Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Brain Abscess
Caricato da
Tamil VillardoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Brain Abscess
Caricato da
Tamil VillardoCopyright:
Formati disponibili
BRAIN ABSCESS A brain abscess is a collection of pus, immune cells, and other material in the brain, usually from
a bacterial or fungal infection. Causes Brain abscesses commonly occur when bacteria or fungi infect part of the brain. Swelling and irritation (inflammation) develop in response to this infection. Infected brain cells, white blood cells, live and dead bacteria, and fungi collect in an area of the brain. Tissue forms around this area and creates a mass. While this immune response can protect the brain by isolating the infection, it can also do more harm than good. The brain swells. Because the skull cannot expand, the mass may put pressure on delicate brain tissue. Infected material can block the blood vessels of the brain. The germs that cause a brain abscess can reach the brain through the blood. The source of the infection is often not found. However, the most common source is a lung infection. Less often, a heart infection is the cause. Germs may also travel from a nearby infected area (for example, an ear infection or a tooth abscess) or enter the body during an injury (such as a gun or knife wound) or neurosurgery. In children with congenital heart disease or a blood vessel birth defect, such as those with Tetralogy of Fallot, infections are more able to reach the brain from the intestines, teeth, or other body areas. The following raise your risk of a brain abscess: A weakened immune system (such as in AIDS patients) Chronic disease, such as cancer Drugs that suppress the immune system (corticosteroids or chemotherapy) Right-to-left heart shunts, usually the result of congenital heart disease Symptoms Symptoms may develop slowly, over a period of 2 weeks, or they may develop suddenly. They may include:
Changes in mental status Confusion Decreasing responsiveness Drowsiness Eventual coma Inattention Irritability Slow thought processes Decreased movement Decreased sensation Decreased speech (aphasia) Fever and chills Headache Language difficulties Loss of coordination Loss of muscle function, typically on one side Seizures Stiff neck Vision changes Vomiting Exams and Tests A brain and nervous system (neurological) exam will usually show signs of increased intracranial pressure and problems with brain function. Tests to diagnose a brain abscess may include: Blood cultures Chest x-ray Complete blood count (CBC) Head CT scan Electroencephalogram (EEG) MRI of head Testing for the presence of antibodies to organisms such as Toxoplasma gondii and Taenia solium A needle biopsy is usually performed to identify the cause of the infection. Treatment A brain abscess is a medical emergency. Pressure inside the skull may become high enough to be life threatening. You will need to stay in the hospital until the condition is stable. Some people may need life support. Medication, not surgery, is recommended if you have: Several abscesses (rare)
A small abscess (less than 2 cm) An abscess deep in the brain An abscess and meningitis Shunts in the brain for hydrocephalus (in some cases the shunt may need to be removed temporarily or replaced) Toxoplasma gondii infection in a person with HIV Antibiotics will be prescribed. Antibiotics that work against a number of different bacteria (broad spectrum antibiotics) are most commonly used. You may be prescribed several different types of antibiotics to make sure treatment works. Antifungal medications may also be prescribed if the infection is likely caused by a fungus. Immediate treatment may be needed if an abscess is injuring brain tissue by pressing on it, or there is a large abscess with a large amount of swelling around that it is raising pressure in the brain. Surgery is needed if : Increased pressure in the brain continues or gets worse The brain abscess does not get smaller after medication The brain abscess contains gas (produced by some types of bacteria) The brain abscess might break open (rupture) Surgery consists of opening the skull, exposing the brain, and draining the abscess. Laboratory tests are often done to examine the fluid. This can help identify what is causing the infection, so that more appropriate antibiotics or antifungal drugs can be prescribed. The surgical procedure used depends on the size and depth of the abscess. The entire abscess may be removed (excised) if it is near the surface and enclosed in a sac. Needle aspiration guided by CT or MRI scan may be needed for a deep abscess. During this procedure, medications may be injected directly into the mass. Certain diuretics and steroids may also be used to reduce swelling of the brain.
