Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Sodium Disorders
Caricato da
andrea_manzioneDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Sodium Disorders
Caricato da
andrea_manzioneCopyright:
Formati disponibili
Sodium Disorders
Stephen Sigworth, MD, MSHA General Internists are often called to consult on sodium disorders in hospitalized patients. Due to its multiple etiologies, a systematic approach is best in evaluating sodium imbalance. This chapter will address both hypernatremia and hyponatremia and offer diagnostic tools to determine the etiology, and discuss treatment modalities to return the patient to a eunatremic state. Hypernatremia Hypernatremia is defined as serum sodium levels greater than 145 mmol/L.1 Hypernatremia is primarily a water deficit in relation to intravascular sodium levels. Individuals with either a thirstimpairment or in a setting that may limit access to fluids are at risk of becoming hypernatremic. Typically, patients with mild hypernatremia may have weakness, lethargy, insomnia or hyperpnea. Those with more extreme levels of hypernatremia exhibit CNS related symptoms due to the intracellular water loss of brain cells, and subsequently have altered mental status, seizures or become comatose. Hypernatremia typically results from three different mechanisms. The first is extrarenal water loss through the skin (excessive sweating, extensive burns), gastrointestinal tract (diarrhea, vomiting, chronic nasogastric suctioning) or lungs (tachypnea). The second mechanism is diuresis due to osmotic and nonosmotic causes. The major osmotic causes include diuretic use, hyperglycemia, uremia, mannitol or a post-obstructive diuresis. The major cause of nonosmotic diuresis is diabetes insipidus. This can originate centrally or from the kidneys. Central diabetes insipidus can result from recent trauma or neurosurgery, tuberculosis, sarcoidosis, meningitis, cerebral aneurysms, encephalitis or Guillain-Barre Syndrome. Nephrogenic diabetes insipidus can result from intrinsic renal disease, hypercalcemia, hypokalemia, or drugs such as lithium, democlocycline, amphotericin B or vasopressin. The third mechanism is sodium overload. This can happen from parenteral infusion of sodium bicarbonate or hypertonic saline, exogenous sodium ingestion, hypertonic dialysis, primary hyperaldosteronism or Cushings Syndrome
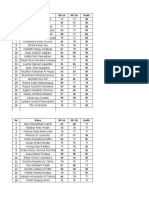
Treatment The method of sodium correction is under debate, but all recommend slow correction over the first 24 hours. Correcting the imbalance too rapidly can result in cerebral edema, which can lead to death. In either case, water replacement is the mainstay of treatment. If the patient has a workable gastrointestinal tract and is able to take water by mouth or via other enteral device, providing free water is the ideal replacement modality. If the patient can only receive parenteral therapy, then a hypotonic solution should be used. In most cases, correcting water deficits are best done with hypotonic saline or D5W (5% dextrose in water). Isotonic saline should only be used if intravascular resuscitation is immediately required to maintain blood pressure. Once the patient is stabilized, the fluid should be switched to one that is hypotonic. One method for safer resolution of hypernatremia can be achieved by decreasing serum sodium levels by 10 mmol/L per day. By using the following formula, the effect of a change in serum sodium with one liter of infusate is calculated, then extrapolated to how many liters are required to achieve a net change of 10 mmol/L. Change in = Serum Na Infusate Na = Infusate Na Serum Na of patient Total body water + 1 0 34 77 154 D5W 0.2% NaCl in D5W 0.45% NaCl in H20 0.9% NaCl in H20
Total Body Water = 0.6 x weight (kg) for males 0.5 x weight (kg) for females 0.5 x weight (kg) for elderly males 0.45 x weight (kg) for elderly females Another method is to calculate the water deficit of the patient (see below), then replace half the water deficit over the first 24 hours, with the remainder replaced over the subsequent one to two days Calculated Water Deficit (L) = 0.6 x (weight in kg) x [(Plasma Na / 140) 1)] Whichever method you choose, be careful to not correct too rapidly due to severe neurological complications or death. Hyponatremia Hyponatremia is a more common consultative problem for the General Internist. It is defined as a
47
