Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
First Bite Syndrome
Caricato da
nicdeepCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
First Bite Syndrome
Caricato da
nicdeepCopyright:
Formati disponibili
C 2012 The American Laryngological, V
The Laryngoscope
Rhinological and Otological Society, Inc.
First Bite Syndrome: Incidence, Risk Factors, Treatment, and Outcomes
Gary Linkov, BS; Luc G. T. Morris, MD; Jatin P. Shah, MD; Dennis H. Kraus, MD
Objectives/Hypothesis: First bite syndrome (FBS) refers to facial pain characterized by a severe cramping or spasm in the parotid region with the first bite of each meal that diminishes over the next several bites.1,2 It is a potential sequela of surgery involving the infratemporal fossa (ITF), parapharyngeal space (PPS), and/or deep lobe of the parotid gland. The incidence, risk factors, treatment options, and outcomes of FBS are poorly understood. We hypothesized that certain clinical and tumor variables independently predict the development of FBS. Study Design: Retrospective cohort study. Methods: We reviewed the records of 499 patients (mean age, 50 years; range, 1281 years) undergoing surgery of the deep lobe of the parotid gland, PPS, and/or ITF between 1992 and 2010. Minimum follow-up time was 3 months (median, 39 months). Patient, tumor, and FBS characteristics were analyzed. Incidence was calculated using the KaplanMeier method. Univariate analyses and multivariate logistic regression were used to identify independent risk factors for FBS. Patients developing FBS were interviewed to assess the efficacy of various treatment modalities. Results: FBS developed in 45 patients (incidence, 9.6%), at a mean time of 97 (range, 6877) days from surgery. On multivariate analysis, three variables were significant independent risk factors for FBS: sympathetic chain sacrifice (odds ratio [OR], 4.7; P .008), PPS dissection (OR, 8.7; P .001), and resection of only the deep lobe of the parotid gland (OR, 4.2; P .002). FBS developed in 48.6% of patients undergoing sympathetic chain sacrifice, 22.4% of patients undergoing PPS dissection, 38.4% of patients undergoing isolated deep lobe parotid resection, and 0.8% of patients undergoing total parotidectomy. Partial resolution of FBS symptoms occurred in 69% and complete resolution in 12%. Of 45 FBS patients, 15 (33%) underwent at least one type of treatment for symptomatic relief. No treatment consistently provided effective symptomatic relief. Conclusions: The strongest independent risk factors for FBS are PPS dissection, deep lobe of parotid resection, and sympathetic chain sacrifice. Patients undergoing surgery with dissection and/or manipulation in these anatomical sites and structures should be thoroughly counseled about the risk of developing FBS. Key Words: First bite syndrome, parapharyngeal space, infratemporal fossa, pain, parotid. Level of Evidence: 2c Laryngoscope, 122:17731778, 2012
INTRODUCTION
First bite syndrome (FBS) refers to facial pain characterized by a severe cramping or spasm in the parotid region with the first bite of each meal that diminishes over the next several bites. It is a potential sequela of surgery involving the infratemporal fossa (ITF), parapharyngeal space (PPS), and/or deep lobe of the parotid gland. The constellation of symptoms varies from transient and mild to persistent and severe.14 The anatomic location most frequently associated with the development of postoperative FBS is the parapharyngeal space, and the mechanism is believed to be a loss of sympa-
thetic innervation to the parotid gland.1,5 The incidence of FBS after head and neck surgery remains unknown. In addition, although the resection of certain structures, such as the sympathetic chain, during surgery has been speculated to be linked with FBS,1,4,5 the factors associated with FBS remain poorly characterized. We hypothesized that certain clinical and tumor variables would independently predict the development of FBS. Our objective was to define the incidence, potential risk factors, treatment, and outcomes of FBS following head and neck surgery.