Outlook (Prognosis) If untreated, a brain abscess is almost always deadly. With treatment, the death rate is about 10 - 30%. The earlier treatment is received, the better. Some patients may have long-term neurological problems after surgery. Possible Complications Brain damage Meningitis that is severe and life threatening Return (recurrence) of infection Seizures When to Contact a Medical Professional Go to a hospital emergency room or call the local emergency number (such as 911) if you have symptoms of a brain abscess. Prevention You can reduce the risk of developing a brain abscess by treating any disorders that can cause them. Have a follow-up examination after infections are treated. Some people, including those with certain heart disorders, may receive antibiotics before dental or urological procedures to help reduce the risk of infection. Alternative Names Abscess - brain; Cerebral abscess; CNS abscess
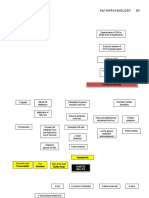
PAYHOPHYSIOLOGY : Brain abscesses may be single or multiple. Each abscess begins as a microscopic focus of septic, microvascular injury, usually within white matter or at the gray-white junction. Growth of bacteria within this focus produces a localized encephalitis or "cerebritis," which undergoes liquefaction (Britt and Enzmann 1983; Enzmann et al 1983; Pendlebury et al 1989). The developing abscess elicits an inflammatory response of lymphocytes and polymorphonuclear leukocytes, with localized, frequently intense cerebral edema. Over time, an abscess capsule forms, consisting of both fibrotic and gliotic elements. The abscess capsule tends to be thickest on its cortical surface and thinnest medially, causing the abscess to expand toward and rupture into the ventricular system (Kastenbauer et al 2004). Death in brain abscess may result from tonsillar herniation, caused by the mass effect of the abscess and its surrounding cerebral edema, or from rupture of the abscess into the ventricular system. Brain abscesses most frequently arise following hematogenous dissemination of organisms from distant sites of infection. The most common associated systemic infections are chronic lung infections, in particular bronchiectasis and lung abscess, and acute bacterial endocarditis (Greenlee and Mandell 1973; Bleck and Greenlee 2000; Kastenbauer et al 2004). Brain abscess is particularly likely in conditions in which a right-to-left cardiac shunt allows organisms to move directly from the venous circulation into left-sided systemic circulation. For this reason, children with cyanotic congenital heart disease are at particular risk for hematogenous brain abscess (Cole et al 2012; Ozsurekci et al 2012), as are patients with hereditary hemorrhagic telangiectasia (Tabakow et al 2005; Galitelli et al 2006a; 2006b; Sell et al 2008; Corre et al 2011). Rarely, brain abscess may also complicate pulmonary arteriovenous fistulae not associated with hereditary hemorrhagic
telangiectasia or in the setting of a patent foramen ovale (Kawano et al 2009). Less frequently, brain abscesses result from spread of organisms through emissary veins during sinusitis, otitis, or mastoiditis (Bleck and Greenlee 2000). Historically, otitis represented the major pericranial infection associated with brain abscess; at present, however, brain abscess is more frequently associated with frontal, ethmoidal, and sphenoidal sinusitis (Kastenbauer et al 2004), and the most common site of brain abscess is the frontal lobe (Roche et al 2003). Less frequent causes of brain abscess include penetrating trauma, neurosurgical procedures, facial infections, and dental sepsis (Kastenbauer et al 2004). A single case report lists brain abscess as a complication of tongue piercing (Herskovitz et al 2009). Brain abscesses of hematogenous origin are most common in the distribution of the middle cerebral artery, followed by those of the anterior cerebral artery and posterior circulation (Kastenbauer et al 2004). Abscesses arising from frontal and ethmoidal sinusitis are most commonly located within the frontal lobe (Bleck and Greenlee 2000). Sphenoid sinusitis may cause frontal or temporal lobe abscesses. Infections of the middle ear or mastoid may spread through emissary veins into the middle fossa to cause temporal lobe abscesses or into the posterior fossa to cause cerebellar abscess (Bleck and Greenlee 2000; Kastenbauer et al 2004).
