Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
GLM0011 Shoulder Dystocia
Caricato da
nityaprasantaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
GLM0011 Shoulder Dystocia
Caricato da
nityaprasantaCopyright:
Formati disponibili
Canterbury DHB
Womens & Childrens Health
SHOULDER DYSTOCIA
DEFINITION Shoulder dystocia is defined as a birth which requires additional manoeuvres to release the shoulders after gentle downward traction has failed1. It occurs due to impaction of the anterior shoulder against the maternal symphysis pubis, or less commonly the posterior shoulder impacted against the sacral promontory 2.
INCIDENCE Incidences of 0.58% to 0.7% vaginal births have been reported.1 RISK FACTORS The following antenatal and intrapartum characteristics have been reported to be associated with shoulder dystocia4: Pre-labour Fetal macrosomia* Maternal BMI > 30kg/m2 Diabetes Induction of Labour Previous shoulder dystocia Intrapartum Prolonged first stage Secondary arrest in labour Prolonged second stage Oxytocin augmentation Assisted vaginal birth
*Although there is a link between fetal size and shoulder dystocia, 48% of incidences occur in infants with a birth weight less than 4000g2 Shoulder dystocia is often an unpredictable and unpreventable event. The large majority of cases occur in the infants of women with no risk factors. In cases of shoulder dystocia resulting in infant morbidity, only 16% had identified risk factors1. COMPLICATIONS Shoulder dystocia is an obstetric emergency that may lead to complications for both the woman and her baby including: Maternal Genital tract trauma Increased rates of 3rdand 4th degree tears - Uterine rupture Symphysial separation Postpartum haemorrhage Psychological distress/trauma
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group Page 1 of 10 Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
Neonatal Brachial plexus injuries (e.g. Erbs, Klumpkes palsies) Clavicular & humeral fractures Fetal acidosis/hypoxia may lead to permanent neurological damage Fetal/neonatal death
Regular training for all health professionals attending births is essential for the reduction of these complications1. PREVENTION In cases of suspected macrosomia: Without diabetes: Elective caesarean section is NOT indicated With diabetes: Elective caesarean section may be considered following discussion with consultant obstetrician In cases of maternal diabetes: Maintain tight glycaemic control Monitor weight gain during preconception and pregnancy care In cases of previous shoulder dystocia: Either caesarean section or vaginal birth is appropriate in women, taking into consideration the severity of previous shoulder dystocia (eg: manoeuvres required, maternal trauma and neonatal morbidity), fetal size in this pregnancy and maternal choice.
RECOGNITION
Prolonged second stage Head comes down to introitus with pushing but retracts back between contractions Head Bobbing Delivered head retracts back into vagina - Turtle sign Delayed restitution of fetal head Gentle traction does not free the shoulder
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 2 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
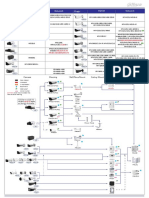
MANAGEMENT Flowchart for the management of shoulder dystocia is included below. This flowchart begins with simple measures and leads to more invasive manoeuvres. The order of these actions may differ according to clinical circumstances (e.g. experience of birth attendants, maternal ability to change position, existing or available analgesia/anaesthesia) Do not delay. Fetal hypoxia will worsen the longer the delay between the birth of the head and the birth of the body (approximate drop in blood pH of 0.04 per minute). Flowchart for the management of shoulder dystocia
CALL FOR HELP Midwifery help Obstetric help Neonatal team
Discourage pushing Avoid excess traction Prepare for newborn resus Prepare for PPH
MATERNAL RE-POSITIONING McRoberts Manoeuvre and/or All Fours position
SUPRAPUBIC PRESSURE Constant and/or rocking pressure on back of anterior fetal shoulder
INTERNAL MANOEUVRES (any order) Rotation of either shoulder into the oblique Delivery of posterior arm Axillary traction
Inform consultant obstetrician and anaesthetist
Consider: Cleidotomy Zavenelli manoeuvre Symphysiotomy
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 3 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
The flowchart is consistent with the H.E.L.P.E.R.R. mnemonic in Appendix 1, taught as part of the Advanced Life Support in Obstetrics (ALSO) course3 The aim of each of the actions in the flowchart is to: Increase functional size of bony pelvis Dislodge fetal shoulder due to pelvic movement Decrease fetal bisacromial diameter by adduction of shoulders Change relationship of bisacromial diameter with the bony pelvis (i.e rotate) Allow more space for internal manoeuvres to be performed Each action in the flowchart is described in more detail below: 1. Call for Help/Initial Actions Press emergency buzzer Request additional assistance for manoeuvres Prepare for neonatal resuscitation and PPH Discourage maternal pushing Avoid excessive traction on fetal head In secondary/ tertiary unit Fast page on 777 - neonatal team, obstetric team and anaesthetic team In primary unit Fast page on 777 - clinical co-ordinator (CCO) and/or obstetric team Dial 111 for ambulance and state Code One (lights and siren) 2. Maternal Re-positioning McRoberts' Manoeuvre (bed flat, buttocks to edge of bed and move knees towards shoulders) and/or
(Ref. Crofts et al.)