MATERIALS AND METHODS
From the Head and Neck Service, Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, New York, U.S.A. Editors Note: This Manuscript was accepted for publication March 28, 2012. An oral presentation of this article was given at the 2012 meeting of the North American Skull Base Society, Las Vegas, Nevada, U.S.A., February 18, 2012. The authors have no funding, financial relationships, or conflicts of interest to disclose. Send correspondence to Luc G. T. Morris, MD, MSc, 1275 York Ave #S-1210A, New York, NY, 10065. E-mail: morrisl@mskcc.org DOI: 10.1002/lary.23372
The records of 499 patients undergoing surgery in any of three anatomic locations between 1992 and 2010 at Memorial Sloan-Kettering Cancer Center (MSKCC) were analyzed. Following institutional review board approval, we conducted a comprehensive search of operative reports and pathologic reports to identify candidate cases of surgery involving the deep lobe of the parotid gland, PPS, and ITF. These anatomic sites were chosen to capture patients at risk of developing FBS based on the current literature and mechanistic understanding of this condition. Patients with exposure to radiation of the head or neck before the operation, for any reason, were included. Both benign and malignant tumors were included. Exclusion criteria
Laryngoscope 122: August 2012
Linkov et al.: First Bite Syndrome
1773
TABLE 1. Patient Characteristics and FBS Incidence.
Characteristic No. (%) Incidence (%) P
Total Sex Male Female Prior RT Yes No Age, y Mean <45 45-58 59-69 70-91 Diabetes Yes No Neuropathy Yes No PVD Yes No Psychiatric History Yes No Anxiety Yes No FN Fully Intact Yes No FN Grade Preop Mean 1-3 4-6 Horners Syndrome Preop Yes No FBS Preop Yes No TMJ Pain Preop Yes No Preop
499 (100) 261(52) 238 (48) 47(9) 452 (91) 56 (2-91) 124 (25) 125 (25) 125 (25) 125 (25) 40 (8) 459 (92) 28 (6) 471 (94) 4 (1) 495 (99) 64 (13) 435 (87) 30 (47) 34 (53) 454 (91) 45 (9) 1.2 478 (96) 21 (4) 4 (1) 495 (99) 0 499 (100) 12 (2) 487 (98)
45 (9) 14 (5) 31 (13) 0 45 (10) 0.003
0.023
details of radiotherapy were recorded. Operative reports were reviewed with a particular focus on dissection in the sites of interest and ligation and/or resection of pertinent vascular and/or nervous structures. The integrity of the sympathetic chain, external carotid artery, and its branches was recorded. Postoperative findings such as facial nerve palsy, Horner syndrome, temporomandibular joint pain, and FBS were recorded. In patients developing FBS, time of onset, treatment, and outcome at last follow-up visit were recorded. Patients who developed FBS, and for whom current contact information was available, were individually interviewed by telephone with a structured questionnaire.
15 (12) 15 (12) 9 (7) 6 (5) 1 (3) 44 (10) 5 (18) 40 (8) 0 45 (9) 11 (17) 34 (8) 7 (23) 4 (12) 44 (10) 1 (2)
0.112
Characteristic
TABLE 2. Tumor Characteristics and FBS Incidence.
No. (%) Incidence (%) p
0.133
Side Right Left Site of Origin PPS ITF Parotid Portion of Parotid Deep Superficial Both Intraparotid Node Status Positive Negative Other Site of interest Path Site of interest Path
233 (47) 266 (53) 73 (15) 14 (3) 257 (52) 122 (47) 7 (3) 128 (50) 28 (11) 229 (89) 155 (31) 114 (74) 41 (26) 28 (6) 41 (8) 100 (20) 330 (66) 482 (97) 17 (3) 217 (44) 265 (53) 3.5 (0.513.4) 89 (18) 90 (18) 90 (18) 91 (18) 139 (28) 145 (29) 69 (14)
19 (8) 26 (10) 20 (27) 0 25 (10) 23 (19) 0 2 (2) 0 25 (11) 0 0 0 10 (36) 9 (22) 20 (20) 6 (2) 45 (9) 0 43 (20) 2 (1)
0.529
0.093
<0.001
0.527
<0.001
0.015
0.066
0.221
N/A
0.095
Histology
Schwannoma Paraganglioma 0.140 Pleomorphic Adenoma Other Presence of Tumor Yes No Tumor Type Benign Malignant Size, cm Mean 2 2.13.1 3.24.5 4.53.4 Margins Positive Negative Close (<5mm)
<0.001
45 (9) 0 0 45 (9) 0 45 (9) 1 (8) 44 (9)
0.527
0.187
N/A
<0.001
0.933
5 (6) 6 (7) 10 (11) 11 (12) 12 (9) 12 (8) 4 (6)
0.331
Abbreviations: FBS, first bite syndrome; RT, radiation; PVD, peripheral vascular disease; FN, facial nerve; TMJ, temporomandibular joint; N/A, not available.
included previous surgery in these anatomic sites prior to referral to MSKCC, procedures limited to biopsy, and postoperative follow-up of <3 months. Patient factors, presenting symptoms, aspects of medical history, details of the operative procedure, pathology, and
0.760
Abbreviations: FBS, first bite syndrome; PPS, parapharyngeal space; ITF, infratemporal fossa; Path, pathology; N/A, not available.
