Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Geriatric Medication Hints and Warnings
Caricato da
Erika HarveryDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Geriatric Medication Hints and Warnings
Caricato da
Erika HarveryCopyright:
Formati disponibili
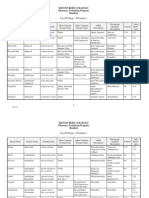
Geriatric Pharmacology: Quick Facts and Tips A. Egbert 7/01 1.
The chance of an adverse drug event (ADE) or drug-drug interaction (DDI) increases with the number of drugs. In age, 15-50% of all hospital admissions are due to ADEs. In a patient taking more than 5 drugs, the statistical chance of a DDI or ADE is 100%. 2. Many drugs are distributed [are active] primarily into the bodys water compartment. Total body water decreases significantly with age. Diuretics and poor oral intake worsen this. Therefore, there is a greater risk of drug toxicity. Examples: digoxin, theophylline, lithium, aminoglycosides, anti-arrhythmics, lidocaine. 3. In age, renal function declines about 1% per year over age 50. This is markedly increased if the patient is also dehydrated. The majority of drugs are renally excreted and are therefore at risk to accumulate. Examples: meperidine, metabolites of morphine, anti-arrhythmics. 4. In age, liver function stays about the same under normal circumstances. However, liver blood flow is decreased with dehydration or CHF, and liver function decline with cachexia or metastases. Therefore many drugs have prolonged half-lives: tricyclic antidepressants, many opioids, verapamil, benzodiazepines. 5. Elderly people are very susceptible to anticholinergic drugs. They cause delirium, memory loss, urinary retention, constipation, dry eyes and mouth) CLUE: Any drug that causes dry mouth is probably anticholinergic. RED-FLAG DRUGS: never use these in elderly people Meperidine (Demerol), toxic metabolite accumulates, delirium) Codeine: must be metabolized by liver to work Propoxyphene (Darvocet, Darvon)no more effective than aspirin, toxic in elderly Careful with fentanyl patches (Duragesic)prolonged T in elder, very potent. Never use in opioid nave pt. Diazepam (Valium), chlordiazepoxide (Librium)prolonged T , up to 90 hours after a single dose Theophylline: toxic, other drugs work better Muscle relaxers [except tizanidine (Zanaflex)]strongly anticholinergic, and not very effective. Ex: Robaxin, Flexeril, Soma 1st generation antihistamines: diphenhydramine (Benadryl), chlorpheniramine, etc, unless for treatment of dystonia. Amitryptaline (very anticholinergic); use desipramine, nortryptaline
Rules of Thumb 1. Think, small frequent feedings. Use small doses of a short acting drug, more frequently, until pt is stabilized on it. Then can switch to a longer acting. For starters, I typically use of the smallest tablet size available and titrate, titrate, titrate! 2. Anticipate drug accumulation at about 3-5 days after any new or changed drug. Opioids and BZP may need to be down titrated. The drug that accumulates is not necessarily the one that is new or increased. 4. If an elderly person on multiple meds becomes nauseated or confused, it is probably a drug side effect. 5. As pts become dehydrated, reduce med doses! 6. To avoid polypharmacy, use time-limited medication trials. If the med does not help within 2 weeks, stop it. Do not leave it on as prnyou never know who will administer it anyway. Cases 1. A 90 y/o, 90-pound woman with end-stage CHF is on digoxin 0.125 mg qd, Lasix 40 mg tid, captopril 25 mg tid, and stool softener. She is anorexic and her oral intake is poor. She is noted to be more edematous and SOA, so her Lasix is increased to 80 mg tid. Five days later, she calls, c/o nausea. What is the most likely cause? 2, A 75 y/o 110 pound man with end -stage lung cancer and severe COPD is started on MS Contin 15 mg bid for generalized discomfort with good results. One month later he c/o radiating, sharp pain in a radicular distribution, thought to be due to tumor invasion of thoracic nerves. He is started on amitryptaline 100 mg hs. Two days later, he becomes more lethargic and restless. His wife calls, stating that he hasnt urinated in two days and is severely constipated. What should you do? 3. A 72 y/o 90-pound woman is admitted to hospice for end-stage breast CA with bony metastases. She has known renal insufficiency (creatinine 2.5). When you examine her, she confused and lethargic, c/o severe pain over her right rib cage. Her attending physician (not Dr Brungardt) has prescribed Darvocet N 100, 1 tab qid prn pain; Indocin (indomethacin) 50 mg tid for bone pain; (methocarbamol) Robaxin 1000 mg tid for muscle spasm; and diazepam (Valium) 5 mg tid for anxiety. What medication recommendations would you make?
