Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pi Is 1877886013000451
Caricato da
cottard2013Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pi Is 1877886013000451
Caricato da
cottard2013Copyright:
Formati disponibili
Scandinavian Journal of Pain 4 (2013) 146147
Contents lists available at SciVerse ScienceDirect
Scandinavian Journal of Pain
journal homepage: www.ScandinavianJournalPain.com
Editorial comment
Buprenorphine The ideal drug for most clinical indications for an opioid?
Harald Breivik a,b,
a b
University of Oslo, Department of Pain Management and Research, Rikshospitalet, Oslo University Hospital, Oslo, Norway University of Oslo, Department of Anaesthesiology, Rikshospitalet, Oslo University Hospital, Oslo, Norway
In this issue of the Scandinavian Journal of Pain, Stephen Butler, former chief of the famous Bonica Pain Clinic at the University of Washington in Seattle, reviews new knowledge of buprenorphine [1]. During the four decades after buprenorphine became available for clinical use persistent misunderstandings have existed in textbooks and in reviews in medical literature. These misunderstandings have misled clinicians and patients so that optimal uses of this drug were reduced. This problem continues to this day [1]. The rst serious misunderstanding was that buprenorphine is not an addicting drug. It was marketed as a drug for moderate to severe pain with low risk of misuse or abuse. Clinicians and addicted persons soon discovered that this is not true. I was surprised and very disappointed to discover soon after the sublingual buprenorphine was available in Norway, already in 198384, that one of my patients sold his sublingual buprenorphine tablets on the illegal market. Addicted persons dissolved the sublingual tablets and injected the drug. So buprenorphine was soon moved on to the narcotic drug list. There are other misunderstandings about buprenorphine, mostly based on animal data. These misunderstandings came into textbooks on pharmacology and pain as medical truths about 30 years ago. They have been difcult to get out of textbooks and guidelines. They continue to live on in teachings to medical students and postgraduate training. It is by now a well-known fact that animal models of pain and analgesia are unreliable as predictors of clinical effects in patients with pain. In clinical practice there is no bell-shaped doseresponse curve and there is no plateau on the doserelief response curve of buprenorphine. There is also no antagonist effect from buprenorphine on other mu-opioid agonists such as morphine or oxycodone. On the contrary, there may be supra-additive or synergistic effects between buprenorphine and morphine, and between buprenorphine and oxycodone for references, see [2]. Buprenorphine is an agonist on the mu-, the delta, and the ORL1 receptors. Buprenorphine is an antagonist at the kappa-receptor. Active metabolites have different effects on the four opioid receptors; all except the norbup-3-glu are analgesic. Buprenorphine itself
is not a respiratory depressant or sedative, but some of its active metabolites are. Buprenorphine and its active metabolites are not excreted by the kidney, so that buprenorphine may be used in patients with advanced renal failure. Buprenorphine has a slow onset-time and a prolonged offsettime. These properties are mostly advantageous. However, when treating strong acute pain, the long onset-time may be a slight disadvantage. It makes buprenorphine less than an ideal opioid for IV patient-controlled-analgesia (PCA). For the same reason it is also not a good alternative for treating so called break-throughpain. The agonist effect of buprenorphine on the ORL-1 receptor reduces reward-effects and slows the development of tolerance to the analgesic effects. Buprenorphine is an excellent alternative for treating chronic pain, especially chronic neuropathic pain and cancer pain when pain is constantly present. Chronic pain in the elderly patients, who often have components of neuropathic pain and often have reduced renal function, is a well documented indication for buprenorphine. The 7-day transdermal buprenorphine patch is well tolerated and easily administered to such patients [3]. Treatment of the opioid-abuse disease with buprenorphine is now a well established indication for buprenorphine. Its slow onset (less kick-effect), and its prolonged offset-time reduces the likelihood of acute withdrawal problems and reduces the craving of opioids for references see Stephen Butlers well documented review [1]. Caveat: Buprenorphine, a potent mu-agonist, may induce or maintain opioid addiction. Illegally obtained high-dose transmucosal buprenorphine, intended for treatment of addiction, is dissolved and injected by opioid abusers, even in the Nordic countries. This is a clear reminder to us all that any mu-opioid receptor agonist is always potentially an abuse-drug. Buprenorphine must always be prescribed to pain-patients with the same strict precautions as any other potent opioid. And the patients, their drug use, and pain condition must be conscientiously monitored [4]. Buprenorphine is now a thoroughly studied drug. It is about time we get rid of the many misunderstandings and false myths around this useful opioid drug. References
[1] Butler S. Buprenorphine clinically useful but often misunderstood. Scand J Pain 2013;4:14852.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2013.05.004. Correspondence address: University of Oslo, Department of Pain Management and Research, Rikshospitalet, Oslo University Hospital, Oslo, Norway. E-mail address: harald.breivik@medisin.uio.no
1877-8860/$ see front matter 2013 Scandinavian Association for the Study of Pain. Published by Elsevier B.V. All rights reserved. http://dx.doi.org/10.1016/j.sjpain.2013.05.005
H. Breivik / Scandinavian Journal of Pain 4 (2013) 146147 [2] Kress HG. Clinical update on the pharmacology, efcacy and safety of transdermal buprenorphine. Eur J Pain 2009;13:21930. [3] Breivik H, Ljosaa TM, Stengaard-Pedersen K, Persson J, Aro H, Villumsen J, Tvinnemose D. A 6-months, randomised, placebo-controlled evaluation of efcacy and tolerability of a low-dose 7-day buprenorphine transdermal
147
patch in osteoarthritis patients nave to potent opioids. Scand J Pain 2010;1: 12241. [4] Breivik H, Gordh T, Butler S. Keeping an open mind: Achieving balance between too liberal and too restrictive prescription of opioids for chronic non-cancer pain: Using a two-edged sword. Scand J Pain 2012;3:14.