Laryngoscope 122: August 2012
Linkov et al.: First Bite Syndrome
1774
The cumulative incidence of FBS was calculated using the KaplanMeier method, censoring patients at the time of last follow-up. Univariate analysis of patient, treatment, and tumor covariates and FBS incidence was carried out using the chisquared statistic and the log-rank test, with significance defined a priori as P < .05. Significant covariates were then entered into a multivariate logistic regression model, ensuring that the omnibus test of model coefficients was significant (P < .001). All statistical analysis was performed using SPSS version 19.0 (SPSS Inc., Chicago, IL).
TABLE 3. Surgical Details and FBS Incidence.
Detail No. (%) Incidence (%) p
Approach Transparotid Transcervical Anterior Mandibulotomy Yes No ITF Dissection Yes No PPS Dissection Yes No PPS Site Pre-styloid Post-styloid Sympathetic Chain Sac Yes No IJV Sac Yes No ECA Ligation Yes No Deep Parotid Resected Yes No Superficial Parotid Resected Yes No Total Parotid Resected Yes No Gross Total Resection Yes No 489 (98) 10 (2) 45 (9) 0 0.315 149 (30) 350 (70) 1 (1) 44 (13) <0.001 290 (58) 209 (42) 4 (1) 41 (20) <0.001 344 (69) 155 (31) 25 (7) 20 (13) 0.042 38 (8) 461 (92) 6 (16) 39 (9) 0.129 34 (7) 465 (93) 0 45 (10) 0.057 21 (4) 478 (96) 9 (43) 36 (8) <0.001 113 (56) 62 (31) 22 (19) 17 (27) 0.227 201 (40) 298 (60) 42 (21) 3 (1) <0.001 110 (22) 389 (78) 2 (2) 43 (11) 0.003 26 (5) 473 (95) 2 (8) 43 (10) 0.808 326 (65) 101 (20) 72 (14) 26 (8) 19 (19) 0 <0.001
RESULTS
Of the 499 patients, 45 (9.6%) developed FBS. The mean age at FBS onset was 50 years (range, 1281 years), with a mean interval since surgery of 97 days (range, 6877 months; median, 54 months). Average follow-up time was 39 months (range, 3224 months) for all patients and 40 months (range, 3149 months) for FBS patients. Patient characteristics and FBS incidence are summarized in Table I. The mean age of all patients in the study was 56 years (range, 291 years). On univariate analysis, patient factors significantly associated with the development of FBS were female gender (odds ratio [OR], 2.6; 95% confidence interval [CI], 1.45.1; P .003), absence of prior radiation (OR $ P .023), and history of psychiatric illness (OR, 2.4; 95% CI, 1.2 5.1; P .015). Forty-seven patients had a prior history of radiation to the head or neck (9%), none of whom developed FBS. Tumor characteristics and FBS incidence are summarized in Table II. Tumor factors significantly associated with the development of FBS on univariate analysis were parotid site of origin (OR, 14.8; 95% CI, 3.464; P < .001), schwannoma (OR, 6.9; 95% CI, 3.016; P < .001), and benign histology (OR, 33; 95% CI, 7.8 140; P < .001). Patients with tumors arising in the PPS and parotid gland accounted for all cases of FBS; no cases were observed in patients with tumors arising in the ITF or other sites. The majority of parotid FBS cases (92%) were associated with tumors limited to the deep lobe. Most FBS cases (87%) were associated with three histological classes: schwannoma (10; 22%), paraganglioma (nine; 20%), or pleomorphic adenoma (20; 44%). Of 265 patients with resection of a malignant tumor, only two developed FBS (0.8%). Surgical details and FBS incidence are summarized in Table III. Surgical factors significantly associated with the development of FBS were transcervical approach (OR, 3.3; 95% CI, 1.86.3; P < .001), ITF dissection (OR, 0.15; 95% CI, 0.040.63; P .003), PPS dissection (OR, 26; 95% CI, 7.985; P < .001), sympathetic chain sacrifice (OR, 9.2; 95% CI, 3.623; P < .001), resection involving the deep lobe of the parotid gland (OR, 0.53; 95% CI, 0.280.98; P .042), resection involving the superficial lobe of the parotid gland (OR, 0.06; 95% CI, 0.020.16; P < .001), and total parotid gland resection (OR, 0.05; 95% CI, 0.0060.34; P < .001). Postoperative findings are summarized in Table IV. Postoperative factors significantly associated with FBS were Horner syndrome (OR, 12; 95% CI, 4.629; P < .001), temporomandibular joint pain (OR, 6.2; 95% CI, Laryngoscope 122: August 2012
Abbreviations: FBS, first bite syndrome; PPS, parapharyngeal space; ITF, infratemporal fossa; IJV, internal jugular vein; ECA, external carotid artery.