Potrebbero piacerti anche
- Cretenism Case StudyDocumento8 pagineCretenism Case StudyMonica Marie MoralesNessuna valutazione finora
- Case Report On Bipolar Affective Disorder: Mania With Psychotic SymptomsDocumento2 pagineCase Report On Bipolar Affective Disorder: Mania With Psychotic SymptomskslhfwoiebvNessuna valutazione finora
- Cerebral Aneurysm Case Analysis and Concept MapDocumento5 pagineCerebral Aneurysm Case Analysis and Concept Mapate NarsNessuna valutazione finora
- Drug Study - PiptazDocumento1 paginaDrug Study - PiptazMutya XDNessuna valutazione finora
- Neonatal Respiratory Distress SyndromenhschoicesDocumento6 pagineNeonatal Respiratory Distress SyndromenhschoicessehatkanNessuna valutazione finora
- Simmond's Disease MSDocumento22 pagineSimmond's Disease MSRocel Devilles100% (1)
- Teaching Plan 7Documento61 pagineTeaching Plan 7dinman_rituraj1683Nessuna valutazione finora
- Cretinism: Amira Fithri R. Supervisor: Dr. Imam Kusmadi, Sp. ADocumento27 pagineCretinism: Amira Fithri R. Supervisor: Dr. Imam Kusmadi, Sp. AAmira FRNessuna valutazione finora
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocumento9 pagineAssessment Diagnosis Planning Intervention Rationale EvaluationYzel Vasquez AdavanNessuna valutazione finora
- Post Cesarean Section DeliveryDocumento5 paginePost Cesarean Section Deliveryᒙᕧᖇᕦᙏᖻ ᗴᔛᓦᗩᖆᗩNessuna valutazione finora
- Discharge Planning PaperDocumento5 pagineDischarge Planning Paperapi-283173905Nessuna valutazione finora
- Surgical Managment of DMDocumento42 pagineSurgical Managment of DMHaroon Malik100% (1)
- Compre Ho PsychDocumento114 pagineCompre Ho PsychRyan Mae Tutor GarciaNessuna valutazione finora
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDocumento8 pagineNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiNessuna valutazione finora
- Case 2 Hydrocephalus Group 4Documento27 pagineCase 2 Hydrocephalus Group 4younggirldavidNessuna valutazione finora
- The Pathophysiology of LabyrinthitisDocumento2 pagineThe Pathophysiology of LabyrinthitisSurya Michael ChanceNessuna valutazione finora
- Case Study Ugib Lower MBDocumento65 pagineCase Study Ugib Lower MBQuolette Constante100% (1)
- Discharge Plan Post SeizureDocumento2 pagineDischarge Plan Post SeizureVecky TolentinoNessuna valutazione finora
- ParacetamolDocumento2 pagineParacetamolsleep whatNessuna valutazione finora
- Case Study - Dengue Fever V - S UtiDocumento12 pagineCase Study - Dengue Fever V - S UtiHarlene Joyce ReyNessuna valutazione finora
- Decreased Cardiac OutputDocumento4 pagineDecreased Cardiac OutputAdnan Khan100% (1)
- Femur FractureDocumento19 pagineFemur FractureMadx VNessuna valutazione finora
- PneumoniaDocumento2 paginePneumoniaPia MedinaNessuna valutazione finora
- Impaired Comfort PruritisDocumento5 pagineImpaired Comfort PruritisBondan PalestinNessuna valutazione finora
- Cefixime: Suprax Class and CategoryDocumento3 pagineCefixime: Suprax Class and CategoryArianne Joy SalvadorNessuna valutazione finora
- Random Blood Sugar Estimation and Its SignificanceDocumento11 pagineRandom Blood Sugar Estimation and Its Significanceapi-38237850% (1)
- Pathophysiology Cushing S SyndromeDocumento4 paginePathophysiology Cushing S SyndromeMaria Luisa VillalunaNessuna valutazione finora
- Drug StudyDocumento40 pagineDrug StudyLyka Milo AvilaNessuna valutazione finora
- PathophysiologyDocumento9 paginePathophysiologySuzette PipoNessuna valutazione finora
