Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Feeding Via Gastric Gavage
Caricato da
neleh grayTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Feeding Via Gastric Gavage
Caricato da
neleh grayCopyright:
Formati disponibili
Feeding Via Gastric Gavage Gastric Gavage is a means of supplying nutritional substance via a small plastic tube direct
to the stomach. This post will help you understand on how to perform feeding via gastric gavage. Objective of Gastric Gavage
Charting of Gastric Gavage
Describe and record procedure Time of feeding Type of Gavage feeding Type and amount of fluid given Amount retained or vomited Patients reaction to the procedure.
To provide a means of alimentation when the oral route is inaccessible.
Indications of Gastric Gavage
Gastrointestinal diseases and surgery Hypermetabolic states (burns,multiple trauma,sepsis,cancer) Certain neurologic disorders (stroke and coma) Following certain types of surgery (head and neck, esophagus)
Equipment Needed for Gastric Gavage Feeding fomula Calibrated drinking glass Bowl Acepto syringe Medicine glass with tap water
Contraindication of Gastric Gavage
Absent bowel sounds
After Care of Gastric Gavage Wash or let the significant other of the patient do the washing of the materials used in feeding. Keep all the materials used in its proper place. Refrigerae the osterized feeding.
Nursing Alert: Tube feedings are contraindicated to patients without bowel sounds. Administration of feeding solution to an improperly placed tube may cause aspiration into the lungs.
Gastric Gavage Nursing Interventions & Rationale Nursing Interventions Explain procedure to client. Assemble equipment. Check amount, concentration, type and frequency tube feeding on clients chart. Wash your hands. Position client with the head of bead elevated at least 30 degrees angel or as near normal position for eating as possible. Unpin tube from clients gown and check to see that the gastric tube is properly located in the stomach. Aspirate all gastric contents with syringe and measure. Return immediately through tube and proceed with feeding if amount of residual does not exceed policy of agency or physicians guidelines. Disconnect syringe from tubing. When using Asepto sringe or Toomey syringe: a.Remove plunger or bulb from syringe and attach syringe to nasogastric tube which has been pinched with finger and introduce the prescribed amount slowly. b.Hold the syringe approximately 12 inches above the stomach. Allow solution to run in by gravity. Raise the syringe to increase the rate of flow, and lower the syringe to decrease the rate of flow. c.Do not let the syringe empty while introducing the nourishment. d.Introduce 30ml 60mL (1 oz 2 oz) of water into the tube after the nourishment is introduced. e.Clamp the gastric tube immediately after nourishment and water are instilled. Disconnect the syringe and cover end of tubing with gauze secured with rubber band. When using a feeding bag: a.Hang bag on IV pole and adjust to about 12 inches above the stomach. Clamp tubing and pour formula into the bag. Release clamp enough to allow formula to run
Rationale Facilitates cooperation and provides reassurance for client. Provide for organized approached to task. Ensures the correct feeding will be administered. Handwashing deters the spread of microorganisms. Minimize possibility of aspiration into trachea. Even when initially positioned correctly, a gastric tube left in place can become dislodged between feedings. The instillation of water or nourishment could lead to serious respiratory problems if a gastric tube is in the trachea or a bronchus, rather than in a stomach. This indicate gastric emptying time. A residual of more than 50% of the previous hours intake is significant and must be reported to physician. Fluid should be returned to stomach so as not to cause any fluid or electrolytes losses. a. The syringe acts to receive the nourishment. Introducing the nourishment slowly gives the stomach time to accommodate the fluid and decreases gastrointestinal distress. b. Nourishment enters the stomach by gravity when gastric gavage is used. c. This technique prevents air from being forced into the stomach when the syringe is refilled. d. Washing the gastric tube with water forces remaining nourishment in the tube into the stomach and prevents nourishment from adhering to the tube and souring. e. Clamping the tube prevents nourishment from draining back into the tube and air from entering the stomach. Cover on end of the tube deters entry of microorganisms and protects client and linens form any fluid leakage from tube.