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 4 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
All fours position
(Ref. PROMPT manual) 3. Suprapubic Pressure Determine position of fetal back Place hands in CPR position Apply downward and lateral pressure to posterior aspect of anterior shoulder to displace shoulder from behind symphysis pubis and rotate into the oblique position Provide constant and/or rocking pressure
4.
Internal Manoeuvres (any order)(with Episiotomy if required)
Internal rotation 4&5 Insert fingers posteriorly Apply pressure to fetal shoulder(s) in order to rotate in a clockwise or anticlockwise direction
Delivery of posterior arm Insert fingers posteriorly, slide hand along fetal arm and bend it at the elbow. Sweep arm across chest and over face.
(Ref. Crofts et al)
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 5 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
Axillary Traction
1. Slide hand along fetal neck to shoulder
2. Grasp axilla with thumb and first finger
3. Apply axillary traction follow curve of sacrum (Photos used with permission of Lesley Ansell6)
5.
Further intervention
Cleidotomy Upward pressure with finger onto the babys clavicle to cause a fracture Zavanelli Manoeuvre Cephalic replacement followed by emergency caesarean delivery Flex fetal head to replace Acute tocolysis will be required
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 6 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
Symphysiotomy Used primarily in developing nations Local anaesthetic injected over symphysis Insert a Foley catheter Vaginal hand displaces urethra laterally Skin incision down to symphysis Scalpel blade to cut ligaments Assistant should support the pelvis on either side to prevent excessive traction Symphysis will then spread, allowing delivery.
POSTPARTUM CARE 1. 2. 3. 4. 5. Active management of 3rd stage. Thorough examination for perineal and cervical injury. Ensure adequate pain relief. Debrief the woman and her family/whanau and birth attendants. Ensure appropriate neonatal follow-up in accordance with neonatal handbook.
DOCUMENTATION
The shoulder dystocia documentation form (Ref: 6775 ) must be completed following the birth of the baby (see Appendix 2)
Complete and submit incident report form.
SUMMARY
Shoulder dystocia is a life-threatening situation Recognise risk factors and be alert at every birth Declare an emergency Stay calm and focussed Work through flowchart or mnemonic Record management and timing of events on procedural record
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 7 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
REFERENCES
1.
2. 3. 4. 5. 6.
Crofts, J., Draycott, T, Montague, I. Winter, C. & Fox, R. (2012) Royal College of Obstetricians & Gynaecologists (RCOG) Greentop Guideline 42 - Shoulder Dystocia; 2nd edition www.rcog.org.uk Baskett T. & Allen, A. (1995) Perinatal Implications of Shoulder Dystocia. Obstet Gynaecol; 86; 14-17 Gobbo E. & Baxley E. (2000) Shoulder Dystocia American Academy of Family Physicians Advanced Life Support in Obstetrics (ALSO), 4th Edition Rubin A. Management of shoulder dystocia. JAMA 1964; 189:835-7. Woods CE, Westbury NYA. Aprinciple of physics as applicable to shoulder delivery. Am J Obstet Gynecol 1943;45:796-804. Ansell (Irving), L., McAra-Couper, J. & Smythe, E. (2011) Shoulder Dystocia. A qualitative exploration of what works. Midwifery. Doi.: 10.1016/j.midw.2011.05.007
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 8 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
Appendix 1
Mnemonic for the management of shoulder dystocia
H E L P E R R mnemonic
H = Help (call for additional assistance) E = Evaluate for episotomy L = Legs (McRoberts manoeuvre) P = Pressure (Suprapubic) E = Enter (Internal manoeuvres) R = Remove (Posterior arm) R = Roll (to hands & knees) (A.L.S.O Advanced Life Support in obstetrics, 1996) Always call for help first Remaining HELPERR mnemonic can be followed in any order, using least invasive manoeuvres first