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocumento5 pagineTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNessuna valutazione finora
- What Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistDocumento12 pagineWhat Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistLidiaAMonroyRNessuna valutazione finora
- Knowledge DeficitDocumento5 pagineKnowledge DeficitteamstrocaNessuna valutazione finora
- 2 - Prevention of Iatrogenic InjuriesDocumento34 pagine2 - Prevention of Iatrogenic InjuriesMariya DantisNessuna valutazione finora
- Preoperative Skin PreparationDocumento16 paginePreoperative Skin PreparationSyahri DzikriNessuna valutazione finora
- Dental Prob NCPDocumento3 pagineDental Prob NCPx483xDNessuna valutazione finora
- JDM Care PlanDocumento5 pagineJDM Care PlangopscharanNessuna valutazione finora
- MicrocephalyDocumento4 pagineMicrocephalykurei_bluflamedNessuna valutazione finora
- ASTHMADocumento9 pagineASTHMAmildred alidonNessuna valutazione finora
- Types of ShocksDocumento33 pagineTypes of Shocksmark OrpillaNessuna valutazione finora
- DRUG STUDY (Dextromethorphan)Documento2 pagineDRUG STUDY (Dextromethorphan)Avianna CalliopeNessuna valutazione finora
- Seizure PathophysiologyDocumento2 pagineSeizure PathophysiologyqwertyuiopNessuna valutazione finora
- Pathophysiology: Risk FactorsDocumento4 paginePathophysiology: Risk FactorsEdson John DemayoNessuna valutazione finora
- Nursing AssessmentDocumento3 pagineNursing AssessmentJanine PelayoNessuna valutazione finora
- 8 PathoDocumento2 pagine8 PathoKris LingadNessuna valutazione finora
- NCP BMDocumento1 paginaNCP BMSourabh MehraNessuna valutazione finora
- Spinal Cord InjuryDocumento28 pagineSpinal Cord InjuryLouie John AbilaNessuna valutazione finora
- CroupDocumento20 pagineCroupFariezuan HamidNessuna valutazione finora
- 2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and ChildDocumento3 pagine2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and Childclint xavier odangoNessuna valutazione finora
- Assessment Nursing Diagnosis Analysis Goal and Objective S Nursing Interventio N Rationale EvaluationDocumento3 pagineAssessment Nursing Diagnosis Analysis Goal and Objective S Nursing Interventio N Rationale EvaluationJhun GonzalesNessuna valutazione finora
- Drug Study ColestipolDocumento3 pagineDrug Study ColestipolAbby AngNessuna valutazione finora
- Nursing Care PlanDocumento3 pagineNursing Care PlanZahrah ZahrahNessuna valutazione finora
- Laryngeal Obstruction: Narciso A. CañibanDocumento54 pagineLaryngeal Obstruction: Narciso A. Cañibanalexandrajane200767% (3)
- Impaired Gas Exchange NCPDocumento3 pagineImpaired Gas Exchange NCPRomel BaliliNessuna valutazione finora
- RABIES Health Teaching BSN1DDocumento24 pagineRABIES Health Teaching BSN1DTheother OneNessuna valutazione finora
- Anti HistamineDocumento15 pagineAnti HistamineOoi Ah GuanNessuna valutazione finora
- Drug Study 1Documento15 pagineDrug Study 1Czarina Isabela TuazonNessuna valutazione finora
- O o o o o o O: Brain AbscessDocumento3 pagineO o o o o o O: Brain Abscessanilk_232Nessuna valutazione finora
- Brain Abscess: All You Need To Know: Symptoms Causes How Infection Enters The Brain Diagnosis Treatment OutlookDocumento11 pagineBrain Abscess: All You Need To Know: Symptoms Causes How Infection Enters The Brain Diagnosis Treatment OutlookAlfrien Ivanovich LarchsonNessuna valutazione finora