1.822; P .001), facial nerve grades 1 to 3 (OR, 8.3; 95% CI, 2.035; P .001), and adjuvant radiotherapy (OR, 0.06; 95% CI, 0.010.23; P < .001). Of 211 patients receiving adjuvant radiotherapy, only two developed FBS (1%). Multivariate analysis was performed to identify variables independently associated with the development of FBS; results are detailed in Table V. The statistically significant factors were sympathetic chain sacrifice (OR, 4.7; 95% CI, 1.515; P .008), PPS dissection (OR, 8.7; 95% CI, 2.530; P .001), and extent of parotidectomy (resection of only deep lobe of parotid gland: OR, 40; Linkov et al.: First Bite Syndrome
1775
TABLE 4. Postoperative Findings and FBS Incidence.
Finding No. (%) Incidence (%) p Variable
TABLE 5. Multivariate Analysis of Factors Associated with the Development of FBS.
No. (%) Incidence (%) OR (95% CI) p
FBS Mean Age at Onset, y 50 (12-81) Average Interval Since Surgery, d 97 Range Interval Since Surgery, d 6-877 FBS Treatment Received Yes No FBS Improved Yes No Horners Syndrome Yes No TMJ Pain Yes No FN Fully Intact Yes No FN Grade Mean 1-3 4-6 Adjuvant RT Yes No Follow Up Time (All Patients), m Mean Follow Up Time (FBS Patients), m Mean 40 (3-149) 2.5 371 (74) 128 (26) 211 (42) 288 (58) 39 (3-224) 43 (12) 2 (2) 2 (1) 43 (15) <0.001 0.001 206 (41) 293 (59) 23 (11) 22 (8) 0.160 11(2) 488 (98) 4 (36) 41 (8) 0.001 21 (4) 478 (96) 10 (48) 35 (7) <0.001 31 (69) 14 (31) 15 (33) 30 (67)
Gender Male Female Prior RT Yes No Psychiatric History Yes No ECA Ligation Yes 261(52) 14 (5) Ref 1.2 (0.56-2.7) 0.596 Ref 5.4E7 (0) 0.997 238 (48) 31 (13) 47 (9) 0
452 (91) 45 (10) 64 (13) 11 (17) 435 (87) 38 (8) 34 (8) 6 (16) 39 (9) 9 (43) 36 (8)
1.9 (0.76-4.7) 0.169 Ref 1.7 (0.50-5.5) 0.412 Ref 4.7 (1.5-15) Ref 8.7 (2.5-30) Ref 1.4 (0.36-5.3) 0.633 Ref 9.5 (1.2-78) 0.036 1.0 0.001 0.001 0.008
No 461 (92) Sympathetic Chain Sac Yes No PPS Dissection Yes No Neuropathy Yes No Parotid Resected No Superficial Lobe Only Deep Lobe Only Subtotal Total 21 (4) 478 (96)
201 (40) 42 (21) 298 (60) 28 (6) 471 (94) 3 (1) 5 (18) 40 (8)
153 (31) 20 (13)
2 (.4) 0 0 56 (11) 21 (38) 40 (4.9-317) 139 (28) 149 (30) 3 (2) 1 (1) Ref
3.7 (0.37-37) 0.266
Abbreviations: FBS, first bite syndrome; RT, radiotherapy; ECA, external carotid artery; Sac, sacrifice; PPS, parapharyngeal space.
