser Med Surg 1998;16(3):153-157. 9. Rizoiu I, Kohanghadosh F, Kimmel AI, Eversole LR. Pulpal thermal responses to an erbium,chromium:YSGG pulsed laser hydrokinetic system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86(2):220-223. 10. Coluzzi DJ. Fundamentals of dental lasers: Science and instruments. Dent Clin North Am 2004;48(4):751770. 11. Moritz A. Oral laser application. Berlin: Quintessenz Verlags-GmbH, 2006:86-88. 12. Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Van Landuyt K, Lambrechts P, Vanherle G. Buonocore memorial lecture. Adhesion to enamel and dentin: Current status and future challenges. Oper Dent 2003;28(3):215-235. 13. Gilpatrick RO, Ross JA, Simonsen RJ. Resin-to-enamel bond strengths with various etching times. Quintessence Int 1991;22(1):47-49. 20 0 8 VO L 16 , N O . 1
14. Sassi JF, Chimello DT, Borsatto MC, Corona SAM, Pecora JD, PalmaDibb RG. Comparative study of the dentin/adhesive systems interface after treatment with Er:YAG laser and acid etching using scanning electron microscope. Lasers Surg Med 2004;34(5):385-390. 15. Ceballos L, Toledano M, Osorio R, Tay FR, Marshall GW. Bonding to Er-YAG-laser-treated dentin. J Dent Res 2002;81(2):119-122. 16. Budavari S, editor. The Merck index: An encyclopedia of chemicals, drugs, and biologicals. Rathway (NJ): Merck & Co., Inc., 1989:1036-1037. 17. Lin S, Caputo AA, Eversole LR, Rizoiu I. Topographical characteristics and shear bond strength of tooth surfaces cut with a laserpowered hydrokinetic system. J Prosthet Dent 1999;82(4):451-455. 18. Tokonabe H, Kouji R, Wantanabe H, NakamuraY, Matsumoto K. Morphological changes of human teeth with Er:YAG laser irradiation. J Clin Laser Med Surg 1999;17(1):7-12. 19. Eliades G, Palaghias G, Vougiouklakis G. Effect of acidic conditioners on dentin morphology, molecular composition and collagen
conformation in situ. Dent Mater 1997;13(1):24-33. 20. Moritz A. Oral laser application. Berlin: Quintessenz Verlags-GmbH, 2006,:105-107. 21. Moritz A, Schoop U, Goharkhay K, Szakacs S, Sperr W, Schweidler E, Wernisch J, Gutknecht N. Procedures for enamel and dentin conditioning: A comparison of conventional and innovative methods. J Esthet Dent 1998;10(2):84-93. 22. Ceballos L, Osorio R, Toledano M, Marshall GW. Microleakage of composite restorations after acid or Er-YAG laser cavity treatments. Dent Mater 2001;17(4):340-346. 23. Dunn WJ, Davis JT, Bush AC. Shear bond strength and SEM evaluation of composite bonded to Er:YAG laser-prepared dentin and enamel. Dent Mater 2005;21(7):616-624. 24. Eversole LR, Rizoiu I, Kimmel AI. Pulpal response to cavity preparation by an erbium,chromium:YSGG laser-powered hydrokinetic system. J Am Dent Assoc 1997;128(8):10991106.
20
JOU R NAL OF L ASER DENTI STRY
Farmakis et al.
CLI N IC AL C ASE STU DI ES
Advanced Proficiency Case Studies
Charles Hoopingarner, DDS; Steven Parker, BDS, LDS, RCS, MFGDP; and Mary Lynn Smith, RDH were the three most recent recipients of Advanced Proficiency during the Academy of Laser Dentistrys 2007 Annual Conference in Nashville, Tennessee. This issue of the Journal will continue to feature cases from these clinicians. Ms. Smith treats a patient with chronic generalized periodontitis. Her therapy includes the adjunctive use of an Nd:YAG laser after scaling is completed with conventional instrumentation. The 1064-nm wavelength is indicated for the removal of the diseased epithelial lining of the periodontal pocket, and thus can be a good addition to the protocol for the initial treatment of the disease. Dr. Parker presents two cases utilizing an 810-nm diode laser. The first case involves soft tissue crown lengthening, uncovering two implant fixtures, and a frenectomy, in preparation for a final fixed bridge. The second case depicts a patient who presents with multiple hemorrhagic lesions caused by trauma on the lower lip. In both treatment plans, the diode laser offers excellent hemostatic assistance during the procedures. Dr. Hoopingarner treats a patient who desired a more esthetic smile. The treatment plan includes soft tissue crown lengthening, closed flap osseous crest removal, and a maxillary frenectomy all of which will reestablish a favorable biologic width after the periodontal tissues are modified. He uses an Er:YAG laser for all of the surgical procedures, demonstrating that wavelengths ability to precisely contour both hard and soft oral tissue. The excellent results shown in these four cases demonstrate how different laser wavelengths can be successfully utilized by the competent practitioner.
Nd:YAG Laser-Assisted Treatment of Moderate Chronic Periodontitis Mary Lynn Smith, RDH McPherson, Kansas Use of an 810-nm Diode Laser in a Combined Gingivoplasty, Frenectomy, and Second-Stage Implant Recovery Procedure Steven Parker, BDS, LDS RCS, MFGDP Harrogate, North Yorks, Great Britain Establishing a Maintainable Esthetic Gingival Smile Line with an Er:YAG Laser Charles R. Hoopingarner, DDS Houston, Texas Use of an 810-nm Diode Laser in the Treatment of Multiple Hemangiomata of the Lip Steven Parker, BDS, LDS RCS, MFGDP Harrogate, North Yorks, Great Britain
22
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
CLINICAL CASE
Nd:YAG Laser-Assisted Treatment of Moderate Chronic Periodontitis
Mary Lynn Smith, RDH; McPherson, Kansas
J Laser Dent 2008;16(1):23-29
SYNOPSIS
This article describes treatment of chronic generalized periodontitis including adjunctive use of an Nd:YAG laser.
P R E T R E AT M E N T
A. Diagnostic Tests 1. Full Clinical Description A 58-year-old Caucasian male presented for routine dental prophylaxis (Figure 1). He expressed no chief complaints. His last dental visit was seven months prior. There were previously diagnosed periodontal and restorative concerns. During the hygiene appointment, the health history was reviewed and tissues visually screened for signs of oral cancer. Comprehensive restorative, periodontal, and radiographic exams were completed. Micro-ultrasonic scaling, biofilm removal, and coronal polishing were performed as well. The patient was educated concerning his oral health and probable progression of untreated disease. The health history revealed he had experienced shortness of breath occasionally, seasonal allergies, episodes of anxiety, and arthritis. The patient was not taking any medications other than over-the-counter pain relievers when needed. He has been treated for anemia and asthma in the past. A recent cardiovascular system evaluation revealed good health. There were no contraindications to treatment. Occlusion was Angles Class I on the right, while on the left it was a super Class I. He experienced fatigue in the TMJ with prolonged joint stress. The moderate-to-severe wear pattern of
Figure 1: Preoperative view at presentation
3. Soft Tissue Status The gingiva was inflamed from plaque and calculus located above and below the gingival margin. A complete six-point periodontal
Smith
JOU R NAL OF L ASER DENTI STRY
incisal edges indicated probable bruxism. He was missing teeth #1, 8, 16, 17, and 32. Teeth #7 and 9 had drifted mesially. Teeth #4, 14, and 30 were treated endodontically and restored with porcelain-fusedto-metal (PFM) crowns. Tooth #13 had root canal therapy but was left with a large filling, no crown, and was compromised with a mesial fracture. Amalgam fillings were present in teeth #5, 15, and 18. Tooth #15 had a fractured filling with mesial decay. Decay was noted on the distal aspect of tooth #18. The patient had been monitored by an oral surgeon since 2002 when a squamous dentigerous cyst with reactive granulomatous inflammation in the right mandible near the TMJ was removed. Radiographically, it appeared to have residual or scar tissue remaining. Three weeks before this appointment the patient saw an oral surgeon for evaluation of the site of the cyst and extraction of tooth #17. The patient was still experiencing jaw and neck discom-
fort from the extraction but was improving daily. The lower anterior teeth were extremely crowded and retained plaque. The gingiva was inflamed from plaque and calculus located above and below the gingival margin. Periodontal pocketing of 2 to 4 mm was present in the posterior regions of all quadrants and the lower anterior region. Areas of recession exposing 1 to 2 mm of root surface were present as well. Class I furcations were noted on teeth #2, 15, 18, 19, 30, and 31. 2. Radiographic Examination A panoramic radiograph was taken 2 years prior (Figure 2). A radiographic full-mouth series was taken to assess current bone loss and possible caries (Figure 3a). Additional radiographs were taken of the area distal to tooth #31, where a cystic structure was noted (Figure 3b). Tooth #24 exhibited a widened periodontal ligament most likely due to occlusal trauma. Radiographs revealed distal decay on tooth #18. Caries on the mesial aspect of tooth #15 was not detected radiographically. Generalized moderate horizontal bone loss in the posterior was noted.
20 0 8 VO L 16 , N O . 1
23
CLINICAL CASE
revealed generalized chronic periodontitis. An oral cancer screening revealed a 4-mm venous lake lower lip left of the midline and an amalgam tattoo on attached mucosa distolingual to tooth #14.
24
JOU R NAL OF L ASER DENTI STRY
4. Hard Tissue Status Occlusion classification was Angles Class I on the right and Figure 2: Panoramic radiograph taken super Class I on the left with two years prior to presentation severe crowding of lower anteFigure 3: Preoperative radiographs rior teeth (Figure 5) Missing teeth were #1, 8, 16, 17, and 32 2. Treatment Plan Outline Mesial a. Restorative treatment to include: drifting noted tooth #13 crown; #15 caries on teeth #7 removal and crown or fourand 9 surface filling; #18 caries Attrition noted on Figure 3a: Full-mouth radiographs taken at initial appointment teeth #6, 7, 9, 10, 11, 13, 20, 21, 22, 23, 24, 25, and 27 Significant fracture noted on tooth #15 amalgam and #13M tooth structure Endodontically treated Figure 3b: Additional film of lower right area indicating possible cyst teeth #4, 13, 14, and 30; all other teeth probing was performed with 5 mm as Figure 4: Initial periodontal probing chart vital the greatest pocket depth. Decay noted on teeth #15M, 18D Generalized bleeding was evident Existing restorations: PFM and moderate subgingival calculus crowns on teeth #4, 14, 30; present. Recession of 1 to 2 mm was amalgam fillings on teeth #5, 15, noted on teeth #3, 5, 6, 11, 12, 13, and 18; composite fillings on teeth 20 buccal and #14, 24, and 26 lingual. #13, 15, and 18 Class I furcation involvements are noted on buccal surfaces of teeth #2, 5. Other Tests 15, 18, 19, and 31, and the lingual TMJ fatigue is experienced with surface of #30. No mobility was prolonged joint stress. detected. Figure 4 shows the preoperFigure 5: Occlusal view of mandibular ative probe chart. The examination anterior area showing crowding
B. Diagnosis and Treatment Plan 1. Diagnoses Provisional diagnosis: Generalized chronic periodontitis Doctors final diagosis: Soft tissue: Moderate generalized chronic periodontitis Hard Tissue: Teeth #15MOBL and 18DOB caries Parafunction with excessive wear of anterior teeth Cyst in the right mandible is being monitored by oral surgeon, currently considered nonprogressing and nonpathogenic.