- Brain Abscess (MEDSURG)Documento3 pagineBrain Abscess (MEDSURG)Yessamin Paith RoderosNessuna valutazione finora
- Immune SystemDocumento1 paginaImmune SystemTamil VillardoNessuna valutazione finora
- BotulismDocumento2 pagineBotulismTamil VillardoNessuna valutazione finora
- Pathophysiology ScribdDocumento8 paginePathophysiology ScribdTamil VillardoNessuna valutazione finora
- Cues Nursing Diagnosis Scientific Rationale Objective Nursing Interventi ON Rationale EvaluationDocumento9 pagineCues Nursing Diagnosis Scientific Rationale Objective Nursing Interventi ON Rationale EvaluationTamil VillardoNessuna valutazione finora
- NCPDocumento14 pagineNCPTamil VillardoNessuna valutazione finora
- Project IN English V: Submitted To: Mrs. Jasmin de La Torre Teacher Submitted By: Nick T. Gorne V-CattleyaDocumento7 pagineProject IN English V: Submitted To: Mrs. Jasmin de La Torre Teacher Submitted By: Nick T. Gorne V-CattleyaTamil VillardoNessuna valutazione finora
- Generic Name: Amikacin SulfateDocumento2 pagineGeneric Name: Amikacin Sulfateichiro017100% (7)
- Drug Name General Action Specific Action Indication Contraindicati ON Adverse Effect NSG ResponsibilityDocumento1 paginaDrug Name General Action Specific Action Indication Contraindicati ON Adverse Effect NSG ResponsibilityTamil VillardoNessuna valutazione finora
- Quadrant of Deception: Quadrant I (Urgent, Important) Quadrant Ii (Not Urgent, Important)Documento1 paginaQuadrant of Deception: Quadrant I (Urgent, Important) Quadrant Ii (Not Urgent, Important)Tamil VillardoNessuna valutazione finora
- Penicillin G BenzathineDocumento1 paginaPenicillin G BenzathineIvanne Hisoler100% (7)
- Fluid Volume ExcessDocumento4 pagineFluid Volume ExcessTamil Villardo100% (2)
- Fluid Volume ExcessDocumento4 pagineFluid Volume ExcessTamil Villardo100% (2)
- Nursing Care of A Child With Respiratory DisorderDocumento69 pagineNursing Care of A Child With Respiratory DisorderTamil Villardo100% (1)
- Nebulization (Final Output)Documento5 pagineNebulization (Final Output)Tamil Villardo100% (2)
- Mpaired Skin Integrity.Documento8 pagineMpaired Skin Integrity.Tamil VillardoNessuna valutazione finora
- Prep, Dressing, Draping The PatientDocumento60 paginePrep, Dressing, Draping The PatientTamil Villardo100% (1)
- CuesDocumento2 pagineCuesTamil VillardoNessuna valutazione finora
- Surgical Stoma Large Intestine Colon Incision Anterior Abdominal Wall Suturing Stoma Appliance FecesDocumento10 pagineSurgical Stoma Large Intestine Colon Incision Anterior Abdominal Wall Suturing Stoma Appliance FecesTamil VillardoNessuna valutazione finora
- BreastDocumento27 pagineBreastRasha HelmyNessuna valutazione finora
- Lung AbscessDocumento30 pagineLung AbscessArmoured SpartanNessuna valutazione finora
- CellulitisDocumento8 pagineCellulitisgrool29rNessuna valutazione finora
- AbscessDocumento4 pagineAbscessShivBalakChauhanNessuna valutazione finora
- Modern Management of Pyogenic Hepatic Abscess: A Case Series and Review of The LiteratureDocumento8 pagineModern Management of Pyogenic Hepatic Abscess: A Case Series and Review of The LiteratureAstari Pratiwi NuhrintamaNessuna valutazione finora
- Peroneal Nerve InjuryDocumento10 paginePeroneal Nerve InjuryDinda_malaikat96okeeNessuna valutazione finora
- Help PrimarysurgeryDocumento881 pagineHelp PrimarysurgeryEzio Auditore da FirenzeNessuna valutazione finora