a. Formula displaces air in the tubing
through tubing. Close clamp. b.Attach tubing to nasogastric tube, open clamp and regulate drip according to physicians order. c.Add 30 ml 60 ml (1 oz 2 oz) of water to feeding bag when feeding is almost completed and allow to run through tube. d.Clamp the tubing immediately after water has been instilled. Disconnect from nasogastric tube and cover gauze secured with a rubber bad. When using pre-filled tube feeding set-up: a.Remove screw-on cap and attach administration set-up with drip chamber and tubing. Hang set on IV pole and adjust to about 12 inches above the stomach. Clamp tubing and squeeze drip chamber to fill one-third to one-half of capacity. Release clamp and run formula through tubing. Close clamp. b.Follow steps 8b and 8d. Feeding pump may be used with the tube feeding set-up to regulate drip. Observe clients response during and after tube feeding. Have client remain in upright position for at least 30 minutes after feeding. Wash and clean equipment or replace according to agency policy. Wash your hands. Record type and amount of feeding and clients response. Monitor urine or blood glucose if ordered by physician. Irrigating a Nasogastric Tube A nasogastric tube is irrigated regularly to determine/ensure the patency of the tube. Learn how to irrigate a nasogastric tube (NGT). Objective b. Introducing the formula at a slow, regular rate allow the stomach to accommodate the feeding and decreases gastrointestinal distress. c. Water rinse the feeding from the tube and helps to keep it patent. d. Clamping the tube prevents air from entering the stomach. Cover on end of nasogastric tube deters entry of microorganisms and protects client and linens from any fluid leakage from tube. a. Formula displaces air in tubing.
Pain may indicate stomach distention which may lead to vomiting. This position minimizes risk of backflow and discourage aspiration should any vomiting occurs. Prevents contamination and deters spread of microorganisms. Provides accurate documentation or procedure. Many feedings contain high loads of carbohydrates. Suction-drainage tube. With double-lumen tube, if main lumen is probably blocked, clear the main lumen, then inject up to 60 cc of air through the short lumen above the level of the stomach where the end of the main lumen is located. Equipment 1. Nasogastric tube connected to continuous or intermittent suction. 2. Irrigation or Toomey syringe and container for irrigating solution. 3. Normal saline for irrigation. 4. Disposable pad or bath towel 5. Disposable gloves (optional) 6. Stethoscope 7. Clamp
To ensure the patency of the nasogastric tube. Indication Stomach contents fail to flow through tube. Contraindication
Some tubes are maintained by airflow, not normal saline solution.
Nursing Alert: Connect proper end (main lumen) of double lumen tube to suction. The short lumen is an airway, not a
Nursing Interventions & Rationale Nursing Interventions Check physicians order for irrigation. Explain procedure to client. Gather necessary equipment. Check expiration dates on irrigating saline and irrigation set. Wash your hands. Assist client to semi-Fowlers position unless this is contraindicated. Check placement of NG tube; a. Attach Asepto or Toomey syringe to the end of tube and aspirate gastric contents.b. Place 10mL-50ml of air in syringe and inject into the tube. Simultaneously, auscultate over the epigastric area with a stethoscope. c. Ask client to speak. Clamp suction tubing near connection site. Disconnect NG tube from suction apparatus and lay on disposasble pad or towel. Pour irrigating solution into container. Draw up 30 ml of saline (or amount ordered by physician) into syringe. Place tip of syringe in NG tube. Hold syringe upright and gently insert the irrigant (or allow solution to flow in by gravity if agency or physician indicates). Do not force solution into NG tube. If unable to irrigate tube, reposition client and attempt irrigation again. Check with physician if repeated attempts to irrigate tube fail. Withdraw or aspirate fluid into syringe. If no return, inject 20 ml of air and aspirate again. Reconnect NG tube to suction. Observe movement of solution or drainage. Measure and record amount and description of irrigant and return solution. Rinse equipment if it will be reused. Wash your hands Record irrigation procedure, description of drainage and clients response.