20 0 8 VO L 16 , N O . 1
Smith
CLINICAL CASE
Smith
JOU R NAL OF L ASER DENTI STRY
removal and a three-surface filling. an appliance to prevent further attrition from bruxing is indicated. Referral to oral surgeon for follow-up on cyst. possible long-term plans include extracting tooth #24 or 25 (depending on prognosis) to re-align teeth orthodontically, and replace tooth #8 with a three-unit bridge or implant. b. Active phase-I periodontal infection therapy to include four periodontal infection therapy appointments, one hour each and scheduled approximately a week apart: assessment of patients plaque management, refining techniques and continuing motivation for thorough daily care micro-ultrasonic instrumentation and hand instrumentation for biofilm and calculus removal laser soft tissue decontamination and superficial coagulation intraoral photographs c. Six-week post-therapy re-infection assessment appointment to include: one appointment for 30 minutes health history review visual evaluation of tissue rehabilitation assessment of patients plaque management, refining techniques and continuing motivation for thorough daily care intraoral photographs micro-ultrasonic biofilm removal at gingival third of tooth probing and sulcular instrumentation is avoided in order to allow undisturbed maturation of connective tissue at the base of the pocket d. Twelve-week post-therapy appointment to include: health history review oral cancer screening
periodontal charting to assess rehabilitation assessment of patients plaque management, refining techniques and continuing motivation for thorough daily care micro-ultrasonic instrumentation for full-mouth bacterial decontamination coronal polishing laser decontamination of unresolved areas intraoral photos determination of recare interval. 3. Indications for Treatment Treatment is indicated to halt the periodontal destruction and rehabilitate the affected tissues. Periodontal infection therapy must include removal of biofilm and calculus from the root surfaces through scaling. The Nd:YAG laser furthers decontamination of the pocket by addressing the periodontal pocket wall. The 1,064-nm laser wavelength is highly absorbed in melanin and hemoglobin. Both of these chromophores are present in inflammatory tissue. Laser-tissue interaction reduces pathogens in the pocket and coagulates hemorrhaging sites, assisting the bodys healing response. This laser enhances the bodys healing process by reducing bacterial counts and achieving superficial coagulation. 4. Contraindications for Therapy and Precautions There are no contraindications for this patient to receive laserassisted treatment of periodontal disease with the Nd:YAG laser. Laser safety precautions were followed for protection of the patient and clinician. The energy from the Nd:YAG laser must be directed toward the soft tissue and away from the tooth and bone.
5. Treatment Alternatives No treatment and progression of disease, eventual tooth loss and systemic impact Conventional scaling and root planing Placement of localized antimicrobials or antibiotics with possible reactions Periodontal surgery. 6. Informed Consent After being educated in the progression of untreated periodontal disease and treatment options, the patient gave verbal and written consent to proceed with the planned therapy. This is documented in the patients record.
T R E AT M E N T
A. Restorative Treatment Objective Restorative treatment: Caries removal from teeth #15 and 18 with composite restorations of #15 on the MOBL surfaces and #18 on the DOB surfaces. A referral to an oral surgeon was made for followup on the cyst. Other restorative needs were discussed and will be treated in phases at the completion of periodontal therapy. B. Periodontal Treatment Objective The treatment objectives are to halt the destruction of the periodontium due to disease processes. Laserassisted periodontal treatment will reduce bacterial load in the periodontal pocket wall, eliminating the related inflammatory response by the body. The Nd:YAG laser wavelength is well absorbed in pigmented and hemoglobin-rich inflamed tissue. Signs of healing, such as decreased probing depths, elimination of hemorrhaging, and normal tissue coloration and texture, are desired. The appointments are designed to provide the patient with customized education in specific daily plaque management techniques, ensuring maximum rehabilitation of the tissues.
20 0 8 VO L 16 , N O . 1
25
CLINICAL CASE
Figure 8: Tooth #3 procedure
Figure 6: Laser fiber is calibrated to pocket depth minus 1 mm
Figure 7: Any debris clinging to the fiber must be wiped off
Beginning with the most infected teeth, each appointment will address quadrants for debridement of root surfaces through scaling followed by tissue decontamination and superficial coagulation through lasing. At the subsequent appointment, approximately 7 to 10 days later, a different quadrant will be debrided and tissues lased. The previously treated area will be revisited for ultrasonic biofilm removal from tooth surfaces and laser decontamination of tissues. Instrumentation with the ultrasonic is concentrated on the cervical area of tooth structure and the fiber was calibrated to 1 mm less than the previous application. This continues the reduction of bacterial load and enhances the bodys healing response. C. Laser Operating Parameters A free-running pulsed Nd:YAG laser (PulseMaster 600 IQ, American Dental Technologies, Corpus Christi, Texas) with a 1064nm emission wavelength was used with a 400-micron contact fiber. For bacterial reduction, the laser parameters were 30 mJ and 60 Hz, average power of 1.8 Watts for approximately 40 seconds per site; for superficial coagulation, the settings were 100 mJ and 20 Hz, with an average power of 2.0 Watts for approximately 20 seconds per site. The total laser emission time for the four sessions of periodontal infection therapy was 76 minutes. D. Treatment Delivery Sequence The treatment delivery sequence at each therapeutic appointment included:
20 0 8 VO L 16 , N O . 1
26
JOU R NAL OF L ASER DENTI STRY
review of health history plaque management assessment and instruction anesthetic consisted of topical administered at the gingival margin and subgingival areas. A compounded preparation called TAC (20% lidocaine, 4% tetracaine, and 2% phenylephrine, was applied micro-ultrasonic and handinstrument debridement of root surfaces laser decontamination and superficial coagulation of pocket epithelium postoperative care instructions given pre- and postoperative photographs. Laser safety measures included: wearing 1,064-nm laser wavelength protective eyewear by all operatory personnel use of 0.1-micron filtration masks environment secured to limit access laser-in-use warning sign placed reflective surfaces minimized high-volume evacuation utilized to control plume and cool the tissue. Chart documentation included laser and wavelength used, fiber size and type, operating parameters, and emission time. The laser fiber was cleaved and the laser test-fired. The fiber was calibrated to 1 mm less than the pocket depth (Figure 6). With the fiber remaining in constant contact with the internal pocket tissue and in constant motion, treatment began at the top of the pocket and progressed apically, moving the fiber vertically and horizontally
Figure 8a: Initial distolingual pocket probing of tooth #3
Figure 8b: Laser treatment of pocket
Figure 8c: Immediate postoperative view
until the calibrated depth was reached. The fiber was always directed away from the root surface and toward the target tissue. Accumulated debris was wiped from the fiber and a proper cleave maintained (Figure 7). The amount of lasing time was influenced by tissue interaction, extent of disease, and depth of the pocket. When fresh bleeding was visible, the laser procedure was deemed complete for that site. High-volume suction was present to eliminate the plume and cool the tissue. Quadrants were addressed in each therapeutic appointment. Examples of initial treatment are shown in the following figures: Figure 8a shows the initial pocket on the distolingual of tooth #3; 8b shows the laser treatment; and 8c shows the immediate postoperative completion of coagulation. Figure 9a shows the initial pocket
Smith
CLINICAL CASE
Figure 9: Tooth #19 procedure.
Figure 10: One-week postoperative views.
Figure 9a: Initial mesiolingual pocket probing of tooth #19.
Figure 10a: Tooth #3.
Figure 10b: Tooth #19 Figure 9b: Laser treatment of pocket.
Figure 11: Twenty-week postoperative probing chart
important aspect of the therapy was the healing process, and minimizing plaque at the gingival margin was critical in preventing re-infection. F. Complications The patient had no complications during or after the laser treatments. At the conclusion of the first therapeutic appointment, he requested 400 mg of ibuprofen for possible jaw discomfort postoperatively. No pain reliever was needed after other appointments. G. Prognosis Prognosis is good as long as he conforms to good oral hygiene and recommended intervals for professional supportive maintenance visits. An appliance to prevent further attrition and possibly relieve excessive occlusal stresses related to buxism is indicated. Restorative treatment planning prioritizes caries removal and restoration of teeth #15 and 18; then, a crown on tooth #13, which was previously treated endodontically, to prevent breakage or tooth loss. H. Documentation All treatment and related information was recorded in the patients treatment record.
F O L LOW- U P C A R E
A. Assessment of Treatment Outcomes The patient was assessed at 1 week, 20 weeks, and 8 months following the initial laser therapy. He was not compliant with recommended intervals for therapy care. Periodontal charts show comparative data of the initial state to 20 weeks post-therapy as well as eight months post-therapy. Significant improvement is noted as 92% reduced hemorrhaging sites and 77% reduced periodontal sites. The one-week examination revealed that the tissues were healing and the patients skill in plaque management was improving. Figure 10a shows the one-week view of tooth #3 and 10b shows tooth #19. Six week post-therapy reinfection assessment appointment was missed due to work-related issues. Twenty-week post-therapy appointment: The patient is becoming more compliant with the recommended interval for professional care and is maintaining improved plaque control. Tissues are exhibiting signs of improved health such as
Figure 9c: Immediate postoperative view
Smith
JOU R NAL OF L ASER DENTI STRY
E. Postoperative Instructions Postoperative instructions were given verbally and in written form. The patient was instructed to avoid (for the first 24 hours) acidic, rough, or crunchy foods. Normal eating could resume following that period. Avoidance of seeds, husks, and other foods that may lodge between the gingiva and tooth was recommended for a week. Subgingival flossing was to be avoided for several days. All other areas were to be cleaned as usual. If discomfort were to occur, the patient was instructed to use warm salt water rinses and over-thecounter pain medication. The patient was informed that the most
20 0 8 VO L 16 , N O . 1
on the mesiolingual aspect of tooth #19; 9b shows the laser treatment; and 9c shows the immediate postoperative completion of coagulation.
27
CLINICAL CASE
Figure 12: Twenty-week postoperative probing.
Figure 14: Eight-month postoperative probing.
Figure 12a: Tooth #3.
Figure 14a: Tooth #3.
Figure 14b: Tooth #19 Figure 12b: Tooth #19 Figure 13: Eight-month postoperative probing chart
JOU R NAL OF L ASER DENTI STRY
decreased probing depths, decreased bleeding on probing, normal tissue coloration and texture, and normal mobility. This appointment included: health history review oral cancer screening six-point pocket and hemorrhaging periodontal charting to assess rehabilitation (Figure 11) assessment of the patients plaque management, refining techniques and continuing motivation for thorough daily care micro-ultrasonic instrumentation for full-mouth bacterial decontamination and hand instrumentation as needed coronal polishing laser decontamination of appropriate areas determination of recare interval at 12 weeks. The previously mentioned Nd:YAG laser was used with a setting of 30 mJ and 60 Hz, 1.8 Watts average power, delivered with a 400-micron contact fiber for 7 minutes total emission time. Oral hygiene instructions were reviewed. There was a 92% decrease in hemorrhaging, 77% decrease in periodontal sites, and 77% fewer teeth with pocketing. Figure 12a shows the 20-week probing of tooth #3 and 12b shows tooth #19.
Eight-month post-therapy appointment: The patient reported very high stress since the last appointment and decreased consistency in daily plaque management routine. Periodontal chartings compare initial, 20-week and 8-month data. There was a slight increase noted, but reasonable results were maintaining. The 8-month therapeutic appointment included: health history review oral cancer screening six-point pocket and hemorrhaging periodontal charting (Figure 13) assessment of the patients plaque management, refining techniques and continuing motivation for thorough daily care micro-ultrasonic instrumentation for full-mouth bacterial decontamination and hand instrumentation as needed coronal polishing laser decontamination of appropriate areas. The previously mentioned Nd:YAG laser was used with a 400micron fiber, with parameters of 30 Hz, 60 mJ, average power of 1.8 Watts. Emission time totaled 8 minutes. Long-term follow-up is illustrated: Figure 14a shows the probing of tooth #3 and 14b shows tooth #19.
B. Complications The patient had no complications related to laser treatments either during or after therapy. He had no soft or hard tissue damage. He was pleased with the results from the laser. C. Long-Term Results Caries removal from teeth #15 and 18 with composite restorations of #15 on the MOBL surfaces and #18 on the DOB surfaces were completed following periodontal infection therapy. At 20 weeks post-therapy there was marked improvement. At 8 months post-therapy, the lower anterior required additional therapy but the molar areas were maintaining improved health. The 8-month periodontal charting compared to his initial state shows improvements of 83% in hemorrhaging, 70% in perio sites, and 59% of teeth affected (Table 1). Figures 15a and 15b show the comparison of tissues initially and at 8 months post-therapy. D. Long-Term Prognosis Although the intervals between therapeutic appointments were not optimal, good results were realized and a good prognosis exists. Good oral hygiene and 12-week supportive therapy must continue. An electric toothbrush with small
28
20 0 8 VO L 16 , N O . 1
Smith
CLINICAL CASE
Figure 15: Comparison views.
Table 1: Results of Laser-Assisted Therapy Treatment Assessment Interval Beginning 20 Weeks 8 Months Number of Teeth Number of Sites with Number of Sites with with Beyond-Normal Periodontal Pockets Bleeding on Probing Periodontal 4 mm or Greater Pocketing 48 4 8 83% 30 7 9 70% 17 4 7 59%
Figure 15a: Preoperative full smile at presentation
Rate of Improvement After 6 Months
Figure 15b: Eight-month postoperative full smile
AUTHOR BIOGRAPHY
Mary Lynn Smith is a registered dental hygienist, working clinically
Smith
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
heads for greater cleaning efficiency, particularly in the crowded lower anterior region, would be beneficial to the patients oral health. If restorative plans are not carried out, periodontal issues may persist due to crowding on the lower and further shifting of the upper teeth. It is critical to reinforce that periodontal disease is site-specific and episodic in nature. It is not cured but maintained through appropriate daily care and recommended professional care.