Abbreviations: FBS, first bite syndrome; TMJ, temporomandibular joint; FN, facial nerve; RT, radiotherapy.
95% CI, 4.9320; P .001; no parotidectomy performed: OR, 9.5; 95% CI, 1.278; P .036). The cumulative incidence of FBS, calculated using the KaplanMeier method, was 9.6%. In patients undergoing sympathetic chain sacrifice, the incidence was 48.6% (P < .001); in patients undergoing PPS dissection, the incidence was 22.4% (P < .001). Whereas patients undergoing only deep lobe of parotid gland resection had a 38.4% incidence of FBS, those undergoing total parotidectomy had an FBS incidence of 0.8% (P < .001). These findings are presented in Figure 1. Patients who received radiation either before or after definitive surgery had a 0.9% incidence of FBS, whereas patients who never received radiation to the head or neck had a 17.5% incidence of FBS (P < .001). At last follow-up, FBS symptoms improved in 69% of patients (31 of 45). Fifteen patients with FBS (33%) received at least one form of treatment, including an analgesic (n 9), an opioid (n 5), a neuropathic pain medication (n 10), acupuncture (n 1), and/or a Botox injection (n 1). Laryngoscope 122: August 2012
Structured telephone interview results are shown in Table VI. After attempting to reach every patient identified with FBS, 16 of 45 were ultimately interviewed. Fourteen patients (88%) reported persistent FBS at time of interview; only two patients (12%) reported
Fig. 1. Incidence of first bite syndrome (FBS) for risk factors independently significant on multivariate analysis. OR odds ratio.
Linkov et al.: First Bite Syndrome
1776
TABLE 6. Results of FBS Phone Questionnaire (n516) and Consent Data.
Item No. (%)
Symptoms Present at Interview Average Intensity of Symptoms (110) Quality of Symptoms Worse with sour food Worse after long food breaks Sharp, shooting pain Treated for FBS Eating Behavior Modified Because of FBS Type of Behavior Modification Mentally Prepare/Close Eyes Chew on Other Side Clench Fist/Bang Foot Small Bites of Food Rub Parotid Area Avoid Sour Foods Recall being told preoperatively about risk of FBS Would Have Liked to Know About FBS Before Surgery If you knew about the risk of FBS, would you have reconsidered having surgery? Yes No Consent Data (n 45)
14 (88) 5.7 7 (44) 6 (38) 4 (25) 5 (31) 12 (75) 3 3 2 2 2 2 2 (13) 9 (56)
clenching fist/banging foot (n 2), taking small bites of food (n 2), rubbing the parotid area with onset of pain (n 2), and avoiding sour foods (n 2). Only two patients recalled being counseled preoperatively on the risk of developing FBS. However, no patient indicated he or she would have declined surgery, had he or she known FBS would develop. Preoperative consent discussions from all 45 FBS patients were reviewed for mention of FBS. Whereas only 3 patients were explicitly told of the risk of developing FBS, 17 were told of the potential for developing dysfunction of swallowing.
DISCUSSION
Our study goals were to identify the incidence, risk factors, treatment, and outcomes of FBS. We identified a comprehensive cohort of patients undergoing surgical procedures in anatomic locations associated with the development of FBS. These locations were the PPS, ITF (containing the middle meningeal artery), and deep lobe of the parotid gland. Of 499 patients, 45 developed FBS postoperatively, for a cumulative incidence of 9.6%. The incidence of FBS was particularly high in patients undergoing PPS dissection (22.4%), resection of only the deep lobe of the parotid gland (38.4%), and sacrifice of the sympathetic chain (48.6%). These three variables were significant independent predictors of FBS on multivariate analysis. The term first bite syndrome was used in 1998 by Netterville et al., referring to facial pain characterized by a severe cramping or spasm in the parotid region with the first bite of each meal that diminishes over the next several bites. FBS was initially attributed to sympathetic denervation. In a case series of 46 patients with vagal paraganglioma, the authors proposed a mechanism of loss of sympathetic innervation to the parotid gland causing a denervation supersensitivity that was activated by parasympathetic neurotransmitters, particularly during initial oral intake. Parasympathetic hyperactivation is speculated to stimulate an exaggerated myoepithelial cell contraction throughout the parotid gland, causing pain. In support of this mechanism, eight of the nine FBS cases in the Netterville et al. series underwent sympathetic trunk resection, and the other patient exhibited sympathetic dysfunction postoperatively as manifested by Horner syndrome.1,2,4
0 16 (100) 17 (38) 3 (7)
Told of potential for dysfunction of speech and swallowing Told of potential for first bite syndrome
Abbreviation: FBS, first bite syndrome.