Rationale Clarifies schedule and irrigating solution. An explanation encourages client cooperation and reduces apprehension. Provides for organized approached to task. Agency policy dictates safe interval for reuse of equipment. Handwashing deters the spread of microorganisms. Minimizes risk of aspiration. a. The tube is in the stomach if its contents can be aspirated.b. A whoosing sound can be heard when the air enters the stomach through the tube. c. If tube is misplaced in trachea, client will not be able to speak. Protects client from leakage of NG drainage. Delivers measured amount of irrigant through NG tube. Saline compensates for electrolytes lost through NG drainage. Position of syringe prevents entry of air into stomach. Gentle insertion of saline (or gravity insertion) is less traumatic to gastric mucosa. Tube may be positioned against gastric mucosa making it difficult to irrigate. Inject of air may reposition the end of tube. Determine patency of NG tube and correct operation of suction apparatus. Irrigant placed in NG tube is considered intake: solution returned is recorded as output. Promotes cleanliness and prepares equipment for next irrigation. Handwashing deters the spread of microorganisms. Facilitates documentation of procedure and provides for comprehensive care.
Removing a Nasogastric Tube Objectives
Measuring nasogastric drainage provides for accurate recording of output. Proper disposal deters spread of microorganisms. 12. Record removal of nasogastric tube, clients response, and measurement of drainage. Facilitates documentation and provides for comprehensive care.
After Care
To check if the patient can tolerate oral feeding.
Contraindications Continuing need for feeding/suction.
Charting
Discard the disposasble equipment used. Wash your hands. Position the patient in a comfortable or in his desired position.
Record date of removal of nasogastric tube. Record clients response. Record measurement of drainage.
Nursing Alert: Removal is easier with the patient in semi-Fowlers position. Equipment:
1. 2. 3. 4.
Tissues Plastic disposable bag Bath towel or disposable pad Clean disposable glove
Nursing Interventions & Rationale 1. Check physicians order for removal of nasogastric tube. Ensures correct implementation of physicians order. 2. Explain procedure to client. Explanation facilitates client cooperation. 3. Gather equipment. Provides for organized approach to task. 4. Wash your hands. Don clean disposable glove on hand that will remove tube. Handwashing deters the spread of microorganisms. Gloves protect hand from contact with abdominal secretions. 5. Discontinue suction and separate tube from suction. Unpin tube from cleints gown and carefully remove adhesive tape from bridge of nose. Allows for unrestricted removal of nasogastric tube. 6. Place towel or disposable pad across clients chest. Hand tissues to client. Protects client from contact with gastric secretions. Tissues are necessary if client wishes to blow his nose when tube is removed. 7. Instruct client to take a deep breath and hold it. Prevents accidental aspiration of any gastric secretions in tube. 8 Clamp tube with fingers. Quickly and carefully remove tube while client holds his breath. Minimizes trauma and discomfort for client. Clamping prevents any drainage of gastric contents in tube. 9 Place tube in disposable plastic bag. Remove glove and place in bag. Prevents contamination with any microorganisms. 10. Offer mouth care to client and make client feel comfortable. Provides comfort. 11. Measure nasogastric drainage. Remove all equipment and dispose according to agency policy. Wash your hands.