serum sodium level less than 136 mmol/L and often results from excess water intake in relation to water excretion.2 The most frequent causes of hyponatremia in hospitalized patients are thiazide use, the post-operative setting and SIADH. Psychiatric patients may exhibit excessive polydipsia as the primary etiology. Importantly, hyponatremia may occur in any volemic state. Mild cases are associated with headache, nausea, lethargy and confusion. Severe cases involve seizures, coma, brainstem herniation and death, which results from cerebral edema as water travels into brain cells. Typically, symptoms become more prominent when sodium levels fall below 125 mmol/L. There are two important laboratory tests to order when evaluating hyponatremia. The first is serum osmolarity, which denotes intravascular tonicity. The second is the urine sodium (can be obtained from a random urine sample), which illustrates the ability of the kidney to retain water and concentrate urinary solutes. In hyperosmotic (>285 mOsm) hyponatremia, an extracellular shift of water occurs secondary to high solute concentrations in the vascular space. The most common etiology is hyperglycemia, or the exogenous infusion of hypertonic solutions such as mannitol. If hyperglycemic, serum sodium levels can be falsely low due to the solute concentration and can be corrected by using the following equation: Corrected Sodium = [0.016 x (serum glucose 100)] + serum Na Isosomotic (280-285 mOsm) hyponatremia can result from isotonic infusion of solutions such as mannitol, without transcellular water shifts. A state of pseudohyponatremia can result from hypertriglyceridemia or hyperproteinemia, which can also give falsely low serum sodium levels and can be corrected with the following equation: Corrected Sodium = . Serum Na x 93 . 99 1.03 (triglyceride gm/L) 0.73 (protein gm/L) Treatment for both isosmotic and hyperosmotic hyponatremia is to treat the underlying cause, which will subsequently correct the sodium imbalance. In hypoosmotic (< 280 mOsm) hyponatremia, determining the volume status of the patient enables one to determine the etiology of the sodium imbalance. Determining volume status is derived
from a constellation of physical exam and laboratory findings, which include but are not limited to: orthostasis, pulse, pulmonary edema, peripheral edema in dependant areas of the body, moisture of oropharynx, and laboratory levels of BUN and creatinine, along with their ratio. If the patient is hypervolemic, the hyponatremia usually results from problems with renal excretion of water and subsequent fluid overload. Nephrotic syndrome, cirrhosis, congestive heart failure and renal failure are the primary disorders that comprise this category. Water restriction and close monitoring of sodium levels are recommended. Occasionally, a diuretic is required in the hypervolemic patient to improve water balance more quickly. If the patient is isovolemic and the urine Na is < 10, the primary cause is excessive water ingestion, with the obvious treatment of water restriction. When urine Na is > 20, causes typically include thiazide use, hypothyroidism, adrenal insufficiency, postoperative state, pain, severe nausea, HIV, positive pressure ventilation and SIADH. The latter syndrome results from retention of water due to excess ADH and the subsequent volume expansion. There are many potential sources for the excess of ADH, including but not limited to neoplastic causes (often associated with oat cell tumors), CNS insults effecting hypothalamic osmoreceptors, pulmonary disease and drugs (tricyclics, SSRIs, phenothiazines, opiates, chlorpropamide, antineoplastics such as vincristine and cyclophosphamide, and related hormones oxytocin and desmopressin). Treatment for SIADH is water restriction (~ 1 L / day). Resistant cases may require democlocycline or lithium. In the hypovolemic patient, renal sodium loss can result from diuretic use, adrenal insufficiency, osmotic diuresis, RTA or salt wasting nephropathies. Extrarenal sodium losses are typically from the gastrointestinal tract, skin or lungs. In these instances, treatment requires infusion of isotonic saline with close monitoring of sodium levels. Once the patient becomes euvolemic, their hyponatremia often resolves. Treatment The fear of correcting hyponatremia too quickly can have profound neurologic consequences, including central pontine myelinolysis and death. Treatment is controversial, but changes in plasma sodium levels should not exceed 8-12 mmol/L over the first 24 hours. Furosemide may be given concomitantly with isotonic saline so as to maintain a euvolemic state
48
and preventing intravascular overload. In very symptomatic cases (seizures or coma), hypertonic saline can be used to correct the hyponatremia more quickly. The same equation used in hypernatremia can be used in hyponatremia. By using the following formula, the effect of a change in serum sodium with one liter of infusate is calculated, then extrapolated to how many liters are required to achieve the desired net change. Change in serum sodium = Infusate Na Serum Na of patient Total body water + 1 Infusate Na = 154 513 855 0.9% NaCl in H20 3% NaCl in H20 5% NaCl in H20
Total Body Water = 0.6 x weight (kg) for males 0.5 x weight (kg) for females 0.5 x weight (kg) for elderly males 0.45 x weight (kg) for elderly females References 1. Adrogue HJ, Madias NE. Hypernatremia. N Engl J Med 2000; 342:20, 1493-1499 2. Adrogue HJ, Madias NE. Hyponatremia. N Engl J Med 2000; 342; 21, 1581-1589 3. Singer GG, Brenner BM. Fluid and Electrolyte Disturbances. In: Fauci AS et al, editors. Harrisons Principles of Internal Medicine.14th ed. New York: McGraw Hill, Inc;1998. p265-277. 4. Szerlip H, Pavelsky PM, Cox M. Disorders of Volume and Tonicity in the Surgical Patient. In: Goldman DR et al, editors. Perioperative Medicine. 2nd ed. McGraw Hill, Inc;1994. p591-605.