complete resolution of symptoms. On a pain scale from 1 to 10, with 1 indicating occasional low-grade pain and 10 representing severe, constant pain with every meal, the average intensity of symptoms was 5.7 (range, 1 10). Patients described the pain as sharp, shooting (four patients), worse with sour foods (seven patients), and worse after long breaks between meals (six patients). Five patients (31%) received some form of treatment, with variable efficacy. Twelve patients (75%) reported modifying their eating behavior to adjust to FBS. Adaptive strategies included mentally preparing/closing the eyes (n 3), chewing on the unaffected side (n 3),
TABLE 7. Summary of Literature Reported Case Series with FBS Development (min. >1 case).
FBS Cases (% incidence of FBS) For FBS Cases (% of total FBS cases) PPS involvement Sympathetic Chain Sacrifice ECA Ligation
Study
Site(s) Assessed
Total Cases
Linkov et al. 2011 Chijiwa et al. 2009 Kawashima 2008 Chiu et al. 2002 Netterville et al. 1998
ITF, PPS, DP PPS PPS PPS PPS
499 24 22 12 46
45 (9.6) 7 (29) 9 (41) 12 (100) 9 (20)
42 (93) 7 (100) 9 (100) 12 (100) 9 (100)
9 (20) N/A 5 (56) 5 (42) 8 (89)
6 (13) N/A 6 (67) 6 (50) N/A
Abbreviations: FBS, first bite syndrome; ITF, infratemporal fossa; PPS, parapharyngeal space; DP, deep lobe of parotid; ECA, external carotid artery; N/ A, not available.
Laryngoscope 122: August 2012
Linkov et al.: First Bite Syndrome
1777
Other case series have supported the role of sympathetic denervation in the development of FBS. In 2002, Chiu et al. published a series of 12 patients with FBS after surgery involving the PPS. Only six patients had their sympathetic chain transected and/or exhibited Horner syndrome postoperatively. The remaining six patients had undergone ligation of their external carotid artery (ECA). The authors revisited salivary gland physiology and anatomy to explain that all 12 patients likely experienced a loss of sympathetic innervation to the parotid gland, supporting the initial theory by Netterville et al.4 In 2008, Kawashima et al. reviewed 22 patients with PPS tumors and identified nine cases of FBS, eight of which involved surgical ablation of the cervical sympathetic chain and/or ECA.5 Further adding support to the sympathetic denervation hypothesis, there have recently been several reports of patients exhibiting FBS preoperatively due to tumor invasion of the sympathetic chain and/or ECA.79 A summary of the published case series (involving >1 case per study) with FBS development, including the results of the present study, can be found in Table VII. In the three small case series assessing only PPS tumors, the incidence of FBS ranges from 20% to 41%.1,5,6 Our results fall within this range for PPS dissection and deep parotid lobe resection, but point to a higher incidence when the sympathetic trunk is resected. In addition to the three variables found to be significant independent predictors of FBS on multivariate analysis (PPS dissection, deep parotid lobe resection, and sympathetic trunk ablation), several other notable variables associated with FBS were identified via univariate analysis. An inverse relationship was noted between receiving radiation therapy to the head and/or neck before or after surgery and developing FBS. It is unclear whether the actual radiation leads to a reduction in FBS incidence (perhaps due to a reduction in functioning parotid gland myoepithelial cells) or if the phenomenon is a byproduct of other related variables, such as more benign disease in the nonradiated group. Another variable of interest is the complete resection of the parotid gland. In the present study, only one case of FBS occurred when a total parotidectomy was performed. Because the pain in FBS is likely generated by enhanced contractility of the myoepithelial cells in parotid tissue,4 it is expected that removal of all ipsilateral parotid tissue would eliminate FBS. This one
unusual case may have been associated with inadvertently retained, or ectopically present, parotid tissue. It appears that preservation of the superficial lobe when performing an isolated deep lobe parotidectomy increases the risk of developing FBS. Several treatment strategies were attempted for some of the patients with FBS, including pain medications, acupuncture, and Botox injections. Most patients with and without treatment improved over time; however, few experienced a complete resolution of symptoms. Although a thorough assessment of the effects of specific treatment types on symptomatology was not performed, there did not appear to be a consistently effective treatment option. As gleaned from telephone interviews, patients had tried various combinations of treatments, including medicinal, procedural, and adaptive behavioral techniques, to help cope with FBS.
