Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cardiac Muscle Properties
Caricato da
Surpreet AroraCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cardiac Muscle Properties
Caricato da
Surpreet AroraCopyright:
Formati disponibili
Physiology Exam 3 Electrical & Mechanical Properties of Cardiac Muscle Blood Flow Deoxygenated Blood o Superior & inferior
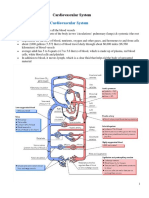
r vena cava o Right Atrium o Tricuspid (Right AV) Valve o Right Ventricle o Pulmonary valve o Right & left pulmonary arteries o Lungs Oxygenated Blood o Lungs o Right & Left Pulmonary Veins o Left Atrium o Mitral (Left AV) Valve o Left Ventricle o Aortic Valve o Aorta o Systemic Circulation Valves o Most blood flows passively into ventricle occurs when atrial pressure > ventricular pressure Tricuspid valve is open & ventricles relaxed o When ventricular pressure > atrial pressure - AV valve will close o Opening & closing of valves depends on the pressure gradient across the valve o There are no valves between the veins & atria Pulmonary Circulation low pressure, low resistance Systemic Circulation high pressure, high resistance o Left ventricle wall is much thicker & stronger organ systems are arranged in parallel o allows body to shut off flow to one area & divert blood to another area o this would not be possible if organ systems blood flow was in series
Cardiac Muscle Characteristics o Striated o Many mitochondria more than skeletal muscle o Intercalated discs adjacent cardiac cells are joined end-to-end Contain gap junctions allows each chamber to function as a single unit (functional syncytium) by allowing the spread of AP And desmosomes holds cells together, can withstand mechanical stress Cardiac cells exhibit autorhythmicity can generate AP on their own allows some cells to become pacemakers Cardiac muscle RMP is closer to -90 mV less Na+ leakage & greater [K+] Properties of Cardiac Muscle Excitability Ability to generate & respond to an action potential
Physiology Exam 3 3 types of cardiac tissues all 3 exhibit excitability to some degree o nodal tissue SA node is primary pacemaker o Purkinje fibers (bundle fibers) o Muscle only exhibits autorythmicity if other tissues arent working properly
Stages of AP o Most of AP myocardial fiber in absolute refractory cannot generate/respond to AP o Relative refractory period o Superexcitatory All-or-None o Applies to a single myocardial fiber either contract or not at all o Can be extended to the entire heart Functional syncytium intercalated discs allow transmission of AP When one fiber generates an AP, depolarization spreads rapidly over entire heart All-or-none refers to ability of all cardiac muscle to contract to a stimulus @ one point or not at all Mechanical behavior of fiber is determined prior to contraction o Resting length o Inotropic state o Each fiber does not always contract maximally when stimulated Rhythmicity autoexcitability cardiac muscle can initiate its own contraction Pacemaker potential o Cardiac muscle undergoes gradual depolarization until threshold is reached AP initiated repolarization gradual depolarization o Due to gradual reduction in K+ conductance (less movement outward) OR a gradual increase in Ca2+ conductance (inward current) o Nodal RMP ~ 60 mV (oscillating RMP) Due to Ca2+ voltage-gated channels ([Ca2+]out > [Ca2+]in) L-type channels long lasting; depolarization phase T-type channels transient; open only a short time; gradual depolarizations (oscillations) Na+ does not play a role Frequencies of Autorhythmicity o SA Node = 70-80 beats/min o AV Node = 40-60 beats/min o Purkinje Fibers = 15-40 beats/min Primary Pacemaker o Normally atrial & ventricular muscle does not exhibit autorhymicity o Overall rhythmicity of heart established by the SA Node (it has the highest rhythmic rate) o Whatever node has the highest frequency will become primary pacemaker (if not SA Node called ectopic focus) Chronotropy o Change in heart rate o Positive chronotropy increase heart rate Higher temperature Atropine epinepherine Sympathetic stimulation o Negative Chronotropy decreased heart rate Hypothermia Parasympathetic stimulation