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 9 of 10
Issued: July 2012 Review: 2015
Canterbury DHB
Womens & Childrens Health
Appendix 2
Procedural Record
W&CH /GL/M/0011 Authorised by Maternity Guidelines Group
Page 10 of 10
Issued: July 2012 Review: 2015
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Power Tube Biasing Operation Manual 15-01-08Documento2 paginePower Tube Biasing Operation Manual 15-01-08MitchNessuna valutazione finora
- Astm C27Documento2 pagineAstm C27nee2790Nessuna valutazione finora
- YOKOGAWADocumento16 pagineYOKOGAWADavide ContiNessuna valutazione finora
- Celiac DiseaseDocumento14 pagineCeliac Diseaseapi-355698448100% (1)
- The Dedication of the Broken Hearted SailorDocumento492 pagineThe Dedication of the Broken Hearted SailorGabriele TorresNessuna valutazione finora
- Nakshatra Exaltation DebilitationDocumento3 pagineNakshatra Exaltation DebilitationBhanu Pinnamaneni100% (1)
- Coloi Eeml Disease: Original ArticlesDocumento67 pagineColoi Eeml Disease: Original ArticlesLuisAngelPonceTorresNessuna valutazione finora
- Dahua Pfa130 e Korisnicko Uputstvo EngleskiDocumento5 pagineDahua Pfa130 e Korisnicko Uputstvo EngleskiSaša CucakNessuna valutazione finora
- CE 581 Reinforced Concrete Structures: Lecture 4: Axial LoadingDocumento36 pagineCE 581 Reinforced Concrete Structures: Lecture 4: Axial LoadingCelil OrakNessuna valutazione finora
- Com Statement (HT APFC22 - 02)Documento2 pagineCom Statement (HT APFC22 - 02)SOUMENNessuna valutazione finora
- NASA Technical Mem Randum: E-Flutter N78Documento17 pagineNASA Technical Mem Randum: E-Flutter N78gfsdg dfgNessuna valutazione finora
- Physics SyllabusDocumento85 paginePhysics Syllabusalex demskoyNessuna valutazione finora
- Qand ADocumento5 pagineQand AJoshua PascasioNessuna valutazione finora
- Progressing Cavity Pump Overhaul GuideDocumento5 pagineProgressing Cavity Pump Overhaul Guidesdsds-54Nessuna valutazione finora
- AS 1418.2 Cranes, Hoists and Winches Part 2 Serial Hoists and WinchesDocumento31 pagineAS 1418.2 Cranes, Hoists and Winches Part 2 Serial Hoists and WinchesDuy PhướcNessuna valutazione finora
- Ericsson Microwave Outlook 2021Documento16 pagineEricsson Microwave Outlook 2021Ahmed HussainNessuna valutazione finora
- Hedging Techniques in Academic WritingDocumento11 pagineHedging Techniques in Academic WritingÛbř ÖňNessuna valutazione finora
- Kendriya vidyalaya reading comprehension and grammar questionsDocumento7 pagineKendriya vidyalaya reading comprehension and grammar questionsRaam sivaNessuna valutazione finora
- Poultry DiseasesDocumento5 paginePoultry DiseasesAnjum IslamNessuna valutazione finora
- BMW Mini COoper Installation InstructionsDocumento1 paginaBMW Mini COoper Installation InstructionsEdiJonNessuna valutazione finora
- Analysis of Financial Statements Project: GUL AHMAD Textile MillsDocumento32 pagineAnalysis of Financial Statements Project: GUL AHMAD Textile MillsHanzala AsifNessuna valutazione finora
- Semen RetentionDocumento3 pagineSemen RetentionMattNessuna valutazione finora
- SmartRunway SmartLandingDocumento39 pagineSmartRunway SmartLandingMikeNessuna valutazione finora
- DerbyCityCouncil Wizquiz Presentation PDFDocumento123 pagineDerbyCityCouncil Wizquiz Presentation PDFShubham NamdevNessuna valutazione finora
- 37th APSDC Scientific PresentationsDocumento7 pagine37th APSDC Scientific PresentationsSatyendra KumarNessuna valutazione finora
- Abundance BlocksDocumento1 paginaAbundance BlockssunnyNessuna valutazione finora
- Personality Types and Character TraitsDocumento5 paginePersonality Types and Character TraitspensleepeNessuna valutazione finora
- Radar PPNDocumento5 pagineRadar PPNSawaf MfNessuna valutazione finora
- 2 Profile OMORIS - Presentation 2020-2Documento20 pagine2 Profile OMORIS - Presentation 2020-2lemuel bacsaNessuna valutazione finora
- PDLAMMPS - made easy: An introductionDocumento8 paginePDLAMMPS - made easy: An introductionSaeed AbdNessuna valutazione finora