Following customized recommendations will ensure the best results. Tooth #13 has a guarded prognosis if it is not restored with a crown. An appliance to prevent further attrition and provide relief from excessive occlusal forces related to bruxing would preserve the dentition and temporomandibular joint from unnecessary cumulative damage. The oral surgeon gave a good prognosis regarding the site of the previous cyst, stating it was nonprogressing and nonpathogenic. Long-term plans to extract tooth #24 or 25 (depending on prognosis) and re-align anterior teeth orthodontically, as well as replace tooth #8 with a bridge or implant, will be discussed at a later time.
for more than 12 years. She achieved her Standard Proficiency in the Nd:YAG (1,064-nm) and diode (810-nm) wavelengths in 2003, and completed her Advanced Proficiency in the Nd:YAG in 2007. Mary Lynn has contributed to the dental community through articles and speaking to fellow hygienists on care of implants, periodontal therapies, and laser-assisted hygiene techniques and principles. She currently resides in McPherson, Kansas and is employed by Dr. Jon Julian, DDS. Mrs. Smith may be contacted by e-mail at mlsrdh@swbell.net.
Disclosure: Mrs. Smith has no commercial relationships relative to this case presentation.
29
CLINICAL CASE
Use of an 810-nm Diode Laser in a Combined Gingivoplasty, Frenectomy, and Second-Stage Implant Recovery Procedure
Steven Parker, BDS, LDS RCS, MFGDP; Harrogate, North Yorks, Great Britain
J Laser Dent 2008;16(1):30-36 Editorial Note: Although the photographic images are overexposed, they do show well the points made in the article and captions.
SYNOPSIS
Multiple procedures using a diode laser are described prior to placement of a fixed bridge.
P R E T R E AT M E N T
A. Outline of Case 1. Full Clinical Description A 78-year-old male patient attended for a routine examination (Figure 1). He had been a regular patient of the practice during a three-year period and had received only examination and hygiene maintenance at six-monthly intervals. At his current visit, he expressed a need to evaluate the possibility of replacing his existing upper and lower cast chrome-cobalt partial dentures with fixed prostheses. He was advised that treatment would involve the provision fixed bridgework in three quadrants, with additional support through implant-retained abutments in the upper left quadrant. MEDICAL HISTORY The patient was in general good health. He had been prescribed beta-blockers for hypertension, which was under control. In addition, he was taking statins for hypercholesterolemia. DENTAL HISTORY The patient had lost several teeth many years previously and had been provided with earlier upper and lower acrylic resin dentures. These had been replaced by cast chrome-cobalt / acrylic resin dentures which had remained satisfactory through the past 10 years. However, the patient expressed dissatFigure 2: Preoperative panoramic radiograph showing several implant fixtures fully osseointegrated Figure 1: Preoperative view at presentation
20 0 8 VO L 16 , N O . 1
isfaction with the comfort of these prostheses during function. Despite his earlier treatment, he had sought regular dental treatment during the latter years and had maintained a high level of oral health. 2. Occlusion During examination of the dental arches in occlusion and the underlying skeletal landmarks, it was noted that the patient had a Class I occlusion, with normal Frankfort and maxillary (FMP) angle. 3. TMJ Examination of both temporomandibular joints, through palpation and radiograph, revealed normal structure and movements. Opening / closing and excursive movements of the mandible revealed no abnormality. With the dentures in place, there was group function of posterior quadrants on both sides. This was noted for duplication in the new prostheses. 4. Radiographic Examination Panoramic (Figure 2) and periapical
Figure 3: Preoperative periapical radiograph of tooth #9
(Figure 3) radiographs were taken to establish both dental and alveolar bone status prior to treatment. These views were repeated at stages during the treatment, as required. With the exception of dental findings listed below, there was no sign of hard tissue pathology in either jaw or TMJ regions. It was noted that there was sufficient alveolar bone in the edentulous upper left region, to allow the placement of dental implants (Figure 4). There was visual evidence of retained root fragments associated with extractions in both maxillary molar regions.
30
JOU R NAL OF L ASER DENTI STRY
Parker
CLINICAL CASE
Figure 4: Interocclusal view showing adequate space for new prosthesis
Figure 6: Preoperative periodontal probe chart
Figure 7: Preoperative view of gingival tissue level around tooth #9
was considered good with signs of calculus deposits only on teeth #22, 23, and 26. 6. Hard Tissue Status At the time of initial active-treatment assessment, the following teeth were charted as missing: Upper jaw: #1, 3, 4, 7, 10, 11, 12, 13, 14, and 16. Lower jaw: #17, 19, 20, 27, 28, 29, 30, and 32. Tooth #9 had been restored with a porcelain-fused-to-metal (PFM) crown, and teeth #2, 5, 18, and 31 restored with amalgam. There was evidence of caries distally at tooth #18. The PFM crown at tooth #9 had been re-cemented several times and this may have been due in part to a short clinical crown height. Tooth vitality test: All teeth tested vital to ethyl chloride. Mobility: There was no mobility recorded at any natural tooth site. Percussion: Percussion testing of all tooth sites revealed no hyperesthesia. 7. Other Tests Pertinent to the presenting oral condition and the proposed treatment plan, it was considered that no further tests were appropriate. B. Diagnosis and Treatment Plan 1. Provisional Diagnosis Treatment for this patient to fully restore his dentition in accordance with his preferences would involve several stages, including implant placement and fixed bridgework.
With regard to laser-assisted therapy, it was considered appropriate that some soft tissue manipulation would be required in the upper left quadrant. 2. Final Diagnosis Laser-assisted treatment could be assigned in accordance with the following clinical needs: a. Gingivoplasty at tooth #9 to remove hyperplastic tissue and achieve some crown-lengthening. The disparity in gingival levels with tooth #8 was acceptable to the patient and the amount of bone and gingival tissue removal required to achieve a balanced appearance was considered prejudicial to the long-term survivability of tooth #9. b. Second-stage recovery of implants placed in the upper left cuspid, bicuspid, and molar regions. c. Lateral frenectomy of low attachment of buccinator fibers to preserve attached gingiva associated with the bicuspid implant. The final diagnosis reflected the observations and needs outlined above. 3. Treatment Plan Outline General: Three dental implants would be placed in the upper left quadrant, as part-support for fixed bridgework. In addition, bridgework would be provided in the other three posterior quadrants. Specific: In order to facilitate optimal soft tissue profiles for both natural and implant abutments in the upper left quadrant, it was
Figure 5: Left lateral view showing posterior frenum attachment near the ridge crest
Parker
JOU R NAL OF L ASER DENTI STRY
5. Soft Tissue Status General oral soft tissue: Examination of all soft tissue structures revealed no abnormality. All tissues appeared normal in appearance, and dorsal and ventral tongue surfaces, together with tongue movements, were within normal expectations. The loss of teeth in the upper left quadrant had resulted in some loss of postextraction keratinized gingival tissue. This was of concern in the bicuspid region, where there was a low frenal attachment, as shown in Figure 5. Gingival soft tissues: All natural tooth sites were examined with a periodontal probe and findings recorded, as shown in Figure 6. Of specific relevance to the treatment provided, there was some false pocketing at tooth #9, with recorded depths of 3 mm on mesial, distal, and facial aspects. Generally, the attached gingiva appeared thickened, yet healthy in appearance (Figure 7). Such hypertrophic change may have been due to antihypertensive medication and did not merit any further intervention. The general level of oral hygiene
20 0 8 VO L 16 , N O . 1
31
CLINICAL CASE
decided to use an 810-nm diode laser to remove hyperplastic gingival tissue associated with tooth #9, to effect second-stage recovery of the implants, and to carry out a relieving frenectomy at the lateral frenal attachment of superficial buccinators fibers. 4. Indication and Contraindications INDICATIONS Treatment: In all areas of soft tissue management within this treatment plan there is an ideal in achieving hemostasis, consistent with the need to provide access for hard tissue treatment and early abutment preparation of tooth and implant sites. In addition, an optimal definition of a stable gingival margin at tooth #9 would allow early placement of a permanent coronal restoration. A further indication would include the delivery of soft tissue surgery that provides minimal postoperative discomfort and complication for the patient. The use of a suitable laser wavelength would seek to meet these requirements. Laser: It is recognized that all laser-tissue interactions in surgical procedures are predominately photothermal in nature. The conversion of incident laser light energy into heat will lead to primary and, through local conduction, secondary heat effects that would allow soft tissue surgery to be carried out through tissue ablation with a supportive hemostasis. As such, the use of laser energy to effect soft tissue surgery is justified. Wavelength: The predominant chromophores of the keratinized and nonkeratinized gingival tissue in this case are melanin (tissue pigment), hemoglobin, and intracellular water. In addition, the prime needs of treatment would be to achieve tissue ablation with hemostasis, indicating the optimum need for using a nearinfrared wavelength, such as the 810-nm diode laser.
20 0 8 VO L 16 , N O . 1
CONTRAINDICATIONS Treatment: The only absolute contraindication to treatment in this case would be to accept the original situation of a well-fitting partial denture. However, in view of the patients wishes, this alternative was abandoned. Consequently, soft tissue manipulation is mandatory and there can be few if any contraindications for treatment. In addition, further considerations apply: a. biologic width (i.e., the sum of the connective tissue attachment, epithelial attachment, and sulcular depth relative to the osseous crest) must be determined and considered when recontouring the periodontium with a subsequent placement of a restoration. b. aesthetic considerations lip line height, etc. in placement of the final gingival contour. Is the patient accepting of the contour, should it match the adjacent teeth, does the lip hide it anyway, and so on. Laser: Any surgery using laser energy carries some risk of tissue damage and this possibility must be borne in mind. Wavelength: The choice of a longer wavelength would offer a more superficial level of tissue ablation. 5. Precautions The benefit of hemostasis offered by near-infrared laser wavelengths is accepted. In comparison to the Nd:YAG laser, the depth of penetration of the 810-nm diode wavelength in oral soft tissue is less, which would reduce the risk of collateral thermal damage. Nonetheless, the use of minimum power parameters, as well as time intervals to allow thermal relaxation and control of carbonization of the tissue and optic fiber, would all reduce the risk of primary and secondary thermal damage. Gingivoplasty: Whenever periodontal contouring and tissue removal is undertaken in association with natural teeth, attention must
be given to the preservation of the biological width. In addition, preservation of a stable result is dependent on good patient home care. Second-Stage Implant Recovery: Care should be exercised to accurately locate the position of the implant. Tissue ablation should proceed slowly and with care to remove any char. Wherever possible, direct contact with the cover screw or any surrounding crestal bone should be avoided. Lateral Frenectomy: Tissue traction during laser incision will assist the ability to resect using minimal power parameters. In addition, the laser fiber tip should be angled as near possible, parallel to the alveolar bone, to avoid damage to the hard tissue and periosteum. 6. Treatment Alternatives Alternative methods for soft tissue incision would include a scalpel, electrosurgery, and soft tissue punch for implant sites. 7. Informed Consent The treatment plan was fully explained to the patient and all associated risks outlined. A written consent form was signed by the patient in the presence of a witness. The consent form was retained in the treatment notes.
T R E AT M E N T
A. Treatment Objectives The objective of this treatment would be to effectively remove or resect soft tissue at each of the treatment sites, with the 810-nm diode laser, with minimal peri- and postoperative complications. B. Laser Operating Parameters 1. Laser: A diode laser (DioLase ST, American Dental Technologies, Corpus Christi, Texas) was used. The operating features are as follows: Wavelength: 810 nm Co-axial aiming beam: Diode Class I laser 630-680 nm, 3 mW
32
JOU R NAL OF L ASER DENTI STRY
Parker
CLINICAL CASE
Emission mode: Continuous wave (CW) with supplementary gated CW, single or repetitive single pulse Maximum power output: 12.0 Watts Delivery system: Quartz fiberoptic (320-m diameter) with conduit handpiece and disposable cannula tip Beam diameter: 320 m. 2. Laser settings: Gingivoplasty / second-stage implant recovery: 1.4 W CW / contact mode. Time taken per site: 1-2 minutes. Lateral frenectomy: 1.7 W CW / contact mode. Time taken: 1-2 minutes. C. Treatment Delivery Sequence 1. Preliminary to patient treatment Secure operating room, define controlled area, and place proper laser warning signs. Set up laser and test proper laser operation. Test-fire laser, employing all safety measures, using minimum power settings and directing beam onto articulating paper. Objective is to ensure correct laser operation, patency of delivery system, and emission of cutting and aiming beams. In addition, the fiber tip can be inspected to ensure that a proper cleave has been carried out and the spot size is uniform. Dispense supplies, and arrange equipment and sterile instruments. Review patient information: charting, X-rays, etc. Patient seated: review treatment plan and informed consent. Safety: place eye protection, patient first followed by operating personnel. 2. Treatment sequence Individual treatment sites were isolated and infiltration local anaesthetic (2% lignocaine 1:80,000 adrenalin) was administered.