Physiology Exam 3 ACh Beta-adrenergic block
Conductivity ability to conduct an AP & how fast conduction occurs Varying degrees on conductivity o Fastest Purkinje fibers (2-4 m/sec) o Slowest Junctional tissue (.02-.05 m/sec) b/t Atria & Ventricles; allows for AV Nodal Delay (ventricular filling) Separates atrial & ventricular systole Dhromotrophy o Speed of conduction o Positive dhromotropy increased rate of conductivity Sympathetic stimulation o Negative dhromotropy decreased rate of conductivity Parasympathetic (vagal) stimulation quinidine Compliance describes elasticity change in dimension w/ respect to a change in stress (force/unit area) applies to both heart & lungs Extensibility ability of a body to extend o x/F = change in distance change in force o 2-deminsional o applies to muscle strips Distensibility ability of a hollow object to distend due to an increase in internal pressure fractional change in volume per unit change in pressure o % V/P o 3-deminsional measurement accounts for original size o applies to cardiac chambers non-compliant large change in pressure causes a small change in volume compliant small change in pressure causes large change in volume Contractibility increasing the strength of contraction ability to shorten/develop tension Cardiac muscle can increase force in 2 ways: (cannot occur simultaneously) o Heterometric Autoregulation Frank-Starling Law More stretch = stronger strength of contraction Resting length of cardiac muscle is NOT optimal length (unlike skeletal muscle) End diastolic volume determines amount of stretch Venous return determines EDV Stroke volume = volume of blood ejected w/ each contraction Starlings Law = venous return = EDV = stretch & contraction = stroke volume Never due to contractility
Physiology Exam 3 o Homeometric Autoregulation Inotropic State Do not vary the length of muscle Inotropic agents cause change in myocardial contractility Positive inotropic agent increase in force of contraction from the same or small EDV or fiber length o Increase [Ca2+]in o NE, digitalis, increased extracellular Ca2+ Negative inotropic agent o Decrease [Ca2+]in o Increased extracellular Na+, quinidine, Ca2+ channel blockers Contractility increase in contractile force independent of fiber length Contractility = [Ca2+]out / [Na+]3out Receptors Adrenergic 1 increase HR & contractility Muscarinic decrease HR Steps Catecholamine binds to 1 receptor Adenylyl cyclase increase cAMP Activates cAMP protein kinase (PK) Phosporylates L-type Ca2+ channel in sarcolemma (prolongs opening) Trigger Ca-Induced Ca release from SR Must have extracellular Ca2+ for heart muscle to contract Na-Ca exchanger Antiport (secondary active transport) 1 Ca out for every 3 Na in (down concentration gradient) Ex: increase extracellular [Na+] o Activates Na-Ca exchanger more Na into cell o ( - ) inotropic effect o smaller contraction Ex: glycosides inhibit Na-K pump o Increase in intracellular [Na+] o Less active Na-Ca exchanger o Increase in intracellular [Ca2+] o (+) inotropic effect o stronger contraction
Potrebbero piacerti anche
- Cardiac DisordersDocumento15 pagineCardiac Disordersgold_enriquez100% (3)
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Da EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Nessuna valutazione finora
- Cardiovascular SystemDocumento58 pagineCardiovascular Systemabromley100% (2)
- Cadiac Cycle, Heart Sound, ECG, HypertensionDocumento110 pagineCadiac Cycle, Heart Sound, ECG, HypertensionNilesh100% (1)
- ECG Guide: Anatomy, Physiology, Interpretation and AbnormalitiesDocumento102 pagineECG Guide: Anatomy, Physiology, Interpretation and AbnormalitiesMustafa A. DawoodNessuna valutazione finora
- EKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasDa EverandEKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasValutazione: 3 su 5 stelle3/5 (5)
- Natalya Master CardioDocumento71 pagineNatalya Master CardioTaman Hoang100% (1)