Potrebbero piacerti anche
- Handbook of Methadone Prescribing and Buprenorphine TherapyDa EverandHandbook of Methadone Prescribing and Buprenorphine TherapyNessuna valutazione finora
- PerioperativeDocumento15 paginePerioperativeJEFFERSON MUÑOZNessuna valutazione finora
- NIH Public Access: Buprenorphine-Nalxone Therapy in Pain ManagementDocumento25 pagineNIH Public Access: Buprenorphine-Nalxone Therapy in Pain ManagementyoiiiNessuna valutazione finora
- Tugas Terjemahan-Manajemen NyeriDocumento50 pagineTugas Terjemahan-Manajemen NyeriNur MuawanaNessuna valutazione finora
- Management of Chronic Pain in The Elderly: Focus On Transdermal BuprenorphineDocumento10 pagineManagement of Chronic Pain in The Elderly: Focus On Transdermal BuprenorphineancoursNessuna valutazione finora
- Invitro Dissolution and Assay of "Ibuprofen"Tablet.Documento59 pagineInvitro Dissolution and Assay of "Ibuprofen"Tablet.Md.Moniruzzaman100% (3)
- Effects of Ascending Buprenorphine Doses On Measur - 2019 - Journal of SubstanceDocumento7 pagineEffects of Ascending Buprenorphine Doses On Measur - 2019 - Journal of SubstanceARACELY RAFAELA CORNEJO MARTINEZNessuna valutazione finora
- Buprenorfin Review - 12 ReasonsDocumento11 pagineBuprenorfin Review - 12 ReasonsPaula RoccaNessuna valutazione finora
- jhmbf01472 Sup 0001Documento10 paginejhmbf01472 Sup 0001simbamed235Nessuna valutazione finora
- Buprenorphine - A Unique Drug With Complex PharmacologyDocumento17 pagineBuprenorphine - A Unique Drug With Complex Pharmacologygigidurul1111Nessuna valutazione finora
- Opioids and Chronic Neuropathic Pain: Kathleen M. Foley, M.DDocumento3 pagineOpioids and Chronic Neuropathic Pain: Kathleen M. Foley, M.DFionita BeelkisNessuna valutazione finora
- AnalgesicsDocumento23 pagineAnalgesicsMuhammad SdiqNessuna valutazione finora
- Acute Pain Management in Patients With Opioid ToleranceDocumento6 pagineAcute Pain Management in Patients With Opioid ToleranceHendrikus Surya Adhi PutraNessuna valutazione finora
- Step LaddrDocumento12 pagineStep LaddrSetyo RahmanNessuna valutazione finora
- Roux 2013Documento7 pagineRoux 2013andrew herringNessuna valutazione finora
- Case Study 1Documento3 pagineCase Study 1Amberly BohackNessuna valutazione finora
- Longer Analgesic Effect With Naproxen Sodium Than Ibuprofen in Post Surgical Dental Pain A Randomized Double Blind Placebo Controlled Single DoseDocumento11 pagineLonger Analgesic Effect With Naproxen Sodium Than Ibuprofen in Post Surgical Dental Pain A Randomized Double Blind Placebo Controlled Single DoseAngélica María AponteNessuna valutazione finora
- Ibuprofen - A Journey From Prescription To Over-The-counterDocumento5 pagineIbuprofen - A Journey From Prescription To Over-The-counterPharmazellNessuna valutazione finora
- Guía de OpioidesDocumento13 pagineGuía de OpioidesJAIME MUÑOZNessuna valutazione finora
- Buvidal PDF 1158123740101Documento7 pagineBuvidal PDF 1158123740101riffs_ahoyNessuna valutazione finora
- Articulo BuprenorfinaDocumento19 pagineArticulo BuprenorfinaAlejandra PerezNessuna valutazione finora
- Opiod RotationDocumento9 pagineOpiod RotationboboNessuna valutazione finora
- Virtual Mentor: Ethics Case Common Misconceptions About Opioid Use For Pain Management at The End of LifeDocumento7 pagineVirtual Mentor: Ethics Case Common Misconceptions About Opioid Use For Pain Management at The End of LifeOana Victoria CucuNessuna valutazione finora
- Prot Sap 000Documento20 pagineProt Sap 000QenquNessuna valutazione finora
- Labour Analgesi2Documento17 pagineLabour Analgesi2manish086Nessuna valutazione finora