CONCLUSION
Head and neck surgeons planning to operate in the PPS or to resect the deep lobe of the parotid should be aware of the potential consequence of FBS and should counsel their patients on its risk and anticipated outcome.
BIBLIOGRAPHY
1. Netterville JL, Jackson CG, Miller FR, Wanamaker JR, Glasscock ME. Vagal paraganglioma: a review of 46 patients treated during a 20-year period. Arch Otolaryngol Head Neck Surg 1998;124:11331140. 2. Netterville JL, Jackson CG, Wanamaker JR, Miller FR, Glasscock ME.Vagal paraganglioma: a review of 44 patients treated over 18 years. Presented at the 40th Annual Meeting of American Society for Head and Neck Surgery/Society of Head and Neck Surgeons at Combined Otolaryngology Spring Meetings; Palm Beach, Florida, U.S.A.; May 1416, 1998. 3. Haubrich WS. The first-bite syndrome. Henry Ford Hosp Med J 1986;34: 275278. 4. Chiu AG, Cohen JI, Burningham AR, Andersen PE, Davidson BJ. First bite syndrome: a complication of surgery involving the parapharyngeal space. Head Neck 2002;24:996999. 5. Kawashima Y, Sumi T, Sugimoto T, Kishimoto S. First-bite syndrome: a review of 29 patients with parapharyngeal space tumor. Auris Nasus Larynx 2008;35:109113. 6. Chijiwa H, Mihoki T, Shin B, Sakamoto K, Umeno H, Nakashima T. Clinical study of parapharyngeal space tumours. J Laryngol Otol 2009; 123(suppl 31):100103. 7. Lieberman SM, Har-El G. First bite syndrome as a presenting symptom of a parapharyngeal space malignancy. Head Neck 2011;33:15391541. 8. Deganello A, Meccariello G, Busoni M, Franchi A, Gallo O. First bite syndrome as presenting symptom of parapharyngeal adenoid cystic carcinoma. J Laryngol Otol 2011;125:428431. 9. Diercks GR, Rosow DE, Prasad M, Kuhel WI. A case of preoperative firstbite syndrome associated with mucoepidermoid carcinoma of the parotid gland. Laryngoscope 2011;121:760762.
Laryngoscope 122: August 2012
Linkov et al.: First Bite Syndrome
1778
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Print - Ectopic Pregnancy - 10min TalkDocumento2 paginePrint - Ectopic Pregnancy - 10min TalknicdeepNessuna valutazione finora
- BRCA1/BRCA2 Genes: Account For 10%Documento2 pagineBRCA1/BRCA2 Genes: Account For 10%nicdeepNessuna valutazione finora
- Overview of Pediatric GeneticsDocumento12 pagineOverview of Pediatric Geneticsnicdeep100% (1)
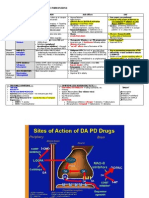
- Pharmacologic TX For Idiopathic Parkinsons: Strategy Class / Drug MOA Side Effects USEDocumento2 paginePharmacologic TX For Idiopathic Parkinsons: Strategy Class / Drug MOA Side Effects USEnicdeepNessuna valutazione finora
- LSU Peds ReviewDocumento27 pagineLSU Peds Reviewnicdeep100% (2)
- PBL - Myasthenia GravisDocumento2 paginePBL - Myasthenia Gravisnicdeep100% (1)
- Neurocutanous SyndromesDocumento3 pagineNeurocutanous SyndromesnicdeepNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- WaterDocumento26 pagineWaterKisna Bhurtel100% (1)
- Reflexology and DementiaDocumento8 pagineReflexology and DementiaNatalie Stubbs100% (1)
- Types of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDocumento4 pagineTypes of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDaisy MellaNessuna valutazione finora
