Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Talk05 SouweidaneBigHeads
Caricato da
Sedaka DonaldsonTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Talk05 SouweidaneBigHeads
Caricato da
Sedaka DonaldsonCopyright:
Formati disponibili
Mark M. Souweidane, M.D., F.A.A.P., F.A.C.S.
Professor and Vice Chairman Department of Neurological Surgery December 8th, 2010
Open fontanels and sutures allow cranial expansion High water content allow compensatory ventricular enlargement
Constitutional macrocephaly
5% of normal children have an occipitofrontal circumference (OFC) greater than the 95 percentile Nondivergent growth curve
Increased subarachnoid spaces of infancy
External hydrocephalus Divergent growth curve
6 month old female Normal birth and development history Growth curve as shown Open and full anterior fontanel No suture diastasis
Chronic subdural hematomas of infancy
Divergent growth curve Usually nonaccidental trauma
Hydrocephalus and other CSF circulation abnormalities
Divergent growth curve
Neurodegenerative disorders (Canavans and Alexander disease)
Divergent growth curve
6 month old female Normal birth and development history Growth curve as shown Open and full anterior fontanel Suture diastasis Irritability, vomiting, seizures, etc.
6 month old female Normal birth and development history Growth curve as shown Open and full anterior fontanel Suture diastasis Irritability, vomiting, seizures, etc. Clinical manifestations of raised ICP
Frontal bossing Forced down gaze Engorgement of scalp veins
Alternative to shunt placement Avoids all complications associated with shunts Restoration of normal CSF outflow and resorption Applicable in all forms of intraventricular obstructive hydrocephalus distal to the posterior third ventricle
Drake JM, Kestle JR, Milner R, et al: Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43:294-305, 1998.
Scalp and Skull Masses
Posttraumatic
Cephalohematoma Leptomeningeal cyst
Congenital
Inclusion cysts Aplasia cutis congenita
Neoplastic
neurofibroma
Vascular
Capillary hemangioma Sinus pericranii AV malformation
Inflammatory
Lymphadenopathy LCH Cranial fasciitis Infantile myofibormatosis
Dysraphic
Cephaloceles
Atretic Encephalocele meningocele
History
Physical Examination
Rate of growth History of trauma including birth history Fevers or associated illnesses Anatomical position (midline or eccentric, supratentorial or infratentorial) Pain on palpation Skin integrity Pulsatile Intracranial pressure transmission Associated lymphadenopathy
Imaging decision
Generalizations
Malignancy is rare Intracrnaial extension is rare Diagnosis is seldom in question Hetereogeneous pathology
1. Inclusion cysts (dermoid cysts, epidermoid cysts) 2. Langerhans cell histiocytosis (eosinophilic granuloma) 3. Cephaloceles 4. Subperiosteal hematoma 5. Lepotomeningeal cyst
Congenital disorder Epidermoid cyst
Failed dysjunction Intracranial Older children/adults Rare association with dermal sinus Extracranial Infants Can be associated with dermal sinus (meningitedes)
Dermoid cyst
Most common scalp mass evaluated by neurosurgeon (60%) Usually present at birth Epidermal and dermal elements Slow growth
Keratin Cholesteral Sebaceum
Anatomical location
Anterior fontanel
Rare dural penetration
Pterion Suboccipital midline
Dermal sinus Occipital sinus duplication Dural penetration typical
Plain radiographs
Lytic Smooth contours Sclerotic margins
Elective surgical excision Split thickness autologous cranioplasty > infancy
Endoscopic Removal of Dermoid Cyst
Histiocytosis X
Uncertain etiology