Potrebbero piacerti anche
- Time Management For New NursesDocumento2 pagineTime Management For New NursesErika HarveryNessuna valutazione finora
- Get Clients Now WorksheetDocumento2 pagineGet Clients Now WorksheetErika HarveryNessuna valutazione finora
- KardexDocumento1 paginaKardexarlee marquez92% (13)
- Documentation ExamplesDocumento5 pagineDocumentation ExamplesErika HarveryNessuna valutazione finora
- Top 200 Drugs WorksheetsDocumento30 pagineTop 200 Drugs WorksheetsErika Harvery100% (1)
- Are You Scratching Your Head or Are You Maybe Even Ready To Tear Your Hair Out Over How To Come Up With Care PlansDocumento8 pagineAre You Scratching Your Head or Are You Maybe Even Ready To Tear Your Hair Out Over How To Come Up With Care PlansErika HarveryNessuna valutazione finora
- Insulin For Clinical S 2 BDocumento2 pagineInsulin For Clinical S 2 BErika HarveryNessuna valutazione finora
- Body Planes Directions CavitiesDocumento14 pagineBody Planes Directions CavitiesErika HarveryNessuna valutazione finora
- Handout Medication Errors Role PlayDocumento1 paginaHandout Medication Errors Role PlayErika HarveryNessuna valutazione finora
- Resident Care Conference Signature SheetDocumento2 pagineResident Care Conference Signature SheetErika HarveryNessuna valutazione finora
- Final Intro To Cardiac PDFDocumento46 pagineFinal Intro To Cardiac PDFErika HarveryNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Pulse Contour Cardiac Output Learning Package PDFDocumento17 paginePulse Contour Cardiac Output Learning Package PDFNurse PractitionerNessuna valutazione finora
- ROLE of OT in NICUDocumento11 pagineROLE of OT in NICUDeepanshi TyagiNessuna valutazione finora
- FREE RANGE CHICKEN AND GOAT PRODUCTION GUIDEDocumento78 pagineFREE RANGE CHICKEN AND GOAT PRODUCTION GUIDEMA DapNessuna valutazione finora
- Myringotomy & MyringoplastyDocumento35 pagineMyringotomy & MyringoplastypriyaNessuna valutazione finora
- FUNDA Part 1Documento5 pagineFUNDA Part 1Jo Hn Vengz100% (1)
- Rapid Review For The Plastic Surgery Inservice & Board ExaminationsDocumento183 pagineRapid Review For The Plastic Surgery Inservice & Board ExaminationsTahaniNessuna valutazione finora
- GRAND PRES - CorrectedDocumento22 pagineGRAND PRES - CorrectedDarlen RabanoNessuna valutazione finora
- Pre-Intermediate Unit 8 VocabularyDocumento6 paginePre-Intermediate Unit 8 VocabularyHama CheikhNessuna valutazione finora
- Dextroamphetamine: Brand Name: DexedrineDocumento23 pagineDextroamphetamine: Brand Name: DexedrineSharry Fe OasayNessuna valutazione finora
- Salbutamol + IpratropiumDocumento3 pagineSalbutamol + IpratropiumShiva TorinsNessuna valutazione finora
- 05 - Cellular Adaptations - SimpleMed - Learning Medicine, SimplifiedDocumento7 pagine05 - Cellular Adaptations - SimpleMed - Learning Medicine, SimplifiedRachel ManaloNessuna valutazione finora
- Literature ReviewDocumento3 pagineLiterature Reviewapi-509948413Nessuna valutazione finora
- Blood-Based Protein Changes in Childhood Are Associated With Increased Risk For Later Psychotic DisorderDocumento34 pagineBlood-Based Protein Changes in Childhood Are Associated With Increased Risk For Later Psychotic DisorderFelicia SaraswatiNessuna valutazione finora
- CDHDocumento47 pagineCDHSameeta PrabhuNessuna valutazione finora
- Medical Equipment and SuppliesDocumento1 paginaMedical Equipment and SuppliesMic GlobalNessuna valutazione finora
- Surgical Treatment of Congenital Syndactyly of the HandDocumento13 pagineSurgical Treatment of Congenital Syndactyly of the HandJose Alejandro Cobas PazNessuna valutazione finora
- HUNNER LESION DIAGNOSISDocumento4 pagineHUNNER LESION DIAGNOSISVasishta NadellaNessuna valutazione finora
- Internship Manual 20-21 PDFDocumento19 pagineInternship Manual 20-21 PDFMsalik1Nessuna valutazione finora
- (2016) Small Animal Abdominal Ultrasonography Liver & GallBladder - Part 1Documento7 pagine(2016) Small Animal Abdominal Ultrasonography Liver & GallBladder - Part 1ludiegues752100% (1)
- Blood Donor Hematocrit Level InformationDocumento1 paginaBlood Donor Hematocrit Level Informationdoppler_Nessuna valutazione finora
- St. Paul University Quezon City College of Health Sciences case study on CholedocholithiasisDocumento5 pagineSt. Paul University Quezon City College of Health Sciences case study on CholedocholithiasisJanelle Kate SaleNessuna valutazione finora
- Norton Healthcare News: February 2010Documento12 pagineNorton Healthcare News: February 2010Norton HealthcareNessuna valutazione finora
- Effect of Cervical Cancer Prevention Education in Middle-School Girl in KoreaDocumento6 pagineEffect of Cervical Cancer Prevention Education in Middle-School Girl in KoreaTrysna Ayu SukardiNessuna valutazione finora
- Drug CarbocisteineDocumento1 paginaDrug CarbocisteineDhan LopezNessuna valutazione finora
- Health: Quarter 3 - Module 2: Coping With Stress, Dying and DeathDocumento10 pagineHealth: Quarter 3 - Module 2: Coping With Stress, Dying and DeathDyanne De JesusNessuna valutazione finora
- Case Study TrichoDocumento6 pagineCase Study TrichoVisanth KumarNessuna valutazione finora
- Burns E 2013 PHD Thesis PDFDocumento338 pagineBurns E 2013 PHD Thesis PDFDr-Rabia AlmamalookNessuna valutazione finora
- Ati Test Bank For 2016 Ati RN Proctored Mental Health Form BDocumento3 pagineAti Test Bank For 2016 Ati RN Proctored Mental Health Form Btheresagreensayxgiwkod100% (47)
- Unit 1 PDFDocumento11 pagineUnit 1 PDFSatendra KumarNessuna valutazione finora
- Assessment of The Healing of Conservatively Treated Scaphoid Fractu - 2021 - BonDocumento10 pagineAssessment of The Healing of Conservatively Treated Scaphoid Fractu - 2021 - BondianaNessuna valutazione finora