- Case Studies On DisordersDocumento5 pagineCase Studies On DisordersAshwin Hemant LawanghareNessuna valutazione finora
- Ofra Ayalon Healing Trauma With Metaphoric Cards PDFDocumento3 pagineOfra Ayalon Healing Trauma With Metaphoric Cards PDFKrisztina MkNessuna valutazione finora
- Peter Pan Syndrome Is A DeepDocumento3 paginePeter Pan Syndrome Is A DeeptucklertNessuna valutazione finora
- CPR and First Aid PowerpointDocumento21 pagineCPR and First Aid PowerpointZawawiIbnuRosyidNessuna valutazione finora
- B PharmacyDocumento26 pagineB PharmacyAkankshaNessuna valutazione finora
- NeutrophilDocumento61 pagineNeutrophilJenivic Empig PuedanNessuna valutazione finora
- ILS 2014 Final Year Revision LectureDocumento54 pagineILS 2014 Final Year Revision LectureokaberntrNessuna valutazione finora
- Dengue Hemorrhagic FeverDocumento86 pagineDengue Hemorrhagic FeverBryan EspanolNessuna valutazione finora
- Sinew Channels by J Yuen002Documento81 pagineSinew Channels by J Yuen002Jonathan100% (1)
- MastitisDocumento27 pagineMastitisLaprida RecoletaNessuna valutazione finora
- Cayman Islands National Youth Policy September 2000Documento111 pagineCayman Islands National Youth Policy September 2000Kyler GreenwayNessuna valutazione finora
- Theta EnergeticsDocumento37 pagineTheta Energeticsghandhi4351100% (4)
- Daftar PustakaDocumento3 pagineDaftar PustakaEKANessuna valutazione finora
- Test Bank For Counseling and Psychotherapy Theories in Context and Practice Skills Strategies and Techniques 3rd Edition John Sommers Flanagan Rita Sommers FlanaganDocumento17 pagineTest Bank For Counseling and Psychotherapy Theories in Context and Practice Skills Strategies and Techniques 3rd Edition John Sommers Flanagan Rita Sommers Flanagancuthbertfinncx2nNessuna valutazione finora
- Chapter 4 A1 Poster Example 2Documento3 pagineChapter 4 A1 Poster Example 2Krisna PamungkasNessuna valutazione finora
- Single DentureDocumento37 pagineSingle DentureDentist Dina SamyNessuna valutazione finora
- Operation Maintenance of EtpDocumento1 paginaOperation Maintenance of Etpaminur rahamanNessuna valutazione finora
- Study Guide - SAPCDocumento7 pagineStudy Guide - SAPCSudhakar KuppireddyNessuna valutazione finora
- PancreatitisDocumento28 paginePancreatitisIndri Chernovita TurnipNessuna valutazione finora
- 02-HK Products AllDocumento154 pagine02-HK Products AllHari SetiawanNessuna valutazione finora
- Wound Care DescriptionDocumento4 pagineWound Care DescriptionRodriguez, Joyce Ann G.Nessuna valutazione finora
- Acute Pain NCPDocumento2 pagineAcute Pain NCPfaye-pamatmat-257080% (5)
- Hypoxic Ischemic Hypoxic Ischemic E HL H E HL H Encephalopathty EncephalopathtyDocumento34 pagineHypoxic Ischemic Hypoxic Ischemic E HL H E HL H Encephalopathty EncephalopathtyKatrinaTandoc100% (1)
- ENLS V4.0 ME Manuscript FINALDocumento17 pagineENLS V4.0 ME Manuscript FINALkoko komarudinNessuna valutazione finora
- Wastewater Characterization1Documento39 pagineWastewater Characterization1ksbbs100% (1)
- ASD Interventions Theories, Age Range and SettingsDocumento4 pagineASD Interventions Theories, Age Range and SettingstracycwNessuna valutazione finora
- FMRI Obs Icu & HduDocumento13 pagineFMRI Obs Icu & HduApoorv JainNessuna valutazione finora