- 05 Cardiovascular System PhysiologyDocumento34 pagine05 Cardiovascular System PhysiologyKaye Alyssa EnriquezNessuna valutazione finora
- 1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Documento73 pagine1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Sezanur Taalaibek kyzyNessuna valutazione finora
- CVS Physiology of HeartDocumento74 pagineCVS Physiology of HeartHEMACHANDRAN G (RA1821002010077)100% (2)
- NCM 103-Cardio Anatomy & PhysioDocumento56 pagineNCM 103-Cardio Anatomy & Physiolouradel100% (1)
- Cardiovascular Physiology:: Circuitry, Hemodynamics, ElectrophysiologyDocumento27 pagineCardiovascular Physiology:: Circuitry, Hemodynamics, Electrophysiologyrsmoney3Nessuna valutazione finora
- Lecture - 3 Properties of Cardiac MuscleDocumento35 pagineLecture - 3 Properties of Cardiac MuscleMRM7MDNessuna valutazione finora
- CVS PhysiologyDocumento43 pagineCVS Physiologyapi-3705050100% (1)
- Anatomi Dan Fisiologi GinjalDocumento32 pagineAnatomi Dan Fisiologi GinjalAlamul Huda100% (1)
- 03 Cardiopulmonary PhysiologyDocumento17 pagine03 Cardiopulmonary Physiologyice cream1000791100% (1)
- Physiology of The HeartDocumento34 paginePhysiology of The Heartalyssa_marie_keNessuna valutazione finora
- ECG Guide: Everything You Need to Know About ElectrocardiogramsDocumento72 pagineECG Guide: Everything You Need to Know About ElectrocardiogramsGaras AnnaBerniceNessuna valutazione finora
- Or Cardiac Physiology, Pathophysiology, and Some PharmacologyDocumento58 pagineOr Cardiac Physiology, Pathophysiology, and Some PharmacologyJacob StoneNessuna valutazione finora
- Life's Progression Through Cardiac PhysiologyDocumento91 pagineLife's Progression Through Cardiac PhysiologyprofcarleyNessuna valutazione finora
- 2015A&PIntro CardiovascularHandoutDocumento16 pagine2015A&PIntro CardiovascularHandoutMaggieHameedNessuna valutazione finora
- Cardio AssessmentDocumento104 pagineCardio Assessmentlowell.cerezo.ihsNessuna valutazione finora
- Cardiac Cycle and Myogenic Control of HeartbeatDocumento25 pagineCardiac Cycle and Myogenic Control of HeartbeatFiona HennahNessuna valutazione finora
- Anatomy & Physiology Training OverviewDocumento50 pagineAnatomy & Physiology Training OverviewAlisa BrownNessuna valutazione finora
- Biochemistry of the Heart and Blood Vessels 2021 3 4Documento44 pagineBiochemistry of the Heart and Blood Vessels 2021 3 4jakukNessuna valutazione finora
- Cardiovascular SystemDocumento40 pagineCardiovascular SystemHeidi MobarakNessuna valutazione finora
- Cardiac Muscles and Conducting System of HeartDocumento37 pagineCardiac Muscles and Conducting System of HeartwalterNessuna valutazione finora
- Circulation WorksheetDocumento3 pagineCirculation Worksheetholagato100% (1)
- No VideoDocumento47 pagineNo VideoTimothy John BautistaNessuna valutazione finora
- Trinity CVS Lecture 1-ECG 12.13.Ppt (Read-Only)Documento24 pagineTrinity CVS Lecture 1-ECG 12.13.Ppt (Read-Only)cystanarisaNessuna valutazione finora
- Cardiac Muscle2Documento39 pagineCardiac Muscle2Darius GanNessuna valutazione finora
- Functional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionDocumento186 pagineFunctional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionBery Agana F. PurbaNessuna valutazione finora
- Prof DR Najneen AkhterDocumento62 pagineProf DR Najneen Akhterislamamirul0487Nessuna valutazione finora
- Blood PressureDocumento22 pagineBlood Pressurenaresh sharmaNessuna valutazione finora
- Read 1 CVS OrgDocumento34 pagineRead 1 CVS OrgEzeudu SomtoNessuna valutazione finora
- Cardiac Arrest: April B. Perez, RN, Man, PHD, FpchaDocumento50 pagineCardiac Arrest: April B. Perez, RN, Man, PHD, Fpchayuuki konnoNessuna valutazione finora
- Cardiovascular Physiology: Cardiac Muscle, Rhythm, Cycle & OutputDocumento26 pagineCardiovascular Physiology: Cardiac Muscle, Rhythm, Cycle & OutputPhai KoemhienNessuna valutazione finora
- PHY3171 Lecture 1Documento6 paginePHY3171 Lecture 1PatrickNessuna valutazione finora
- CardiovascularDocumento40 pagineCardiovascularÁñèsh Kåøs100% (1)