Potrebbero piacerti anche
- Nasogastric Tube InsertionDocumento8 pagineNasogastric Tube InsertionMayaPopbozhikovaNessuna valutazione finora
- Tube Feeding (GavageDocumento2 pagineTube Feeding (GavageevergrayelleNessuna valutazione finora
- Gastric Gavage OR Enteral: Naso/Orogastric Gastrostomy: Mrs .Jenifer Kaliso TutorDocumento39 pagineGastric Gavage OR Enteral: Naso/Orogastric Gastrostomy: Mrs .Jenifer Kaliso TutorSharon LawrenceNessuna valutazione finora
- ) Administering Nasogastric Tube or Orogastric Tube FeedingDocumento6 pagine) Administering Nasogastric Tube or Orogastric Tube FeedingJohn Pearl FernandezNessuna valutazione finora
- NGT Feeding: by Group 2Documento25 pagineNGT Feeding: by Group 2karl montano100% (1)
- Administering Tube Feedings SafelyDocumento2 pagineAdministering Tube Feedings SafelyJoyce Madarang100% (1)
- Gordon's Health Pattern ChecklistDocumento3 pagineGordon's Health Pattern ChecklistNavora, Bryle TrixthaneNessuna valutazione finora
- Nso ErcpDocumento3 pagineNso Ercptry dokkNessuna valutazione finora
- Colostomy Irrigation ProcedureDocumento3 pagineColostomy Irrigation Proceduresenyorakath0% (1)
- NCM 116 ChecklistsDocumento14 pagineNCM 116 Checklistsmark OrpillaNessuna valutazione finora
- Checklist NGT - FinalDocumento5 pagineChecklist NGT - FinalKim Tan100% (2)
- Colostomy Care ChecklistDocumento5 pagineColostomy Care ChecklistLynette JavaNessuna valutazione finora
- NGT Feeding ChecklistDocumento1 paginaNGT Feeding ChecklistJoycee BoNessuna valutazione finora
- Administering An EnemaDocumento2 pagineAdministering An EnemaJazzmin Angel ComalingNessuna valutazione finora
- Lab Clin Clin Tasks Attempted 1 2 3 4 5 6 7: ST ND RD TH TH TH THDocumento4 pagineLab Clin Clin Tasks Attempted 1 2 3 4 5 6 7: ST ND RD TH TH TH THRichard Patterson100% (1)
- Procedure Checklist Chapter 27: Continuous Bladder IrrigationDocumento2 pagineProcedure Checklist Chapter 27: Continuous Bladder IrrigationjthsNessuna valutazione finora
- Nasogastric Tube InsertionDocumento11 pagineNasogastric Tube InsertionDiane Kate Tobias Magno100% (1)
- Nasogastric Tube Feeding Definition:: University of Eastern PhilippinesDocumento2 pagineNasogastric Tube Feeding Definition:: University of Eastern PhilippinesJerika Shane MañosoNessuna valutazione finora
- Colostomy IrrigationDocumento3 pagineColostomy IrrigationJikko Verra GarciaNessuna valutazione finora
- Nursing Procedure Guide - Urinary Catheter InsertionDocumento3 pagineNursing Procedure Guide - Urinary Catheter Insertionmharmukim03Nessuna valutazione finora
- Water Seal Chest DrainageDocumento5 pagineWater Seal Chest DrainageAmadelle FaithNessuna valutazione finora
- Gastric LavageDocumento2 pagineGastric LavageIrish Eunice FelixNessuna valutazione finora
- NG TubeDocumento3 pagineNG TubeKenny JosefNessuna valutazione finora
- Newborn Care ChecklistDocumento5 pagineNewborn Care Checklistburntashes100% (1)
- PATENTE - Worksheet - Nasogastric Tube Insertion, Feeding, and RemovalDocumento11 paginePATENTE - Worksheet - Nasogastric Tube Insertion, Feeding, and RemovalSelwynVillamorPatenteNessuna valutazione finora
- NGT GavageDocumento29 pagineNGT GavageMaan LapitanNessuna valutazione finora
- CHECKLIST Hot and Cold Application WITH RATIONALEDocumento5 pagineCHECKLIST Hot and Cold Application WITH RATIONALEBryle NavoraNessuna valutazione finora