Figure 8: Diode laser beginning the removal of gingiva on tooth #9
Figure 11: Diode laser beginning the removal of tissue covering implant fixture on tooth #11
Figure 9: Laser procedure finished on tooth #9
Figure 12: Healing cap placed on #11. Diode laser beginning the removal of tissue covering implant fixture on tooth #14
Figure 10: Curette used to clean edges of soft tissue
Parker
JOU R NAL OF L ASER DENTI STRY
Gingivoplasty tooth #9: Laser power setting: 1.4 Watts CW. The soft tissue pocket was explored with a periodontal probe. The laser fiber was lightly initiated using articulating paper and, perpendicular to the surface, a series of points were developed on the labial gingiva to outline the incision line (Figure 8). With a light contact of the fiber with tissue, the incision line was developed, with minimum depth. Any char on the tissue or fiber tip was removed with damp gauze. Successive sweeps of the fiber allowed precise tissue cleavage to be carried out, as shown in Figure 9. The final excess tissue removal was achieved with a sharp curette, as shown in Figure
Figure 13: Healing cap placed on #14. Diode laser beginning the removal of tissue covering implant fixture on tooth #13
10. In this way, direct contact with the underlying tooth was avoided. Second-Stage Implant: Laser power setting: 1.4 Watts CW. At each site, the location of the cover screw was identified with an explorer. With the fiber freshly cleaved and lightly initiated, a circular incision was developed in the overlying keratinized gingiva. This was gradually deepened, with care to avoid the build-up of char, until the cover screw was uncovered. Excess tissue was removed to completely expose the extent of the screw and healing caps were placed (Figures 11-13).
20 0 8 VO L 16 , N O . 1
33
CLINICAL CASE
Figure 14: Healing cap placed on #13. Diode laser beginning frenectomy
Figure 17: One-week postoperative view of soft tissue healing around the implants and the frenum
Figure 20: Two-week postoperative view of soft tissue around implant #13
Figure 15: Immediate postoperative view of completed diode laser procedures
Figure 18: Two-week postoperative view of soft tissue around implant #11
Figure 21: Abutments fitted on implants
20 0 8 VO L 16 , N O . 1
Figure 16: One-week postoperative view of gingival tissue around tooth #9
Figure 22: Telescoping thimble restoration on tooth #9 Figure 19: Two-week postoperative view of soft tissue around implant #14
JOU R NAL OF L ASER DENTI STRY
Lateral Frenectomy: Laser power setting: 1.7 Watts CW. The buccal tissue was placed under tension to identify the profile of the muscle fiber insertion. The optic fiber was freshly cleaved and lightly initiated. With the fiber held perpendicular to the tissue surface and parallel to the alveolus at 2-3 mm away from fixed gingival tissue, an initial incision was performed. With the tissue under tension, the incision was developed to a depth where superficial muscle fibers were parted, as shown in Figure 14, and no blanching or movement of gingival tissue was observed. Care was taken to avoid char build-up in the tissue or on the fiber tip and the incision was restricted to achieve the surgical objective (Figure 15).
At this time, adjunctive treatment including implant healing cap placement was carried out and the denture adjusted to allow correct seating. D. Postoperative Instructions The surgical sites were shown to the patient and their appearance was explained. A chlorhexidine mouthwash was prescribed and the patient instructed to carefully apply this with cotton wool, avoiding disturbance of the coagulum; this should be carried out three times daily during the fiveday postoperative period. The patient was advised that the appearance of the treatment sites
would change, with detachment of the coagulum at fixed gingival sites and softening and hydration of loose tissue at the frenectomy site at 3-5 days post-operation. The patient would be reviewed at one week and light toothbrushing commenced at the tooth site. Postoperative analgesia was prescribed for use as required. There were considered no limitations on eating or drinking. The patient was instructed to call should any problem occur and was called by phone after 24 hours. E. Complications Complications that can be expected following laser soft tissue surgery can include pain, tissue swelling and deformation, bleeding, and
34
Parker
CLINICAL CASE
Figure 23: Immediate postoperative view of prosthesis in place
Figure 26: Three-month postoperative probing of implant #13
Figure 29: Six-month postoperative panoramic radiograph
Figure 27: Three-month postoperative probing of implant #14 Figure 24: Three-month postoperative probing of tooth #9
Figure 30: Ten-month postoperative periodontal chart
Figure 28: Six-month postoperative view of prosthesis Figure 25: Three-month postoperative probing of implant #11
F O L LOW- U P C A R E
A. Assessment of Treatment Outcome The patient was reviewed at one week. The healing was progressing well, as shown in Figures 16 and 17. At two weeks, the healing caps were removed to inspect the tissue contour around the implants, and the contours were excellent (Figures 18-20). The gingivoplasty site resolved rapidly at two weeks and the frenectomy site gradually healed during four weeks after surgery. The implant abutments (Figure 21) and the telescoping thimble on tooth #9 (Figure 22) were fitted during this time. Shortly thereafter, the final prosthesis was delivered, as shown in Figure 23. Subsequent appointments at weekly intervals allowed regular
infection. In this case, no such complications were encountered. F. Prognosis Laser-assisted soft tissue procedures, employing correct power parameters and technique, generally have a very good prognosis. It was felt that in this case a similar outcome could be expected. G. Treatment Records All procedural details, both generally and specifically with reference to the laser use, were entered in the patients treatment notes, along with the consent details, radiographs, and chartings. As such, the treatment records would reflect the treatment outlined above.
Parker
JOU R NAL OF L ASER DENTI STRY
review of the tissue. The soft tissue sites were therefore regularly reviewed initially and at three months, six months, and one year. Figure 24 shows excellent gingival health and minimal pocket depth around tooth #9 and identical findings existed around the three implants, as shown in Figures 25-27. In all cases, the healing was as expected and normal oral function was maintained. Tooth #9 was vitality-tested and a positive response recorded. Figure 28 shows the six-month post operative view, and Figure 29 depicts a panoramic radiograph at that same interval. The 10-month probing chart, shown in Figure 30, exhibits good periodontal health. The one-year postoperative view of the prosthesis is shown in Figure 31. At one year, the tissue tone is excellent and the physiologic contour shows very good adaptation to the abutments. Periodontal probings of the implant abutments, shown in Figures 32-34, demonstrate excellent tissue attachment. Radiographs at one year also confirm the health and fit of the restorations (Figures 35-37).
20 0 8 VO L 16 , N O . 1
35
CLINICAL CASE
Figure 31: One-year postoperative view of prosthesis
Figure 34: One-year postoperative probing of implant #14
Figure 36: One-year postoperative radiograph of implants #11 and 13.
Figure 32: One-year postoperative probing of implant #11
Figure 37: One-year postoperative radiograph of implants #13 and 14.
Figure 35: One-year postoperative radiograph of tooth #9
Figure 33: One-year postoperative probing of implant #13 20 0 8 VO L 16 , N O . 1
JOU R NAL OF L ASER DENTI STRY
B. Complications No long-term complications were observed. Some concern was expressed that the amount of attached gingiva adjacent to the frenectomy site might compromise the health and function of the implant cuff, but this tissue has remained stable and normal in appearance. C. Long-Term Results The long-term results are in keeping with the objectives of the original treatment plan. The restorative phases of treatment were satisfactorily completed and the patient was very satisfied with the outcome. D. Long-Term Prognosis The long-term prognosis of the
treatment provided should be considered as good. The patient continues to maintain good oral hygiene and attends for assessment as required. He is pleased with the aesthetic and functional result obtained.
AUTHOR BIOGRAPHY
Dr. Steven Parker studied dentistry at University College Hospital Medical School, University of London, UK and graduated in 1974. He is in Private Practice in Harrogate, UK. He holds Fellowship and Diplomate status with the International Congress of Oral Implantologists. Dr. Parker has been involved in the use of lasers in dentistry since 1990. Prior to joining the Academy of Laser Dentistry in 1993, he was President of the British Dental Laser Association. He joined the Board of Directors of the Academy in 1996 and became chair of the International Relations Committee. From 1999 through
2004, he was chair of the Committee for Proficiency Recognition and co-editor of Wavelengths, the former journal of the Academy of Laser Dentistry. He was awarded the Leon Goldman award for Excellence in Clinical Laser Dentistry by the Academy in 1998. In addition, Dr. Parker holds Advanced Proficiency status in multiple laser wavelengths and completed the Academy Educator Course at the University of California San Francisco in 2000. He is an ALDRecognized Standard Proficiency Course Provider. He has held consultancies with multiple laser companies and has presented courses, lectures, and workshops worldwide. He has authored numerous articles on the use of lasers in dentistry, including a chapter The Use of Lasers in Fixed Prosthodontics in the October 2004 Dental Clinics of North America. Dr. Parker was the 2005 President of the Academy of Laser Dentistry. Dr. Parker may be contacted by e-mail at thewholetooth@easynet.co.uk.
Disclosure: Dr. Parker has no current affiliations with any company.
36
Parker
CLINICAL CASE
Establishing a Maintainable Esthetic Gingival Smile Line with an Er:YAG Laser
Charles R. Hoopingarner, DDS, Houston, Texas
J Laser Dent 2008;16(1):37-42
SYNOPSIS
This article describes aesthetic crown lengthening involving both soft and hard tissue.
P R E T R E AT M E N T
A. Outline of Case 1. Full Clinical Description A 31-year-old black female presented with no significant medical conditions or limitations to treatment. Her vital signs were within normal limits (blood pressure 100/70, pulse 67). She had no known allergies and was taking no medications. The patient had small occlusal restorations on teeth #30 and 19. She had a resin-based crown on tooth #8, which was placed approximately 8 years prior to the examination date. Teeth #16 and 17 were impacted with no oral communication. The teeth were in Class I dental occlusion. Her chief complaint was an unaesthetic gingival presentation in the maxillary anterior region. She stated that her crown was too short (Figure 1). 2. Radiographic Examination A panoramic radiograph and decaydetecting radiographs were evaluated, revealing a normal bone contour and impaction of teeth #16 and #17. No interproximal carious
lesions were present. A periapical film of tooth #8 is shown in Figure 2. 3. Soft Tissue Status Oral cancer screening was negative. Probing depths were 2-3 mm in all but the molar areas (Figure 3). She had 3-4 mm depths in the upper right and upper left molar areas. There was a high fibrous frenum attachment in the maxillary midline. There was slight blunting of the papillae in general and generalized marginal gingivitis in the posterior segments. The anterior segment was characterized by excessive fibrous gingival display. 4. Hard Tissue Status There were no carious lesions detected and no direct indication
Figure 2: Periapical radiograph of tooth #8
for vitality testing except for tooth #8 which tested vital. There was no mobility or fremitis. 5. Other Tests There was modest tooth wear and faceting present. There was no muscle or joint tenderness, joint sounds, or limitations in range of motion present. Smile evaluation revealed excessive gingival display
Figure 1: Preoperative full smile
Figure 3: Preoperative charting showing minimal pocket depths in anterior areas
Hoopingarner
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
37
CLINICAL CASE
and a width-to-length ratio of 110%. The gingival extension on the maxillary centrals was significantly more incisal than that of the canines. B. Diagnosis and Treatment Plan 1. Provisional Diagnosis Mild generalized chronic gingivitis, excessive gingival display, gingival hyperplasia adjacent to teeth #710, incisally positioned maxillary midline frenum which could possibly put tension on the gingival tissues if the gingival margin were raised to the planned level. 2. Final Diagnosis Mild generalized chronic gingivitis, excessive gingival display, gingival hyperplasia adjacent to teeth #710, incisally positioned maxillary midline frenum which placed tension on the gingival margin. Additionally the existing resin crown restoration on tooth #8 was found to be defective. After contouring the gingiva appropriately there was an inadequate attachment width present resulting in a violation of the biologic width. 3. Treatment Plan Outline The objective was to perform gingival and osseous recontouring with an Er:YAG laser to allow for ideal aesthetic width-to-length ratio throughout the maxillary anterior segment. The laser would also be used to revise the maxillary frenum attachment. Therapy for gingivitis is to consist of oral hygiene review and motivation, dental prophylaxis, and follow-up fine scale and polish. Tooth #8 will be restored with a modified pressed ceramic crown. 4. Indications for Treatment Indications for gingival recontouring are largely aesthetic. However it was felt that over the life of the dentition the hyperplastic tissue would be a contributing factor to decreased periodontal health in the anterior segment. The esthetic contouring will be achieved by both gingival sculpting and osseous removal.