- Ibuprofen BookDocumento259 pagineIbuprofen BookbabithyNessuna valutazione finora
- Acep Equal Opiod Wave IiDocumento43 pagineAcep Equal Opiod Wave IiJesse M. MassieNessuna valutazione finora
- A Comprehensive Review of Opioid-Induced HyperalgesiaDocumento18 pagineA Comprehensive Review of Opioid-Induced HyperalgesiaJose Miguel Arce RomoNessuna valutazione finora
- Pharmacology of Opiates 1Documento18 paginePharmacology of Opiates 1bobo100% (1)
- Pharmacologic Management of Adult Breakthrough Cancer Pain: Palliative Care FilesDocumento4 paginePharmacologic Management of Adult Breakthrough Cancer Pain: Palliative Care Filesousama aklan100% (1)
- Randomized, Placebo-Controlled Trial Pregabalin For The Treatment of Postherpetic Neuralgia: ADocumento12 pagineRandomized, Placebo-Controlled Trial Pregabalin For The Treatment of Postherpetic Neuralgia: AadityaNessuna valutazione finora
- Keywords: Ambulatory Epidurals, Labour Analgesia, Recent AdvancesDocumento12 pagineKeywords: Ambulatory Epidurals, Labour Analgesia, Recent Advancesmanish086Nessuna valutazione finora
- Effect of Different Doses of Butorphanol On Postoperative Shivering in Elderly Patients A Randomized Double-Blind Placebo-Controlled TrialDocumento12 pagineEffect of Different Doses of Butorphanol On Postoperative Shivering in Elderly Patients A Randomized Double-Blind Placebo-Controlled TrialRahmat CesNessuna valutazione finora
- Adjuvant Neuroaxial BlokDocumento12 pagineAdjuvant Neuroaxial BlokDadanaja AjaNessuna valutazione finora
- Essential Notes in Pain Medicine Oxford Speciality Training Rev Notes Sep 14 2022 - 0198799446 - Oxford University Press Enrique Collantes Celador Full ChapterDocumento68 pagineEssential Notes in Pain Medicine Oxford Speciality Training Rev Notes Sep 14 2022 - 0198799446 - Oxford University Press Enrique Collantes Celador Full Chaptermargaret.jones429100% (4)
- Case Study PropofolDocumento7 pagineCase Study PropofolaliasLiew100% (1)
- Acute Post-Op Pain ManagementDocumento4 pagineAcute Post-Op Pain Management1234chocoNessuna valutazione finora
- Briefly: PointsDocumento3 pagineBriefly: Pointscarlina_the_bestNessuna valutazione finora
- Opioids in The Management of Persistent Non-Cancer PainDocumento3 pagineOpioids in The Management of Persistent Non-Cancer Painafernandezd28Nessuna valutazione finora
- Treatment Without OpioidesDocumento20 pagineTreatment Without OpioidesDanii LaverdeNessuna valutazione finora
- Pain Acute Pain OpioidTolerantDocumento20 paginePain Acute Pain OpioidTolerantRoy LizalNessuna valutazione finora
- The Ashton Manual - Benzo DependencyDocumento58 pagineThe Ashton Manual - Benzo DependencySermoniaNessuna valutazione finora
- Revista Colombiana de AnestesiologíaDocumento5 pagineRevista Colombiana de AnestesiologíaNikolas GilNessuna valutazione finora
- Art Dolor GeriátricoDocumento9 pagineArt Dolor GeriátricoarrlyNessuna valutazione finora
- Subutex Quick-Start-GuideDocumento6 pagineSubutex Quick-Start-GuideDanNessuna valutazione finora
- WHO Ladder 20anosdepois PDFDocumento4 pagineWHO Ladder 20anosdepois PDFIahel ManonNessuna valutazione finora
- Schuster 2018Documento23 pagineSchuster 2018Poly ArenaNessuna valutazione finora
- KJP 23 99Documento10 pagineKJP 23 99Edvan BenevidesNessuna valutazione finora
- Acta Anaesthesiologica Taiwanica: Editorial ViewDocumento2 pagineActa Anaesthesiologica Taiwanica: Editorial ViewShuaib AhmedNessuna valutazione finora
- IASP 2016 Poster Abstracts - Wednesday PDFDocumento731 pagineIASP 2016 Poster Abstracts - Wednesday PDFHendriik ViicarloNessuna valutazione finora