Eosinophilic granuloma Hand-Schuller-Christian Disease (diabetes insipidus, hypothalamic lesions) Letterer-Siwe syndrome
Skull is most common site Painful scalp mass Age 4-12 years
28% polyostotic disease Rarely intracranial
Abnormal proliferation of histiocytes
Painful scalp mass Relatively short history Age 4-12 years Radiology
Plain films (punched out, no sclerotic margins, scalloped edges) CT
External table remodeling Diploic interspace
Treatment
Surgical
Curettage Complete excision
Adjunctive Rx
Radiation therapy chemotherapy
Outcome
Negative prognostic features
< 2 years age Polyostotic disease Hepatosplenomegaly Thrombocytopenia
Poorly defined Local recurrence 6% New recurrence 22%*
*Kilpatrick et al. Cancer 1995
Subperiosteal hematoma resulting from birthing (prolonged labor, forceps delivery, etc.) Physical examination Treatment/Outcome
Absent intracranial extension Respects suture anatomy
Spontaneous resolution, no need for treatment or aspiration Minority of subperiosteal hematomas calcify cephalohematoma deformans that may require recontouring
Growing skull fracture Rare sequelae of linear skull fractures in infants Herniation of leptomeninges and varying cerebral tissue Clinical Features
Repair directed at cranial defect
Delayed swelling following trauma Progressive seizure disorder or neurological deficits Plain X-ray is diagnostic (widely separated linear fracture)
October 2007
Leptomeningeal Cyst
March 2008
Congenital disorders (encephaloceles, meningoceles) of nondysjunction
Skin Calvarium Meninges Cerebrum
Always midline (cranial base to craniocervical junction), transillumination Classification is varied Treatment is aimed at repair of defect Outcome dependent upon associated intracranial anomalies
aborted cephaloceles Congenital disorder, failed dysjunction Typically parietaloccipital Skin is atypical (discolored, attenuated, hypertrichosis) Associated structural cerebral anomalies Treatment aimed at normal skin covering Outcome dependent upon associated cerebral anomalies
Spontaneous osteogenesis Autologous cranioplasty Synthetic cranioplasty
Acrylic Titanium
Age dependent
Split thickness
6 month old female Normal birth and development history Growth curve as shown Open anterior fontanel
Appropriate management includes:
a. Transfontanel sonogram b. MRI of brain c. Neurosurgical referral d. Neurology referral e. None of the above
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Brachial PlexusDocumento62 pagineBrachial PlexusTutankhamoun Akhenatoun100% (2)
- Understanding Stroke-Brain Anatomy and Cerebral CirculationDocumento47 pagineUnderstanding Stroke-Brain Anatomy and Cerebral CirculationNaveen Eldose100% (4)
- Infantile, Childhood, and Adolescent Epilepsies.9Documento34 pagineInfantile, Childhood, and Adolescent Epilepsies.9Silviana IlieNessuna valutazione finora
- Checklist For All Loan TypesDocumento2 pagineChecklist For All Loan TypesSedaka DonaldsonNessuna valutazione finora
- Neurophysiology of PainDocumento32 pagineNeurophysiology of PainShivan A.C.Nessuna valutazione finora
- Bed Sore 48Documento45 pagineBed Sore 48Sedaka DonaldsonNessuna valutazione finora
- Wound Closure ManualDocumento127 pagineWound Closure ManualDougyStoffell100% (5)
- Ihbas ReportDocumento11 pagineIhbas ReportSeema YadavNessuna valutazione finora
- MCCQE 1 Scope of Questions - CDMDocumento11 pagineMCCQE 1 Scope of Questions - CDMmiadelfior100% (2)
- Stroke 1Documento35 pagineStroke 1Aisyah IcahNessuna valutazione finora
- Creutzfeldt-Jakob Disease 1Documento16 pagineCreutzfeldt-Jakob Disease 1anu1643Nessuna valutazione finora
