Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Addisons Disease
Caricato da
Andreia PaladeCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Addisons Disease
Caricato da
Andreia PaladeCopyright:
Formati disponibili
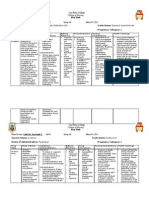
Nursing Care Plan A Client with Addisons Disease
A 51-year-old unemployed salesman, Mr. Don Sardoff, is brought to the emergency room by his wife, Ellen, at 8 A.M. Mrs. Sardoff tells the emergency room nurse that her husband has not been feeling well for the last week, but that when he got up this morning, he was so weak he couldnt dress himself and didnt know where he was. Mrs. Sardoff also tells the nurse that her husband has been taking a cortisone drug for treatment of his rheumatoid arthritis for the past 2 years, but notes,We didnt have the money to buy it this month. Regain normal peripheral perfusion with blood pressure within normal range. Verbalize knowledge of the causes and effects of adrenal insufficiency.
PLANNING AND IMPLEMENTATION
Monitor intake and output closely. Take and record weight at the same time daily. Monitor blood pressure, pulses, and skin turgor every 2 hours until stable, then 4 times a day. Monitor electrolytes, and report abnormal results. Discuss a diet that is high in sodium, low in potassium, and has an increased fluid intake (3000 mL per day).Discuss the types of fluids desired and the best times for intake of increased fluids. Assist during activity to prevent falls. Provide verbal and written instructions, and encourage verbal feedback about the causes and effects of the disease, the effects of medications, the effects of not taking long-term cortisone drugs, the diet, and self-care at home.
ASSESSMENT
On admission to the emergency room, Mr. Sardoff is dehydrated, with dry oral mucous membranes and tongue, poor skin turgor, and sunken eyeballs. His blood pressure is 94/44, and his pulse is rapid and thready. He is weak, dizzy, and disoriented about time and place. Diagnostic tests reveal the following abnormal findings at 8:30 A.M.: EKG: widening QRS complex and increased PR interval Sodium: 129 mEq/L (normal range: 135 to 145 mEq/L) Glucose: 54 mg/dL (normal range: 70 to 110 mg/dL) Potassium: 5.3 mEq/L (normal range: 3.5 to 5 mEq/L) Cortisol: 2 mg/dL (normal for A.M.: 5 to 23 mg/dL)
EVALUATION
Following treatment for acute adrenal insufficiency, Mr. Sardoff is no longer dehydrated, and his blood pressure has returned to his normal reading of 132/88. He is alert and oriented, and anxious to learn to care for himself at home. After dietary instructions and teaching for self-care that included his wife, Mr. Sardoff verbalizes an understanding of his illness and the need to take his medication carefully and accurately. A referral is made to a social worker for assistance with costs of medications.
The medical orders for Mr. Sardoff include intravenous administration of 5% dextrose in normal saline (D5NS) at 250 mL/h and hydrocortisone (Solu-Cortef ) 200 mg. After the fluids and medication are initiated, Mr. Sardoff is moved to an in-hospital medical bed.
DIAGNOSIS
Deficient fluid volume, related to hypovolemia secondary to adrenal insufficiency Ineffective tissue perfusion: Peripheral, related to fluid volume deficit Anxiety, related to lack of knowledge about the effects and treatment of adrenal insufficiency
Critical Thinking in the Nursing Process
1. Adrenal insufficiency is often diagnosed only when the client becomes seriously ill in response to a stressor. Explain why this statement is or is not true. 2. Describe the physical assessments that are found in the severely dehydrated client. 3. Outline a teaching plan for Mr. Sardoff with foods for a highsodium, low-potassium diet. See Evaluating Your Response in Appendix C.
EXPECTED OUTCOMES
Regain normal fluid balance.