- New Topics in phaRMcology (97-2003)Documento18 pagineNew Topics in phaRMcology (97-2003)api-3761895Nessuna valutazione finora
- Practice Guidelines For The Prevention, Detection, and Management of Respiratory Depression Associated With Neuraxial Opioid Administration AnDocumento12 paginePractice Guidelines For The Prevention, Detection, and Management of Respiratory Depression Associated With Neuraxial Opioid Administration AnMadalina TalpauNessuna valutazione finora
- An Update On AnalgesicsDocumento6 pagineAn Update On AnalgesicsShailaja DesaiNessuna valutazione finora
- 460 Oxycodone in Pain ManagementDocumento93 pagine460 Oxycodone in Pain ManagementSinta Chaira Maulanisa100% (1)
- Comparative Study of Epidural Fentanyl and Buprenorphine For Post Operative Analgesia in Lower Abdominal and Lower Limb SurgeriesDocumento8 pagineComparative Study of Epidural Fentanyl and Buprenorphine For Post Operative Analgesia in Lower Abdominal and Lower Limb SurgeriesIOSRjournalNessuna valutazione finora
- Nonsteroidal Anti-Inflammatory Drugs Like Ibuprofen Act in Reversible Inhibition of The EnzymesDocumento5 pagineNonsteroidal Anti-Inflammatory Drugs Like Ibuprofen Act in Reversible Inhibition of The EnzymesIekzkad RealvillaNessuna valutazione finora
- Bupe and Acute PainDocumento14 pagineBupe and Acute PainHollowbinNessuna valutazione finora
- Annexure - II Product DevelopmentDocumento50 pagineAnnexure - II Product DevelopmentLife PearlNessuna valutazione finora
- ArticuloDocumento12 pagineArticuloNallely De LSNessuna valutazione finora
- The Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613Documento9 pagineThe Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613เพียงแค่ แอนโทนี่Nessuna valutazione finora
- The European Redemption Pact: An Illustrative GuideDocumento23 pagineThe European Redemption Pact: An Illustrative Guidecottard2013Nessuna valutazione finora
- Appendix II Web ResourcesDocumento8 pagineAppendix II Web Resourcescottard2013Nessuna valutazione finora
- Religious Studies 0500: Theory and Practice of Buddhist MeditationDocumento7 pagineReligious Studies 0500: Theory and Practice of Buddhist Meditationcottard2013Nessuna valutazione finora
- Scandinavian Journal of Forest ResearchDocumento17 pagineScandinavian Journal of Forest Researchcottard2013Nessuna valutazione finora
- Scandinavian Journal of Forest ResearchDocumento15 pagineScandinavian Journal of Forest Researchcottard2013Nessuna valutazione finora
- Inventory of Sanskrit ScholarsDocumento365 pagineInventory of Sanskrit ScholarsAlok SharmaNessuna valutazione finora
- Pi Is 1877886013000426Documento2 paginePi Is 1877886013000426cottard2013Nessuna valutazione finora
- Additional Fiscal Measures PDFDocumento2 pagineAdditional Fiscal Measures PDFcottard2013Nessuna valutazione finora
- Sedative and HypnoticsDocumento37 pagineSedative and Hypnoticsprajyot khedekarNessuna valutazione finora
- Ibuprofen and Acetaminophen (Tylenol)Documento2 pagineIbuprofen and Acetaminophen (Tylenol)vikrizkaNessuna valutazione finora
- The Effectiveness of Drug Rehabilitation Program in MindanaoDocumento13 pagineThe Effectiveness of Drug Rehabilitation Program in MindanaoJane PearlNessuna valutazione finora
- Top 100 DrugsDocumento5 pagineTop 100 DrugsGiacenNessuna valutazione finora
- Bahan Dri KhemedDocumento7 pagineBahan Dri KhemedgustiNessuna valutazione finora
- Price ListDocumento15 paginePrice ListmahinggarNessuna valutazione finora
- Advil - PLUS - FA - For - Download - ENGLISHDocumento2 pagineAdvil - PLUS - FA - For - Download - ENGLISHShuvroNessuna valutazione finora