49
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Screening: of Litsea Salicifolia (Dighloti) As A Mosquito RepellentDocumento20 pagineScreening: of Litsea Salicifolia (Dighloti) As A Mosquito RepellentMarmish DebbarmaNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Tan vs. Macapagal, 43 SCRADocumento6 pagineTan vs. Macapagal, 43 SCRANikkaDoriaNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Tugas 3Documento20 pagineTugas 3dellaayuNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- TugasFilsS32019.AnthoniSulthanHarahap.450326 (Pencegahan Misconduct)Documento7 pagineTugasFilsS32019.AnthoniSulthanHarahap.450326 (Pencegahan Misconduct)Anthoni SulthanNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Business Administration: Hints TipsDocumento11 pagineBusiness Administration: Hints Tipsboca ratonNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Rubrics For Field Trip 1 Reflective DiaryDocumento2 pagineRubrics For Field Trip 1 Reflective DiarycrystalNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- 10-C# Forms InteractionDocumento22 pagine10-C# Forms InteractionMaria Anndrea MendozaNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grade 3Documento4 pagineGrade 3Shai HusseinNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Coronally Advanced Flap With Connective Tissue GraDocumento13 pagineCoronally Advanced Flap With Connective Tissue GrasutriNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- 2,3,5 Aqidah Dan QHDocumento5 pagine2,3,5 Aqidah Dan QHBang PaingNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Sample Questions 2019Documento21 pagineSample Questions 2019kimwell samson100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Site Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerDocumento95 pagineSite Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerKodhamagulla SudheerNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- E 05-03-2022 Power Interruption Schedule FullDocumento22 pagineE 05-03-2022 Power Interruption Schedule FullAda Derana100% (2)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Key Performance IndicatorsDocumento15 pagineKey Performance IndicatorsAbdul HafeezNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- CN and OS Lab ManualDocumento53 pagineCN and OS Lab Manualsudheer mangalampalliNessuna valutazione finora
- Average Waves in Unprotected Waters by Anne Tyler - Summary PDFDocumento1 paginaAverage Waves in Unprotected Waters by Anne Tyler - Summary PDFRK PADHI0% (1)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- MOtivating Your Teenager PDFDocumento66 pagineMOtivating Your Teenager PDFElleMichelle100% (1)
- Data Science Online Workshop Data Science vs. Data AnalyticsDocumento1 paginaData Science Online Workshop Data Science vs. Data AnalyticsGaurav VarshneyNessuna valutazione finora
- German Monograph For CannabisDocumento7 pagineGerman Monograph For CannabisAngel Cvetanov100% (1)
- Em 1.4 RMDocumento18 pagineEm 1.4 RMMangam RajkumarNessuna valutazione finora
- "We Like": Rohit Kiran KeluskarDocumento43 pagine"We Like": Rohit Kiran Keluskarrohit keluskarNessuna valutazione finora
- Crime Scene Manual FullDocumento19 pagineCrime Scene Manual FullMuhammed MUZZAMMILNessuna valutazione finora
- Digital Sytems Counters and Registers: Dce DceDocumento17 pagineDigital Sytems Counters and Registers: Dce DcePhan Gia AnhNessuna valutazione finora
- Ar 2003Documento187 pagineAr 2003Alberto ArrietaNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Contract of PledgeDocumento4 pagineContract of Pledgeshreya patilNessuna valutazione finora
- Multiple Linear RegressionDocumento26 pagineMultiple Linear RegressionMarlene G Padigos100% (2)
- Oldham Rules V3Documento12 pagineOldham Rules V3DarthFooNessuna valutazione finora
- Reported Speech Step by Step Step 7 Reported QuestionsDocumento4 pagineReported Speech Step by Step Step 7 Reported QuestionsDaniela TorresNessuna valutazione finora
- Kami Export - Document PDFDocumento2 pagineKami Export - Document PDFapi-296608066Nessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- HRM and The Business EnvironmentDocumento18 pagineHRM and The Business Environmentsuzzette91Nessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)