Potrebbero piacerti anche
- Generic NameDocumento2 pagineGeneric NamePerdie Branden ReizNessuna valutazione finora
- Propranolol 1 PresentationDocumento17 paginePropranolol 1 Presentationapi-284092317100% (1)
- Terazosin Hytrin Drug CardDocumento1 paginaTerazosin Hytrin Drug CardSheri490Nessuna valutazione finora
- Case Study - Addison's DiseaseDocumento1 paginaCase Study - Addison's DiseaseBadette EndayaNessuna valutazione finora
- Epoetin AlfaDocumento3 pagineEpoetin Alfaapi-3797941Nessuna valutazione finora
- MetronidazoleDocumento4 pagineMetronidazoleapi-3797941100% (4)
- Drug Study HaldolDocumento2 pagineDrug Study HaldolGracia EvangelistaNessuna valutazione finora
- Atomoxetine Hydro ChlorideDocumento3 pagineAtomoxetine Hydro Chlorideapi-3797941Nessuna valutazione finora
- NardilDocumento4 pagineNardilTemerNessuna valutazione finora
- Final Case StudyDocumento18 pagineFinal Case Studyapi-487702467100% (1)
- DRUGSTUDY RANITIDINE, METRONIDAZOLE, CEFUROXIME, KEtorolac NUBainDocumento7 pagineDRUGSTUDY RANITIDINE, METRONIDAZOLE, CEFUROXIME, KEtorolac NUBainKyle Cholo CholoNessuna valutazione finora
- Olmesartan Drug StudyDocumento2 pagineOlmesartan Drug StudydyndzNessuna valutazione finora
- Co DiovanDocumento2 pagineCo DiovanianecunarNessuna valutazione finora
- Darbepoetin AlfaDocumento3 pagineDarbepoetin Alfaapi-3797941Nessuna valutazione finora
- RisperidoneDocumento3 pagineRisperidoneapi-3797941Nessuna valutazione finora
- Risk For Bleeding - Cirrhosis NCPDocumento2 pagineRisk For Bleeding - Cirrhosis NCPPaula AbadNessuna valutazione finora
- What Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistDocumento12 pagineWhat Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistLidiaAMonroyRNessuna valutazione finora
- NCP 1Documento7 pagineNCP 1NataCo100% (1)
- HIV Case Study: Priority Nursing Diagnoses and CareDocumento3 pagineHIV Case Study: Priority Nursing Diagnoses and CarechoobiNessuna valutazione finora
- Case Study PP - AdhdDocumento21 pagineCase Study PP - Adhdapi-482726932100% (1)
- LevofloxacinDocumento3 pagineLevofloxacinapi-3797941100% (2)
- Drug StudyDocumento3 pagineDrug StudyKorina FranciscoNessuna valutazione finora
- Page 17 ACUTE PAIN Related To Joint Stiffness Secondary To Aging.Documento3 paginePage 17 ACUTE PAIN Related To Joint Stiffness Secondary To Aging.Senyorita KHayeNessuna valutazione finora
- Drug Study GuideDocumento2 pagineDrug Study GuideAubrey Sunga100% (1)
- HNBBDocumento3 pagineHNBBManelle SingzonNessuna valutazione finora
- SalmeterolDocumento2 pagineSalmeterolapi-3797941Nessuna valutazione finora
- ChlorpromazineDocumento1 paginaChlorpromazineimthebossNessuna valutazione finora
- Drug Study March 03 2011Documento10 pagineDrug Study March 03 2011zhapper2002Nessuna valutazione finora
- Zolpidem TartrateDocumento2 pagineZolpidem Tartrateapi-3797941Nessuna valutazione finora
- Chromium Picolinate Drug StudyDocumento1 paginaChromium Picolinate Drug StudyjoellaNessuna valutazione finora
- Levofloxacin: A Potent Fluoroquinolone AntibioticDocumento2 pagineLevofloxacin: A Potent Fluoroquinolone AntibioticEliza Rahardja100% (1)
- Drug Profile - AmantadinDocumento14 pagineDrug Profile - AmantadinAna TanNessuna valutazione finora
- Drug StudyDocumento8 pagineDrug StudyRizzi DeveraNessuna valutazione finora
- Furosemid Citicoline Clexane, LevofloxacinDocumento9 pagineFurosemid Citicoline Clexane, Levofloxacincotyboy50% (2)