Frenum revision was indicated to prevent apical migration of the gingival margin on teeth #8 and #9. Although for financial reasons the restoration was done as a secondstage procedure, the Er:YAG laser would have allowed for immediate restorative treatment. Compared to conventional modalities, this wavelength has the advantage of decreased healing time with minimal patient discomfort. The Er:YAG laser is also beneficial since it can be utilized for both soft tissue ablation and osseous recontouring for biologic width maintenance. Final gingival position is very predictable using this laser and scoring of the periosteum is easily accomplished during the frenum revision. 5. Contraindications There were no contraindications for treatment. However care in treatment planning must be exercised to leave an adequate dimensional band of gingival tissue to prevent mucogingival dehiscence. 6. Precautions for Wavelength Standard safety precautions for laser operation should be strictly adhered to. As this wavelength readily interacts with both hard and soft tissue, care must be taken to avoid excessive tissue removal. In particular, care must be taken to avoid premature osseous ablation when using the laser without cooling water spray. This may be done by directing the light energy perpendicular to the tooth during soft tissue removal until the tissue can be easily removed by hand instrumentation or sequentially removing some osseous tissue prior to completion of the final soft tissue contours. Another alternative is to use a water spray when applying laser energy to the soft tissue when it may be possible to encounter osseous tissue. Adequate water spray must be used during the osseous phase. The angle of energy application is also critical in avoiding the tooth itself. Care must be used to avoid interacting
with tooth structure. Care must be taken to avoid emphysema by turning the cooling air off or down to an appropriate level and using digital pressure to compress the tissue at the muccogingival border. 7. Treatment Alternatives Conventional periodontal surgical procedures with subsequent healing time prior to restoration would be treatment alternatives. No treatment was also an alternative. 8. Informed Consent After a discussion of risks and possible complications, written informed consent was obtained for both the surgical and restorative procedures.
T R E AT M E N T
A. Treatment Objectives Strategy The periodontal tissue of the maxillary anterior teeth will be recontoured with an Er:YAG laser to establish proper soft tissue heights and proper tissue scallop and zenith of the individual teeth. To establish an attachment distance consistent with the patients biologic width, osseous recontouring will be performed, and the frenum attachment will be revised along with scoring the periosteum to prevent reattachment. In order to achieve the aesthetic goals, the gingival tissues must be contoured from tooth #6 across to #11, leaving the cuspids and centrals at the same level and the lateral incisor 0.5 mm incisal to that level. To achieve a 77.5% width-to-length ratio, it would be necessary to remove 4.5 mm of gingival tissue. Since there was adequate gingival tissue present, the limiting factors were the location of the cementoenamel junction (CEJ) (which should not be exposed) and the position of the osseous crest. Probing indicated the osseous crest to be 5 mm apical to the gingival margin. To maintain the patients individual attachment width of 1.75 mm (connective tissue
38
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
Hoopingarner
CLINICAL CASE
Figure 4a: Preoperative width measurement.
Figure 5: Probing for crestal bone level, preoperatively
Figure 6: Initial tissue ablation, following the outline
Figure 4b: Intended new gingival height
Hoopingarner
JOU R NAL OF L ASER DENTI STRY
B. Laser Operating Parameters Laser: Er:YAG (DELight, HOYA ConBio, Fremont, Calif.): Delivery system: Fiber-optic system with varying quartz tips: 600-micron for initial tissue ablation, 400-micron for osseous recontouring, and 1200 x 300micron chisel tip for tissue and osseous smoothing Wavelength: 2940 nm Mode: Free-running pulsed Pulse width: 300 microseconds Power: 1.5 Watts (30 Hz and 50 mJ) Beam Diameter: Varied, 400 to 600 microns using light contact
20 0 8 VO L 16 , N O . 1
attachment and epithelial attachment) and allow for 1 mm of sulcus depth, osseous recontouring was necessary. The gingival revision is performed and then the osseous tissue is recontoured to a level 2.75 mm apical to the intended free margin of the gingiva. The Er:YAG laser has the advantage of being able to be utilized for both soft tissue ablation and osseous recontouring for biologic width maintenance and scoring the periosteum. The restoration on tooth #8 was replaced as a secondary procedure.
and defocused pattern Repetition rate: 30 Hz Continuous air only for soft tissue surgery; reduced volume of water spray for osseous procedure Laser settings: Soft tissue ablation: 30 Hz and 50 mJ, air cooling and no water Frenum revision, osseous recontouring, and scoring of periosteum: 30 Hz and 50 mJ with air and water spray and decreased air volume C. Treatment Delivery Sequence Pretreatment: The operatory was secured and the laser warning sign was posted. The laser unit was properly placed and connected to an air supply. Safety glasses with 4+ optical density for the 2940-nm laser wavelength that met ANSI standards Z136.1 and Z136.3 were used. All shiny reflective objects were removed. The operatory was set up and supplied according to the standard for a surgical procedure. Charting and radiographs were visible to the operator. The procedure was reviewed with staff in the morning report meeting. Prior to administration of anesthesia, the treatment was reviewed with the patient and informed consent was confirmed. The patient was properly draped and 3.8 cc Septocaine 4% 1:200,000 epinephrine was distributed by infiltration in the maxillary anterior segment. Eye protection was placed on the patient as well as the operator and assistant. The laser was test-fired in a safe direction. Figure 4a shows the caliper used
for width-to-length measurement. After calculation, the periodontal probe was placed at the desired new tooth length, as depicted in Figure 4b. Since there was more than 2 mm of attached gingival tissue apical to the intended finish line, the limiting factor became the position of the CEJ. This was assessed by probing and marked with stab punctures. Crestal bone was identified by probing and subsequently marked, as shown in Figure 5. The refined intended gingival finish line was appreciated and indicated with tissue-marking ink. The laser was set with a chiselshaped quartz tip at an energy setting of 50 mJ and repetition rate of 30 Hz. The gingival tissues were then ablated to the level of this marking without the use of water spray, as seen in Figure 6. This was done using axially directed noncontact strokes until the desired amount of tissue was ablated, while stopping short of scoring the tooth itself. The tissue was beveled (Figure 7). The bulk of the tissue was then removed by instrumentation, and the final tissue contour was performed with the laser, paying close attention to establishing the proper alignment and zenith placement. All teeth in the segment were treated in this manner, and Figure 8 shows the immediate soft tissue surgical result. Next, the distance to the crestal bone was probed (Figure 9). The intended biologic width was reestablished by projecting the patients individual biologic width
39
CLINICAL CASE
Figure 7: Soft tissue bevel placed prior to bulk removal
Figure 10: Osseous contouring begins and the tip is extended into the sulcus up to the 3 mm mark
Figure 13: Immediate postoperative view of the final tissue contour prior to the frenum revision
Figure 8: Immediate postoperative view of the intended gingival contours
Figure 11: Beveling of the bone with a chisel tip
Figure 14: Frenectomy proceeding with ablation of muscle fibers and scoring of periosteum
20 0 8 VO L 16 , N O . 1
Figure 9: The crestal bone depth was determined before osseous recontouring
Figure 12: Measuring the osseous crest
40
JOU R NAL OF L ASER DENTI STRY
onto the tissue and confirming adequate gingiva remained to complete the osseous recontouring. The osseous tissue in this case was contoured using a 400-micron tip at 30 Hz and 50 mJ with adequate water spray. The protective sleeve on the tip was measured at 3 mm and used as a depth guide during the procedure, as shown in Figure 10. (Tips lacking a convenient sleeve length can be marked with a stopper or ink for reference.) Care was taken to avoid emphysema by compressing the tissue with digital manipulation and decreasing the cooling air pressure. The bone was then beveled with the chisel tip in a noncontact defocused mode with water spray (Figure 11).
Care was taken to extend the recontouring interproximally and through to the palatal surface. The contact-area-to-osseous-papillacrest distance was not allowed to exceed the 4.5 mm level. Figure 12 depicts the biologic width measurement, which was confirmed at 2.75 mm from the osseous crest to the intended final free gingival margin. The immediate postoperative view of the final tissue contouring is shown in Figure 13. The frenum was then revised with longitudinal noncontact strokes that were directed around larger vessels until all fibrous bands had been ablated. This was accomplished using a chisel tip with no water spray at 30 Hz and
Figure 15: Immediate postoperative view of finished frenectomy
50 mJ of energy. The effectiveness of the revision was checked by confirming that there was no tension present on the gingival tissue when elevating the upper lip. The tip was then rotated 90 degrees and with the addition of water spray the periosteum was scored to the level of the bone using horizontal light contact strokes, as shown in Figure 14. Again, care was taken to avoid emphysema by reducing the cooling air and applying digital pressure around the operated area. Figure 15 illustrates the completed frenum revision.
Hoopingarner
CLINICAL CASE
Figure 20: Twenty-one month postoperative radiographs Figure 16: Four-day postoperative view Figure 18: Six-month postoperative view
Figure 17: Two-week postoperative view
Figure 19: Eighteen-month postoperative view showing frenum stability
Figure 21: Twenty-one month postoperative periodontal probing showing minimum sulcus depth.
D. Postoperative Instructions The patient was told to avoid foods warmer than room temperature for 48 hours and then begin hot saline mouth rinses. The area was to be cleaned with hydrogen peroxide on cotton tip applicators for the first 48 hours. After the first postoperative visit, the patient was cleared for normal hygiene procedures which included nonsulcular brushing with an ultrasoft brush dipped in hot water and gentle flossing. Emergency care contact numbers were given. No analgesics were prescribed and the patient was instructed to take over-the-counter ibuprofen if necessary. E. Complications No complications arose during surgery or recovery. F: Prognosis Due to the extent of the tissue bulk removed, some variation in tissue position may occur and require slight soft tissue revision. This was particularly expected in the area of the poorly contoured crown on tooth #8. The overall prognosis was very good for tissue health maintenance and esthetic acceptance.
G: Treatment Records The treatment record reflects the treatment described including estimated exposure times totaling 37 minutes and postoperative instructions.
Vivadent Inc., Amherst, N.Y.), with cut-back and refractory porcelain correction was fabricated and cemented at 10 weeks. B. Complications No complications were appreciated. No analgesic medication was necessary. While there was the expected immediate postoperative tenderness, there was no infection. Since the patient followed instructions and did no sulcular brushing for one week, the reattachment was not impeded. C. Long-Term Results At 6 months (Figure 18) the tissues were maintaining a good level of health. The patient had maintained a healthy aesthetic gingival display and there were no further changes to gingival contour once the definitive restoration was placed. Figure 19 shows an 18-month postoperative view, with the tissues stable. At 21 months, radiographs depict a healthy periodontium (Figure 20); the intended tooth length was maintained and there was a 1 mm sulcus present, as shown in Figure 21.
F O L LOW- U P C A R E
A. Assessment of Treatment Outcome The patient was assessed at 4 days, 2 weeks, 6 weeks, and 10 weeks and has returned to a semiannual recare program in our office. At 48 hours there were no pain reports and the tissues, while reddened, showed no sign of infection. Healing appeared to be progressing nicely. The 4-day postoperative view is shown in Figure 16. At two weeks (Figure 17) there were no complications. Oral hygiene was excellent. Expectedly, the tissue was rebounding on the undercontoured tooth #8. This was remedied at 6 weeks with the restoration of proper contour and emergence profile. Tooth #8 was prepared and a provisional restoration was placed using a BIS-GMA resin. A Lucitereinforced pressed ceramic material, IPS Empress (Ivoclar
Hoopingarner
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
41
CLINICAL CASE
D. Long-Term Prognosis The patient has now been seen on re-care evaluation for nearly two years and has shown no sign of inflammation, regression, or recurrence of the hyperplasia. Sulcus depth has remained constant at 1 mm. While there is a color variation where the incisal extent of the frenum was not revised, there has been no reattachment incisal to the scored periosteum. There is an excellent prognosis for continued health and aesthetics.