- Compendium For Surgery Tutorials - NewDocumento835 pagineCompendium For Surgery Tutorials - NewAbdullahi HabibNessuna valutazione finora
- Mehu525 - U2 - T7 - Cutaneous Bacterial Infections Caused by Staphylococcus Aureus and Streptococcus Pyogenes in Infants and ChildrenDocumento22 pagineMehu525 - U2 - T7 - Cutaneous Bacterial Infections Caused by Staphylococcus Aureus and Streptococcus Pyogenes in Infants and ChildrenJorge OtoyaNessuna valutazione finora
- SURGICAL SITE INFECTION. - Prevention and CareDocumento68 pagineSURGICAL SITE INFECTION. - Prevention and Caretummalapalli venkateswara rao50% (2)
- Pyomyositis (Ca1)Documento66 paginePyomyositis (Ca1)Emman Ramos60% (5)
- Diabetic FootDocumento7 pagineDiabetic FootWiindha Tahta Alfina CiigejeeNessuna valutazione finora
- Mohomad Al-Sawah, Guy Richard Pupp, DPM, FACFAS : DPM Priya Samant, DPM Dustan Mascarenhas, MDDocumento1 paginaMohomad Al-Sawah, Guy Richard Pupp, DPM, FACFAS : DPM Priya Samant, DPM Dustan Mascarenhas, MDbaoNessuna valutazione finora
- Dermatologia Pediatrica Pediatric Dermatology For The Primary Care Provider 2014 PDFDocumento247 pagineDermatologia Pediatrica Pediatric Dermatology For The Primary Care Provider 2014 PDFJacquelin DiazNessuna valutazione finora
- Infection & Specific Wound InfectionsDocumento39 pagineInfection & Specific Wound InfectionsAhmed ShorshNessuna valutazione finora
- Gastrointestinal Fistula: DR Vihar Kotecha M.D, M.MED Gen Surg (Nbi), FCS Gen Surg (ECSA) Lecturer CUHASDocumento60 pagineGastrointestinal Fistula: DR Vihar Kotecha M.D, M.MED Gen Surg (Nbi), FCS Gen Surg (ECSA) Lecturer CUHASSangija kamataNessuna valutazione finora
- Week 6 SpondyloarthropathiesDocumento124 pagineWeek 6 SpondyloarthropathiesJoeNessuna valutazione finora
- CDC/NHSN Surveillance Definitions For Specific Types of InfectionsDocumento30 pagineCDC/NHSN Surveillance Definitions For Specific Types of InfectionssofiaNessuna valutazione finora
- Puerperium ComplicationsDocumento28 paginePuerperium ComplicationsyayayanizaNessuna valutazione finora
- Parameters of Care Supplement: Parameter On Acute Periodontal DiseasesDocumento4 pagineParameters of Care Supplement: Parameter On Acute Periodontal DiseasesThaisOliveiraNessuna valutazione finora
- Odessa National Medical University: Surgical InfectionsDocumento34 pagineOdessa National Medical University: Surgical InfectionsDrRajneesh ShastriNessuna valutazione finora
- MUEDocumento269 pagineMUEKian GonzagaNessuna valutazione finora
- InflammationDocumento41 pagineInflammationbharath goNessuna valutazione finora
- Musculoskeleta L Infection) : Ismail BastomiDocumento46 pagineMusculoskeleta L Infection) : Ismail BastomiYUFFANessuna valutazione finora
- StaphDocumento1 paginaStaphPrabhjot Singh BakshiNessuna valutazione finora
- Chest Trauma: Prof. Anjum Sohail Ansari H.O.D Surgery Cims, BahawalpurDocumento37 pagineChest Trauma: Prof. Anjum Sohail Ansari H.O.D Surgery Cims, BahawalpurAmnaNessuna valutazione finora
- Case Report Tuberculous Otitis MediaDocumento23 pagineCase Report Tuberculous Otitis MediahwelpNessuna valutazione finora
- Abses GluteusDocumento6 pagineAbses GluteusAndreas NatanNessuna valutazione finora
- All Case Rate 3 PDFDocumento2 pagineAll Case Rate 3 PDFAmanda JonesNessuna valutazione finora
- Assessment of WoundDocumento113 pagineAssessment of WoundChalie MequanentNessuna valutazione finora