- Circulatory SystemDocumento56 pagineCirculatory SystemillyaniNessuna valutazione finora
- Physiology DES Explains Organ Blood Flow & ExceptionsDocumento56 paginePhysiology DES Explains Organ Blood Flow & ExceptionsJoseph KimNessuna valutazione finora
- The Circulatory System: The Heart, Blood Vessels, Blood TypesDocumento51 pagineThe Circulatory System: The Heart, Blood Vessels, Blood Typescut irnandaNessuna valutazione finora
- CCN Cardio Upd.Documento209 pagineCCN Cardio Upd.Kimberly SungaNessuna valutazione finora
- The Circulatory System: The Heart, Blood Vessels, Blood TypesDocumento51 pagineThe Circulatory System: The Heart, Blood Vessels, Blood Typesghisma ocvintiaNessuna valutazione finora
- Disrythmia Recognition ACLS ASHIDocumento127 pagineDisrythmia Recognition ACLS ASHIJulisa FernandezNessuna valutazione finora
- Cardiovascular Physiology 1Documento44 pagineCardiovascular Physiology 1maxmus4Nessuna valutazione finora
- Lab 5 Cardiovascular Examination, ECG and BPDocumento43 pagineLab 5 Cardiovascular Examination, ECG and BP202310446Nessuna valutazione finora
- The Circulatory System ExplainedDocumento51 pagineThe Circulatory System ExplainedJonalynCollodChewacheoNessuna valutazione finora
- Cardiac MuscleDocumento39 pagineCardiac MuscleAndhini Virgiannisa100% (2)
- Cardiovascular System TamreedDocumento8 pagineCardiovascular System TamreedslmylwkaaNessuna valutazione finora
- Cardiovascular Physiology Lecture 1Documento95 pagineCardiovascular Physiology Lecture 1Freelance LeagueNessuna valutazione finora
- Lecture5 - Electrocardiogram Electromyogram - 1Documento33 pagineLecture5 - Electrocardiogram Electromyogram - 1AbdullahNessuna valutazione finora
- Physiology of the Heart FunctionsDocumento26 paginePhysiology of the Heart FunctionsぴよんNessuna valutazione finora
- Cardiovascular System: Unit 3 Slide 1Documento79 pagineCardiovascular System: Unit 3 Slide 1Nestor BalboaNessuna valutazione finora
- Circulatory System: Heart, Blood Vessels & TypesDocumento51 pagineCirculatory System: Heart, Blood Vessels & TypesTina TalmadgeNessuna valutazione finora
- N5sampleDocumento12 pagineN5sampleshaikhbakhtiyar3669Nessuna valutazione finora
- 2-Cardiac Electical ActivityDocumento26 pagine2-Cardiac Electical ActivityhalayehiahNessuna valutazione finora
- Components of The Cardiovascular SystemDocumento23 pagineComponents of The Cardiovascular SystemMr. DummyNessuna valutazione finora
- 10 General Anatomy of The Cardiovascular SystemDocumento140 pagine10 General Anatomy of The Cardiovascular SystemSuzana VoiculescuNessuna valutazione finora
- Cardiac Anatomy and Physiology: Iris Ken R. Rico, OTRPDocumento90 pagineCardiac Anatomy and Physiology: Iris Ken R. Rico, OTRPAndra HijratulNessuna valutazione finora
- Test 1 ReviewDocumento5 pagineTest 1 ReviewSurpreet AroraNessuna valutazione finora
- Medical Emergency CE Current HODocumento173 pagineMedical Emergency CE Current HOSurpreet AroraNessuna valutazione finora
- Bacteria GroupsDocumento3 pagineBacteria GroupsSurpreet AroraNessuna valutazione finora
- Gross Anatomy Board ReviewDocumento1 paginaGross Anatomy Board ReviewSurpreet AroraNessuna valutazione finora
- Skeletal Muscle Auto Saved)Documento8 pagineSkeletal Muscle Auto Saved)Surpreet AroraNessuna valutazione finora
- Nasal Obstruction and Facial Growth: The Strength of Evidence For Clinical AssumptionsDocumento9 pagineNasal Obstruction and Facial Growth: The Strength of Evidence For Clinical AssumptionsSurpreet AroraNessuna valutazione finora
- BirdbrainDocumento1 paginaBirdbrainplastoneNessuna valutazione finora
- BirdbrainDocumento1 paginaBirdbrainplastoneNessuna valutazione finora
- Chapter 1Documento2 pagineChapter 1Surpreet AroraNessuna valutazione finora
- Immuno Missed LectureDocumento2 pagineImmuno Missed LectureSurpreet AroraNessuna valutazione finora
- J. Nutr.-2010-Kalupahana-1915-22Documento8 pagineJ. Nutr.-2010-Kalupahana-1915-22Surpreet AroraNessuna valutazione finora
- UNMcatalogueDocumento668 pagineUNMcatalogueSurpreet AroraNessuna valutazione finora