AUTHOR BIOGRAPHY
Dr. Charles Hoopingarner attended the University of Texas Health Science Center at Houston
(UTHSCH) Dental Branch, graduating with a DDS in 1973. He has maintained a private practice in Houston, Texas since 1973. He was an adjunct associate professor in anatomical sciences at UTHSCH Dental Branch for 11 years. Currently he is adjunct clinical faculty in the Restorative Dentistry Department at UTHSCH and has been a clinical instructor at the Las Vegas Institute for Advanced Dental Studies since 1997, teaching Advanced Anterior Aesthetics and Comprehensive Aesthetic Reconstruction and Laser Dentistry. Dr. Hoopingarner is a member of the Academy of Laser Dentistry (ALD) and has
used dental lasers of various wavelengths as integral parts of his patient care delivery system for the last 10 years. He holds Advanced and Standard Proficiency certification from the ALD and has lectured internationally on the safety and use of laser technology in the dental practice. He may be contacted by e-mail at choop@swbell.net.
Disclosure: Dr. Hoopingarner has no direct financial or ownership positions with commercial companies relative to this case presentation. He has received honoraria and expenses from HOYA ConBio to present material on laser dentistry.
42
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
Hoopingarner
CLINICAL CASE
Use of an 810-nm Diode Laser in the Treatment of Multiple Hemangiomata of the Lip
Steven Parker, BDS, LDS RCS, MFGDP; Harrogate, North Yorks, Great Britain
J Laser Dent 2008;16(1):43-47
SYNOPSIS
The use of a diode laser for dealing with multiple hemorrhagic lesions is described.
P R E T R E AT M E N T
A. Outline of Case 1. Full Clinical Description A 68-year-old female patient attended for treatment including the provision of dentin-bonded crowns at several tooth sites. At examination, it was noted that there were several discrete pigmented lesions of the right lower lip, which appeared to be blood-filled. Otherwise, the appearance and function of the lip was normal. MEDICAL HISTORY The patient was in general good health. She had been receiving hormone replacement therapy for many years and had recently been prescribed statins for hypercholesterolemia, which was maintained within normal limits. DENTAL HISTORY The patient had been a regular and well-motivated attendee of the practice during many years. Teeth #1, 12, 16, 17, 19, 28, 29, and 30
had been lost, with the latter three being replaced by a fixed bridge (Figure 1). Her general oral health was good, with no caries, and the periodontal condition was satisfactory. The lesions on the right lower lip had appeared during a period of several months. Although considered unsightly, they did not arouse any concern for the patient. 2. Occlusion The patient had an increased overbite at 5 mm and slightly retroclined upper incisors, although these had been cosmetically enhanced by crowning. Her molar relationship, together with the incisal appearance, was consistent with a Class II division 2 occlusion. 3. TMJ Examination of both temporomandibular joints, through palpation, revealed normal structure and movements. Opening / closing and excursive movements of the mandible revealed no abnormality.
Figure 2: Preoperative appearance of lip lesions
Figure 3: Close-up view of lesions 20 0 8 VO L 16 , N O . 1 JOU R NAL OF L ASER DENTI STRY |
4. Radiographic Examination The presentation and scope for treatment of the lip lesions did not warrant any radiographic investigation. 5. Soft Tissue Examination General oral soft tissue: Examination of all oral soft tissue structures revealed no abnormality. All tissues appeared normal in appearance, and dorsal and ventral tongue surfaces, together with tongue movements, were within normal expectations. Regional lymph node palpation was normal. Specific: The appearance of the pigmented lesions on the lip was consistent with some traumatic etiology. There was no associated pulse on palpation, nor was there
Figure 1: Patient chart
Parker
43
CLINICAL CASE
any emptying of each lesion on pressure, such findings being consistent with a cavernous hemangioma. As such, each lesion was discrete, with a nonpedunculated base and a thin epithelial cover (Figures 2-3). 6. Hard Tissue Status Further to the comments above, the general hard tissue status was good, with multiple full-veneer crown restorations that were satisfactory. 7. Other Tests In view of the age of the patient and presentation of the lesions, it was felt prudent to contact the patients general medical practitioner. Although no tests specific to this proposed oral treatment were arranged, systemic conditions such as any blood dyscrasias were eliminated through her recent treatment of hypercholesterolemia and there was no report of any skin ecchymosis, suggestive of blood vessel fragility. It was concluded that the lip lesions were due to isolated capillary dilatation and probably traumatic in origin. Further questioning of the patient did not reveal any contributory factors such as lip-biting. B. Diagnosis and Treatment Plant 1. Provisional Diagnosis A provisional diagnosis was made of unsightly multiple raised hemorrhagic lesions of the lower lip. 2. Final Diagnosis Following the investigations outlined above, it was felt that these lesions were isolated hemangiomata of possible traumatic origin. Laser-assisted treatment could be assigned in accordance with the need to excise these unsightly lesions with minimal tissue disruption or postoperative complication. 3. Treatment Plan Outline It was felt that, with the use of a
laser wavelength that would maximize the interaction with blood pigments, these lesions could be excised and contributory capillary supply sealed to prevent recurrence. In view of the need to anticipate unforeseen bleeding, it was felt prudent to administer an adrenaline-enhanced local anaesthetic, and to have hemostat instruments in case of hemorrhage. 4. Indication and Contraindications INDICATIONS Treatment: In all areas of soft tissue management within this treatment plan there is an ideal in achieving hemostasis, consistent with the need to provide unhindered access to the surgical site. The appearance of these lesions was cosmetically distracting and potentially hazardous due to the inherent fragility. A further indication would include the delivery of soft tissue surgery that provides minimal postoperative discomfort and complication for the patient. The use of a suitable laser wavelength would seek to meet these requirements. Laser: It is recognized that all laser-tissue interaction in surgical procedures are predominately photothermal in nature. The conversion of incident laser light energy into heat will lead to primary and, through local conduction, secondary heat effects that would allow soft tissue surgery to be carried out through tissue ablation with a supportive hemostasis. As such, the use of laser energy to effect soft tissue surgery is justified. Wavelength: The predominant chromophores in this case are melanin (tissue pigment) and hemoglobin. In addition, the prime needs of treatment would be to achieve tissue ablation with hemostasis, indicating the optimal need for using a near-infrared wavelength, such as the 810-nm diode laser.
CONTRAINDICATIONS Treatment: The only absolute contraindication to treatment in this case would be to accept the original situation. However, in view of the recent etiology and a presumed wish to prevent further exaggeration, together with the presumed improvement in function and aesthetics, such inaction could not be justified. Laser: Any surgery using laser energy carries some risk of tissue damage and this possibility must be borne in mind. Wavelength: The choice of a longer wavelength would offer a more superficial level of tissue ablation. However, in view of the need for hemostasis, longer wavelengths would require greater power parameters in order to induce conductive heat effects and this may prove damaging. Other near-infrared or visible wavelengths such as Nd:YAG (1064 nm) or KTP (532 nm) would prove suitable for such surgery, subject to correct power parameters. 5. Precautions The benefit of hemostasis offered by near-infrared laser wavelengths is accepted. In comparison to the Nd:YAG laser, the depth of penetration of the 810-nm diode laser wavelength in oral soft tissue is less, which would reduce the risk of collateral thermal damage. Nonetheless, the use of minimum power parameters, and time intervals to allow thermal relaxation and control of carbonization of the tissue and optic fiber, would all reduce the risk of primary and secondary thermal damage. General precautions applicable to the use of the 810-nm diode laser wavelength would include the need to observe caution in continuouswave laser energy delivery. Sufficient interaction to ablate structural components may not be sufficient to provide hemostasis, and power required to achieve control of blood flow may be injurious to
44
JOU R NAL OF L ASER DENTI STRY
20 0 8 VO L 16 , N O . 1
Parker
CLINICAL CASE
Figure 4: Diode laser being applied to lesion
Figure 5: Brisk hemorrhage as lesion is incised
Figure 6: Lesion excised
6. Treatment Alternatives Alternative methods for soft tissue incision would include a scalpel with possible associated suture placement or electrosurgery.
Treatment sequence Individual treatment sites were isolated and infiltration local anaesthetic (2% lignocaine 1:80,000 adrenalin) was administered. The laser was programmed to deliver 1.7 Watts CW and the laser fiber was lightly initiated using articulating paper. Each lesion was treated in turn; using tissue forceps; each lesion was placed
Parker
JOU R NAL OF L ASER DENTI STRY
surrounding soft tissue. Consequently, the ability to accurately deliver laser energy through an optic fiber can do much to prevent unwanted tissue exposure. In addition, during such procedures as this, there will be a rapid accumulation of denatured proteinaceous material onto the fiber tip and care must be exercised to remove such accumulations in order to minimize carbonization of debris. Further care should be exercised to avoid the temptation of using the optic fiber as a scalpel; it is essential that, although in contact with the tissue, the fiber be used solely as the conduit of laser energy and therefore play no part in the incision of tissue through mechanical force. Specific precautions relate to the precise delivery of laser energy to isolated soft tissue sites; wherever possible, nontarget tissue should be protected through the placement of damp gauze and positioning of a high-speed suction tube in the line of the laser beam. In addition, no reflective surfaces such as a mouth mirror should be used. The target lesion should be placed under tension, using tissue forceps to facilitate incision using minimal power parameters. Points of excessive bleeding should be treated with increased power, sufficient to induce coagulation without causing collateral damage.
7. Informed Consent The treatment plan was fully explained to the patient and all associated risks outlined. A written consent form was signed by the patient in the presence of a witness. The consent form was retained in the treatment notes.
with intervals. Total time taken: 6 minutes. C. Treatment Delivery Sequence Preliminary to patient treatment Secure operating room, define controlled area, and place proper laser warning signs. Set up laser and test proper laser operation. Test-fire laser, employing all safety measures, using minimum power settings and directing beam onto articulating paper. The objective is to ensure correct laser operation, patency of delivery system, and emission of cutting and aiming beams. In addition, the fiber tip can be inspected to ensure a proper cleave has been carried out and the spot size is uniform. Dispense supplies, and arrange equipment and sterile instruments. Review patient information. Patient seated: review treatment plan and informed consent. Safety: place eye protection, patient first followed by operating personnel.
T R E AT M E N T
A. Treatment Objectives The objective of this treatment would be to effectively remove or resect soft tissue at each of the treatment sites, with an 810-nm diode laser, with minimal peri- and postoperative complications. B. Laser Operating Parameters Laser: A diode laser (DioLase ST, American Dental Technologies, Corpus Christi, Texas, USA) was used. The operating features are as follows: Wavelength: 810 nm Co-axial aiming beam: Diode Class I laser 630-680 nm, 3 mW Emission mode: Continuous Wave (CW) with supplementary Gated CW, single pulse or repetitive single pulse Maximum power output: 12.0 Watts Delivery system: Quartz fiberoptic (320-m diameter) with conduit handpiece and disposable cannula tip Beam diameter: 320 m. Laser settings: Excision of hemangioma: 1.7 Watts. Selective coagulation of bleeding points: 2.0 Watts. Time taken per site: 1-2 minutes,
20 0 8 VO L 16 , N O . 1
45
CLINICAL CASE
Figure 7: Coagulum developed at surgical site
Figure10: Diode laser being applied to minor lesion
Figure 13: One-month postoperative view
Figure 8: Excision completed. Note buildup of debris on fiber tip
Figure 11: Excision of minor lesion complete
Figure 14: Three-month postoperative view
20 0 8 VO L 16 , N O . 1
Figure 9: Immediately postoperative
Figure 12: One-week postoperative view
Figure 15: Six-month postoperative view
JOU R NAL OF L ASER DENTI STRY
under tension and the fiber tip applied to the base. The laser energy was delivered to the tissue in a brush stroke to initiate an incision, with the fiber tip in contact mode with the tissue (Figure 4). This was developed to expose half of the lesion base. At this time, due to breach of the epithelium, some bleeding occurred which was controlled by increasing the power output to 2.0 Watts and applying the fiber tip within the bleeding site (Figures 5-6). With the absorption of energy, there was evidence of coagulation of the blood (Figures 7-8). Once controlled, the coagulum was wiped clear with a damp gauze and the process continued until a flat surface was obtained and the lesion excised, using a reverted 1.7
Watts setting. Finally, the fiber was cleaned and applied in a noncontact mode, 1-2 mm away from the surface, to define a protective coagulum (Figure 9). The process was repeated for the other treatment sites (Figures 10-11). D. Postoperative Instructions The surgical sites were shown to the patient and their appearance was explained. A chlorhexidine mouthwash was prescribed and the patient instructed to carefully apply this with cotton wool, avoiding disturbance of the coagulum; this was to be carried out three times daily during the fiveday postoperative period. The patient was advised that the appearance of the treatment sites
would change, with detachment of the coagulum and softening and hydration of the tissue at 3-5 days postoperation. The patient would be reviewed at one week. Postoperative analgesia was prescribed for use as required. There were considered no limitations on eating or drinking. The patient was instructed to call should any problem occur and was called by phone after 24 hours. E. Complications Complications that can be expected following laser soft tissue surgery can include pain, tissue swelling and deformation, bleeding, and infection. In this case, no such complications were encountered.