- AminophyllineDocumento6 pagineAminophyllineapi-3797941100% (1)
- PrednisoneDocumento22 paginePrednisoneAlthea AlicandoNessuna valutazione finora
- P 398Documento1 paginaP 398Arup Ratan PaulNessuna valutazione finora
- Drug StudyDocumento8 pagineDrug StudyzenNessuna valutazione finora
- Thioridazine hydrochloride for schizophrenia treatmentDocumento1 paginaThioridazine hydrochloride for schizophrenia treatmentGritoNessuna valutazione finora
- Sleep Pattern DisturbanceDocumento4 pagineSleep Pattern DisturbanceVirusNessuna valutazione finora
- MorphineDocumento3 pagineMorphineAizat KamalNessuna valutazione finora
- Case Presentation Hypokalemic ManDocumento61 pagineCase Presentation Hypokalemic ManHussain AzharNessuna valutazione finora
- Isosorbide NitratesDocumento3 pagineIsosorbide Nitratesapi-3797941Nessuna valutazione finora
- HydroxyzineDocumento3 pagineHydroxyzineapi-3797941100% (2)
- Activated CharcoalDocumento1 paginaActivated CharcoalSupreeth PrasadNessuna valutazione finora
- Case StudyDocumento11 pagineCase StudyRadenroro Atih Utari RizkyNessuna valutazione finora
- Chloral Hydrate (Drug Study)Documento3 pagineChloral Hydrate (Drug Study)Franz.thenurse6888Nessuna valutazione finora
- Vit B1 ReportDocumento19 pagineVit B1 ReportNatasha Faye UntalanNessuna valutazione finora
- Drug mechanism indication contraindication side effects nursingDocumento1 paginaDrug mechanism indication contraindication side effects nursinghahahahaaaaaaaNessuna valutazione finora
- VI. Laboratory ResultsDocumento5 pagineVI. Laboratory ResultsCendaña LorelynNessuna valutazione finora
- COPD Drug Study: Ipratropium Bromide and Albuterol SulfateDocumento9 pagineCOPD Drug Study: Ipratropium Bromide and Albuterol SulfateShane Arroyo100% (1)
- Dynastat: What Is in This LeafletDocumento4 pagineDynastat: What Is in This LeafletBenj GilbuenaNessuna valutazione finora
- DRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDocumento7 pagineDRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDewinta AbutNessuna valutazione finora
- Esomeprazole MagnesiumDocumento3 pagineEsomeprazole Magnesiumapi-3797941100% (1)
- Nortriptyline Hydro ChlorideDocumento3 pagineNortriptyline Hydro Chlorideapi-3797941Nessuna valutazione finora
- CCMH Drug StudyDocumento5 pagineCCMH Drug StudyJoy JarinNessuna valutazione finora
- Colchicine Dosage Guide for Acute Gout and MoreDocumento6 pagineColchicine Dosage Guide for Acute Gout and MoreHam SotheaNessuna valutazione finora
- Surg2 Primary Aldosteronism AssignmentDocumento8 pagineSurg2 Primary Aldosteronism AssignmentDarain Mohammed MeirNessuna valutazione finora
- HypertensionDocumento38 pagineHypertensionmariatheressamercadoNessuna valutazione finora
- LIBRO - Shengmai SanDocumento151 pagineLIBRO - Shengmai SanEduardoArellanoFrancoNessuna valutazione finora
- Adrian Castelan Resume 3Documento2 pagineAdrian Castelan Resume 3api-532744620Nessuna valutazione finora
- 1st QTR MAPEH 6 Notes 2 Proper NutritionDocumento4 pagine1st QTR MAPEH 6 Notes 2 Proper NutritionRen PandesNessuna valutazione finora
- Continuing Nursing Education: Importance of Lifelong LearningDocumento6 pagineContinuing Nursing Education: Importance of Lifelong LearningDebashrita MisraNessuna valutazione finora
- What's in A Name? - The Kew AsylumDocumento9 pagineWhat's in A Name? - The Kew AsylumIsabelle FarlieNessuna valutazione finora
- HRH Data Mapping TemplateDocumento24 pagineHRH Data Mapping TemplateJohn DanielNessuna valutazione finora