- Lorazepam (Ativan)Documento1 paginaLorazepam (Ativan)ENessuna valutazione finora
- Tutorial Anxiolytic and Hypnotic DrugsDocumento3 pagineTutorial Anxiolytic and Hypnotic DrugsRachnaNessuna valutazione finora
- Vicodin Drug Study Que Fransis A.Documento3 pagineVicodin Drug Study Que Fransis A.Irene Grace BalcuevaNessuna valutazione finora
- Presentation ArunaDocumento7 paginePresentation ArunaAruna uikeyNessuna valutazione finora
- Annotated BibliographyDocumento6 pagineAnnotated Bibliographyapi-451590039Nessuna valutazione finora
- Incompatibilitati in SeringaDocumento1 paginaIncompatibilitati in SeringaNadia BadacăNessuna valutazione finora
- The Truth About: Prescription Drug AbuseDocumento32 pagineThe Truth About: Prescription Drug AbuseklockNessuna valutazione finora
- BP402T - Med - Chem-I, 1st Sessional Que - PaperDocumento2 pagineBP402T - Med - Chem-I, 1st Sessional Que - PaperSajid khanNessuna valutazione finora
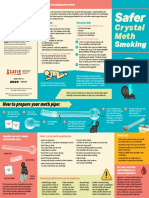
- CATIE SaferSmoking CrystalMeth E 2020 FINAL WEBDocumento2 pagineCATIE SaferSmoking CrystalMeth E 2020 FINAL WEBJeff PuglisiNessuna valutazione finora
- REF Drug Distribution by RX 20230301Documento3 pagineREF Drug Distribution by RX 20230301AnnNessuna valutazione finora
- What Are Amphetamines?Documento4 pagineWhat Are Amphetamines?Asmaa LabibNessuna valutazione finora
- Women and Pain Fact SheetDocumento2 pagineWomen and Pain Fact SheetMustafa FahamNessuna valutazione finora
- Opiate Abuse PaperDocumento7 pagineOpiate Abuse Paperapi-272576949Nessuna valutazione finora
- Crisis Intervention ProformaDocumento6 pagineCrisis Intervention Proformamathan kNessuna valutazione finora
- General Orientation of R.A. 9165Documento64 pagineGeneral Orientation of R.A. 9165Cristian Jay VirayNessuna valutazione finora
- Tugas Etika Dan Hukum Farmasi: Nama Obat Psikotropika Dan NarkotikaDocumento7 pagineTugas Etika Dan Hukum Farmasi: Nama Obat Psikotropika Dan NarkotikahabbooshaNessuna valutazione finora
- Drug Study Name of Drug Classification Adverse Effect Indication Contraindication Nursing ConsiderationDocumento3 pagineDrug Study Name of Drug Classification Adverse Effect Indication Contraindication Nursing ConsiderationCarmie CorpusNessuna valutazione finora
- Final Annotated BibliographyDocumento11 pagineFinal Annotated Bibliographyapi-358143741Nessuna valutazione finora
- Detailed Lesson Plan in Health 5: (Third Quarter)Documento40 pagineDetailed Lesson Plan in Health 5: (Third Quarter)Kring Sandagon100% (3)
- Drug AddictionDocumento8 pagineDrug AddictionNgan TracKimNessuna valutazione finora
- Top 200 DrugsDocumento9 pagineTop 200 DrugsSachin KumarNessuna valutazione finora
- ROTC Drug EducationDocumento13 pagineROTC Drug EducationCalvin Keith YadaoNessuna valutazione finora
- Cholinergic Drugs Quiz 16 - 20Documento8 pagineCholinergic Drugs Quiz 16 - 20Killer VNessuna valutazione finora
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (31)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 4.5 su 5 stelle4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDa EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisValutazione: 5 su 5 stelle5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDa EverandTroubled: A Memoir of Foster Care, Family, and Social ClassValutazione: 4.5 su 5 stelle4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDa EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingValutazione: 4 su 5 stelle4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)