46
Parker
CLINICAL CASE
F. Prognosis Laser-assisted soft tissue procedures, employing correct power parameters and technique, generally have a very good prognosis. It was felt that in this case a similar outcome could be expected. G. Treatment Records All procedural details, both generally and specifically with reference to the laser use, were entered in the patients treatment notes, along with the consent details. As such, the treatment records would reflect the treatment outlined above.
F O L LOW- U P C A R E
A. Assessment of Treatment Outcome The patient was reviewed at one week, with successive examination thereafter at one month, three months, and six months (Figures 12-15). In all cases, the healing was as expected and normal lip function was maintained. B. Complications No long-term complications were observed.
dentistry since 1990. Prior to joining the Academy of Laser Dentistry in 1993, he was President of the British Dental Laser Association. He joined the Board of Directors of the Academy in 1996 and became chair of the International Relations Committee. From 1999 through 2004, he was chair of the Committee for Proficiency Recognition and coeditor of Wavelengths, the former journal of the Academy of Laser Dentistry. He was awarded the Leon Goldman award for Excellence in Clinical Laser Dentistry by the Academy in 1998. In addition, Dr. Parker holds Advanced Proficiency status in multiple laser wavelengths and completed the Academy Educator Course at the University
of California San Francisco in 2000. He is an ALD-Recognized Standard Proficiency Course Provider. He has held consultancies with multiple laser companies and has presented courses, lectures, and workshops worldwide. He has authored numerous articles on the use of lasers in dentistry, including a chapter The Use of Lasers in Fixed Prosthodontics in the October 2004 Dental Clinics of North America. Dr. Parker was the 2005 President of the Academy of Laser Dentistry. Dr. Parker may be contacted by e-mail at thewholetooth@easynet.co.uk.
Disclosure: Dr. Parker has no current affiliations with any company.
AUTHOR BIOGRAPHY
Dr. Steven Parker studied dentistry at University College Hospital Medical School, University of London, UK and graduated in 1974. He is in Private Practice in Harrogate, UK. He holds Fellowship and Diplomate status with the International Congress of Oral Implantologists. Dr. Parker has been involved in the use of lasers in
Parker
JOU R NAL OF L ASER DENTI STRY
D. Long-Term Prognosis The long-term prognosis of the treatment provided should be considered as good. The original etiology remained speculative.
20 0 8 VO L 16 , N O . 1
C. Long-Term Results The long-term results are in keeping with the objectives of the original treatment. The patient was very satisfied with the outcome. No further lesions appeared.
47
R ESEARCH AB STR ACTS
Editors Note: The following three abstracts are offered as topics of current interest. Readers are invited to submit to the editor inquiries concerning laser-related scientific topics for possible inclusion in future issues. Well scan the literature and present relevant abstracts.
L A S E R T R E AT M E N T O F VA S C U L A R L E S I O N S O F T H E L I P
In his case study involving hemangiomas of the lip (4347), Dr. Steven Parker utilizes an 810-nm diode laser with power settings between 1.7 and 2.0 Watts in continuous wave and gated pulsed modes to effect successful treatment. Relatively few reports of lip hemangioma treatment via laser appear in the dental literature per se. Case reports by Imai and colleagues1 (who used an Nd:YAG laser at unspecified operating parameters) and Sun2 (who utilized an argon laser at 1.25 Watts in pulsed mode) are notable examples. Rice3 and Kotlow4 describe treatment of venous lake of the lip, another type of vascular lesion; both practitioners used an 810-nm diode laser Rice at 1.0 Watt continuous wave, and Kotlow at 0.6 Watt continuous wave. Most reported instances of laser-assisted treatment of hemangiomas and other vascular lesions of the lips appear in the dermatologic, plastic surgery, and oral surgery literature. There, researchers and clinicians identify a variety of lasers, including 488- and 514.5nm argon,5-6 577-nm flashlamp-pumped dye,7-8 578.2-nm copper vapor,7, 9 1064-nm Nd:YAG,10-11 and 10.6-m carbon dioxide.12-13 Each author describes the rationale for wavelength choice, generally based on a particular lasers interaction with the primary chromophores of interest in these cases, oxyhemoglobin and melanin; a lasers relative depth of penetration into tissue; and its photocoagulative or hemostatic capability. A considerable portion of the published literature is devoted to treating such lesions in infants and children. Based on a classification of hemangiomas and vascular malformations formulated by Mulliken and Glowacki,14 Vesnaver and Dovsak10 note that hemangiomas tend to develop after birth, grow during the first year of life, and then gradually involute; in contrast, vascular lesions are usually noted at birth, grow as the body matures, and tend not to regress. Knowledge and diagnosis of the different types of lesions affect the selection of preferred treatment, whether administered to pediatric or adult patients. Various authors8-10, 13, 15 outline the variety of treatment modalities for treating vascular lesions of the lip: conventional surgery, embolization, oral corticosteroid therapy, cryosurgery, electrodessication, electrocautery, intralesional injection of fibrosing agents, administraV
48
JOU R NAL OF L ASER DENTI STRY
tion of interferon, laser-assisted surgery. Each has its advantages and drawbacks, and a careful study of the underlying characteristics and indications for use is warranted. Bradley16 and Vesnaver and Dovsak10 review some of the precautions to consider when using Nd:YAG lasers in treating vascular lesions, although these considerations may well apply to other laser wavelengths, particularly those exhibiting deeper penetration and those used at higher powers: Avoid perforating the mucosa covering the lesion or damaging the skin surface to avoid scarring Keep the laser tip moving to avoid overexposing a given area and minimize damage to nerves Use care when performing laser treatment near salivary glands to lessen the risk of post-treatment stenosis Consider simultaneous cooling of the skin surface to decrease skin damage. Attention to proper laser technique and precautions is always advisable. Vesnaver and Dovsak10 noted minor complications in some patients: One involved deep necrosis of lip tissue which healed uneventfully once the necrotic tissue was removed and the wound sutured in layers. Another experienced mild, transient paresthesia of the right half of the lower lip after photocoagulation of a small lesion in the right lower oral vestibulum; sensory recovery took two weeks. It bears mentioning that these investigators used 8 to 12 Watts of Nd:YAG laser power at 35-55 Hz to perform their treatments far higher power levels than dental practitioners typically employ. In the oral surgical field, treatment of large, cavernous lip hemangiomas using lasers of even higher power is not uncommon.16 Van Doorne and colleagues9 state that while complications of laser treatment of lip lesions are unusual, they may include skin atrophy, transient hyperpigmentation, slight depression of the skin, and scarring. Waner7 and Van Doorne et al.9 emphasize that principal considerations of surgery at this anatomic site require preserving the integrity of the orbicularis muscle and satisfactory lip function, maintaining oral competence, and paying special attention to cosmetic considerations including symmetry and lip length. They indicate that combining treatment modalities can
V V
20 0 8 VO L 16 , N O . 1
R ESEARCH AB STR ACTS
provide satisfactory cosmesis and lip function in most cases. As always, clinicians are advised to review the specific indications for use of their lasers and to review their operator manuals for guidance on operating parameters before attempting similar techniques on their patients.
8. Kim HJ, Colombo M, Frieden IJ. Ulcerated hemangiomas: Clinical characteristics and response to therapy. J Am Acad Dermatol 2001;44(6):962-972. 9. Van Doorne L, De Maeseneer M, Stricker C, Vanrensbergen R, Stricker M. Diagnosis and treatment of vascular lesions of the lip. Br J Oral Maxillofac Surg 2002;40(6):497-503. 10. Vesnaver A, Dovsak DA. Treatment of vascular lesions in the head and neck using Nd:YAG laser. J Craniomaxillofac Surg 2006;34(1):17-24.
V
R EF ER ENCES
1. Imai T, Matsuo N, Yamashita T, Ito A, Kamiya Y, Mizuno K, Takai Y, Fuakaya M. Two cases of hemangiomas of the upper lip in infants Treatment using the Nd:YAG laser. Aichi Gakuin Dent Sci 1991;4:35-44. 2. Sun G. Argon laser treatment of traumatic hemangiomas. Wavelengths 2000;8(3):23. 3. Rice JH. Removal of venous lake using a diode laser (810 nm). Wavelengths 2004;12(1):20-21. 4. Kotlow LA. Elimination of a venous lake on the vermilion of the lower lip via 810-nm diode laser. J Laser Dent 2007;15(1):20-22. 5. Neumann RA, Knobler RM. Venous lasers (Bean-Walsh) of the lips Treatment experience with the argon laser and 18 months follow-up. Clin Exp Dermatol 1990;15(2):115118. 6. Treloar V. Late complication of laser treatment. J Am Acad Dermatol 2003;49(6):1198. 7. Waner M. Combination approach to lip hemangiomas improves results. Clin Laser Monthly 1994;12(4):56-57.
11. Bekhor PS. Long-pulsed Nd:YAG laser treatment of venous lakes: Report of a series of 34 cases. Dermatol Surg 2006;32(9):1151-1154. 12. Ohshiro T. The CO2 laser in the treatment of cavernous hemangioma of the lower lip: A case report. Lasers Surg Med 1981;1(4):337-345. 13. Whang KK, Cho S, Seo SL. Excision of hemangioma and sculpting of the lip using carbon dioxide laser. Dermatol Surg 2004;30(12 Pt 2):1601-1602. 14. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg 1982;69(3):412-422. 15. Shapshay SM, David LM, Zeitels S. Neodymium-YAG laser photocoagulation of hemangiomas of the head and neck. Laryngoscope 1987;97(3 Pt 1):323-330. 16. Bradley PF. A review of the use of the neodymium YAG laser in oral and maxillofacial surgery. Br J Oral Maxillofac Surg 1997;35(1):26-35.
T H E C O 2 L A S E R I N T H E T R E AT M E N T O F C A V E R N O U S H A E M A N G I O M A O F T H E LOW E R L I P : A C AS E R E P O R T
Toshio Ohshiro, MD
Department of Plastic and Reconstructive Surgery, Keio University School of Medicine, Tokyo, Japan Lasers Surg Med 1981;1(4):337-345
Copyright 1981 Alan R. Liss, Inc.
JOU R NAL OF L ASER DENTI STRY
A case is reported of a 14-year-old girl who had a large cavernous haemangioma and haemangioma simplex of the lower lip. Although a few reports of such a haemangioma and the operation for it can be found in the literature, the blood loss problem and the final cosmesis leave much to be desired. We excised the tumour in two stages using the CO2 laser, retaining full
function and obtaining good configuration of the affected part. The suitability of the CO2 laser for this procedure, because of its haemostatic effect, was noted. The importance of both the physiological and psychological problems of such a patient were treated by applying our total treatment concept.