- Barry E. Kosofsky, MD, PHD Adapted From Wayne Blount, MDDocumento34 pagineBarry E. Kosofsky, MD, PHD Adapted From Wayne Blount, MDSedaka DonaldsonNessuna valutazione finora
- International Observership HandbookDocumento51 pagineInternational Observership HandbookSedaka DonaldsonNessuna valutazione finora
- Fluids - Electrolytes ICU PDFDocumento91 pagineFluids - Electrolytes ICU PDFAhmed Shihab AhmedNessuna valutazione finora
- Gen Medicine - Finalized Scheme of ExaminationDocumento30 pagineGen Medicine - Finalized Scheme of Examinationsp_rao2000Nessuna valutazione finora
- Laryngeal Dystonia (Spasmodic Dysphonia) : SymptomsDocumento3 pagineLaryngeal Dystonia (Spasmodic Dysphonia) : SymptomschalixchassreenNessuna valutazione finora
- Imagenes Psicologia FisiologicaDocumento18 pagineImagenes Psicologia FisiologicaMayra VillegasNessuna valutazione finora
- Mithyantha2017 PDFDocumento7 pagineMithyantha2017 PDFRifki Sanjaya PratamaNessuna valutazione finora
- Different Types of Diseases/disorders of The Nervous System.Documento23 pagineDifferent Types of Diseases/disorders of The Nervous System.Saba Parvin Haque100% (4)
- 1 s2.0 S1474442222004318 MainDocumento15 pagine1 s2.0 S1474442222004318 MainItamar MeirelesNessuna valutazione finora
- Multiple Choice Questions For Part IVDocumento18 pagineMultiple Choice Questions For Part IVTarek MohsenNessuna valutazione finora
- Differential Diagnosis of Neurological Diseases ofDocumento25 pagineDifferential Diagnosis of Neurological Diseases ofRajesh kumarNessuna valutazione finora
- Epilepsy Syndromes in Children - UpToDateDocumento26 pagineEpilepsy Syndromes in Children - UpToDatecapt_zoeNessuna valutazione finora
- Journal of Neurology and NeurocienceDocumento49 pagineJournal of Neurology and NeurocienceInternational Medical PublisherNessuna valutazione finora
- TalkDocumento18 pagineTalkapi-338453738Nessuna valutazione finora
- Neuroradiology: Sony Sutrisno Department of Radiology Krida Wacana Christian UniversityDocumento46 pagineNeuroradiology: Sony Sutrisno Department of Radiology Krida Wacana Christian UniversityPaulus AnungNessuna valutazione finora
- Clinical Examination and Management of Impairments in VariousDocumento34 pagineClinical Examination and Management of Impairments in Variousmukesh pokharelNessuna valutazione finora
- Case Study For AphasiaDocumento4 pagineCase Study For AphasiaYell Yint MyatNessuna valutazione finora
- Chronic Inflammatory Demyelinating PolyradiculoneuropathyDocumento5 pagineChronic Inflammatory Demyelinating PolyradiculoneuropathyDiego Fernando AlegriaNessuna valutazione finora
- Simulation Questions Cooper MadisonDocumento2 pagineSimulation Questions Cooper MadisonJohn MixerNessuna valutazione finora
- Management of Traumatic Brain Injury (TBI) - A Clinical Neuroscience-Led Pathway For The NHSDocumento8 pagineManagement of Traumatic Brain Injury (TBI) - A Clinical Neuroscience-Led Pathway For The NHS彭金辉 KIVINessuna valutazione finora
- Management of Unconscious PatientDocumento51 pagineManagement of Unconscious PatientHylman Mahendra100% (1)
- Brain AbscessDocumento25 pagineBrain AbscessprembarnabasNessuna valutazione finora
- What Is A Brain Aneurysm?Documento2 pagineWhat Is A Brain Aneurysm?shinNessuna valutazione finora
- Bigler 2013 PDFDocumento41 pagineBigler 2013 PDFCarolina SalazarNessuna valutazione finora
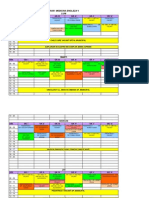
- Orar Medicina Engleza V Luni: ORA Gr. I Gr. Ii Gr. Iii Gr. Iv Gr. V Gr. ViDocumento3 pagineOrar Medicina Engleza V Luni: ORA Gr. I Gr. Ii Gr. Iii Gr. Iv Gr. V Gr. ViCornel MihaiNessuna valutazione finora