- Vitamin Chart 2009Documento1 paginaVitamin Chart 2009Surpreet AroraNessuna valutazione finora
- This Content Downloaded From 193.52.209.134 On Wed, 08 Dec 2021 14:53:17 UTCDocumento3 pagineThis Content Downloaded From 193.52.209.134 On Wed, 08 Dec 2021 14:53:17 UTCAONessuna valutazione finora
- The Normal Kidney: Pediatrics 2 The Urinary System and Urinary Tract InfectionsDocumento4 pagineThe Normal Kidney: Pediatrics 2 The Urinary System and Urinary Tract Infectionssarguss14Nessuna valutazione finora
- Biology Reviewer PrelimsDocumento10 pagineBiology Reviewer PrelimsShaira CogollodoNessuna valutazione finora
- Blok 10 03.11.2017Documento174 pagineBlok 10 03.11.2017VaniaNessuna valutazione finora
- Uddin Et Al., 2022Documento4 pagineUddin Et Al., 2022James BondNessuna valutazione finora
- Revision Eye and BrainDocumento8 pagineRevision Eye and BrainEllie AbelNessuna valutazione finora
- What Are Spinal Tracts?Documento2 pagineWhat Are Spinal Tracts?Ahsan JamilNessuna valutazione finora
- Anatomical Position: - Other Body PositionsDocumento21 pagineAnatomical Position: - Other Body PositionsBeaune V. VillarazaNessuna valutazione finora
- BODY TISSUES Reviewer 3Documento3 pagineBODY TISSUES Reviewer 3Jaira EmmarinaNessuna valutazione finora
- Chapter 41 - Animal NutritionDocumento7 pagineChapter 41 - Animal Nutritionliennev02Nessuna valutazione finora
- Metabolism in Liver Kidney and PlacentaDocumento22 pagineMetabolism in Liver Kidney and PlacentaBikash SahNessuna valutazione finora
- Histology: Ust Faculty of Medicine and Surgery Class of 2016Documento14 pagineHistology: Ust Faculty of Medicine and Surgery Class of 2016Ashley Beatriz PascualNessuna valutazione finora
- Chapter 14Documento17 pagineChapter 14Fathimath AliNessuna valutazione finora
- Control and Coordination: One Mark QuestionsDocumento7 pagineControl and Coordination: One Mark QuestionsJillianne JillNessuna valutazione finora
- Syllab BSC Rgit1819-22102018Documento36 pagineSyllab BSC Rgit1819-22102018mujahedul islamNessuna valutazione finora
- AUBF Chapter 3-ReviewerDocumento4 pagineAUBF Chapter 3-ReviewerSalvani, Shane JudeNessuna valutazione finora
- Anatomy & PhysiologyDocumento80 pagineAnatomy & Physiologydr amjadNessuna valutazione finora
- Selaginella Morphology and AnatomyDocumento30 pagineSelaginella Morphology and AnatomyD K SRIVASTAVANessuna valutazione finora
- Anatomy and PhysiologyDocumento13 pagineAnatomy and PhysiologyernestoNessuna valutazione finora
- Imj 13707Documento11 pagineImj 13707Santiago López JosueNessuna valutazione finora
- Red Blood Cell Phenotyping of Blood Donors in Islamabad, PakistanDocumento5 pagineRed Blood Cell Phenotyping of Blood Donors in Islamabad, PakistanAHNS123Nessuna valutazione finora
- Musculoskeletal System Anatomy and Physiology:-: Dr. Hussein Hadi AtiyahDocumento43 pagineMusculoskeletal System Anatomy and Physiology:-: Dr. Hussein Hadi AtiyahAli FalihNessuna valutazione finora
- Digestion and Absorption: Anatomy and Functions of the Human Digestive SystemDocumento8 pagineDigestion and Absorption: Anatomy and Functions of the Human Digestive Systemzwindows123456789Nessuna valutazione finora
- General Expressions in Medical DiagnosisDocumento6 pagineGeneral Expressions in Medical DiagnosisSergej ElekNessuna valutazione finora
- Gastrointestinal - Mucosal.repair - And.experimental - Therapeutics Ublog - TKDocumento261 pagineGastrointestinal - Mucosal.repair - And.experimental - Therapeutics Ublog - TKpotaiskiNessuna valutazione finora
- Pathophysiologic Evidence of The Osteopathic LesionDocumento5 paginePathophysiologic Evidence of The Osteopathic LesionTariq J FaridiNessuna valutazione finora
- Physiology of Milk ProductionDocumento22 paginePhysiology of Milk ProductionRajeev NepalNessuna valutazione finora
- Cardiac - Anatomy of The HeartDocumento9 pagineCardiac - Anatomy of The HeartRiya ThoratNessuna valutazione finora
- Pollen DevelopmentDocumento33 paginePollen DevelopmentAshish ChoudharyNessuna valutazione finora