- Blood Pressure ChartDocumento5 pagineBlood Pressure Chartmahajan1963100% (1)
- Assignment On Unconciousness: Subject:-Advanced Nursing PracticeDocumento15 pagineAssignment On Unconciousness: Subject:-Advanced Nursing PracticeShaells JoshiNessuna valutazione finora
- Why Bladder Training Prior To Foley Catheter Removal Is Not BestDocumento10 pagineWhy Bladder Training Prior To Foley Catheter Removal Is Not BestManoj KumarNessuna valutazione finora
- Invent A RioDocumento56 pagineInvent A RioJhoel Eusebio Parraga IsidroNessuna valutazione finora
- NURSING DIAGNOSIS ANALYSIS: PAIN MANAGEMENTDocumento1 paginaNURSING DIAGNOSIS ANALYSIS: PAIN MANAGEMENTdude06blumNessuna valutazione finora
- NCP DrainageDocumento3 pagineNCP DrainageRuby GuarinNessuna valutazione finora
- EPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREDocumento6 pagineEPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREArjun CVNessuna valutazione finora
- Sam PDFDocumento134 pagineSam PDFPunit Garg100% (2)
- Cavite State University: I. ObjectivesDocumento7 pagineCavite State University: I. ObjectivesChamy CruzNessuna valutazione finora
- Hepatic Dysfunction in Dengue Fever - A ProspectiveDocumento20 pagineHepatic Dysfunction in Dengue Fever - A ProspectiveSanjay RaoNessuna valutazione finora
- Knee Joint Aspiration and InjectionDocumento4 pagineKnee Joint Aspiration and InjectionaimanshalpyNessuna valutazione finora
- East Africa University Bosaso, Puntland Somalia Faculty of Medicine Communicable Disease MR Buruj Ali SaladDocumento42 pagineEast Africa University Bosaso, Puntland Somalia Faculty of Medicine Communicable Disease MR Buruj Ali SaladShaimaa AbdulkadirNessuna valutazione finora
- Toxoplasmosis: Causes, Symptoms & PreventionDocumento27 pagineToxoplasmosis: Causes, Symptoms & PreventionKnjigeNessuna valutazione finora
- Dwi Warna Aju FatmawatiDocumento4 pagineDwi Warna Aju FatmawatiAnonymous FiiSmGgNessuna valutazione finora
- Clinical Assessment and Examination in OrthopedicsDocumento196 pagineClinical Assessment and Examination in OrthopedicsMom of twoNessuna valutazione finora
- Incidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyDocumento7 pagineIncidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyGusBlomkvistSomocurioNessuna valutazione finora
- NCP For Impaired MobilityDocumento4 pagineNCP For Impaired MobilityBettinaFernandoNessuna valutazione finora
- Mantoux TestDocumento3 pagineMantoux Testfarrukhhussain2006Nessuna valutazione finora
- 7 Computer Generated Nursing Care Plans QuestionnaireDocumento4 pagine7 Computer Generated Nursing Care Plans QuestionnaireangeldreddNessuna valutazione finora
- A Standardized Endodontic Technique Utilizing Newly Designed Instruments and Filling Materials PDFDocumento9 pagineA Standardized Endodontic Technique Utilizing Newly Designed Instruments and Filling Materials PDFCristian FernandoNessuna valutazione finora
- Case Study SLDocumento5 pagineCase Study SLCharmie Mei Paredes-RoqueNessuna valutazione finora
- Apply now: OSHA inspector positions open in Tanzania zonesDocumento4 pagineApply now: OSHA inspector positions open in Tanzania zonesMc Eddy MarshalNessuna valutazione finora
- PBRL 420 Unilever Media KitDocumento8 paginePBRL 420 Unilever Media Kitapi-650275339Nessuna valutazione finora
- Laporan Harian Pasien Puskesmas JatinegaraDocumento8 pagineLaporan Harian Pasien Puskesmas JatinegaraanggaNessuna valutazione finora