- Tools of the Public Health NurseDocumento23 pagineTools of the Public Health NurseNiño PaoloNessuna valutazione finora
- Nursing Ear Irrigation ChecklistDocumento1 paginaNursing Ear Irrigation ChecklistOrl Trinidad0% (1)
- Using Mechanical Aids For WalkinDocumento38 pagineUsing Mechanical Aids For Walkinshannon c. lewisNessuna valutazione finora
- Care of WoundsDocumento6 pagineCare of WoundsKimpoy Tu-osNessuna valutazione finora
- Gastrostomy FeedingDocumento9 pagineGastrostomy FeedingJamie Luz Tongco0% (1)
- Tracheostomy Care With ChecklistDocumento5 pagineTracheostomy Care With ChecklistHollan GaliciaNessuna valutazione finora
- Nasogastric Tube Feeding GuideDocumento20 pagineNasogastric Tube Feeding GuideKrishna Sonu SoniNessuna valutazione finora
- NGT InsertionDocumento10 pagineNGT Insertionapi-3722454100% (3)
- Gavage Syringe or Funnel MethodDocumento2 pagineGavage Syringe or Funnel MethodLea Jean Lobrigo OleaNessuna valutazione finora
- Assessment-Checklist EyesDocumento2 pagineAssessment-Checklist EyesJL Rebese100% (2)
- Procedure - Gastric LavageDocumento2 pagineProcedure - Gastric LavageJose Paul RaderNessuna valutazione finora
- NSO Gastric LavageDocumento3 pagineNSO Gastric Lavagetry dokkNessuna valutazione finora
- Ostomies: LessonDocumento21 pagineOstomies: Lessonlovelykiss100% (1)
- Gastric Lavage TechniqueDocumento15 pagineGastric Lavage TechniqueEm BelandoNessuna valutazione finora
- Catheter ExamDocumento2 pagineCatheter ExamAnjo CincoNessuna valutazione finora
- PBBN 1St Yr Child Health Nursing CBIMNCIDocumento29 paginePBBN 1St Yr Child Health Nursing CBIMNCIcopy smart100% (1)
- Nursing Care for Patients with ColostomyDocumento26 pagineNursing Care for Patients with ColostomyKyle Ü D. CunanersNessuna valutazione finora
- NGT Feeding and Meds Administration Via NGTDocumento25 pagineNGT Feeding and Meds Administration Via NGTPaul Michael BaguhinNessuna valutazione finora
- Gastric LavageDocumento17 pagineGastric LavageCharizza Yvette100% (1)
- 17 Enteral and Parenteral NutritionDocumento47 pagine17 Enteral and Parenteral NutritionKathleen AngNessuna valutazione finora
- NG Tube, Lavage and Gavage Procedure ChecklistDocumento6 pagineNG Tube, Lavage and Gavage Procedure ChecklistBitew Tefera ZewudieNessuna valutazione finora
- Wound CareDocumento3 pagineWound CaregrangerhermionepNessuna valutazione finora
- Post-Op Bed Making ChecklistDocumento6 paginePost-Op Bed Making ChecklistRoselyn Y. QuintoNessuna valutazione finora
- Care of Patients with Chest Drainage SystemsDocumento29 pagineCare of Patients with Chest Drainage SystemsMSc. PreviousNessuna valutazione finora
- Per Cutaneous Trans Hepatic Cholangiogram (PTC)Documento15 paginePer Cutaneous Trans Hepatic Cholangiogram (PTC)Hamzeh AlmasriNessuna valutazione finora
- Colostomy Care ChecklistDocumento6 pagineColostomy Care ChecklistTensai Olive DundundNessuna valutazione finora
- Colostomy Care PDFDocumento5 pagineColostomy Care PDFBrian96cortez100% (3)
- Wound Care ChecklistDocumento4 pagineWound Care ChecklistGelo BallartaNessuna valutazione finora
- NCM - PC & VeDocumento5 pagineNCM - PC & VeYanna Habib-Mangotara100% (1)
- Language, Orientation, Memory, Attention Span and Calculation, LOCDocumento7 pagineLanguage, Orientation, Memory, Attention Span and Calculation, LOCYessamin Paith RoderosNessuna valutazione finora