20 0 8 VO L 16 , N O . 1
49
R ESEARCH AB STR ACTS
U L C E R AT E D H E M A N G I O M A S : C L I N I C A L C H A R A C T E R I S T I C S A N D R E S P O N S E TO T H E R A P Y
Ho Jin Kim, MD
Division of Pediatric Dermatology, Childrens Hospital of Philadelphia, Pennsylvania
Mary Columbo, RN and Ilona J. Frieden, MD
University of California, San Francisco, California J Am Acad Dermatol 2001;44(6):962-972 doi:10.1067/mjd.2001.112382
20 0 8 VO L 16 , N O . 1
Background: Hemangiomas represent the most common benign tumor of infancy, with ulceration its most frequent complication. Objective: Our purpose was to review our experience with this challenging problem by evaluating the clinical features, management, and therapeutic responses of ulcerated hemangiomas. Methods: A retrospective analysis of ulcerated hemangiomas at the University of California, San Francisco outpatient pediatric dermatology clinics and Oakland Childrens Hospital from 1987 to 1997 was performed. Results: The medical records of 60 patients were examined. Forty-nine female and 11 male patients were seen with a female/male ratio of 4.5:1. The majority of ulcerated hemangiomas were of the plaque type (n = 50; 83%) and relatively large; 47 (78%) were larger than 6 cm2. The perineum was the single most frequently involved site, affected in 20 cases (33%). Topical antibiotics, barrier creams, and bio-occlusive dressings were used in most cases. Systemic antibiotics were used in 26 cases (43%) for overt or presumed infection. Systemic corticosteroids were used in 21 children (37%), 5 of whom did not show a response. Intralesional triamcinolone was used in 7 cases (12%), with 4 showing definite improvement. The flashlamp pulsed-
dye laser was the modality used in 22 children (37%), 11 (50%) of whom showed definite improvement, 4 (18%) who showed no significant response, and 1 (5%) who showed definite worsening. Interferon alfa-2a was required in 5 patients (8%), all of whom showed improvement without appreciable neurologic side effects. Immediate surgical excision was required in only 2 cases (3%). Pain control with oral acetaminophen, acetaminophen with codeine, and topical 2.5% lidocaine ointment was effective in managing the pain of lip and perineal hemangiomas, with no side effects noted. Conclusion: No one uniformly effective treatment modality was found, and frequently several were used concurrently. The decision to use specific therapies was dependent on the age of the patient, as well as the location, size, and stage of growth or involution of the hemangioma. Our approach to management included 4 major areas: local wound care, management of infection, specific therapeutic modalities (systemic and intralesional corticosteroids, flashlamp pulsed-dye laser, and interferon alfa-2a), and pain management.
Copyright 2001 American Academy of Dermatology
T R E AT M E N T O F VA S C U L A R L E S I O N S I N T H E H E A D A N D N E C K U S I N G N D : YA G L A S E R
Ales Vesnaver, MD, M.Sc.
V
Department of Maxillofacial and Oral Surgery, University Medical Center, Ljubljana, Slovenia
David A. Dovsak
V
J Craniomaxillofac Surg 2006;34(1):17-24. Epub 2005 Dec 13 doi:10.1016/j/jcms.2005.07.009
JOU R NAL OF L ASER DENTI STRY
Introduction: Vascular lesions in the head and neck region, including both haemangiomas and vascular malformations, are common and many different treatment modalities have been used for their removal. In the past decade, the Nd:YAG laser has emerged as a new mode of treatment for vascular lesions, and the purpose of this paper was to determine its clinical value. Patients and Methods: A prospective study was conducted in 111 patients with vascular lesions in the head and neck region. They were treated with the Nd:YAG laser by photocoagulation. Of these, 96 had small lesions, with surface diameters of less than 3 x 3
cm2, and 5 had large lesions, with surface diameters of more than 3 x 3 cm2. The patients were all followed up carefully until complete healing was recorded, along with any complications. Results: In both groups of patients, tissue sloughing occurred within 2-3 days. Healing time in small lesions was 2-3 weeks, and in large lesions 3-4 weeks. Three patients with small lesions and one patient with a large lesion experienced minor complications. Conclusion: The Nd:YAG laser is a safe and effective tool for treating vascular lesions.
Copyright 2005 European Association for Cranio-Maxillofacial Surgery
50
Potrebbero piacerti anche
- Health Risks and How To Quit (PDQ®)Documento20 pagineHealth Risks and How To Quit (PDQ®)Eliza DNNessuna valutazione finora
- Radiological Patterns of Lung Involvement in Inflammatory Bowel Disease.Documento10 pagineRadiological Patterns of Lung Involvement in Inflammatory Bowel Disease.Eliza DNNessuna valutazione finora
- Treatments For ConstipationDocumento27 pagineTreatments For ConstipationEliza DNNessuna valutazione finora
- Smoking Resumption After Heart or Lung TransplantationDocumento10 pagineSmoking Resumption After Heart or Lung TransplantationEliza DNNessuna valutazione finora
- Acs 33 233Documento8 pagineAcs 33 233Eliza DNNessuna valutazione finora
- 2018 Korean Clinical Imaging Guideline For HemoptysisDocumento6 pagine2018 Korean Clinical Imaging Guideline For HemoptysisEliza DNNessuna valutazione finora
- 2008 NOHC - JPHDSupplementDocumento62 pagine2008 NOHC - JPHDSupplementEliza DNNessuna valutazione finora
- Modified Reasons For Smoking ScalDocumento7 pagineModified Reasons For Smoking ScalEliza DNNessuna valutazione finora
- Supplementary File Survey Question Response OptionsDocumento3 pagineSupplementary File Survey Question Response OptionsEliza DNNessuna valutazione finora
- Orh cdh21-4 P1to11Documento11 pagineOrh cdh21-4 P1to11Eliza DNNessuna valutazione finora
- Interdisciplinary Culture FinalDocumento3 pagineInterdisciplinary Culture FinalEliza DNNessuna valutazione finora
- DambrunRicardetal2012 MeasuringHappinessDocumento11 pagineDambrunRicardetal2012 MeasuringHappinessEliza DNNessuna valutazione finora
- Dental Public Health MSCDocumento4 pagineDental Public Health MSCEliza DNNessuna valutazione finora
- Wirth Et Al 2011 PnecDocumento10 pagineWirth Et Al 2011 PnecEliza DNNessuna valutazione finora
- Optimal Management of Collagenous Colitis A Review 021016Documento9 pagineOptimal Management of Collagenous Colitis A Review 021016Eliza DNNessuna valutazione finora
- Oral Health Inequalities PolicyDocumento13 pagineOral Health Inequalities PolicyEliza DNNessuna valutazione finora
- Understanding Inequalities of Maternal Smoking-Bridging The Gap With Adapted Intervention StrategiesDocumento16 pagineUnderstanding Inequalities of Maternal Smoking-Bridging The Gap With Adapted Intervention StrategiesEliza DNNessuna valutazione finora
- Chapter 10global Hazards of Tobacco and The Benefits of Smoking Cessation and Tobacco TaxesDocumento363 pagineChapter 10global Hazards of Tobacco and The Benefits of Smoking Cessation and Tobacco TaxesEliza DN100% (1)
- An Updated Review of Case-Control Studies of Lung Cancer and Indoor Radon-Is Indoor Radon The Risk Factor For Lung Cancer?Documento9 pagineAn Updated Review of Case-Control Studies of Lung Cancer and Indoor Radon-Is Indoor Radon The Risk Factor For Lung Cancer?Eliza DNNessuna valutazione finora
- Scand J Work Environ Health:310-318 Doi:10.5271/sjweh.3334: Original ArticleDocumento10 pagineScand J Work Environ Health:310-318 Doi:10.5271/sjweh.3334: Original ArticleEliza DNNessuna valutazione finora
- Nater & Rohleder-sAA & SNS-PNEC 09Documento11 pagineNater & Rohleder-sAA & SNS-PNEC 09Eliza DNNessuna valutazione finora
- InTech-Physiological Response As Biomarkers of Adverse Effects of The Psychosocial Work EnvironmentDocumento17 pagineInTech-Physiological Response As Biomarkers of Adverse Effects of The Psychosocial Work EnvironmentEliza DNNessuna valutazione finora
- Alpha Amylase StressDocumento10 pagineAlpha Amylase StressEliza DNNessuna valutazione finora
- KoreaDocumento7 pagineKoreaEliza DNNessuna valutazione finora
- PerfectionismDocumento7 paginePerfectionismEliza DNNessuna valutazione finora
- Amilaza FearDocumento3 pagineAmilaza FearEliza DNNessuna valutazione finora
- Hansen Review CortisolDocumento12 pagineHansen Review CortisolEliza DNNessuna valutazione finora
- Cognitiive Emotion RegulationDocumento6 pagineCognitiive Emotion RegulationEliza DNNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Churches That Have Left RCCG 0722 PDFDocumento2 pagineChurches That Have Left RCCG 0722 PDFKadiri JohnNessuna valutazione finora
- PT - Science 5 - Q1Documento4 paginePT - Science 5 - Q1Jomelyn MaderaNessuna valutazione finora
- Transfer Pricing 8Documento34 pagineTransfer Pricing 8nigam_miniNessuna valutazione finora
- Logic of English - Spelling Rules PDFDocumento3 pagineLogic of English - Spelling Rules PDFRavinder Kumar80% (15)
- Performance MeasurementDocumento13 paginePerformance MeasurementAmara PrabasariNessuna valutazione finora
- Caregiving Learning Activity Sheet 3Documento6 pagineCaregiving Learning Activity Sheet 3Juvy Lyn CondaNessuna valutazione finora
- Roman Roads in Southeast Wales Year 3Documento81 pagineRoman Roads in Southeast Wales Year 3The Glamorgan-Gwent Archaeological Trust LtdNessuna valutazione finora
- An Etymological Dictionary of The Scottivol 2Documento737 pagineAn Etymological Dictionary of The Scottivol 2vstrohmeNessuna valutazione finora
- TN Vision 2023 PDFDocumento68 pagineTN Vision 2023 PDFRajanbabu100% (1)
- Berrinba East State School OSHC Final ITO For Schools Final 2016Documento24 pagineBerrinba East State School OSHC Final ITO For Schools Final 2016hieuntx93Nessuna valutazione finora
- W2-Prepares Feasible and Practical BudgetDocumento15 pagineW2-Prepares Feasible and Practical Budgetalfredo pintoNessuna valutazione finora
- APICS-Houston Newsletter Sept 2012Documento16 pagineAPICS-Houston Newsletter Sept 2012Christopher SeifertNessuna valutazione finora
- Name: Kartikeya Thadani Reg No.: 19bma0029Documento4 pagineName: Kartikeya Thadani Reg No.: 19bma0029Kartikeya ThadaniNessuna valutazione finora
- Debarchana TrainingDocumento45 pagineDebarchana TrainingNitin TibrewalNessuna valutazione finora
- 60617-7 1996Documento64 pagine60617-7 1996SuperhypoNessuna valutazione finora
- Athena 60 Installation Manual EN 2022.07.03Documento30 pagineAthena 60 Installation Manual EN 2022.07.03joaquin.cadondonNessuna valutazione finora
- Malate SynthaseDocumento8 pagineMalate SynthaseMinichNessuna valutazione finora
- Conductivity MeterDocumento59 pagineConductivity MeterMuhammad AzeemNessuna valutazione finora
- Tangazo La Kazi October 29, 2013 PDFDocumento32 pagineTangazo La Kazi October 29, 2013 PDFRashid BumarwaNessuna valutazione finora
- Torah Hebreo PaleoDocumento306 pagineTorah Hebreo PaleocamiloNessuna valutazione finora
- Entrepreneurial Skills and Intention of Grade 12 Senior High School Students in Public Schools in Candelaria Quezon A Comprehensive Guide in Entrepreneurial ReadinessDocumento140 pagineEntrepreneurial Skills and Intention of Grade 12 Senior High School Students in Public Schools in Candelaria Quezon A Comprehensive Guide in Entrepreneurial ReadinessAngelica Plata100% (1)
- Seminar On DirectingDocumento22 pagineSeminar On DirectingChinchu MohanNessuna valutazione finora
- Undertaking:-: Prime Membership Application Form (Fill With All Capital Letters)Documento3 pagineUndertaking:-: Prime Membership Application Form (Fill With All Capital Letters)Anuj ManglaNessuna valutazione finora
- Outline - Criminal Law - RamirezDocumento28 pagineOutline - Criminal Law - RamirezgiannaNessuna valutazione finora
- Government by Algorithm - Artificial Intelligence in Federal Administrative AgenciesDocumento122 pagineGovernment by Algorithm - Artificial Intelligence in Federal Administrative AgenciesRone Eleandro dos SantosNessuna valutazione finora
- Dummies Guide To Writing A SonnetDocumento1 paginaDummies Guide To Writing A Sonnetritafstone2387100% (2)
- Alice (Alice's Adventures in Wonderland)Documento11 pagineAlice (Alice's Adventures in Wonderland)Oğuz KarayemişNessuna valutazione finora
- 2017 - The Science and Technology of Flexible PackagingDocumento1 pagina2017 - The Science and Technology of Flexible PackagingDaryl ChianNessuna valutazione finora
- Jurnal UlkusDocumento6 pagineJurnal UlkusIndri AnggraeniNessuna valutazione finora
- Animal Welfare in Bangladesh and The Role of Obhoyaronno CaseDocumento11 pagineAnimal Welfare in Bangladesh and The Role of Obhoyaronno CaseZarin Tanjim WoyshorjoNessuna valutazione finora