- NGT DemoDocumento5 pagineNGT Demoeliza luisNessuna valutazione finora
- Nasogastric & Gavage - NsoDocumento5 pagineNasogastric & Gavage - NsojamesNessuna valutazione finora
- Sarasota Memorial Hospital Nursing Procedure Title: Date: Reviewed: Pages: Issued For: ResponsibilityDocumento5 pagineSarasota Memorial Hospital Nursing Procedure Title: Date: Reviewed: Pages: Issued For: Responsibilitybalab2311Nessuna valutazione finora
- ncm105 /mental HealthDocumento8 paginencm105 /mental Healthneleh grayNessuna valutazione finora
- Glossary of Immune System TermsDocumento5 pagineGlossary of Immune System Termsneleh grayNessuna valutazione finora
- Peptic UlcerDocumento4 paginePeptic Ulcerneleh grayNessuna valutazione finora
- Immunology Notes 104Documento29 pagineImmunology Notes 104neleh grayNessuna valutazione finora
- Vital Signs TableDocumento5 pagineVital Signs Tableneleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- BurnsDocumento7 pagineBurnsneleh grayNessuna valutazione finora
- Peptic UlcerDocumento4 paginePeptic Ulcerneleh grayNessuna valutazione finora
- Physical Assessment Guide of Head-To-ToeDocumento9 paginePhysical Assessment Guide of Head-To-Toeneleh gray100% (2)
- Key Areas of ResponsibilityDocumento2 pagineKey Areas of Responsibilityneleh grayNessuna valutazione finora
- Fundamentals of Nursing NotesDocumento11 pagineFundamentals of Nursing Notesneleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- Terms and AbbreviationsDocumento67 pagineTerms and Abbreviationsneleh grayNessuna valutazione finora
- Dehydration Causes and SymptomsDocumento7 pagineDehydration Causes and Symptomsneleh grayNessuna valutazione finora
- CBVDDocumento55 pagineCBVDneleh grayNessuna valutazione finora
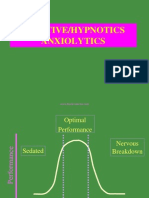
- An Xy Olitics HypnoticsDocumento59 pagineAn Xy Olitics Hypnoticsneleh grayNessuna valutazione finora
- CASE STUDY of AGE With Moderate DehydrationDocumento13 pagineCASE STUDY of AGE With Moderate Dehydrationneleh grayNessuna valutazione finora
- Sedative Hypnotics Anxiolytics Benzodiazepines BarbituratesDocumento60 pagineSedative Hypnotics Anxiolytics Benzodiazepines Barbituratesneleh grayNessuna valutazione finora
- Neurological DisorderDocumento262 pagineNeurological Disorderneleh grayNessuna valutazione finora
- Small Bowel ObstructionDocumento3 pagineSmall Bowel Obstructionneleh grayNessuna valutazione finora
- Terms and AbbreviationsDocumento89 pagineTerms and Abbreviationsneleh grayNessuna valutazione finora
- Small Bowel ObstructionDocumento3 pagineSmall Bowel Obstructionneleh grayNessuna valutazione finora
- Small Bowel ObstructionDocumento3 pagineSmall Bowel Obstructionneleh grayNessuna valutazione finora
- Fundamentals of NursingDocumento3 pagineFundamentals of Nursingneleh grayNessuna valutazione finora
- Family PlanningDocumento9 pagineFamily Planningneleh grayNessuna valutazione finora
- Cerebral Anatomy and Physiology Part Iids08Documento25 pagineCerebral Anatomy and Physiology Part Iids08rocketwapNessuna valutazione finora
- Blood Supply of The BrainDocumento11 pagineBlood Supply of The Brainneleh grayNessuna valutazione finora
- Feeding Via Gastric GavageDocumento3 pagineFeeding Via Gastric Gavageneleh gray0% (1)
- Feeding Via Gastric GavageDocumento3 pagineFeeding Via Gastric Gavageneleh gray0% (1)